Cnrstn 09.10 - Winthrop University Hospital
Cnrstn 09.10 - Winthrop University Hospital
Cnrstn 09.10 - Winthrop University Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
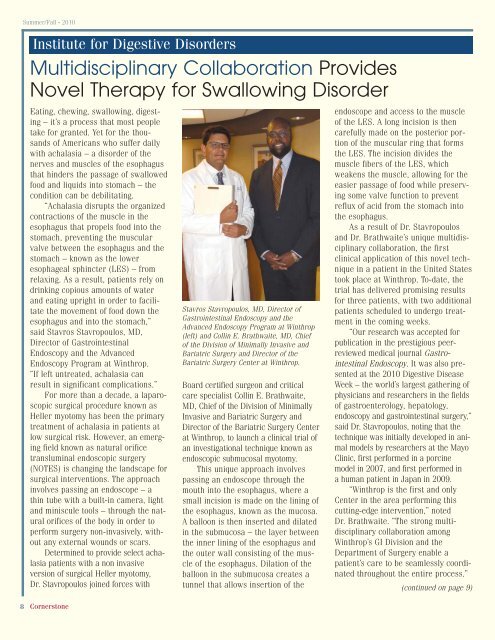
Summer/Fall • 2010Institute for Digestive DisordersMultidisciplinary Collaboration ProvidesNovel Therapy for Swallowing DisorderEating, chewing, swallowing, digesting– it’s a process that most peopletake for granted. Yet for the thousandsof Americans who suffer dailywith achalasia – a disorder of thenerves and muscles of the esophagusthat hinders the passage of swallowedfood and liquids into stomach – thecondition can be debilitating.“Achalasia disrupts the organizedcontractions of the muscle in theesophagus that propels food into thestomach, preventing the muscularvalve between the esophagus and thestomach – known as the loweresophageal sphincter (LES) – fromrelaxing. As a result, patients rely ondrinking copious amounts of waterand eating upright in order to facilitatethe movement of food down theesophagus and into the stomach,”said Stavros Stavropoulos, MD,Director of GastrointestinalEndoscopy and the AdvancedEndoscopy Program at <strong>Winthrop</strong>.“If left untreated, achalasia canresult in significant complications.”For more than a decade, a laparoscopicsurgical procedure known asHeller myotomy has been the primarytreatment of achalasia in patients atlow surgical risk. However, an emergingfield known as natural orificetransluminal endoscopic surgery(NOTES) is changing the landscape forsurgical interventions. The approachinvolves passing an endoscope – athin tube with a built-in camera, lightand miniscule tools – through the naturalorifices of the body in order toperform surgery non-invasively, withoutany external wounds or scars.Determined to provide select achalasiapatients with a non invasiveversion of surgical Heller myotomy,Dr. Stavropoulos joined forces with8 CornerstoneStavros Stavropoulos, MD, Director ofGastrointestinal Endoscopy and theAdvanced Endoscopy Program at <strong>Winthrop</strong>(left) and Collin E. Brathwaite, MD, Chiefof the Division of Minimally Invasive andBariatric Surgery and Director of theBariatric Surgery Center at <strong>Winthrop</strong>.Board certified surgeon and criticalcare specialist Collin E. Brathwaite,MD, Chief of the Division of MinimallyInvasive and Bariatric Surgery andDirector of the Bariatric Surgery Centerat <strong>Winthrop</strong>, to launch a clinical trial ofan investigational technique known asendoscopic submucosal myotomy.This unique approach involvespassing an endoscope through themouth into the esophagus, where asmall incision is made on the lining ofthe esophagus, known as the mucosa.A balloon is then inserted and dilatedin the submucosa – the layer betweenthe inner lining of the esophagus andthe outer wall consisting of the muscleof the esophagus. Dilation of theballoon in the submucosa creates atunnel that allows insertion of theendoscope and access to the muscleof the LES. A long incision is thencarefully made on the posterior portionof the muscular ring that formsthe LES. The incision divides themuscle fibers of the LES, whichweakens the muscle, allowing for theeasier passage of food while preservingsome valve function to preventreflux of acid from the stomach intothe esophagus.As a result of Dr. Stavropoulosand Dr. Brathwaite’s unique multidisciplinarycollaboration, the firstclinical application of this novel techniquein a patient in the United Statestook place at <strong>Winthrop</strong>. To-date, thetrial has delivered promising resultsfor three patients, with two additionalpatients scheduled to undergo treatmentin the coming weeks.“Our research was accepted forpublication in the prestigious peerreviewedmedical journal GastrointestinalEndoscopy. It was also presentedat the 2010 Digestive DiseaseWeek – the world’s largest gathering ofphysicians and researchers in the fieldsof gastroenterology, hepatology,endoscopy and gastrointestinal surgery,”said Dr. Stavropoulos, noting that thetechnique was initially developed in animalmodels by researchers at the MayoClinic, first performed in a porcinemodel in 2007, and first performed ina human patient in Japan in 2009.“<strong>Winthrop</strong> is the first and onlyCenter in the area performing thiscutting-edge intervention,” notedDr. Brathwaite. “The strong multidisciplinarycollaboration among<strong>Winthrop</strong>’s GI Division and theDepartment of Surgery enable apatient’s care to be seamlessly coordinatedthroughout the entire process.”(continued on page 9)