Induced Moderate Hypothermia After Cardiac Arrest - American ...
Induced Moderate Hypothermia After Cardiac Arrest - American ...
Induced Moderate Hypothermia After Cardiac Arrest - American ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
MCKEAN<br />
AACN Advanced Critical Care<br />
is beneficial only if the health care team knows<br />
how to care for this patient population. Nursing<br />
care and support is crucial. Patient management<br />
and the vital nursing care needed for this<br />
patient population are described below.<br />
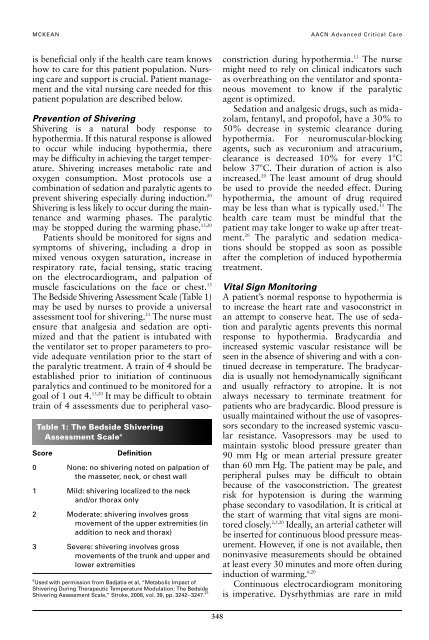
Table 1: The Bedside Shivering<br />
Assessment Scale a<br />
Score<br />
Definition<br />
0 None: no shivering noted on palpation of<br />
the masseter, neck, or chest wall<br />
1 Mild: shivering localized to the neck<br />
and/or thorax only<br />
2 <strong>Moderate</strong>: shivering involves gross<br />
movement of the upper extremities (in<br />
addition to neck and thorax)<br />
3 Severe: shivering involves gross<br />
movements of the trunk and upper and<br />
lower extremities<br />
a Used with permission from Badjatia et al, “Metabolic Impact of<br />
Shivering During Therapeutic Temperature Modulation: The Bedside<br />
Shivering Assessment Scale,” Stroke, 2008, vol. 39, pp. 3242--3247. 21<br />
Prevention of Shivering<br />
Shivering is a natural body response to<br />
hypothermia. If this natural response is allowed<br />
to occur while inducing hypothermia, there<br />
may be difficulty in achieving the target temperature.<br />
Shivering increases metabolic rate and<br />
oxygen consumption. Most protocols use a<br />
combination of sedation and paralytic agents to<br />
prevent shivering especially during induction. 20<br />
Shivering is less likely to occur during the maintenance<br />
and warming phases. The paralytic<br />
may be stopped during the warming phase. 13,20<br />
Patients should be monitored for signs and<br />
symptoms of shivering, including a drop in<br />
mixed venous oxygen saturation, increase in<br />
respiratory rate, facial tensing, static tracing<br />
on the electrocardiogram, and palpation of<br />
muscle fasciculations on the face or chest. 13<br />
The Bedside Shivering Assessment Scale (Table 1)<br />
may be used by nurses to provide a universal<br />
assessment tool for shivering. 21 The nurse must<br />
ensure that analgesia and sedation are optimized<br />
and that the patient is intubated with<br />
the ventilator set to proper parameters to provide<br />
adequate ventilation prior to the start of<br />
the paralytic treatment. A train of 4 should be<br />
established prior to initiation of continuous<br />
paralytics and continued to be monitored for a<br />
goal of 1 out 4. 13,20 It may be difficult to obtain<br />
train of 4 assessments due to peripheral vasoconstriction<br />
during hypothermia. 13 The nurse<br />
might need to rely on clinical indicators such<br />
as overbreathing on the ventilator and spontaneous<br />
movement to know if the paralytic<br />
agent is optimized.<br />
Sedation and analgesic drugs, such as midazolam,<br />
fentanyl, and propofol, have a 30% to<br />
50% decrease in systemic clearance during<br />
hypothermia. For neuromuscular-blocking<br />
agents, such as vecuronium and atracurium,<br />
clearance is decreased 10% for every 1C<br />
below 37C. Their duration of action is also<br />
increased. 20 The least amount of drug should<br />
be used to provide the needed effect. During<br />
hypothermia, the amount of drug required<br />
may be less than what is typically used. 13 The<br />
health care team must be mindful that the<br />
patient may take longer to wake up after treatment.<br />
20 The paralytic and sedation medications<br />
should be stopped as soon as possible<br />
after the completion of induced hypothermia<br />
treatment.<br />
Vital Sign Monitoring<br />
A patient’s normal response to hypothermia is<br />
to increase the heart rate and vasoconstrict in<br />
an attempt to conserve heat. The use of sedation<br />
and paralytic agents prevents this normal<br />
response to hypothermia. Bradycardia and<br />
increased systemic vascular resistance will be<br />
seen in the absence of shivering and with a continued<br />
decrease in temperature. The bradycardia<br />
is usually not hemodynamically significant<br />
and usually refractory to atropine. It is not<br />
always necessary to terminate treatment for<br />
patients who are bradycardic. Blood pressure is<br />
usually maintained without the use of vasopressors<br />
secondary to the increased systemic vascular<br />
resistance. Vasopressors may be used to<br />
maintain systolic blood pressure greater than<br />
90 mm Hg or mean arterial pressure greater<br />
than 60 mm Hg. The patient may be pale, and<br />
peripheral pulses may be difficult to obtain<br />
because of the vasoconstriction. The greatest<br />
risk for hypotension is during the warming<br />
phase secondary to vasodilation. It is critical at<br />
the start of warming that vital signs are monitored<br />
closely. 2,5,20 Ideally, an arterial catheter will<br />
be inserted for continuous blood pressure measurement.<br />
However, if one is not available, then<br />
noninvasive measurements should be obtained<br />
at least every 30 minutes and more often during<br />
induction of warming. 6,20<br />
Continuous electrocardiogram monitoring<br />
is imperative. Dysrhythmias are rare in mild<br />
348