New Staff - Children's Hospital Boston
New Staff - Children's Hospital Boston
New Staff - Children's Hospital Boston
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Shoulder Dislocations<br />
Donald S. Bae, MD<br />
Kickoff<br />
The air has turned cooler, snow is starting to fall, and the <strong>New</strong><br />
England Patriots and <strong>Boston</strong> Celtics are back to their winning<br />
ways…all sure signs that winter is here. With the change in seasons,<br />
many children and adolescents are looking forward to the<br />
return of winter sports. Sports participation continues to rise<br />
both regionally and nationally. It is estimated that over 35 million<br />
children and adolescents participate in organized sports, and the<br />
majority of households will have at least one child participating<br />
in athletic activities.<br />
As sports participation continues to<br />
rise, particularly in younger<br />
children and adolescents at<br />
higher levels of competition,<br />
so too has our awareness<br />
of sports related injuries,<br />
including shoulder<br />
dislocations.<br />
More Than Just a Ball<br />
and Socket<br />
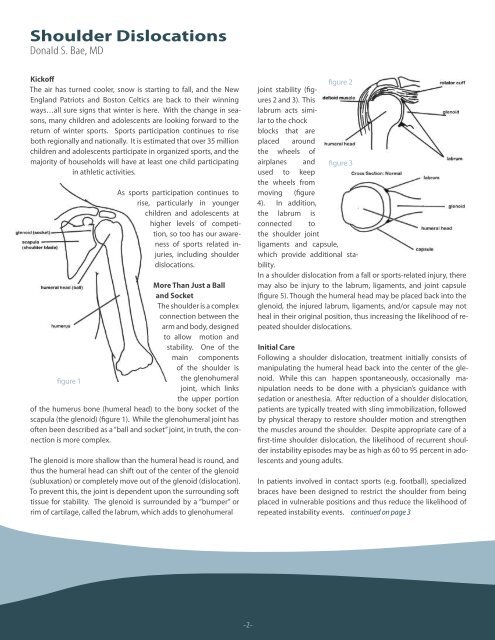
The shoulder is a complex<br />
connection between the<br />
arm and body, designed<br />
to allow motion and<br />
stability. One of the<br />
main components<br />
of the shoulder is<br />
figure 1<br />
the glenohumeral<br />
joint, which links<br />
the upper portion<br />
of the humerus bone (humeral head) to the bony socket of the<br />
scapula (the glenoid) (figure 1). While the glenohumeral joint has<br />
often been described as a “ball and socket” joint, in truth, the connection<br />
is more complex.<br />
The glenoid is more shallow than the humeral head is round, and<br />
thus the humeral head can shift out of the center of the glenoid<br />
(subluxation) or completely move out of the glenoid (dislocation).<br />
To prevent this, the joint is dependent upon the surrounding soft<br />
tissue for stability. The glenoid is surrounded by a “bumper” or<br />
rim of cartilage, called the labrum, which adds to glenohumeral<br />
figure 2<br />
joint stability (figures<br />
2 and 3). This<br />
labrum acts similar<br />
to the chock<br />
blocks that are<br />
placed around<br />
the wheels of<br />
airplanes and figure 3<br />
used to keep<br />
the wheels from<br />
moving (figure<br />
4). In addition,<br />
the labrum is<br />
connected to<br />
the shoulder joint<br />
ligaments and capsule,<br />
which provide additional stability.<br />
In a shoulder dislocation from a fall or sports-related injury, there<br />
may also be injury to the labrum, ligaments, and joint capsule<br />
(figure 5). Though the humeral head may be placed back into the<br />
glenoid, the injured labrum, ligaments, and/or capsule may not<br />
heal in their original position, thus increasing the likelihood of repeated<br />
shoulder dislocations.<br />
Initial Care<br />
Following a shoulder dislocation, treatment initially consists of<br />
manipulating the humeral head back into the center of the glenoid.<br />
While this can happen spontaneously, occasionally manipulation<br />
needs to be done with a physician’s guidance with<br />
sedation or anesthesia. After reduction of a shoulder dislocation,<br />
patients are typically treated with sling immobilization, followed<br />
by physical therapy to restore shoulder motion and strengthen<br />
the muscles around the shoulder. Despite appropriate care of a<br />
first-time shoulder dislocation, the likelihood of recurrent shoulder<br />
instability episodes may be as high as 60 to 95 percent in adolescents<br />
and young adults.<br />
In patients involved in contact sports (e.g. football), specialized<br />
braces have been designed to restrict the shoulder from being<br />
placed in vulnerable positions and thus reduce the likelihood of<br />
repeated instability events. continued on page 3<br />
Welcome <strong>New</strong> <strong>Staff</strong><br />
Virginia Brunelle<br />
The Department of Orthopaedic Surgery is<br />
pleased to announce that Kimberly Bayliss, RN<br />
and Erin Dawicki PA-C, have joined our clinical<br />
support team.<br />
The Orthopaedic clinical support team includes,<br />
nurses, nurse practitioners, and physician assistants.<br />
Each member of the clinical support<br />
team contributes a fundamental role in providing<br />
care to our patients and families with integrity,<br />
compassion, and expertise.<br />
Kimberly Bayliss, RN<br />
Kimberly attended Northeastern University,<br />
where she received a Bachelor of Science in<br />
Shoulder Dislocations,<br />
continued from page 2<br />
These braces may be used to allow athletes<br />
to return to sports participation for<br />
the remainder of their season or indefinitely.<br />
Surgical Treatment<br />
In patients with recurrent shoulder dislocations<br />
that do not improve with physical<br />
therapy and activity modification, surgical<br />
treatment is an option. Ultimately the<br />
decision to pursue surgery is made by<br />
the patient/parents and treating orthopaedic<br />
surgeon after careful evaluation<br />
and discussion.<br />
Surgery for shoulder instability is designed<br />
to repair and/or tighten the<br />
labrum, ligaments, and joint capsule<br />
around the shoulder. In most situations,<br />
this may be performed using arthroscopy.<br />
Small incisions are made around the<br />
shoulder and an arthroscope (or pencilsized<br />
camera) is used to look inside the<br />
glenohumeral joint.<br />
-2- -3-<br />
Nursing. Prior to joining the Orthopedic Clinic,<br />
Kimberly worked at Children’s on 10 Northwest,<br />
an inpatient unit. She has also worked at<br />
<strong>New</strong> England Medical Center, in the Pediatric<br />
Intensive Care Unit, and Franciscan <strong>Hospital</strong> for<br />
Children.<br />
Erin Dawicki, PA-C<br />
Erin attended the Medical University of South<br />
Carolina where she received a Master of Science<br />
in Physician Assistant Studies. Erin most recently<br />
worked as an EMT on the Disaster Medical Assistance<br />
Team at Rhode Island <strong>Hospital</strong>.<br />
Specialized instruments are then used to<br />
repair the injured labrum, ligaments, and<br />
capsule.<br />
There are some situations in which arthroscopic<br />
techniques are not used.<br />
figure 4<br />
figure 5<br />
Instead, the shoulder surgery is<br />
performed using a longer incision<br />
over the front of the shoulder joint.<br />
This is often referred to as “open” surgery.<br />
Your Home Team<br />
The Department of Orthopaedic Surgery<br />
at Children’s <strong>Hospital</strong> <strong>Boston</strong> has a number<br />
of healthcare providers who are available<br />
to help young athletes with shoulder<br />
instability. Our team of orthopaedic surgeons,<br />
physical therapists, nurses, and orthotists<br />
is well trained and ready to assist<br />
young athletes pursue successful, enjoyable,<br />
and safe sports seasons. In this<br />
game, we want everyone to be a winner.<br />
1. Candy cane<br />
2. Hockey<br />
3. Superbowl<br />
6. Patriots<br />
Across Down<br />
Kid’s Corner Answers<br />
4. Penguin<br />
5. Gingerbread<br />
6. Plow<br />
7. Salt<br />
8. Ski<br />
9. Snowflake