00050
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
IJRPC 2011, 1(3) Srinivasan et al. ISSN: 22312781<br />
INTERNATIONAL JOURNAL OF RESEARCH IN PHARMACY AND CHEMISTRY<br />
Available online at www.ijrpc.com<br />
Review Article<br />
ADVERSE DRUG REACTION-CAUSALITY ASSESSMENT<br />
Srinivasan R* and Ramya G<br />
PES College of Pharmacy, Department of Pharmacy Practice, 50 Ft. Road, Hanumanth Nager,<br />
Bangalore, Karnataka, India.<br />
*Corresponding Author: cdmseena@gmail.com<br />
INTRODUCTION<br />
Adverse drug reactions (ADRs) are considered<br />
as one among the leading causes of morbidity<br />
and mortality 1 . .The epidemiological<br />
importance of ADR is justified by its high<br />
prevalence rate – they cause from 3% to 6% of<br />
hospital admissions at any age, and up to 24%<br />
in the elderly population; they rank fifth<br />
among all causes of death and, moreover, they<br />
represent from 5 to 10% of hospital costs 2 . and<br />
is a great cause of concern to the medical<br />
profession. Every occasion when a patient is<br />
exposed to a medical product, is a unique<br />
situation and we can never be certain about<br />
what might happen. A good example for this<br />
is thalidomide tragedy in late 1950s and<br />
1960s.Thalidomide prescribed as a safe<br />
hypnotic to many thousands of pregnant<br />
women caused severe form of limb<br />
abnormality known as phocomelia in many of<br />
the babies born to those women. It was a<br />
seminal event that led to the development of<br />
modern drug regulations aimed to identify,<br />
confirm and quantify ADRs. An adverse drug<br />
reaction (ADR) is any undesirable effect of a<br />
drug beyond anticipated therapeutic effects<br />
occurring during clinical use 14 . Hence every<br />
health care professional who give advice to<br />
patients need to know the frequency and<br />
magnitude of the risks involved in medical<br />
treatment along with its beneficial effects.<br />
Recent epidemiological studies estimated that<br />
ADRs are fourth to sixth leading cause of<br />
death 3 . It has been estimated that<br />
approximately 2.9-5% of all hospital admission<br />
are caused by ADRs and as many as 35% of<br />
hospitalised patients experience an ADR<br />
during their hospital stay 4 . An incidence of<br />
fatal ADRs is 0.23%-0.4%. 5 Although many of<br />
the ADRs are relatively mild and disappear<br />
when drug is stopped or dose is reduced,<br />
others are more serious and last longer.<br />
Therefore there is a little doubt that ADRs<br />
increase not only morbidity and mortality but<br />
also add to the overall health care cost 6, 7 .<br />
Adverse drug reaction (ADR)<br />
Definitions of ADRs exist, including those of<br />
the World Health Organization (WHO) 8 .<br />
Karch and Lasagna 9 and the Food and Drug<br />
Administration (FDA) 10 .<br />
WHO<br />
Any response to a drug which is noxious and<br />
unintended, and which occurs at doses<br />
normally used in man for prophylaxis,<br />
diagnosis, or therapy of disease, or for the<br />
modification of physiological function.<br />
Karch and Lasagna<br />
Any response to a drug that is noxious and<br />
unintended, and that occurs at doses used in<br />
humans for prophylaxis, diagnosis, or therapy,<br />
excluding failure to accomplish the intended<br />
purpose.<br />
FDA<br />
For reporting purposes, FDA categorizes a<br />
serious adverse event (events relating to drugs or<br />
devices) as one in which “the patient outcome<br />
is death, life-threatening (real risk of dying),<br />
hospitalization (initial or prolonged), disability<br />
(significant, persistent, or permanent),<br />
congenital anomaly, or required intervention<br />
to prevent permanent impairment or damage.<br />
Classification of Adverse Drug Reactions<br />
ADRs can be divided schematically into two<br />
major categories:<br />
606
IJRPC 2011, 1(3) Srinivasan et al. ISSN: 22312781<br />
Type A and Type B (Table 1).<br />
Type A reactions are common, predictable and<br />
may occur in any individual. Type B ADRs are<br />
uncommon and unpredictable and only occur<br />
in susceptible individuals 11 .<br />
Type A reactions are the most frequent and<br />
can be observed in as many as 25–45% of<br />
patients. These represent an exaggeration of<br />
the known primary and/or secondary<br />
pharmacological actions of the drug, they are<br />
dose related and could probably be avoided<br />
and/or foreseen 12 . Multi-factorial, involving<br />
not only defects at multiple gene loci but also<br />
environmental factors such as concomitant<br />
infections. Most work has focused on enzyme<br />
polymorphism in drug oxidation and<br />
conjugation as risk factors for drug toxicity but<br />
genes involved in cell repair mechanisms,<br />
elaboration of cytokines and immune<br />
responsiveness cannot be excluded to predict<br />
individual susceptibility to different forms of<br />
ADRs 12,14 . . Genetic polymorphisms are a<br />
source of variation of drug response in the<br />
human body. In relation to ADRs, most<br />
interest has centred on the involvement of<br />
pharmacokinetic factors and, in particular,<br />
drug metabolism. However, there is now<br />
increasing realization that genetic variation in<br />
drug targets (Pharmacodynamic factors) might<br />
also predispose to ADRs, although research<br />
into this area is in its infancy 15 .<br />
Mechanism by which ADR Occurs 16<br />
ADRs can be classified as either<br />
pharmacological reactions representing an<br />
augmentation of the known pharmacological<br />
actions of the drug or idiosyncratic reactions<br />
that are not predictable. Pharmacological<br />
reactions are most common, usually doserelated<br />
and are due to the primary or<br />
secondary pharmacological characteristics of<br />
the drug. Factors that predispose to these<br />
ADRs include dose, pharmaceutical variation<br />
in drug formulation, pharmacokinetic or<br />
pharmacodynamic abnormalities, and drugdrug<br />
interactions. Pharmacological ADRs<br />
occur when drug concentration in plasma or<br />
tissue exceeds the “therapeutic window” or<br />
when there is increased sensitivity to the drug<br />
(even in concentrations considered normal for<br />
the general population). Idiosyncratic ADRs<br />
are less common, often serious, not dose<br />
dependent and show no simple relationship<br />
between the dose and the occurrence of<br />
toxicity or the severity of the reaction. The<br />
toxic reactions may affect many organ systems<br />
either in isolation or combination. The<br />
mechanism of these is not clear but is thought<br />
to include receptor abnormality, abnormality<br />
of a biological system that is unmasked by the<br />
drug, immunological response, drug-drug<br />
interactions, or be multi-factorial.<br />
Adverse drug reaction (ADR) monitoring<br />
involves following steps<br />
1. Identifying adverse drug reaction<br />
(ADR).<br />
2. Assessing causality between drug and<br />
suspected reaction by using various<br />
algorithms.<br />
3. Documentation of ADR in patient’s<br />
medical records.<br />
4. Reporting serious ADRs to<br />
pharmacovigilance centres /ADR<br />
regulating authorities<br />
Identifying the Adverse Drug Reaction<br />
The ADRs produced by a certain new drug are<br />
often recognized when the medication is<br />
undergoing its phase three randomized<br />
controlled trials. Both in the USA and in the<br />
UK there is post marketing surveillance of<br />
ADRs. In the UK this involves reporting<br />
suspected ADRs to the Commission on<br />
Human Medicine using the yellow card<br />
system. In this system new or intensively<br />
monitored medicines should have all<br />
suspected ADRs reported and other medicines<br />
should have any suspected serious ADR<br />
reported. In spite of these mechanisms ADRs<br />
are vastly under reported, 17 and initial reports<br />
of adverse reactions to drugs have taken up to<br />
seven years for trends to begin to appear in the<br />
literature. Under reporting of ADRs is likely to<br />
be due to a number of reasons. Reporting is<br />
not mandatory to clinicians in the UK and so is<br />
likely to be forgotten about amongst the many<br />
other work pressures. A clinician may have<br />
problems recognizing the scenario as an ADR,<br />
because of the background symptoms of the<br />
patient’s original illness. Clinicians might also<br />
be wary of reporting an ADR, because of<br />
worries of inducing a complaint, even in this<br />
no blame culture NHS. It should be pointed<br />
out that the yellow card clearly states you do<br />
not need to be sure if it is or is not an ADR<br />
before you report it. In recognizing an ADR<br />
there are a number of important factors one is<br />
identifying those individuals in whom ADRs<br />
are most likely to occur. This includes the aged<br />
and the premature, those with liver<br />
607
IJRPC 2011, 1(3) Srinivasan et al. ISSN: 22312781<br />
Post marketing surveillance<br />
Post marketing surveillance can be done by<br />
different methods:<br />
Anecdotal reporting 18<br />
The majority of the first reports of ADR come<br />
through anecdotal reports from individual<br />
doctors when a patient has suffered some<br />
peculiar effect. Such anecdotal reports need to<br />
be verified by further studies and these<br />
sometimes fail to confirm problem.<br />
Intensive monitoring studies 19,24<br />
These studies provide systematic and detailed<br />
collection of data from well defined groups of<br />
inpatients .The surveillance was done by<br />
specially trained health care professionals who<br />
devote their full time efforts towards<br />
recording all the drugs administered and all<br />
the events, which might conceivably be drug<br />
induced. Subsequently, statistical screening for<br />
drug-event association may lead to special<br />
studies. Popular example for this methodology<br />
is Boston collaborative drug surveillance<br />
program.<br />
Spontaneous reporting system (SRS) 20<br />
It is the principal method used for monitoring<br />
the safety of marketed drugs. In UK, USA,<br />
India and Australia, the ADR monitoring<br />
programs in use are based on spontaneous<br />
reporting systems. In this system, clinicians<br />
encourage reporting any or all reactions that<br />
believe may be associated with drug use<br />
usually, attention is focused on new drugs and<br />
serious ADRs. The rationale for SRS is to<br />
generate signals of potential drug problems, to<br />
identify rare ADRs and theoretically to<br />
monitor continuously all drug used in a<br />
variety of real conditions from the time they<br />
are first marketed. 15<br />
Cohort studies (Prospective studies) 19<br />
In these studies, patients taking a particular<br />
drug are identified and events are then<br />
recorded. The weakness of this method is<br />
relatively small number patients likely to be<br />
studied, and the lack of suitable control group<br />
to assess the background incidence of any<br />
adverse events. Such studies are expensive<br />
and it.<br />
Case control studies (retrospective studies) 18<br />
In these studies, patients who present with<br />
symptoms or an illness that could be due to an<br />
adverse drug reaction are screened to see if<br />
they have taken the drug. The prevalence of<br />
drug taking in this group is then compared<br />
with the prevalence in a reference population<br />
who do not have the symptoms or illness. The<br />
case control study is thus suitable for<br />
determining whether the drug causes a given<br />
adverse event once there is some initial<br />
indication that it might. However, it is not a<br />
method for detecting completely new adverse<br />
reactions.<br />
Case cohort studies 18<br />
The case cohort study is a hybrid of<br />
prospective cohort study and retrospective<br />
case control study, Patients who present with<br />
symptoms or an illness that could be due to an<br />
adverse drug reaction are screened to see if<br />
they have taken the drug. The results are then<br />
compared with the incidence of the symptoms<br />
or illness in a prospective cohort of patients<br />
who are taking the drug.<br />
Record linkage 18<br />
The idea here is to bring together a variety of<br />
patient records like general practice records of<br />
illness events and general records of<br />
prescriptions. In this way it may be possible to<br />
match illness events with drugs prescribed. A<br />
specific example of the use of record linkage is<br />
the so called prescription event monitoring<br />
scheme in which all the prescriptions issued<br />
by selected parishioners for a particular drug<br />
are obtained from the prescription pricing<br />
authority. The prescribers are then asked to<br />
inform those running scheme of any events in<br />
the patients taking the drugs. This scheme is<br />
less expensive and time consuming than other<br />
surveillance methods<br />
Meta analysis 21<br />
Meta analysis is a quantitative analysis of two<br />
or more independent studies for the purpose<br />
of determining an overall effect and of<br />
describing reasons for variation in study<br />
results, is another potential tool for identifying<br />
ADRs and assessing drug safety.<br />
Use of population statistics 22<br />
Birth defect registers and cancer registers can<br />
be used If drug induced event is highly<br />
remarkable or very frequent. If suspicions are<br />
aroused then case control and observational<br />
cohort studies will be initiated.<br />
608
IJRPC 2011, 1(3) Srinivasan et al. ISSN: 22312781<br />
II. Causality Assessment Between Drug and<br />
Suspected reaction 23<br />
Causality assessment is the method by which<br />
the extent of relationship between a drug and<br />
a suspected reaction is established.<br />
It is often difficult to decide if an adverse<br />
clinical event is an ADR or due to<br />
deterioration in the primary condition.<br />
Furthermore, if it is an ADR, which medicine<br />
caused it, as many patients are on multiple<br />
new medications when ill, particularly if<br />
admitted to hospital. In spite of these<br />
problems, the decision that a particular drug<br />
caused an ADR is usually based on clinical<br />
judgment alone. Studies have shown that there<br />
is a lot of variation in between rater and<br />
within rater decisions on causality of ADRs;<br />
this applies both to pharmacologists and<br />
physicians 25,26 .<br />
There are various approaches in the first<br />
approach an individual who is an expert in<br />
the area of ADRs would evaluate the case. In<br />
the process of evaluation, he or she may<br />
consider and critically evaluate all the data<br />
obtained to assess whether the drug has<br />
caused the particular reaction. A panel of<br />
experts adopts a similar procedure to arrive at<br />
a collective opinion. using algorithms<br />
including standardization of methods.<br />
Algorithms being structured systems<br />
specifically designed for the identification of<br />
an ADR, should theoretically make a more<br />
objective decision on causality. As such<br />
algorithms should have a better between and<br />
within rater agreement than clinical judgment.<br />
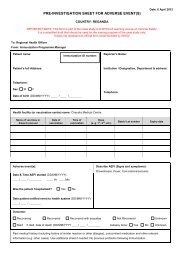
A number of algorithms or decision aids have<br />
been published including the Jones’<br />
algorithm, 28 the Naranjo algorithm, 27 the<br />
Yalealgorithm, 29 the Karch algorithm, 30 the<br />
Begaud algorithm, 31 the ADRAC, 32 the WHO-<br />
UMC, 33 and a newer quantitative approach<br />
Algorithm.34 Each of these algorithms has<br />
similarities and differences. And the most<br />
commonly used algorithms; the Naranjo<br />
algorithm (Fig :1) is shown below<br />
The Naranjo Algorithm is a questionnaire<br />
designed by Naranjo et al for determining the<br />
likelihood of whether an ADR (adverse drug<br />
reaction) is actually due to the drug rather<br />
than the result of other factors. Probability is<br />
assigned via a score termed definite, probable,<br />
possible or doubtful. Values obtained from the<br />
algorithm are sometimes used in peer reviews<br />
to verify the validity of author’s conclusions<br />
regarding adverse drug reactions. It is also<br />
called the Naranjo Scale or Naranjo Score.<br />
III. Documentation of ADRs in Patient’s<br />
Medical Records<br />
This aids as reference for alerting clinicians<br />
and other health care professionals to the<br />
possibility of a particular drug causing<br />
suspected reaction.<br />
IV. Reporting Serious ADRs to<br />
Pharmacovigilance Centres / ADR<br />
Regulating Authorities<br />
According to FDA, a serious reaction is<br />
classified as one which is fatal, life threatening,<br />
prolonging hospitalisation, and causing a<br />
significant persistent disability, resulting in a<br />
congenital anomaly and requiring intervention<br />
to prevent permanent damage or resulting in<br />
death 35 Hatwig SC, Seigel J and Schneider PJ<br />
categorised ADRs into seven levels as per their<br />
severity. Level 1&2 fall under mild category<br />
whereas level 3& 4 under moderate and level<br />
5, 6&7 fall under severe category . 36 (fig:2). Karch<br />
and Lasanga classify severity into minor,<br />
moderate, severe and lethal. In minor severity,<br />
there is no need of antidote, therapy or<br />
prolongation of hospitalisation. To classify as<br />
moderate severity, a change in drug therapy,<br />
specific treatment or an increase in<br />
hospitalization by at least one day is required.<br />
Severe class includes all potentially life<br />
threatening reactions causing permanent<br />
damage or requiring intensive medical care.<br />
Lethal reactions are the one which directly or<br />
indirectly contributes to death of the patient.<br />
Different ADR regulatory authorities are -<br />
Committee on safety of medicine (CSM),<br />
Adverse drug reaction advisory committee<br />
(ADRAC), 37 MEDWATCH, Vaccine Adverse<br />
Event Reporting System 38 WHO-UMC<br />
international database maintains all the data of<br />
ADRs.<br />
CONCLUSION<br />
India has more than half a million qualified<br />
doctors and 15,000 hospitals having bed<br />
strength of 6, 24,000. It is the fourth largest<br />
producer of pharmaceuticals in the world. It is<br />
emerging as important clinical trial hub in the<br />
world. Many new drugs are being introduced<br />
every year and so every health care<br />
professional must have knowledge about<br />
importance of ADR monitoring and<br />
pharmacovigilance. Every health care<br />
professional should see it as a part of his/her<br />
professional duty keeping in mind about<br />
Hippocrates admonition” at least does no<br />
harm”.<br />
609
IJRPC 2011, 1(3) Srinivasan et al. ISSN: 22312781<br />
Table 1: Characteristics of Type A and Type B Adverse Reactions<br />
Characteristics Type A Type B<br />
Dose dependency Usually shows good relationship No simple relation ship<br />
Predictable from<br />
known pharmacology<br />
Yes<br />
Not usually<br />
Host factors Genetic factors might be important<br />
Dependent on host<br />
factors<br />
Frequency Common Uncommon<br />
Severity<br />
Variable but usually mild<br />
Variable,<br />
proportionately more<br />
severe<br />
Clinical burden High morbidity and low mortality<br />
High morbidity and<br />
mortality<br />
Overall portion of<br />
adverse drug reaction<br />
80% 20%<br />
First detection<br />
Phase1-III<br />
Phase IV, occasionally<br />
phase III<br />
Animal models Usually reproducible in animals<br />
No known animal<br />
models<br />
Level 1<br />
Level 2<br />
Level 3<br />
Level 4<br />
Level 5<br />
Level 6<br />
Level 7<br />
Table 2: Hartwig’s Severity Assessment Scale<br />
An ADR occurred but required no change in treatment with the suspected drug.<br />
The ADR required that treatment with the suspected drug be held, discontinued, or otherwise<br />
changed. No antidote or other treatment requirement was required. No increase in length of stay<br />
(LOS)<br />
The ADR required that treatment with the suspected drug be held, discontinued, or otherwise<br />
changed.<br />
AND/OR<br />
An Antidote or other treatment was required. No increase in length of stay (LOS)<br />
Mild= level 1 and 2, moderate= level 3 and 4, severe= 5, 6 and 7.<br />
Any level 3 ADR which increases length of stay by at least 1 day . OR<br />
The ADR was the reason for the admission<br />
Any level 4 ADR which requires intensive medical care<br />
The adverse reaction caused permanent harm to the patient<br />
The adverse reaction either directly or indirectly led to the death of the patient<br />
1) Are there previous conclusive reports of this reaction?<br />
If YES = +1, NO = 0, Do not know or not done = 0<br />
2) Did the adverse event appear after the suspected drug was Given?<br />
If YES = +2, NO = -1, Do not know or not done = 0<br />
3) Did the adverse reaction improve when the drug was discontinued or a specific antagonist was given?<br />
If YES = +1, NO = 0, Do not know or not done = 0<br />
4) Did the adverse reaction appear when the drug was Re-administered?<br />
If YES = +2, NO = -2, Do not know or not done = 0<br />
5) Are there alternative causes that could have caused the reaction?<br />
If YES = -1, NO = +2, Do not know or not done = 0<br />
6) Did the reaction reappear when a placebo was given?<br />
If YES = -1, NO = +1, Do not know or not done = 0<br />
7) Was the drug detected in any body fluid in toxic Concentrations?<br />
If YES = +1, NO = 0, Do not know or not done = 0<br />
610
IJRPC 2011, 1(3) Srinivasan et al. ISSN: 22312781<br />
8) Was the reaction more severe when the dose was increased or less severe when the dose was decreased?<br />
If YES = +1, NO = 0, Do not know or not done = 0<br />
9) Did the patient have a similar reaction to the same or similar drugs in any previous exposure?<br />
If YES = +1, NO = 0, Do not know or not done = 0<br />
10) Was the adverse event confirmed by any objective evidence?<br />
If YES = +1, NO = 0, Do not know or not done = 0<br />
SCORING<br />
9 = DEFINITE ADR, 5-8 = PROBABLE ADR,<br />
1-4 = POSSIBLE ADR , 0 = DOUBTFUL ADR<br />
Fig. 1: Naranjo Algorithm.<br />
REFERENCES<br />
1. Ditto AM. Drug allergy. In Grammer<br />
LC, Greenberger PA, editors.<br />
Patterson’s allergic diseases. 6th ed.;<br />
Philadelphia: Lippincott Williams &<br />
Wilkins. 2002;295.<br />
2. Onder G, Pedone C, Landi F, Cesari<br />
M, Della VC and Bernabei R. Adverse<br />
Drug Reactions as Cause of Hospital<br />
Admissions Results from the Italian<br />
Group of Pharmacoepidemiology in<br />
the Elderly (GIFA). J Am Geriatr Soc.<br />
2002;50(12):1962-1968.<br />
3. Brown SD and Landry FJ. Recognizing<br />
Reporting and Reducing Adverse<br />
Drug Reactions. Southern Medical<br />
Journal. 2001;94:370-372.<br />
4. Murphy BM and Frigo LC.<br />
Development, Implementation and<br />
Results of a Successful<br />
Multidisciplinary Adverse Drug<br />
Reaction Reporting Program in a<br />
University Teaching Hospital.<br />
Hospital Pharmacy.1993;28:1199-1204.<br />
5. Lazarou J, Pomeranz BH and Corey<br />
PN. Incidence of Adverse Drug<br />
Reactions in Hospitalized Patients. A<br />
Meta analysis of Prospective Studies.<br />
Journal of American medical<br />
Association. 1998;279(15):1200-1205.<br />
6. David WB, Nathan S, David JC.<br />
Elisabeth B, Nan L, Laura A and<br />
Petersen . The Cotrst of Adverse Drug<br />
Events in Hospitalized Patients.<br />
Journal of American Medical<br />
Association. 1997;277(4):307-311<br />
7. Bordet S, Gautier H, Lelouet B and<br />
Dupuis J. Caron. Analysis of the Direct<br />
Cost of Adverse Drug Reaction in<br />
Hospitalised Patients. European<br />
Journal of Clinical Pharmacology.<br />
2001; 56:935-39.<br />
8. Requirements for adverse reaction<br />
reporting. Geneva, Switzerland:<br />
World Health Organization.1975.<br />
9. Karch FE, Lasagna L. Adverse drug<br />
reactions. A Critical<br />
Review.JAMA.1975; 234:1236–41.<br />
10. Kessler DA. Introducing MedWatch,<br />
using FDA for 3500. A New Approach<br />
to Reporting Medication and Device<br />
Adverse Effects and Product<br />
problems. JAMA.1993;269:2765–68.<br />
11. Pirmohamed M and Park BK. Genetic<br />
Susceptibility to Adverse Drug<br />
Reactions. Trends Pharmacol Sci.<br />
2001;22:298–305.<br />
12. Moore N. The role of the Clinical<br />
Pharmacologist in the Management of<br />
Adverse Drug Reactions. Drug Safety<br />
2001;24:1–7.<br />
13. Knowles SR, Uetrecht J and Shear NH.<br />
Idiosyncratic Drug Reactions. The<br />
reactive Metabolite Syndromes.<br />
Lancet. 2000;356:1587–91.<br />
14. Pirmohamed M, Breckenridge AM,<br />
Kitteringham NR and Park BK.<br />
Adverse drug Reactions. BMJ.<br />
1998;316:1295–98.<br />
15. Alvarado I, Wong ML and Licinio J.<br />
Advances in the Pharmacogenomics of<br />
Adverse Reactions. Pharmacogenom J.<br />
2002;2:273.<br />
611
IJRPC 2011, 1(3) Srinivasan et al. ISSN: 22312781<br />
16. Mann R and Andrews E.<br />
Pharmacovigilance. Chichester<br />
England: John Wiley and Sons Ltd;<br />
2002.<br />
17. Laepe LL, Brennan TA and Laird N.<br />
The Nature of Adverse Events in<br />
Hospitalized Patients. Results of the<br />
Harvard Medical Practice Study II.<br />
New Engl. J Med. 1991;324:377–84.<br />
18. Graham smith DG and Ransom JK.<br />
Adverse Drug Reactions to Drugs.<br />
Oxford Text Book of Clinical<br />
Pharmacology and Drug Therapy.3rd<br />
ed. Oxford university press. 202: 101-<br />
104.<br />
19. Lee B and Turner MW. Food and Drug<br />
Administrations Adverse Drug<br />
Reaction Monitoring Program.<br />
American Journal of Hospital<br />
Pharmacy. 1978; 35: 828-832.<br />
20. MC Nell JJ, Gash EA and Mcdonald<br />
MM. Post Marketing Surveillance<br />
Strengths and Limitations. The<br />
Medical Journal of Australia.<br />
1999;170:270-273.<br />
21. Brewer T and Colditz GA. Post<br />
Marketing Surveillance and Adverse<br />
Drug Reactions. Current Prospective<br />
and needs. Journal of American<br />
Medical Association. 1999;281: 824-<br />
829.<br />
22. Laurence DR, Bennett PN and Browm<br />
MJ. Unwanted Effects and Adverse<br />
Drug Reactions. Clinical<br />
Pharmacology. Eighth ed. Churchill<br />
Livingston.1998;121-137.<br />
23. Edwards IR and Aronson JK. Adverse<br />
Drug Reactions. Definition Diagnosis<br />
and Management. Lancet. 356: 1255-59<br />
24. Hurwitz N and Wade O.L. Intensive<br />
Monitoring of Adverse Drug<br />
Reactions to Drugs. British Medical<br />
Journal. 1969;1:531-536.<br />
25. Blanc S, Leuenberger P, Berger JP,<br />
Brooke M and Schelling JL.<br />
Judgements of Trainedobservers on<br />
Adverse Drug Reactions. Clin<br />
Pharmacol Ther. 1979;25:493–98.<br />
26. Karsh FE, Smith CL, Kerzner B,<br />
Mazzullo JM, Weintraub M and<br />
Lasanga L. Adverse Drug Reactions. A<br />
Matter of Opinion. Clin Pharmacol<br />
Ther. 1976;19:489–92.<br />
27. Naranjo CA, Busto U, Sellars EM,<br />
Sandor P, Ruiz I, Roberts EA and<br />
Janecek E. Method for Estimating the<br />
Probability of Adverse Drug<br />
Reactions. Clin Pharmacol Ther.<br />
1981;30:239–45.<br />
28. Jones JK. Adverse Drug Reactions in<br />
the Community Health Setting.<br />
Approach to Recognizing, Counseling<br />
and Reporting. Fam Community<br />
Health. 1982;5(2):58–67.<br />
29. Kramer MS and Hutchinson TA. The<br />
Yale algorithm. Special workshopclinical.<br />
Drug Inf J. 1984;18:283–91.<br />
30. Karch FE and Lasagna L. Towards the<br />
Operational Identification of Adverse<br />
Drug Reaction. Clin Pharmacol Ther.<br />
1977;21:247–54.<br />
31. Begaud B, Evreux JC, Jouglard J and<br />
Lagier G. Imputation of the<br />
Unexpected or Toxic Effects of Drugs.<br />
Actualisation of the Methods Used in<br />
France. Therapie.1985;40:115–18.<br />
32. Mashford MI. The Australian Method<br />
of Drug Event Assessment. Drug Inf J.<br />
1984;18:271–73.<br />
33. WHO-UMC causality assessment<br />
system. Available from<br />
.<br />
34. Koh Y, Chu WY and Shu CL. A<br />
Quantitative Approach Using Genetic<br />
Algorithm in Designing a Probability<br />
Scoring System of an Adverse Drug<br />
Reaction Assessment System. Int J<br />
Med Inf. 2008;77:421–30.<br />
35. Hubes ML, Whittlesea CMC and<br />
Lusconbe DK. Symptoms or Adverse<br />
Reaction. An Investigation into How<br />
Symptoms are Recognized as Side<br />
Effects of Medication. Pharmacy<br />
journal. 2002;269:719-722.<br />
36. Hartwig SC, Siegel J and Schneider PJ.<br />
Preventability and Severity<br />
Assessment in Reporting Adverse<br />
Drug reactions. American Journal of<br />
Hospital Pharmacy. 1992;49:2229-31<br />
37. Information About Adverse Drug<br />
Reaction Advisory Committee<br />
(Available<br />
from<br />
URL:http//www.helth.gov.av/tga/a<br />
dr/adrfaq.htm<br />
38. Information About Vaccine Adverse<br />
Event Reporting System (Available<br />
from URL:http//www.vaers.org).<br />
612