PROGRAM
1G506sT
1G506sT
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
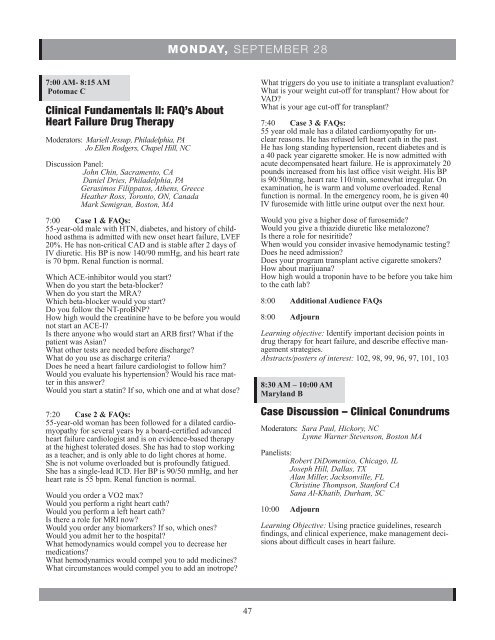
MONDAY, SEPTEMBER 28<br />
7:00 AM- 8:15 AM<br />
Potomac C<br />
Clinical Fundamentals II: FAQ’s About<br />
Heart Failure Drug Therapy<br />
Moderators: Mariell Jessup, Philadelphia, PA<br />
Jo Ellen Rodgers, Chapel Hill, NC<br />
Discussion Panel:<br />
John Chin, Sacramento, CA<br />
Daniel Dries, Philadelphia, PA<br />
Gerasimos Filippatos, Athens, Greece<br />
Heather Ross, Toronto, ON, Canada<br />
Mark Semigran, Boston, MA<br />
7:00 Case 1 & FAQs:<br />
55-year-old male with HTN, diabetes, and history of childhood<br />
asthma is admitted with new onset heart failure, LVEF<br />
20%. He has non-critical CAD and is stable after 2 days of<br />
IV diuretic. His BP is now 140/90 mmHg, and his heart rate<br />
is 70 bpm. Renal function is normal.<br />
Which ACE-inhibitor would you start?<br />
When do you start the beta-blocker?<br />
When do you start the MRA?<br />
Which beta-blocker would you start?<br />
Do you follow the NT-proBNP?<br />
How high would the creatinine have to be before you would<br />
not start an ACE-I?<br />
Is there anyone who would start an ARB first? What if the<br />
patient was Asian?<br />
What other tests are needed before discharge?<br />
What do you use as discharge criteria?<br />
Does he need a heart failure cardiologist to follow him?<br />
Would you evaluate his hypertension? Would his race matter<br />
in this answer?<br />
Would you start a statin? If so, which one and at what dose?<br />
7:20 Case 2 & FAQs:<br />
55-year-old woman has been followed for a dilated cardiomyopathy<br />
for several years by a board-certified advanced<br />
heart failure cardiologist and is on evidence-based therapy<br />
at the highest tolerated doses. She has had to stop working<br />
as a teacher, and is only able to do light chores at home.<br />
She is not volume overloaded but is profoundly fatigued.<br />
She has a single-lead ICD. Her BP is 90/50 mmHg, and her<br />
heart rate is 55 bpm. Renal function is normal.<br />
Would you order a VO2 max?<br />
Would you perform a right heart cath?<br />
Would you perform a left heart cath?<br />
Is there a role for MRI now?<br />
Would you order any biomarkers? If so, which ones?<br />
Would you admit her to the hospital?<br />
What hemodynamics would compel you to decrease her<br />
medications?<br />
What hemodynamics would compel you to add medicines?<br />
What circumstances would compel you to add an inotrope?<br />
What triggers do you use to initiate a transplant evaluation?<br />
What is your weight cut-off for transplant? How about for<br />
VAD?<br />
What is your age cut-off for transplant?<br />
7:40 Case 3 & FAQs:<br />
55 year old male has a dilated cardiomyopathy for unclear<br />
reasons. He has refused left heart cath in the past.<br />
He has long standing hypertension, recent diabetes and is<br />
a 40 pack year cigarette smoker. He is now admitted with<br />
acute decompensated heart failure. He is approximately 20<br />
pounds increased from his last office visit weight. His BP<br />
is 90/50mmg, heart rate 110/min, somewhat irregular. On<br />
examination, he is warm and volume overloaded. Renal<br />
function is normal. In the emergency room, he is given 40<br />
IV furosemide with little urine output over the next hour.<br />
Would you give a higher dose of furosemide?<br />
Would you give a thiazide diuretic like metalozone?<br />
Is there a role for nesiritide?<br />
When would you consider invasive hemodynamic testing?<br />
Does he need admission?<br />
Does your program transplant active cigarette smokers?<br />
How about marijuana?<br />
How high would a troponin have to be before you take him<br />
to the cath lab?<br />
8:00 Additional Audience FAQs<br />
8:00 Adjourn<br />
Learning objective: Identify important decision points in<br />
drug therapy for heart failure, and describe effective management<br />
strategies.<br />
Abstracts/posters of interest: 102, 98, 99, 96, 97, 101, 103<br />
8:30 AM – 10:00 AM<br />
Maryland B<br />
Case Discussion – Clinical Conundrums<br />
Moderators: Sara Paul, Hickory, NC<br />
Lynne Warner Stevenson, Boston MA<br />
Panelists:<br />
Robert DiDomenico, Chicago, IL<br />
Joseph Hill, Dallas, TX<br />
Alan Miller, Jacksonville, FL<br />
Christine Thompson, Stanford CA<br />
Sana Al-Khatib, Durham, SC<br />
10:00 Adjourn<br />
Learning Objective: Using practice guidelines, research<br />
findings, and clinical experience, make management decisions<br />
about difficult cases in heart failure.<br />
47