Ritodrine and Isoxsuprine in Management of Preterm Labor
Ritodrine and Isoxsuprine in Management of Preterm Labor
Ritodrine and Isoxsuprine in Management of Preterm Labor
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Yogol et al. <strong>Ritodr<strong>in</strong>e</strong> <strong>and</strong> <strong>Isoxsupr<strong>in</strong>e</strong> <strong>in</strong> <strong>Management</strong> <strong>of</strong> <strong>Preterm</strong> <strong>Labor</strong><br />
agent, is associated with fewer maternal side effects. 3,4<br />
<strong>Isoxsupr<strong>in</strong>e</strong> is a slight selective ß 2 –adrenoreceptor tocolytic<br />
agent, whose use has been superseded by more selective<br />
ß 2 -agonists. 5,6 Studies have shown that <strong>Ritodr<strong>in</strong>e</strong> is more<br />
efficacious <strong>in</strong> arrest<strong>in</strong>g preterm labor, delay<strong>in</strong>g delivery<br />
<strong>and</strong> <strong>in</strong>creas<strong>in</strong>g fetal maturity than <strong>Isoxsupr<strong>in</strong>e</strong>. 6-8<br />
<strong>Isoxsupr<strong>in</strong>e</strong> is still used <strong>in</strong> develop<strong>in</strong>g countries due to<br />
its lower price. Though <strong>Ritodr<strong>in</strong>e</strong> is affordable to the<br />
patient it is comparatively expensive. The higher failure<br />
rate <strong>and</strong> the related consequences <strong>of</strong> <strong>Isoxsupr<strong>in</strong>e</strong> make<br />
treatment with <strong>Ritodr<strong>in</strong>e</strong> more cost effective. The failure<br />
<strong>of</strong> preterm labor management results <strong>in</strong> preterm birth or<br />
<strong>in</strong>fant mortality. <strong>Preterm</strong> birth accounts for 70% neonatal<br />
morbidity <strong>and</strong> <strong>in</strong>crease expenses on neonatal care. 9 Many<br />
studies have shown that <strong>Isoxsupr<strong>in</strong>e</strong> has not only caused<br />
<strong>in</strong>creased neonatal morbidity but also shows maternal<br />
<strong>and</strong> fetal side effects. 7-10<br />
METHODS<br />
The prospective observational study was conducted at<br />
Gynecology <strong>and</strong> Obstetric ward <strong>of</strong> Dhulikhel Kathm<strong>and</strong>u<br />
University Teach<strong>in</strong>g Hospital <strong>and</strong> Ante-neonatal Care Unit <strong>of</strong><br />
Maternity Hospital, Thapathali from January 2007 to June<br />
2007. This study was ethically approved by ethical review<br />
committee Kathm<strong>and</strong>u University, School <strong>of</strong> Medical Science.<br />
With <strong>in</strong>formed consent, a total <strong>of</strong> sixty-one pregnant women<br />
were <strong>in</strong>cluded <strong>in</strong> the study. The <strong>in</strong>clusion criteria were:<br />
nulliparous or multiparous ladies <strong>in</strong> between a gestational age<br />
<strong>of</strong> 28-36 weeks, bishops score less than or equal to six <strong>and</strong><br />
with symptoms <strong>and</strong> signs <strong>of</strong> preterm labor. The patients with<br />
cardiovascular disease or asthma or antepartum bleed<strong>in</strong>g were<br />
excluded from the study. Bishops score was assessed to<br />
confirm whether patient is <strong>in</strong> active stage <strong>of</strong> labor or not.<br />
S<strong>in</strong>ce Maternity Hospital at Thapathali <strong>and</strong> Dhulikhel Hospital<br />
have their own protocol for treatment <strong>of</strong> preterm labor, the<br />
patients were assigned accord<strong>in</strong>g to the treatment protocol<br />
<strong>of</strong> concerned hospitals. The subjects at Maternity Hospital,<br />
Thapathali (n=30) were treated with <strong>Isoxsupr<strong>in</strong>e</strong> 10mg every<br />
eight hours. The subjects at Dhulikhel Hospital (n=31) were<br />
treated with <strong>in</strong>travenous <strong>in</strong>fusion <strong>of</strong> <strong>Ritodr<strong>in</strong>e</strong> 10mg with<br />
dextrose 5% at the rate <strong>of</strong> ten drops per m<strong>in</strong>ute (50mcg/m<strong>in</strong>)<br />
<strong>and</strong> the drip rate was <strong>in</strong>creased by 5-10 drops every hour<br />
followed by oral adm<strong>in</strong>istration <strong>of</strong> 5-10mg <strong>Ritodr<strong>in</strong>e</strong> eight<br />
hourly depend<strong>in</strong>g on the severity <strong>of</strong> patient. Maternal pulse,<br />
blood pressure, fetal heart rate <strong>and</strong> uter<strong>in</strong>e contraction were<br />
monitored prior to drug adm<strong>in</strong>istration, then hourly for first<br />
six hours <strong>of</strong> <strong>in</strong>itial dos<strong>in</strong>g <strong>and</strong> then two hourly till the last<br />
dose. In case <strong>of</strong> the subject receiv<strong>in</strong>g <strong>in</strong>travenous <strong>in</strong>fusion <strong>of</strong><br />
<strong>Ritodr<strong>in</strong>e</strong>, the drip rate was adjusted if the pulse rate was<br />
more than 100 per m<strong>in</strong>ute. When there was no control <strong>in</strong><br />
labor pa<strong>in</strong> despite tocolytic therapy, the subjects were subjected<br />
to elective cesarean section.<br />
Basel<strong>in</strong>e evaluation <strong>in</strong>cluded height, weight, maternal age,<br />
socioeconomic status, literacy, gravidity, parity, gestational<br />
period, age at marriage, previous history <strong>of</strong> spontaneous<br />
abortion or preterm delivery, symptoms <strong>of</strong> ur<strong>in</strong>ary tract<br />
<strong>in</strong>fection, history <strong>of</strong> smok<strong>in</strong>g <strong>and</strong> alcohol consumption <strong>and</strong><br />
underly<strong>in</strong>g medical <strong>and</strong> obstetric disorders.<br />
The efficacy was predicted with dim<strong>in</strong>ution <strong>of</strong> abdom<strong>in</strong>al pa<strong>in</strong><br />
<strong>and</strong> backache with absence <strong>of</strong> vag<strong>in</strong>al discharge <strong>and</strong> uter<strong>in</strong>e<br />
contraction. The safety <strong>of</strong> drugs was assessed with abnormal<br />
fetal <strong>and</strong> maternal heart rate <strong>and</strong> maternal side effects. The<br />
total cost <strong>of</strong> management was calculated.<br />
Statistical analysis was done with SPSS version 11.5 data<br />
sheet. Pearson Chi Square test was used to compare efficacy,<br />
prolongation <strong>of</strong> pregnancy <strong>and</strong> adverse effects <strong>of</strong> drugs.<br />
Monitor<strong>in</strong>g parameters pre-<strong>and</strong> post- use <strong>of</strong> drug were compared<br />
by us<strong>in</strong>g paired sample t-test. Mean <strong>and</strong> median were used<br />
as statistical tools to compare cost <strong>of</strong> treatments.<br />
RESULTS<br />
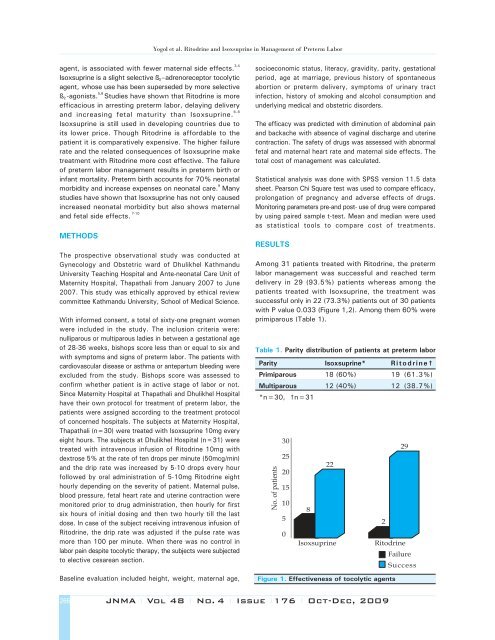
Among 31 patients treated with <strong>Ritodr<strong>in</strong>e</strong>, the preterm<br />
labor management was successful <strong>and</strong> reached term<br />
delivery <strong>in</strong> 29 (93.5%) patients whereas among the<br />
patients treated with <strong>Isoxsupr<strong>in</strong>e</strong>, the treatment was<br />
successful only <strong>in</strong> 22 (73.3%) patients out <strong>of</strong> 30 patients<br />
with P value 0.033 (Figure 1,2). Among them 60% were<br />
primiparous (Table 1).<br />
Table 1. Parity distribution <strong>of</strong> patients at preterm labor<br />
Parity <strong>Isoxsupr<strong>in</strong>e</strong>* <strong>Ritodr<strong>in</strong>e</strong>†<br />
Primiparous 18 (60%) 19 (61.3%)<br />
Multiparous 12 (40%) 12 (38.7%)<br />
*n=30, †n=31<br />
No. <strong>of</strong> patients<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
8<br />
22<br />
<strong>Isoxsupr<strong>in</strong>e</strong><br />
2<br />
29<br />
<strong>Ritodr<strong>in</strong>e</strong><br />
Figure 1. Effectiveness <strong>of</strong> tocolytic agents<br />
Failure<br />
Success<br />
266<br />
JNMA I Vol 48 I No. 4 I Issue I176 I Oct-Dec, 2009