ALBUTEROL SULFATE (Proventil Ventolin )
ALBUTEROL SULFATE (Proventil®, Ventolin
ALBUTEROL SULFATE (Proventil®, Ventolin
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
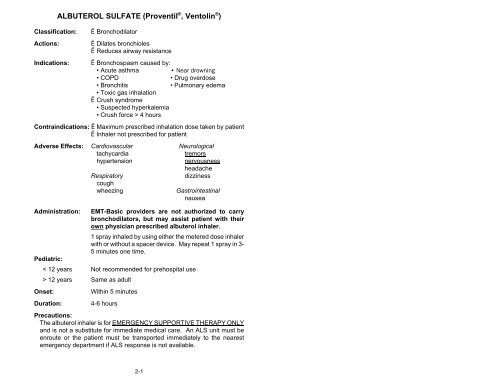
Classification:Actions:Indications:<strong>ALBUTEROL</strong> <strong>SULFATE</strong> (<strong>Proventil</strong> ® , <strong>Ventolin</strong> ® )Ë BronchodilatorË Dilates bronchiolesË Reduces airway resistanceË Bronchospasm caused by:• Acute asthma• Near drowning• COPD• Drug overdose• Bronchitis• Pulmonary edema• Toxic gas inhalationË Crush syndrome• Suspected hyperkalemia• Crush force > 4 hoursContraindications: Ë Maximum prescribed inhalation dose taken by patientË Inhaler not prescribed for patientAdverse Effects: Cardiovascular NeurologicaltachycardiatremorshypertensionnervousnessheadacheRespiratorydizzinesscoughwheezingGastrointestinalnauseaAdministration: EMT-Basic providers are not authorized to carrybronchodilators, but may assist patient with theirown physician prescribed albuterol inhaler.1 spray inhaled by using either the metered dose inhalerwith or without a spacer device. May repeat 1 spray in 3-5 minutes one time.Pediatric:< 12 years Not recommended for prehospital use> 12 years Same as adultOnset:Duration:Within 5 minutes4-6 hoursPrecautions:The albuterol inhaler is for EMERGENCY SUPPORTIVE THERAPY ONLYand is not a substitute for immediate medical care. An ALS unit must beenroute or the patient must be transported immediately to the nearestemergency department if ALS response is not available.2-1
<strong>ALBUTEROL</strong> <strong>SULFATE</strong> (<strong>Proventil</strong> ® , <strong>Ventolin</strong> ® )(Continued)Hypoxic patients may experience dysrhythmias. Monitor pulse periodicallyfor irregularity. Administer supplemental O 2 before and after treatment todecrease hypoxemia.Note:Directions for Using Metered Dose Inhaler Without a Spacer Device1. Shake container vigorously several times.2. Instruct patient to exhale deeply.3. Instruct patient to place lips around mouthpiece.4. Instruct patient to take a slow, deep breath and depress themedication canister while patient inhales.5. Instruct patient to remove mouthpiece and hold breath for aslong as possible.6. Instruct patient to exhale slowly through pursed lips.7. Replace patient O 2 and reevaluate breath sounds.8. Repeat procedure one time if needed.Directions for Using Metered Dose Inhaler With a Spacer Device1. Shake container vigorously several times.2. Remove cap from spacer.3. Attach spacer to inhaler.4. Instruct patient to exhale deeply.5. Instruct patient to place lips around mouthpiece.6. Depress the medication canister to fill the spacer chamber.7. Instruct patient to take several slow, deep breaths to inhalemedication in spacer. (There may be a whistling sound if thepatient inhales too rapidly.)8. Instruct patient to remove mouthpiece and hold breath for aslong as possible.9. Instruct patient to exhale slowly through pursed lips.10. Replace patient O 2 and reevaluate breath sounds.11. Repeat procedure one time if needed. (1/00)Included in Los Angeles County "Expanded" Scope of Practice2-2
CHARCOAL (ACTIVATED)(Acta-Char ® , Actidose ® , Charcoaid ® , Insta-Char ® , Liqui-Char ® )Classification:Actions:Indications:Ë Chemical absorbentË Absorbs ingested drugs and chemicalsË Suspected drug overdose or ingestion of poisonsContraindications: Ë Altered level of consciousness or risk of decreasedconsciousness in the fieldË Absent gag reflexAdverse effects: Gastrointestinal RespiratoryvomitingaspirationAdministration:Use preparations without Sorbitol25-50g PO as toleratedPediatric:0-2 years Not recommended for prehospital use.> 2 years Same as adult.Onset:Duration:Immediate24 hoursPrecautions:DO NOT ADMINISTER IF THERE IS A POTENTIAL FOR ALTEREDLEVEL OF CONSCIOUSNESS. There is a risk of vomiting and aspirationif a decrease in consciousness occurs. Patient must be able to drinkwithout assistance.DO NOT ADMINISTER CHARCOAL WITH SORBITOL TO PATIENTSLESS THAN 2 YEARS OLD. Sorbitol acts as a potent cathartic and maycause fluid and electrolyte disturbances.Note:Shake bottle vigorously prior to administration to ensure that charcoal isthoroughly suspended.Charcoal is most effective if administered within 30 minutes of overdose orpoison ingestion.Charcoal does not absorb cyanide, ethanol, methanol, ferrous sulfate,caustic alkali or mineral acids. (1/00)Not included in Los Angeles County Scope of Practice2-3
CHEMOTHERAPEUTIC AGENTClassification:Actions:Indications:Ë Cytotoxic agentË Eradicates or controls rapidly reproducing cells suchas cancer cellsË Cancer treatmentContraindications: Ë Not significant during interfacility transportAdverse effects:Administration:Pediatric:Onset:Duration:Ë Not significant during interfacility transportInfusion pump is required. Rate must be adjustedby hospital/home health personnel.Same as adultDetermined by specific medication48 hours - 7 daysPrecautions:Pregnant or nursing mothers should defer patient care to partner. Exposureto chemotherapeutic agents places the primary care provider at risk fordeveloping cancer, genetic damage, and may cause birth defects. Healthcare professionals must wear protective clothing when caring for patient.Immediate first aid treatment is required for exposure. Direct contact withsome chemotherapeutic agents may cause irritation, burning and tissuedestruction.Spills must be immediately cleaned up. All units must have a spill kitreadily available since IV leakage and spills can occur. IV tubing shouldhave luerlock connections and a plastic-backed absorbent liner should beplaced under the IV tubing.All soiled linens, dressings and absorbent padding must be disposed ofseparately and not placed in regular waste containers. Chemotherapeuticagents are excreted in body fluids.Notes:hhProtective ClothingLatex gloves at least .007 inch thickGown; lint-free, low permeability fabric, closed front, longsleeves and tight-fitting cuffs2-4
CHEMOTHERAPEUTIC AGENT(Continued)Spill Kithhhhhhhhhh2 pairs of disposable gloves:• inner -- latex, powder free, at least .007 inch thick• outer -- utility strengthGown: lint-free, low permeability fabric, closed front,long sleeves and tight-fitting cuffsShoe coversSplash gogglesRespirator (special mask)Absorbent, plastic-backed sheetsDisposable toweling2 prelabeled plastic hazardous disposal bagsPlastic scoop for broken glassPuncture-resistant container for glass fragmentsFirst AidhhSkin -- wash immediately with soap and water.Eyes-- flush with normal saline solution for 5 minutes(1/00)***All exposures must be reported andevaluated by a physician***Included in Los Angeles County “ Expanded” Scope of Practice2-5
Classification:Actions:Indications:DEXTROSE PREPARATIONS (ORAL)DEXTROSE CARBONATE SOLUTIONandGLUCOSE PASTE / GLUCOSE GELË Hyperglycemic agent (carbohydrate)Ë Immediate source of glucose which is needed forcellular metabolismË Conscious diabetic patient who has signs/symptoms ofhypoglycemiaContraindications: Ë Unresponsive patientsË Patients who are unable to swallow or have adiminished gag reflexË Patients complaining of nauseaAdverse Effects: Gastrointestinal RespiratoryvomitingAdministration:SolutionPaste/GelPediatric:SolutionPaste/GelOnset:Duration:75-100g (10g/oz) PO, sipped slowly.aspirationobstructed airway1 tube of paste/gel swallowed or 1 inch placed betweencheek and gum.1g/kg PO, sipped slowlyNot recommended for prehospital useWithin 20 minutesDepends on the degree and cause of hypoglycemiaPrecautionsAdminister solution only to patients who can hold the bottle and drinkwithout assistance or administer paste/gel if the patient has the ability toswallow. There is a risk of airway obstruction, vomiting, and aspiration ifthe patient is unable to swallow or has a diminished gag reflex.Note:The entire amount does not need to be administered if the patient'scondition improves.Signs/Symptoms of hypoglycemia: rapid onset, cool, moist skin, hunger,bizarre/combative behavior, anxiety, restlessness, weakness, appearanceof intoxication or stroke such as slurred speech and staggering gait, andseizures. (1/00)Included in Los Angeles County "Expanded" Scope of Practice2-6
DEXTROSE 5% IN WATER (D 5 W) SOLUTIONClassification:Actions:Indications:Ë Isotonic/hypotonic solution (5g dextrose/100ml water)Ë Provides some sugar for cellular metabolismË Supplies body waterË Intravenous access for drug administrationContraindications: Ë Not significant during interfacility transportAdverse Effects:Administration:Pediatric:Onset:Duration:Ë Increases free water and may cause intracellularedemaMay transport with infusion adjusted to a TKO rate byhospital personnel.Must transport with a volume-control set and rateadjusted to a TKO rate by hospital personnel.Immediate20-40 minutesPrecautions:Monitor infusion rate frequently; if signs of fluid overload, turn off IV drip.Infusion may result in fluid overload.Check IV site frequently and if infiltration is noted, turn off IV drip. IV mayinfiltrate during transport.Note:Signs of fluid overload: distended neck veins (JVD), rapid respirations,shallow tidal volume, fine auscultatory crackles, dyspnea, and peripheraledema.Signs of infiltration: swelling and pain around IV site. (1/00)2-7
EPINEPHRINE HYDROCHLORIDE (Adrenalin ® )EPIPEN AUTO-INJECTORClassification:Actions:Indications:Ë Sympathomimetic agent (catecholamine)Ë Dilates bronchiolesË Constricts blood vesselsË Anaphylaxis (severe allergic reaction)Contraindications: Ë Not significant in above indicationAdverse effects: Cardiovascular Neurologicaltachycardiaseizureshypertensioncerebral hemorrhagechest painheadacheventricular fibrillation tremorsdizzinessGastrointestinalanxietynausea/vomitingAdministration:Pediatric:Onset:Duration:EMT-Basic providers are not authorized to carry theEpiPen Auto-Injector, but may assist patients withtheir own physician prescribed device.EpiPen Auto-Injector (0.3mg) IM in the upper-outerthigh. No repeat.EpiPen Jr. Auto-Injector (0.15mg) IM in the upper-outerthigh. No repeat.5-10 minutes20 minutesPrecautions:The EpiPen is for EMERGENCY SUPPORTIVE THERAPY ONLY and isnot a substitute for immediate medical care. An ALS unit must be enrouteor the patient must be transported immediately to the nearest emergencydepartment if ALS response is not available.DO NOT INJECT INTO BUTTOCKS, HANDS, FEET, OR ADMINISTERINTRAVENOUSLY. Injection into buttocks, hands or feet may result in lossof blood flow to the affected area and result in delayed absorption andtissue necrosis. Intravenous injection may result in an acute myocardialinfarction or cerebral hemorrhage.2-8
EPINEPHRINE HYDROCHLORIDE (Adrenalin ® )EPIPEN AUTO-INJECTOR(Continued)Only administer if solution is clear and not expired. A solution that isdiscolored, contains particles, or if outdated may be chemically alteredand may lose its potency or result in muscle damage.Note:The EpiPen contains 2ml (2mg) of epinephrine. The Auto-Injectordelivers 0.3ml (0.3mg); approximately 1.7ml remains in the pen afteractivation.Anaphylaxis may be caused by insect stings or bites, foods, drugs, otherallergens, exercise, or may be spontaneous.Signs/symptoms of anaphylaxis: flushed skin, nervousness, syncope,tachycardia, thready or unobtainable pulse, hypotension, convulsions,vomiting, diarrhea, abdominal cramps, urinary incontinence, wheezing,stridor, difficulty breathing, itching, rash, hives, and generalized edema.Directions for Using EpiPen Auto-Injector1. Pull off gray safety cap.2. Cleanse injection site with alcohol swab.**3. Place black tip on the upper-outer thigh, at right angle to theleg.4. Press EpiPen hard into thigh until Auto-Injector activates andhold in place for several seconds.5. Remove EpiPen and place in needle container.6. Massage the injection site for 10 seconds with alcohol swab.** Patient's may have been instructed that they can use EpiPen throughclothing. This is not recommended for basic life support providers.(1/00)Included in Los Angeles County "Expanded" Scope of Practice.2-9
FOLIC ACID (Vitamin B 9 ) INFUSIONClassification:Action:Indication:Ë Nutritional supplement (water soluble vitamin)Ë Aids in the development of red and white blood cellsand formation of plateletsË Suspected malnutrition, especially in the presence ofchronic alcohol abuse, poor diet, and impaired foodabsorptionContraindications: Ë Not significant during interfacility transportAdverse Effects:Administration:Pediatric:Ë Not significant during interfacility transportMay transport a maximum IV solution concentration of1mg/1000ml IV solution. Infusion must be adjusted to aTKO rate by hospital personnel.Concentration same as adult. Infusion must be on avolume-control set and adjusted to a TKO rate byhospital personnel.Precautions:Check IV site frequently and if infiltration is noted, turn off IV drip. IV mayinfiltrate during transport.Note:Folic acid may be administered in conjunction with multi-vitamin infusion.(1/00)Included in Los Angeles County "Expanded" Scope of Practice2-10
INSULINviaPATIENT-CONTROLLED PUMPClassification:Action:Indication:Ë Hypoglycemic agentË Decreases blood sugarË Insulin dependent diabetesContraindications: Ë Not significant during interfacility transportAdverse Effects:Administration:Pediatric:Ë HypoglycemiaEMT-Basic providers may not activate or adjustinfusion pump.May transport patients with either an internal orexternal administration pump. Medication infusion isprogrammed for the individual patient and may only beactivated by patient or caregiver.Same as adultPrecautions:Evaluate level of consciousness and behavior frequently. Patients mayexperience hypoglycemia; If mild signs/symptoms develop, administeroral hyperglycemic agent.Note:Signs/symptoms of hypoglycemia: nervousness, trembling, irritability,combative behavior, weakness, incoordination, confusion, weak andrapid pulse, cold and clammy skin, drowsiness, seizures, and alteredlevel of consciousness.(1/00)Included in Los Angeles County "Expanded" Scope of Practice2-11
LACTATED RINGER'S SOLUTIONClassification:Action:Ë Isotonic solution (crystalloid)Ë Replaces fluid and electrolytes lost from theintravascular and intracellular spacesIndications: Ë Initial fluid replacement for hypovolemia anddehydrationË IV access for drug administrationContraindications: Ë Not significant during interfacility transportAdverse effects:Administration:Pediatrics:Onset:Duration:Ë Circulatory fluid volume overloadMay transport with infusion adjusted to a TKO rate byhospital personnel.Must transport with a volume-control set and rate mustbe adjusted to a TKO rate by hospital personnel.Immediate< 1 hourPrecautions:Monitor infusion rate frequently. Infusion may result in fluid overload.Check IV site frequently and if infiltration is noted, turn off IV drip. IV mayinfiltrate during transport.Note:Signs of fluid overload: distended neck veins (JVD), rapid respirations,shallow tidal volume, fine auscultatory crackles, dyspnea, and peripheraledema.Signs of infiltration: swelling and pain around IV site. (1/00)2-12
Classification:Actions:Indications:MEPERIDINE HYDROCHLORIDE (DEMEROL ® )viaPATIENT-CONTROLLED ANALGESIC PUMPË Narcotic analgesicË Alters pain perception and produces euphoriaË Moderate to severe painContraindications: Ë Not significant during interfacility transportAdverse effects: Cardiovascular NeurologicaltachycardiasedationbradycardiadizzinesshypotensionheadachehypertensionconfusiontremorsRespiratoryseizuresdepressionhallucinationsarrestGastrointestinalnausea/vomitingAdministration:Pediatric:Onset:Duration:EMT-Basic providers may not activate or adjustinfusion pump.May transport with locked settings. Medication infusionis programmed for individual patient and may only beactivated by patient or caregiver.Same as adult2-5 minutesIndividual per patient programPrecautions:Monitor pulse quality and blood pressure. Infusion may cause hypotension.If hypotension persists, place patient in shock position.Monitor respiratory status frequently and ventilate with bag-valve maskdevice if necessary. Infusion may cause respiratory depression or arrest.Note:There are different Patient-Controlled Analgesic pumps. Transferringpersonnel must provide the EMT-B provider with emergency shut offinstructions regarding the specific pump used. (1/00)Included in Los Angeles County "Expanded" Scope of Practice2-13
Classification:Actions:Indications:MORPHINE <strong>SULFATE</strong>viaPATIENT-CONTROLLED ANALGESIC PUMPË Narcotic analgesicË Alters pain perception and produces euphoriaË Moderate to severe painContraindications: Ë Not significant during interfacility transportAdverse effects: Cardiovascular NeurologicaltachycardiasedationbradycardiadizzinesshypotensionheadachehypertensionconfusiontremorsRespiratoryseizuresdepressionhallucinationsarrestGastrointestinalnausea/vomitingAdministration:Pediatric:Onset:Duration:EMT-Basic providers may not activate or adjustinfusion pump.May transport with locked settings. Medication infusionis programmed for individual patient and may only beactivated by patient or caregiver.Same as adult2-5 minutesIndividual per patient programPrecautions:Monitor pulse quality and blood pressure. Infusion may cause hypotension.If hypotension persists, place patient in shock position.Monitor respiratory status frequently and ventilate with bag-valve maskdevice if necessary. Infusion may cause respiratory depression or arrest.Note:There are different types of Patient-Control Analgesic pumps. Transferringpersonnel must provide the EMT-B provider with emergency shut offinstructions regarding the specific pump used. (1/00)Included in Los Angeles County "Expanded" Scope of Practice2-14
MULTI-VITAMIN INFUSIONClassification:Action:Indication:Ë Nutritional supplementË Vitamins are organic compounds needed for growth,resistance to infection, and normal metabolismË Suspected malnutritionContraindications: Ë Not significant during interfacility transportAdverse Effects:Administration:Pediatrics:Ë Not significant during interfacility transportMay transport a maximum concentration of 1 vial/1000mlIV solution. Infusion must be adjusted to a TKO rate byhospital personnel/home health personnel.Concentration same as adult. Infusion must be on avolume-control set and adjusted to a TKO rate byhospital/home health personnel.Precautions:Check IV site frequently; if infiltration is noted, turn off IV drip. IV mayinfiltrate during transport.Note:Multi-vitamins for infusion contain both water and fat soluble vitamins.When added to an IV infusion, it gives a yellow color to the fluid. (1/00)Included in Los Angeles County "Expanded" Scope of Practice2-15
NITROGLYCERINTABLETS or LINGUAL AEROSOL (Nitrolingual ® Spray)Classification:Actions:Indications:Ë VasodilatorË Dilates blood vesselsË Dilates coronary arteriesË Decreases the workload of the heartË Chest painContraindications: Ë Blood pressure below 100 systolicË Patient has taken three doses prior to the arrival ofEMT-B providersË Sildenafil citrate (Viagra ® ) taken within 24 hoursAdverse effects: Cardiovascular Neurologicalhypotensionthrobbing headachebradycardiadizziness/faintnessreflex tachycardiaconfusionrebound hypertension blurred visionAdministration:TabletSprayPediatric:Onset:Duration:Gastrointestinalnausea/vomitingdry mouthGeneralflushed skinsublingual burningEMT-Basic providers are not authorized to carrynitroglycerin tablets or aerosol, but may assistpatients with their own physician prescribedmedication.1 tablet (1/150gr or 0.4mg) SL1 spray (0.4mg) SL or TM (transmucosal)Not recommended for prehospital use1-3 minutes30-60 minutesPrecautions:Nitroglycerin administration is for EMERGENCY SUPPORTIVE THERAPYONLY and is not a substitute for immediate medical care. An ALS unitmust be enroute or the patient must be transported immediately to thenearest emergency department if ALS response is not available.DO NOT ADMINISTER IF BLOOD PRESSURE IS BELOW 100SYSTOLIC. May cause hypotension due to vasodilation. Always takeblood pressure before and 5 minutes after administration of Nitroglycerin.2-16
NITROGLYCERINTABLETS OR LINGUAL AEROSOL (Nitrolingual ® Spray)(Continued)DO NOT SHAKE CONTAINER. One spray delivers 0.4mg of nitroglycerin.If the container is shaken it will alter the dose delivered.INSTRUCT PATIENT NOT TO INHALE SPRAY. Inhaling spray affectsabsorption rate.Note:Directions for Administering Nitroglycerin Tablets1. DO NOT ADMINISTER IF B/P IS BELOW 100 SYSTOLIC. Takeblood pressure before administration.2. Place tablet under tongue and instruct patient not to swallow, butto allow tablet to dissolve under tongue.3. Retake blood pressure and pulse after 5 minutes. If hypotensiondevelops, place patient in shock position.Directions for Administering Nitroglycerin Aerosol1. DO NOT ADMINISTER IF B/P IS BELOW 100 SYSTOLIC. Takeblood pressure before administration.2. Instruct patient not to inhale spray and do not shake container.3. Administer spray on or under the tongue.4. Retake blood pressure and pulse after 5 minutes. If hypotensiondevelops, place patient in shock position. (1/00)Included in Los Angeles County "Expanded" Scope of Practice2-17
OXYGENClassification:Actions:Indications:Ë Gaseous element (21% of room air)Ë Essential element for normal metabolic function(aerobic metabolism)Ë Assists in the breakdown of glucose into a useableenergy formË HypoxemiaË Increased oxygen demandË Chest pain of myocardial originË Respiratory insufficiencyË Cardiopulmonary arrestContraindications: Ë Not significant in above indicationsAdverse effects:Administration:Ë Not significant in above indicationsOxygen percentage may vary slightly depending ontechnique and equipment.Delivery Device Flow Rate DeliveredNasal Cannula 2-6 L/min 23-44%Face Mask 8-15 L/min 40-60%Face Mask with O 2 Reservoir6-10 L/min 60-95%Bag-Valve-Mask with O 2Reservoir 10-15 L/min 40-90%ET -- Bag-Valve Device with O 2Reservoir 10-15 L/min 100%ET -- T-tube 10-15 L/min 60-70%ETC (combitube) -- Bag-ValveDevice with O 2 Reservoir 10-15 L/min 40-90%Pediatric:Same as adult except the ETC (combitube) is contraindicated inpediatric patients less than 4 feet tall.2-18
OXYGEN(Continued)Onset:Duration:1-2 minutesUp to 30 minutesPrecautions:Observe the patient closely for changes in respiratory and mental status.Be prepared to assist ventilations if necessary. In some CO 2 retainingCOPD patients, administration of oxygen may decrease their respiratorydrive.DO NOT ADMINISTER MORE THAN 6 L/MIN VIA NASAL CANNULA.Oxygen is not humidified and may dry out or irritate mucus membranes.DO NOT USE HIGH FLOW OXYGEN-POWERED-BREATHING-DEVICESIN PEDIATRIC PATIENTS LESS THAN 12 YEARS OF AGE OR INCONJUNCTION WITH AN ET TUBE. These devices may result in gastricdistention or pneumothorax due to high pressures.Note:Oxygen should never be withheld from a patient in respiratory distress.High flow oxygen-powered-breathing-devices are manually triggered, ordemand valves which have a flow rate of 100 liters/minute. (1/00)2-19
POTASSIUM CHLORIDE (KCl) INFUSIONClassification:Actions:.Indications:Ë ElectrolyteË Regulates nerve conduction and muscle contractionË Potassium deficiencyContraindications: Ë Not significant during interfacility transportAdverse effects: Cardiovascular Neurologicaldysrhythmiasparesthesiaarrestmuscular paralysisconfusionRespiratorydepressionGeneralarresthyperkalemiavenous thrombosisGastrointestinalnausea/vomitingabdominal painAdministration:Pediatric:Infusion pump is required. Rate must be adjustedby hospital personnel.May transport a maximum IV solution concentration of20mEq/1000ml IV solution.Same as adult. Infusion must be on a volume-controlset and adjusted to a TKO rate by hospital personnel.Precautions:Monitor pulse periodically for irregularity; if change in regularity occurs, turnof IV drip. KCl may cause dysrhythmias.Check IV site frequently for infiltration; if present, turn off IV drip. IV mayinfiltrate during transport, and cause tissue necrosis.Note:If concentration is greater than 20mEq/1000ml of IV solution, patient mustbe transported by ALS unit and patient placed on an ECG monitor. (1/00)Included in Los Angeles County "Expanded" Scope of Practice2-20
SODIUM CHLORIDE 0.9% (Normal Saline) SOLUTIONClassification:Actions:Indications:Ë Isotonic solutionË Replaces fluid and sodium lost from the intravascularand intracellular spacesË Initial fluid replacement for hypovolemia,dehydration, and crush syndromeË Intravenous access for drug administrationContraindications: Ë Not significant during interfacility transportAdverse effects:Administration:Pediatric:Onset:Duration:Ë Circulatory fluid volume overloadMay transport with infusion adjusted to a TKO rate byhospital personnel.Must transport with a volume-control set and the rateadjusted to a TKO rate by hospital personnel or fieldparamedic in a multiple casualty situation.Immediate< 1 hourPrecautions:Infusion may result in fluid overload. Monitor infusion rate frequently; ifsigns/symptoms of fluid overload, turn off IV dripIV may infiltrate during transport. Check IV site frequently; if infiltrationnoted, turn off IV drip.Note:Signs of fluid overload: distended neck veins (JVD), rapid respirations,shallow tidal volume, fine auscultatory crackles, dyspnea, and peripheraledema.Signs of infiltration: swelling and pain around IV site.(1/00)2-21
THIAMINE (Vitamin B 1 ) INFUSIONClassification:Action:Indication:Ë Nutritional supplement (water soluble vitamin)Ë Aids in metabolizing carbohydrates, fats and aminoacids and detoxifying alcoholË Suspected malnutrition, especially in the presence ofchronic alcohol abuseContraindications: Ë Not significant during interfacility transportAdverse Effects:Administration:Pediatric:Ë Not significant during interfacility transportMay transport a maximum IV solution concentration of100mg/1000ml IV solution. Infusion must be adjustedto a TKO rate by hospital/home health personnel.Concentration same as adult. Infusion must be on avolume-control set and rate adjusted to a TKO rate byhospital/home health personnel.Precautions:Check IV site frequently; if infiltration noted, turn off IV drip. There is apotential for IV to infiltrate during transport.Note:Thiamine may be administered in conjunction with multi-vitamininfusion.(1/00)Included in Los Angeles County "Expanded" Scope of Practice2-22
TOTAL PARENTERAL NUTRITION (TPN)Classification:Actions:.Indications:Ë Caloric agentË Provides total nutritional needs to sustain lifeË Patients unable to take food orally or absorbadequate nutrition through the gastrointestinal tractContraindications: Ë Not significant during interfacility transportAdverse effects:Administration:Pediatric:Ë Not significant during interfacility transportMust transport with an infusion pump. The infusion isadjusted for the individual patient and the rate mayonly be adjusted by hospital or home health personnel.Same as adultPrecautions:Prevent separation of IV tubing. A break in the system may result in anair embolism which may be fatal.Prevent disruption of infusion and insure that an adequate amount ofTPN solution is available throughout transport. Interruption of TPNinfusions may result in hypoglycemia.(1/00)Included in Los Angeles County "Expanded" Scope of Practice2-23