Spirometry - FMF
Spirometry - FMF
Spirometry - FMF
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
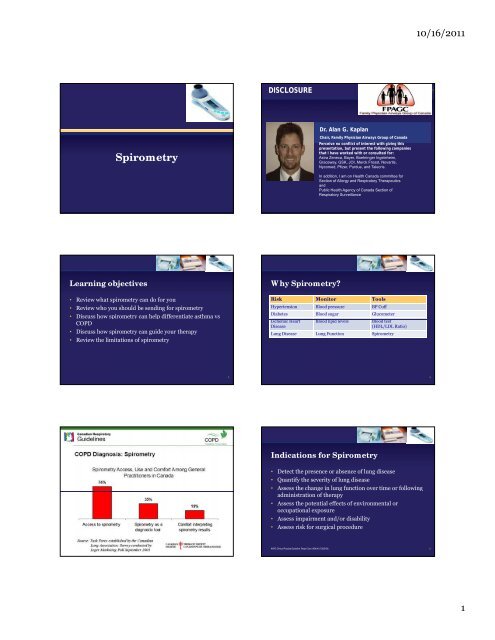
<strong>Spirometry</strong><br />
Learning objectives<br />
• Review what spirometry can do for you<br />
• Review who you should be sending for spirometry<br />
• Discuss how spirometry can help differentiate asthma vs<br />
COPD<br />
• Discuss how spirometry can guide your therapy<br />
• Review the limitations of spirometry<br />
3<br />
DISCLOSURE<br />
Why <strong>Spirometry</strong>?<br />
Dr. Alan G. Kaplan<br />
Chair, Family Physician Airways Group of Canada<br />
Perceive no conflict of interest with giving this<br />
presentation presentation, but present the following companies<br />
that I have worked with or consulted for:<br />
Astra Zeneca, Bayer, Boehringer Ingeleheim,<br />
Graceway, GSK, JOI, Merck Frosst, Novartis,<br />
Nycomed, Pfizer, Purdue, and Talecris.<br />
In addition, I am on Health Canada committee for<br />
Section of Allergy and Respiratory Therapeutics<br />
and<br />
Public Health Agency of Canada Section of<br />
Respiratory Surveillance<br />
Risk Monitor Tools<br />
Hypertension Blood pressure BP Cuff<br />
Diabetes Blood sugar Glucometer<br />
IIschemic h i Heart H t Bl Blood d lipid li id levels l l Bl Blood d test t t<br />
Disease<br />
(HDL/LDL Ratio)<br />
Lung Disease Lung Function <strong>Spirometry</strong><br />
COPD Diagnosis: <strong>Spirometry</strong> Indications for <strong>Spirometry</strong><br />
• Detect the presence or absence of lung disease<br />
• Quantify the severity of lung disease<br />
• Assess the change in lung function over time or following<br />
administration of therapy<br />
• Assess the potential effects of environmental or<br />
occupational exposure<br />
• Assess impairment and/or disability<br />
• Assess risk for surgical procedure<br />
AARC Clinical Practice Guideline. Respir Care 1996;41(7):629-36.<br />
10/16/2011<br />
4<br />
6<br />
1
Benefits of <strong>Spirometry</strong><br />
• Confirms the diagnosis of Asthma or COPD<br />
• Assesses the severity of the illness<br />
• Assesses the response to therapy<br />
• Provides education and opportunity to teach delivery<br />
devices<br />
• Opens a dialogue for a conversation on Smoking Cessation<br />
• Allows assessment of lung Restriction<br />
Assessment of COPD:<br />
Canada Lung Health Test<br />
1. Do you cough regularly?<br />
2. Do you cough up phlegm regularly?<br />
33. Do even simple chores make you short of breath?<br />
4. Do you wheeze when you exert yourself, or at night?<br />
5. Do you get frequent colds that persist longer than<br />
those of other people you know?<br />
If the patient is a smoker or ex-smoker and = 40 yrs old<br />
and answers yes to any of the listed questions,<br />
referrals should be made for further assessment,<br />
including spirometry.<br />
2008 Canadian Thoracic Society recommendations for COPD. Can Respir J 2008;15 Suppl A: 1A-8A<br />
Terms and Abbreviations<br />
• FVC –is the volume of air<br />
that can be forcibly expelled<br />
from the lung from<br />
maximum inspiration to<br />
maximum expiration<br />
c)<br />
• FEV1 –the volume of air<br />
that can be forcibly expelled<br />
from maximum inspiration<br />
in the first second<br />
• FEV1 /FVC –Ratio<br />
• PEFR – the maximum flow<br />
rate attained during an FVC<br />
maneuver<br />
Flow (L/sec<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
PEFR<br />
FEV1<br />
FVC<br />
0 1 2 3 4<br />
Volume (L)<br />
7<br />
11<br />
Who should be tested?<br />
• All patients with suspected Asthma or COPD<br />
• Smokers of > 20 pack years<br />
– Screening vs. case finding<br />
• Patients with significant occupational exposure to<br />
respiratory irritants<br />
• Patients with family history of respiratory diseases<br />
• Patients undergoing lung surgery<br />
Access to Spirometric Testing<br />
• Portable spirometers – office use<br />
• Pulmonary function laboratory – Respirologist’s office<br />
• Other medical laboratories (must assure quality control)<br />
• Need results immediately available to the clinician in order<br />
to make treatment decisions<br />
Lung Function Testing : Normal Effort<br />
Flow (L/s)<br />
6<br />
5 5<br />
4<br />
3<br />
2<br />
1<br />
Flow-Volume Curve Volume-Time Curve<br />
Peak Expiratory Flow<br />
0<br />
0 1 2 3 4 5 6 7 8<br />
Volume (L)<br />
Normal curve<br />
FEV1/ FVC >0.70<br />
Forced Vital Capacity<br />
Volume (L)<br />
6<br />
4<br />
3<br />
2<br />
1<br />
Normal<br />
Forced Expired Volume in 1 second<br />
(FEV 1)<br />
0<br />
0 1 2 3 4 5 6 7 8<br />
Time (sec)<br />
10/16/2011<br />
Forced Vital Capacity (FVC)<br />
FEV 1/ FVC >0.70<br />
8<br />
10<br />
12<br />
2
Lung Function Testing : Obstruction<br />
Flow (L/s)<br />
6<br />
Flow-Volume Curve Volume-Time Curve<br />
5 5<br />
4<br />
3<br />
2<br />
1<br />
Peak Expiratory Flow<br />
Obstruction<br />
• FEV1/FVC < 0.70<br />
• Low expiratory flows<br />
• Low vital capacity (if severe)<br />
0<br />
0 1 2 3 4 5 6 7 8<br />
Volume (L)<br />
Normal curve<br />
FEV1/ FVC >0.70<br />
Forced Vital Capacity<br />
Volume (L)<br />
6<br />
4<br />
3<br />
2<br />
1<br />
Normal<br />
Mild obstruction<br />
0<br />
0 1 2 3 4 5 6 7 8<br />
Time (sec)<br />
FVC<br />
FEV1 FVC<br />
Severe obstruction<br />
FEV1/ FVC = 0.44<br />
FEV1 Normal, Obstruction & Restriction<br />
Flow (L/sec)<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
Normal<br />
Obstruction<br />
Restriction<br />
0<br />
0 1 2 3 4 5 6<br />
Volume (L)<br />
<strong>Spirometry</strong> Criteria:<br />
Obstruction<br />
– reduction in flow relative<br />
to volume (FEV1/FVC)<br />
• expiratory time<br />
prolonged<br />
• airway i narrowing i f for<br />
many reasons<br />
– bronchial smooth<br />
muscle, inflammation of<br />
mucosa, mucus plugging<br />
Restriction<br />
–reduction in volume<br />
• Bellows action of chest<br />
– kyphoscoliosis, gross<br />
obesity<br />
• Lung parenchyma<br />
– fibrosis<br />
• Minimum of 3 acceptable FVC maneuvers should be<br />
performed<br />
– Discontinue testing after 8 attempts<br />
– N No cough, h especially i ll dduring i th the fi first t second d<br />
• Good ‘start-of-test’ includes:<br />
– Extrapolated volume of ≤ 5% of the FVC or 150 mL, whichever is<br />
greater<br />
– No hesitation or false start<br />
– Rapid start to rise time<br />
• Minimum exhalation time of 6 seconds<br />
AARC Clinical Practice Guideline. Respir Care 1996;41(7):629-36. 17<br />
13<br />
15<br />
Lung Function Testing : Restriction<br />
Flow (L/s)<br />
6<br />
Flow-Volume Curve Volume-Time Curve<br />
5 5<br />
4<br />
3<br />
2<br />
1<br />
Peak Expiratory Flow<br />
Restriction<br />
• FEV1/FVC>0.80<br />
• High expiratory flows<br />
• Low vital capacity<br />
0<br />
0 1 2 3 4 5 6 7 8<br />
Volume (L)<br />
Normal curve<br />
FEV1/ FVC >0.70<br />
Forced Vital Capacity<br />
Performing <strong>Spirometry</strong><br />
Volume (L)<br />
6<br />
4<br />
3<br />
2<br />
1<br />
Normal<br />
Forced Expired Volume in 1 second<br />
(FEV1) FEV1 Restriction<br />
0<br />
0 1 2 3 4 5 6 7 8<br />
Time (sec)<br />
10/16/2011<br />
Forced Vital Capacity (FVC)<br />
FEV 1/ FVC >0.70<br />
FVC<br />
FEV1/FVC=1.00 • Ensure the patient is seated, has both feet flat on the<br />
ground (not crossed), nose clips on nose and lips sealed<br />
around mouthpiece<br />
• EExplain l i the h procedure d to the h patient i<br />
• Demonstrate the procedure to the patient<br />
• Observe the patient’s inhalation and exhalation<br />
• Coach: Maximum inspiration, with a good start, smooth<br />
continuous exhalation, with maximum effort<br />
What is not acceptable?<br />
• Unsatisfactory start with excessive hesitation<br />
• Coughing during the first second of maneuver<br />
• Early termination – minimum 6 second exhalation time<br />
• Glottis closure<br />
• Leak<br />
• Obstructed mouthpiece – tongue, false teeth, chewing gum<br />
14<br />
16<br />
18<br />
3
Predicted Normal Values<br />
Age FEV1, FVC and PEF increases, while FEV1/FVC %<br />
decreases with age until about 20 years old in females and<br />
25 years in males<br />
Gender For a given height and age, males have a larger FEV1, FVC<br />
and PEF but a slightly lower FEV1/FVC %<br />
Height All indices other than FEV1/FVC % increase with standing<br />
height (never rely on stated height – shoes off, arm span)<br />
Race 10-15% adjustment for Asians and African Americans<br />
Reference value only, not absolute right or wrong!<br />
Diagnostic Flow Diagram For<br />
Restriction<br />
Is FEV 1 / FVC Ratio Low? (
Assessing Disability in COPD<br />
<strong>Spirometry</strong> Contraindications<br />
• Contraindications (safety or reliability issues)<br />
– Hemoptysis of unknown origin<br />
– Pneumothorax<br />
– UUnstable t bl cardiovascular di l status t t ( (eg. recent t myocardial di l iinfarction f ti or<br />
pulmonary embolus)<br />
– Thoracic, abdominal, or cerebral aneurysms<br />
– Recent eye, thorax or abdomen surgery<br />
– Suspected TB or other contagious respiratory infection<br />
AARC Clinical Practice Guideline. Respir Care 1996;41(7):629-36. 27<br />
Julie’s History<br />
Previous Previous visits for acute<br />
bronchitis<br />
treated with antibiotics<br />
four episodes episodes in last two years<br />
Half Half a pack/day for 20 years<br />
Grew Grew up in family of smokers<br />
Survival in COPD – Relationship to Lung Function and Disability<br />
Julie, 58 years old<br />
Presentation<br />
Worsening Worsening x 3 months<br />
Complains Complains of SOB when walking<br />
up stairs<br />
Wheezing Wh Wheezing i at night i h and d productive d i<br />
cough<br />
10/16/2011<br />
5
Volume<br />
(L)<br />
4<br />
3<br />
2<br />
1<br />
0<br />
Flow<br />
(L/sec)<br />
12<br />
10<br />
VOLUME/TIME CURVE<br />
FEV<br />
1<br />
FVC<br />
0 1 2 3 4 5 6 7 8<br />
8<br />
6<br />
4<br />
2<br />
0<br />
Time (seconds)<br />
OBSTRUCTION<br />
PEFR<br />
FEV 1<br />
0 1 2 3 4 5 6<br />
Volume<br />
(L)<br />
NORMAL, ORMAL, OBSTRUCTION<br />
BSTRUCTION AND ND<br />
RESTRICTION<br />
ESTRICTION COMPARED<br />
OMPARED<br />
Flow<br />
(L/sec)<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
Normal<br />
Obstruction<br />
Restriction<br />
0 1 2 3 4 5 6<br />
Volume<br />
(L)<br />
NORMAL EXPIRATORY FLOW<br />
VOLUME CURVE<br />
12<br />
10<br />
8<br />
4<br />
2<br />
0<br />
PEFR<br />
Flow 6<br />
(L/sec) FEV1 Flow<br />
(L/sec)<br />
0 1 2 3 4 5 6<br />
Volume (L)<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
RESTRICTION<br />
ESTRICTION<br />
PEFR<br />
FEV 1<br />
0 1 2 3 4 5 6<br />
Volume<br />
(L)<br />
NORMAL ORMAL WITH ITH WEAK EAK EFFORT FFORT<br />
Flow<br />
(L/sec)<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
FEV 1<br />
PEFR<br />
FEV 1<br />
0 1 2 3 4 5 6<br />
Volume (L)<br />
10/16/2011<br />
6
Flow (LL/sec)<br />
12<br />
8<br />
4<br />
Julie’s <strong>Spirometry</strong> Results<br />
0<br />
0 2 4<br />
Volume (L)<br />
Key Points for Julie<br />
6<br />
Age: 58<br />
Height: 160 cm<br />
Sex: Female<br />
Ethnicity: Caucasian<br />
Smoking Smoking cessation can prevent further<br />
long long-term term lung damage or slow the rate of<br />
decline of lung function<br />
If If one bronchodilator b h dil f fails, il ensure patient i i is<br />
compliant and able to use prescribed delivery<br />
system properly<br />
Use Use stepwise approach to treatment plan<br />
Canadian Respiratory Review Panel, 1998.<br />
Pre-bronchodilator<br />
Post-bronchodilator<br />
Terms and Abbreviations<br />
FVC - forced vital capacity<br />
FEV FEV1 1second<br />
FEV 1 /FVC<br />
/FVC Ratio<br />
- forced expired volume in<br />
PEFR -peak peak expiratory flow<br />
FEF 25 25-75% 75% -forced forced expiratory flow between<br />
25 25-75% 75% of the vital capacity<br />
Julie’s <strong>Spirometry</strong> Results<br />
Pre-Bronchodilator Post-Bronchodilator<br />
Predicted Measured<br />
%<br />
Predicted Measured<br />
10/16/2011<br />
%<br />
Change<br />
FVC 4.37 L 4.65 L 106% 4.65 L 0%<br />
FEV1 3.78 L 2.79 L 74% 2.94 L 7%<br />
FEV 1/ FVC (%) 86% 60% 63%<br />
Decline of FEV FEV1 with Age and<br />
Smoking History<br />
100<br />
75<br />
50<br />
25<br />
Symptoms<br />
Smoked regularly and<br />
susceptible to smoke<br />
Disability<br />
Death<br />
0<br />
25 50 75<br />
Age (years)<br />
Never smoked or not<br />
susceptible to<br />
smoke<br />
Stopped at 45<br />
Stopped at 65<br />
Fletcher C. BMJ 1977;1:1645-1648.<br />
7
Smokers with airway obstruction<br />
are more likely to quit<br />
Smoking quit ratess<br />
at 12 months (%)<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
Usual smoking quit rate with physician advice = 4 – 6%<br />
p = 00.0003 0003 p = 00.003 003 p = 00.005 005 p = 0229 0.229<br />
16.3%<br />
18.5%<br />
16.1%<br />
14.6%<br />
Any airway<br />
obstruction<br />
Severe<br />
Obstruction<br />
Moderate<br />
obstruction<br />
Bednarek M et al. Thorax 2006;61:869<br />
2006;61:869-73. 73.<br />
Treat the COPD<br />
12.0%<br />
Mild obstruction No obstruction<br />
Smoking cessation<br />
Vaccinations<br />
Post BD ratio 79%<br />
Moderate COPD<br />
LABD either LAAC or LABA<br />
ICS in combination to prevent exacerbations<br />
More coming later<br />
Julie’s <strong>Spirometry</strong> Results/2<br />
Pre-Bronchodilator Post-Bronchodilator<br />
Predicted Measured<br />
%<br />
Predicted Measured<br />
%<br />
Change<br />
FVC 4.37 L 4.65 L 106% 4.65 L 0%<br />
FEV1 3.78 L 2.79 L 74% 3.50 L 21%<br />
FEV 1/ FVC (%) 86% 60% 73%<br />
What’s in a Cigarette?<br />
♦Tobacco smoke: ≥ 4000 chemicals 1 , ≥ 50<br />
carcinogenic 2<br />
Chemicals in<br />
Tobacco Smoke 1 Also Found In…<br />
Acetone<br />
Butane<br />
Arsenic<br />
Cadmium<br />
Carbon monoxide<br />
Toluene<br />
Paint stripper<br />
Lighter fluid<br />
Ant poison<br />
Car batteries<br />
Car exhaust fumes<br />
Industrial solvent<br />
Nicotine is responsible for the addiction, but other chemicals<br />
are also involved. 2<br />
Smoking cigarettes with lower tar and nicotine provides no health<br />
benefit. 2<br />
1. World Health Organization. Tobacco: deadly in any form or disguise, 2006.<br />
2. Health Canada. What’s in Cigarette smoke?, August 2005.<br />
Julie’s <strong>Spirometry</strong> Results<br />
Pre-Bronchodilator Post-Bronchodilator<br />
Predicted Measured<br />
%<br />
Predicted Measured<br />
10/16/2011<br />
%<br />
Change<br />
FVC 4.37 L 4.65 L 106% 4.65 L 0%<br />
FEV1 3.78 L 2.79 L 74% 2.94 L 7%<br />
FEV 1/ FVC (%) 86% 60% 63%<br />
How long after B2 to wait for repeat FEV!?<br />
So what if…..<br />
8
Asthma: Diagnostic Algorithm<br />
Symptoms consistent with asthma<br />
<strong>Spirometry</strong> before and after bronchodilator<br />
(if unavailable: peak flow monitoring, trial of therapy)<br />
S<strong>Spirometry</strong> i t results lt normall<br />
• Consider an alternative diagnosis and/or<br />
• Peak flow monitoring and/or<br />
• Bronchoprovocation challenge testing<br />
• Introduction of treatment (appropriate only<br />
for those with high likelihood of asthma;<br />
diagnostic confirmation should occur at<br />
some later date)<br />
Kaplan A et al. CMAJ 2009;181:e210-20<br />
<strong>Spirometry</strong> results consistent with asthma<br />
• Administer short-acting β-agonist as needed<br />
to relieve symptoms<br />
• Commence anti-inflammatory therapy (usually<br />
low-dose inhaled corticosteroids)<br />
• Look for triggers by history and occupational<br />
exposure, and consider allergy testing (allergen<br />
specific skin or blood tests)<br />
• Consider comorbidities (e.g.: rhinitis, GERD)<br />
Arrange follow-up to reassess diagnosis, control, and treatment<br />
GERD: gastroesophageal reflux disease<br />
Do you want to learn more about<br />
<strong>Spirometry</strong>?<br />
FPAGC has a Mainpro C workshop on<br />
spirometry interpretation that can be brought to<br />
your community<br />
www.fpagc.com<br />
www www.fpagc.com fpagc com<br />
SpiroTrec is a program that teaches your staff<br />
how to appropriately DO spirometry<br />
www.resptrec.org/spirotrec.php<br />
(51 of 32)<br />
Pulmonary function testing = /<br />
<strong>Spirometry</strong><br />
Also includes:<br />
Measurement of Oxygen<br />
Measurement of gas exchange<br />
Diffusion capacity<br />
Measurement of lung volumes<br />
This is NOT needed for the diagnosis of<br />
COPD, so do not order it!!<br />
I look forward to being<br />
able to assist you in your<br />
respiratory needs!<br />
www www.fpagc.com fpagc com<br />
for4kids@gmail.com<br />
10/16/2011<br />
9