Single-pass-CO2-Laser-Skin-Resurfacing-of-Light - Washington ...
Single-pass-CO2-Laser-Skin-Resurfacing-of-Light - Washington ...
Single-pass-CO2-Laser-Skin-Resurfacing-of-Light - Washington ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
, ,<br />
~,<br />
j Cosmetic & <strong>Laser</strong> Ther 2003; 5: 39-42<br />
© j Cosmetic & <strong>Laser</strong> Ther. All rights reserved ISSN 1476-4172<br />
001: 10.1080/14764170310000835<br />
<strong>Single</strong>-<strong>pass</strong> <strong>CO2</strong> laser skin<br />
resurfacing <strong>of</strong> light and dark skin:<br />
t. Taylor&Francis<br />
• healthsciences 39<br />
extended experience with 52 patients<br />
Tina S Alster & Ranella J Hirsch<br />
Authors:<br />
T S Alster<br />
R J Hirsch<br />
<strong>Washington</strong> Institute <strong>of</strong><br />
Dermatologic <strong>Laser</strong> Surgery,<br />
<strong>Washington</strong>, DC, USA<br />
Received 30 July 2002<br />
Accepted 11 December 2002<br />
Introduction<br />
The goal <strong>of</strong> cutaneous resurfacing is to render the skin as<br />
smooth as possible. While there are many different<br />
treatments available to achieve this goal, the carbon<br />
dioxide (C02) laser remains the gold standard <strong>of</strong> laser<br />
Correspondence: Tina S Alster, MD, <strong>Washington</strong> Institute <strong>of</strong><br />
Dermatologic <strong>Laser</strong> Surgery, 2311 M Street, NW Suite 200, <strong>Washington</strong>,<br />
DC 20037, USA.<br />
Tel: (+ 1) 202 785 8855; Fax: (+ 1) 202 785 8858;<br />
E-mail: talster@skinlaser.com<br />
BACKGROUND: Multiple-<strong>pass</strong> carbon<br />
dioxide (C02) laser skin resurfacing<br />
has been a favored treatment modality<br />
for photodamaged and acnescarred<br />
skin over the past several<br />
years. Its association with numerous<br />
side effects and complications, particularly<br />
prolonged erythema and<br />
dyspigmentation, however, has dampened<br />
the initial enthusiasm reserved<br />
for its use. By reducing the laserassociated<br />
tissue ablation depth and<br />
degree <strong>of</strong> thermal necrosis, it is<br />
possible that the incidence <strong>of</strong> these<br />
side effects can also be reduced.<br />
PURPOSE: To evaluate the clinical<br />
efficacy and side effect pr<strong>of</strong>ile <strong>of</strong><br />
single-<strong>pass</strong> <strong>CO2</strong> laser skin resurfacing<br />
in a large series <strong>of</strong> patients.<br />
MATERIALS AND METHODS: A total <strong>of</strong><br />
52 consecutive patients (skin phototypes<br />
I-VI) with mild facial rhytides,<br />
atrophic scars, or infraorbital hyperpigmentation<br />
underwent single-<strong>pass</strong><br />
treatment with a high-energy, pulsed<br />
<strong>CO2</strong> laser. Side effects to treatment<br />
were closely monitored and tabulated.<br />
Clinical improvement using a quartile<br />
grading scale was assessed<br />
independently by two masked medical<br />
evaluators at 1, 3, 6, and 12<br />
months postoperatively.<br />
RESULTS: Significant clinical improvement<br />
was seen in all patients, with<br />
peak improvement scores noted at<br />
12 months. Greater clinical improvement<br />
was seen in patients with<br />
darker skin tones despite the near<br />
universal incidence <strong>of</strong> transient<br />
postoperative hyperpigmentation in<br />
these patients.<br />
CONCLUSIONS: <strong>Single</strong>-<strong>pass</strong> <strong>CO2</strong> laser<br />
skin resurfacing can improve the<br />
appearance <strong>of</strong> fine rhytides, mild<br />
atrophic scars, and infraorbital<br />
hyperpigmentation in all skin types.<br />
The severity and duration <strong>of</strong> side<br />
effects and complications are<br />
reduced with this technique (compared<br />
with multiple-<strong>pass</strong> procedures)<br />
and may <strong>of</strong>fer a possible solution to<br />
the problem <strong>of</strong> treating patients with<br />
darker complexions. J Cosmetic & <strong>Laser</strong><br />
Ther 2003; 5: 39-42<br />
skin resurfacing.l " With a wavelength <strong>of</strong> 10600 nm, the<br />
<strong>CO2</strong> laser is well suited for cutaneous resurfacing because<br />
<strong>of</strong> the strong absorption <strong>of</strong> its infrared wavelength by<br />
water-containing tissue in the skin. Such tissue comprises<br />
70% <strong>of</strong> total skin volume.<br />
The success <strong>of</strong> <strong>CO2</strong> laser skin resurfacing was historically<br />
limited by the emission <strong>of</strong> light in a continuous wave mode<br />
that produced zones <strong>of</strong> thermal destruction ranging from<br />
200 p.m to 2 mm beyond the target tissue, resulting in<br />
unintended scarring and fibrosis. With the application <strong>of</strong><br />
the modern theory <strong>of</strong> selective photothermolysis, as first
40 TS Alster & RJ Hirsch<br />
Original Research<br />
'0,1<br />
described by Anderson and Parrish in 1983,4 controlled<br />
destruction <strong>of</strong> target tissues could be achieved while<br />
limiting unwanted thermal damage to the surrounding<br />
skin. This is accomplished in part by limiting the pulse<br />
duration to a time shorter than the thermal relaxation time<br />
<strong>of</strong> the target. Consequently, when short pulsed « 1ms)<br />
<strong>CO2</strong> lasers were introduced in the mid-1990s, vaporization<br />
<strong>of</strong> very thin layers <strong>of</strong> skin (20-30 pm per <strong>pass</strong>) was made<br />
possible.c"<br />
Cutaneous resurfacing with the <strong>CO2</strong> laser has since been<br />
shown to be highly effective in the treatment <strong>of</strong><br />
photodamaged and acne-scarred skin, as well as for<br />
removal <strong>of</strong> a variety <strong>of</strong> epidermal and dermal lesions. 7 - 15<br />
Despite its high clinical satisfaction rate, <strong>CO2</strong> laser<br />
resurfacing has been associated with multiple side effects<br />
and complications, ranging from prolonged erythema to<br />
fibrosis and scarring. 16,17 One <strong>of</strong> the most common<br />
postoperative sequelae is transient cutaneous dyspigmentation.<br />
Over one-third <strong>of</strong> all patients who undergo <strong>CO2</strong> laser<br />
resurfacing develop moderate hyperpigmentation lasting<br />
several months, with a near universal occurrence in patients<br />
with darker skin photo types (Fitzpatrick type III or<br />
greaterj.l" Hypopigmentation is a far less frequent side<br />
effect and tends to be permanent. Patients must be clearly<br />
motivated to tolerate the extended recuperation from <strong>CO2</strong> laser resurfacing, which includes 7-10 days <strong>of</strong> intense<br />
erythema, edema, crusting, and discomfort. Viral, bacterial,<br />
and fungal infections can be seen during the first<br />
postoperative week before full re-epithelialization has<br />
been effected. Prompt, aggressive intervention with an<br />
emphasis on prevention is mandatory.<br />
The depth <strong>of</strong> ablation and residual thermal necrosis seen<br />
in the dermis correlates directly with the number <strong>of</strong> laser<br />
<strong>pass</strong>es perrorrne c d. 56", 18 19 W'Ith mcreasmg . . dept h and degree<br />
<strong>of</strong> thermal damage, the risk <strong>of</strong> pigmentary alteration<br />
rises. 20 - 23<br />
It stands to reason that limiting the ablation<br />
depth and extent <strong>of</strong> residual thermal necrosis would<br />
lower the incidence <strong>of</strong> postoperative side effects and<br />
complications.<br />
The purpose <strong>of</strong> this study was to evaluate the clinical<br />
efficacy and associated complication rates <strong>of</strong> single-<strong>pass</strong><br />
<strong>CO2</strong> laser resurfacing in a large series <strong>of</strong> patients with light<br />
and dark skin and to compare the results with those<br />
previously reported in the literature for traditional multi<strong>pass</strong><br />
<strong>CO2</strong> laser treatment.<br />
Materials and methods<br />
A total <strong>of</strong> 52 consecutive patients (47 females, 5 males; aged<br />
15-67 years, mean 52 years) with mild to moderate<br />
rhytides, infraorbital hyperpigmentation, or atrophic scars<br />
were included for study evaluation. <strong>Skin</strong> phototypes I-VI<br />
were represented (Table 1).<br />
Cutaneous anesthesia was obtained with appropriate<br />
facial nerve blocks using 1% lidocaine with 1:200000 units<br />
epinephrine. For full-face procedures, intravenous anesthesia<br />
was administered by a certified nurse anesthetist<br />
using a combination <strong>of</strong> prop<strong>of</strong>ol, Versed®, fentanyl, and<br />
ketamine.<br />
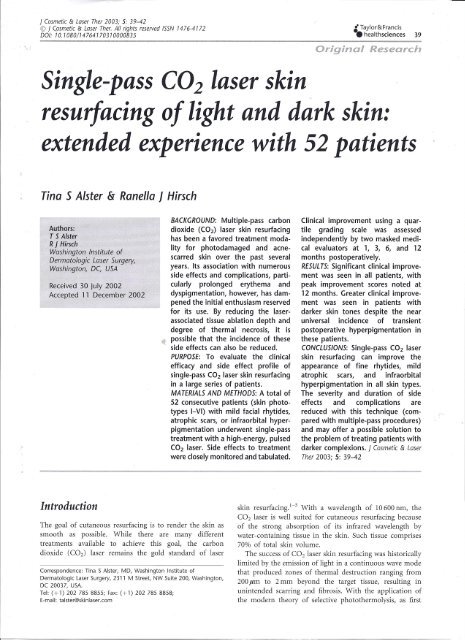
<strong>Skin</strong> type No. <strong>of</strong> Facial Infraorbital Atrophic<br />
patients rhytides hyperpigmentation scars<br />
I 5 3 2 0<br />
II 34 24 6 4<br />
III 10 5 3 2<br />
IV 1 0 0 1<br />
V 1 0 1 0<br />
VI 1 0 1 0<br />
Table 1<br />
Patient characteristics.<br />
The entire treatment area received adjacent nonoverlapping<br />
8 mm laser scans with a high-energy, pulsed<br />
<strong>CO2</strong> laser (UltraPulse; Coherent <strong>Laser</strong>, Ine., Palo Alto, CA,<br />
USA) at 300 m] <strong>of</strong> energy, 60 watts <strong>of</strong> power, and a CPG<br />
density <strong>of</strong> 5 by a single operator (TSA). Treatment edges<br />
and 'skip' areas were finished with single 3 mm spots<br />
(300 m] <strong>of</strong> energy, 5 watts <strong>of</strong> power). Partially desiccated<br />
tissue was left intact to serve as a biologic wound dressing<br />
(rather than being removed with saline or water-soaked<br />
gauze). Concomitant chemical peeling <strong>of</strong> the adjacent neck<br />
skin was performed in all patients undergoing full-face laser<br />
treatment using 25% trichloracetic acid (TCA) to achieve a<br />
light frost (2 minute acid application followed by cool<br />
water rinse).<br />
Immediately following treatment, healing ointment<br />
(Aquaphor; Beiersdorf, Ine., Norwalk, CT, USA) was<br />
applied to the irradiated skin. Each patient was instructed<br />
to perform gentle facial rinses with cool water several times<br />
daily, followed by liberal ointment application. Ice packs<br />
and round-the-clock acetaminophen were prescribed<br />
during the first 24-48 hours postoperatively to reduce<br />
swelling and discomfort. Full-face laser patients received a<br />
prednisone taper for 5 days. All patients were prescribed<br />
twice daily oral prophylactic antiviral treatment (valacyclovir<br />
500 mg) beginning on the day <strong>of</strong> surgery and<br />
continuing for 10 days. No other antibiotic prophylaxis was<br />
used. Patients were followed closely in the first postoperative<br />
week, during which time any residual coagulated<br />
debris was removed with dilute acetic acid compresses. Side<br />
effects and complications <strong>of</strong> treatment were monitored and<br />
treated as appropriate. All patients were able to apply<br />
camouflage makeup by 7-10 days postoperatively.<br />
Clinical response to treatment was documented by<br />
sequential digital photographs using identical camera<br />
settings, lighting, and patient positioning. Assessments <strong>of</strong><br />
treated areas compared with baseline pretreatment photographs<br />
were performed by two masked medical evaluators<br />
preoperatively and at 1, 3, 6, and 12 months postoperatively<br />
using a quartile rating scale (0 = 75% improvement).<br />
Results<br />
Significant improvement in skin tone, texture, and<br />
appearance <strong>of</strong> skin was noted in all patients. Average<br />
-
" I<br />
Singl~-<strong>pass</strong> C02 laser skin resurfacing 41<br />
clinical improvement scores peaked at 12 months regardless<br />
<strong>of</strong> skin type (Figure 1).<br />
Greater clinical improvement was seen in patients with<br />
darker skin tones (phototypes III-VI) (Figure 2). Postoperative<br />
erythema was rated as mild and lasted an average<br />
<strong>of</strong> 3.5 weeks (range 2-5 weeks). Hyperpigmentation was<br />
the most common side effect (average incidence <strong>of</strong> 46%,<br />
mean duration <strong>of</strong> 12.7 weeks), with 100% incidence in<br />
patients with skin phototypes III or darker, and was the<br />
reason for lower early clinical improvement scores in these<br />
patients (Table 2).<br />
Bacterial infections were observed in five patients (9%)<br />
within 3-5 days <strong>of</strong> the procedure. Four patients cultured<br />
positive for Staphylococcus aureus and one patient had<br />
superficial Enterococcus. All infections cleared on a 7-day<br />
course <strong>of</strong> appropriate oral antibiotics without sequelae. No<br />
herpetic or other infections were seen.<br />
Discussion<br />
By utilizing a single-<strong>pass</strong> <strong>CO2</strong> laser technique without posttreatment<br />
removal <strong>of</strong> desiccated epidermal debris, a<br />
biological (tissue) wound dressing is created. Ross et al<br />
previously reported speedier re-epithelialization in a pig<br />
model when partially desiccated tissue was left intact.r' The<br />
results <strong>of</strong> our study support this observation, with patients<br />
demonstrating complete re-epithelialization within 5-7<br />
days postoperatively (compared to 7-10 days following<br />
multi-<strong>pass</strong> <strong>CO2</strong> laser resurfacing procedures). In addition,<br />
the severity and duration <strong>of</strong> postoperative erythema seen in<br />
our patients was less than that typically observed after<br />
multi-<strong>pass</strong> <strong>CO2</strong> and erbium:YAG laser procedures - a<br />
finding also reported by others. 18,22,23In our study,<br />
erythema was more pronounced in patients with paler<br />
skin tones and lasted for a longer period <strong>of</strong> time,<br />
presumably due to the fact that it was easier to observe,<br />
rather than because <strong>of</strong> any differences in the extent <strong>of</strong><br />
thermal damage.<br />
Postoperative pigmentary changes remain a dreaded side<br />
effect <strong>of</strong> laser resurfacing, particularly in patients with<br />
darker complexions. As a consequence, individuals with<br />
dark skin phototypes have <strong>of</strong>ten not been considered to be<br />
suitable candidates for laser skin resurfacing procedures?4-27<br />
Analysis <strong>of</strong> our treatment series indicates that<br />
single-<strong>pass</strong> <strong>CO2</strong> laser resurfacing may <strong>of</strong>fer a possible<br />
solution to this problem. While the incidence <strong>of</strong><br />
Original Research<br />
<strong>Skin</strong> type Total no. <strong>of</strong> Hyperpigmentation Onset Duration Infection Onset Organisms Duration<br />
patients (n) (n) (weeks) (weeks) (n) (postoperative day) cultured (days)<br />
I 5 1 4 4-6 1 4 5. aureus 5<br />
II 34 10 4 3-6 2 3-5 5. aureus Enterobacter 4<br />
III 10 10 3 6 2 2 5. aureus 7<br />
IV 1 1 3 5 0<br />
V 1 1 4 9 0<br />
VI 1 1 5 9 0<br />
Table 2<br />
Incidence <strong>of</strong> side effects and complications.<br />
• Daric skin (SPT 11I-VI. n = 13)<br />
o <strong>Light</strong> skin (SPT I-II, n = 49)<br />
Figure 1<br />
Clinical improvement scores (0= 75% improvement).<br />
Figure 2<br />
(A) Patient with infraorbital hyperpigmentation (skin phototype V)<br />
before laser treatment; (8) 6 months after single-<strong>pass</strong> <strong>CO2</strong> laser<br />
resurfacing (clinical improvement score=2).<br />
(A)<br />
(8)
42 TS Alster & RJ Hirsch<br />
Original Research<br />
'~I<br />
hyperpigmentation remained high in our patients with<br />
dark skin tones, its intensity and duration were less than<br />
that reported after multi-<strong>pass</strong> <strong>CO2</strong> laser procedures (3-6<br />
months). In contrast to the findings reported by Ross and<br />
colleagues.l" where increased hyperpigmention was<br />
observed in periorbital regions (compared with perioral<br />
, areas), no differences in the rate <strong>of</strong> hyperpigmentation were<br />
seen in different facial areas in this study.<br />
References<br />
1. Alster TS, Lupton JR. An overview <strong>of</strong> cutaneous laser<br />
resurfacing. Clin Plast Surg 2001; 28: 37-52.<br />
2. Alster TS. Carbon dioxide laser skin resurfacing In:<br />
Alster TS, eds. Manual <strong>of</strong> cutaneous laser techniques, 2nd<br />
ed. Philadelphia: Lippincott, Williams & Wilkins, 2000:<br />
119-34.<br />
3. Alster TS. Cutaneous resurfacing with the <strong>CO2</strong> and<br />
erbium:YAG lasers: preoperative, intraoperative, and<br />
postoperative considerations. Plast Reconstr Surg 1999;<br />
103: 619-32.<br />
4. Anderson RR, Parrish JA. Selective photothermolysis:<br />
precise microsurgery by selective absorption <strong>of</strong> pulsed<br />
radiation. Science 1983; 220: 524-7.<br />
5. Alster TS, Nanni CA, Williams CM. Comparison <strong>of</strong> four<br />
<strong>CO2</strong> resurfacing lasers: a clinical and histopathologic<br />
evaluation. Dermatol Surg 1999; 25: 153-9.<br />
6. Alster TS, Kauvar ANB, Geronemus RG. Histology <strong>of</strong><br />
high energy, pulsed <strong>CO2</strong> laser resurfacing. Semin Cutan<br />
Med Surg 1996; 15: 189-93.<br />
7. Alster TS, Garg S. Treatment <strong>of</strong> facial rhytides with a<br />
high energy pulsed carbon dioxide laser. Plast Reconstr<br />
Surg 1996; 98: 791--4.<br />
8. Alster TS, West TB. <strong>Resurfacing</strong> <strong>of</strong> atrophic facial acne<br />
scars with a high energy, pulsed carbon dioxide laser.<br />
Dermatol Surg 1996; 22: 151-5.<br />
9. Fitzpatrick RE, Goldman MP, Satur NM, Tope W.<br />
Pulsed carbon dioxide laser resurfacing <strong>of</strong> photoaged<br />
facial skin. Arch Dermatol 1996; 132: 395-402.<br />
10. Alster TS, West TB. Ultrapulse <strong>CO2</strong> laser ablation <strong>of</strong><br />
xanthelasma. J Am Acad Dermatol 1996; 34: 848-9.<br />
11. West TB, Alster TS. Improvement <strong>of</strong> infraorbital<br />
hyperpigmentation following carbon dioxide laser resurfacing.<br />
Dermatol Surg 2000; 24: 65-6.<br />
12. Walia S, Alster TS. Prolonged clinical and histological<br />
effects from <strong>CO2</strong> laser resurfacing <strong>of</strong> atrophic acne scars.<br />
Dermatol Surg 1999; 25: 926-30.<br />
13. Schwartz RT, Burns AT, Rohrich RJ et al. Long term<br />
assessment <strong>of</strong> <strong>CO2</strong> facial laser resurfacing: aesthetic<br />
results and complications. Plast Reconstr Surg 1999; 103:<br />
592-601.<br />
14. Handrick C, Alster TS. <strong>Laser</strong> treatment <strong>of</strong> atrophoderma<br />
vermiculata. J Am Acad Dermatol 2001; 44: 693-5.<br />
','<br />
Conclusions<br />
<strong>Single</strong>-<strong>pass</strong> <strong>CO2</strong> laser skin resurfacing can improve the<br />
appearance <strong>of</strong> fine rhytides, mild atrophic scars, and<br />
infraorbital hyperpigmentation in all skin types. The<br />
severity and duration <strong>of</strong> side effects and complications<br />
are reduced with this procedure compared with those<br />
previously reported for multi-<strong>pass</strong> <strong>CO2</strong> laser procedures.<br />
15. Boyce S, Alster TS. <strong>CO2</strong> laser treatment <strong>of</strong> epidermal<br />
nevi: long-term success. Dermatol Surg 2002;<br />
28: 1-3.<br />
16. Alster TS, Lupton JR. Prevention and treatment <strong>of</strong> side<br />
effects and complications <strong>of</strong> cutaneous laser resurfacing.<br />
Plast Reconstr Surg 2002; 109: 308-16.<br />
17. Nanni CA, Alster TS. Complications <strong>of</strong> carbon dioxide<br />
laser resurfacing. An evaluation <strong>of</strong> 500 patients.<br />
Dermatol Surg 2000; 24: 315-20.<br />
18. Ross EV, Miller C, Meehan K et al. One-<strong>pass</strong> <strong>CO2</strong><br />
versus multiple-<strong>pass</strong> Er:YAG laser resurfacing in the<br />
treatment <strong>of</strong> rhytides: a comparison side-by-side study<br />
<strong>of</strong> pulsed <strong>CO2</strong> and Er:YAG lasers. Dermatol Surg 2001;<br />
27: 709-15.<br />
19. Burkhardt BR, Maw R. Are more <strong>pass</strong>es better? Safety<br />
versus efficacy with the pulsed <strong>CO2</strong> laser. Plast Reconstr<br />
Surg 1997; 100: 1532--4.<br />
20. Ross EV, Domankevitz Y, Skrobal M, Anderson RR.<br />
Effects <strong>of</strong> <strong>CO2</strong> laser pulse duration in ablation and<br />
residual thermal damage: implications for skin resurfacing.<br />
<strong>Laser</strong>s Surg Med 1996; 19: 123-9.<br />
21. Ross EV, Mowlavi A, Barnette D et al. The effect <strong>of</strong><br />
wiping on skin resurfacing in a pig model using a high<br />
energy pulsed <strong>CO2</strong> laser system. Dermatol Surg 1999; 25:<br />
81-8.<br />
22. Ruiz-Esparza J, Barba Gomez JM. Long term effects <strong>of</strong><br />
one general <strong>pass</strong> laser resurfacing: a look at dermal<br />
tightening and skin quality. Dermatol Surg 1999; 25:<br />
169-74.<br />
23. Ruiz-Esparza J, Barba Gomez JM, Labastida Gomez De<br />
La Torre 0, David L. Erythema after skin laser<br />
resurfacing. Dermatol Surg 2000; 24: 31--4.<br />
24. Horton S, Alster TS. Preoperative and postoperative<br />
considerations for cutaneous laser resurfacing. Cutis<br />
1999; 64: 399--406.<br />
25. Ho C, Nguyen Q, Lowe NJ et al. <strong>Laser</strong> resurfacing in<br />
pigmented skin. Dermatol Surg 1995; 21: 1035-7.<br />
26. Kim JW, Lee JO. <strong>Skin</strong> resurfacing with laser in Asians.<br />
Aesthetic Plast Surg 1997; 21: 115-17.<br />
27. Macedo 0, Alster TS. <strong>Laser</strong> treatment <strong>of</strong> darker skin<br />
tones: a practical approach. Dermatol Ther 2000; 13:<br />
114-26.