C L I N I C A L S T U D Y S U M M A R Y
C L I N I C A L S T U D Y S U M M A R Y
C L I N I C A L S T U D Y S U M M A R Y
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
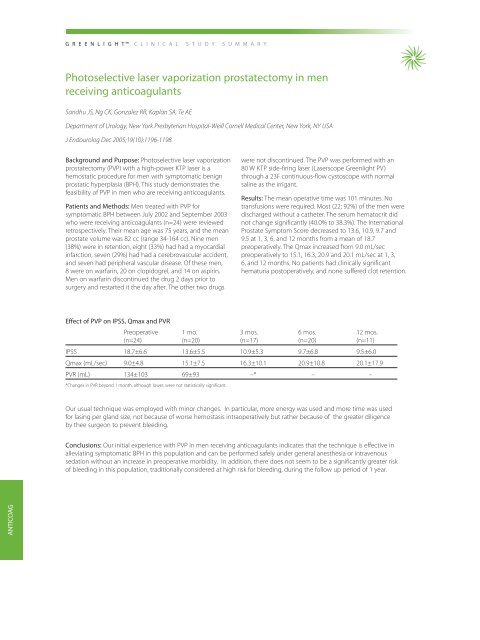
151557_GreenLightSummary_B 5/31/07 4:29 PM Page 26G R E E N L I G H TC L I N I C A L S T U D Y S U M M A R YPhotoselective laser vaporization prostatectomy in menreceiving anticoagulantsSandhu JS, Ng CK, Gonzalez RR, Kaplan SA, Te AEDepartment of Urology, New York Presbyterian Hospital-Weill Cornell Medical Center, New York, NY USAJ Endourolog Dec 2005;19(10):1196-1198Background and Purpose: Photoselective laser vaporizationprostatectomy (PVP) with a high-power KTP laser is ahemostatic procedure for men with symptomatic benignprostatic hyperplasia (BPH). This study demonstrates thefeasibility of PVP in men who are receiving anticoagulants.Patients and Methods: Men treated with PVP forsymptomatic BPH between July 2002 and September 2003who were receiving anticoagulants (n=24) were reviewedretrospectively. Their mean age was 75 years, and the meanprostate volume was 82 cc (range 34-164 cc). Nine men(38%) were in retention, eight (33%) had had a myocardialinfarction, seven (29%) had had a cerebrovascular accident,and seven had peripheral vascular disease. Of these men,8 were on warfarin, 20 on clopidogrel, and 14 on aspirin.Men on warfarin discontinued the drug 2 days prior tosurgery and restarted it the day after. The other two drugswere not discontinued. The PVP was performed with an80 W KTP side-firing laser (Laserscope Greenlight PV)through a 23F continuous-flow cystoscope with normalsaline as the irrigant.Results: The mean operative time was 101 minutes. Notransfusions were required. Most (22; 92%) of the men weredischarged without a catheter. The serum hematocrit didnot change significantly (40.0% to 38.3%). The InternationalProstate Symptom Score decreased to 13.6, 10.9, 9.7 and9.5 at 1, 3, 6, and 12 months from a mean of 18.7preoperatively. The Qmax increased from 9.0 mL/secpreoperatively to 15.1, 16.3, 20.9 and 20.1 mL/sec at 1, 3,6, and 12 months. No patients had clinically significanthematuria postoperatively, and none suffered clot retention.Effect of PVP on IPSS, Qmax and PVRPreoperative 1 mo. 3 mos. 6 mos. 12 mos.(n=24) (n=20) (n=17) (n=20) (n=11)IPSS 18.7±6.6 13.6±5.5 10.9±5.3 9.7±6.8 9.5±6.0Qmax (mL/sec) 9.0±4.8 15.1±7.5 16.3±10.1 20.9±10.8 20.1±17.9PVR (mL) 134±103 69±93 –* – –*Changes in PVR beyond 1 month, although lower, were not statistically significant.Our usual technique was employed with minor changes. In particular, more energy was used and more time was usedfor lasing per gland size, not because of worse hemostasis intraoperatively but rather because of the greater diligenceby thee surgeon to prevent bleeding.Conclusions: Our initial experience with PVP in men receiving anticoagulants indicates that the technique is effective inalleviating symptomatic BPH in this population and can be performed safely under general anesthesia or intravenoussedation without an increase in preoperative morbidity. In addition, there does not seem to be a significantly greater riskof bleeding in this population, traditionally considered at high risk for bleeding, during the follow up period of 1 year.ANTICOAG