Critically Appraised Topic – Meta-analysis Human recombinant ...
Critically Appraised Topic – Meta-analysis Human recombinant ...
Critically Appraised Topic – Meta-analysis Human recombinant ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
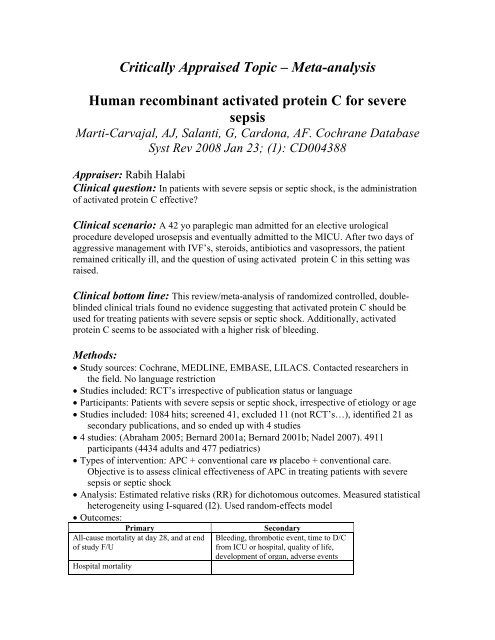
<strong>Critically</strong> <strong>Appraised</strong> <strong>Topic</strong> <strong>–</strong> <strong>Meta</strong>-<strong>analysis</strong><strong>Human</strong> <strong>recombinant</strong> activated protein C for severesepsisMarti-Carvajal, AJ, Salanti, G, Cardona, AF. Cochrane DatabaseSyst Rev 2008 Jan 23; (1): CD004388Appraiser: Rabih HalabiClinical question: In patients with severe sepsis or septic shock, is the administrationof activated protein C effective?Clinical scenario: A 42 yo paraplegic man admitted for an elective urologicalprocedure developed urosepsis and eventually admitted to the MICU. After two days ofaggressive management with IVF’s, steroids, antibiotics and vasopressors, the patientremained critically ill, and the question of using activated protein C in this setting wasraised.Clinical bottom line: This review/meta-<strong>analysis</strong> of randomized controlled, doubleblindedclinical trials found no evidence suggesting that activated protein C should beused for treating patients with severe sepsis or septic shock. Additionally, activatedprotein C seems to be associated with a higher risk of bleeding.Methods:• Study sources: Cochrane, MEDLINE, EMBASE, LILACS. Contacted researchers inthe field. No language restriction• Studies included: RCT’s irrespective of publication status or language• Participants: Patients with severe sepsis or septic shock, irrespective of etiology or age• Studies included: 1084 hits; screened 41, excluded 11 (not RCT’s…), identified 21 assecondary publications, and so ended up with 4 studies• 4 studies: (Abraham 2005; Bernard 2001a; Bernard 2001b; Nadel 2007). 4911participants (4434 adults and 477 pediatrics)• Types of intervention: APC + conventional care vs placebo + conventional care.Objective is to assess clinical effectiveness of APC in treating patients with severesepsis or septic shock• Analysis: Estimated relative risks (RR) for dichotomous outcomes. Measured statisticalheterogeneity using I-squared (I2). Used random-effects model• Outcomes:PrimaryAll-cause mortality at day 28, and at endof study F/UHospital mortalitySecondaryBleeding, thrombotic event, time to D/Cfrom ICU or hospital, quality of life,development of organ, adverse events
Evidence/Validity:• Original evidence for effectiveness of APC came from the PROWESS trial (Bernard2001b). It contains two sub studies, one with 720 participants where the trial wascarried out following the initial protocol and another with 970 participants where theregistered protocol had been amended. This information was not reported by thePROWESS trial; it came from the FDA 2001 report.• One important change seen in the amended protocol was the addition of an exclusioncriterion that prevented further enrollment of participants with septic shock(obviously mortality is higher in septic shock patients)• The other change altered the placebo from 0.9% sodium chloride solution to 0.1%human serum albumin• Almost all the enrolled participants in the PROWESS trial were Caucasian.Primary objectives according to original and the final amended protocolOriginal protocolAmended protocol1.To demonstrate that rhAPC reduces 28-daymortality in patients with severe sepsisand/or septic shock.2.To demonstrate that rhAPC reduces 28-daymortality in protein C deficient patientswith severe sepsis and/or septic shock.1.To demonstrate that rhAPC reduces 28-daymortality in patients with severe sepsis.Results:• Using only the studies in adults, the RR for overall 28-day mortality was 0.92 (95%CI0.72 to 1.18; P = 0.42, I2 = 72.0%).• For FDA data, APC had no significant effect on 28-day mortality rates compared toplacebo participants in the first half of the study. The relative risk (RR) was 0.94(95% CI 0.75 to 1.1; P = 0.57). In the second half of the study, APC had a markedbeneficial effect compared to placebo. The RR was 0.71 (95% CI 0.57 to 0.87; P =0.0001); for overall mortality the RR was 0.81 (95% CI 0.61 to 1.07; P = 0.14, I2 =
68.5%). These data were not reported by Bernard 2001b or in any of the severalduplicate publications derived from the PROWESS study.• .Performed a sensitivity <strong>analysis</strong> by excluding the data from Bernard 2001b after theprotocol was amended. By excluding this second part of the PROWESS study theheterogeneity dropped to 0% and the pooled estimate was 1.01 (95% CI 0.89 to 1.15;P = 0.84).Validity check list:• Was a focused clinical question addressed? Yes• Were study inclusion criteria appropriate? Yes• What is the likelihood that a relevant study which would change the overview’sconclusion was omitted? Very unlikely given the search criteria. Also justified thereason to exclude Bernard’s modified protocol in the <strong>analysis</strong> to demonstrate thatthere’s no heterogeneity• Was the validity of the included studies assessed with reproducible standards? Yes• What is the degree of heterogeneity between included studies? With the inclusion ofboth parts of the PROWESS trial, I2 is 72 %, and it drops to 0 % with the exclusionof the second part of the PROWESS trial• Was follow-up of sufficient duration? Were all patients accounted for and analyzed?Yes & Yes• Do the study population characteristics describe your patient? Almost all participantsin the PROWESS trial are Caucasians (~50% of pts analyzed in this meta<strong>analysis</strong>).My patient is African American. He is also in septic shock, which wouldhave excluded him from the second part of the PROWESS trial. Otherwise, hadother characteristics (SIRS, organ dysfunction, …)Comments:• Well-designed <strong>Meta</strong>-<strong>analysis</strong>; study sources, design of studies included, number ofstudies screened,….• Sensitivity <strong>analysis</strong> is helpful this study. It made the conclusion stronger when thesecond part of the PROWESS trial was excluded• In November 2001, the (FDA) approved APC for use in people with severe sepsis,based on their APACHE II score, but there are many controversies re: PROWESStrial…• PROWESS trial is sponsored by Eli Lilly Pharm• Prowess broken into 2 trials where the protocol was amended and the study drug waschemically altered• Two studies (Abraham 2005; Nadel 2007) were stopped early to avoid harm. ThePROWESS study was not stopped after the first half of the study, without anyevidence of any beneficial effect of APC; but the protocol was modified and thereasons for this decision are unclear.• The 95% CI of the effect of APC changed from RR 0.94, 95% CI 0.75 to 1.17 (usingthe original protocol) to 0.71 95% CI 0.57 to 0.87 (with the amended protocol).
• Also, there is no relationship between the effect of the drug and the importance ofprotein C deficiency. On the contrary, the effect of the drug is more evident in thegroup without protein C deficiency• The play of chance could explain the positive effect on 28-day mortality in participantswith APACHE II score of 25 or more. This possibility is supported by the ADDRESSstudy (Abraham 2005)• The risk of bias in the included studies is not negligible. Three of the four studiesincluded in this review (Abraham 2005; Bernard2001a; Nadel 2007) did not describe their randomization procedure.• Another major aspect that applied to all included studies was sponsorship by thepharmaceutical industry• More randomized trials are needed to establish the role of APC in management ofpatients with severe sepsis