Insulin administration - Yeovil District Hospital NHS Foundation Trust
Insulin administration - Yeovil District Hospital NHS Foundation Trust
Insulin administration - Yeovil District Hospital NHS Foundation Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
PROTOCOL ON THE SAFE<br />
ADMINISTRATION OF INSULIN IN<br />
HOSPITAL<br />
Version number 1 Version date: December 2010<br />
Author Diabetes Nurse Specialist<br />
First approval date 19 January 2011<br />
Forum approved Diabetes Team Meeting (adult care)<br />
Approved by Diabetes Team<br />
Next review date January 2013
Contents<br />
1. Purpose 2<br />
2. Introduction 2<br />
3. Prescribing of insulin 2<br />
4. Administration of insulin 2<br />
5. Self administering 3<br />
6. Mixing insulin 3<br />
7. <strong>Insulin</strong> delivery devices 3<br />
8. Timing of insulin injections 4<br />
9. Injection sites and injection technique 4<br />
10. Storage of insulin 5<br />
Annex A Substitutions if a patients usual insulin is unavailable 6<br />
Appendix 1 <strong>Insulin</strong> delivery devices 7<br />
1. Purpose<br />
1
1.1 The purpose of this protocol is to ensure that all insulin is administered safely and<br />
in accordance with best practice guidelines.<br />
2. Introduction<br />
2.1 As a result of significant numbers of patient safety incidents involving insulin the<br />
National Patient Safety Agency (NPSA) issued a Rapid Response Report in June<br />
2010 regarding the safer <strong>administration</strong> of insulin (NPSA/2010./RRR013).<br />
2.2 The two most common errors identified were:<br />
the inappropriate use of non-insulin (IV) syringes, which were marked in ml<br />
and not insulin units; and<br />
the use of abbreviations such as “U” or “IU” for units.<br />
2.3 This protocol aims to reduce the risk of harm to inpatients which may be caused by<br />
the improper use of insulin.<br />
2.4 A mandatory e-learning programme is also available to provide further training for<br />
those involved in the prescribing, preparation and administering of insulin from:<br />
www.diabetes.nhs.uk/safeuseofinsulin<br />
3. Prescribing of insulin<br />
3.1 The insulin prescription must be checked before each dose of insulin is given; it<br />
must be dated and signed.<br />
3.2 The name of each insulin must be written out in full, followed by the word “<strong>Insulin</strong>”<br />
with the dose prescribed with the words “units” spelt in full and not abbreviated as<br />
“U” or “IU”.<br />
3.3 Any abbreviation is unacceptable as it may be interpreted as a zero, with the<br />
consequence of an insulin overdose.<br />
3.4 If a patients’ usual insulin is not available see Annex A for a suitable substitution<br />
which may be used until the patients own insulin can be obtained.<br />
4. Administration of insulin<br />
4.1 The <strong>Yeovil</strong> <strong>District</strong> <strong>Hospital</strong> <strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong> Medicines Management Policy,<br />
available on the intranet, should be adhered to at all times with regard to the<br />
<strong>administration</strong> of all medicines.<br />
4.2 All patients with diabetes who usually administer their own insulin should be<br />
enabled to continue doing so, if their condition permits this – see below.<br />
5. Self administering<br />
2
5.1 The section on self medication within the <strong>Trust</strong>’s Medicines Management Policy<br />
must be adhered to; this includes appropriate, documented assessment of the<br />
patient for suitability for self medication. The patients ability to self medicate may<br />
alter several times during one admission and this should be documented on the<br />
assessment.<br />
5.2 Any proposed changes made to patients’ insulin doses should be communicated to<br />
the patient immediately.<br />
5.3 Some patients may give variable doses of quick acting insulin and adjust doses of<br />
longer acting insulin. The <strong>Insulin</strong> prescription chart should reflect this practice.<br />
5.4 Illness and admission to hospital are stressful events and blood glucose levels may<br />
rise as a result. Patients who are used to adjusting their own insulin doses should<br />
be encouraged to continue to do so as necessary.<br />
5.5 If patients are not mobile enough to access a ward sharps container they should be<br />
provided with a 1 litre sharps container at the bedside, in order to minimise the risk<br />
of sharps accident.<br />
6. Mixing insulin<br />
6.1 Many of the commonly used insulins are premixed e.g. Novo Mix 30. Some older<br />
insulin regimens involve the mixing of two different insulins in a syringe prior to<br />
<strong>administration</strong>. Soluble, or short acting insulins, such as Humulin S or Actrapid,<br />
and rapid acting insulins, such as Humalog or NovoRapid, must only be mixed<br />
with an isophane insulin, such as Humulin I or Insulatard.<br />
6.2 Under no circumstances should soluble insulins be mixed with Levemir or<br />
Lantus, or insulin zinc suspensions e.g. Hypurin Bovine Protamine Zinc.<br />
6.3 <strong>Insulin</strong> suspensions (cloudy insulins) must be mixed thoroughly by gently rolling -<br />
not vigorously as this will destroy the insulin molecule before drawing up. Contact<br />
the Diabetes Department on ext 4517 should you need further advice before<br />
mixing or giving insulins.<br />
7. <strong>Insulin</strong> delivery devices<br />
7.1 Subcutaneous insulin must be delivered via insulin syringes or with a commercial<br />
<strong>Insulin</strong> pen. Under no circumstances must intravenous syringes be used to<br />
measure and administer insulin doses.<br />
7.2 The standard insulin syringe used by the <strong>Trust</strong> is the BD 0.5 ml insulin syringe with<br />
an integrated 8mm needle. The ‘twin bin’ service will ensure that each clinical area<br />
has a sufficient supply of insulin syringes. (These must be stored separately from<br />
the 1ml IV syringes). <strong>Insulin</strong> pen needles can be obtained from pharmacy.<br />
7.3 Commercial insulin pens are available on prescription for people with diabetes<br />
using insulin therapy. If a patient starts insulin treatment whilst in hospital the<br />
3
Diabetes Specialist Nurses will supply appropriate pens (if using a disposable pen<br />
these will be dispensed from pharmacy). If the patient is already using insulin pens,<br />
they will need to bring their own into hospital.<br />
7.4 A chart showing currently available insulin delivery devices can be found in<br />
Appendix 2.<br />
8. Timing of insulin injections<br />
8.1 Refer to the chart below for specific timings for different insulins.<br />
8.2 Levemir and Lantus insulins should be given within ½ an hour of the same time(s)<br />
each day.<br />
TIMING OF DIFFERENT TYPES OF INSULIN IN RELATION TO FOOD<br />
To be given just before or<br />
immediately after food<br />
intake<br />
Rapid acting insulin<br />
analogue<br />
NovoRapid<br />
Humalog<br />
Apidra<br />
Mixed insulin using a rapid<br />
acting insulin analogue<br />
Humalog Mix25<br />
Humalog Mix50<br />
NovoMix 30<br />
To be given 20 - 30<br />
minutes before food<br />
intake<br />
Short acting soluble insulin<br />
Actrapid<br />
Humulin S<br />
Hypurin Porcine Neutral<br />
Mixed insulin using short<br />
acting soluble insulin<br />
Humulin M3<br />
Hypurin Porcine 30/70 Mix<br />
9. Injection sites and injection technique<br />
Administration unrelated<br />
to food intake<br />
Medium acting insulin<br />
Insulatard<br />
Humulin I<br />
Hypurin Porcine Isophane<br />
Long acting insulin<br />
Hypurin Bovine Protamine Zinc<br />
Long acting insulin analogue<br />
Lantus<br />
Levemir<br />
9.1 <strong>Insulin</strong> must be injected into the subcutaneous fat of the abdomen, thighs or<br />
buttocks. These are the best sites for injection as they have a layer of fat to absorb<br />
the insulin just under the skin.<br />
9.2 Ideally, insulin should be injected into the same general area at the same time<br />
each day. For example, an individual using a twice daily regimen of Novomix 30<br />
may inject into the abdomen in the morning and the thighs before the evening<br />
meal. If the patient is not self administering insulin, a record should be made of the<br />
injection site used.<br />
9.3 To avoid lipohypertrophy (fatty lumps at insulin injections sites), which cause<br />
erratic insulin absorption, the same square inch of flesh should not be used again<br />
for a week. If you suspect a patient has lipohypertrophy please ask the Diabetes<br />
Nurse Specialist to review the patient as this may often be a cause of erratic<br />
control.<br />
9.4 Always inject at an angle of 90 <br />
using either an 8mm insulin syringe or the patients<br />
own pen needles – the length of these may vary depending on patient size.<br />
4
9.5 Always ensure the injection is given into a “pinch up” skin fold (If the patient is<br />
using 5 or 6mm needles this is not necessary).<br />
9.6 A new syringe or pen needle must be used for each injection.<br />
9.7 If using an insulin pen the needle should be removed after each injection.<br />
10. Storage of insulin<br />
10.1 For those patients who are self administering their insulin, the insulin and device<br />
must be clearly labelled with the patient’s name and hospital number. On discharge<br />
they should be taken home by the patient or returned to pharmacy.<br />
10.2 Stock insulin must be stored in a locked refrigerator. Patients spare insulin<br />
cartridges or disposable pens should be stored as above with the patients name<br />
recorded on the box.<br />
10.3 Disposable and reusable insulin pens in use must not be stored in the refrigerator.<br />
10.4 <strong>Insulin</strong> may be kept for 28 days not above 25 C and away from direct heat and light.<br />
The date from which it is first used should be noted, after 28 days it must be<br />
discarded.<br />
5
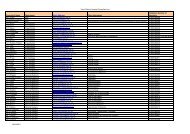
Substitutions if a patients usual insulin is unavailable<br />
<strong>Insulin</strong>s within the same colour band are interchangeable. Please ensure on discharge that the patient has their usual insulin<br />
with the correct pen.<br />
<strong>Insulin</strong> Type <strong>Insulin</strong> Name<br />
Rapid Analogue a) Humalog (Lispro)<br />
b) NovoRapid (Aspart)<br />
c) Apidra (Glulisine)<br />
Short Soluble a) Humulin S<br />
b) Actrapid<br />
c) Insuman Rapid<br />
Mixed Analogue<br />
(rapid and<br />
protamine<br />
suspension)<br />
Mixed Soluble &<br />
Isophane<br />
Intermediate<br />
Isophane<br />
Long-acting<br />
Analogue<br />
a) Humalog Mix 25<br />
b) Novomix 30<br />
c) non available<br />
a) Humulin M3<br />
b) Mixtard 30<br />
c) Insuman Comb 25<br />
a) Humulin I<br />
b) Insulatard<br />
c) Insuman basal<br />
a) non available<br />
b) Levemir (Detemir)<br />
c) Lantus (Glargine)<br />
Pharmaceutical<br />
Company<br />
a) Eli Lilly<br />
b) Novo Nordisk<br />
c) Aventis<br />
a) Eli Lilly<br />
b) Novo Nordisk<br />
c) Aventis<br />
a) Eli Lilly<br />
b) Novo Nordisk<br />
c) Aventis<br />
a) Eli Lilly<br />
b) Novo Nordisk<br />
c) Aventis<br />
a) Eli Lilly<br />
b) Novo Nordisk<br />
c) Aventis<br />
a) Eli Lilly<br />
b) Novo Nordisk<br />
c) Aventis<br />
Administration Action<br />
Up to 15 mins before, during<br />
or just after meals<br />
Action onset 15 mins<br />
Peak 2 hours<br />
Duration up to 5 hours<br />
15 - 30 mins prior to meals Action onset 30 - 60 mins<br />
Peak 2 - 4 hours<br />
Duration up to 8 hours<br />
Up to 15 mins before, during<br />
or just after breakfast and<br />
evening meal<br />
15 - 30 mins prior to<br />
breakfast and evening meal<br />
Early morning and/or late<br />
evening<br />
May be administered without<br />
food<br />
Usually – early morning or<br />
late evening at a set time.<br />
May be administered without<br />
food<br />
As rapid analogue and<br />
protamine<br />
suspension similar to action of<br />
intermediate isophane<br />
(mixed together)<br />
As short soluble and<br />
intermediate isophane<br />
mixed together<br />
Action onset 60 - 90 mins<br />
Peak 4 - 12 hours<br />
Duration up to 24 hours<br />
Action onset 3 - 4 hours<br />
Peak up to 14 hours<br />
Duration up to 24 hours<br />
If a patient is admitted on an insulin not listed above, please contact the Department of Diabetes on ext. 4517 for advice<br />
6
Appendix 2<br />
7