CMS IPPS 2014 Final Rule
CMS IPPS 2014 Final Rule
CMS IPPS 2014 Final Rule
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
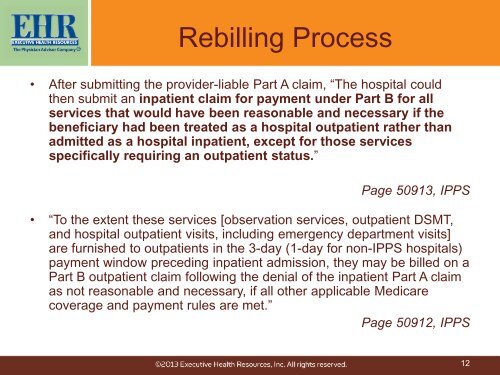
Rebilling Process• After submitting the provider-liable Part A claim, “The hospital couldthen submit an inpatient claim for payment under Part B for allservices that would have been reasonable and necessary if thebeneficiary had been treated as a hospital outpatient rather thanadmitted as a hospital inpatient, except for those servicesspecifically requiring an outpatient status.”Page 50913, <strong>IPPS</strong>• “To the extent these services [observation services, outpatient DSMT,and hospital outpatient visits, including emergency department visits]are furnished to outpatients in the 3-day (1-day for non-<strong>IPPS</strong> hospitals)payment window preceding inpatient admission, they may be billed on aPart B outpatient claim following the denial of the inpatient Part A claimas not reasonable and necessary, if all other applicable Medicarecoverage and payment rules are met.”Page 50912, <strong>IPPS</strong>12