Double Plus.indd - CAMAF
Double Plus.indd - CAMAF
Double Plus.indd - CAMAF
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
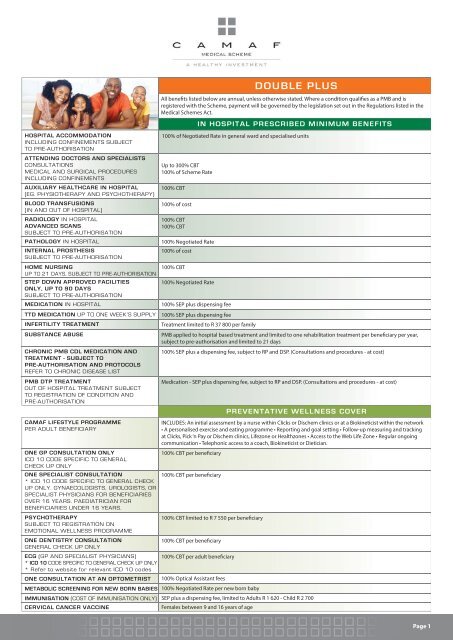
HOSPITAL ACCOMMODATION<br />
INCLUDING CONFINEMENTS SUBJECT<br />
TO PRE-AUTHORISATION<br />
ATTENDING DOCTORS AND SPECIALISTS<br />
CONSULTATIONS<br />
MEDICAL AND SURGICAL PROCEDURES<br />
INCLUDING CONFINEMENTS<br />
AUXILIARY HEALTHCARE IN HOSPITAL<br />
(EG. PHYSIOTHERAPY AND PSYCHOTHERAPY)<br />
BLOOD TRANSFUSIONS<br />
(IN AND OUT OF HOSPITAL)<br />
RADIOLOGY IN HOSPITAL<br />
ADVANCED SCANS<br />
SUBJECT TO PRE-AUTHORISATION<br />
PATHOLOGY IN HOSPITAL<br />
INTERNAL PROSTHESIS<br />
SUBJECT TO PRE-AUTHORISATION<br />
HOME NURSING<br />
UP TO 21 DAYS, SUBJECT TO PRE-AUTHORISATION<br />
STEP DOWN APPROVED FACILITIES<br />
ONLY, UP TO 90 DAYS<br />
SUBJECT TO PRE-AUTHORISATION<br />
MEDICATION IN HOSPITAL<br />
TTD MEDICATION UP TO ONE WEEK’S SUPPLY<br />
INFERTILITY TREATMENT<br />
SUBSTANCE ABUSE<br />
CHRONIC PMB CDL MEDICATION AND<br />
TREATMENT - SUBJECT TO<br />
PRE-AUTHORISATION AND PROTOCOLS<br />
REFER TO CHRONIC DISEASE LIST<br />
PMB DTP TREATMENT<br />
OUT OF HOSPITAL TREATMENT SUBJECT<br />
TO REGISTRATION OF CONDITION AND<br />
PRE-AUTHORISATION<br />
<strong>CAMAF</strong> LIFESTYLE PROGRAMME<br />
PER ADULT BENEFICIARY<br />
DOUBLE PLUS<br />
All benefi ts listed below are annual, unless otherwise stated. Where a condition qualifi es as a PMB and is<br />
registered with the Scheme, payment will be governed by the legislation set out in the Regulations listed in the<br />
Medical Schemes Act.<br />
IN HOSPITAL PRESCRIBED MINIMUM BENEFITS<br />
100% of Negotiated Rate in general ward and specialised units<br />
Up to 300% CBT<br />
100% of Scheme Rate<br />
100% CBT<br />
100% of cost<br />
100% CBT<br />
100% CBT<br />
100% Negotiated Rate<br />
100% of cost<br />
100% CBT<br />
100% Negotiated Rate<br />
100% SEP plus dispensing fee<br />
100% SEP plus dispensing fee<br />
Treatment limited to R 37 800 per family<br />
PMB applied to hospital based treatment and limited to one rehabilitation treatment per benefi ciary per year,<br />
subject to pre-authorisation and limited to 21 days<br />
100% SEP plus a dispensing fee, subject to RP and DSP. (Consultations and procedures - at cost)<br />
Medication - SEP plus dispensing fee, subject to RP and DSP. (Consultations and procedures - at cost)<br />
PREVENTATIVE WELLNESS COVER<br />
INCLUDES: An initial assessment by a nurse within Clicks or Dischem clinics or at a Biokineticist within the network<br />
• A personalised exercise and eating programme • Reporting and goal setting • Follow-up measuring and tracking<br />
at Clicks, Pick ‘n Pay or Dischem clinics, Lifezone or Healthzones • Access to the Web Life Zone • Regular ongoing<br />
communication • Telephonic access to a coach, Biokineticist or Dietician.<br />
ONE GP CONSULTATION ONLY<br />
100% CBT per benefi ciary<br />
ICD 10 CODE SPECIFIC TO GENERAL<br />
CHECK UP ONLY<br />
ONE SPECIALIST CONSULTATION<br />
100% CBT per benefi ciary<br />
* ICD 10 CODE SPECIFIC TO GENERAL CHECK<br />
UP ONLY. GYNAECOLOGISTS, UROLOGISTS, OR<br />
SPECIALIST PHYSICIANS FOR BENEFICIARIES<br />
OVER 16 YEARS. PAEDIATRICIAN FOR<br />
BENEFICIARIES UNDER 16 YEARS.<br />
PSYCHOTHERAPY<br />
100% CBT limited to R 7 550 per benefi ciary<br />
SUBJECT TO REGISTRATION ON<br />
EMOTIONAL WELLNESS PROGRAMME<br />
ONE DENTISTRY CONSULTATION<br />
100% CBT per benefi ciary<br />
GENERAL CHECK UP ONLY<br />
ECG (GP AND SPECIALIST PHYSICIANS)<br />
100% CBT per adult benefi ciary<br />
* ICD 10 CODE SPECIFIC TO GENERAL CHECK UP ONLY<br />
* Refer to website for relevant ICD 10 codes<br />
ONE CONSULTATION AT AN OPTOMETRIST 100% Optical Assistant fees<br />
METABOLIC SCREENING FOR NEW BORN BABIES 100% Negotiated Rate per new born baby<br />
IMMUNISATION (COST OF IMMUNISATION ONLY) SEP plus a dispensing fee, limited to Adults R 1 620 - Child R 2 700<br />
CERVICAL CANCER VACCINE<br />
Females between 9 and 16 years of age<br />
Page 1
BASIC AND ADVANCED RADIOLOGY<br />
OUT OF HOSPITAL<br />
Must be performed by a registered radiologist,<br />
on referral from medical practitioner only.<br />
Advanced scans subject to pre-authorisation<br />
PATHOLOGY OUT OF HOSPITAL<br />
Performed by a registered pathologist and<br />
referred by a medical practitioner<br />
POST-HOSPITALISATION UP TO 90 DAYS<br />
MEDICATION FOR ADDITIONAL CHRONIC<br />
CONDITIONS<br />
(SUBJECT TO PRE-AUTHORISATION) REFER TO<br />
ADDITIONAL CHRONIC CONDITIONS LIST<br />
EXTERNAL APPLIANCES<br />
IN AND OUT OF HOSPITAL<br />
PURCHASE, HIRE AND MAINTENANCE<br />
HEARING AIDS - 1 CLAIM PER 3 YEAR<br />
CYCLE FOR OVER 16 YEARS OF AGE<br />
YOUNGER THAN 16 YEARS OF AGE<br />
- 18 MONTH CYCLE<br />
WHEELCHAIRS - 3 YEAR CYCLE<br />
INSULIN PUMPS, SUBJECT TO<br />
PRE-AUTHORISATION - 4 YEAR CYCLE<br />
NETCARE 911<br />
EMERGENCY SERVICES<br />
DAY TO DAY BENEFITS<br />
BENEFITS BELOW ARE SUBJECT TO THE<br />
OVERALL ANNUAL LIMIT<br />
GP’S, SPECIALISTS AND DENTISTS<br />
CONSULTATIONS, PROCEDURES AND<br />
RADIOLOGY PERFORMED BY THESE<br />
PRACTITIONERS; BASIC DENTISTRY<br />
ACUTE MEDICATION<br />
INCLUDING INJECTIONS AND MATERIALS<br />
NON-DSP VISITS TO DOCTORS’ ROOMS<br />
CASUALTY AND OUT PATIENT<br />
TREATMENT AT A HOSPITAL<br />
ALL MEDICATIONS WILL BE PAID OUT OF<br />
ACUTE MEDICATION BENEFIT<br />
HOME NURSING<br />
AUXILIARY HEALTH<br />
AUDIOLOGY, CHIROPRACTORS, OPTICIANS,<br />
HOMEOPATHS, OCCUPATIONAL THERAPY,<br />
PHYSIOTHERAPISTS, PODIATRY AND SPEECH<br />
THERAPY<br />
ADVANCED DENTISTRY<br />
CROWNS, BRIDGES AND DENTURES<br />
ANTE-NATAL CLASSES SUBJECT TO<br />
ENROLMENT ON THE MOTHER-TO-BE PROGRAMME<br />
SPECTACLES AND LENSES<br />
FROM OPTOMETRIST ONLY<br />
ANNUAL BENEFIT, UNLESS OTHERWISE<br />
STATED<br />
100% CBT<br />
100% Negotiated Rate<br />
300% CBT for attending practitioners<br />
100% CBT for auxiliary services<br />
100% SEP plus a dispensing fee, subject to RP and DSP<br />
Consultations 100% CBT<br />
Unlimited<br />
Subject to Netcare 911 authorisation<br />
OTHER BENEFITS<br />
(per Beneficiary) SUBJECT TO THE ANNUAL OVERALL BENEFIT LIMIT<br />
Annual Overall Limits<br />
Adult R 8 000<br />
Child<br />
80% CBT<br />
R 5 590<br />
80% SEP plus a dispensing fee<br />
Not applicable<br />
80% CBT<br />
80% CBT up to 21 days<br />
80% CBT<br />
80% CBT limited to:<br />
Mo R 8 000<br />
M1 R 11 660<br />
M2+ R 15 660<br />
Subject to Annual Benefi ts<br />
DOUBLE PLUS<br />
OTHER BENEFITS<br />
(per Beneficiary) NOT SUBJECT TO THE ANNUAL OVERALL BENEFIT LIMIT<br />
100% of cost subject to the overall limit of R43 200 per benefi ciary and subject to the following sub-limits:<br />
Hearing Aids: R 43 200<br />
Wheelchairs for Quadriplegics: R 43 200<br />
Standard Wheelchairs: R 27 550<br />
Insulin Pumps: R 28 080<br />
Other external appliances: R 9 180<br />
• Baby Apnoea monitors: R 1 600<br />
• Breast pumps: R 2 700<br />
OTC MEDICATION<br />
80% SEP plus a dispensing fee, limited to R 1 190 per benefi ciary<br />
LASER K<br />
80% CBT limited to R 3 000 per eye<br />
NO APPROVAL FOR SURGERY WHERE SPECTACLES<br />
OBTAINED IN PREVIOUS 12 MONTHS<br />
ANTE-NATAL FOETAL SCANS PER PREGNANCY 3 Scans at 80% CBT<br />
80% CBT limited to R 1 190 per pregnancy<br />
Consultion: See Preventative Wellness<br />
Add ons R 700<br />
Single Vision R 700 OR<br />
Bifocal R 1 900 OR<br />
Varifocal R 2 920 AND<br />
Frames R 1 950 OR<br />
Contact lenses R 2 700<br />
Lenses, frames etc 80% Optical Assistant Fees<br />
Page 2
MONTHLY RISK CONTRIBUTION Adult R 2 040<br />
Child R 1 240<br />
MONTHLY MSA CONTRIBUTION<br />
Adult R 260<br />
Child R 173<br />
TOTAL MONTHLY CONTRIBUTION<br />
Adult R 2 300<br />
Child R 1 413<br />
DOUBLE PLUS<br />
MONTHLY CONTRIBUTION RATES<br />
GLOSSARY<br />
* More details available on the website www.camaf.co.za - for full explanations, consult the Registered Rules<br />
ADULT<br />
CBT<br />
CDL<br />
CML/ Formulary<br />
CHILD<br />
DISPENSING FEES<br />
DSP<br />
DTP<br />
ICD 10 CODE<br />
METABOLIC SCREENING Newborn screening whereby rare disorders are detected by a blood test done 48-72 hours after birth.<br />
MMAP<br />
Maximum Medical Aid Price - is a reference price model and determines the maximum medical scheme price that medical schemes will reimburse<br />
for an interchangeable multi-source pharmaceutical product (generic) on the relevant option. MMAP applies to all options for chronic medication.<br />
MSA<br />
NEGOTIATED RATE<br />
PMB<br />
PRE-AUTHORISATION<br />
PROTOCOL<br />
RISK CONTRIBUTIONS<br />
RP<br />
SALARY<br />
SCHEME RATE<br />
SEP<br />
TTO<br />
Refers to the member and dependants who are 22 or older at any time in the year of cover.<br />
<strong>CAMAF</strong> Base Tariff - the maximum rate paid by the Scheme to providers of healthcare services, based on 2009 RPL (Medical Aid) rates,<br />
increased annually by CPI. Tariff diff ers per type of service provider and % paid on diff erent options.<br />
Chronic Disease List - the list of PMB’s includes 27 common chronic conditions called CDL’s. Schemes must provide cover for the diagnosis,<br />
treatment and care of these conditions. Members must register their conditions to qualify for benefi ts. Schemes can provide protocols in terms of<br />
the range (RP and Formularies) and delivery of medication (DSP’s).<br />
Condition Medicine List - once a patient’s chronic condition has been registered, a patient will have access to the CML. This is a list of drugs, appropriate<br />
for the condition, that do not require authorisation. This is maintained by the Scheme and diff ers per Option. Reference pricing may still apply.<br />
Refers to a dependant who is younger than an adult, as defi ned above.<br />
Fee negotiated by the Scheme with Network pharmacies and added to SEP.<br />
The network of service providers contracted to provide healthcare services to members, eg. Diabetes programme (CDE), HIV programme<br />
(LifeSense) PPN for optical benefi ts on First Choice and Network Choice, Pharmacy networks for all chronic medications and Netcare hospital group<br />
for Network Choice hospital admissions.<br />
The regulations to the Medical Schemes Act in Annexure A provide a list of conditions identifi ed as Prescribed Minimum Benefi ts. The List is in<br />
the form of Diagnosis Treatment Pairs (DTP’s). A DTP links a specifi c diagnosis to a treatment/procedure and therefore broadly indicates how<br />
each of the 270 PMB conditions should be treated. These treatment pairs cover serious and acute medical problems that include the cost of<br />
diagnosis, treatment and care of these conditions.<br />
Stands for International Classifi cation of Diseases and Related Health Problems (10th revision). It is a coding system developed by the World<br />
Health Organisation (WHO) that translates the written description of medical and health information into standard codes, e.g. Jo3.9 is a ICD-10<br />
code for acute tonsillitis (unspecifi ed) and G40.9 denotes epilepsy (unspecifi ed). These codes are used to inform medical schemes about what<br />
conditions their members were treated for so that claims can be paid from the correct benefi t.<br />
Medical Savings Account - accrued monthly but the annualised amount of savings is available immediately and can be used for :<br />
• top up on cost of service charged by a doctor<br />
• extension when an overall benefi t has been exceeded<br />
• exclusion from benefi ts<br />
This is the rate, negotiated by the scheme with the service provider/group of service providers, eg. hospitals and pathologists.<br />
Prescribed Minimum Benefi ts - as set down in the Medical Schemes Act, 1998. Medical schemes have to cover the costs related to the<br />
diagnosis, treatment and care of:<br />
• Any emergency medical condition<br />
• A limited set of 270 medical conditions (Defi ned in DTP’s)<br />
• 27 chronic conditions defi ned in the CDL<br />
• These costs may not be paid from member’s savings benefi t and cost saving measures can be used by way of utilising DSP’s, Reference<br />
Pricing and Formularies.<br />
A member must obtain prior approval for an intended admission to hospital. Failure to pre-authorise could result in wholly or partly<br />
disallowing the claim or imposing a penalty of 20% of related accounts up to a maximum of R 2 500. Emergency treatment is not subject to<br />
Pre-authorisation but members should notify the Scheme as soon as possible after the event.<br />
Means a set of guidelines in relation to diagnostic testing and treatments for specifi c conditions and includes, but is not limited to, clinical<br />
practice guidelines, standard treatment guidelines and disease management guidelines.<br />
Those funds allocated to the overall pool of funds for the payment of all claims other than those paid from the MSA.<br />
Reference pricing is the maximum price for which the Scheme will be liable for specifi c medicine or classes of medicine, listed on the<br />
Scheme’s Condition Medicine List (CML). The reference price varies per option and where a drug is above the reference price it is indicated<br />
that a co-payment will apply. This includes MMAP.<br />
Total cost to company prior to deductions.<br />
The maximum rate paid by the scheme to providers of healthcare services, based on SAMA (Private) rates, increased annually by CPI. Tariff<br />
diff ers per type of service provider and % paid on diff erent options.<br />
Single Exit Price - nationally applied pricing for medication as determined by the Department of Health and the pharmaceutical manufacturers.<br />
“To Take Out” - medication supplied by the hospital for use after the date of discharge from hospital - limited to a 7 day supply.<br />
Page 3