Prior Authorization Guidelines - Group Health Cooperative of Eau ...
Prior Authorization Guidelines - Group Health Cooperative of Eau ...
Prior Authorization Guidelines - Group Health Cooperative of Eau ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
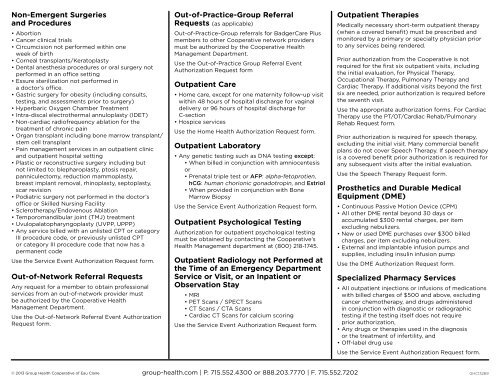
Non-Emergent Surgeries<br />
and Procedures<br />
• Abortion<br />
• Cancer clinical trials<br />
• Circumcision not performed within one<br />
week <strong>of</strong> birth<br />
• Corneal transplants/Keratoplasty<br />
• Dental anesthesia procedures or oral surgery not<br />
performed in an <strong>of</strong>fice setting<br />
• Essure sterilization not performed in<br />
a doctor’s <strong>of</strong>fice.<br />
• Gastric surgery for obesity (including consults,<br />
testing, and assessments prior to surgery)<br />
• Hyperbaric Oxygen Chamber Treatment<br />
• Intra-discal electrothermal annuloplasty (IDET)<br />
• Non-cardiac radi<strong>of</strong>requency ablation for the<br />
treatment <strong>of</strong> chronic pain<br />
• Organ transplant including bone marrow transplant/<br />
stem cell transplant<br />
• Pain management services in an outpatient clinic<br />
and outpatient hospital setting<br />
• Plastic or reconstructive surgery including but<br />
not limited to: blepharoplasty, ptosis repair,<br />
panniculectomy, reduction mammoplasty,<br />
breast implant removal, rhinoplasty, septoplasty,<br />
scar revision<br />
• Podiatric surgery not performed in the doctor’s<br />
<strong>of</strong>fice or Skilled Nursing Facility<br />
• Sclerotherapy/Endovenous Ablation<br />
• Temporomandibular joint (TMJ) treatment<br />
• Uvulopalatopharyngoplasty (UVPP, UPPP)<br />
• Any service billed with an unlisted CPT or category<br />
III procedure code, or previously unlisted CPT<br />
or category III procedure code that now has a<br />
permanent code<br />
Use the Service Event <strong>Authorization</strong> Request form.<br />
Out-<strong>of</strong>-Network Referral Requests<br />
Any request for a member to obtain pr<strong>of</strong>essional<br />
services from an out-<strong>of</strong>-network provider must<br />
be authorized by the <strong>Cooperative</strong> <strong>Health</strong><br />
Management Department.<br />
Use the Out-<strong>of</strong>-Network Referral Event <strong>Authorization</strong><br />
Request form.<br />
Out-<strong>of</strong>-Practice-<strong>Group</strong> Referral<br />
Requests (as applicable)<br />
Out-<strong>of</strong>-Practice-<strong>Group</strong> referrals for BadgerCare Plus<br />
members to other <strong>Cooperative</strong> network providers<br />
must be authorized by the <strong>Cooperative</strong> <strong>Health</strong><br />
Management Department.<br />
Use the Out-<strong>of</strong>-Practice <strong>Group</strong> Referral Event<br />
<strong>Authorization</strong> Request form<br />
Outpatient Care<br />
• Home care, except for one maternity follow-up visit<br />
within 48 hours <strong>of</strong> hospital discharge for vaginal<br />
delivery or 96 hours <strong>of</strong> hospital discharge for<br />
C-section<br />
• Hospice services<br />
Use the Home <strong>Health</strong> <strong>Authorization</strong> Request form.<br />
Outpatient Laboratory<br />
• Any genetic testing such as DNA testing except:<br />
• When billed in conjunction with amniocentesis<br />
or<br />
• Prenatal triple test or AFP: alpha-fetoprotien,<br />
hCG: human chorionic gonadotropin, and Estriol<br />
• When provided in conjunction with Bone<br />
Marrow Biopsy<br />
Use the Service Event <strong>Authorization</strong> Request form.<br />
Outpatient Psychological Testing<br />
<strong>Authorization</strong> for outpatient psychological testing<br />
must be obtained by contacting the <strong>Cooperative</strong>’s<br />
<strong>Health</strong> Management department at (800) 218-1745.<br />
Outpatient Radiology not Performed at<br />
the Time <strong>of</strong> an Emergency Department<br />
Service or Visit, or an Inpatient or<br />
Observation Stay<br />
• MRI<br />
• PET Scans / SPECT Scans<br />
• CT Scans / CTA Scans<br />
• Cardiac CT Scans for calcium scoring<br />
Use the Service Event <strong>Authorization</strong> Request form.<br />
Outpatient Therapies<br />
Medically necessary short-term outpatient therapy<br />
(when a covered benefit) must be prescribed and<br />
monitored by a primary or specialty physician prior<br />
to any services being rendered.<br />
<strong>Prior</strong> authorization from the <strong>Cooperative</strong> is not<br />
required for the first six outpatient visits, including<br />
the initial evaluation, for Physical Therapy,<br />
Occupational Therapy, Pulmonary Therapy and<br />
Cardiac Therapy. If additional visits beyond the first<br />
six are needed, prior authorization is required before<br />
the seventh visit.<br />
Use the appropriate authorization forms. For Cardiac<br />
Therapy use the PT/OT/Cardiac Rehab/Pulmonary<br />
Rehab Request form.<br />
<strong>Prior</strong> authorization is required for speech therapy,<br />
excluding the initial visit. Many commercial benefit<br />
plans do not cover Speech Therapy. If speech therapy<br />
is a covered benefit prior authorization is required for<br />
any subsequent visits after the initial evaluation.<br />
Use the Speech Therapy Request form.<br />
Prosthetics and Durable Medical<br />
Equipment (DME)<br />
• Continuous Passive Motion Device (CPM)<br />
• All other DME rental beyond 30 days or<br />
accumulated $300 rental charges, per item<br />
excluding nebulizers.<br />
• New or used DME purchases over $300 billed<br />
charges, per item excluding nebulizers.<br />
• External and implantable infusion pumps and<br />
supplies, including insulin infusion pump<br />
Use the DME <strong>Authorization</strong> Request form.<br />
Specialized Pharmacy Services<br />
• All outpatient injections or infusions <strong>of</strong> medications<br />
with billed charges <strong>of</strong> $500 and above, excluding<br />
cancer chemotherapy, and drugs administered<br />
in conjunction with diagnostic or radiographic<br />
testing if the testing itself does not require<br />
prior authorization,<br />
• Any drugs or therapies used in the diagnosis<br />
or the treatment <strong>of</strong> infertility, and<br />
• Off-label drug use<br />
Use the Service Event <strong>Authorization</strong> Request form.<br />
© 2013 <strong>Group</strong> <strong>Health</strong> <strong>Cooperative</strong> <strong>of</strong> <strong>Eau</strong> Claire<br />
group-health.com | P. 715.552.4300 or 888.203.7770 | F. 715.552.7202<br />
GHC13269