HSS Rheumatology Annual Report 2017-2018
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
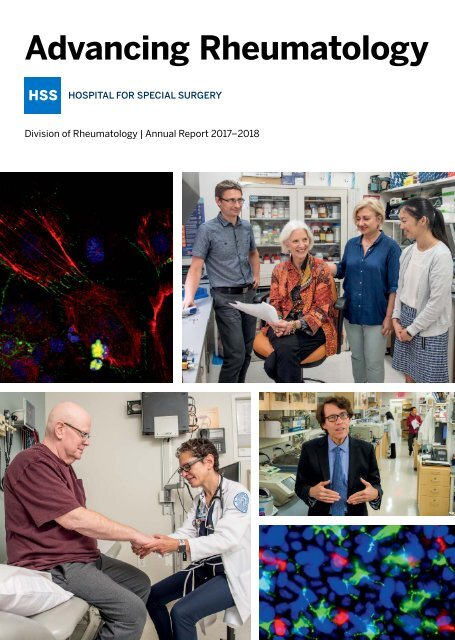
Advancing <strong>Rheumatology</strong><br />
Division of <strong>Rheumatology</strong> | <strong>Annual</strong> <strong>Report</strong> <strong>2017</strong>–<strong>2018</strong>
Table of Contents<br />
<strong>2017</strong> –<strong>2018</strong> Achievements and<br />
Fast Facts<br />
2<br />
Cutting-Edge Initiatives<br />
Identifying high-risk pregnancies<br />
in patients with lupus<br />
Improving outcomes for RA patients<br />
undergoing joint replacement<br />
Creating a better future for<br />
scleroderma patients<br />
Advancing high-value care and<br />
outcomes for patients<br />
Targeting interferon for better<br />
control of lupus<br />
Defining a new form of arthritis<br />
in cancer patients<br />
Improving bone health in patients<br />
with ankylosing spondylitis<br />
New possibilities for<br />
scleroderma treatment<br />
Using precision medicine to refine<br />
RA treatment<br />
Battling bone loss with a promising<br />
microRNA-targeting therapy<br />
Unraveling the molecular<br />
mysteries of lupus<br />
A promising new target for treating<br />
autoimmune diseases<br />
Investigating stem cells for<br />
repairing fibrotic skin<br />
Optimizing postsurgical outcomes<br />
Complex Cases<br />
Empowering Patients Through<br />
Support and Education Programs<br />
<strong>Rheumatology</strong> Leaders of the Future<br />
Notable References<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9<br />
10<br />
11<br />
12<br />
13<br />
14<br />
15<br />
16<br />
17<br />
18<br />
24<br />
26<br />
31<br />
Message from the Physician-in-Chief<br />
and Chief of the Division of<br />
<strong>Rheumatology</strong><br />
<strong>HSS</strong> rheumatologists have a long history of<br />
commitment to advancing our field through<br />
our many leadership roles, our engagement<br />
in the education of future physicians, and<br />
our contributions to unraveling the complex<br />
mechanisms responsible for autoimmune and<br />
inflammatory rheumatic diseases.<br />
I want to congratulate Anne R. Bass, MD,<br />
Attending Physician, on completing her term as<br />
Chair of the American College of <strong>Rheumatology</strong>’s<br />
(ACR) Committee on <strong>Rheumatology</strong> Training and<br />
Workforce Issues. In view of the acknowledged<br />
need to grow the number of adult rheumatologists<br />
and pediatric rheumatologists in the U.S., recruiting<br />
and training physicians is a high priority nationally<br />
and at <strong>HSS</strong>. Dr. Bass has done an outstanding<br />
job in her ACR role and as Director of the <strong>HSS</strong><br />
<strong>Rheumatology</strong> Training Program.<br />
<strong>HSS</strong> rheumatologists also have high visibility and<br />
critical roles in the programs at our academic<br />
partner institution, Weill Cornell Medicine. Jane<br />
E. Salmon, MD, Attending Physician, serves as<br />
Associate Dean for Faculty Affairs. Juliet B. Aizer,<br />
MD, Assistant Attending Physician, and Edward J.<br />
Parrish, MD, Assistant Attending Physician, have<br />
designed significant portions of the curriculum<br />
for first- and second-year medical students and<br />
guide nearly all members of our faculty in teaching<br />
activities at the medical school.<br />
“<strong>HSS</strong> rheumatologists and scientists are revolutionizing the care of patients<br />
with some of the most challenging, complex medical conditions through<br />
transformative research and global professional education.”<br />
— Louis A. Shapiro, President and Chief Executive Officer, and Todd J. Albert, MD, FACS,<br />
Surgeon-in-Chief and Medical Director, Korein-Wilson Professor of Orthopaedic Surgery<br />
On cover, top left: From Nathalie Burg, MD, Instructor. Lower right: From Shipman et al., “A protective Langerhans cell-keratinocyte axis that is<br />
dysfunctional in photosensitivity.” Science Translational Medicine 15 Aug <strong>2018</strong>: Vol. 10, Issue 454, eaap9527. Reprinted with permission from AAAS.
Perhaps only second to our focus on expert<br />
patient care is our commitment to studying the<br />
mechanisms of lupus, scleroderma, myositis and<br />
other rheumatic diseases: Why do they occur? Why<br />
do they affect some people and not others? Why<br />
are they more common in women than in men?<br />
<strong>HSS</strong> has a long history of supporting physicianscientists.<br />
Over the last five years, we’ve recruited<br />
seven junior faculty members who are pursuing<br />
careers in clinical and translational research. We<br />
also founded the <strong>HSS</strong> <strong>Rheumatology</strong> Council, a<br />
committee of supporters and donors dedicated to<br />
raising the <strong>Rheumatology</strong> Division’s visibility and<br />
enabling research.<br />
Working in partnership with the Development<br />
Department, we initiated a research grant program<br />
and were pleased to award the first <strong>Rheumatology</strong><br />
Council Grants to the following physicians:<br />
• Karmela K. Chan, MD,<br />
Assistant Attending Physician<br />
• Jessica K. Gordon, MD,<br />
Assistant Attending Physician<br />
• Nathalie Burg, MD, Instructor<br />
• David R. Fernandez, MD, PhD,<br />
Assistant Attending Physician<br />
Other grant recipients include Bella Mehta,<br />
MBBS, MD, Assistant Attending Physician,<br />
who received the C. Ronald MacKenzie Young<br />
Scientist Endowment Award. Michela Manni, PhD,<br />
Instructor, received the Lockshin Fellowship Award<br />
from the Barbara Volcker Center for Women and<br />
Rheumatic Disease.<br />
Our five Centers of Excellence and Division of<br />
Pediatric <strong>Rheumatology</strong> facilitate collaboration<br />
among physicians with disease-related academic<br />
interests. Clinical care, research and patient<br />
support are organized through most of the<br />
Centers. Dr. Salmon, Director of the Lupus and<br />
Antiphospholipid Syndrome Center of Excellence,<br />
and colleagues oversee the recruitment of<br />
patients for translational research studies on<br />
lupus and APS and prioritize interventional clinical<br />
trials of candidate therapeutics. The Center also<br />
works closely with <strong>HSS</strong> social workers to lead<br />
support groups and educational programs for<br />
patients. <strong>HSS</strong> has been dedicated to advancing<br />
the understanding of the immunopathogenesis<br />
of systemic lupus erythematosus for many years,<br />
and we continue to identify biomarkers that<br />
predict complications of disease and molecular<br />
targets that hold promise of leading to new<br />
drug therapies.<br />
Dr. Gordon and Robert F. Spiera, MD, Director of<br />
the Scleroderma, Vasculitis & Myositis Center of<br />
Excellence and Attending Physician, have worked<br />
closely with Franck Barrat, PhD, Senior Scientist<br />
at the <strong>HSS</strong> Research Institute, to study the role of<br />
plasmacytoid dendritic cells in systemic sclerosis.<br />
They have identified Toll-like receptor 8 as a novel<br />
pathway for immune system activation in patients<br />
with the disease. Drs. Gordon and Spiera are also<br />
designing investigator-initiated studies of novel<br />
therapeutics and participating in multicenter<br />
sponsored clinical trials.<br />
<strong>HSS</strong> rheumatologists recognize the value of<br />
close collaboration with basic scientists in the<br />
laboratory as well as with orthopaedic surgeons.<br />
With the rich patient resources available at<br />
<strong>HSS</strong>, clinical data and synovial tissue samples<br />
collected at the time of arthroplasty have been<br />
studied to characterize the cell populations<br />
that are associated with flares in rheumatoid<br />
arthritis. Vivian P. Bykerk, MD, Director of the<br />
Inflammatory Arthritis Center of Excellence<br />
and Associate Attending Physician, and Susan<br />
M. Goodman, MD, Director of the Integrative<br />
<strong>Rheumatology</strong> and Orthopedic Center of<br />
Excellence and Attending Physician, have<br />
established protocols that provide the clinical<br />
data necessary for productive analysis of<br />
tissue samples. These researchers and their<br />
collaborators are using machine learning to<br />
analyze gene expression data from synovial<br />
tissue cells in relation to pathologic patterns of<br />
tissue histology in rheumatoid arthritis patients.<br />
In our Bone Health and Osteoporosis Center<br />
of Excellence, Emily M. Stein, MD, Associate<br />
Attending Physician and Associate Scientist, is<br />
working closely with the <strong>HSS</strong> Spine Service to<br />
study bone quality.<br />
Our commitment to young investigators and the<br />
success of their academic careers will ensure<br />
that we sustain our long tradition of leadership in<br />
rheumatology and our history of advancing patient<br />
care. Our application of current technologies<br />
to characterize the molecular mechanisms that<br />
underlie the diseases we treat exemplifies our<br />
unwavering commitment to achieve better lives for<br />
our patients.<br />
Mary K. Crow, MD<br />
Physician-in-Chief<br />
Chair, Department of Medicine<br />
Chief, Division of <strong>Rheumatology</strong><br />
Benjamin M. Rosen Chair in Immunology and<br />
Inflammation Research<br />
Joseph P. Routh Professor of Rheumatic Disease Medicine
2<br />
Division of <strong>Rheumatology</strong><br />
<strong>2017</strong>–<strong>2018</strong> Achievements<br />
#3 in the nation<br />
for <strong>Rheumatology</strong> by U.S. News & World <strong>Report</strong> “Best Hospitals”<br />
(<strong>2018</strong>–2019 rankings)<br />
The Division of <strong>Rheumatology</strong>, the Department of Social<br />
Work Programs and the Digital Communications team created<br />
LupusMinder, a smartphone app that helps lupus patients manage<br />
their condition. In <strong>2018</strong>, the app received a Platinum award in<br />
the category of Best Native Mobile App from the eHealthcare<br />
Leadership Awards.<br />
Mary K. Crow, MD, Physician-in-Chief and Chief, Division<br />
of <strong>Rheumatology</strong>, received the Presidential Gold Medal<br />
from the American College of <strong>Rheumatology</strong> (ACR)<br />
in <strong>2018</strong>. It is awarded in recognition of outstanding<br />
achievements in rheumatology over the course of a career.<br />
Dr. Crow is Co-Chair of the Scientific Advisory Board<br />
of the Lupus Research Alliance and a member of the<br />
Executive Committee of the Lupus Clinical Investigators<br />
Network (LuCIN).<br />
Franck Barrat, PhD, Senior Scientist; Robert F. Spiera,<br />
MD, Director of the Scleroderma, Vasculitis & Myositis<br />
Center of Excellence and Attending Physician; Jessica<br />
K. Gordon, MD, Assistant Attending Physician; David<br />
R. Fernandez, MD, Assistant Attending Physician; and<br />
other <strong>HSS</strong> investigators published a significant study<br />
in Science Translational Medicine in <strong>2018</strong> identifying<br />
the plasmacytoid dendritic cell and Toll-like receptor<br />
8 as important contributors to the pathogenesis of<br />
systemic sclerosis.<br />
Anne R. Bass, MD, Attending Physician, served as Chair<br />
of the ACR Committee on <strong>Rheumatology</strong> Training and<br />
Workforce Issues.<br />
Vivian P. Bykerk, MD, Director of the Inflammatory<br />
Arthritis Center of Excellence and Associate Attending<br />
Physician, is the lead investigator of a rheumatoid arthritis<br />
(RA) study funded by the National Institutes of Health<br />
(NIH) and partnering pharmaceutical companies as part<br />
of the Accelerating Medicines Partnership (AMP). The<br />
study is focused on identifying molecular processes in<br />
synovial tissue that reflect disease flare.<br />
Doruk Erkan, MD, MPH, Associate Attending Physician and<br />
Clinical Co-Director of the Mary Kirkland Center for Lupus<br />
Care, is Executive Committee Chair of the international APS<br />
research network APS ACTION (Antiphospholipid Syndrome<br />
Alliance for Clinical Trials and International Networking).<br />
Susan M. Goodman, MD, Director of the Integrative<br />
<strong>Rheumatology</strong> and Orthopedic Center of Excellence and<br />
Attending Physician, led the expert panel that created the<br />
first-ever Guideline for the Perioperative Management<br />
of Antirheumatic Medication in Patients With Rheumatic<br />
Diseases Undergoing Elective Total Hip or Total Knee<br />
Arthroplasty. The Guideline is sponsored by the American<br />
College of <strong>Rheumatology</strong> and the American Association of<br />
Hip and Knee Surgeons.<br />
Kyriakos A. Kirou, MD, DSc, Assistant Attending<br />
Physician, is the <strong>HSS</strong> Site Director of LuCIN.<br />
Michael D. Lockshin, MD, Director of the Barbara<br />
Volcker Center for Women and Rheumatic Disease and<br />
Attending Physician, is author of The Prince at the Ruined<br />
Tower: Time, Uncertainty & Chronic Illness, which was<br />
published in <strong>2017</strong>.<br />
Dr. Lockshin and Dr. Erkan are editors of<br />
Antiphospholipid Syndrome: Current Research Highlights<br />
and Clinical Insights, which was published in <strong>2017</strong>.<br />
Theresa T. Lu, MD, PhD, Associate Scientist, was<br />
awarded a research grant from the Lupus Research<br />
Alliance to study the involvement of the lymphatic<br />
system in ultraviolet light-induced cutaneous lupus.<br />
Catherine H. MacLean, MD, PhD, Chief Value<br />
Medical Officer and Director of the <strong>HSS</strong> Center for the<br />
Advancement of Value in Musculoskeletal Care, was<br />
named in the inaugural “Notable Women in Health Care<br />
in NYC” list in Crain’s New York Business. In addition,<br />
she serves on and is the immediate past chair of the<br />
performance measures committee for the American<br />
College of Physicians.<br />
Bella Mehta, MBBS, MD, Assistant Attending Physician,<br />
received the ACR Distinguished Fellow Award in <strong>2018</strong>.
Hospital for Special Surgery 3<br />
Karen B. Onel, MD, Chief of the Division of Pediatric<br />
<strong>Rheumatology</strong> and Attending Physician, is Chair of the<br />
Childhood Arthritis and <strong>Rheumatology</strong> Research Alliance<br />
(CARRA) Ethics Committee. She is Co-Chair of the CARRA<br />
Systemic Juvenile Idiopathic Arthritis working group.<br />
Jillian Rose, LCSW, MPH, Director of Community<br />
Engagement, Diversity and Research, received the<br />
Distinguished Educator Award from the Association of<br />
<strong>Rheumatology</strong> Health Professionals in <strong>2018</strong>.<br />
Linda A. Russell, MD, Director of the Bone Health<br />
and Osteoporosis Center of Excellence and Associate<br />
Attending Physician, was appointed by the American<br />
College of <strong>Rheumatology</strong> as a member of its Committee<br />
on Rheumatologic Care.<br />
Jane E. Salmon, MD, Director of the Lupus and<br />
Antiphospholipid Syndrome Center of Excellence and<br />
Attending Physician, and Dr. Crow were named Honorary<br />
Members of the European League Against Rheumatism<br />
(EULAR) in <strong>2018</strong> and <strong>2017</strong>, respectively. They are among<br />
the first four Americans to achieve this honor, which<br />
recognizes their contributions to research, education and<br />
service to EULAR.<br />
Dr. Salmon is a member of the Steering Committee of<br />
LuCIN and the Scientific Advisory Board of the Lupus<br />
Research Alliance. She was named a Master of the<br />
American College of <strong>Rheumatology</strong> in <strong>2017</strong>.<br />
Lisa R. Sammaritano, MD, Associate Attending<br />
Physician, was Principal Investigator of the American<br />
College of <strong>Rheumatology</strong> Reproductive Health in<br />
Rheumatic Diseases Guideline.<br />
Robert F. Spiera, MD, Director of the Scleroderma,<br />
Vasculitis & Myositis Center of Excellence and Attending<br />
Physician, was a member of a group of investigators that<br />
designed and executed a clinical trial for a new therapy<br />
for giant-cell arteritis. Tocilizumab, an interleukin (IL)-6<br />
blocking agent, was the first therapy approved by the<br />
U.S. Food & Drug Administration and European Medicines<br />
Agency for this indication.<br />
Dr. Spiera is Chair of the Medical and Scientific Advisory<br />
Board of the Scleroderma Foundation, Tri-State Chapter.<br />
He and Jessica K. Gordon, MD, Assistant Attending<br />
Physician, are members of this Board.<br />
Dr. Spiera and Dr. Gordon are members of the National<br />
Medical and Scientific Advisory Board of the Scleroderma<br />
Foundation.<br />
Sarah F. Taber, MD, Assistant Attending Physician,<br />
is a co-author of the chapter on Systemic Lupus<br />
Erythematosus in Childhood and Adolescence in the<br />
<strong>2018</strong> edition of Dubois’ Lupus Erythematosus and<br />
Related Syndromes.<br />
Fast Facts<br />
Division of <strong>Rheumatology</strong><br />
The Division of <strong>Rheumatology</strong> comprises five Centers of Excellence and the Division of Pediatric <strong>Rheumatology</strong>.<br />
The Centers bring together <strong>HSS</strong> faculty and staff members with an interest in a particular disease area to<br />
develop projects and new research initiatives. They include physicians and healthcare professionals from other<br />
departments, such as Orthopaedics, Social Work, Nursing and Research.<br />
• Bone Health and Osteoporosis Center of Excellence<br />
• Inflammatory Arthritis Center of Excellence<br />
• Integrative <strong>Rheumatology</strong> and Orthopedic Center of Excellence<br />
• Lupus and Antiphospholipid Syndrome Center of Excellence<br />
• Scleroderma, Vasculitis & Myositis Center of Excellence<br />
• Division of Pediatric <strong>Rheumatology</strong><br />
Adult rheumatologists<br />
36 36,027<br />
Pediatric rheumatologists<br />
5 2,969<br />
Scientists<br />
9 2,728<br />
Perioperative<br />
17 medicine physicians 15,665<br />
9<br />
<strong>Rheumatology</strong><br />
support and<br />
education programs for patients<br />
Adult rheumatology<br />
patient visits<br />
Pediatric rheumatology<br />
patient visits<br />
Endocrinology<br />
patient visits<br />
Perioperative<br />
patient visits<br />
All figures pertain to the <strong>2017</strong>–<strong>2018</strong> academic year.
4<br />
Division of <strong>Rheumatology</strong><br />
Identifying high-risk pregnancies<br />
in patients with lupus<br />
Most women with lupus can<br />
have successful pregnancies,<br />
but some develop complications,<br />
such as preeclampsia, fetal<br />
and neonatal death, and<br />
fetal growth restriction. We<br />
cannot predict in whom these<br />
adverse outcomes will occur.<br />
In experimental laboratory<br />
models, complement activation<br />
causes adverse pregnancy<br />
outcomes. To investigate the<br />
role of complement in patients,<br />
Jane E. Salmon, MD, Collette<br />
Kean Research Chair, Attending<br />
Physician and Director of the<br />
Lupus and Antiphospholipid<br />
Syndrome Center of Excellence;<br />
Michael D. Lockshin, MD, Director<br />
of the Barbara Volcker Center<br />
for Women and Rheumatic<br />
Disease and Attending Physician;<br />
and Lisa R. Sammaritano, MD,<br />
Associate Attending Physician,<br />
and colleagues mined the data<br />
and samples from PROMISSE<br />
(Predictors of Pregnancy<br />
Outcome: Biomarkers in<br />
Antiphospholipid Antibody<br />
Syndrome and Systemic Lupus<br />
Erythematosus). The results of<br />
their study, which was published<br />
in the Annals of the Rheumatic<br />
Diseases in April <strong>2018</strong>, included<br />
the evaluation of 487 pregnant<br />
women with SLE and/or aPL<br />
antibodies and 204 pregnant<br />
healthy controls. At each<br />
month of pregnancy, samples<br />
were obtained to measure<br />
complement activation products<br />
in patients’ blood. Adverse<br />
pregnancy outcomes occurred<br />
in approximately 20 percent of<br />
SLE and/or aPL pregnancies<br />
and were associated with<br />
lupus anticoagulant, history of<br />
hypertension, and non-white<br />
race. Levels of complement<br />
products early in pregnancy<br />
were significantly higher in<br />
A recent finding by Jane E. Salmon, MD, Director of the Lupus and<br />
Antiphospholipid Syndrome Center of Excellence and Attending Physician<br />
(left), may help pregnant women with lupus have healthy babies, such as<br />
the patient shown at right. Marta M. Guerra, MS, Project Coordinator for<br />
Dr. Salmon’s study (center), admires the baby.<br />
patients who experienced<br />
pregnancy complications.<br />
These findings suggest that,<br />
as in the experimental models,<br />
complement activation<br />
contributes to abnormal placental<br />
development, which leads to<br />
pregnancy complications.<br />
TNF-α is released by<br />
inflammatory cells as a<br />
consequence of complement<br />
activation, and it too contributes<br />
to placental dysfunction,<br />
preeclampsia and fetal growth<br />
restriction in experimental<br />
models. To translate these<br />
findings to patients, Dr. Salmon<br />
and her team are conducting<br />
a trial in which they will treat<br />
pregnant women with APS and<br />
SLE at high risk for serious<br />
pregnancy complications with<br />
certolizumab, a TNF inhibitor used<br />
Dr. Salmon’s<br />
research suggests<br />
that complement<br />
activation contributes<br />
to abnormal placental<br />
development, which<br />
leads to pregnancy<br />
complications.<br />
to treat rheumatoid arthritis and<br />
psoriatic arthritis that does not<br />
cross the placenta. “If the trial<br />
prevents pregnancy complications<br />
in patients with SLE and APS, it<br />
may also prevent preeclampsia<br />
in women without autoimmune<br />
disease who are at risk for<br />
placental insufficiency,” says<br />
Dr. Salmon. “We hope our studies<br />
of SLE and APS have implications<br />
for the general population.”
Hospital for Special Surgery 5<br />
Improving outcomes for<br />
RA patients undergoing<br />
joint replacement<br />
Although rheumatoid arthritis<br />
(RA) patients have experienced<br />
improvements in healthrelated<br />
quality of life and<br />
functional status, rates of total<br />
hip replacement and total<br />
knee replacement procedures<br />
have remained stable. Most<br />
RA patients who undergo<br />
arthroplasty are taking diseasemodifying<br />
antirheumatic drugs<br />
and biologic therapies, which<br />
are known to increase their risk<br />
of developing a prosthetic joint<br />
infection. As a result, patients<br />
are typically instructed to stop<br />
taking their medications prior<br />
to surgery. This may increase<br />
their risk of having a flare<br />
perioperatively, which may have<br />
a negative effect on rehabilitation<br />
efforts and outcomes.<br />
To investigate patient-reported<br />
RA flares, <strong>HSS</strong> researchers<br />
launched the RA Perioperative<br />
Flare Study. This is likely the<br />
first study to prospectively<br />
assess postoperative, patientreported<br />
flares of RA in patients<br />
undergoing THA and TKA using<br />
the RA-FQ, a validated, patientreported<br />
outcome instrument for<br />
identifying RA flares.<br />
In the study, which was published<br />
in The Journal of <strong>Rheumatology</strong><br />
in May <strong>2018</strong>, 120 <strong>HSS</strong> patients<br />
answered a questionnaire each<br />
week for six consecutive weeks<br />
after surgery. Patients who<br />
reported flares after surgery were<br />
compared to those who did not<br />
experience them. Lead author<br />
Susan M. Goodman, MD, Director<br />
of the Integrative <strong>Rheumatology</strong><br />
and Orthopedic Center of<br />
Excellence and Attending<br />
From left to right: Mark P. Figgie, MD, Chief of the Surgical Arthritis Service,<br />
Allan E. Inglis MD Chair in Surgical Arthritis, and Attending Orthopaedic<br />
Surgeon, and Susan M. Goodman, MD, Director of the Integrative<br />
<strong>Rheumatology</strong> and Orthopedic Center of Excellence and Attending<br />
Physician, are investigating flares in RA patients after arthroplasty.<br />
Physician, and colleagues found<br />
that 63 percent of the patients<br />
experienced a flare by six weeks<br />
after surgery. The patients who<br />
flared had significantly higher<br />
disease activity at baseline, but<br />
preoperative antirheumatic<br />
medication withdrawal was not an<br />
independent risk factor for flares.<br />
To improve outcomes and<br />
reduce the risk of infection in<br />
RA patients, <strong>HSS</strong> researchers<br />
are investigating the effects<br />
of changing the perioperative<br />
medication protocol. “We can<br />
withhold biologic medications<br />
for one-dose intervals around<br />
the time of surgery,” says<br />
Dr. Goodman. “Now we’re looking<br />
at pain and functionality in these<br />
patients after a year.”<br />
Rheumatoid arthritis<br />
patients who<br />
experienced flares<br />
after arthroplasty<br />
had significantly<br />
higher disease<br />
activity at baseline.
6<br />
Division of <strong>Rheumatology</strong><br />
Creating a better future for<br />
scleroderma patients<br />
Scleroderma is one of the<br />
most debilitating rheumatic<br />
diseases. It is associated with<br />
significant morbidity and<br />
disability and has the highest<br />
rate of all-cause mortality<br />
among the rheumatic diseases.<br />
To date, no medication has<br />
been specifically approved for<br />
this condition. Fortunately,<br />
<strong>HSS</strong> physicians and scientists<br />
have made significant progress<br />
in investigating promising<br />
new treatment options. One<br />
area of focus is lenabasum,<br />
a cannabinoid receptor<br />
type 2 (CB2) agonist. In<br />
<strong>2017</strong>, Robert F. Spiera, MD,<br />
Director of the Scleroderma,<br />
Vasculitis & Myositis Center<br />
of Excellence and Attending<br />
Physician, led a Phase II<br />
study of the drug sponsored<br />
by Corbus Pharmaceuticals.<br />
It demonstrated acceptable<br />
safety and tolerability and<br />
suggested a possible benefit<br />
in scleroderma patients. He<br />
presented the results at the<br />
<strong>2017</strong> American College of<br />
<strong>Rheumatology</strong> <strong>Annual</strong> Meeting.<br />
CB2 receptors are expressed on<br />
immune system cells, including<br />
T cells, macrophages and B<br />
cells. They appear to modulate<br />
immune function. “Triggering<br />
these cells turns off the<br />
propagation of the inflammation<br />
phase of the innate immune<br />
response and promotes<br />
expression of resolvins, which<br />
contribute to resolving the<br />
inflammatory response, thereby<br />
ultimately diminishing tissue<br />
fibrosis,” says Dr. Spiera.<br />
In a one-year, open label<br />
extension study that followed<br />
the Phase II trial, patients<br />
taking lenabasum continued to<br />
see significant improvements<br />
in inflammation and fibrosis.<br />
From left to right: Jessica K. Gordon, MD, Assistant Attending Physician,<br />
and Robert F. Spiera, MD, Director of the Scleroderma, Vasculitis & Myositis<br />
Center of Excellence and Attending Physician, are studying two drugs that<br />
may be effective in scleroderma patients.<br />
Dr. Spiera presented these<br />
results at the European League<br />
Against Rheumatism Congress<br />
in Amsterdam in June <strong>2018</strong>. Now<br />
<strong>HSS</strong> is the lead site for a yearlong<br />
Phase III trial of lenabasum,<br />
which is currently enrolling<br />
patients around the world.<br />
Positive results could help to<br />
advance the drug on the path to<br />
FDA approval. “What’s appealing<br />
about this drug is it appears to<br />
be very safe,” says Dr. Spiera.<br />
Unlike medications that<br />
suppress the immune system,<br />
lenabasum doesn’t appear to<br />
increase the risk of infection.<br />
Dr. Spiera is also optimistic<br />
about belimumab. In an <strong>HSS</strong>sponsored,<br />
investigator-initiated<br />
trial of the drug, patients with<br />
early diffuse scleroderma who<br />
received the medication saw<br />
significant improvements in skin<br />
thickness scores. The findings<br />
were published in Arthritis and<br />
<strong>Rheumatology</strong> in January <strong>2018</strong>.<br />
The researchers also<br />
determined that the drug<br />
affects patients’ gene<br />
expression in skin biopsies.<br />
“Significant decreases in the<br />
expression of B-cell signaling<br />
and pro-fibrotic gene pathways<br />
were observed in patients who<br />
improved on the drug and not<br />
in those who didn’t improve,”<br />
says Dr. Spiera. This supports<br />
the idea that the drug was<br />
having an effect on the relevant<br />
cellular mechanisms. Dr. Spiera<br />
and his colleague, Jessica<br />
K. Gordon, MD, Assistant<br />
Attending Physician, plan to<br />
initiate a larger study of this<br />
strategy, which will begin in<br />
early 2019.<br />
Although there’s a long road<br />
ahead for getting a new drug<br />
to market, the prospects are<br />
promising. “It will be very<br />
exciting if either drug pans<br />
out,” says Dr. Spiera. “This is a<br />
totally unmet need.”
Hospital for Special Surgery 7<br />
Advancing high-value care<br />
and outcomes for patients<br />
Catherine H. MacLean, MD, PhD, Chief Value Medical Officer, is studying<br />
patient-reported outcome measures, or PROMs.<br />
Our commitment to providing<br />
value-based care is reflected in<br />
our high-quality services and<br />
low complication rates. “<strong>HSS</strong><br />
leads the country in performance<br />
on a number of different safety<br />
measures,” says Catherine H.<br />
MacLean, MD, PhD, Chief Value<br />
Medical Officer. “As a result,<br />
our total cost for an episode of<br />
care is lower than that of other<br />
hospitals.” While safety is of<br />
paramount importance, patients<br />
come to <strong>HSS</strong> to get better. So we<br />
are focused on studying patientreported<br />
outcome measures,<br />
or PROMs. “We’re measuring<br />
PROMs as a standard of care<br />
because we want to understand<br />
how our patients are doing in<br />
terms of improving their pain<br />
and functional status,” says<br />
Dr. MacLean.<br />
<strong>HSS</strong> physicians also aim to be<br />
responsible when prescribing<br />
medications. “Rheumatologists<br />
are the stewards of a number of<br />
very expensive drugs, including<br />
adalimumab, infliximab,<br />
etanercept and rituximab—four<br />
of the five drugs with the highest<br />
dollar sales worldwide,” says<br />
Dr. MacLean. “These medications<br />
are often effective for rheumatoid<br />
arthritis (RA) patients, but there<br />
are less expensive alternatives<br />
that may be appropriate for<br />
certain patients. By routinely<br />
assessing disease activity and<br />
patient outcomes, we can be<br />
more thoughtful about the drugs<br />
we prescribe.” At the same time,<br />
physicians need to have open,<br />
honest conversations with their<br />
patients about the costs of<br />
medical care—in particular, these<br />
very expensive medications,<br />
which cost thousands of dollars<br />
per month. Given the choice<br />
between two similarly effective<br />
drugs, patients might prefer the<br />
less expensive option, especially<br />
if they have a high co-pay or<br />
no insurance.<br />
The highest value care for<br />
rheumatoid arthritis is that which<br />
prevents long-term disease or<br />
joint damage. Hence, our first<br />
objective is to treat early and<br />
aggressively with the best drug<br />
for the individual patient, be that<br />
a conventional drug or a more<br />
expensive biologic one. This has<br />
resulted in a marked reduction in<br />
the development of joint damage,<br />
deformity and disability. “When<br />
I was a fellow, there were always<br />
wheelchairs in the rheumatology<br />
waiting room,” says Dr. MacLean.<br />
“They are a pretty rare sight<br />
these days.”<br />
How a rheumatologist became Chief Value Medical Officer<br />
Catherine H. MacLean, MD, PhD, is a<br />
rheumatologist as well as Chief Value<br />
Medical Officer. She currently directs the<br />
<strong>HSS</strong> Center for the Advancement of Value<br />
in Musculoskeletal Care. In this role, Dr.<br />
MacLean develops programs, systems<br />
and tools to deliver high-value care at<br />
<strong>HSS</strong> and beyond. She has had a full and<br />
varied career, with stints in academic<br />
medicine, research and the insurance<br />
industry. After attending Washington<br />
University School of Medicine in St.<br />
Louis, Dr. MacLean completed training<br />
in internal medicine at Harbor-UCLA<br />
Medical Center and rheumatology at<br />
UCLA Center for the Health Sciences. As<br />
part of UCLA’s first Scientific Training and<br />
Advanced Research fellowship class, she<br />
also earned a PhD in health services from<br />
UCLA’s School of Public Health. Upon<br />
completing her training, she joined the<br />
faculty at UCLA with joint appointments<br />
at the RAND Corporation and the West<br />
Los Angeles VAMC, where her research<br />
focused on defining, measuring and<br />
improving healthcare quality. She was<br />
recruited by Anthem/WellPoint to help<br />
drive quality improvement and eventually<br />
led quality and care management<br />
programs there. In 2015, she joined <strong>HSS</strong>.<br />
Dr. MacLean was the principal<br />
investigator on many academic research<br />
projects at UCLA and RAND, and has<br />
been a director, chair or participant on<br />
numerous national committees and<br />
panels related to healthcare quality and<br />
value. She is the immediate past chair of<br />
the performance measures committee at<br />
the American College of Physicians (ACP)<br />
and currently serves on the ACP’s Quality<br />
Improvement Learning Collaborative<br />
Task Force and the National Committee<br />
for Quality Assurance’s Bone and Joint<br />
Measurement Advisory Panel.
8<br />
Division of <strong>Rheumatology</strong><br />
Targeting interferon for<br />
better control of lupus<br />
<strong>HSS</strong> has been a leader in the<br />
quest to better understand<br />
systemic lupus erythematosus<br />
(SLE), thanks in large part to<br />
research directed by Mary K.<br />
Crow, MD, Physician-in-Chief<br />
and Chief of the Division of<br />
<strong>Rheumatology</strong>. About 17 years<br />
ago, she and two other groups<br />
observed that type I interferon<br />
was responsible for the genes<br />
expressed in blood from lupus<br />
patients. This suggested that<br />
a virus or virus-like stimulus<br />
might play a role in the wide<br />
range of immune alterations and<br />
autoimmunity associated with<br />
SLE. This finding became known<br />
as the “interferon signature” and<br />
continues to be an important<br />
way of characterizing lupus<br />
patients for research.<br />
Over the last decade, Dr. Crow<br />
and her team identified an<br />
association between a positive<br />
interferon signature and<br />
active and severe disease.<br />
They also found that the<br />
interferon signature was<br />
associated with the presence<br />
of autoantibodies that target<br />
RNA or RNA-binding proteins.<br />
That observation indicated that<br />
immune complexes containing<br />
RNA, as well as RNA within<br />
cells, might be triggers for the<br />
production of type I interferon.<br />
This was confirmed in other<br />
studies. “Our lab has been<br />
particularly interested in the<br />
potential role of RNA encoded by<br />
endogenous virus-like elements<br />
in our own genomes—LINE-1<br />
retrotransposons—as drivers<br />
of type I interferon in SLE,”<br />
says Dr. Crow. “We showed<br />
that cells from patients with<br />
SLE or Sjogren’s syndrome<br />
express elevated RNAs encoding<br />
LINE‐1 and that LINE-1 RNA can<br />
induce the production of type I<br />
interferon. Overall, we think that<br />
type I interferon is responsible<br />
for many of the immune system<br />
alterations in SLE patients.”<br />
Currently, Dr. Crow is studying<br />
agents aimed at reducing the<br />
interferon signature—and the<br />
production or action of type I<br />
interferon. “We are continuing<br />
to investigate the role of<br />
endogenous retroelements<br />
as drivers of type I interferon<br />
production, but we have<br />
Left: SLE is characterized by<br />
sustained activation of the type I<br />
interferon pathway, in contrast to<br />
the brief expression of interferon<br />
after a viral infection.<br />
Above, top: Mary K. Crow, MD, Physician-in-Chief and Chief of the Division<br />
of <strong>Rheumatology</strong> (center), and her research team discuss their findings on<br />
the role of type I interferon in systemic lupus erythematosus.<br />
expanded the scope of our<br />
research to include additional<br />
molecular pathways involved<br />
in SLE,” says Dr. Crow. “We<br />
are currently analyzing gene<br />
expression data that we think<br />
will provide new insights into<br />
mechanisms responsible for<br />
lupus nephritis, an important<br />
organ system manifestation<br />
of SLE and a reason for poor<br />
patient outcomes.”
Hospital for Special Surgery 9<br />
Defining a new form of<br />
arthritis in cancer patients<br />
“Studying a new form<br />
of arthritis linked to<br />
immunotherapy drugs<br />
may help us to figure<br />
out the immunologic<br />
pathways that lead<br />
to arthritis. That may<br />
allow us to target those<br />
pathways early on and<br />
potentially prevent RA in<br />
the general population.”<br />
Anne R. Bass, MD,<br />
Attending Physician<br />
Anne R. Bass, MD, Attending Physician, examines a patient who is taking<br />
immunotherapy medications.<br />
Immunotherapy drugs known<br />
as “checkpoint inhibitors” can<br />
have dramatic, often lifesaving<br />
benefits for cancer patients.<br />
But they are also known to<br />
have problematic side effects.<br />
“Patients are staying on these<br />
drugs for longer periods of<br />
time, and we’re starting to see<br />
arthritis as a side effect more<br />
commonly,” says Anne R. Bass,<br />
MD, Attending Physician. “My<br />
theory is that some patients<br />
are genetically predisposed to<br />
arthritis and develop it when<br />
they take these immunestimulating<br />
therapies.”<br />
Collaborating with oncologists<br />
at a major New York City<br />
cancer center, Dr. Bass has<br />
been working to clinically<br />
define this new form of<br />
inflammatory arthritis,<br />
which causes joint swelling<br />
and pain and occasionally is<br />
associated with rheumatoid<br />
arthritis (RA) markers in<br />
the blood. In some patients,<br />
symptoms resemble RA, and<br />
in others, they are similar<br />
to polymyalgia rheumatica.<br />
Dr. Bass is investigating<br />
why and how the condition<br />
develops on an immunological<br />
level and is establishing<br />
treatment protocols. One key<br />
question: Is the “RA-like” form<br />
of inflammatory arthritis the<br />
same as the RA that develops<br />
in people who haven’t taken<br />
immunotherapy drugs? “If it<br />
is, then these patients offer<br />
an opportunity to study RA<br />
developing over a compressed<br />
period of time,” says Dr. Bass.<br />
This shortened timeline “may<br />
enable us to identify predictors<br />
for RA and figure out the<br />
immunologic pathways that<br />
lead to arthritis. That may allow<br />
us to target those pathways<br />
early on and potentially prevent<br />
RA in the general population.”<br />
While we aim to treat the<br />
arthritis that develops in<br />
cancer patients who are taking<br />
immunotherapy medications, we<br />
don’t want to interfere with the<br />
curative effects of the drugs by<br />
suppressing the immune system<br />
too much. Says Dr. Bass: “This<br />
is an important opportunity<br />
for clinical and research<br />
collaboration with our oncology<br />
colleagues, especially now that<br />
immunotherapy is being used<br />
for an ever-expanding array<br />
of cancers.”
10<br />
Division of <strong>Rheumatology</strong><br />
Susan M. Goodman, MD, Director of the Integrative <strong>Rheumatology</strong> and Orthopedic Center of Excellence and<br />
Attending Physician, and <strong>HSS</strong> colleagues are studying the effects of the drug secukinumab on the skeleton.<br />
Improving bone health in patients<br />
with ankylosing spondylitis<br />
While people with ankylosing<br />
spondylitis (AS) tend to<br />
experience overactive bone<br />
growth and develop abnormal<br />
bone spurs, they are also prone<br />
to osteoporosis. Studies have<br />
estimated that the prevalence<br />
of osteoporosis is as high as<br />
25 percent for these patients—<br />
more than double the 10 percent<br />
prevalence in the general<br />
population. Although these<br />
patients produce more cortical<br />
bone, the trabecular bone is<br />
abnormally weak. As a result,<br />
they are at risk of spinal fractures,<br />
which can lead to changes in<br />
posture and pain.<br />
Bisphosphonates, calcium and<br />
vitamin D can be prescribed<br />
to prevent fractures, but AS<br />
patients don’t respond well<br />
to these therapies. In <strong>2018</strong>,<br />
<strong>HSS</strong> physicians launched a<br />
pilot study to investigate the<br />
effects of secukinumab—a<br />
monoclonal antibody used to<br />
treat autoimmune diseases—<br />
on the skeleton. The drug is<br />
currently approved for treatment<br />
of AS, moderate to severe plaque<br />
psoriasis and psoriatic arthritis.<br />
It targets interleukin-17A and<br />
may protect against bone loss<br />
by suppressing the function of<br />
osteoclasts and promoting the<br />
activity of osteoblasts.<br />
In the study, which will last two<br />
years, patients with the condition<br />
will undergo assessments, such<br />
as X-ray imaging of the skeleton to<br />
measure bone density and scoring<br />
of the spine for the presence<br />
of spurs or erosions. “What<br />
makes the disease so disabling<br />
is new bone formation that fuses<br />
the vertebrae,” says Susan M.<br />
Goodman, MD, Director of the<br />
Integrative <strong>Rheumatology</strong> and<br />
Orthopedic Center of Excellence<br />
and Attending Physician, who is<br />
leading the study. “Preliminary<br />
data supporting the use of the<br />
drug suggest that you don’t get<br />
“Preliminary data<br />
supporting the use<br />
of secukinumab, a<br />
monoclonal antibody<br />
used to treat<br />
autoimmune diseases,<br />
suggest that AS<br />
patients don’t get<br />
the bony proliferation<br />
as rapidly.”<br />
Susan M. Goodman, MD, Director<br />
of the Integrative <strong>Rheumatology</strong><br />
and Orthopedic Center of<br />
Excellence and Attending Physician<br />
the bony proliferation as rapidly.”<br />
Study participants will also<br />
be tested for markers of bone<br />
growth and resorption, as well as<br />
inflammation levels. If the results<br />
are positive, Dr. Goodman’s team<br />
will study the drug’s effects in a<br />
larger patient population.
Hospital for Special Surgery 11<br />
New possibilities for<br />
scleroderma treatment<br />
Scleroderma, one of the most<br />
life-threatening rheumatic<br />
diseases, is among the most<br />
challenging to understand and<br />
treat. But breakthrough research<br />
from the lab of Franck Barrat,<br />
PhD, Michael R. Bloomberg Chair<br />
and Senior Scientist, could lead<br />
to new therapeutic possibilities.<br />
Dr. Barrat’s research focuses<br />
on plasmacytoid dendritic<br />
cells (pDCs), which normally<br />
produce interferon to combat<br />
infection. In a study published in<br />
Science Translational Medicine<br />
in January <strong>2018</strong>, Dr. Barrat<br />
and <strong>HSS</strong> and international<br />
colleagues revealed that pDCs<br />
are chronically activated in<br />
scleroderma patients. They<br />
infiltrate the skin, where<br />
they trigger fibrosis and<br />
inflammation. “In the field<br />
of scleroderma, people have<br />
focused on how to stop<br />
fibrosis,” says Dr. Barrat.<br />
“But the correlation between<br />
inflammation and the main<br />
players that drive inflammation<br />
in fibrosis hasn’t been explored<br />
as much. This is pointing us in a<br />
direction that people had not<br />
looked at before.” As a result,<br />
the finding has generated<br />
considerable excitement from<br />
scientists and industry. “Some<br />
companies are looking really<br />
hard at this now,” says Dr. Barrat.<br />
Top: In our model, the secretion of CXCL4, a marker of systemic sclerosis<br />
(SSc), by patients’ plasmacytoid dendritic cells (pDCs) is due to the<br />
aberrant presence of TLR8 on these cells. CXCL4 potentiates the IFN<br />
production by pDCs, which promotes the autoimmune response and<br />
potentially fibrosis in patients. Depleting pDCs prevented disease in a<br />
preclinical model of scleroderma, suggesting that pDC is an essential<br />
cell type involved in the pathogenesis of SSc.<br />
Bottom, from left to right: Jessica K. Gordon, MD, Assistant Attending<br />
Physician, and Franck Barrat, PhD, Senior Scientist, as well as other<br />
<strong>HSS</strong> researchers, discovered that plasmacytoid dendritic cells (pDCs)<br />
are chronically activated in scleroderma patients, opening the door to<br />
investigations of new treatments.<br />
In a disease model, Dr. Barrat and<br />
colleagues showed that depleting<br />
pDCs prevented fibrosis. The<br />
research has helped to delineate<br />
important mechanisms of the<br />
aberrant cell activity. It has<br />
implicated a receptor on the<br />
surface of pDCs, called TLR8,<br />
as a culprit behind the cell<br />
activity. As a result, there may<br />
be several potential therapeutic<br />
targets and some existing drugs<br />
as possible candidates for<br />
study in scleroderma patients.<br />
“We have identified pDCs as<br />
potentially very important in the<br />
establishment and development<br />
of fibrosis,” says Dr. Barrat.<br />
“Now we can investigate new<br />
therapeutic options for targeting<br />
the cells, the ways they become<br />
activated, and some of the<br />
product they make.”<br />
These findings have led to new<br />
research funding, including<br />
nearly $1.8 million in grants from<br />
the National Institutes of Health<br />
and the Scleroderma Research<br />
Foundation. “What excites me<br />
is all of the possibilities that<br />
this research has opened up,”<br />
says Dr. Barrat. “We’ve put<br />
scleroderma on the map.”
12<br />
Division of <strong>Rheumatology</strong><br />
Using precision medicine<br />
to refine RA treatment<br />
The promise of precision<br />
medicine is to personalize<br />
therapy for patients with<br />
notoriously difficult-to-treat<br />
diseases such as rheumatoid<br />
arthritis (RA). To that end, <strong>HSS</strong><br />
scientists and physicians are<br />
investigating differences in RA<br />
patients’ responses to drugs as<br />
part of the five-year Accelerating<br />
Medicines Partnership (AMP)<br />
study, funded by the National<br />
Institutes of Health and<br />
partnering pharmaceutical<br />
companies. Our researchers<br />
are also investigating molecular<br />
pathways involved in flares.<br />
“We’re trying to discover new<br />
pathways, which could lead<br />
to new therapeutic targets,”<br />
says Lionel B. Ivashkiv, MD,<br />
Richard L. Menschel Chair and<br />
Chief Scientific Officer, David<br />
H. Koch Chair for Arthritis and<br />
Tissue Degeneration Research,<br />
and Director of the David Z.<br />
Rosensweig Genomics Research<br />
Center. “The ultimate goal is<br />
to use this information to help<br />
us choose the best drug for<br />
each patient at the beginning<br />
of treatment.”<br />
“Using advanced genomic<br />
technologies involving single<br />
cells, we are studying synovial<br />
tissue samples to find out how<br />
they relate to disease activity<br />
in the patient,” says Vivian P.<br />
Bykerk, MD, lead investigator<br />
of the RA study, Director of the<br />
Inflammatory Arthritis Center<br />
of Excellence and Associate<br />
Attending Physician. In the first<br />
phase of the study, which is<br />
now complete, our researchers<br />
were able to identify eight new<br />
cell types in RA joints using<br />
next-generation sequencing<br />
techniques. “These are<br />
subsets we’d want to target<br />
with new drugs,” says Laura<br />
Donlin, PhD, Co-Director of the<br />
Derfner Foundation Precision<br />
Medicine Laboratory and<br />
Assistant Scientist.<br />
In the second phase of the<br />
study, which is currently<br />
underway, our researchers are<br />
following a large cohort of RA<br />
patients who will have tissue<br />
samples taken before and after<br />
a new treatment is provided.<br />
Researchers will monitor them<br />
and look for commonalities<br />
that could serve as biomarkers<br />
for treatment response. “<strong>HSS</strong><br />
is a critical player in the AMP<br />
consortium because we provide<br />
unique scientific expertise<br />
and patient resources,” says<br />
Dr. Ivashkiv. “This study has<br />
changed the way we perform<br />
translational research, have<br />
scientific collaborations,<br />
and link clinical data with<br />
scientific data.”<br />
From left to right: Laura Donlin, PhD, Co-Director of the Derfner Foundation Precision Medicine Laboratory and<br />
Assistant Scientist, and Vivian P. Bykerk, MD, Director of the Inflammatory Arthritis Center of Excellence and<br />
Associate Attending Physician, review data for the AMP study.
Hospital for Special Surgery 13<br />
Baohong Zhao, PhD, Assistant Scientist, has identified two different methods for protecting against excessive<br />
osteoclast formation and bone destruction in disease models of osteoporosis and rheumatoid arthritis.<br />
Battling bone loss with<br />
a promising microRNAtargeting<br />
therapy<br />
Small non-coding RNA molecules<br />
that are approximately 21 to<br />
25 nucleotides in length, or<br />
microRNAs (miRNAs), regulate<br />
gene expression and functions<br />
in a variety of biological and<br />
pathological settings. While<br />
miRNA-based therapies have<br />
recently shown significant<br />
promise in the treatment of<br />
diseases like cancer, diabetes<br />
and hepatitis C, their use<br />
has been underexplored in<br />
osteoporosis and rheumatoid<br />
arthritis—until now. Baohong<br />
Zhao, PhD, Assistant Scientist<br />
in the Arthritis and Tissue<br />
Degeneration Program and The<br />
David Z. Rosensweig Genomics<br />
Research Center, has been using<br />
miRNA-sequencing techniques<br />
to profile genome-wide changes<br />
in miRNAs that are involved in<br />
the differentiation of osteoclasts.<br />
She has identified two different<br />
methods for protecting against<br />
excessive osteoclast formation<br />
and bone destruction in disease<br />
models of ovariectomy-induced<br />
osteoporosis and rheumatoid<br />
arthritis. One approach involves<br />
using a genetic knockout of<br />
miR-182 and the other involves<br />
a specific inhibitor targeting<br />
miR-182. “Our exciting genetic<br />
evidence and outstanding<br />
pharmacological results<br />
obtained from disease models<br />
provide a proof of concept for<br />
the efficacy of therapeutic<br />
targeting of miR-182 to prevent<br />
bone loss and highlight the<br />
translational implications<br />
of targeting miR-182 in<br />
treating osteolytic diseases,”<br />
says Dr. Zhao. “Now we are<br />
collaborating with translational<br />
researchers to see if we can<br />
develop more appropriate<br />
approaches to deliver a miR-<br />
182 inhibitor to patients with<br />
osteoporosis and arthritis to<br />
suppress bone loss.”<br />
While developing a safe and<br />
effective delivery system<br />
for this therapy is a priority,<br />
Dr. Zhao hopes that this<br />
miRNA will eventually be used<br />
as a biomarker to predict the<br />
progression of these diseases to<br />
prevent bone loss early on.
14<br />
Division of <strong>Rheumatology</strong><br />
Unraveling the molecular<br />
mysteries of lupus<br />
<strong>HSS</strong> Research Institute scientists<br />
are conducting studies at the<br />
molecular level to uncover new<br />
targets for lupus treatment.<br />
Alessandra Pernis, MD, The<br />
Peter Jay Sharp Chair in Lupus<br />
Research and Senior Scientist, is<br />
identifying molecular pathways<br />
of autoimmunity in the disease.<br />
Her work focuses on B cells,<br />
important players in autoimmune<br />
disease, including a subset called<br />
age-associated B cells, also<br />
known as ABCs. Dr. Pernis has<br />
discovered that ABC cells play two<br />
key roles in autoimmunity. “They<br />
can behave like B cells by making<br />
autoantibodies, and they can<br />
behave like inflammatory cells by<br />
making inflammatory cytokines,”<br />
she says. “Understanding the<br />
pathways that regulate these cells<br />
could represent a major advance<br />
in lupus as well as autoimmunity<br />
in general.”<br />
Using genome-wide transcriptional<br />
and epigenetic analysis of ABCs,<br />
Dr. Pernis and her team have<br />
uncovered the mechanism<br />
by which ABCs are regulated.<br />
“The majority of patients with<br />
autoimmunity are women, but<br />
until now we have not been able<br />
to find a molecular link,” says<br />
Dr. Pernis. “This is the first time<br />
we can see clear differences in<br />
males and females and how they<br />
behave at the transcriptional<br />
as well as the epigenetic level.”<br />
This research will enable us to<br />
uncover new treatment targets.<br />
Separately, Theresa T. Lu,<br />
MD, PhD, Associate Scientist,<br />
whose research is supported<br />
by the St. Giles Research Chair,<br />
is making headway toward<br />
understanding photosensitivity,<br />
whereby the sun’s ultraviolet<br />
(UV) light can trigger skin rashes<br />
as well as flares in patients.<br />
Photosensitivity affects 30 to<br />
60 percent of lupus patients.<br />
Dr. Lu’s research centers on<br />
Langerhans cells, immune<br />
cells in the top layer of skin. In<br />
a study published in Science<br />
Translational Medicine in <strong>2018</strong>,<br />
Dr. Lu, <strong>HSS</strong> colleagues and<br />
scientists at other institutions<br />
found that in healthy people,<br />
these cells protect the skin from<br />
UV damage. “With UV exposure,<br />
Langerhans cells normally<br />
activate ADAM17, a molecule<br />
that activates epidermal growth<br />
factor receptor (EGFR) ligands,<br />
helping skin cells to survive,”<br />
says Dr. Lu. In lupus models,<br />
Langerhans cells expressed less<br />
of the ADAM17 molecule, so<br />
they were less able to protect<br />
the skin. However, when EGFR<br />
ligand was added to the skin<br />
in lupus models, fewer lesions<br />
developed. More research is<br />
needed, but “stimulating EGFR<br />
in the skin may be an approach<br />
to ameliorating photosensitivity<br />
and systemic disease in lupus<br />
patients,” says Dr. Lu.<br />
Above: Langerhans cells (in red) sit<br />
among and protect the keratinocytes<br />
(in blue) in the skin epidermis.<br />
Photo Credit: William D. Shipman,<br />
PhD, Lu Lab, Autoimmunity and<br />
Inflammation Program<br />
Left, from left to right:<br />
Alessandra Pernis, MD, Senior<br />
Scientist, is identifying molecular<br />
pathways that play key roles in<br />
lupus, and Theresa T. Lu, MD,<br />
PhD, Associate Scientist, is<br />
gaining a better understanding of<br />
photosensitivity in lupus patients.
Hospital for Special Surgery 15<br />
From left to right: Jane E. Salmon, MD, Director of the Lupus and Antiphospholipid Syndrome Center of<br />
Excellence and Attending Physician, and Carl P. Blobel, MD, PhD, Director of the Arthritis and Tissue<br />
Degeneration Program and Senior Scientist, have discovered that iRhom2 may be an attractive new target for<br />
treating patients with lupus and hemophilic arthropathy.<br />
A promising new target for<br />
treating autoimmune diseases<br />
<strong>HSS</strong> scientists have identified a<br />
key protein that helps to regulate<br />
inflammation and could become<br />
a target for treating autoimmune<br />
diseases. The protein iRhom2<br />
appears to play a critical role<br />
in causing kidney damage in<br />
patients with lupus and seems to<br />
contribute to osteoporosis and<br />
joint damage in patients with<br />
hemophilic arthropathy.<br />
In a study published in the<br />
April <strong>2018</strong> issue of The Journal<br />
of Clinical Investigation, <strong>HSS</strong><br />
researchers and international<br />
colleagues found that<br />
inactivating iRhom2—which<br />
regulates ADAM17, whose<br />
substrates, such as TNF-α<br />
and heparin-binding EGF (HB-<br />
EGF), have been implicated in<br />
the pathogenesis of chronic<br />
kidney disease—prevented<br />
inflammation and irreversible<br />
scarring in lupus nephritis<br />
models. These same pathways<br />
were found to be upregulated<br />
in kidney biopsies from lupus<br />
patients. “The benefit of this<br />
approach is selective and<br />
simultaneous inhibition of two<br />
major pathological mediators<br />
of tissue damage in lupus,” says<br />
Jane E. Salmon, MD, Director of<br />
the Lupus and Antiphospholipid<br />
Syndrome Center of Excellence,<br />
Collette Kean Research Chair,<br />
and Attending Physician.<br />
In another study, published<br />
in Blood in September <strong>2018</strong>,<br />
<strong>HSS</strong> researchers found that<br />
inactivating iRhom2/TNF-α<br />
prevented the bone erosion and<br />
joint inflammation often seen in<br />
hemophilic arthropathy. “This is<br />
a major breakthrough because<br />
it points toward exciting new<br />
approaches for treatment of<br />
“The benefit of<br />
inactivating iRhom2<br />
is selective and<br />
simultaneous<br />
inhibition of two major<br />
pathological mediators<br />
of tissue damage in<br />
lupus.”<br />
Jane E. Salmon, MD, Director of<br />
the Lupus and Antiphospholipid<br />
Syndrome Center of Excellence<br />
and Attending Physician<br />
these two major manifestations<br />
of hemophilic arthropathy,” says<br />
Carl P. Blobel, MD, PhD, Director<br />
of the Arthritis and Tissue<br />
Degeneration Program, Virginia F.<br />
and William R. Salomon Chair<br />
in Musculoskeletal Research,<br />
and Senior Scientist.
16<br />
Division of <strong>Rheumatology</strong><br />
Investigating stem cells for<br />
repairing fibrotic skin<br />
“We think there<br />
are particular<br />
subpopulations of<br />
ADSCs that help to<br />
repair fibrotic skin, and<br />
we think there is a role<br />
for immune cells.”<br />
Theresa T. Lu, MD, PhD,<br />
Associate Scientist<br />
lymphotoxin to injected ADSCs<br />
would improve ADSC survival<br />
and effectiveness. They found<br />
that this combined regimen was<br />
able to partially reverse fibrosis.<br />
The question now is how exactly<br />
the ADSCs are working to repair<br />
fibrotic skin. “We think there<br />
are particular subpopulations<br />
of ADSCs that help to repair<br />
fibrotic skin, and we think there<br />
is a role for immune cells,”<br />
says Dr. Lu.<br />
Theresa T. Lu, MD, PhD, Associate Scientist, is studying adiposederived<br />
stromal cells (ADSCs) as a potential therapy for patients with<br />
scleroderma and other diseases.<br />
One of the major challenges<br />
in managing scleroderma<br />
patients is the lack of effective<br />
treatments for skin fibrosis.<br />
This condition is not only<br />
painful and can lead to severe<br />
joint contractures and loss<br />
of hand function, but it can<br />
also cause asymmetric limb<br />
or facial growth in children.<br />
In addition, wound healing is<br />
compromised. Theresa T. Lu,<br />
MD, PhD, Associate Scientist<br />
and a member of the Division<br />
of Pediatric <strong>Rheumatology</strong>,<br />
and members of her lab<br />
have been studying adiposederived<br />
stromal cells (ADSCs),<br />
which contribute to the repair<br />
and regeneration of tissues,<br />
including skin. Her lab has found<br />
that ADSC numbers are reduced<br />
in skin fibrosis—most likely<br />
due to cell death—suggesting<br />
that effective replenishment of<br />
these cells could repair fibrotic<br />
skin and be a possible therapy<br />
in a multipronged approach for<br />
scleroderma patients. In a study<br />
published in The Journal<br />
of Clinical Investigation,<br />
Dr. Lu and colleagues found that<br />
certain immune cells known<br />
as dendritic cells help ADSCs<br />
survive in fibrotic skin. There is<br />
an interest in the scleroderma<br />
field in injecting ADSCs to<br />
repair the skin, but one of the<br />
limitations is that ADSCs do<br />
not survive a long time. Dr. Lu’s<br />
group reasoned that adding<br />
the dendritic cell-derived signal<br />
In <strong>2017</strong>, Dr. Lu received a<br />
grant from the Scleroderma<br />
Foundation to determine which<br />
ADSC subpopulations are<br />
reparative and which ones may<br />
be harmful. Dr. Lu also recently<br />
received funding from the nonprofit<br />
organization A Lasting<br />
Mark to begin to examine the<br />
role of immune cells in mediating<br />
ADSC effects. One future goal<br />
is to find out whether ADSC<br />
populations in children’s skin<br />
are more or less susceptible to<br />
damage by fibrosis compared<br />
to adults’ skin. “We know that<br />
children’s skin heals better<br />
than adults’ skin,” says Dr. Lu.<br />
“Determining whether there<br />
are ADSC subpopulations that<br />
are more protective in children<br />
will help us gain a better<br />
understanding of scleroderma—<br />
and potentially improve therapies<br />
for patients.”
Hospital for Special Surgery 17<br />
Optimizing postsurgical outcomes<br />
Ensuring that patients are<br />
medically ready for surgery can<br />
help improve outcomes—and<br />
their overall experience at <strong>HSS</strong>.<br />
“Our orthopaedic surgeons were<br />
one of the first groups in the<br />
nation to embrace the concept<br />
of co-management of the<br />
patient,” says Linda A. Russell,<br />
MD, Director of the Division of<br />
Perioperative Medicine, Anne<br />
and Joel Ehrenkranz Chair in<br />
Perioperative Medicine, and<br />
Associate Attending Physician.<br />
“Every single patient who’s<br />
admitted to <strong>HSS</strong> has a surgeon<br />
and a medical physician familiar<br />
with the perioperative care of the<br />
orthopaedic patient.”<br />
Physicians in perioperative<br />
medicine, a field that has<br />
emerged over the last 15 years,<br />
are assigned to follow specific<br />
patients to help ensure continuity<br />
of care. “Perioperative medicine<br />
physicians see patients before<br />
surgery and try to get them in<br />
as good a shape as they can,”<br />
says Dr. Russell. “They also see<br />
patients when they’re in the<br />
hospital. Then they’re available to<br />
patients for up to 90 days or so<br />
after the surgery for any related<br />
medical conditions.”<br />
Prior to surgery, <strong>HSS</strong> patients<br />
are carefully assessed to identify<br />
and address any medical<br />
problems that could impact<br />
surgical outcomes, including<br />
uncontrolled diabetes, cardiac<br />
issues, skin infections and, most<br />
recently, obesity. “There’s a lot<br />
of research that says if your<br />
BMI is 40 or higher, your risk of<br />
postoperative complications is<br />
much higher,” says Dr. Russell.<br />
In July <strong>2018</strong>, the Division of<br />
Perioperative Medicine added<br />
a weight-loss program to help<br />
obese patients lose at least<br />
5 percent of their total body<br />
weight before surgery. “We are<br />
probably the first hospital in the<br />
country that’s really focused on<br />
perioperative weight loss,” says<br />
Dr. Russell. Obese patients see a<br />
weight-management physician<br />
and nutritionist at <strong>HSS</strong> at least<br />
two to three months before<br />
surgery to jump-start healthy<br />
eating habits and weight loss.<br />
“We continue to follow up with<br />
these patients after surgery<br />
as well for long-term weight<br />
management,” says Caroline A.<br />
Andrew, MD, Assistant Attending<br />
Physician, who directs the<br />
weight management program<br />
at <strong>HSS</strong>. “Losing weight after<br />
surgery helps with recovery<br />
and can reduce postsurgical<br />
osteoarthritis, in addition to<br />
improving other comorbidities<br />
of obesity.”<br />
Many obese patients have<br />
diabetes, so perioperative<br />
medicine practitioners help them<br />
get the condition under control.<br />
These patients may work with<br />
an endocrinologist to achieve<br />
the healthiest A1C levels prior<br />
to surgery.<br />
Dr. Russell’s team of physicians,<br />
physician assistants and nurse<br />
practitioners also work to<br />
optimize the use of opioids and<br />
other pain medications before<br />
and after surgery. “A chronic<br />
pain physician sees patients who<br />
take opioids daily to taper pain<br />
medications preoperatively and<br />
design the postoperative pain<br />
program,” she says.<br />
After surgery, wound issues,<br />
leg swelling and other<br />
complications can be treated<br />
by the perioperative medicine<br />
staff, saving the patient a trip<br />
to an urgent care facility or the<br />
emergency room.<br />
From left to right: Caroline A. Andrew, MD, Assistant Attending Physician,<br />
and Linda A. Russell, MD, Director of the Division of Perioperative<br />
Medicine and Associate Attending Physician, collaborate to ensure<br />
patients are medically ready for surgery.<br />
Over the last decade, the<br />
Division of Perioperative<br />
Medicine has developed<br />
numerous surgical guidelines,<br />
including rules about when<br />
medications should be stopped<br />
preoperatively and started<br />
postoperatively; which patients<br />
with diabetes can be cleared for<br />
the OR; and which patients are<br />
candidates for bilateral knee<br />
replacements. “The goal is to<br />
help decrease postoperative<br />
complications and readmission<br />
rates,” says Dr. Russell. “We also<br />
hope the guidelines can provide<br />
a better patient experience.”
18<br />
Division of <strong>Rheumatology</strong><br />
Complex Cases<br />
Case 1<br />
Eosinophilic Fasciitis<br />
Associated with Cancer<br />
Immunotherapy<br />
19<br />
Case 2<br />
Inflammatory Erosive<br />
Arthritis and Tendon<br />
Rupture in Sarcoidosis<br />
20<br />
Case 3<br />
Severe Lupus with<br />
Nephritis and Catatonia;<br />
Excellent Response to<br />
Aggressive Treatment<br />
21<br />
Case 4<br />
Subacute Bacterial<br />
Endocarditis Masquerading<br />
as Polymyalgia Rheumatica<br />
22<br />
Case 5<br />
Retiform Purpura<br />
Initially Concerning for<br />
Granulomatosis with<br />
Polyangiitis<br />
23<br />
<strong>HSS</strong> rheumatologists frequently receive calls from physicians around the world<br />
asking for advice in treating complex cases. Recent calls have come from Sri Lanka,<br />
France, Kuwait and Puerto Rico. The following five cases are excerpted from Grand<br />
Rounds from <strong>HSS</strong>: Management of Complex Cases, which includes follow-up data<br />
and a clinical treatment discussion.<br />
Visit the entire list of Case references online at hss.edu/complexcases
Hospital for Special Surgery 19<br />
Case 1 presented by David R. Fernandez, MD, PhD, and Anne R. Bass, MD<br />
Eosinophilic Fasciitis Associated<br />
with Cancer Immunotherapy<br />
Case <strong>Report</strong><br />
A 48-year-old man was referred for<br />
complaints of “stiffness” in his legs. One<br />
year prior to presentation he was diagnosed<br />
with stage IV lung adenocarcinoma (EGFR<br />
exon 19 deletion) with lung metastases. He<br />
was treated with nivolumab and erlotinib and<br />
experienced 50 percent tumor regression.<br />
Six months into treatment, he began to<br />
note tightness and pain in his thigh and calf<br />
muscles, shoulders, ankles and wrists. He<br />
had trouble walking and rising from a chair.<br />
He also noted calf cramps and leg swelling.<br />
He denied Raynaud’s phenomenon.<br />
Laboratory testing revealed CPK 933<br />
and an absolute eosinophil count of 700.<br />
CPK normalized without intervention,<br />
but total eosinophils climbed to 3,500<br />
over the next three months. Nivolumab<br />
was discontinued and the patient was<br />
referred to rheumatology. Examination<br />
revealed thickening of the fascia of the<br />
forearms and of the legs below the knees,<br />
which limited mobility at the elbows,<br />
wrists, knees and ankles. The patient<br />
could barely pronate or supinate the<br />
right elbow. Extension of the right wrist<br />
was limited to 20° due to tightening<br />
of the fascia, and there were flexion<br />
contractures of both knees. A “groove<br />
sign” was noted over the left leg and right<br />
forearm (Figure 1). The superficial skin,<br />
nailfold capillaries and joints themselves<br />
were normal. The patient was treated<br />
with high-dose oral corticosteroids with<br />
moderate improvement. Deep skin biopsy<br />
was consistent with eosinophilic fasciitis<br />
(Figure 2). The patient continued treatment<br />
with high-dose corticosteroids and<br />
experienced gradual softening of the fascia<br />
and increased mobility of the arms and,<br />
to a lesser degree, the legs. Methotrexate<br />
was added to his regimen to enable a rapid<br />
steroid taper prior to lobectomy for residual<br />
disease. The patient continued to require<br />
low doses of prednisone 10 months after the<br />
onset of his disease.<br />
Discussion<br />
Eosinophilic fasciitis is a rare disease of<br />
unknown etiology. It is characterized by<br />
peripheral eosinophilia and induration of<br />
the deep fascia underlying the skin. [1] It is<br />
generally steroid-responsive, but it often<br />
requires prolonged therapy and not all<br />
changes may be reversible. Eosinophilic<br />
fasciitis can be associated with trauma,<br />
drugs, infections, autoimmune conditions<br />
and cancer, but to our knowledge, this<br />
is the first case associated with cancer<br />
immunotherapy. [2] The timing of this<br />
patient’s presentation suggests that the<br />
Figure 1: Photograph of the left leg demonstrating a “groove sign” along the path of a superficial vein.<br />
nivolumab and not the cancer itself<br />
was responsible.<br />
Nivolumab is one of a new class of<br />
medications directed at enhancing<br />
antitumor immunity by inhibiting normal<br />
checkpoints on immune cell function.<br />
Immune checkpoint blockade has<br />
revolutionized the treatment of many<br />
cancers but at the expense of frequent<br />
immune-mediated side effects. [3] The<br />
programmed cell death-1 (PD-1) receptor<br />
is an immune checkpoint molecule<br />
expressed on activated T cells, which<br />
transmits inhibitory signals to T cells and<br />
enhances the generation of regulatory<br />
T cells. High expression of PD-1 on T<br />
cells can be seen in the setting of chronic<br />
infections and is associated with a<br />
phenomenon called “exhaustion,” which<br />
is associated with poor T cell function and<br />
high expression of inhibitory molecules<br />
on T cells. [4]<br />
Normally, cells in the peripheral organs can<br />
increase expression of programmed cell<br />
death ligand 1 (PD-L1) in certain settings.<br />
However, cancer cells also frequently<br />
express PD-L1, leading to diminished<br />
T cell-directed immune responses<br />
against tumors. Nivolumab blocks PD-1<br />
signaling, leading to enhanced antitumor<br />
immunity, but has important side effects<br />
related to induction of autoimmunity,<br />
such as rash, hepatitis, pneumonitis and<br />
thyroiditis. Interestingly, the autoimmune<br />
manifestations associated with<br />
immunotherapy can be short-lived when<br />
treated with steroids or tumor necrosis<br />
factor inhibitors. They generally lack<br />
the characteristic autoantibodies<br />
associated with spontaneous-onset<br />
rheumatologic diseases. [5]<br />
This case implies a potential role for PD-1<br />
signaling as a key tolerance mechanism,<br />
Figure 2: Deep skin biopsy demonstrating<br />
broad, hyalinized collagen bundles within the<br />
fascia with deposition of mucin and a<br />
lymphocytic and plasma cell infiltrate.<br />
preventing the development of eosinophilic<br />
fasciitis in susceptible individuals.<br />
References<br />
1. Lebeaux D, Frances C, Barete S, et al.<br />
Eosinophilic fasciitis (Shulman disease): new<br />
insights into the therapeutic management<br />
from a series of 34 patients. <strong>Rheumatology</strong><br />
2012;51(3):557–61.<br />
2. Pinal-Fernandez I, Selva-O’Callaghan A., Grau<br />
JM. Diagnosis and classification of eosinophilic<br />
fasciitis. Autoimmun Rev 2014;13(4–5):379–82.<br />
3. Haanen JB a. G, Thienen H Van, Blank CU.<br />
Toxicity Patterns With Immunomodulating<br />
Antibodies and Their Combinations. Semin<br />
Oncol 2015;42(3):423–8.<br />
4. Wherry EJ, Kurachi M. Molecular and cellular<br />
insights into T cell exhaustion. Nat Rev<br />
Immunol 2015;15(8):486–99.<br />
5. Villadolid J, Amin A. Immune checkpoint<br />
inhibitors in clinical practice: update on<br />
management of immune-related toxicities.<br />
Transl lung cancer Res 2015;4(5):560–75.<br />
Author Disclosures<br />
Dr. David R. Fernandez does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.<br />
Dr. Anne R. Bass does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.
20<br />
Division of <strong>Rheumatology</strong><br />
Case 2 presented by Arthur M. F. Yee, MD, PhD<br />
Inflammatory Erosive Arthritis<br />
and Tendon Rupture in Sarcoidosis<br />
Case <strong>Report</strong><br />
A 64-year-old woman was referred to<br />
the <strong>HSS</strong> Division of <strong>Rheumatology</strong> for a<br />
second opinion regarding chronic pain<br />
and swelling of the right wrist and acute<br />
loss of extension of the right small finger.<br />
The patient had a 20-year history of<br />
sarcoidosis, initially presenting as right<br />
eye uveitis, retinal vasculitis and acute<br />
polyarthritis. Evaluation at the time revealed<br />
mediastinal lymphadenopathy, the biopsy<br />
of which led to the diagnosis of sarcoidosis.<br />
The patient was treated chronically for<br />
many years with varying dosages of<br />
prednisone before the eventual addition of<br />
weekly methotrexate enabled subsequent<br />
withdrawal of all corticosteroid therapies.<br />
After several months of clinical remission,<br />
methotrexate was also discontinued. She<br />
remained symptom-free for several months<br />
before developing insidiously progressive<br />
chronic right wrist pain and swelling. MRI<br />
demonstrated extensive inflammatory<br />
arthritis and tenosynovitis with marked<br />
erosions in the distal radius and ulna and<br />
encroachment upon the extensor tendons<br />
(Figure 1). She was treated with nonsteroidal<br />
anti-inflammatory drugs and periodic<br />
short courses of systemic corticosteroids<br />
with marginal responses. After two years<br />
of waxing and waning inflammatory right<br />
wrist arthritis, she developed an acutely<br />
dropped right small finger, prompting<br />
referral to <strong>HSS</strong>.<br />
Physical examination was notable for<br />
moderate swelling, tenderness and<br />
warmth of the right wrist; loss of extension<br />
of the right small finger; and baseline loss<br />
of visual acuity of the right eye without<br />
active inflammation. There was no<br />
evidence of active synovitis elsewhere.<br />
Complete blood count, metabolic panel,<br />
erythrocyte sedimentation rate, C-reactive<br />
protein, angiotensin-converting enzyme,<br />
rheumatoid factor, and anti-cyclic<br />
citrullinated protein antibodies were normal<br />
or negative. Large erosions of the distal<br />
right ulna and radius were evident on plain<br />
radiography (Figure 2).<br />
An immediate consultation to the Hand<br />
and Upper Extremity Service was made,<br />
and the patient underwent prompt<br />
synovectomy and repair of the ruptured<br />
extensor tendons. Histopathology<br />
showed inflammatory synovitis and<br />
excluded infectious etiologies. After<br />
a brief, uncomplicated postoperative<br />
period, oral methotrexate was initiated<br />
and was expeditiously titrated to 15 mg<br />
weekly. The patient has done well for five<br />
years without recurrence of inflammatory<br />
arthritis or uveitis.<br />
Discussion<br />
Sarcoidosis is an enigmatic systemic<br />
inflammatory disorder characterized<br />
by non-caseating granulomatous<br />
inflammation of potentially any tissue.<br />
While nonspecific arthralgias are<br />
common, frank inflammatory arthritis<br />
is infrequent and can be categorized<br />
as acute or chronic. In one recent<br />
long-term North American series,<br />
one‐tenth of all patients developed acute<br />
inflammatory arthritis/periarthritis, [1]<br />
typically oligoarticular or polyarticular,<br />
although prevalence may range widely<br />
depending on the population examined.<br />
The most stereotypical presentation<br />
is Lofgren’s syndrome (acute bilateral<br />
ankle periarthritis, erythema nodosum,<br />
and uveitis), which can be quite painful<br />
but is fortunately self-limited and<br />
nondestructive. [2] In most cases, acute<br />
sarcoid arthritis is reminiscent of<br />
exacerbations of inflammatory arthritis<br />
seen in other systemic conditions,<br />
likely reflecting nonspecific systemic<br />
inflammatory processes rather than<br />
direct granulomatous infiltration in the<br />
joint. In contrast, infiltrative chronic<br />
granulomatous synovitis, as seen<br />
in the presented case, is much less<br />
common, is sometimes quite resistant<br />
to medical therapy, and occasionally<br />
leads to local tissue injury. [3] A diverse<br />
array of clinical scenarios, such as<br />
bursitis, enthesopathies, sacroiliitis, and<br />
carpal tunnel syndrome, resulting from<br />
granulomatous inflammation have<br />
been reported. [4]<br />
The challenges facing <strong>HSS</strong> physicians in<br />
this case were to first repair the ruptured<br />
fifth extensor mechanism and then to<br />
implement a medical regimen to prevent<br />
recurrence. After adequate postoperative<br />
healing and rehabilitation, medical<br />
management was initiated.<br />
Steroid-sparing agents are increasingly<br />
being used for the treatment of sarcoidosis,<br />
but none are formally approved. Nonetheless,<br />
methotrexate has emerged as the preferred<br />
steroid-sparing agent. [5] Controlled clinical<br />
studies of methotrexate in the treatment<br />
of sarcoidosis have demonstrated efficacy<br />
in specific common phenotypes, such as<br />
pulmonary disease, cardiomyopathy and<br />
panuveitis. There are ample case reports<br />
and series of use in other manifestations,<br />
such as involvement of the skin, bone,<br />
neuraxis, muscle, etc. [4]<br />
The acknowledged efficacy of methotrexate<br />
has led to the development of proposed<br />
guidelines for its use in sarcoidosis. [5] Many<br />
recommendations echo those for the use<br />
of methotrexate in rheumatoid arthritis, but<br />
some reflect the personal practice and expert<br />
opinion of “sarcoidologists.” It is very notable<br />
that the majority of experts recommended<br />
weekly methotrexate maintenance dosages<br />
of no more than 15 mg. Therefore, it is<br />
possible that methotrexate is underutilized<br />
in sarcoidosis.<br />
References<br />
1. Ungprasert P, Crowson C S, et al. Clinical<br />
characteristics of sarcoid arthropathy: a<br />
population-based study. Arthritis Care Res<br />
2016; 68: 695–9.<br />
2. Mana J, Gomez-Vaquero C, et al. Lofgren’s<br />
syndrome revisited: a study of 186 patients.<br />
Am J Med 1999; 107: 240–5.<br />
3. Chu A, Ginat D, et al. Chronic sarcoid arthritis<br />
presenting as an intra-articular knee mass.<br />
J Clin Rheumatol 2009; 15: 190–2.<br />
4. Yee AMF. Sarcoidosis: rheumatology<br />
perspective. Best Pract Res Clin Rheumatol.<br />
5. Cremers JP, Drent M, et al. Multinational<br />
evidence-based World Association of<br />
Sarcoidosis and Other Granulomatous<br />
Disorders recommendations for the use<br />
of methotrexate in sarcoidosis: integrating<br />
systematic literature research and expert<br />
opinion of sarcoidologists worldwide. Current<br />
Opin Pulm Med 2013; 19: 545–61.<br />
Author Disclosures<br />
Dr. Yee is on a Speaker’s Bureau and has<br />
participated on Advisory Boards for Bristol-<br />
Myers Squibb and has stock shares in Abbvie<br />
and Pfizer.<br />
Figure 1: Fat-suppressed MRI (coronal view) of<br />
the dorsum of the right wrist/hand. Bulky<br />
inflammatory synovitis (enclosed in red oval)<br />
impinges on the extensor digitorum longus<br />
tendon (arrows) to the small finger.<br />
Figure 2: Frontal view of the right wrist/hand.<br />
Large erosions (encircled) are evident in the distal<br />
radius and ulna.
Hospital for Special Surgery 21<br />
Case 3 presented by Naveed Chaudhry, MD, Steven P. Salvatore, MD,<br />
and Kyriakos A. Kirou, MD<br />
Severe Lupus with Nephritis and<br />
Catatonia; Excellent Response to<br />
Aggressive Treatment<br />
Case <strong>Report</strong><br />
A 34-year-old woman was diagnosed with<br />
systemic lupus erythematosus (SLE) in<br />
2011 after she presented with arthritis,<br />
photosensitivity, alopecia and oral ulcers.<br />
She was treated with short courses of<br />
prednisone. Her serologic profile was<br />
positive for ANA, anti-dsDNA, anti-Sm<br />
and anti-RNP antibodies. In January 2013,<br />
she was admitted to another hospital for<br />
left popliteal vein deep vein thrombosis<br />
(DVT) and pulmonary embolism (PE). She<br />
was also noted to have nephrotic range<br />
proteinuria and pleuropericarditis. She was<br />
treated with anticoagulation (enoxaparin to<br />
warfarin) and prednisone 60 mg/day with<br />
improved symptoms.<br />
She first presented to us in February 2013<br />
with marked leg edema and dyspnea on<br />
exertion. Past medical and family histories<br />
were unremarkable. Her blood pressure<br />
was 112/82, pulse 85, and she had 2+ leg<br />
edema. Her Hgb was 13.9 gm/dl, serum<br />
creatinine (Cr) 0.64 mg/dL, albumin<br />
1.7 gm/dl, cholesterol 366 mg/dl, ESR 72<br />
mm/hr, C3 167 mg/dL, C4 64 mg/dL, and<br />
anti-DNA 2+.<br />
Her urine sediment was bland, but her urine<br />
protein-creatinine ratio (UPCR) was 5.2.<br />
She was on prednisone 50 mg/day, and<br />
mycophenolate mofetil (MMF) was added to<br />
her regimen.<br />
Her edema got much worse, however,<br />
and she was readmitted three weeks later<br />
(March 2013) with severe anasarca. She<br />
received IV methylprednisolone 500 mg<br />
daily for three days and, after switching<br />
from warfarin to heparin, a renal biopsy<br />
was performed. This revealed ISN/RPS<br />
Class V membranous lupus nephritis<br />
(Figures 1–2). MMF was discontinued<br />
because of diarrhea, and she was treated<br />
with IV cyclophosphamide (IVCY). The<br />
patient was discharged on dexamethasone<br />
9 mg, losartan 25 mg, bumetanide 1 mg,<br />
warfarin, atorvastatin 40 mg, calcium,<br />
vitamin D3, and alendronate 70 mg weekly.<br />
She was readmitted to the hospital in early<br />
April 2013 after she developed symptoms<br />
of mania, depression and psychosis with<br />
paranoia. She was also noted to have<br />
severe edema and pneumonia.<br />
The patient was treated with IV antibiotics<br />
and diuretics, and glucocorticoids<br />
were continued. After treatment with<br />
haloperidol, she developed catatonia<br />
with motor rigidity, immobility, staring,<br />
mutism and negativism. She was not<br />
hyperthermic, and creatine kinase and<br />
electroencephalogram were normal.<br />
She was treated with IV lorazepam 2 mg,<br />
and high-dose glucocorticoids were<br />
continued. Her mental status normalized<br />
after a few days. Pulmonary infiltrates<br />
cleared 11 days later and she was given<br />
her second IVCY dose as well as IV<br />
rituximab 1,000 mg. She was discharged<br />
on prednisone 40 mg daily with a slow<br />
taper. She continued with monthly IVCY<br />
for a total of five cycles (the last one<br />
was in August 2013) and had gradual<br />
improvement of proteinuria and edema.<br />
By September 2013, her UPCR was<br />
0.37 and her albumin had normalized.<br />
She was started on azathioprine<br />
50 mg BID as maintenance treatment<br />
while the prednisone was tapered to<br />
5 mg/day. Warfarin was discontinued<br />
without recurrent thrombosis. Her<br />
antiphospholipid antibodies, including<br />
lupus anticoagulant, have remained<br />
negative. The patient was able to go back<br />
to her job full-time.<br />
Discussion<br />
We have described a complex case of<br />
lupus with active disease in several<br />
organs and excellent response to prompt<br />
and aggressive management. The<br />
patient first presented with nephrosis<br />
and secondary DVT-PE. Then she<br />
developed pleuropericarditis and, finally,<br />
neuropsychiatric (NP) SLE with bipolar<br />
symptoms, psychosis and catatonia.<br />
Although glucocorticoids may cause<br />
psychosis, it was unlikely they were the<br />
culprit here, as they had been tolerated<br />
well. The patient’s NP symptoms occurred<br />
concurrently with disease activity in<br />
other organs. Catatonia is a rare NP<br />
manifestation of SLE, often associated<br />
with an underlying bipolar disorder. [1]<br />
It may be triggered by antipsychotics<br />
like haloperidol and often responds to<br />
lorazepam, as in our case. Treatment of<br />
lupus with glucocorticoids, IVCY and/or<br />
plasma exchange is also effective. [1]<br />
Pure membranous lupus nephritis,<br />
when accompanied by nephrotic range<br />
proteinuria, is also a severe manifestation<br />
of SLE and demands treatment with<br />
MMF, IVCY or cyclosporine. [2, 3] We added<br />
rituximab, as it is often effective in severe<br />
lupus as well as NPSLE. [4]<br />
References<br />
1. Grover S, Parakh P, Sharma A et al. Catatonia<br />
in systemic lupus erythematosus: a case<br />
report and review of literature. Lupus 2013;<br />
22: 634–8.<br />
2. Austin HA, 3rd, Illei GG, Braun MJ, Balow JE.<br />
Randomized, controlled trial of prednisone,<br />
cyclophosphamide, and cyclosporine in<br />
lupus membranous nephropathy. J Am Soc<br />
Nephrol 2009; 20: 901–11.<br />
3. Radhakrishnan J, Moutzouris DA, Ginzler EM<br />
et al. Mycophenolate mofetil and intravenous<br />
cyclophosphamide are similar as induction<br />
therapy for class V lupus nephritis. Kidney Int<br />
2010; 77: 152–60.<br />
4. Tokunaga M, Saito K, Kawabata D et al.<br />
Efficacy of rituximab (anti-CD20) for<br />
refractory systemic lupus erythematosus<br />
involving the central nervous system. Ann<br />
Rheum Dis 2007; 66: 470–5.<br />
Author Disclosures<br />
Dr. Naveed Chaudhry does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.<br />
Dr. Kyriakos A. Kirou does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.<br />
Dr. Steven P. Salvatore does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.<br />
Figure 1: C3 staining by immunofluorescence<br />
microscopy showing global 3+ capillary wall<br />
deposits (40x).<br />
Figure 2: Electron microscopy revealing global<br />
subepithelial electron dense deposits (arrows).
22<br />
Division of <strong>Rheumatology</strong><br />
Case 4 presented by Alana B. Levine, MD<br />
Subacute Bacterial<br />
Endocarditis Masquerading<br />
as Polymyalgia Rheumatica<br />
Case <strong>Report</strong><br />
A 70-year-old woman was referred to the<br />
<strong>HSS</strong> Division of <strong>Rheumatology</strong> for a second<br />
opinion regarding polymyalgia rheumatica<br />
(PMR). She had been diagnosed with PMR<br />
at another hospital eight months prior<br />
to presentation based on fatigue and an<br />
elevated ESR. Her fatigue resolved rapidly<br />
after starting prednisone 20 mg daily,<br />
which was tapered off over the course<br />
of two months. Fatigue recurred after<br />
discontinuing steroids and the patient was<br />
restarted on prednisone and, eventually,<br />
methotrexate.<br />
One month prior to presentation at <strong>HSS</strong>,<br />
the patient developed a new non-painful,<br />
non-pruritic leg rash. Skin biopsy revealed<br />
leukocytoclastic vasculitis. At the time, she<br />
was taking prednisone 5 mg daily, which<br />
was increased to 40 mg daily, and the<br />
rash resolved.<br />
On presentation to <strong>HSS</strong>, the patient<br />
complained of severe fatigue, nocturnal<br />
fevers to 101°F, night sweats and anorexia<br />
with a 20-pound weight loss.<br />
The patient’s past medical history was<br />
significant for mitral valve prolapse and<br />
osteopenia. She had dental work one<br />
month prior to the PMR diagnosis and had<br />
two caesarian sections in the past. Her<br />
medications included methylprednisolone<br />
4 mg daily, rabeprazole 20 mg daily, and<br />
calcium supplementation.<br />
On physical examination, the patient was in<br />
no acute distress. Her blood pressure was<br />
110/65 mm Hg, pulse 112, and temperature<br />
100.2°F. She weighed 104 pounds and was<br />
62 inches tall. Her exam was remarkable for<br />
a loud systolic murmur, heard throughout<br />
the precordium but most pronounced at<br />
the apex. She had fingernail clubbing and<br />
several non-blanching 2-mm palpable<br />
purpuric lesions over the shins. Her lung<br />
exam was unremarkable, pulses were<br />
strong throughout and without bruits,<br />
and she had no synovitis. The differential<br />
diagnosis at that time included systemic<br />
vasculitis, malignancy and endocarditis.<br />
Labs were significant for hemoglobin<br />
8.7 g/dL, serum creatinine 2.2 mg/dL<br />
(0.9 mg/dL one month prior), rheumatoid<br />
factor 222 IU/mL, ESR 53 mm/hr, CRP<br />
125 mg/L, C3 31 mg/dL, and C4 7 mg/dL.<br />
Urinalysis showed 2+ protein, 3+ blood,<br />
>30 WBC/hpf and >30 RBC/hpf.<br />
Antinuclear antibodies, double-stranded<br />
DNA antibodies, extractable nuclear<br />
antigens, and anti-CCP antibodies<br />
were negative.<br />
The patient was admitted for evaluation of<br />
acute renal failure. Multiple sets of blood<br />
cultures were drawn and held for slowgrowing<br />
organisms, and the patient was<br />
started on broad-spectrum antibiotics.<br />
A renal ultrasound was unremarkable. A<br />
transthoracic echocardiogram showed<br />
severe mitral regurgitation with a<br />
1.9 x 1.8 cm vegetation on the posterior<br />
mitral leaflet. Blood cultures grew<br />
gram-variable rods, which were later<br />
speciated as Suttonella indologenes.<br />
Due to the size of the vegetation and<br />
severe mitral regurgitation, the patient<br />
was recommended for mitral valve<br />
replacement surgery.<br />
Discussion<br />
Subacute bacterial endocarditis may cause<br />
a constellation of symptoms, including<br />
fatigue and malaise, fevers, valvular<br />
dysfunction, renal failure secondary to<br />
glomerulonephritis, and leukocytoclastic<br />
vasculitis. Suttonella indologenes is a<br />
gram-negative, rod-shaped bacterium<br />
found in normal respiratory tract flora, but it<br />
[1, 2]<br />
has been known to cause endocarditis.<br />
References<br />
1. Ozcan F, Yildiz A, Ozlu MF, et al. A case of fatal<br />
endocarditis due to Suttonella indologenes.<br />
Anadolu Kardiyol Derg 2011;11:85–7.<br />
2. Yang EH, Poon K, Pillutla P, Budoff MJ, Chung<br />
J. Pulmonary embolus caused by Suttonella<br />
indologenes prosthetic endocarditis<br />
in a pulmonary homograft. J Am Soc<br />
Echocardiogr 2011;24:592 e1–3.<br />
Author Disclosures<br />
Dr. Alana B. Levine does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.<br />
Figure 1: Transthoracic echocardiogram showing<br />
1.9 x 1.8 cm vegetation on the mitral valve.<br />
Figure 2: Transesophageal echocardiogram<br />
showing vegetation and flail posterior<br />
mitral leaflet.<br />
Figure 3: Transesophageal echocardiogram<br />
showing severe mitral regurgitation and<br />
perforation of the posterior mitral leaflet.
Hospital for Special Surgery 23<br />
Case 5 presented by Danielle Ramsden-Stein, MD, Sonali Narain MD, MPH, and<br />
Michael D. Lockshin, MD<br />
Retiform Purpura Initially<br />
Concerning for Granulomatosis<br />
with Polyangiitis<br />
Case <strong>Report</strong><br />
A 47-year-old woman with recurrent<br />
sinusitis and bronchitis, intermittent febrile<br />
rashes and depression presented to an<br />
outside hospital with rapidly progressing<br />
skin rash after eating at a seafood<br />
restaurant. She had bruises on her left<br />
shoulder, left thigh and under her left<br />
breast accompanied by fever to 102°F,<br />
arthralgias and fatigue. The rash worsened<br />
within 24 hours to involve her upper and<br />
lower extremities, cheeks, ears, breasts<br />
and abdomen. She denied trauma, toxic<br />
exposures, new medications, sick contacts,<br />
or recent travel.<br />
On examination, she had saddle nose<br />
deformity and necrotizing purpura<br />
with bullae developing over the<br />
dependent areas. She had proteinuria<br />
and pancytopenia. Lumbar puncture<br />
was negative, but chest X-ray showed<br />
left lower lobe consolidation. She was<br />
started on ceftriaxone/vancomycin. She<br />
developed a cough with blood-tinged<br />
sputum and gross hematuria. Head CT<br />
scan showed pansinusitis. Intravenous<br />
methylprednisolone 40 mg every six hours<br />
was prescribed. The lesions progressed<br />
from pruritic to tender, with darkening of<br />
color to purple, peaking on the third day<br />
of hospitalization, affecting approximately<br />
70 percent of her body surface area.<br />
Biopsy revealed leukocytoclastic<br />
vasculitis, and the patient requested<br />
transfer for further management.<br />
On admission, corticosteroid was<br />
continued, since new onset granulomatosis<br />
with polyangiitis (Wegener’s) was<br />
suggested by the rash, nose deformity,<br />
proteinuria and recurrent sinusitis.<br />
Antibody to proteinase 3 was strongly<br />
positive. Review of her pathology<br />
slides deemed the underlying process<br />
to be classic for a cocaine-induced<br />
vasculitis. After an initial dose of pulse<br />
methylprednisolone, the patient was<br />
started on oral prednisone 1 mg/kg dose<br />
tapered over a 20-day period. There was<br />
very slow improvement in the cutaneous<br />
lesions, and she eventually underwent<br />
multiple sessions of skin grafting. At the<br />
time of discharge, there was marked<br />
improvement with mild scarring. Despite<br />
repeated questioning, the patient did not<br />
admit to cocaine use.<br />
Discussion<br />
Although we were unable to confirm that<br />
the presentation of this rash in our patient<br />
was related to cocaine use, the pathology<br />
report prompted us to understand the<br />
pathophysiology of cocaine-induced<br />
vasculitis. Unlike granulomatosis with<br />
polyangiitis, cocaine-induced vasculitis<br />
is less commonly a true vasculitis but<br />
rather a vasculopathy with thrombosis. Its<br />
occurrence is associated with cocaine that<br />
has been contaminated with levamisole,<br />
a veterinary antihelminthic agent, although<br />
recently it has been hypothesized that<br />
cocaine itself may enhance complement<br />
synthesis and trigger the formation of<br />
C5b-9, resulting in endothelial cell injury.<br />
While levamisole has been acknowledged as<br />
possessing immunomodulatory properties<br />
since the 1960s, the mechanism is not<br />
well understood. It reportedly potentiates<br />
the psychotropic effects of cocaine and<br />
therefore makes it highly desirable to<br />
manufacturers of illegal cocaine. <strong>Report</strong>s<br />
consistently state that it is added to<br />
approximately 70 percent of cocaine<br />
available in the United States.<br />
In cocaine-induced disease, the classic<br />
skin finding is that of retiform purpura, a<br />
net-like pattern of irregular nonblanching,<br />
violaceous plaques. Skin biopsy shows a<br />
very distinctive intravascular occlusion<br />
without vasculitis, termed vasculopathy,<br />
primarily targeting capillaries and<br />
venules. Gross et al. found, in 16 patients,<br />
that 13 percent had a pure small vessel<br />
vasculitis, 40 percent thrombotic<br />
vasculopathy, and 47 percent vasculitis<br />
and thrombosis. [1]<br />
While ANCA positivity has been<br />
documented with both cocaine use<br />
and with levamisole use individually,<br />
normalization of ANCA and APL antibodies<br />
after levamisole exposure tended to take<br />
place within 2–14 months in Rongioletti’s<br />
study. [2] Given this patient’s history,<br />
repeat serologies at 6–12 months will<br />
be useful.<br />
References<br />
1. Gross RL, et al. A novel cutaneous<br />
vasculitis syndrome induced by levamisolecontaminated<br />
cocaine. ClinRheumatol 2011;<br />
30(10):1385.<br />
2. Rongioletti F, et al. Purpura of the ears: a<br />
distinctive vasculopathy with circulating<br />
autoantibodies complicating long-term<br />
treatment with levamisole in children. Br J<br />
Dermatol 1999;140:948–951.<br />
Author Disclosures<br />
Dr. Danielle Ramsden-Stein does not have<br />
a financial interest or relationship with the<br />
manufacturers of products or services.<br />
Dr. Sonali Narain does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.<br />
Dr. Michael D. Lockshin does not have a financial<br />
interest or relationship with the manufacturers<br />
of products or services.<br />
Figure 1: Extensive retiform purpuric lesions on<br />
patient’s bilateral lower extremities, Day 5.<br />
Figure 2: Saddle nose deformity. Resolving<br />
retiform purpura on cheeks.<br />
Figure 3: Skin biopsy shows a very distinctive<br />
intravascular occlusion without vasculitis primarily<br />
targeting capillaries and venules.
24<br />
Division of <strong>Rheumatology</strong><br />
<strong>HSS</strong> staff members, including Jillian Rose, LCSW, MPH, Director of Community Engagement, Diversity and<br />
Research (center), and Lillian Mendez, Program Associate, Charla de Lupus (Lupus Chat®) (second from right),<br />
with members of Charla de Lupus (Lupus Chat®) during the “Walk With Us to Cure Lupus” fundraiser, which<br />
benefits the Lupus Research Alliance.<br />
Empowering Patients Through<br />
Support and Education Programs<br />
At <strong>HSS</strong>, providing patient<br />
support and education is a key<br />
part of our mission to deliver<br />
the highest quality care. We<br />
offer a variety of services<br />
for patients with rheumatic<br />
diseases; in fact, we provide<br />
more support and education<br />
programs for lupus patients<br />
than any other hospital in the<br />
country. “Not only do we have<br />
the most programs, but we’ve<br />
been doing this the longest—for<br />
over 25 years,” says Stephen<br />
A. Paget, MD, Attending<br />
Physician and Physician-in-<br />
Chief Emeritus.<br />
<strong>HSS</strong> patients can learn more<br />
about their conditions in<br />
several different ways. Our<br />
physicians educate patients<br />
through Facebook Live events,<br />
video chats and in-person<br />
support group meetings.<br />
In addition, several of our<br />
Centers of Excellence offer<br />
webinars. Over the past year,<br />
the Inflammatory Arthritis<br />
Center of Excellence developed<br />
three educational webinars<br />
for patients in collaboration<br />
with the <strong>HSS</strong> Department of<br />
Social Work Programs, the <strong>HSS</strong><br />
Education Institute, the Arthritis<br />
Foundation and the Spondylitis<br />
Association of America. The<br />
Scleroderma, Vasculitis &<br />
Myositis Center of Excellence<br />
at <strong>HSS</strong> delivers a monthly email<br />
news blast to patients, and<br />
the <strong>HSS</strong> Division of Pediatric<br />
<strong>Rheumatology</strong> has developed<br />
patient education materials in<br />
multiple languages.<br />
Patient support and education<br />
programs are integral to the<br />
mission of the Department<br />
of Social Work Programs<br />
at <strong>HSS</strong>. “Our department<br />
partners with <strong>HSS</strong> physicians<br />
and healthcare teams to help<br />
support, empower and enhance<br />
the quality of life for people<br />
with rheumatologic conditions,”<br />
says Roberta Horton, LCSW,<br />
ACSW, Assistant Vice President,<br />
Department of Social Work<br />
Programs. <strong>HSS</strong> offers programs<br />
for patients with specific<br />
rheumatologic conditions,<br />
including the following:
Hospital for Special Surgery 25<br />
Lupus<br />
SLE Workshop<br />
This support and education program for lupus<br />
patients and their families and friends has been<br />
ongoing since 1985. Lupus care experts give<br />
lectures, which are followed by informal discussions.<br />
LANtern® (Lupus Asian Network)<br />
LANtern is the only national, hospital-based<br />
bilingual support and education program<br />
dedicated to serving Asian Americans with lupus<br />
and their families. Asians are more likely to develop<br />
lupus than Caucasian people, and their illness<br />
may be more severe. LANtern offers a bilingual,<br />
toll-free telephone support line of peer educators.<br />
These trained volunteers—either Asian Americans<br />
with lupus or Asian Americans who have family<br />
members with lupus—can help callers better<br />
understand their condition, address any concerns,<br />
and offer advice on how to work effectively with<br />
their physicians.<br />
Charla de Lupus (Lupus Chat®)<br />
This unique national program provides peer<br />
support and education to English- and Spanishspeaking<br />
people with lupus. It includes the Charla<br />
Line, a toll-free support and education helpline<br />
that screens and matches callers with peers.<br />
In addition, the program offers peer support at<br />
several rheumatology clinics in New York City.<br />
“Since 1988, we’ve trained lupus patients to<br />
provide specific support to families while they<br />
are sitting in the waiting room,” says Jillian Rose,<br />
LCSW, MPH, Director of Community Engagement,<br />
Diversity and Research. Program staff members<br />
conduct more than 30 community and professional<br />
presentations annually to raise awareness of lupus<br />
and provide access to educational resources.<br />
Additional programs offer support to teens and<br />
their parents.<br />
Rheumatoid Arthritis<br />
Living with Rheumatoid Arthritis provides<br />
monthly education and support for patients with<br />
moderate to severe rheumatoid arthritis (RA) and<br />
their families. RA care experts give lectures, which<br />
are followed by a discussion facilitated by a clinical<br />
social worker and rheumatology nurse.<br />
The Early RA Support and Education Program was<br />
developed for people who were recently diagnosed<br />
with RA. Participants meet for a free, four-session<br />
workshop series, which provides tips on how to<br />
communicate with their physician about RA and<br />
manage activities of daily living.<br />
Myositis<br />
<strong>HSS</strong> sponsors a Myositis Support Group, and meetings are generally held once a month at the<br />
Hospital. During the first hour, speakers such as myositis specialists, social workers and patients give<br />
presentations on topics as varied as managing your medical team, fatigue, and current research and<br />
treatments. During the second hour, members are able to share their thoughts and feelings about<br />
the illness.<br />
Scleroderma<br />
<strong>HSS</strong> hosts a monthly scleroderma support group sponsored by the Tri-State Chapter of the Scleroderma<br />
Foundation. In addition, the Scleroderma, Vasculitis & Myositis Center of Excellence hosts two<br />
Scleroderma Foundation patient forums every year.<br />
For more information on these programs, visit hss.edu/support-programs<br />
Using technology to assist lupus patients<br />
In <strong>2017</strong>, <strong>HSS</strong> launched LupusMinder, a mobile app designed to help lupus patients track medications,<br />
daily symptoms and appointments. Unlike other apps, this one was created with significant input from<br />
lupus patients themselves. The app enables users to take photos of their symptoms to share with their<br />
physician and chart daily symptoms, such as pain.
26<br />
Division of <strong>Rheumatology</strong><br />
<strong>Rheumatology</strong><br />
Leaders<br />
of the Future<br />
Bella Mehta, MBBS, MD<br />
Iris Navarro-Millán, MD, MSPH<br />
Medha Barbhaiya, MD, MPH<br />
<strong>Rheumatology</strong> has always attracted physicians who<br />
enjoy problem solving and managing some of the most<br />
complex cases in medicine. This is especially evident<br />
among the newest rheumatologists at <strong>HSS</strong>, who are<br />
committed to performing cutting-edge research and<br />
revolutionizing patient care. Here are their hopes for<br />
the future of the field.<br />
David R. Fernandez, MD, PhD
Hospital for Special Surgery 27<br />
Medha Barbhaiya, MD, MPH<br />
Medha Barbhaiya, MD, MPH, Assistant Attending Physician, is developing<br />
new classification criteria for APS and researching environmental risk<br />
factors for lupus.<br />
Medha Barbhaiya, MD, MPH,<br />
Assistant Attending Physician,<br />
is poised to become a leading<br />
researcher on lupus and<br />
Antiphospholipid Syndrome<br />
(APS). In 2015, Dr. Barbhaiya<br />
received the <strong>Rheumatology</strong><br />
Research Scientist Development<br />
Award to study environmental<br />
risk factors for lupus. “One of<br />
the biggest mysteries is why<br />
lupus seems to affect young,<br />
previously healthy patients,”<br />
she says. “Some patients may<br />
have an underlying genetic<br />
predisposition, but we hope<br />
to identify additional factors<br />
that contribute to their risk of<br />
developing lupus.” Dr. Barbhaiya<br />
studies lupus risk factors in<br />
over 230,000 participants in<br />
the Nurses’ Health Study and<br />
59,000 participants in the<br />
Black Women’s Health Study.<br />
She is examining the role of<br />
smoking, alcohol intake, diet<br />
(including the Mediterranean,<br />
Alternative Healthy Eating<br />
Index, and Inflammatory diets),<br />
UV light exposure, and even<br />
psychological factors, such<br />
as child abuse. In a study<br />
published in <strong>2018</strong> in Annals<br />
of the Rheumatic Diseases,<br />
Dr. Barbhaiya found that while<br />
cigarette smoking was not<br />
associated with a greater risk<br />
of developing lupus overall,<br />
it was for a subset of lupus<br />
patients who had a specific<br />
type of antibody known as antidouble<br />
stranded DNA (dsDNA).<br />
In another study published in<br />
August <strong>2018</strong> in Arthritis Care<br />
& Research, she demonstrated<br />
that while smoking slightly<br />
elevated the risk of developing<br />
lupus, moderate alcohol<br />
intake seemed protective. “In<br />
moderate amounts, alcohol<br />
may have an anti-inflammatory<br />
effect,” she says.<br />
In addition to her ongoing<br />
lupus-related research studies,<br />
Dr. Barbhaiya has been involved<br />
in APS research since medical<br />
school. She received a “Young<br />
Scholar” award from the APS<br />
Alliance for Clinical Trials<br />
and International Networking<br />
(APS ACTION) in 2014. In<br />
<strong>2018</strong>, she was the recipient<br />
of an Investigator Award from<br />
the <strong>Rheumatology</strong> Research<br />
Foundation to support her<br />
APS research. Currently, she<br />
is investigating risk factors<br />
for the development of<br />
thrombosis in APS in a spinoff<br />
study of an ACR/EULARsupported<br />
multidisciplinary<br />
effort to develop new APS<br />
classification criteria, for which<br />
she is one of the core planning<br />
group members. Studies of<br />
APS have been limited by<br />
small sample sizes, varying<br />
definitions of the disease,<br />
and laboratory tests that are<br />
not standardized. “There’s an<br />
urgent need for rigorous, highperforming<br />
APS classification<br />
criteria,” says Dr. Barbhaiya.<br />
As part of the classification<br />
criteria development efforts,<br />
Dr. Barbhaiya has been working<br />
with a large, international group<br />
of APS researchers, including<br />
other specialists, such as<br />
hematologists, pathologists and<br />
dermatologists. She plans to<br />
use international, multicenter<br />
patient data to investigate<br />
associations between potentially<br />
modifiable environmental<br />
factors and the risk of<br />
developing APS. Ultimately,<br />
she hopes that identifying risk<br />
factors will lead to improved<br />
prevention strategies.<br />
“For lupus and APS, there are so<br />
many unanswered questions,”<br />
says Dr. Barbhaiya. “Hopefully,<br />
I can help answer some of<br />
these questions and see the<br />
impact of my research on my<br />
patients’ care.” There is no<br />
better institution to support<br />
this work than <strong>HSS</strong>, since<br />
the Hospital takes a multidisciplinary<br />
approach to lupus<br />
and APS, says Dr. Barbhaiya.<br />
“There’s a lot of camaraderie<br />
and synergy between clinicians<br />
and researchers,” she says.<br />
“There’s also a tremendous<br />
amount of support for junior<br />
faculty. We are given time to<br />
perform research while serving<br />
as clinicians.”
28<br />
Division of <strong>Rheumatology</strong><br />
David R. Fernandez, MD, PhD<br />
David R. Fernandez, MD, PhD, Assistant Attending Physician, aims to study the molecular mechanisms that<br />
drive myositis to develop better treatments.<br />
David R. Fernandez, MD, PhD,<br />
Assistant Attending Physician,<br />
has dedicated his career to<br />
researching and caring for<br />
patients with myositis. While he<br />
has successfully treated many,<br />
he’s haunted by thoughts of<br />
those who haven’t responded to<br />
treatment. “This provides strong<br />
motivation to try to help patients<br />
further,” says Dr. Fernandez,<br />
who is researching the causes<br />
and treatment of myositis.<br />
“Uncommon disorders like these<br />
could use more support, and<br />
<strong>HSS</strong> is in a great position to<br />
provide that.”<br />
Dr. Fernandez is creating a<br />
registry of myositis patients to<br />
study the natural history of the<br />
disease. “At <strong>HSS</strong>, we see a high<br />
volume of patients, which helps<br />
to inform research and move the<br />
field forward,” he says. Currently,<br />
Dr. Fernandez is collecting blood<br />
samples to determine whether<br />
T cells and B cells in myositis<br />
patients have some of the<br />
same abnormalities commonly<br />
found in lupus patients. “There<br />
are a lot of clinical similarities<br />
between the two diseases, so<br />
we’re hoping we may be able<br />
to confirm that on a molecular<br />
level,” he explains. Dr. Fernandez<br />
is also participating in a clinical<br />
trial focusing on the effects<br />
of the lupus drug belimumab<br />
to treat dermatomyositis and<br />
polymyositis. He is studying the<br />
protein mTOR, which is altered<br />
in people with lupus. “One recent<br />
clinical trial found that a drug<br />
that targeted mTOR showed<br />
some benefit in lupus patients,<br />
so we’d like to see if this protein<br />
is also affected in myositis,<br />
which may indicate similar<br />
therapies might help some of our<br />
myositis patients,” he explains.<br />
Dr. Fernandez is the physician<br />
advisor to the <strong>HSS</strong> Myositis<br />
Support and Education Program.<br />
He attends support group<br />
meetings and speaks to patients<br />
about the latest advances in<br />
treatment and research. “I spend<br />
80 percent of my time doing<br />
research, but the 20 percent<br />
of time spent with patients is<br />
invaluable,” he says. “It reminds<br />
me of the acuity of these<br />
illnesses and how important it<br />
is to move the field forward. It<br />
also benefits me as a researcher<br />
because it helps me understand<br />
how much these diseases can<br />
vary from person to person.”<br />
Ultimately, Dr. Fernandez<br />
hopes to run his own myositis<br />
laboratory at <strong>HSS</strong>, which would<br />
allow him to study the molecular<br />
mechanisms that drive the<br />
disease. “I have many colleagues<br />
with expertise in different<br />
diseases,” he says. “If I’m having<br />
trouble with a case history or<br />
designing a study protocol,<br />
they’re just down the hall. I can’t<br />
imagine a better environment to<br />
do research and treat patients.”
Hospital for Special Surgery 29<br />
Bella Mehta, MBBS, MD<br />
Bella Mehta, MBBS, MD,<br />
Assistant Attending Physician,<br />
became interested in the<br />
field of rheumatology when<br />
she came to <strong>HSS</strong> in 2010 as<br />
a visiting medical student<br />
from India. One of her first<br />
cases involved diagnosing a<br />
patient who had suffered from<br />
persistent, unexplained fevers<br />
for many years. It took multiple<br />
specialists to come up with a<br />
diagnosis: adult-onset Still’s<br />
disease, a rare autoimmune<br />
disorder. “<strong>Rheumatology</strong> cases<br />
are never straightforward<br />
and simple,” says Dr. Mehta.<br />
“There’s something very<br />
satisfying about making the<br />
right diagnosis.”<br />
Today, Dr. Mehta is putting her<br />
sleuthing skills to good use,<br />
analyzing <strong>HSS</strong> registries and large<br />
data sets to address important<br />
questions about healthcare<br />
disparities and outcomes for<br />
patients with arthritis. Using<br />
geospatial epidemiology, she<br />
and several colleagues, including<br />
Susan M. Goodman, MD, Director<br />
of the Integrative <strong>Rheumatology</strong><br />
and Orthopedic Center of<br />
Excellence and Attending<br />
Physician, investigated how<br />
neighborhood characteristics—<br />
specifically the proportion<br />
of impoverished people and<br />
immigrants—influence outcomes<br />
after joint replacement surgery at<br />
<strong>HSS</strong>. “Geospatial epidemiology is<br />
usually thought of as a marketing<br />
tool (businesses use it in different<br />
neighborhoods to figure out what<br />
types of food residents eat),<br />
but it can help us understand<br />
how where a person lives affects<br />
health outcomes.”<br />
While pain and function scores<br />
after total hip replacement<br />
were similar for blacks<br />
and whites in middle-class<br />
or affluent communities,<br />
Bella Mehta, MBBS, MD, Assistant Attending Physician, is investigating<br />
disparities in healthcare among arthritis patients.<br />
Dr. Mehta found that blacks<br />
in poorer neighborhoods<br />
fared significantly worse than<br />
their white counterparts. In<br />
other research, Dr. Mehta<br />
discovered that education can<br />
help mitigate the effects of<br />
these outcomes. “In poorer<br />
communities, those who have<br />
some college education have<br />
significantly better pain and<br />
function scores than those who<br />
don’t,” she says. These findings<br />
suggest that patients without<br />
a college education who live in<br />
economically disadvantaged<br />
neighborhoods should be<br />
targeted for preoperative and<br />
postoperative interventions,<br />
including being encouraged<br />
to have procedures like joint<br />
replacement earlier to achieve<br />
better outcomes.<br />
In <strong>2017</strong>, Dr. Mehta’s work on<br />
epidemiology and rheumatology<br />
outcomes was selected as one<br />
of the top three research studies<br />
at the American College of<br />
<strong>Rheumatology</strong> annual meeting.<br />
Dr. Mehta’s goal is to decrease<br />
disparities, reduce disability and<br />
improve outcomes in arthritis<br />
patients. “It’s a different level<br />
of disparity than what I was<br />
used to in India, where many<br />
impoverished people simply go<br />
without health care because<br />
resources such as Medicare aren’t<br />
available,” she says. “In the U.S.,<br />
even if someone has Medicare<br />
or Medicaid, they still might not<br />
have surgery or see their primary<br />
care physician. The question<br />
becomes, what other factors are<br />
holding people back, and why?”<br />
Dr. Mehta is confident she will be<br />
able to answer these questions at<br />
<strong>HSS</strong>. “The intellectual stimulation<br />
here is so energizing,” she says.<br />
“We have some of the greatest<br />
minds in medicine here.”
30<br />
Division of <strong>Rheumatology</strong><br />
Iris Navarro-Millán, MD, MSPH<br />
Iris Navarro-Millán, MD, MSPH, Assistant Attending Physician, is<br />
studying the prevalence and incidence of cardiovascular risk factors<br />
among patients with psoriatic and rheumatoid arthritis.<br />
For more than half a century,<br />
research has shown that<br />
rheumatoid arthritis (RA)<br />
raises the risk of developing<br />
cardiovascular disease (CVD).<br />
Despite this, many physicians<br />
and patients are unaware of<br />
the connection: One recent<br />
study found that about half of<br />
all patients with RA and their<br />
primary care providers were<br />
unaware of the link and were<br />
not taking steps to implement<br />
preventive care. Iris Navarro-<br />
Millán, MD, MSPH, Assistant<br />
Attending Physician, is<br />
attempting to close that gap.<br />
Over the last few years, she has<br />
been studying the prevalence<br />
and incidence of cardiovascular<br />
risk factors—high blood<br />
pressure, elevated cholesterol<br />
levels, obesity and Type 2<br />
diabetes—among patients<br />
with psoriatic and rheumatoid<br />
arthritis. She published a study<br />
in Annals of the Rheumatic<br />
Diseases highlighting the<br />
association of high levels of<br />
inflammatory markers, such as<br />
C-reactive protein (CRP) and<br />
erythrocyte sedimentation rate<br />
(ESR), with an increased risk of<br />
heart attack and stroke among<br />
veterans with RA. “Our research<br />
shows that this inflammation<br />
is driving the increase in<br />
cardiovascular disease among<br />
people with rheumatoid<br />
arthritis,” she explains.<br />
Managing cardiovascular<br />
risk factors in RA patients<br />
is key, yet a study published<br />
by Dr. Navarro-Millán in the<br />
Journal of International Medical<br />
Research in <strong>2018</strong> found that<br />
patients with inflammatory<br />
arthritis (rheumatoid arthritis,<br />
psoriatic arthritis and ankylosing<br />
spondylitis) were no more<br />
likely to be treated for high<br />
cholesterol than people without<br />
any cardiovascular risk factors.<br />
In her most recent study, she<br />
found that only 37 percent of<br />
patients with RA are screened<br />
for hyperlipidemia. This article<br />
was published in November <strong>2018</strong><br />
in Arthritis Care and Research,<br />
and it was highlighted as one<br />
of the must-read articles for<br />
the first week of December by<br />
<strong>Rheumatology</strong> News Clinical<br />
Edge. As a result, Dr. Navarro-<br />
Millán is currently developing<br />
an intervention to address the<br />
gaps in patient care. “We’re<br />
focusing mainly on improving<br />
screening and management<br />
of hyperlipidemia among<br />
patients with RA,” she says.<br />
“We’re developing a series of<br />
brief videos for patients that<br />
explain the short- and long-term<br />
effects of RA and medications.<br />
The videos will also cover the<br />
importance of screening and<br />
management of cholesterol<br />
levels as a way of decreasing<br />
their risk of complications.” The<br />
videos will be available online<br />
for patients to watch on their<br />
own, but they can also receive<br />
the assistance of a peer coach<br />
to guide them. Peer coaches<br />
are individuals who have RA<br />
and have received training to<br />
provide guidance regarding the<br />
video content and support. “We<br />
do not anticipate that everyone<br />
with RA will need a peer coach,<br />
but this option will be available<br />
for those individuals who have<br />
limited experience navigating<br />
the healthcare system and may<br />
need guidance and support to<br />
understand the importance of<br />
CVD risk as part of having RA,”<br />
says Dr. Navarro-Millán. “We<br />
aim to make these resources<br />
accessible to everyone in<br />
this country.”<br />
Dr. Navarro-Millán is confident<br />
that the community of physicianresearchers<br />
at <strong>HSS</strong> will help her<br />
achieve her goal of improving<br />
the care of RA patients. “Having<br />
such a diverse cadre of clinicians<br />
to collaborate with and to help<br />
me generate questions I can<br />
develop into meaningful clinical<br />
research studies is, for me, the<br />
biggest asset of working at <strong>HSS</strong>,”<br />
she says.
Hospital for Special Surgery 31<br />
Notable References<br />
Ah Kioon MD, Tripodo C, Fernandez D, Kirou KA, Spiera RF,<br />
Crow MK, Gordon JK, Barrat FJ. Plasmacytoid dendritic<br />
cells promote systemic sclerosis with a key role for TLR8.<br />
Sci Med. <strong>2018</strong> Jan 10;10(423).<br />
Bass AR, Fields KG, Goto R, Turissini G, Dey S, Russell<br />
LA. Clinical Decision Rules for Pulmonary Embolism<br />
in Hospitalized Patients: A Systematic Literature<br />
Review and Meta-analysis. Thromb Haemost. <strong>2017</strong><br />
Nov;117(11):2176–2185.<br />
Brunner HI, Rider LG, Kingsbury DJ, Co D, Schneider R,<br />
Goldmuntz E, Onel KB, Giannini EH, Lovell DJ; PRCSG<br />
Advisory Council. Pediatric <strong>Rheumatology</strong> Collaborative<br />
Study Group—over four decades of pivotal clinical drug<br />
research in pediatric rheumatology. Pediatr Rheumatol<br />
Online J. <strong>2018</strong> Jul 11;16(1):45.<br />
Chan K, Bass AR. Checkpoint inhibitor-induced<br />
polymyalgia rheumatica controlled by cobimetinib, a<br />
MEK 1/2 inhibitor. Annals of the Rheumatic Diseases.<br />
May <strong>2018</strong>, annrheumdis-<strong>2018</strong>-213672; doi: 10.1136/<br />
annrheumdis-<strong>2018</strong>-213672.<br />
Donlin LT, Rao DA, Wei K, Slowikowski K, McGeachy MJ,<br />
Turner JD, Meednu N, Mizoguchi F, Gutierrez-Arcelus M,<br />
Lieb DJ, Keegan J, Muskat K, Hillman J, Rozo C, Ricker<br />
E, Eisenhaure TM, Li S, Browne EP, Chicoine A, Sutherby<br />
D, Noma A; Accelerating Medicines Partnership RA/<br />
SLE Network, Nusbaum C, Kelly S, Pernis AB, Ivashkiv<br />
LB, Goodman SM, Robinson WH, Utz PJ, Lederer JA,<br />
Gravallese EM, Boyce BF, Hacohen N, Pitzalis C, Gregersen<br />
PK, Firestein GS, Raychaudhuri S, Moreland LW, Holers<br />
VM, Bykerk VP, Filer A, Boyle DL, Brenner MB, Anolik JH.<br />
Methods for high-dimensional analysis of cells dissociated<br />
from cyropreserved synovial tissue. Arthritis Res Ther.<br />
<strong>2018</strong> Jul 11;20(1):139.<br />
Fields TR, Batterman A. How Can We Improve Disease<br />
Education in People with Gout? Curr Rheumatol Rep. <strong>2018</strong><br />
Mar 8;20(3):12.<br />
Fu MC, Boddapati V, Gausden EB, Samuel AM, Russell LA,<br />
Lane JM. Surgery for a fracture of the hip within 24 hours<br />
of admission is independently associated with reduced<br />
short-term post-operative complications. Bone Joint J.<br />
<strong>2017</strong> Sep;99-B(9):1216–1222.<br />
Gage BF, Bass AR, Lin H, Woller SC, Stevens SM, Al-<br />
Hammadi N, Li J, Rodríguez T Jr, Miller JP, McMillin<br />
GA, Pendleton RC, Jaffer AK, King CR, Whipple BD,<br />
Porche-Sorbet R, Napoli L, Merritt K, Thompson AM,<br />
Hyun G, Anderson JL, Hollomon W, Barrack RL, Nunley<br />
RM, Moskowitz G, Dávila-Román V, Eby CS. Effect of<br />
Genotype-Guided Warfarin Dosing on Clinical Events and<br />
Anticoagulation Control Among Patients Undergoing Hip<br />
or Knee Arthroplasty: The GIFT Randomized Clinical Trial.<br />
JAMA. <strong>2017</strong> Sep 26;318(12):1115–1124.<br />
Garcia D, Erkan D. Diagnosis and Management of the<br />
Antiphospholipid Syndrome. N Engl J Med. <strong>2018</strong> May<br />
24;378(21):2010–2021.<br />
Goodman SM, Bykerk VP, DiCarlo E, Cummings RW, Donlin<br />
LT, Orange DE, Hoang A, Mirza S, McNamara M, Andersen<br />
K, Bartlett SJ, Szymonifka J, Figgie MP. Flares in Patients<br />
with Rheumatoid Arthritis after Total Hip and Total Knee<br />
Arthroplasty: Rates, Characteristics, and Risk Factors.<br />
J Rheumatol. <strong>2018</strong> May;45(5):604–611.<br />
Goodman SM, Mandl LA, Mehta B, Navarro-Millán I, Russell<br />
LA, Parks ML, Dey SA, Crego D, Figgie MP, Nguyen JT,<br />
Szymonifka J, Zhang M, Bass AR. Does Education Level<br />
Mitigate the Effect of Poverty on Total Knee Arthroplasty<br />
Outcomes? Arthritis Care Res (Hoboken). <strong>2018</strong><br />
Jun;70(6):884–891.<br />
Goodman SM, Springer B, Guyatt G, Abdel MP, Dasa V,<br />
George M, Gewurz-Singer O, Giles JT, Johnson B, Lee<br />
S, Mandl LA, Mont MA, Sculco P, Sporer S, Stryker L,<br />
Turgunbaev M, Brause B, Chen AF, Gililland J, Goodman<br />
M, Hurley-Rosenblatt A, Kirou K, Losina E, MacKenzie R,<br />
Michaud K, Mikuls T, Russell L, Sah A, Miller AS, Singh<br />
JA, Yates A. <strong>2017</strong> American College of <strong>Rheumatology</strong>/<br />
American Association of Hip and Knee Surgeons Guideline<br />
for the Perioperative Management of Antirheumatic<br />
Medication in Patients With Rheumatic Diseases<br />
Undergoing Elective Total Hip or Total Knee Arthroplasty.<br />
J Arthroplasty. <strong>2017</strong> Sep;32(9):2628–2638.<br />
Gordon JK, Martyanov V, Franks JM, Bernstein EJ,<br />
Szymonifka J, Magro C, Wildman HF, Wood TA, Whitfield<br />
ML, Spiera RF. Belimumab for the Treatment of Early<br />
Diffuse Systemic Sclerosis: Results of a Randomized,<br />
Double-Blind, Placebo-Controlled, Pilot Trial. Arthritis<br />
Rheumatol. <strong>2018</strong> Feb;70(2):308–316.<br />
Horton DB, Onel KB, Beukelman T, Ringold S. Attitudes<br />
and Approaches for Withdrawing Drugs for Children<br />
with Clinically Inactive Nonsystemic JIA: A Survey of the<br />
Childhood Arthritis and <strong>Rheumatology</strong> Research Alliance.<br />
J Rheumatol. <strong>2017</strong> Mar;44(3):352–360.<br />
Kim MY, Guerra MM, Kaplowitz E, Laskin CA, Petri M,<br />
Branch DW, Lockshin MD, Sammaritano LR, Merrill JT,<br />
Porter TF, Sawitzke A, Lynch AM, Buyon JP, Salmon JE.<br />
Complement activation predicts adverse pregnancy<br />
outcome in patients with systemic lupus erythematosus<br />
and/or antiphospholipid antibodies. Ann Rheum Dis. <strong>2018</strong><br />
Apr;77(4):549-555.<br />
Lafyatis R, Mantero JC, Gordon J, Kishore N, Carns M,<br />
Dittrich H, Spiera R, Simms RW, Varga J. Inhibition of<br />
β-Catenin Signaling in the Skin Rescues Cutaneous<br />
Adipogenesis in Systemic Sclerosis: A Randomized,<br />
Double-Blind, Placebo-Controlled Trial of C-82. J Invest<br />
Dermatol. <strong>2017</strong> Dec;137(12):2473–2483.<br />
Liu Y, Carrino JA, Dash AS, Chukir T, Do H, Bockman RS,<br />
Hughes AP, Press JM, Stein EM. Lower spine volumetric<br />
bone density in patients with a history of epidural steroid<br />
injections. J Clin Endocrinol Metab. <strong>2018</strong> Jul 2. doi:<br />
10.1210/jc.<strong>2018</strong>-00558.
32<br />
Division of <strong>Rheumatology</strong><br />
Liu Y, Dimango E, Bucovsky M, Agarwal S, Nishiyama K,<br />
Guo XE, Shane E, Stein EM. Abnormal microarchitecture<br />
and stiffness in postmenopausal women using chronic<br />
inhaled glucocorticoids. Osteoporos Int. <strong>2018</strong> Jun 11. doi:<br />
10.1007/s00198-018-4591–9.<br />
Manni M, Gupta S, Ricker E, Chinenov Y, Park SH, Shi<br />
M, Pannellini T, Jessberger R, Ivashkiv LB, Pernis AB.<br />
Regulation of age-associated B cells by IRF5 in systemic<br />
autoimmunity. Nat Immunol. <strong>2018</strong> Apr;19(4):407–419.<br />
Marangoni RG, Lu TT. The roles of dermal white adipose<br />
tissue loss in scleroderma skin fibrosis. Curr Opin<br />
Rheumatol. <strong>2017</strong> Nov;29(6):585–590.<br />
Mavragani CP, Nezos A, Sagalovskiy I, Seshan S, Kirou<br />
KA, Crow MK. Defective regulation of L1 endogenous<br />
retroelements in primary Sjogren’s syndrome and systemic<br />
lupus erythematosus: Role of methylating enzymes.<br />
J Autoimmun. <strong>2018</strong> Mar;88:75–82.<br />
Mehta BY, Bass AR, Goto R, Russell LA, Parks ML, Figgie<br />
MP, Goodman SM. Disparities in Outcomes for Blacks<br />
versus Whites Undergoing Total Hip Arthroplasty:<br />
A Systematic Literature Review. J Rheumatol. <strong>2018</strong><br />
May;45(5):717–722.<br />
Navarro-Millán I, Zinski A, Shurbaji S, Johnson B,<br />
Fraenkel L, Willig J, Danila MI, Yun H, Curtis JR, Safford<br />
MM. Perspectives of Rheumatoid Arthritis Patients on<br />
Electronic Communication and Patient <strong>Report</strong>ed Outcome<br />
Data Collection: A Qualitative Study. Arthritis Care Res<br />
(Hoboken). <strong>2018</strong> Apr 18. doi: 10.1002/acr.23580.<br />
Orange DE, Agius P, DiCarlo EF, Robine N, Geiger H,<br />
Szymonifka J, McNamara M, Cummings R, Andersen KM,<br />
Mirza S, Figgie M, Ivashkiv LB, Pernis AB, Jiang CS, Frank<br />
MO, Darnell RB, Lingampali N, Robinson WH, Gravallese<br />
E; Accelerating Medicines Partnership in Rheumatoid<br />
Arthritis and Lupus Network, Bykerk VP, Goodman SM,<br />
Donlin LT. Identification of Three Rheumatoid Arthritis<br />
Disease Subtypes by Machine Learning Integration of<br />
Synovial Histologic Features and RNA Sequencing Data.<br />
Arthritis Rheumatol. <strong>2018</strong> May;70(5):690–701.<br />
Park SH, Kang K, Giannopoulou E, Qiao Y, Kang K, Kim<br />
G, Park-Min KH, Ivashkiv LB. Type I interferons and the<br />
cytokine TNF cooperatively reprogram the macrophage<br />
epigenome to promote inflammatory activation. Nat<br />
Immunol. <strong>2017</strong> Oct;18(10):1104–1116.<br />
Park-Min KH. Mechanisms involved in normal and<br />
pathological osteoclastogenesis. Cell Mol Life Sci. <strong>2018</strong><br />
Jul;75(14):2519–2528.<br />
Qing X, Chinenov Y, Redecha P, Madaio M, Roelofs JJ,<br />
Farber G, Issuree PD, Donlin L, Mcllwain DR, Mak TW,<br />
Blobel CP, Salmon JE. iRhom2 promotes lupus nephritis<br />
through TNF-α and EGFR signaling. J Clin Invest. <strong>2018</strong><br />
Apr 2;128(4):1397–1412.<br />
Russell LA, Sigmund AE, Szymonifka J, Jawetz ST, Grond<br />
SE, Dey SA, Bass AR. Does my patient have a pulmonary<br />
embolism? The Wells vs. PISA 2 rule in orthopedic patients.<br />
J Thromb Thrombolysis. <strong>2018</strong> Apr;45(3):417–422.<br />
Schulman E, Bartlett SJ, Schieir O, Andersen KM,<br />
Boire G, Pope JE, Hitchon C, Jamal S, Thorne JC, Tin D,<br />
Keystone EC, Haraoui B, Goodman SM, Bykerk VP; CATCH<br />
Investigators. Overweight, Obesity, and the Likelihood<br />
of Achieving Sustained Remission in Early Rheumatoid<br />
Arthritis: Results From a Multicenter Prospective Cohort<br />
Study. Arthritis Care Res (Hoboken). <strong>2017</strong> Nov 30. doi:<br />
10.1002/acr.23457.<br />
Shipman WD, Chyou S, Ramanathan A, Izmirly PM, Sharma<br />
S, Pannellini T, Dasoveanu DC, Qing X, Magro CM, Granstein<br />
RD, Lowes MA, Pamer EG, Kaplan DH, Salmon JE, Mehrara<br />
BJ, Young JW, Clancy RM, Blobel CP, Lu TT. A prospective<br />
Langerhans cell-keratinocyte axis that is dysfunctional in<br />
photosensitivity. Sci Transl Med. <strong>2018</strong> Aug 15;10(454).<br />
Smith MH, Bass AR. Arthritis after cancer immunotherapy:<br />
symptom duration and treatment response. Arthritis Care<br />
Res (Hoboken). <strong>2017</strong> Nov 10.<br />
Stephenson W, Donlin LT, Butler A, Rozo C, Bracken B,<br />
Rashidfarrokhi A, Goodman SM, Ivashkiv LB, Bykerk VP,<br />
Orange DE, Darnell RB, Swerdlow HP, Satija R. Single-cell<br />
RNA-seq of rheumatoid arthritis synovial tissue using lowcost<br />
microfluidic instrumentation. Nat Commun. <strong>2018</strong> Feb<br />
23;9(1):791.<br />
Stone JH, Tuckwell K, Dimonaco S, Klearman M, Aringer<br />
M, Blockmans D, Brouwer E, Cid MC, Bhaskar D, Rech J,<br />
Salvarani C, Schett G, Schulze-Koops H, Spiera R, Unizony<br />
SH, Collinson N. Trial of Tocilizumab in Giant-Cell Arteritis.<br />
N Engl J Med. <strong>2017</strong>;377(4):317–328.<br />
Wei W, Knapp K, Wang L, Chen CI, Craig GL, Ferguson<br />
K, Schwartzman S. Treatment Persistence and Clinical<br />
Outcomes of Tumor Necrosis Factor Inhibitor Cycling<br />
or Switching to a New Mechanism of Action Therapy:<br />
Real-world Observational Study of Rheumatoid<br />
Arthritis Patients in the United States with Prior Tumor<br />
Necrosis Factor Inhibitor Therapy. Adv Ther. <strong>2017</strong><br />
Aug;34(8):1936–1952.<br />
Yi W, Gupta S, Ricker E, Manni M, Jessberger R, Chinenov<br />
Y, Molina H, Pernis AB. The mTORC1-4E-BP-eIF4E<br />
axis controls de novo Bcl6 protein synthesis in T cells<br />
and systemic autoimmunity. Nat Commun. <strong>2017</strong> Aug<br />
15;8(1):254.<br />
Zhao Y, Wu EY, Oliver MS, Cooper AM, Basiaga ML, Vora SS,<br />
Lee TC, Fox E, Amarilyo G, Stern SM, Dvergsten JA, Haines<br />
KA, Rouster-Stevens KA, Onel KB, Cherian J, Hausmann<br />
JS, Miettunen P, Cellucci T, Nuruzzaman F, Taneja A, Barron<br />
KS, Hollander MC, Lapidus SK, Li SC, Ozen S, Girschick H,<br />
Laxer RM, Dedeoglu F, Hedrich CM, Ferguson PJ; Chronic<br />
Nonbacterial Osteomyelitis/Chronic Recurrent Multifocal<br />
Osteomyelitis Study Group and the Childhood Arthritis and<br />
<strong>Rheumatology</strong> Research Alliance Scleroderma, Vasculitis,<br />
Autoinflammatory and Rare Diseases Subcommittee.<br />
Consensus Treatment Plans for Chronic Nonbacterial<br />
Osteomyelitis Refractory to Nonsteroidal Antiinflammatory<br />
Drugs and/or With Active Spinal Lesions. Arthritis Care Res<br />
(Hoboken). <strong>2017</strong> Nov 7. doi: 10.1002/acr.23462
About Hospital for Special Surgery<br />
Founded in 1863, Hospital for Special Surgery (<strong>HSS</strong>) is a world leader in orthopaedics, rheumatology and rehabilitation.<br />
<strong>HSS</strong> is ranked #1 in the U.S. for Orthopaedics and #3 for <strong>Rheumatology</strong> by U.S. News & World <strong>Report</strong> “Best Hospitals”<br />
(<strong>2018</strong>–2019 rankings). It is also ranked Best in New York City for Pediatric Orthopaedics and #21 nationally by U.S.<br />
News & World <strong>Report</strong> “Best Hospitals” (<strong>2018</strong>–2019 rankings). It is the first hospital in New York State to receive the<br />
Magnet® designation for Excellence in Nursing Service from the American Nurses Credentialing Center four consecutive<br />
times. Located in New York City, <strong>HSS</strong> also serves patients in the regional area with outpatient centers in Westchester<br />
County, New York; Connecticut; New Jersey; Long Island and Queens. In 2019, there will be a new <strong>HSS</strong> location in West<br />
Palm Beach, FL. Patients choose to come to <strong>HSS</strong> from across the U.S. and from around the world. <strong>HSS</strong> has one of the<br />
lowest infection rates in the country. The Hospital’s Research Institute is internationally recognized as a leader in the<br />
investigation of musculoskeletal and autoimmune diseases. To learn more, please visit hss.edu.<br />
Attributions<br />
The <strong>HSS</strong> Division of <strong>Rheumatology</strong> <strong>Annual</strong> <strong>Report</strong> is published by the Communications Department, Hospital for Special<br />
Surgery, 535 East 70th Street, New York, NY 10021. 866-976-1196<br />
Hospital for Special Surgery is an affiliate of Weill Cornell Medical College.<br />
©<strong>2018</strong> Hospital for Special Surgery. All rights reserved.<br />
Officers<br />
Co-Chairs<br />
Thomas Lister<br />
Robert K. Steel<br />
Vice Chair<br />
Michael Esposito<br />
President and<br />
Chief Executive Officer<br />
Louis A. Shapiro<br />
Surgeon-In-Chief and<br />
Medical Director<br />
Todd J. Albert, MD<br />
Executive Vice President and<br />
Chief Operating Officer<br />
Lisa A. Goldstein<br />
Executive Vice President and<br />
Chief Financial Officer<br />
Stacey L. Malakoff<br />
Executive Vice President,<br />
Chief Legal Officer and Secretary<br />
Irene Koch, Esq.<br />
Chairmen Emeriti<br />
Winfield P. Jones<br />
Richard L. Menschel<br />
Aldo Papone<br />
Kendrick R. Wilson III<br />
Credits<br />
Executive Editorial Board<br />
Todd Albert, MD<br />
Mary K. Crow, MD<br />
John Englehart<br />
Lionel Ivashkiv, MD<br />
Louis A. Shapiro<br />
Executive Editor<br />
Rachel Sheehan, MA, MBA<br />
Editor-in-Chief<br />
Deborah Pike Olsen<br />
Writers<br />
Stacey Colino<br />
Beth Howard<br />
Hallie Levine<br />
Design<br />
Suka Creative<br />
Photo Editor<br />
Deborah Garcia<br />
Printing<br />
Earth Color<br />
Photography<br />
John Abbott<br />
Robert Essel
HOSPITAL FOR SPECIAL SURGERY<br />
535 East 70th Street<br />
New York, NY 10021<br />
212-606-1000<br />
hss.edu