Ovacome Summer 2014
Ovacome Summer 2014
Ovacome Summer 2014
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
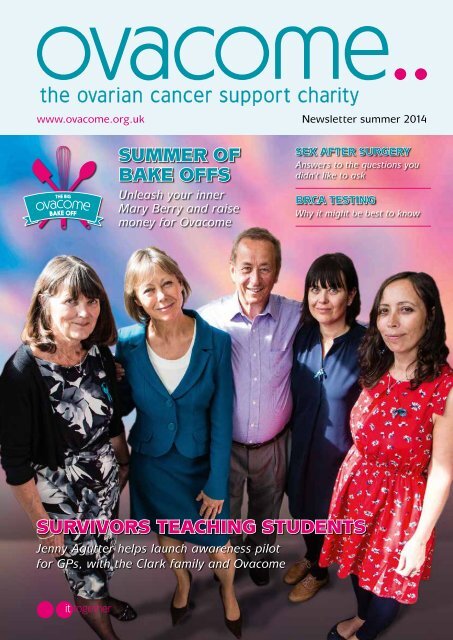
www.ovacome.org.uk Newsletter summer <strong>2014</strong><br />
SUMMER OF<br />
BAKE OFFS<br />
Unleash your inner<br />
Mary Berry and raise<br />
money for <strong>Ovacome</strong><br />
SEX AFTER SURGERY<br />
Answers to the questions you<br />
didn’t like to ask<br />
BRCA TESTING<br />
Why it might be best to know<br />
SURVIVORS TEACHING STUDENTS<br />
Jenny Agutter helps launch awareness pilot<br />
for GPs, with the Clark family and <strong>Ovacome</strong><br />
it together
comments<br />
contact <strong>Ovacome</strong><br />
Chief executive:<br />
Louise Bayne<br />
Support services nurse:<br />
Ruth Payne<br />
Susan Morgan-Walters<br />
Volunteer and<br />
information manager:<br />
Ruth Grigg<br />
Administrator:<br />
Sonia Vig<br />
Support line: 0845 371 0554<br />
020 7299 6650<br />
Email: support@ovacome.org.uk<br />
Administration line:<br />
020 7299 6654<br />
Email: ovacome@ovacome.org.uk<br />
Address: <strong>Ovacome</strong>,<br />
B5, City Cloisters, 196 Old Street,<br />
London EC1V 9FR<br />
Office hours:<br />
Monday to Friday 10am – 5pm.<br />
Follow <strong>Ovacome</strong><br />
on Twitter and Facebook<br />
for daily news, or visit<br />
www.ovacome.org.uk<br />
Registered Charity Number 1058026<br />
To register as a member of <strong>Ovacome</strong><br />
please send your details to the following<br />
address or call the telephone number<br />
above<br />
© <strong>2014</strong> <strong>Ovacome</strong><br />
B5, City Cloisters, 196 Old Street,<br />
London EC1V 9FR.<br />
OVACOME is a voluntary organisation<br />
and relies on donations<br />
The information gathered in this newsletter<br />
is from many sources and is provided for<br />
guidance only. <strong>Ovacome</strong> has made every<br />
effort to ensure that it is accurate but can<br />
make no undertakings as to its accuracy<br />
or completeness. All medical information<br />
should be used in conjunction with advice<br />
from medical professionals<br />
Front cover: At the launch of<br />
the Survivors Teaching Students<br />
programme: the Clark family with<br />
<strong>Ovacome</strong>’s patron, Jenny Agutter.<br />
Image taken by Skye Brackpool at<br />
Brightontogs.<br />
Designed, produced and printed by<br />
Berforts Information Press Ltd<br />
www.informationpress.com<br />
Welcome to <strong>Ovacome</strong>’s summer newsletter<br />
We are entering a new era for cancer treatment, with a<br />
staggering 50% of people diagnosed with the disease today<br />
likely to be cured.<br />
While ovarian cancer is one of the more tricky areas to treat,<br />
Dr Richard Osborne, a consultant medical oncologist at Dorset<br />
Cancer Centre, told Members’ Day attendees that he wanted to share<br />
his “enthusiasm and optimism about progress in ovarian cancer treatment”.<br />
It’s largely down to the personalised way that women are now being managed with<br />
the introduction of multi-displinary teams working together to come up with tailored<br />
treatment plans, rather than a one approach suits all strategy, he said.<br />
The amount of options available to treat the disease is increasing with newcomers like<br />
Avastin making positive change. And a new armoury of drugs, such as Olaparib (see<br />
pages 6 and 7), are lining up to give the next generation of precision medicine.<br />
So Cancer Research UK’s ambitious plans to see three-quarters of all cancer patients<br />
surviving their disease in the next 20 years could well be within grasp. After all its<br />
recent landmark figures show a massive improvement from the early 1970s, when just<br />
a quarter of people diagnosed with cancer survived 10 years.<br />
It’s true that for many with ovarian cancer their disease is caught too late to be cured.<br />
But reassuringly it has become a disease that can be lived with using maintenance<br />
medicine, such as hormone therapy, and top up chemotherapy or surgery. This allows<br />
women to get on with their lives and to think of ovarian cancer more as a chronic<br />
illness such as diabetes.<br />
Hopefully this newsletter will help you get into this positive mindset. Happy reading.<br />
Juliet Morrison, newsletter editor.<br />
Thoughts from the chair<br />
Hello. I am absolutely delighted to be writing this comment piece<br />
as the new <strong>Ovacome</strong> chair of trustees.<br />
I have been a supporter of the charity since I read Sarah Dickinson’s<br />
article in Good Housekeeping in 1996 and have watched it grow (and<br />
support the women I was working with) into the amazing organisation<br />
that it is today.<br />
I want to thank Noëline Young for all her hard work over the past 10 years as chair and<br />
only hope that I can at least half fill her shoes - for this would be a job well done! I also<br />
want to thank Noëline for her personal support which I hope will continue.<br />
I was pleased to meet so many people at the recent Members’ Day. This was a truly<br />
inspiring event with great speakers and the opportunity to ask questions and share stories<br />
which made the day so much more valuable and enjoyable. There was a real sense of<br />
what has already been achieved for women with ovarian cancer and of the way that<br />
things will be improved in the future.<br />
Thank you again for welcoming me and for giving me the opportunity to use my<br />
experience (and time now the children have grown up!) to help steward the organisation<br />
to continue to do great things.<br />
Cathy Hughes.<br />
<strong>Ovacome</strong> was founded in 1996 by Sarah Dickinson.<br />
Trustees to the charity are: Cathy Hughes (chair), Simon Chantrey (treasurer),<br />
Sean Kehoe (medical adviser), Clare Barsby, Adrian Dickinson and Noëline Young.<br />
2 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 it together
news<br />
Teaching ovarian<br />
cancer away from<br />
the text book<br />
<strong>Ovacome</strong>’s new Survivors Teaching Students<br />
project, which brings the voices of ovarian<br />
cancer survivors to medical and other clinical<br />
students, was successfully launched in<br />
May with a pioneering presentation to our<br />
supporters and funders.<br />
Presenters Jackie Rose, Samixa Shah and Jenny Hayes spoke<br />
movingly about their experiences of diagnosis, treatment and<br />
living with ovarian cancer to drive home crucial information<br />
that will help to improve outcomes for women.<br />
<strong>Ovacome</strong> patron Jenny Agutter hosted the event and told<br />
how learning of the diagnosis of a woman she knew had<br />
convinced her to join the charity and support its innovative<br />
campaigning to raise awareness.<br />
Survivors Teaching Students is supported by the family of<br />
Dr Lisa Jayne Clark, a consultant in emergency medicine<br />
who died of ovarian cancer aged just 40 in October 2012.<br />
She trained at Charing Cross Hospital, which welcomed the<br />
<strong>Ovacome</strong> launch and gave the venue for free. The event<br />
began with a film about her life and her family’s support for<br />
the project in her memory.<br />
Talking it over: <strong>Ovacome</strong> supporters after presentation.<br />
Presenter Samixa Shah says: “It was a great experience,<br />
I thoroughly enjoyed being a presenter and although I was<br />
nervous about speaking I am so pleased to be able to use what<br />
happened to me in a positive way to help other women.”<br />
A powerful voice: Jackie Rose, Jenny Hayes, Samixa Shah<br />
and Jenny Agutter (back row first, left to right).<br />
Now <strong>Ovacome</strong> is receiving enquiries from medical schools,<br />
nursing schools and other education settings from across the<br />
UK and the next STS date is firmly booked. Many <strong>Ovacome</strong><br />
members have volunteered to take part as presenters.<br />
“This is an exciting pioneering programme that <strong>Ovacome</strong><br />
is offering for free as a<br />
practical and positive way<br />
of communicating with the<br />
doctors and nurses of the<br />
future,” says <strong>Ovacome</strong>’s chief<br />
executive, Louise Bayne.<br />
“The programme has been<br />
proved to be an effective way<br />
of giving information that<br />
is retained by putting real<br />
women’s voices and faces<br />
to ovarian cancer. It brings<br />
the story of ovarian cancer<br />
alive for students, rather than<br />
Noteworthy talks.<br />
relying on a dry text book.”<br />
Survivors Teaching Students: Saving Women’s Lives is<br />
owned and trademarked by the Ovarian Cancer National<br />
Alliance in the US.<br />
Would you like to be involved? To find out more email<br />
Ruth Grigg at r.grigg@ovacome.org.uk<br />
it together<br />
Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 3
Photography: Daily Echo, Bournemouth<br />
news<br />
Singing to recovery<br />
Gareth Malone, the preppy choirmaster credited with reigniting our interest in<br />
choral singing through his BBC Two series The Choir, would be proud. For word<br />
is getting around about how uplifting being part of a singing group can be and the<br />
benefits are numerous when dealing with illness.<br />
Rising Voices - a community choir for people affected by<br />
cancer in Dorset, Hampshire and Wiltshire - has found in<br />
a study that members have benefited from being part of a<br />
mutually empathetic community, in which they were not<br />
treated as victims.<br />
Altogether Rising Voices: Noëline Young (fourth from left, front row).<br />
As well as getting enjoyment from singing as a group,<br />
members liked the social interaction at weekly rehearsals and<br />
the travel to events, which could be anywhere from a local<br />
shopping centre or Women’s Institute meeting to a twinned<br />
event in Cherbourg.<br />
Concentrated chemo<br />
A<br />
decision on whether to<br />
progress with a new method of<br />
chemotherapy for treating ovarian cancer<br />
could be made soon.<br />
PETROC is a study of the use of<br />
chemotherapy that is given into the<br />
peritoneal space (IP) for ovarian cancer,<br />
rather than into a vein (IV). This<br />
increases the concentration of the drug<br />
around the cancer and can increase its<br />
effectiveness. The study is for patients<br />
who need to complete their treatment<br />
after primary chemotherapy for three<br />
cycles and a successful interval operation.<br />
This technique was new to the UK<br />
while it had been tested previously in<br />
the USA. The early studies had a lot of<br />
problems with toxicity which delayed<br />
acceptance in the UK. However,<br />
medical staff have learnt how to give<br />
the treatment much more safely, and<br />
UK centres have been trained so that<br />
after the first 150 patients there was<br />
no difference in toxicity between the<br />
Carboplatin and Paclitaxel given in the<br />
IP arm or the control IV arm.<br />
There was a third arm in the study using<br />
IP Cisplatin instead of the Carboplatin,<br />
however the independent data<br />
monitoring committee recommended<br />
that this be stopped as it was no more<br />
effective and more toxic.<br />
Member and <strong>Ovacome</strong> trustee Noëline Young says that the<br />
established associations between music and health, both<br />
physical and spiritual, have been well documented and<br />
highlighted in a report by Cardiff University.*<br />
“Participation in music making has been shown to improve<br />
well being and music has the power to communicate with<br />
individuals at times of difficulty. This formed the background<br />
to the establishment of our survivors’ choir, Rising Voices,”<br />
says Noëline, an ovarian cancer survivor herself.<br />
“The intention was to encourage participation in singing<br />
to boost confidence and social interaction and promote<br />
wellbeing, as an aid to recovery from cancer.”<br />
The choir has been supported by a start-up grant from<br />
Macmillan Cancer Support and Dorset Cancer Network, but<br />
longer term it plans to be self-sufficient, supported through<br />
voluntary donations by members, friends, donations and<br />
money raised from public performances.<br />
If you are interested in joining Rising Voices, it rehearses<br />
weekly at St John’s Church in Parkstone, Poole.<br />
e-mail admin@risingvoices.org.uk or phone 07500 676083.<br />
*Gale NS, Enright S, Reagon C, Lewis I, van Deursen R.<br />
A pilot investigation of quality of life and lung function following<br />
choral singing in cancer survivors and their carers. Cancer,<br />
2012; 6:261<br />
The study has now been resubmitted to<br />
Cancer Research UK with the planned<br />
interim analysis to allow the number<br />
of centres giving IP treatment in the<br />
UK to increase from nine to 28 and<br />
to include a further 630 patients in<br />
the trial, to prove whether it increases<br />
survival.<br />
Dr Sean Kehoe, a gynae surgeon.<br />
has reviewed the medical stories on<br />
page 4 and 5<br />
4 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 it together
Around the<br />
world support<br />
Cancer charities from across the globe united this<br />
summer in a powerful effort to raise awareness<br />
of the symptoms of the disease in the second World<br />
Ovarian Cancer Day.<br />
In a global movement, which took place on May 8, women<br />
pledged to tell at least five others about the most serious<br />
gynaecological cancer.<br />
<strong>Ovacome</strong> was delighted to take part in the UK, helping to<br />
build a sense of solidarity in the fight against the disease,<br />
says its chief executive, Louise Bayne: “We’re very proud<br />
to take part in World Ovarian Cancer Day in which all the<br />
ovarian cancer charities come together in a joint effort to<br />
raise awareness and to give women living with the disease a<br />
feeling of solidarity.”<br />
In the UK, the Department of Health has been investing<br />
in an awareness programme for ovarian cancer. It has<br />
undertaken a regional pilot for ovarian cancer symptoms<br />
Overcoming it together<br />
Improving survival rates, earlier<br />
diagnosis and access to appropriate<br />
treatments recommended by clinicians<br />
for ovarian cancer were among the key<br />
issues which <strong>Ovacome</strong> members have<br />
called for in a report which the charity<br />
presents to MPs this month.<br />
The charity has been polling its<br />
members to come up with priorities for<br />
improving ovarian cancer care, to give<br />
a series of recommendations to help<br />
news<br />
awareness<br />
in the<br />
North West and Borders as part of its<br />
Be Clear On Cancer campaign.<br />
Centred on the main message that if you<br />
feel bloated for three weeks or more you should see your GP,<br />
a television advert was included in the campaign.<br />
<strong>Ovacome</strong> awaits the pilot results to see what impact<br />
it has had in the regions. If the initiative has been<br />
successful, the charity will again call for ovarian cancer<br />
to be one of the cancers included in a national level<br />
campaign in 2015. To see the advert online visit:<br />
http://www.nhs.uk/be-clear-on-cancer/ovarian-cancer/home<br />
GSK withdraws Votrient application<br />
Initial hopes that the drug Votrient<br />
could be used in treating late stage<br />
ovarian cancer have been dashed, with<br />
GlaxoSmithKline withdrawing its<br />
application to the European Medicines<br />
Agency.<br />
It was found that the drug, also<br />
known as Pazopanib and licensed for<br />
kidney cancer and some types of soft<br />
cell sarcomas, did not give a positive<br />
the Government and the NHS achieve<br />
these goals.<br />
For despite positive steps to improve<br />
the quality of care and treatment, the<br />
survival of ovarian cancer patients<br />
living in the UK is still poorer than in<br />
comparable countries.<br />
The launch of the ‘Overcoming it<br />
together’ report at the parliamentary drop<br />
in event on 16 July, will give <strong>Ovacome</strong><br />
members attending the ear of MPs. They<br />
benefit-risk scenario after further<br />
analysis of data from the late-stage trial.<br />
GSK said it was disappointed by the<br />
findings, which came after it found the drug<br />
caused an improvement in progression-free<br />
survival in its Phase III study.<br />
GSK’s director of patient relations,<br />
Geraint Thomas, says while the company<br />
is disappointed by the latest results, it will<br />
progress additional analyses which may<br />
will be able to talk about their personal<br />
experiences and give input on what<br />
would have made their journey easier.<br />
They will also hear from Fiona<br />
Mactaggart, MP (Slough), who<br />
will give a talk on how <strong>Ovacome</strong><br />
members might engage effectively with<br />
politicians to raise areas of concern on<br />
a local and national level. Materials<br />
giving practical advice on this are<br />
available from <strong>Ovacome</strong>’s head office.<br />
add to the body of scientific evidence in<br />
this disease setting.<br />
“GSK remains committed to<br />
understanding the utility of pazopanib<br />
in relapsed ovarian cancer as more<br />
data become available through other<br />
studies,” he says.<br />
<strong>Ovacome</strong>’s chief executive Louise<br />
Bayne, says: “We are naturally<br />
disappointed.”<br />
it together<br />
Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 5
ask the doctor<br />
Better to know<br />
A<br />
new drug called Olaparib is proving successful in stopping cancer<br />
cells thriving by repairing damaged DNA, and is particularly effective<br />
on patients found to have faulty BRCA genes. It has just hit a regulatory<br />
setback in the US, but Dr James Mackay (left), consultant genetic oncologist<br />
at University College London, explains why he hopes it gets approval here.<br />
What is BRCA and why<br />
is it a problem?<br />
JM: BRCA1 and BRCA2 are genes that produce proteins that<br />
suppress tumours. These proteins are vital in helping repair<br />
damaged DNA. However, if BRCA genes are mutated, this<br />
damage repair may not take place, meaning that cells may be<br />
more likely to develop alterations in their genetic make-up that<br />
can lead to cancer.<br />
Why and how do we test<br />
for the BRCA mutation?<br />
JM: Up until a couple of years ago, the NHS tended to carry<br />
out BRCA testing based on family history. A blood sample<br />
was taken to see if a woman carried the mutation. If they did,<br />
doctors would offer the test to female family members who could<br />
decide whether to have preventative ovarian or breast surgery,<br />
as they could be at higher risk of developing these cancers.<br />
Now an increasing number of UK cancer centres – including<br />
the Royal Marsden in London as well as Cambridge and<br />
Glasgow – are offering women diagnosed with ovarian cancer<br />
BRCA blood testing as routine. The advantage is that targeted<br />
drugs can be used to treat women with the BRCA mutation<br />
which can be more effective than standard chemotherapy.<br />
This has meant that there has been a big change over the past<br />
year from believing that women should be tested based chiefly<br />
on their family background.<br />
The change in thinking has been fuelled by the arrival of<br />
Olaparib, which has been found to be effective as a treatment<br />
for women who test positive for BRCA.<br />
Some 14% of patients with serous ovarian cancer have the<br />
BRCA mutation. However, we don’t think it is necessary to<br />
screen the wider population because the chances of having a<br />
faulty BRCA gene is just one in 400, so the risk is low even for<br />
women who don’t know their family history.<br />
What are the tests<br />
designed to find out?<br />
JM: There are three possible results. The test can be normal,<br />
it can detect a fault indicating increased risk of cancer, or<br />
it can find a change in the DNA sequence. Previously this<br />
variance used to be dismissed, but now it is recognised that<br />
it could mean that the woman is at higher risk. Under a<br />
method that many specialists use, including myself, called<br />
the Myriad Genetics test, these inconclusive variances come<br />
up in about one in 100 tests. Standard NHS testing gives one<br />
in 10 people an inconclusive result.<br />
What is Olaparib?<br />
Olaparib is a PARP-1 inhibitor. A cancer cell has damaged<br />
DNA and relies on an enzyme called PARP – or Poly ADPribose<br />
polymerase – to repair it. Olaparib can stop the PARP<br />
from repairing DNA damage.<br />
Olaparib is the first of many PARP inhibitors in development<br />
at the moment to reach clinical use. It is in phase III clinical<br />
studies in platinum sensitive relapse (SOLO2) and first line<br />
maintenance (SOLO1).<br />
However, although it represents a significant step, it is<br />
important not to get carried away about its success in<br />
treating late stage ovarian cancer. One interesting question is<br />
whether the drug can be effective used at an earlier stage of<br />
treatment.<br />
Who will Olaparib be available to?<br />
People with relapsed ovarian cancer or those sensitive to<br />
platinum or platinum type drugs.<br />
AstraZeneca submitted Olaparib for its European licence in<br />
September 2013, based on the availability of tissue as well as<br />
blood BRCA testing.<br />
It will be available initially through the Cancer Drugs Fund<br />
and private sector, but as early as the end of this year, NICE<br />
could clear the drug to be used on the NHS by 2016.<br />
Olaparib was dealt a setback this June when the US Food<br />
and Drug Adminstration’s Oncologic Drugs Advisory<br />
Committee (ODAC) voted 11-2 against the accelerated<br />
approval of the drug as a maintenance therapy for women<br />
with platinum-sensitive relapsed ovarian cancer with<br />
germline BRCA mutations.<br />
It said until there was further data to judge by, there were<br />
too many troubling questions about potential side effects<br />
of the drug as well as uncertainties about the efficacy data<br />
demonstrating an improvement on progression-free survival.<br />
6 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 it together
ask the doctor<br />
It’s not over yet, though. AstraZeneca continues with<br />
its confirmatory Phase III study of the PARP inhibitor,<br />
SOLO-2. And the R&D group will need to report clear<br />
signs of a benefit to get this drug to the U.S. market.<br />
In Europe, AstraZeneca is hoping for a smoother journey.<br />
It goes without saying that we want to get Olaparib<br />
available in clinical practice as soon as possible.<br />
Do you think that all women<br />
with ovarian cancer should be<br />
BRCA tested now and ask for<br />
the test at their hospital?<br />
It looks like Olaparib could make a significant impact on<br />
the treatment of late stage ovarian cancer. That’s why<br />
we are hoping that everyone will be offered testing at<br />
diagnosis: as a first step with blood and eventually with<br />
tissue. We want this so that we can see which women will<br />
benefit from Olaparib.<br />
I think BRCA should be more widely available to other<br />
women too who might not necessarily have a strong case<br />
with regard to their family history, but could well benefit.<br />
I’m thinking of, for instance, a woman in her early 30s<br />
who has triple negative breast cancer. Even if she doesn’t<br />
have a strong family history, there is still a reasonably<br />
high risk of her having the BRCA1 or BRCA2 fault and<br />
so she will be at high risk of developing ovarian cancer. It<br />
would be a nightmare to get through breast cancer only to<br />
develop ovarian cancer in her early 40s when this could<br />
be avoided.<br />
Should a positive BRCA test<br />
always lead to a recommendation<br />
for preventative treatment?<br />
JM: If, say, a patient is found to be BRCA positive and she<br />
has an 18–year-old daughter, would we recommend having her<br />
daughter tested? I would question that as she might have 22 years<br />
ahead of her before she decided to have her ovaries removed<br />
Photography by Tony Larkin/Rex Features.<br />
Hollywood actress Angelina Jolie has already shone the spotlight on the<br />
importance of high-risk women knowing their BRCA status.<br />
in her early 40s after having a family. This might be different,<br />
of course, if the daughter had breast cancer. A lot depends too<br />
on the clinical context and such matters should always be the<br />
patient’s decision rather than having rules about it.<br />
This piece has been reviewed by<br />
Chris Jacobs, consultant genetic<br />
counsellor and joint lead for cancer<br />
genetics clinical genetics department at<br />
Guy’s Hospital, London.<br />
She says: The article mentions that standard<br />
NHS BRCA1 and BRCA2 genetic testing<br />
gives one in 10 people an inconclusive result,<br />
whereas private testing via the company<br />
Myriad Genetics gives inconclusive results<br />
to around one in 100 tests. This difference<br />
is likely to be due to the greater number of<br />
tests undertaken by Myriad genetics than<br />
the NHS laboratories which enables them to<br />
classify more inconclusive resuts as cancer<br />
causing (pathogenic) or non-cancer causing<br />
(non pathogenic). If all laboratories, including<br />
private genetic testing companies, were to share<br />
this type of data, it would enable all BRCA1/2<br />
genetic testing to improve.<br />
The article mentions that genetic testing<br />
should be more widely available and gives an<br />
example of a woman in her early 30s with<br />
triple negative breast cancer and no cancer<br />
family history. The NICE guidelines for<br />
familial breast cancer, which were published<br />
in June 2013, recommended that BRCA1<br />
and BRCA2 genetic testing is offered to any<br />
woman in England and Wales with at least a<br />
10% chance of a fault in one of these genes.<br />
This would include women with ovarian cancer<br />
and women with triple negative breast cancer<br />
who are diagnosed at a young age and have no<br />
family history of the disease. Women in this<br />
situation can be referred to their local regional<br />
genetics service to discuss genetic testing.<br />
it together<br />
Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 7
fundraising<br />
Tea with <strong>Ovacome</strong> <strong>2014</strong><br />
Tea with <strong>Ovacome</strong> has become the social event of the year in the ovarian cancer calendar:<br />
smashing records in <strong>2014</strong> with 200 attendees and £8,228 raised for the charity.<br />
The T.W.O. team, led by <strong>Ovacome</strong><br />
member Adele Sewell, is thrilled and<br />
has set itself<br />
the ambitious<br />
goal of<br />
£10,000 for<br />
the next<br />
fundraiser to<br />
be held in<br />
March 2015.<br />
This was the<br />
fifth Tea with<br />
<strong>Ovacome</strong><br />
and as usual<br />
planning<br />
started early.<br />
Tickets went<br />
on sale in Where it all started: Adele Sewell,<br />
early October at event, with her daughter Zindzi.<br />
and were sold<br />
out six weeks later. Also, Adele secured<br />
some top drawer supporters for the<br />
entertainment on the day.<br />
Key note speaker was Helen Fawkes,<br />
the BBC journalist who writes a regular<br />
column for <strong>Ovacome</strong>’s newsletter<br />
about her journey with ovarian cancer.<br />
“Helen told us her story of living<br />
with ovarian cancer with her natural<br />
humour and professionalism; at once<br />
making us laugh and then the next<br />
minute bringing tears to our eyes,”<br />
says Adele.<br />
Apricot store displays.<br />
Then there was the singer Ayanna Blair-<br />
Ford. “At a private family event last year,<br />
I found myself in the same room<br />
as the incredible voice that is<br />
Ayanna Blair-Ford. Only 17, doing<br />
A-Levels and hoping to pursue a<br />
career in architecture. We were<br />
delighted when Ayana agreed to<br />
be our featured entertainer at this<br />
year’s event,” says Adele.<br />
But the models - all ovarian cancer<br />
patients at some time - were the<br />
stars of the show, says Adele.<br />
“They brought their energy and<br />
enthusiasm to the room.”<br />
They were<br />
dressed top<br />
to toe in<br />
clothing<br />
from Apricot,<br />
generously<br />
donated by the<br />
fashion retailer<br />
for the second<br />
year running.<br />
They strutted<br />
their stuff on<br />
three catwalks,<br />
each with a<br />
different theme.<br />
The final one was all teal and included<br />
the beautiful Apricot dress which was<br />
designed exclusively for <strong>Ovacome</strong>,<br />
Retail therapy<br />
with all proceeds from it going to the<br />
charity.<br />
A special thanks should also be given<br />
to Barry M, which provided two<br />
manicurists for the day to paint visitors’<br />
nails teal, as well as teal varnish for the<br />
goody bags. This was part of the Teal<br />
Tips campaign which ran throughout<br />
Ovarian Cancer Awareness Month in<br />
March, raising hundreds of pounds and<br />
awareness for the charity.<br />
Thanks also to <strong>Ovacome</strong> supporter,<br />
the milliner Philip Treacy who kindly<br />
donated another hat to be auctioned<br />
on the day, raising £500.<br />
All together: <strong>Ovacome</strong> members empowered in teal.<br />
• If you would like to take part in Tea<br />
with <strong>Ovacome</strong> 2015, please email<br />
TEAwithOVACOME@yahoo.co.uk.<br />
The beautiful teal dress and the <strong>Ovacome</strong> branded canvas tote bag that fashion retailer Apricot<br />
designed especially for us this awareness month have raised a staggering £17,000 for the charity.<br />
During March Apricot stores had special displays for the items and staff were dressed in teal. The<br />
outlets sold <strong>Ovacome</strong> pin badges, with collection tins and information on ovarian cancer at tills.<br />
This is all thanks to <strong>Ovacome</strong> member Adele Sewell. She persuaded Apricot to produce the dress<br />
and bag after a chance meeting at a friend’s daughter’s 21st birthday party with Karen McGhie, who<br />
drove the project forward.<br />
The <strong>Ovacome</strong> dress, above, is still available in sizes 8, 12 and 16 at the reduced price of £25.<br />
www.apricotonline.co.uk<br />
8 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 it together
A day of empowerment<br />
Some 40 members gathered for <strong>Ovacome</strong>’s annual Members’ Day in what was an<br />
uplifting and informative occasion on the latest treatments, how to deal with sex<br />
after surgery and to be confident in dealing with cancer specialists.<br />
Topping the bill for the day was Dr Richard Osborne, a<br />
medical oncologist at the Dorset Cancer Centre in Poole. He<br />
set the tone by telling members that he wanted to “transfer<br />
my personal enthusiasm about the progress in treatment for<br />
ovarian cancer”, which he said was making steady year-onyear<br />
and discernible decade-on-decade improvements.<br />
He assured members<br />
that we are entering<br />
a time of change with<br />
the “chemotherapyalone<br />
era” coming to<br />
an end. Personalised<br />
treatment plans, he<br />
said, are replacing a<br />
one-shot approach<br />
for all and multiple<br />
options are available to fight the late stage disease which<br />
three out of four ovarian cancer patients are diagnosed with.<br />
With this being the case, many women will face a life of<br />
treating the ovarian cancer as a chronic disease, he said.<br />
“We want to cure ovarian<br />
cancer, but have to accept<br />
that in the majority of<br />
cases it will be about<br />
disease modification: To<br />
make the cancer inactive<br />
and give women a longer<br />
life. Actually, doctors very<br />
rarely cure anything, but<br />
modify it as we see with<br />
high blood pressure and<br />
diabetes.”<br />
A fond farewell<br />
Noëline Young (pictured above<br />
receiving flowers of thanks from<br />
<strong>Ovacome</strong>’s chief executive Louise<br />
Bayne) stepped down as chair at<br />
Members’ Day after 10 years.<br />
Members’ feedback:<br />
‘As always, a great day. My only complaint is<br />
that there is never enough time to talk with as<br />
many people as one might wish’<br />
‘It was worth coming for Dr Richard Osborne’s<br />
presentation alone- very informative and useful.<br />
All speakers very good and well organised day.’<br />
The introduction of<br />
avastin, as a maintenance<br />
drug to treat late stage<br />
disease, fits with this.<br />
But while it gives cause<br />
for optimism we should<br />
not be cracking open the<br />
champagne yet, said Dr<br />
Osborne. “Avastin is not a magic wand. It has its place, but<br />
we should not get too worked up about it. There’s uncertainty<br />
about who to treat with it. Those higher-risk women with<br />
residual disease after treatment seem to do better.”<br />
Other new and exciting strategies<br />
are emerging, he said, including<br />
personalised therapy based<br />
on molecular profiling and<br />
immunotherapy, in which the immune<br />
system is reactivated to fight the<br />
cancer. Then there is<br />
supra-radical surgery<br />
involving lasers and<br />
around 12 hours on<br />
the operating table<br />
and anti-androgen<br />
therapy, to ‘switch off’ male hormones in<br />
women (Coral trial).<br />
Meanwhile, hot topics being debated in<br />
the medical community include giving<br />
oophorectomy surgery for BRCA mutation carriers; surgery<br />
or chemotherapy first (CHORUS trial); giving dosedense<br />
paclitaxel (ICON 8 trial) and PARP inhibitors as<br />
maintenance therapy to BRCA carriers (see pages 6 and 7).<br />
This is all shows that the chemotherapy alone era is ending,<br />
said Dr Osborne. “New strategies are emerging of targeting<br />
therapy, turning switches off, using the patient’s personalised<br />
genetic make up and harmonising the immune system. But at<br />
the same time earlier diagnosis remains a very high priority.”<br />
• Talks were also given by Dr Helen Fairhurst on sex after<br />
surgery (see pages 10 and 11) and there was a confidence<br />
building workshop from trainer Deb Puleston (see<br />
<strong>Ovacome</strong>’s autumn/winter <strong>2014</strong> newsletter).<br />
Senior help<br />
members’ day<br />
Dr Richard Osborne: end of<br />
chemo-only era.<br />
Senior research associate, Lindsay Fraser, appealed<br />
for members to help her with a new area of research<br />
‘exploring the journey of women diagnosed with ovarian<br />
cancer’ in the Gynaecological Cancer Research Centre<br />
at UCL’s Institute for Women’s Health. The research will<br />
explore the journey of women diagnosed with ovarian cancer,<br />
from the patient perspective by talking to women and their<br />
families, rather than examining medical records. Seven<br />
women came forward, but Lindsay sill needs women aged<br />
70-plus, along with their partners, adult children and friends<br />
to help with the scope of the first interview study. Contact<br />
l.fraser@ucl.ac.uk or phone Lindsay on 020 3447 2114.<br />
it together<br />
Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 9
feature<br />
The big taboo<br />
Sex may be the last thing on your mind when recovering from an ovarian cancer<br />
diagnosis. But there is plenty help available to get your mind and body in the<br />
right place after treatment, says Dr Helen Fairhurst from the Winton Psychosexual<br />
Medicine Clinic.<br />
For many, returning to a normal sex life after treatment<br />
for ovarian cancer can be difficult. But it is even more of a<br />
problem if the subject remains taboo for patients, partners<br />
and the medical profession. A study in the British Journal of<br />
Cancer in 2003 * found that while a majority of healthcare<br />
professionals thought most women<br />
with ovarian cancer would experience<br />
difficulties, only one in four doctors<br />
and one in five nurses brought the<br />
subject up with patients.<br />
Things may have moved on since the<br />
2003 study and some cancer centres<br />
– such as Dorset, where I work<br />
offer exceptional support to women<br />
through their gynaecological nurses.<br />
However, clinicians – and patients<br />
themselves – often need to do more.<br />
Dr Helen Fairhurst<br />
For instance, there is a network of<br />
pyschosexual clinics on hand throughout the UK, run by<br />
members of The Institute of Psychosexual Medicine. Women<br />
can access these clinics by self-referral or referral by their GP or<br />
other health professionals.<br />
And women themselves need to feel empowered to ask<br />
questions. Your focus may be on getting over the cancer. But<br />
don’t be afraid to bring up the subject of sexuality and how<br />
it may be affected by the type of treatment you are having<br />
as soon as you feel ready to discuss it. The sooner the better.<br />
We know quality of life and general wellbeing can be greatly<br />
enhanced if problems with sexuality are addressed early on.<br />
Sexual problems are not always just down to physical reasons.<br />
Emotional factors, not always experienced at a conscious<br />
level, interfere with sexual pleasure. The underlying causes<br />
of a problem may be physical or psychological in varying<br />
proportions, but are rarely limited to one or the other.<br />
There are several ways cancer and its treatments can undermine<br />
a person’s sexuality. The impact of surgery, chemotherapy and<br />
radiotherapy will be direct and physical. But there may be other<br />
obstacles when it comes to intimacy, such as feeling disfigured,<br />
too tired to bother, changes in sensory perception and difficulty<br />
reaching orgasm. Also women can feel that their body, which<br />
has been prodded and probed by the health professionals, is no<br />
longer really part of them.<br />
But remember, however, that the ‘core’ of your being inside<br />
you is maintained, regardless of the treatment you have had.<br />
Lack of libido<br />
Low sexual desire or libido is a common problem. Many<br />
different emotional and physical factors can affect sexual<br />
desire and may be present in women living with cancer.<br />
Tiredness, stress, relationship problems, menopause<br />
symptoms, worries about children, elderly relatives, finances<br />
and work, or difficulties accepting the changes in body image<br />
that come after surgery are just some examples. And of<br />
course, in some cases sex may be a low priority after facing a<br />
cancer diagnosis and treatment.<br />
Coping with illness symptoms and the effects of treatment<br />
can be challenging enough. Women may feel too unwell to<br />
summon up the energy for the exertions of sex, but still long<br />
for physical closeness. Others find it difficult to enjoy sex<br />
without thinking of their cancer.<br />
At the same time, partners may have difficulty relating to<br />
the anxieties and fears that come with a cancer diagnosis.<br />
They might not understand why their partner feels less<br />
sexy, especially once treatment is complete, and they<br />
can see an outward return to normality. This can lead to<br />
communication misfirings and a downward spiral becomes<br />
established, just at the time when some love and support is<br />
vital. If a woman is harbouring anger and resentment towards<br />
her partner, it can be difficult to get in the right frame of<br />
mind to enjoy sex.<br />
Solutions will vary from person to person, but discussion with<br />
partners, friends and health professionals is often beneficial.<br />
Patients often ask about using hormones to improve their<br />
libido. While it is true that both oestrogen and testosterone<br />
are needed for good sexual function, and are reduced by the<br />
removal of both ovaries, many other factors can influence<br />
sexual desire. This means that hormone replacement may<br />
not be the solution. Also, there is uncertainty about whether<br />
taking these hormones to deal with a sudden surgical<br />
menopause could increase cancer recurrence risk.<br />
A recent study showed that women given Hormone<br />
Replacement Therapy (HRT) after a surgically induced<br />
menopause following treatment for epithelial ovarian<br />
cancer ** had improved longevity as well as a good control of<br />
10 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554<br />
it together
feature<br />
symptoms such as hot flushes. However, it is still difficult to<br />
be confident that HRT is not a risk factor for recurrence.<br />
Change in sensation<br />
Altered sexual pleasure is another common problem found in<br />
women who have had surgery for gynaecological cancer.<br />
For some women, orgasms have always been generated by<br />
the muscle contraction of their uterus at the time of climax.<br />
Following hysterectomy, they are no longer able to feel this<br />
sensation and may find it difficult to orgasm through clitoral<br />
stimulation instead.<br />
They may even be scared to try clitoral stimulation fearing<br />
it might harm the healing process or possibly even lead to a<br />
recurrence of their cancer. While logic tells them that this is<br />
not correct, they find it difficult to get rid of this fear.<br />
Physical examination by a doctor trained in psychosexual<br />
medicine, although not always welcomed by women<br />
after treatment, can then be useful helping correct<br />
misunderstandings about effects of surgery, improve body<br />
image and sexual confidence and to face feelings of loss in a<br />
caring environment.<br />
Painful sex<br />
Painful sex, or dyspareunia can also start after a surgical<br />
menopause. The lower level of oestrogen caused by this can<br />
lead to the vagina becoming dry, thin and losing its former<br />
elasticity.<br />
Local creams and pessaries containing oestrogen hormones<br />
can help. Examples include Vagifem pessaries (which contain<br />
oestrogen hormones), Sylk natural lubricants and Replens<br />
moisturisers. But, as with libido, this might not be the<br />
complete solution and looking at emotional factors can be<br />
very important too.<br />
Vaginismus, the involuntary spasm of the muscles at<br />
the entrance of the vagina often due to subconscious<br />
unacknowledged emotions, is another painful complaint.<br />
One woman I have met with this problem coped very well<br />
during her hospital admission for surgical treatment, but<br />
the true impact of her cancer diagnosis came later when she<br />
started to experience anxiety about her health and also anger.<br />
Her previously active and fulfilling sex life had become<br />
virtually non-existent and painful. Her self-confidence<br />
suffered: she felt ugly and unattractive. Her husband seemed<br />
to take the brunt of her anger not least because he was<br />
apparently unable to empathise with her anxiety about<br />
cancer recurrence. He just didn’t understand that she needed<br />
compliments, to be understood, to be listened to.<br />
Physical examination revealed dryness of the vagina wall,<br />
as well as some vaginismus: both likely to be contributing<br />
to the painful sex. She was not at all keen to use hormone<br />
replacement, even in the form of locally applied oestrogens,<br />
despite reassurance from her cancer specialist that it would<br />
not increase her likelihood of cancer recurrence.<br />
She used a vibrator to help open up her vaginal tissue – this<br />
was her choice as she hated the idea suggested by her surgeon<br />
to use graded vaginal dilators instead. Most importantly, we<br />
were able to make the link between her vaginismus and her<br />
emotional difficulties, resulting in her angry wretched vagina<br />
barring entry to her ‘annoying’ husband.<br />
She also gained some valuable support from friends,<br />
including holding a virtual funeral for her womb and also<br />
from other women at the local cancer support group.<br />
• Dr Helen Fairhurst gave a talk on sexuality after treatment<br />
for gynaecological cancer at <strong>Ovacome</strong>’s recent Members’<br />
Day.<br />
The two studies cited in this piece are: Lack of communication<br />
between healthcare professionals and women with ovarian cancer<br />
about sexual issues * British Journal of Cancer 2003, Stead,<br />
Brown, Fallowfield and Selby and ** Eeles RA et al, Adjuvant<br />
Hormone Therapy Improves Survival in Epithelial Ovarian<br />
Cancer: Results of the AHT randomised trial, submitted to the<br />
British Medical Journal June <strong>2014</strong>.<br />
Helpful resources<br />
<strong>Ovacome</strong> has some useful fact sheets in this area -<br />
‘Ovarian cancer and sexuality’ and ‘Treatment-induced<br />
menopause’ - www.ovacome.org.uk<br />
http://www.macmillan.org.uk/Cancerinformation/<br />
Livingwithandaftercancer/Relationshipscommunication/<br />
Sexuality/Sexuality.aspx<br />
Institute of Pyschosexual Medicine for a list of therapist<br />
locations - www.ipm.org.uk<br />
College of Sexual and Relationship Therapists -<br />
www.cosrt.org.uk<br />
The Menopause Exchange -<br />
www.menopause-exchange.co.uk<br />
Dana-Farber Cancer Institute in Boston: Dr Sharon<br />
Bober’s Sexual Health Program and videos -<br />
www.dana-farber.org/Health-Library/How-cancertreatment-affects-sexuality-in-women.aspx.<br />
This piece has been reviewed by Dr Richard Osborne,<br />
a consultant medical oncologist at the Dorset Cancer<br />
Centre in Poole.<br />
it together<br />
Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 11
Our magnificent<br />
marathon team<br />
Ovarian cancer survivor Jackie Rose was among the<br />
runners who competed in April’s London Marathon<br />
for <strong>Ovacome</strong>, with the group raising an enormous<br />
£28,220.62 for the charity.<br />
Jackie Rose: fulfils personal ambition running London Marathon.<br />
Jackie, from Hackney in North<br />
London, was diagnosed with stage 1C<br />
clear cell carcinoma ovarian cancer six<br />
years ago. She has always wanted to run<br />
the London Marathon and on the day<br />
she completed it in just over six hours,<br />
raising £981.12.<br />
Julie Caudle,<br />
from Cowes,<br />
the Isle of<br />
Wight, has<br />
raised £3,647.<br />
She took up<br />
running after<br />
her mother<br />
died of<br />
ovarian cancer<br />
aged 67 in<br />
2009, which<br />
drove Julie<br />
Julie Caudle: now a<br />
“runaholic”.<br />
on to becoming a self-confessed<br />
“runaholic”. She says the only running<br />
she did before her mother’s death was<br />
for the bus. Training for the marathon<br />
was “very hard work” says Julie,<br />
“but nothing<br />
compared with<br />
what people who<br />
have the disease<br />
are suffering”.<br />
Other London<br />
marathon runners<br />
<strong>Ovacome</strong> would<br />
like to thank are:<br />
Gareth Rosser,<br />
who raised<br />
£2,593.16;<br />
Richard Stock<br />
(£4,507.50);<br />
Eleanor Bancroft (£1,599.38); Claire<br />
Zahra (£3,168.31); Michael Lawlor<br />
(£1,453.16); Zare de Haldevang<br />
(£8,601.99); Lizzy Pollot (£910) and<br />
Preethi Sundaram (£759).<br />
fundraising<br />
A funny walk…<br />
for a very serious cause<br />
Comedian Nick Banks and his<br />
entourage of fellow funnymen<br />
from the north-east raised £4,048.94<br />
for <strong>Ovacome</strong> with their Hadrian’s Wall<br />
Walk <strong>2014</strong>.<br />
The group walked 84 miles<br />
along the famous landmark,<br />
taking in venues along the<br />
way with a week’s worth of<br />
gigs. Among the group was<br />
TV comic Patrick Monahan<br />
and well-known performers<br />
Seymour Mace and Silky.<br />
Nick, who runs the event for<br />
a different charity every year,<br />
Kevin Stephens<br />
smashes £10K<br />
of £100K target<br />
Kevin Stephens’ pledge to raise<br />
£100,000 for <strong>Ovacome</strong> may have<br />
seemed wildly ambitious when he made<br />
it back in autumn 2012.<br />
But, Kevin has smashed £10,000 so far<br />
by being on fundraising duty 24/7. He<br />
never misses an opportunity to boost<br />
the charity’s coffers; whether that is<br />
by getting local businesses to display<br />
collection tins, friends to take part in<br />
sponsored runs or new acquaintances to<br />
dispose of loose change.<br />
But Kevin’s ambition is twofold. He has<br />
also worked tirelessly to raise awareness<br />
about the symptoms of the disease,<br />
which took his wife Loraine nearly two<br />
years ago. He has immersed himself in<br />
finding out the latest developments<br />
about the disease, becoming part of the<br />
ovarian cancer community as a regular<br />
and very welcome face at <strong>Ovacome</strong>’s<br />
Members’ Day and the fundraising<br />
event Tea With <strong>Ovacome</strong>.<br />
To support Kevin visit<br />
www.justgiving.com/Loraine-Stephens<br />
says the journey is becoming harder<br />
each time. “It was great fun, but we<br />
were a year older than last time and<br />
I damaged my achilles heel and Jim<br />
Bayes, his knee,” he laughs.<br />
Funnymen don their walking boots for <strong>Ovacome</strong>.<br />
12 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 it together
postbag<br />
A safe place<br />
Meet <strong>Ovacome</strong>’s new wellbeing columnist, Samixa Shah, who will be answering<br />
questions from fellow members in the winter newsletter onwards.<br />
Samixa, who has been treated for ovarian cancer herself, worked as a pharmacist for almost 25 years before deciding “to<br />
help people understand how to take responsibility of their own health, rather than just rely on medicines”.<br />
She did a course in neuro-linguistic programming (NLP) in 2005 and completed a life coaching diploma in 2009. She<br />
then completed a Diploma in Wellness Coaching Skills in 2013.<br />
Samixa has been working as a wellbeing coach at an NHS health centre in London since January 2012 and is still<br />
registered as a pharmacist, which she says helps her “immensely” as a wellbeing coach, “since I understand a number of<br />
health conditions and their treatments and can therefore coach anybody who is having difficulty in their life either due to<br />
their health condition or their lifestyle”.<br />
She says: “I also feel that my interest in alternative therapies helps me coach people who may have difficulties managing<br />
their health with prescribed medicines and feel that they want to use alternative therapies.”<br />
“I strongly believe that the mind-body<br />
connection is of paramount importance<br />
in any healing process as well as in<br />
maintaining a state of wellbeing.<br />
Looking after your mental health during<br />
investigations and after an ovarian<br />
cancer diagnosis is just as important as<br />
the physical side and I have been doing<br />
this in a number of ways myself before<br />
and since being diagnosed with FIGO<br />
stage 4, grade 3 serous carcinoma of the<br />
ovary, primary peritoneum and tubal in<br />
May 2012, aged 49.<br />
Louise L. Hay states in her book – ‘You<br />
Can Heal Your Life’ – “Every cell within<br />
your body responds to every thought you<br />
think and every word you speak.”<br />
This has also been researched in the<br />
book ‘The Hidden Messages in Water’,<br />
by Masaru Emoto.<br />
I informed all my close friends and family<br />
as soon as I was diagnosed. When I was<br />
undergoing treatment and thereafter I<br />
carefully chose to be around friends and<br />
family members who would be positive<br />
and would not bring me down.<br />
I made sure I told everyone what support<br />
I needed from them and was very clear<br />
about when they could come and visit<br />
me and also who could come with me<br />
when I went for my chemotherapy. My<br />
main priority was to be strong both<br />
mentally and physically so that my<br />
husband - who is registered blind - and<br />
my 23-year-old son and other people<br />
around me did not feel helpless. I also<br />
made sure that if someone called I<br />
would only answer the call if it was<br />
someone I wished to speak to. I decided<br />
I had to be in charge since it was<br />
my body and ME going through this<br />
experience!!<br />
I also made sure that during the seven<br />
months I underwent chemotherapy<br />
and surgery, I surrounded myself with<br />
positive books, television programmes,<br />
podcasts and radio shows. I got a lot of<br />
resources from the Macmillan Cancer<br />
Support Centre and did a course in<br />
Mindfulness as well.<br />
My training as a pharmacist and<br />
wellbeing coach came in very<br />
useful since I understood how the<br />
drugs worked and was able to<br />
coach myself to think positively<br />
and make use of my resources to<br />
achieve my health related goals.<br />
I went back to work as a<br />
wellbeing coach in February<br />
2013 and was still undergoing<br />
treatment every three weeks<br />
as I was having Avastin, which<br />
stopped in October 2013.<br />
During this time and even<br />
today I continue with my<br />
mindfulness practice and<br />
make sure that I live for the present<br />
moment and enjoy each day to the<br />
fullest.<br />
I have learnt to appreciate even the<br />
smallest joys of life like watching a<br />
butterfly fly past me or the birds singing<br />
in the garden. I do not worry about the<br />
future since I do not have control over<br />
that. I can only have control over my<br />
thoughts and the present moment.”<br />
Edgware, Middlesex.<br />
- If you would like to send in<br />
a question to Samixa, write to<br />
ovacome@ovacome.org.uk<br />
it together<br />
Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 13
postbag<br />
From the frontline<br />
The other day I was at hospital for a check-up. As I waited I showed the woman<br />
who sat next to me some photographs of cows that I’d taken. It may seem a bit<br />
strange but we were doing something that most ordinary people think nothing<br />
of. We’d got talking because of a shared interest.<br />
She sang in classical<br />
music concerts and she<br />
thought I might be<br />
creative in my spare<br />
time. I told her it was<br />
Helen Fawkes: turns to photography distraction.<br />
funny she should say that as I was a<br />
keen photographer and was having an<br />
exhibition of my pictures of cattle. I<br />
got my mobile out to show her some<br />
of the images.<br />
Coming from the countryside I enjoy<br />
taking snaps of these beautiful, big<br />
beasts. So when I came up with my<br />
bucket list, which I call my List for<br />
Living, number 21 was to have my<br />
very own exhibition.<br />
I’ve taken hundreds of photos of cows<br />
and steers on my dad’s farm. I like it<br />
when they look straight at the camera<br />
and seem to pose for me. Something<br />
Strong sense of purpose<br />
remember thinking that I had pulled<br />
I a muscle and blaming the pain on<br />
dancing in impossibly high heels at a<br />
wedding party. The pain went away,<br />
but a month later I went to another<br />
wedding, same dress, same heels, same<br />
dancing and the pain came back - only<br />
this time it didn’t go away.<br />
I went to work as usual on that fateful<br />
day in October 2012, but I had to leave<br />
mid morning as the pain got substantially<br />
worse. I drove to my surgery. The<br />
receptionist took one look at my teary<br />
face and next minute I was sat with a GP.<br />
The words ‘mass’ and ‘cyst’ floated across<br />
my consciousness, which hospital would<br />
I prefer? Could I drive to the emergency<br />
department?<br />
I didn’t call my husband until quite a bit<br />
later, stupid really but he was busy and I<br />
had only put four hours on the car park<br />
ticket. I remember the lovely registrar<br />
in the emergency department and the<br />
look on the face of the radiologist as<br />
the ultrasound scan passed over my<br />
abdomen, I remember them asking<br />
which consultant<br />
was on call and if the<br />
gynaecological registrar<br />
could come down,<br />
I remember thinking<br />
I’ve got cancer.<br />
It was in fact stage<br />
4 advanced ovarian<br />
cancer, with some lung<br />
mets and a breast lump<br />
thrown in for good<br />
measure. I found out on<br />
Friday and on Sunday<br />
I spent five hours in<br />
surgery. I was home five days later and<br />
five weeks later started my Carboplatin<br />
and Paclitaxel chemo regime.<br />
Amanda Barnes: nobody<br />
knows the future.<br />
Photography, with thanks to<br />
The News, Portsmouth.<br />
Fast forward and I have been back<br />
at work full-time, post chemo, for a<br />
year. I’ve finished my dissertation and<br />
graduated with my masters in advanced<br />
which appears to come easily to them!<br />
These are the ones I selected for the<br />
display at my friend’s tea shop in<br />
Worcestershire.<br />
Seeing my pictures on the walls felt like<br />
such an achievement. Something that<br />
had nothing to do with cancer. When<br />
you live with this disease it’s hard not<br />
to be defined by it. The cheeky cows in<br />
my photos have no idea how they have<br />
helped me with this.<br />
• Keep an eye on Helen’s blog<br />
to see where her photographic<br />
exhibition will be displayed next at<br />
helenfawkes.wordpress.com<br />
clinical practice, travelled to Verona<br />
to watch opera in the open air, seen<br />
La Bohème at the Albert Hall, been<br />
on the Queen Mary to drink<br />
champagne in the sunshine on<br />
my birthday, bought a building<br />
site of a house and am enjoying<br />
choosing paint and bricks! Life<br />
is good - bracketed with three<br />
monthly checks that still make<br />
me worry and more CT scans<br />
than I would like.<br />
I still have my mets, but I also<br />
have a strong sense of purpose<br />
and a fabulous husband who<br />
is my soulmate and my rock.<br />
There is no way that I am ready<br />
for anything less than a fantastic life.<br />
Ovarian cancer hasn’t changed me,<br />
but it has made me acknowledge my<br />
spirituality and embrace my life. None<br />
of us know what tomorrow will bring<br />
and that’s just fine by me.<br />
Amanda Barnes, Havant, Hampshire.<br />
14 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 it together
postbag<br />
The comfort of words<br />
The <strong>Ovacome</strong> newsletter was my first link to other ladies who had been diagnosed<br />
with ovarian cancer, when I myself was diagnosed with stage 3c of the disease in<br />
May 2013.<br />
Reading other people’s stories gave<br />
me hope and made me realise that<br />
for many of us life does go on. So it<br />
was interesting to attend <strong>Ovacome</strong>’s<br />
members’ day this year and meet some<br />
of those people and the team who<br />
compile the newsletter.<br />
We all know the frustrations of being<br />
first diagnosed and learning that the<br />
cancer has been there a while and<br />
for many of us that it has spread. But<br />
what was heartening to hear was that<br />
the treatment of ovarian cancer has<br />
improved considerably over the past<br />
10 years and scientists and doctors seem<br />
to be on the verge of new treatments.<br />
Fingers crossed we will be enjoying life<br />
despite the cancer for years to come.<br />
What I also learned at the members’<br />
day was that several people were quite<br />
young when diagnosed - and there<br />
was me thinking that it only affected<br />
older women. I was aged 65. It was my<br />
youngest of three boys’ birthdays!<br />
I have been lucky on my journey<br />
with having few side effects from the<br />
chemotherapy - neuropathy in my feet<br />
is uncomfortable, but not painful and<br />
having mouth ulcers and losing my hair<br />
was tolerable. I now have a wonderful<br />
collection of caps and scarves.<br />
I was given four doses of Carboplatin<br />
and Paclitaxel, followed by debulking<br />
surgery - on my second son’s birthday<br />
- and two more rounds of the same<br />
chemotherapy.<br />
From February this year I have been on<br />
caelyx. This seems to be working and<br />
my hair is growing back. I just hope<br />
my immune system doesn’t collapse<br />
again and that I don’t have to have any<br />
more fluid drained from my abdomen or<br />
pleural cavity.<br />
We all have a different wish list<br />
of things we want to do. One<br />
thing I would like to do is see my<br />
grandchildren become adults.<br />
My 16-year-old granddaughter has<br />
set me a challenge to write a book<br />
of poetry - well it is more likely to<br />
be a booklet. My first attempt was<br />
about cancer and was written in the<br />
Living in the moment<br />
Jenny Hayes: ‘I feel<br />
like I’m on parole.’<br />
chemotherapy unit while having my<br />
fourth of six doses of caelyx.<br />
As a semiretired<br />
teacher of<br />
English as<br />
a foreign<br />
language<br />
I love<br />
language<br />
and find<br />
writing poetry<br />
cathartic.<br />
Sometimes<br />
poetry has<br />
a deeper<br />
meaning than<br />
other writing<br />
and it allows you to say things that you<br />
can’t any other way.<br />
Let me throw out a challenge to you<br />
all to have a go and write a poem.<br />
Maybe we can publish some in the<br />
next magazine.<br />
Send me yours to pat_abra@hotmail.com<br />
Pat Abra, Margate, Kent.<br />
was diagnosed in 2007 with breast cancer. My treatment was radiotherapy and tamoxifen with three<br />
I monthly checks with my oncologist. At that time I felt my oncologist was my knight in shining armour.<br />
Every visit to him, with his kind voice and caring personality, gave me another three months, then six<br />
months and eventually a whole year of freedom to live and plan for the future. I took every opportunity to<br />
enjoy life after breast cancer.<br />
Then in 2012 I was<br />
diagnosed with<br />
ovarian cancer,<br />
stage 3c, with the<br />
added bonus of being BRCA 2 positive.<br />
I was given chemotherapy and some<br />
hard to swallow statistics.<br />
As a result, I make carefully chosen<br />
plans for the future. I avoid getting<br />
into a relationship with a partner, and<br />
although I would love to, I won’t get<br />
another dog.<br />
Now I view my oncologist as my prison<br />
parole officer. I see him every three<br />
months and he gives me another three<br />
months to get on with things. Parole,<br />
yippee! Now that does make me live in<br />
the moment.<br />
Pat Abra: writing poetry<br />
can be cathartic.<br />
I’m fortunate that I run a couple of<br />
businesses which affords me to shop till<br />
I drop and if I want cheering up and see<br />
something I want, I will buy it.<br />
I am ‘on parole’ just now with my body<br />
behaving. I’ve just returned from a holiday<br />
to Dubai and I will eat cake today.<br />
Jenny Hayes, Leighton Buzzard,<br />
Bedfordshire.<br />
it together<br />
Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 15
fundraising<br />
A bake off<br />
challenge<br />
for summer<br />
The sun should be shining and<br />
it’s time to put your inner<br />
Mary Berry or Paul Hollywood<br />
talents to good use by holding a<br />
Big <strong>Ovacome</strong> Bake Off.<br />
All you need is a venue, contestants to bring along<br />
their bakes a judge or two and a Big <strong>Ovacome</strong><br />
Bake Off party pack which is available free to help<br />
members hold baking<br />
fundraisers throughout<br />
the summer.<br />
Why not pull out the<br />
gingham table cloths<br />
and host an event for<br />
friends and family in your<br />
own garden to help raise<br />
money for the charity.<br />
The bake off could be<br />
part of your village fête.<br />
Or perhaps you could stage a village verses village<br />
competition, asking local chefs to judge the bakes<br />
and create a bit of a fanfare by inviting along local<br />
dignitories, celebrities and press.<br />
The packs, sponsored by national convenience store<br />
chain Nisa, were originally launched for awareness<br />
month. They have been so successful, however, that<br />
<strong>Ovacome</strong> is making them available on-going.<br />
Each pack - available from <strong>Ovacome</strong>’s office -<br />
contains bunting, guidelines on how to run an event,<br />
recipe ideas, a certificate for the winner and even a<br />
branded tea towel to clean up afterwards.<br />
Further tea towels and also aprons can be purchased<br />
from <strong>Ovacome</strong> to use as prizes for the bake off<br />
perhaps, with respective retails of £5 and £10 a piece.<br />
Other merchandise - such as <strong>Ovacome</strong>-branded<br />
balloons and T-shirts to wear on the day - is also<br />
available to help your event go as smoothly as if<br />
Mary Berry were organising it herself.<br />
• For your free party pack and other <strong>Ovacome</strong><br />
merchandise contact Sonia Vig in <strong>Ovacome</strong>’s<br />
head office on 020 7299 6654.<br />
Ready<br />
baked<br />
Tens of <strong>Ovacome</strong> supporters have been holding bake offs since<br />
spring to help raise thousands of pounds for the charity.<br />
• Top fundraising bake off was an event organised by Kirsti Fox,<br />
who has won tea for two at The Ritz with <strong>Ovacome</strong>’s patron<br />
Jenny Agutter. Together with the<br />
Mildenhall Lions volunteers she<br />
raised £900 for the charity. They<br />
recruited local chefs to judge the<br />
Great Mildenhall Bake Off, which<br />
helped attract the media and also<br />
some 70 contestants.<br />
Contestants paid to enter, the cakes were<br />
sold and there was a raffle. Kirsti decided<br />
to have seven categories: a sponge of up<br />
to eight inches; a tray bake; cup cakes;<br />
a signature bake, scones; 12s and under<br />
and a showstopper.<br />
Most interest came from the children’s Kirsti and Andy Fox and<br />
Ann Taylor-Balls (left to right).<br />
section which had more than<br />
35 entrants. And the crowds were wooed<br />
with a four tier wedding cake and another depicting a beach scene.<br />
“It was fun, and I couldn’t have managed it without the help of the<br />
other Lions Club volunteers,” says Kirsti, who is now planning a<br />
parachute jump to raise further money for <strong>Ovacome</strong> this summer.<br />
• Elizabeth Buckley’s bake off, which<br />
she held at a friend’s restaurant in<br />
Sandbach, raised £555. She charged<br />
£3 on the door, to cover the cost of<br />
refreshments, combined the event<br />
with a raffle and sold the cake after<br />
judging.<br />
A fun day for all.<br />
She needed nerves of steel with just<br />
10 people signing up on Eventbrite the weekend before. In the end<br />
20 people baked, including five children, and it was a “truly fantastic<br />
fun day”, with tens of people attending says Elizabeth.<br />
She would like to give a special thank<br />
you to her friend Suzanne Gee who not<br />
only allowed the bake off to be held at<br />
her restaurant, Gee’s Kitchen, but also<br />
ran the Marbury 10K raising a further<br />
£305 for <strong>Ovacome</strong>. This helped bring<br />
Elizabeth’s final fundraising tally, which<br />
included donations for her posting bald<br />
photos of herself as famous characters<br />
online, to almost £1,600.<br />
Elizabeth Buckley (right)<br />
rewards entrant.<br />
16 Phone <strong>Ovacome</strong>’s nurse led support line on 0845 371 0554 it together