uRoloGIC onColoGy - University of Michigan Health System
uRoloGIC onColoGy - University of Michigan Health System
uRoloGIC onColoGy - University of Michigan Health System
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
the MIChIGAn dIFFeRenCe<br />
department <strong>of</strong> urology<br />
3875 taubman Center<br />
1500 e. Medical Center dr., sPC 5330<br />
Ann Arbor, MI 48109-5330<br />
InsIde thIs Iss ue...<br />
A Tailored Approach to the Management <strong>of</strong> Small Renal Masses . . . . . 2<br />
Recent Developments in Kidney Cancer Treatment . . . . . . . . . . . . . . . . 3<br />
Minimally Invasive Treatment Options . . . . . . . . . . . . . . . . . . . . . . . . . 4<br />
u n I v e R s I t y o F M I C h I G A n<br />
dePARtMent oF uRoloGy<br />
the CuRRent stAte oF<br />
<strong>uRoloGIC</strong> <strong>onColoGy</strong><br />
At the unIveRsIty oF MIChIGAn<br />
issue 1 Winter 2012<br />
GreetinGs from UroloGic oncoloGy<br />
our division has grown from four clinical urological oncologists<br />
in 2006 to our current status <strong>of</strong> eight clinical urologic<br />
oncologists (one full time at the Veterans Administration<br />
Hospital) and three basic scientists. this increase in clinical<br />
research has allowed us to better meet the urologic cancer<br />
needs <strong>of</strong> michigan’s population. With the aging population<br />
and better treatment for cardiovascular and pulmonary diseases,<br />
urologic cancer is becoming a more frequent issue in<br />
the health <strong>of</strong> our patients. the incidence <strong>of</strong> prostate, bladder,<br />
and renal cancers continue to increase with the aging population.<br />
With improved early detection methods, the average<br />
age <strong>of</strong> surgical treatment <strong>of</strong> our patients with urologic cancer<br />
continues to decrease, suggesting that long term functional<br />
outcomes will be critical.<br />
our division is saddened by the loss <strong>of</strong> Dr. Dave Wood<br />
who recently accepted a position at Beaumont Hospital<br />
as President <strong>of</strong> Beaumont Physician Partners and clinical<br />
faculty effective January 1, 2012. His main responsibilities<br />
will be to facilitate physician-hospital integration, establish<br />
clinical faculty responsibilities with the newly established<br />
William Beaumont/oakland <strong>University</strong> medical school, and<br />
lead quality improvement. His departure is a loss for us but a<br />
unique and challenging administrative opportunity for Dave.<br />
Personally, i have known Dave since he was a medical student<br />
at U-m and have tremendous respect for his character,<br />
judgment, and clinical skills. the Department <strong>of</strong> Urology<br />
at U-m wishes him nothing but success in his new venture.<br />
filling his shoes is not really possible but we have initiated a<br />
search process to identify a new division head.<br />
We have decided to dedicate this newsletter to our advances<br />
in renal surgery. Due to the wide spread use <strong>of</strong> abdominal<br />
imaging the identification <strong>of</strong> small renal masses less than<br />
4cm in size is more common. management <strong>of</strong> such tumors<br />
is complex since many <strong>of</strong> these may have little impact on<br />
the patient’s life, yet renal cancer is one <strong>of</strong> the more unpredictable<br />
malignancies that we deal with on a regular basis.<br />
therefore, over the years we have pioneered the development<br />
<strong>of</strong> minimally invasive techniques to identify, characterize, and<br />
treat these small renal masses. this includes sophisticated<br />
abdominal imaging, routine use <strong>of</strong> percutaneous biopsy <strong>of</strong> the<br />
small renal masses, and employment <strong>of</strong> minimally invasive<br />
continued on p. 2<br />
Managing Patients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5<br />
Rising Incidence Rates <strong>of</strong> Renal Cell Carcinoma . . . . . . . . . . . . . . . . . . 6<br />
Urologic Oncology Faculty . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
The CurrenT STaTe <strong>of</strong> urologiC onCology | iSSue 1 | winTer 2012<br />
continued from p. 1<br />
laparoscopic and robotic techniques for<br />
partial nephrectomy. Despite the early<br />
detection <strong>of</strong> many renal cell cancers, there<br />
is a stable population <strong>of</strong> patients who<br />
present with very large renal masses that<br />
have vascular extension into the vena<br />
cava and occasionally into the heart. the<br />
management <strong>of</strong> these patients is quite<br />
challenging; at the <strong>University</strong> <strong>of</strong> michigan<br />
we have developed a coordinated team <strong>of</strong><br />
urologists, vascular surgeons, cardiovascular<br />
surgeons, and support staff to manage<br />
these complex patients. With this team<br />
concept, we have significantly improved<br />
the outcomes <strong>of</strong> these patients with lethal<br />
cancers and have been able to <strong>of</strong>fer sophisticated<br />
adjuvant clinical trials using newly<br />
available biological agents.<br />
Because <strong>of</strong> our clinical and research<br />
growth, within these pages we also highlight<br />
and introduce the members <strong>of</strong> the<br />
Division <strong>of</strong> Urologic oncology with brief<br />
descriptions <strong>of</strong> their clinical and research<br />
focuses. if you have any patient care questions<br />
or concerns or have any patient with<br />
a urologic malignancy that you would<br />
like to refer to the <strong>University</strong> <strong>of</strong> michigan,<br />
please do hesitate to contact us:<br />
<strong>University</strong> <strong>of</strong> michigan cancer center<br />
Hotline : 734-647-8903<br />
or contact me personally at:<br />
734-936-0054.<br />
Best Wishes<br />
Jim montie, mD<br />
Interim Head, Division <strong>of</strong> Urologic<br />
Oncology<br />
Valassis Pr<strong>of</strong>essor <strong>of</strong> Urologic Oncology<br />
2<br />
A tailored Approach to the management <strong>of</strong><br />
small renal masses<br />
Alon Weizer, MD, MS<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> Urology Surgery<br />
renal cell carcinoma affects more than<br />
50,000 people each year and roughly 14,000<br />
die <strong>of</strong> the disease annually. However, most<br />
people diagnosed with kidney cancer have<br />
small tumors (< 4 cm) that are picked up<br />
when they undergo radiographic evaluation<br />
because <strong>of</strong> other symptoms. on cursory<br />
review, it would seem like this would lead to<br />
more people getting treated earlier and fewer<br />
people dying from kidney cancer. there are<br />
several problems with this logic. first, it is still<br />
the people diagnosed with large tumors that<br />
die from kidney cancer, while a much smaller<br />
number <strong>of</strong> people with small renal masses die<br />
from their disease despite receiving aggressive<br />
surgical treatment. second, many <strong>of</strong> the small<br />
renal masses identified incidentally on imaging<br />
are non-cancerous, so treating these patients<br />
not only does not impact survival but also<br />
exposes them to the risk <strong>of</strong> surgery. finally,<br />
many patients continue to undergo radical<br />
nephrectomy (removal <strong>of</strong> the entire kidney)<br />
despite the fact that partial nephrectomy<br />
(removal <strong>of</strong> just the tumor) might be equally<br />
affective as might be ablative therapy, which<br />
destroys the tumor in place. the chief benefit<br />
<strong>of</strong> removing the tumor while preserving the<br />
kidney over total kidney removal is that preservation<br />
<strong>of</strong> kidney function protects patients<br />
from the risk <strong>of</strong> chronic kidney disease over<br />
a long period <strong>of</strong> time without compromising<br />
cancer control.<br />
over the last several years, we have worked<br />
to improve the treatment <strong>of</strong> patients with<br />
small renal masses. for instance, we now have<br />
a team <strong>of</strong> urologists dedicated to individualizing<br />
treatment for each patient who is seen<br />
at U-m’s Department <strong>of</strong> Urology. this means<br />
that we first try to determine whether a person<br />
with a newly diagnosed kidney tumor<br />
needs treatment at all. most <strong>of</strong> our patients<br />
with a tumor < 4 cm are evaluated with a<br />
renal mass biopsy, which our radiology colleagues<br />
perform as an outpatient procedure<br />
in patients under sedation. this well-tolerated<br />
biopsy allows us to identify the almost 30 percent<br />
<strong>of</strong> patients with non-cancerous tumors<br />
who do not require any further treatment.<br />
A biopsy positive for kidney cancer provides<br />
us with information about the type <strong>of</strong> cancer<br />
and its aggressiveness, allowing us to counsel<br />
patients regarding the best treatment option<br />
for them. treatment options include close surveillance<br />
<strong>of</strong> patients with non-aggressive kidney<br />
cancers, kidney preserving surgeries (ablation,<br />
partial nephrectomy through an open<br />
incision or a laparoscopic/robotic approach),<br />
and complete kidney removal when the biopsy<br />
findings identify a very aggressive cancer that<br />
would benefit from this approach.<br />
in conclusion, we’re working<br />
hard at U-m to find the most<br />
effective treatment regimen<br />
for each individual patient<br />
with a small renal mass.<br />
However, our personalized<br />
care program for patients<br />
with small renal masses and<br />
early kidney cancer is at an<br />
early stage. through cuttingedge<br />
translational research,<br />
we hope to further refine<br />
our ability to determine<br />
who can avoid treatment<br />
for their renal mass, who<br />
would benefit from nephron<br />
sparing procedures, and who<br />
requires multidisciplinary<br />
care by our excellent team <strong>of</strong><br />
doctors at U-m.
ecent Developments in Kidney cancer treatment<br />
Bruce Redman, DO<br />
Pr<strong>of</strong>essor <strong>of</strong> Internal Medicine<br />
in the past five years, the fDA has approved<br />
six new agents for the treatment <strong>of</strong> metastatic<br />
kidney cancer. though the common target<br />
<strong>of</strong> these agents is angiogenesis, they can be<br />
grouped into three distinct classes based on<br />
their mechanisms <strong>of</strong> action.<br />
1. tyrosine kinase inhibition (tKi):<br />
represented by sunitinib, pazopanib,<br />
and sorafenib<br />
2. monoclonal antibody: represented<br />
by bevacizumab<br />
3. mammalian target <strong>of</strong> rapamycin<br />
(mtor) inhibition: represented by<br />
everolimus and temsirolimus<br />
the fDA approved all <strong>of</strong> these agents<br />
because they demonstrated clinical benefits<br />
in randomized trials. specifically, these compounds<br />
delayed metastatic disease progression;<br />
temsirolimus was the only agent, however,<br />
to show an overall survival advantage<br />
(albeit compared to the inactive interferon<br />
alfa). yet none <strong>of</strong> these agents are curative<br />
for metastatic clear cell carcinoma <strong>of</strong> the kidney,<br />
the only curative therapy for metastatic<br />
kidney cancer remains high-dose interleukin-2,<br />
and it only works in highly selected<br />
patients. Patients with metastatic clear cell<br />
carcinoma should be referred to a cancer<br />
center that has experience in, and expertise<br />
at, utilizing high-dose il-2 to discuss this<br />
potentially curative treatment option. for a<br />
more detailed discussion <strong>of</strong> the agents and<br />
how they fit in the treatment paradigm <strong>of</strong><br />
advanced kidney cancer, visit the national<br />
comprehensive cancer network treatment<br />
Guidelines webpage (www.nccn.org).<br />
As in the case <strong>of</strong> all clinical research, advances<br />
lead to additional questions. the following<br />
represent several <strong>of</strong> the more prominent<br />
research questions that have arisen in regard<br />
to the care <strong>of</strong> patients with kidney cancer.<br />
1. What role does cytoreductive<br />
nephrectomy play in the treatment<br />
<strong>of</strong> stage iV kidney cancer in the<br />
current era <strong>of</strong> targeted therapies?<br />
2. What are the mechanisms <strong>of</strong> resistance<br />
to targeted therapies?<br />
a. in primary failure (no<br />
response to initial therapy)<br />
b. in acquired resistance (initial<br />
response followed by disease<br />
progression)<br />
3. What is the role, if any, for the<br />
adjuvant treatment <strong>of</strong> high-risk<br />
patients after definitive surgery?<br />
4. When and how do we evaluate<br />
novel investigational therapies in<br />
the treatment <strong>of</strong> stage iV kidney<br />
cancer?<br />
Cytoreductive Nephrectomy<br />
there is currently no clinical trial data defining<br />
what role cytoreductive nephrectomy, in<br />
conjunction with the use <strong>of</strong> targeted therapies,<br />
plays in the outcome <strong>of</strong> patients with kidney<br />
cancer. Previous clinical trial results supported<br />
the use <strong>of</strong> cytoreductive nephrectomy plus<br />
interferon in selected patients with metastatic<br />
kidney cancer, but these results are difficult to<br />
translate to other targeted agents. interferon is<br />
now considered an inactive therapy for kidney<br />
cancer. the current front line tyrosine kinase<br />
inhibitors (tKis) have much greater clinical<br />
activity than interferon and thus may abrogate<br />
any benefit from cytoreductive nephrectomy.<br />
the question <strong>of</strong> whether cytoreductive<br />
nephrectomy, followed by the use <strong>of</strong> a tKi, is<br />
most effective is being addressed in ongoing<br />
national and international trials.<br />
Mechanisms <strong>of</strong> Resistance<br />
At the present time, we have no definitive<br />
answer to the question: What are the mechanisms<br />
<strong>of</strong> resistance to targeted therapies? We<br />
are, however, testing multiple hypotheses in<br />
our active clinical research.<br />
Adjuvant Treatment<br />
there is currently no validated adjuvant<br />
therapy for the treatment <strong>of</strong> high-risk resected<br />
kidney cancer. However, at U-m, we are<br />
participating in a national cooperative group<br />
trial, led by the southwest oncology Group,<br />
<strong>of</strong> a randomized double blind placebo controlled<br />
trial <strong>of</strong> everolimus as adjuvant therapy.<br />
Investigational Therapy<br />
there are no curative treatment options for<br />
patients who have not responded to il-2<br />
or who are not candidates for il-2. While<br />
current targeted therapies can meaningfully<br />
improve progression free survival, resistance<br />
ultimately develops in all patients. At U-m,<br />
we are performing clinical trials to evaluate<br />
new novel therapies for patients with metastatic<br />
kidney cancer; these are either part <strong>of</strong><br />
our ongoing Phase ii trial <strong>of</strong> anti-PD-1 immunomodulating<br />
trial or they are part <strong>of</strong> our<br />
Phase i program.<br />
3
The CurrenT STaTe <strong>of</strong> urologiC onCology | iSSue 1 | winTer 2012<br />
minimally invasive treatment options for Patients with Kidney cancer<br />
J. Stuart Wolf, Jr., MD<br />
David A. Bloom Pr<strong>of</strong>essor <strong>of</strong> Urology<br />
Co-Director, <strong>Michigan</strong> Center for Minimally Invasive Urology<br />
most kidney cancers are localized to the<br />
kidney and can be addressed with minimally<br />
invasive techniques. Broadly speaking, there<br />
are two surgical procedures (nephrectomy<br />
and nephron-sparing surgery) used in treating<br />
the disease, two methods <strong>of</strong> getting rid <strong>of</strong> it<br />
(tissue removal and tissue ablation), and two<br />
minimally invasive surgical approaches (laparoscopic/robotic<br />
surgery, and percutaneous<br />
techniques) (see figure at right). Among these,<br />
laparoscopic radical nephrectomy was the first<br />
procedure <strong>of</strong>fered to patients. it took almost<br />
10 years from its inception in 1990 to achieve<br />
widespread use, but it is now accepted as a<br />
standard treatment for cancer requiring complete<br />
kidney removal. the first laparoscopic<br />
radical nephrectomy in the state <strong>of</strong> michigan<br />
was performed at U-m, and our pioneering<br />
work with this hand-assisted laparoscopic<br />
technique enabled many practitioners to start<br />
using this approach. 1 our extensive experience<br />
at U-m with renal laparoscopy allows<br />
us to <strong>of</strong>fer this procedure even to patients<br />
with adrenal, renal vein, and/or lymph node<br />
involvement; only renal tumors with extensive<br />
regional involvement are managed with open<br />
surgical radical nephrectomy.<br />
one <strong>of</strong> the unfortunate downstream effects<br />
<strong>of</strong> the popularization <strong>of</strong> laparoscopic radical<br />
nephrectomy, however, is that it may have<br />
retarded the promulgation <strong>of</strong> partial nephrectomy.<br />
At about the same time that laparoscopic<br />
radical nephrectomy was introduced,<br />
data was established suggesting that partial<br />
nephrectomy for small renal masses provided<br />
cancer control equivalent to that provided by<br />
radical nephrectomy. Because urologists were<br />
motivated to deliver the “latest” care, and<br />
patients were understandably attracted to the<br />
less-invasive technique <strong>of</strong> laparoscopy, many<br />
laparoscopic radical nephrectomies were<br />
performed in patients who should have been<br />
managed with partial nephrectomy. the technical<br />
difficulty <strong>of</strong> partial nephrectomy, even<br />
when performed with open surgery, undoubtedly<br />
contributed to its slow gain in popularity<br />
as well. more recent evidence suggests that<br />
4<br />
partial nephrectomy may provide a long-term<br />
survival advantage over radical nephrectomy,<br />
owing to the health benefits <strong>of</strong> better renal<br />
function.<br />
thanks to the advent <strong>of</strong> laparoscopic partial<br />
nephrectomy, there is now a solution to the<br />
problem <strong>of</strong> <strong>of</strong>fering patients a less-invasive<br />
procedure while also sparing nephrons.<br />
Having performed the first laparoscopic partial<br />
nephrectomy in the state <strong>of</strong> michigan at<br />
U-m and since then 500 more, we now have<br />
an extensive experience with this procedure. 2<br />
more recently, we also began to perform<br />
robotic partial nephrectomy, and already have<br />
an institutional experience <strong>of</strong> more than 150<br />
cases. 3 our ability to <strong>of</strong>fer both laparoscopic<br />
and robotic partial nephrectomy, performed<br />
by surgeons with extensive experience, is a<br />
distinct advantage <strong>of</strong> our program.<br />
finally, renal tumor ablation <strong>of</strong>fers a management<br />
option <strong>of</strong> considerable benefit in certain<br />
situations. there are a variety <strong>of</strong> reasons why<br />
partial nephrectomy might not be the right<br />
option for some patients: recurrence <strong>of</strong> renal<br />
cancer in a previously operated site, whether<br />
it be a fossa recurrence after radical nephrectomy,<br />
a local recurrence or multifocal recur-<br />
rence after partial nephrectomy, or continuing<br />
development <strong>of</strong> renal tumors in the setting <strong>of</strong><br />
a hereditary syndrome such as Von Hippellindau<br />
disease, presents great surgical challenges.<br />
second, surgery might be more dangerous<br />
for patients with hostile abdomens (owing<br />
to prior surgery, radiation, crohn’s disease,<br />
etc.) than a renal tumor ablation. finally,<br />
some patients have normal life expectancies<br />
but cannot tolerate surgical complications<br />
such as a hemorrhage. With these patients,<br />
renal tumor ablation <strong>of</strong>fers a good alternative<br />
to partial or radical nephrectomy.<br />
At U-m, we work closely with our colleagues<br />
in the Department <strong>of</strong> radiology, who perform<br />
percutaneous radi<strong>of</strong>requency ablations and<br />
percutaneous cryo-ablationa. less commonly,<br />
a tumor that we would prefer to treat with<br />
ablation is not accessible through the percutaneous<br />
route. With these cases, we perform<br />
laparoscopic cryo-ablations.<br />
in addition to publishing reports on the<br />
surgical developments described above, the<br />
Department <strong>of</strong> Urology has played a leadership<br />
role in assessing problems in the management<br />
<strong>of</strong> kidney cancer that have arisen<br />
given nationwide trends in the disease. these
include the rising incidence <strong>of</strong> small renal<br />
masses, 4 the underutilization <strong>of</strong> partial<br />
nephrectomy, 5 impediments to the adoption<br />
<strong>of</strong> laparoscopic renal surgery, 6 and<br />
unintended consequences <strong>of</strong> laparoscopic<br />
radical nephrectomy. 7<br />
care for localized kidney cancer at the<br />
<strong>University</strong> <strong>of</strong> michigan is provided by<br />
urologists who are clinical pioneers,<br />
experienced surgeons, and innovative<br />
researchers.<br />
references<br />
1. Wolf, J. s., Jr., moon, t. D., and nakada, s.<br />
y.: Hand assisted laparoscopic nephrectomy:<br />
comparison to standard laparoscopic nephrectomy.<br />
J. Urol., 160: 22–27, 1998.<br />
2. Weizer, A. Z., Gilbert, s. m., roberts, W. W.,<br />
Hollenbeck, B. K., and Wolf, J. s., Jr.: tailoring technique<br />
<strong>of</strong> laparoscopic partial nephrectomy to tumor<br />
characteristics. J. Urology, 180: 1273–78, 2008.<br />
3. ellison, J. s., montgomery, J. s., Hafez, K. s.,<br />
miller, D. c., Wolf, J. s., Jr., and Weizer, A. Z.:<br />
tumor characteristics and outcomes <strong>of</strong> robotic<br />
assisted laparoscopic and conventional laparoscopic<br />
partial nephrectomy. J endourology, 24 supplement<br />
1: A152–53, 2010.<br />
4. Hollingsworth J. m., miller D. c., Daignault s.,<br />
and Hollenbeck, B. K.: rising incidence <strong>of</strong> small<br />
renal masses: A need to reassess treatment effect. J<br />
natl cancer inst, 2006; 98: 1331–34.<br />
5. miller D. c., Hollingsworth J. m., Hafez K. s.,<br />
Daignault s., and Hollenbeck, B.K.: Partial nephrectomy<br />
for small renal masses: An emerging quality <strong>of</strong><br />
care concern? J Urol 2006; 175: 853.<br />
6. filson, c. P., Banerjee, m., Wolf, J. s., Jr., ye, Z.,<br />
Wei, J. t. and miller, D. c.: surgeon characteristics<br />
and long-term trends in the adoption <strong>of</strong> laparoscopic<br />
radical nephrectomy. J. Urology, 185:2072 – 77,<br />
2011.<br />
7. tan, H-J., Wolf, J. s., Jr., ye, Z., Wei, J. t., and<br />
miller, D. c.: Population-level comparative effectiveness<br />
<strong>of</strong> laparoscopic versus open radical nephrectomy<br />
for patients with kidney cancer. cancer, in press.<br />
managing Patients with locally Advanced<br />
Kidney cancer and familial/Hereditary renal<br />
cancer<br />
Khaled Hafez, MD<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Urology<br />
in the past, patients with renal cell carcinoma<br />
(rcc) commonly had locally advanced rcc<br />
at the time <strong>of</strong> their diagnosis. today, however,<br />
approximately 70 percent <strong>of</strong> patients are<br />
diagnosed incidentally as a result <strong>of</strong> enhanced<br />
imaging techniques. nevertheless, rcc is a<br />
highly vascular malignancy with a tendency to<br />
invade the venous system, resulting in a tumor<br />
thrombus in the renal vein or in the inferior<br />
vena cava (iVc).<br />
Although a majority <strong>of</strong> patients with rcc<br />
are now diagnosed with low-stage tumors, in<br />
the case <strong>of</strong> four to ten percent <strong>of</strong> them, the<br />
tumor is present in the venous circulation,<br />
specifically in the renal vein or in the iVc.<br />
Despite recent advances in systemic therapy,<br />
the standard treatment for patients with rcc<br />
with tumor thrombus remains removing the<br />
kidney with the attached tumor thrombus, a<br />
complex procedure <strong>of</strong>ten requiring a multidisciplinary<br />
approach. surgeons are required<br />
to utilize techniques commonly employed in<br />
cardiovascular surgery, such as extracorporeal<br />
circulation and hypothermia, as well as liver<br />
mobilization techniques derived from liver<br />
transplant surgery. in patients without evidence<br />
<strong>of</strong> metastasis, surgery is performed with<br />
curative intent.<br />
for patients with distant metastasis, we use a<br />
multidisciplinary approach at U-m, consisting<br />
<strong>of</strong> cytoreduction followed by possible immunotherapy<br />
and/or targeted therapy. our team<br />
<strong>of</strong> specialists includes a specialized anesthesia<br />
team with expertise in cardiac monitoring<br />
using trans-esophageal echocardiography,<br />
while our surgical team includes nurses, circulatory<br />
bypass technicians, and surgeons<br />
familiar with the nuances <strong>of</strong> this high-risk<br />
procedure. the latter consists <strong>of</strong> a urologist,<br />
a liver transplant surgeon, and a cardiac surgeon.<br />
With this team <strong>of</strong> specialists in place,<br />
we are well prepared for those cases requiring<br />
extensive liver mobilization and/or venous or<br />
cardiac bypass.<br />
At the outset, we perform a pre-operative<br />
evaluation <strong>of</strong> the patient in order to determine<br />
the extent <strong>of</strong> the disease. our postoperative<br />
care includes routine admission to the surgical<br />
intensive care unit for close monitoring.<br />
Improving Outcomes for Hereditary<br />
Renal Cancer Patients<br />
the true prevalence <strong>of</strong> hereditary renal cancer<br />
(Hrc) is poorly understood since many cases<br />
go unrecognized. According to conservative<br />
estimates, three to five percent <strong>of</strong> renal<br />
cancer patients have inherited forms <strong>of</strong> the<br />
disease. to improve their survival rate, it is<br />
critical that we identify familial renal cancer<br />
syndromes. By doing so, we can provide early<br />
screening <strong>of</strong>, and careful follow-up for, these<br />
individuals and their relatives. Known hereditary<br />
kidney cancer syndromes with identified<br />
genetic mutations include von Hippel–lindau<br />
disease (VHl), hereditary papillary renal<br />
cancer (HPrc), Birt–Hogg–Dube syndrome<br />
(BHD), hereditary leiomyomatosis renal cell<br />
carcinoma syndrome (Hlrcc), and tuberous<br />
sclerosis. recognizing the clinical features<br />
associated with Hrc is <strong>of</strong>ten the most important<br />
step in establishing the diagnosis.<br />
At U-m, we have developed conservative<br />
management strategies for Hrc syndromes,<br />
including the use <strong>of</strong> nephron sparing procedures<br />
aimed at limiting treatment-related<br />
morbidity, and the use <strong>of</strong> renal replacement<br />
therapy for patients with chronic kidney<br />
disease. A well-coordinated and experienced<br />
team <strong>of</strong> specialists evaluates patients with<br />
Hrc, which is led by a geneticist and includes<br />
physicians and surgeons from several other<br />
disciplines including urology, general surgery,<br />
neurosurgery, endocrinology, ophthalmology,<br />
otolaryngology, radiology, and social work.<br />
U-m is currently preparing to host the<br />
Annual national VHl conference in 2012,<br />
which will provide us with an opportunity to<br />
highlight the exceptional VHl clinical care<br />
Program available here.<br />
5
The CurrenT STaTe <strong>of</strong> urologiC onCology | iSSue 1 | winTer 2012<br />
rising incidence rates <strong>of</strong> renal cell carcinoma:<br />
challenges for the 21st century<br />
David Miller, MD<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> Urology Surgery<br />
national incidence rates for renal cell carcinoma<br />
(rcc) have risen steadily during the past<br />
two decades. this trend is mediated mainly<br />
by an increase in the number <strong>of</strong> patients with<br />
early-stage cancers. During this time period,<br />
the treatment paradigm for solid renal masses<br />
has favored their expedient removal upon<br />
detection. consequently, an increase in the<br />
frequency <strong>of</strong> kidney cancer surgery has paralleled<br />
the rising incidence <strong>of</strong> rcc. Although<br />
it is not endorsed universally, the current<br />
treatment paradigm is based on the assumption<br />
that early intervention (i.e., treatment <strong>of</strong><br />
patients presumed to have early, low-stage<br />
disease) will result in better survival outcomes.<br />
in many ways, the rising incidence <strong>of</strong> renal<br />
cell carcinoma, and the concurrent increase in<br />
surgical therapy, provides a useful framework<br />
for considering the major challenges and<br />
opportunities for improving care and outcomes<br />
for patient with renal cell carcinoma<br />
in the 21st century. first, there is still a need<br />
to continue improving surgical patterns <strong>of</strong><br />
care among patients with early-stage rcc.<br />
open radical nephrectomy has long been the<br />
standard treatment for this group <strong>of</strong> patients.<br />
in recent years, however, easier convalescence<br />
and equivalent cancer control established<br />
laparoscopy as an alternative standard <strong>of</strong> care<br />
for most patients treated with radical nephrectomy.<br />
concurrent with the gradual dissemination<br />
<strong>of</strong> laparoscopic radical nephrectomy,<br />
studies have demonstrated that for patients<br />
with small rccs (i.e., generally those ≤ 4<br />
cm), partial instead <strong>of</strong> radical nephrectomy<br />
achieves identical cancer control while better<br />
preserving long-term renal function and<br />
reducing overtreatment <strong>of</strong> benign or clinically<br />
indolent tumors.<br />
from a clinical perspective, therefore, it can<br />
be argued that the benefits <strong>of</strong> partial nephrectomy<br />
and laparoscopy support the application<br />
<strong>of</strong> one or both <strong>of</strong> these techniques for a<br />
vast majority <strong>of</strong> patients with organ-confined<br />
rccs. However, recent studies suggest that<br />
6<br />
open radical nephrectomy remains an all-toocommon<br />
surgical treatment for many patients<br />
with early-stage rcc. Among the many factors<br />
that may be impeding the adoption <strong>of</strong><br />
laparoscopy and/or partial nephrectomy are<br />
the technical complexity <strong>of</strong> these procedures,<br />
and a lingering absence <strong>of</strong> pr<strong>of</strong>essional consensus<br />
regarding optimal surgical therapy for<br />
patients with small rccs. in light <strong>of</strong> these<br />
concerns, several mentored- and simulatorbased<br />
types <strong>of</strong> training have now emerged to<br />
facilitate the development and transfer <strong>of</strong> minimally<br />
invasive surgical techniques, including<br />
both robotics and standard laparoscopy. in<br />
order to complement these efforts, members<br />
<strong>of</strong> the urology community now also have a<br />
clear opportunity (and arguably strong motivation)<br />
to support additional research and/or<br />
development <strong>of</strong> clinical guidelines that clarify<br />
optimal treatment algorithms for patients with<br />
kidney cancer. the recently released AUA<br />
guidelines for management <strong>of</strong> patients with<br />
small renal masses represent an important<br />
step forward in this area.<br />
in many ways, the rising incidence <strong>of</strong> renal<br />
cell carcinoma, and the concurrent increase in<br />
surgical therapy, provides a useful framework<br />
for considering the major challenges and<br />
opportunities for improving care and outcomes<br />
for patient with renal cell carcinoma<br />
in the 21st century.<br />
A second, and related, challenge stems from<br />
the biological heterogeneity <strong>of</strong> rcc and<br />
the physiological heterogeneity <strong>of</strong> patients<br />
presenting with these tumors. in particular,<br />
the growing recognition that a non-trivial<br />
proportion <strong>of</strong> rccs may have an indolent<br />
clinical course, and that many patients with<br />
these tumors ultimately die from other causes,<br />
has heightened interest in the expansion <strong>of</strong><br />
active surveillance as an initial management<br />
strategy for patients with early-stage kidney<br />
cancer. the potential merits and pitfalls <strong>of</strong><br />
this approach, including the potentially pivotal<br />
role <strong>of</strong> percutaneous renal mass biopsy<br />
for patient selection, are discussed in a separate<br />
section <strong>of</strong> this newsletter. moreover, the<br />
evidence base and rationale for active surveillance<br />
would also be enhanced greatly by a<br />
better understanding <strong>of</strong> the implications <strong>of</strong><br />
co-morbid disease among patients with kidney<br />
cancer. in fact, at least one recent study suggests<br />
that nearly 25 percent <strong>of</strong> patients with<br />
rcc have at least two significant comorbidities<br />
at the time <strong>of</strong> their cancer diagnosis.<br />
Given this, an important 21st-century challenge<br />
for urologists is to better define longterm<br />
survival outcomes among patients with<br />
rcc, including the frequency <strong>of</strong> deaths due<br />
to causes unrelated to the cancer diagnosis.<br />
these data, when combined with detailed<br />
information on the duration and severity <strong>of</strong><br />
comorbid conditions, may prove invaluable<br />
to understanding and predicting competing<br />
causes <strong>of</strong> death among patients considering<br />
surgical treatment for<br />
kidney cancer. this<br />
information will, in<br />
turn, inform ongoing<br />
debates surrounding<br />
the appropriate treatment<br />
intensity (versus<br />
expectant approaches)<br />
for populations <strong>of</strong><br />
patients with earlystage<br />
rcc.<br />
in summary, the<br />
incidence <strong>of</strong> rcc continues to rise in the 21st<br />
century. As the physicians responsible for the<br />
treatment <strong>of</strong> a majority <strong>of</strong> patients with this<br />
common malignancy, we in the urology community<br />
have a tremendous opportunity to<br />
work together to continually refine and optimize<br />
the surgical and non-surgical treatment<br />
<strong>of</strong> patients with renal cell carcinoma. i look<br />
forward to joining you in this effort.
UroloGic oncoloGy fAcUlty<br />
Clinicians<br />
KHAleD sAmir HAfeZ, mD<br />
Faculty Appointment: Associate Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Degree: 1988, mD, cairo <strong>University</strong> school <strong>of</strong><br />
medicine, cairo, egypt<br />
Residency: 1993, Urology, cairo <strong>University</strong> school <strong>of</strong><br />
medicine, cairo, egypt<br />
2004, Urology, <strong>University</strong> <strong>of</strong> michigan<br />
Fellowship: 1997, Kidney cancer, renal-vascular and<br />
kidney transplantation, cleveland clinic foundation,<br />
cleveland, ohio<br />
Clinical and Research Interests: Dr Hafez’s clinical work focuses on urologic oncology,<br />
including bladder, kidney, and testis cancer. He has extensive clinical expertise<br />
with advanced renal cancer and with nephron sparing surgery for treating the<br />
cancer. He also has vast experience in the treatment <strong>of</strong> bladder cancer and such<br />
surgical options as radical cystectomy with neobladder urinary diversion. He has<br />
conducted multiple basic science projects, investigating renal physiology, oncology,<br />
and immunology, and performed multiple clinical trials to investigate the benefits<br />
<strong>of</strong> using adjuvant therapy with high-risk renal cancer.<br />
Brent KeitH HollenBecK, mD<br />
Faculty Appointment: Associate Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Degree: mD, 1997, indiana <strong>University</strong><br />
Residency: <strong>University</strong> <strong>of</strong> michigan, 1997–2003<br />
Fellowships: minimally invasive surgery, 2004,<br />
<strong>University</strong> <strong>of</strong> michigan medical center<br />
Urologic oncology, 2005, <strong>University</strong> <strong>of</strong> michigan<br />
medical center<br />
Clinical Interests: Dr. Hollenbeck has become increasingly specialized in the care<br />
<strong>of</strong> patients with prostate and bladder cancers. this has afforded him the ability<br />
to maintain his commitment to research while continuing to deliver cuttingedge,<br />
high-quality care. His research interests are policy-oriented and are focused<br />
squarely on understanding the upstream influences and downstream consequences<br />
<strong>of</strong> variation in physician practice style. His current initiatives include measuring the<br />
effects <strong>of</strong> physician financial incentives and identifying best practices for early stage<br />
bladder cancer. He is firmly committed to training the future leaders in urologic<br />
health services research. further, he strongly believes that populating the surgical<br />
specialties with health services researchers will yield long-term benefits to both our<br />
specialty and our patients.<br />
7
The CurrenT STaTe <strong>of</strong> urologiC onCology | iSSue 1 | winTer 2012<br />
cHeryl tAylore<br />
lee, mD<br />
Faculty Appointment:<br />
Associate Pr<strong>of</strong>essor, Dr.<br />
robert H. and eva m. moyad<br />
Pr<strong>of</strong>essor, Department <strong>of</strong><br />
Urology<br />
Degree: mD, 1991, Albany<br />
medical college<br />
Residency: <strong>University</strong> <strong>of</strong><br />
michigan, 1997<br />
Fellowship: Urologic oncology, 2000, memorial sloan-<br />
Kettering cancer center, new york<br />
Clinical Interests: Bladder cancer, urethral cancer, pelvic<br />
tumors, and urothelial cancers <strong>of</strong> the upper tract.<br />
Research Interests: cancer survivorship, quality <strong>of</strong> life,<br />
and novel multidisciplinary treatment strategies for bladder<br />
cancer patients.<br />
for more than a decade, Dr. lee has dedicated her practice<br />
to the treatment <strong>of</strong> high-risk bladder cancer in a<br />
wide spectrum <strong>of</strong> patients spanning the range from early<br />
stage to locally advanced disease . this has been possible<br />
because <strong>of</strong> long-term partnerships with urologists, medical<br />
oncologists, and general healthcare providers. During<br />
this time, she has explored strategies to improve surgical<br />
and cancer outcomes and has worked to optimize quality<br />
<strong>of</strong> life in patients requiring radical surgery. she specializes<br />
in organ and nerve-preserving radical cystectomy in<br />
men and women, and performs a range <strong>of</strong> incontinent and<br />
continent urinary diversion that will suit the needs <strong>of</strong> the<br />
patient. in an effort to treat the whole patient and improve<br />
their cancer survivorship experience, she has recently<br />
focused greater attention to the physical and psychosocial<br />
impairments that patients experience after treatment.<br />
8<br />
UroloGic oncoloGy fAcUlty<br />
DAViD cHristoPHer miller, mD,<br />
mPH<br />
Faculty Appointment: Assistant Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Degrees: mD, 1999, Washington <strong>University</strong> school <strong>of</strong><br />
medicine, st. louis<br />
mPH, 2005, <strong>University</strong> <strong>of</strong> michigan school <strong>of</strong> Public<br />
<strong>Health</strong><br />
Residency: <strong>University</strong> <strong>of</strong> michigan, 2005<br />
Fellowships: Urologic oncology, 2008, <strong>University</strong> <strong>of</strong> california, los Angeles<br />
Urological <strong>Health</strong> services research, 2007, <strong>University</strong> <strong>of</strong> california, los Angeles/<br />
rAnD<br />
<strong>Health</strong> services research training Program, 2006, <strong>University</strong> <strong>of</strong> michigan<br />
Department <strong>of</strong> Urology<br />
Clinical Interests: Dr. miller’s clinical interests focus on providing high-quality and<br />
compassionate care for patients with urological cancers. He has extensive experience<br />
and particular expertise in performing minimally invasive surgical treatments<br />
for prostate and kidney cancer, including robotic-assisted radical prostatectomy,<br />
partial nephrectomy, and laparoscopic nephrectomy. He also performs focal and<br />
total cryosurgical ablation <strong>of</strong> the prostate as a minimally invasive treatment option<br />
for patients with prostate cancer, including those with radio-recurrent prostate<br />
cancer. His overarching emphasis is on partnering with patients, primary care<br />
physicians, and his colleagues in urology to achieve the best possible outcomes for<br />
patients with prostate and kidney cancer.<br />
Jeffrey scott montGomery, mD,<br />
mHsA<br />
Faculty Appointment: Assistant Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Degree: mD, 2001, columbia college <strong>of</strong> Physicians<br />
and surgeons<br />
mHsA, 2007 <strong>University</strong> <strong>of</strong> michigan school <strong>of</strong> Public<br />
<strong>Health</strong><br />
Residency: <strong>University</strong> <strong>of</strong> michigan, 2007<br />
Fellowship: Urologic oncology, 2008, <strong>University</strong> <strong>of</strong> texas mD Anderson cancer<br />
center<br />
Clinical Interests: Dr. montgomery’s clinical practice focuses on the diagnosis and<br />
treatment <strong>of</strong> bladder, prostate, kidney, penile and testicular cancers. His advanced<br />
training in urologic oncology and minimally invasive surgical techniques, such as<br />
robotic and laparoscopic surgery, allows him to deliver state-<strong>of</strong>-the-art care to his<br />
patients. He also conducts clinical research focused on the management <strong>of</strong> bladder,<br />
prostate and kidney cancers, including cost-analyses and health-related quality <strong>of</strong><br />
life outcomes.
JAmes eDWArD montie, mD<br />
Faculty Appointment: Pr<strong>of</strong>essor, Department <strong>of</strong><br />
Urology, Valassis Pr<strong>of</strong>essor <strong>of</strong> Urologic oncology,<br />
cancer center member<br />
Degree: mD, 1971, <strong>University</strong> <strong>of</strong> michigan<br />
Fellowship: Urologic oncology, 1979, memorial sloan-<br />
Kettering cancer center, new york<br />
Certifications: Urology 1978, American Board <strong>of</strong><br />
Urology<br />
UroloGic oncoloGy fAcUlty<br />
Clinical Interests: Dr. montie’s clinical interests comprise cancers <strong>of</strong> the bladder,<br />
kidney, and prostate. His research interests include active surveillance for prostate<br />
cancer, the identification <strong>of</strong> prostate cancer biomarkers, performing urinary diversions,<br />
and, most recently, health services research in urologic oncology. He has<br />
been active in the development <strong>of</strong> physician-led collaboratives for progress in quality<br />
<strong>of</strong> care and care delivery.<br />
teD AlBert sKolArUs, mD, mPH<br />
Faculty Appointment: Assistant Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Degrees: mD, 2003, Wayne state <strong>University</strong> school <strong>of</strong><br />
medicine<br />
mPH, 2010, <strong>University</strong> <strong>of</strong> michigan school <strong>of</strong> Public<br />
<strong>Health</strong><br />
Residency: Washington <strong>University</strong> school <strong>of</strong> medicine,<br />
2008, st. louis, missouri<br />
Fellowships: Urologic oncology, 2011, <strong>University</strong> <strong>of</strong> michigan<br />
<strong>Health</strong> services research, 2010, <strong>University</strong> <strong>of</strong> michigan, Department <strong>of</strong> Urology<br />
Research Interests: <strong>Health</strong> services and implementation research, improving quality<br />
<strong>of</strong> care for urologic malignancies<br />
Dr. skolarus provides urologic cancer care at the VA Ann Arbor <strong>Health</strong>care<br />
system. As part <strong>of</strong> the U-m Department <strong>of</strong> Urology and the VA center for<br />
clinical management research, he is part <strong>of</strong> a team <strong>of</strong> experts who work together<br />
with other physicians, nurses, and managers to test innovative solutions to health<br />
care challenges as well as to translate research into meaningful strategies and best<br />
practices. Dr. skolarus’ research interests aim to better understand the delivery <strong>of</strong><br />
prostate cancer survivorship care, support the ongoing needs <strong>of</strong> prostate cancer<br />
survivors and identify opportunities to improve care coordination among cancer<br />
specialists and primary care providers. His current projects focus on engaging<br />
patients and their primary care providers in prostate cancer survivorship care<br />
through tailored self-management strategies and guidelines.<br />
Alon ZADoK<br />
WeiZer, mD, ms<br />
Faculty Appointment:<br />
Assistant Pr<strong>of</strong>essor,<br />
Department <strong>of</strong> Urology,<br />
Director <strong>of</strong> the clinical<br />
Urologic research endeavor<br />
Degrees: mD, 1999, Baylor<br />
college <strong>of</strong> medicine, Houston,<br />
tX<br />
ms clinical research statistical Design and Analysis,<br />
2009, <strong>University</strong> <strong>of</strong> michigan<br />
Residency: Duke <strong>University</strong> medical center, 2005,<br />
Durham, north carolina<br />
Fellowships: Urologic oncology, 2006, <strong>University</strong> <strong>of</strong><br />
michigan<br />
minimally invasive surgery, 2007, <strong>University</strong> <strong>of</strong> michigan<br />
Clinical/Research Interests: Dr. Weizer brings expertise in<br />
minimally invasive urologic oncology procedures, including<br />
robotic-assisted partial nephrectomy, nephroureterectomy,<br />
distal ureterectomy, cystectomy, and prostatectomy.<br />
However, he is also pr<strong>of</strong>icient in the breadth <strong>of</strong> procedures<br />
in urologic oncology, utilizing the surgical approach<br />
(open, robotic, laparoscopic) and management regimen<br />
that is appropriate for a particular patient. His research<br />
interests include risk stratification <strong>of</strong> non-muscle invasive<br />
bladder cancer, the role <strong>of</strong> active surveillance in small<br />
renal masses, and understanding the outcomes <strong>of</strong> minimally<br />
invasive urologic oncology procedures. He currently<br />
directs cUre (clinical Urologic research endeavor),<br />
which comprises prospective clinical databases for a variety<br />
<strong>of</strong> urologic diseases, as well as a robust clinical trial<br />
program <strong>of</strong>fering cutting-edge care.<br />
9
The CurrenT STaTe <strong>of</strong> urologiC onCology | iSSue 1 | winTer 2012<br />
J. stUArt Wolf Jr., mD<br />
Faculty Appointment: Pr<strong>of</strong>essor and David A. Bloom<br />
Pr<strong>of</strong>essor <strong>of</strong> Urology, Department <strong>of</strong> Urology,<br />
co-director, michigan center for minimally invasive<br />
Urology<br />
Degree: mD, 1988, northwestern <strong>University</strong>, chicago<br />
Residency: <strong>University</strong> <strong>of</strong> california, 1994, san<br />
francisco, california<br />
Fellowship: Urology, 1996, Washington <strong>University</strong>, st.<br />
louis<br />
10<br />
UroloGic oncoloGy fAcUlty<br />
Clinical Interests: Dr. Wolf specializes in minimally invasive surgery <strong>of</strong> the kidney,<br />
ureter, and related organs. He performs such procedures as laparoscopy (surgery<br />
performed through small incisions with the aid <strong>of</strong> a telescope, and with or without<br />
robotic-assistance), endoscopy (a procedure using a telescope that is moved into<br />
the lumen <strong>of</strong> the urinary tract), and percutaneous routes ( a procedure conducted<br />
through a single small incision with the use <strong>of</strong> a non-visualizing “needle”). Dr.<br />
Wolf treats such common diseases as stones, obstructions, and various other noncancerous<br />
problems <strong>of</strong> the kidney and ureter, as well as cancers involving the kidney<br />
(kidney cancer) and the lining <strong>of</strong> the kidney and ureter (urothelial cancer). Dr.<br />
Wolf pioneered many <strong>of</strong> the treatments for kidney cancer in the state <strong>of</strong> michigan;<br />
he performed, for instance, the first laparoscopic radical nephrectomy and the first<br />
laparoscopic partial nephrectomy.<br />
Researchers<br />
mArK DAy, PhD<br />
Faculty Appointment:<br />
Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology and the<br />
<strong>University</strong> <strong>of</strong> michigan<br />
comprehensive cancer<br />
center<br />
Degree: PhD cellular and<br />
molecular Biology, 1992,<br />
Washington <strong>University</strong><br />
school <strong>of</strong> medicine<br />
Research Interests: Dr. Day’s laboratory focuses on the<br />
regulation <strong>of</strong> cell surface proteins in prostate and bladder<br />
cancer. recent findings from the Day lab indicate<br />
that these proteins are promising targets for therapeutic<br />
development to prevent the metastatic progression <strong>of</strong><br />
these tumors. Dr. Day has also trained a large number<br />
medical students, graduate students, urology residents<br />
and fellows who continue to pursue research careers in<br />
Urology and GU oncology.<br />
Jill A. mAcosKA,<br />
PhD<br />
Faculty Appointment:<br />
Pr<strong>of</strong>essor <strong>of</strong> Urology<br />
faculty, Programs<br />
in cancer Biology,<br />
computational medicine<br />
and Bioinformatics, and<br />
cellular and molecular<br />
Biology<br />
Degree: PhD, Biochemistry, 1988, city <strong>University</strong> <strong>of</strong><br />
new york (cUny)<br />
Fellowship: Harvard <strong>University</strong>, cambridge, mA,<br />
1989; michigan cancer foundation, Detroit, mi, 1991<br />
Clinical Interests: Dr. Jill macoska is performing laboratory<br />
studies in collaboration with Dr. Wolf to identify<br />
new biomarkers to predict renal cancer prognosis<br />
and response to therapy.
leADers AnD Best in UroloGic oncoloGy<br />
the <strong>University</strong> <strong>of</strong> michigan Hospital and <strong>Health</strong> system is in the top 5% nationally in these procedures.<br />
UniVersity <strong>of</strong> micHiGAn comPreHensiVe cAncer center<br />
At the <strong>University</strong> <strong>of</strong> michigan comprehensive cancer<br />
center, our goal is to provide our patients with strategies<br />
to optimize their overall health and wellness—now and in<br />
the future.<br />
Our physicians are available<br />
Monday - Friday, 8 am to 5pm<br />
Average wait time is one week*<br />
*Wait times may be longer if a specific physician may be requested<br />
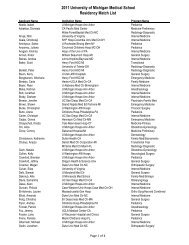
2010 QUAlity metrics<br />
Procedure Median Length Average Blood Loss Surgical Volume<br />
<strong>of</strong> Stay (days) (cc)<br />
radical Prostatectomy 1 149 286<br />
robotic cystectomy 8 380 35<br />
open cystectomy 7 555 88<br />
endoscopic Bladder cancer Procedures n/A n/A 329<br />
laparoscopic Partial nephrectomy 2 269 29<br />
open Partial nephrectomy 3 374 35<br />
robotic Partial nephrectomy 2 336 56<br />
radical nephrectomy lap 3 237 33<br />
robotic 3 331 5<br />
open 5.5 994 19<br />
caval tumor thrombus 7 1464 8<br />
nUmBer <strong>of</strong> UroloGic oncoloGy Visits<br />
Type <strong>of</strong> Visit 2009 2010<br />
new Patient Visits 2,293 2,338<br />
total Visits 12,737 13,373<br />
To make an appointment:<br />
call (734) 647-6743<br />
cancer Answer line (800)865-1125<br />
referal line (734) 763-9114, 1 (800) 211-8181<br />
1500 e. medical center Dr.<br />
Ann Arbor, mi 48109-5913<br />
room 229 reception D, level B1-229<br />
Phone: (734) 647-8903 fax: (734) 647-8860<br />
www.med.umich.edu/cancer<br />
11
the MIChIGAn dIFFeRenCe<br />
department <strong>of</strong> urology<br />
3875 taubman Center<br />
1500 e. Medical Center dr., sPC 5330<br />
Ann Arbor, MI 48109-5330<br />
HOld tHe dAtes!<br />
<strong>Health</strong> services research symposium:<br />
sept 6-7, 2012<br />
this symposium will bring together leading clinicians and researchers<br />
from within and outside urology to discuss the current and future impact<br />
<strong>of</strong> health services and outcomes research in urology, including its relevance<br />
for patients, policymakers, payers, and practicing urologists. We<br />
anticipate a novel and provocative program that will include lectures and<br />
participation from Peter Carroll, Mark litwin, Joel nelson, david Penson<br />
Khaled Hafez, MD<br />
Associate Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Brent Hollenbeck, MD<br />
Associate Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Cheryl T. Lee, MD<br />
Dr . Robert & Eva Moyad<br />
Research Pr<strong>of</strong>essor, Associate<br />
Pr<strong>of</strong>essor, Department <strong>of</strong><br />
Urology<br />
David C. Miller, MD, MPH<br />
Assistant Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
Jeffrey Scott Montgomery, MD<br />
Assistant Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
James E. Montie, MD<br />
Pr<strong>of</strong>essor, Department <strong>of</strong><br />
Urology<br />
Valassis Pr<strong>of</strong>essor <strong>of</strong> Urologic<br />
Oncology<br />
Alon Weizer, MD<br />
Assistant Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Urology<br />
J. Stuart Wolf, Jr., MD<br />
David A . Bloom Pr<strong>of</strong>essor <strong>of</strong><br />
Urology<br />
COntACt us<br />
If you have any questions regarding the Renal<br />
Carcinoma database, please contact Rick saur<br />
at 734-615-5446.<br />
to learn more about giving to the department <strong>of</strong><br />
urology, please contact steffanie samuels, director <strong>of</strong><br />
development, at 734-615-9843 or send an e-mail to<br />
ssamuels@umich.edu.<br />
and other thought leaders in the field. this edition <strong>of</strong> The Current State <strong>of</strong> Urologic Oncology<br />
at U-M was compiled by department <strong>of</strong> urology<br />
students/researchers: stephanie durphey, Michael<br />
Coelho, Peter Blank, and Will Kane.<br />
KiDney cAncer reseArcH teAm<br />
Executive Officers <strong>of</strong><br />
the <strong>University</strong> <strong>of</strong> <strong>Michigan</strong> <strong>Health</strong> <strong>System</strong><br />
ora Hirsch Pescovitz, executive Vice President for medical Affairs;<br />
James o. Woolliscr<strong>of</strong>t, Dean, U-m medical school; Douglas strong,<br />
chief executive <strong>of</strong>ficer, U-m Hospitals and <strong>Health</strong> centers; Kathleen<br />
Potempa, Dean, school <strong>of</strong> nursing<br />
The Regents <strong>of</strong> the <strong>University</strong> <strong>of</strong> <strong>Michigan</strong><br />
Julia Donovan Darlow, laurence B. Deitch, Denise ilitch, olivia P.<br />
maynard, Andrea fischer newman, Andrew c. richner, s. martin<br />
taylor, Katherine e. White,<br />
mary sue coleman (ex <strong>of</strong>ficio)<br />
the <strong>University</strong> <strong>of</strong> michigan is a non-discriminatory, affirmative action<br />
employer.<br />
copyright © 2012<br />
the regents <strong>of</strong> the <strong>University</strong> <strong>of</strong> michigan<br />
Ann Arbor, michigan, 48109<br />
mmD 110410