Wellness Foods & Supplements 3/2020
- Text
- Harnischcom
- Supplements
- Foods
- Wellness
- Clinical
- Salts
- Protein
- Dairy
- Vaginal
- Products
- Yogurt
- Mineral
- Calcium
- Magnesium
Clinical trials Photo ®
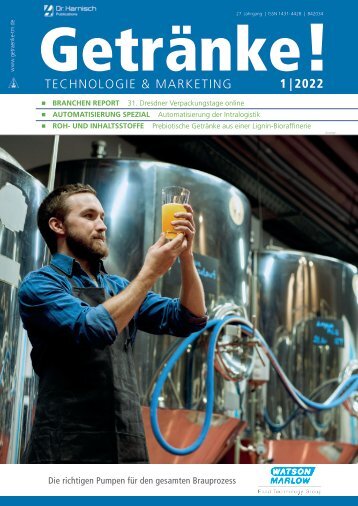
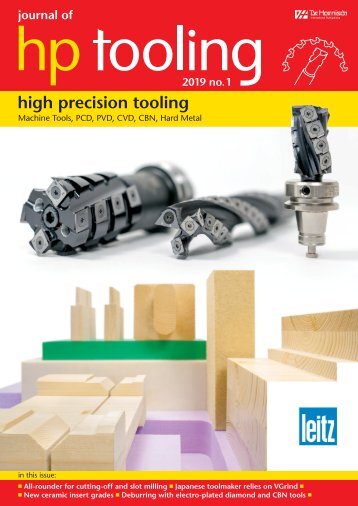
Clinical trials Photo ® : Adobe Stock/Robert Wilson Adaptive designs in clinical trials: when, why and how? The use of dietary supplements and nutraceuticals has been constantly growing among people who are looking for ways to promote wellbeing and health. Additionally, their demand for clarity around the attributes on product labeling is on the rise. Particularly, they want to know that the products they are ingesting are safe and effective based on rigorous clinical evidence obtained from studies testing the same products. This shift of consumers’ attitude highlights the importance of well-designed and well-conducted clinical trials in building and growing market of the products. A clinical trial can be conducted to assess absorption/bioavailability active ingredients, safety or tolerance, and/or efficacy of product, as well as consumers’ acceptance and satisfaction of product. All information and clinical results gathered in clinical trials serve as a foundation for marketing and scientific communications, as well as regulatory requirements. Biofortis a CRO (Contract Research Organization) that is part of Mérieux NutriSciences, specializes in clinical services for nutraceutical and food products and has successfully completed over 250 trials since 2002. Biofortis provides all expertise required for clinical study, ranging from scientific insights to fieldwork and data valorization needed to successfully manage international multicentric studies to assess bioavailability, efficacy, safety/tolerance. A team of scientists, statisticians and methodologists, focuses on each clients’ unique expectations and needs, and works to adapt persona lized, customized and robust designs. Traditionally, clini cal trials are run in three phases: design, execution, and data analysis. An alternative approach is the Adaptive Design trial which can be used to optimize the scientific data delivery and decrease cost and time to market, while still using robust and specific statistics models. The adaptive designs can be applied across all phases of clinical research, from early-phase dose response and safety designs to confirmatory trials. We interviewed two Biofortis experts; Hélène Chevallier (Clinical Methodologist) and Florence Gillaizeau (Senior Biostatistician), on the basics of adaptive design and why you could consider this for your future study with Biofortis. What is an adaptive design clinical trial? There is no universal definition of an adaptive design. As compared to traditional design trials, where you design, then you conduct the study, and finally you analyze the results, adaptive design is more flexible in that it allows the data to drive modifications of the original design (if scientifically justified and necessary) prior to the formal completion of the study. This clinical study design uses 28 No. 3 November/December 2020
Clinical trials accumulating data to decide how to modify certain aspects of the study without undermining the validity and integrity of the trial. After almost ten years since the first draft, the Food and Drug Administration (FDA) finally edited the final version of the “Adaptive Designs for Clinical Trials of Drugs and Biologics Guidance for Industry” last year (FDA, November 2019). In this guidance, the following definition is used: “an adaptive design is defined as a clinical trial design that allows for prospectively planned modifications to one or more aspects of the design based on accumulating data from subjects in the trial”. There are some main concepts common to all the references that discuss adaptive designs. First, during the study, every single modification needs to be prospectively planned into the protocol. After reviewing results of data analysis, usually through an interim analysis, with full control of the type I error (which means the control of the risk of a false positive conclusion), some modifications including but not limited to, changes to the sample size and population or premature discontinuation of one study arm, can be implemented. According to the FDA guidance, the interim analysis is defined as “any examination of data obtained from subjects in a trial while that trial is ongoing”. The analysis can be done in a fully blinded procedure or unblinded procedure. Could you explain more specifically the interim analyses? According to the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH), involving regulatory members (e. g. the European Commission, the US FDA, the Ministry of Health, Labour and Welfare of Japan) and industry Members (e. g. the Pharmaceutical Research and Manufacturers of America), an interim analysis is any analysis intended to compare treatment arms with respect to efficacy or safety at any time prior to the formal completion of a trial. The results are prepared by an independent statistician (other than the study statistician) and reported to an independent Data Monitoring Committee (DMC) that recommends to the sponsor whether to continue, modify or stop the trial. The DMC members must have no financial or intellectual conflicts of interests in the outcome of the study. Therefore, the participation of employees of the sponsor in this committee is discouraged. DMCs typically include clinicians and at least one biostatistician with expertise in clinical trial and interim data analysis. To avoid introducing bias into ensuing study design, conduct or interpretation, all interim analyses are carefully planned and described in the protocol and it is strongly recommended to maintain interim analysis blind for investigators, sponsors or anyone outside DMCs. Are there different kinds of adaptive design? There are several types of adaptive designs and more than one can be applied to the same trial. Below is a summary of the most common types. Fig. 1 : Different types of adaptive designs Adaptive designs are applicable to both early and confirmatory clinical trials. Adaptive designs for early clinical trials such as the Continual Reassessment Method (CRM) and seamless designs deal mainly with establishing safe and effective doses or dose–response relationships. The CRM aims to identify the dose with optimal efficacy/ response and is more accurate in estimating the maximum tolerable dose compared to a conventional design. Meanwhile, a seamless adaptive design combines two phases traditionally carried out in separate trials into one single study. Based on the review of interim results, change(s) to a study can occur in different development phases. For example, an adaptive randomization design involves shifting study participant allocation ratio towards more promising or informative treatment(s); an enrichment or subgroup design allows for adjustments to the recruitment of a specific subgroups based on efficacy endpoint; a group sequential design may lead to the premature termination of a trial based on efficacy, safety, and futility endpoints; adaptive-hypotheses design allows for changes in hypotheses, study endpoints and/or statistical No. 3 November/December 2020 29
- Seite 1: No. 3, November/December 2020 www.h
- Seite 4 und 5: Contents Health Convenience Food Fo
- Seite 6 und 7: Oils and fats Photo © : 123rf/jirk
- Seite 8 und 9: Oils and fats sive “key figure”
- Seite 10 und 11: Functional sugars Photo © : Jennew
- Seite 12 und 13: Nutrition and ageing Photo © : Ado
- Seite 14 und 15: Nutrition and ageing demineralizati
- Seite 16 und 17: Nutrition and ageing Proferrin ® ,
- Seite 18 und 19: Energy and endurance system is conn
- Seite 20 und 21: Minerals Photo ® : Adobe Stock/nd3
- Seite 22 und 23: Minerals Health Claims Magnesium co
- Seite 24 und 25: Women‘s health Probiotics for wom
- Seite 26 und 27: Women‘s health How can oral probi
- Seite 30 und 31: Clinical trials methods; and the sa
- Seite 32 und 33: Fortified dairy alternatives Minera
- Seite 34 und 35: Fortified dairy alternatives Dairy
- Seite 36 und 37: Fortified dairy alternatives theref
- Seite 38 und 39: Fortified dairy alternatives instea
- Seite 40 und 41: Dairy products lactose digestion”
- Seite 42 und 43: Dairy products EPILAC premium yogur
- Seite 44: Come and see for yourself: www.harn
Unangemessen
Laden...
Magazin per E-Mail verschicken
Laden...
Einbetten
Laden...