Current Concepts in Plantar Plate Repair - Weil Foot & Ankle Institute
Current Concepts in Plantar Plate Repair - Weil Foot & Ankle Institute
Current Concepts in Plantar Plate Repair - Weil Foot & Ankle Institute
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Current</strong> <strong>Concepts</strong> <strong>in</strong> <strong>Plantar</strong> <strong>Plate</strong> <strong>Repair</strong><br />
Podiatry Today, April 2012<br />
weil4feet.com<br />
(847) 390.7666<br />
Lowell <strong>Weil</strong> Jr., DPM, MBA, FACFAS Er<strong>in</strong> E. Kle<strong>in</strong>, DPM, MS, AACFAS<br />
With any surgical procedure, there are problems and complications. The most commonly discussed<br />
problem associated with the <strong>Weil</strong> osteotomy is the “float<strong>in</strong>g toe.” Studies had identified the float<strong>in</strong>g toe to<br />
occur 15 to 50 percent of the time follow<strong>in</strong>g a <strong>Weil</strong> osteotomy 1-3 .The float<strong>in</strong>g toe does not touch the floor<br />
with neutral weight-bear<strong>in</strong>g after undergo<strong>in</strong>g a metatarsal osteotomy.<br />
Additionally, there is weakness and decreased ability to actively plantarflex the toe. Many have theorized<br />
as to the cause of float<strong>in</strong>g toe and have suggested modifications to the procedure <strong>in</strong> order to prevent its<br />
occurrence 4-7 . However, most of these changes have not altered the outcome and <strong>in</strong>creased other<br />
complications (transfer metatarsalgia, stiffness, edema, etc.) and disability postoperatively.<br />
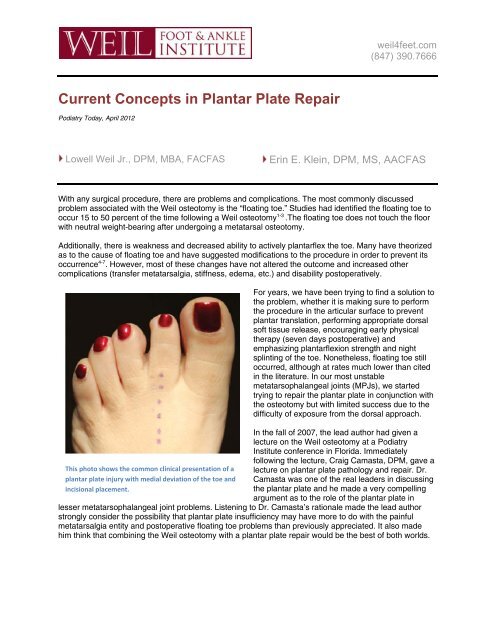
This photo shows the common cl<strong>in</strong>ical presentation of a<br />
plantar plate <strong>in</strong>jury with medial deviation of the toe and<br />
<strong>in</strong>cisional placement.<br />
For years, we have been try<strong>in</strong>g to f<strong>in</strong>d a solution to<br />
the problem, whether it is mak<strong>in</strong>g sure to perform<br />
the procedure <strong>in</strong> the articular surface to prevent<br />
plantar translation, perform<strong>in</strong>g appropriate dorsal<br />
soft tissue release, encourag<strong>in</strong>g early physical<br />
therapy (seven days postoperative) and<br />
emphasiz<strong>in</strong>g plantarflexion strength and night<br />
spl<strong>in</strong>t<strong>in</strong>g of the toe. Nonetheless, float<strong>in</strong>g toe still<br />
occurred, although at rates much lower than cited<br />
<strong>in</strong> the literature. In our most unstable<br />
metatarsophalangeal jo<strong>in</strong>ts (MPJs), we started<br />
try<strong>in</strong>g to repair the plantar plate <strong>in</strong> conjunction with<br />
the osteotomy but with limited success due to the<br />
difficulty of exposure from the dorsal approach.<br />
In the fall of 2007, the lead author had given a<br />
lecture on the <strong>Weil</strong> osteotomy at a Podiatry<br />
<strong>Institute</strong> conference <strong>in</strong> Florida. Immediately<br />
follow<strong>in</strong>g the lecture, Craig Camasta, DPM, gave a<br />
lecture on plantar plate pathology and repair. Dr.<br />
Camasta was one of the real leaders <strong>in</strong> discuss<strong>in</strong>g<br />
the plantar plate and he made a very compell<strong>in</strong>g<br />
argument as to the role of the plantar plate <strong>in</strong><br />
lesser metatarsophalangeal jo<strong>in</strong>t problems. Listen<strong>in</strong>g to Dr. Camasta’s rationale made the lead author<br />
strongly consider the possibility that plantar plate <strong>in</strong>sufficiency may have more to do with the pa<strong>in</strong>ful<br />
metatarsalgia entity and postoperative float<strong>in</strong>g toe problems than previously appreciated. It also made<br />
him th<strong>in</strong>k that comb<strong>in</strong><strong>in</strong>g the <strong>Weil</strong> osteotomy with a plantar plate repair would be the best of both worlds.
Position a McGlamry elevator to mobilize the plantar<br />
plate with preservation of collateral ligaments.<br />
weil4feet.com<br />
(847) 390.7666<br />
Later <strong>in</strong> the exhibit hall, the lead author came<br />
across a company that was show<strong>in</strong>g bone anchor<br />
concepts that were the standard of care for<br />
arthroscopic rotator cuff repair at the time. The<br />
delivery system for repair<strong>in</strong>g the rotator cuff was<br />
someth<strong>in</strong>g with which he was totally unfamiliar but<br />
he watched the salesman demonstrate the<br />
placement of sutures <strong>in</strong>to tissue <strong>in</strong> a tight space. At<br />
that moment, he realized that he now had a way to<br />
suture the plantar plate through the same dorsal<br />
exposure as the <strong>Weil</strong> osteotomy.<br />
The follow<strong>in</strong>g week, the lead author and his<br />
Fellow, Jason Glover, DPM, tried different<br />
comb<strong>in</strong>ed <strong>Weil</strong> osteotomy/plantar plate repairs on<br />
cadavers and came up with a reproducible<br />
technique. They started perform<strong>in</strong>g the procedure<br />
for patients with the most unstable, pa<strong>in</strong>ful metatarsalgia and closely followed the patients and their<br />
results. The lead author presented the first series of cases at the International Federation of <strong>Foot</strong> and<br />
<strong>Ankle</strong> Surgeons the follow<strong>in</strong>g fall <strong>in</strong> Brazil with very encourag<strong>in</strong>g early results show<strong>in</strong>g high function and<br />
dim<strong>in</strong>ished <strong>in</strong>cidence of float<strong>in</strong>g toe.<br />
WHY SHORTEN THE METATARSAL?<br />
Metatarsalgia is one of the most common problems we see as foot and ankle specialists. Typically, the<br />
position and length of the second metatarsal (and occasionally the third) has created a biomechanical<br />
imbalance <strong>in</strong> the forefoot, caus<strong>in</strong>g pa<strong>in</strong> and subsequent <strong>in</strong>jury to the surround<strong>in</strong>g soft tissue structures,<br />
particularly the plantar plate. Dur<strong>in</strong>g the propulsive phase of gait, an elongated metatarsal will be<br />
overloaded with every step. Over time, that overload will cause attrition to the plantar plate and<br />
surround<strong>in</strong>g soft tissue structures, lead<strong>in</strong>g to pa<strong>in</strong>, swell<strong>in</strong>g, deviation of the jo<strong>in</strong>t, crossover toe deformity,<br />
hammertoe and ultimately dislocation.<br />
Radiographically, this manifests as a subtle difference <strong>in</strong> the length of the second metatarsal <strong>in</strong><br />
comparison to the contralateral foot (for unilateral pathology) or <strong>in</strong> comparison to the expected normal<br />
second metatarsal protrusion distance (for bilateral pathology). In our patients with unilateral plantar plate<br />
tears, the side with the plantar plate pathology had a second metatarsal protrusion distance of 4.4 + 1.0<br />
mm, which is 0.6 mm longer than the contralateral/non-pathological side (3.8 + 1.0 mm) 8 .
This is a cadaveric cross‐section with a correspond<strong>in</strong>g<br />
sagittal MRI demonstrat<strong>in</strong>g the plantar plate (p<strong>in</strong>k<br />
arrows) and association with flexor tendons (yellow<br />
arrows).<br />
weil4feet.com<br />
(847) 390.7666<br />
It is necessary to correct the underly<strong>in</strong>g deformity<br />
by shorten<strong>in</strong>g the metatarsal. Without metatarsal<br />
shorten<strong>in</strong>g, soft tissue corrections will fail over<br />
time. Not correct<strong>in</strong>g the metatarsal <strong>in</strong> this situation<br />
is much like address<strong>in</strong>g a posterior tendon<br />
dysfunction solely by repair<strong>in</strong>g the tendon without<br />
chang<strong>in</strong>g the structural component with<br />
appropriate calcaneal osteotomies, arthroereisis or<br />
fusion procedures.<br />
WHY REPAIR THE PLANTAR PLATE?<br />
The earliest description of the plantar plate can be<br />
credited to Cruveilhier, who described the plantar<br />
plate as a static structure that served to “protect”<br />
the lower portion of the lesser MPJ while<br />
<strong>in</strong>creas<strong>in</strong>g jo<strong>in</strong>t space area 9 . More recently,<br />
authors have theorized the plantar plate to serve<br />
as both a static and dynamic structure hav<strong>in</strong>g<br />
attachments to the deep transverse <strong>in</strong>termetatarsal<br />
ligament, the lateral collateral ligaments and the<br />
plantar fascia 10 .<br />
The plantar plate is one of the ma<strong>in</strong> stabilizers of<br />
the lesser metatarsophalangeal jo<strong>in</strong>t. In concert<br />
with the collateral ligament complex, the plantar plate ma<strong>in</strong>ta<strong>in</strong>s stability at the level of the MTPJ.<br />
Section<strong>in</strong>g of the plantar plate will decrease the amount of force necessary to dislocate the MPJ by 30<br />
percent 11 . Section<strong>in</strong>g of the collateral ligaments will decrease the amount of force to dislocate the MPJ by<br />
45 percent. Section<strong>in</strong>g of both structures will decrease the amount of force needed to dislocate the MPJ<br />
by 79 percent 11 .<br />
This photo demonstrates visualization of the plantar<br />
plate (black arrow) from a dorsal approach with a<br />
distraction device <strong>in</strong> place.<br />
It stands to reason, therefore, that pathology of the<br />
plantar plate needs repair <strong>in</strong> order to restore<br />
stability to the lesser MPJ. This concept is similar<br />
to that of a Brostrom procedure for lateral ankle<br />
stabilization. When the primary stabiliz<strong>in</strong>g structure<br />
of a jo<strong>in</strong>t undergoes repair, the jo<strong>in</strong>t becomes more<br />
stable.<br />
HOW COMMON IS PLANTAR PLATE<br />
PATHOLOGY?<br />
In the experience of our <strong>in</strong>stitution, plantar plate<br />
pathology is responsible for much of the lesser<br />
MPJ pa<strong>in</strong>/metatarsalgia <strong>in</strong> our patients. As many<br />
as 50 percent of our patients with metatarsalgia<br />
present to our cl<strong>in</strong>ic seek<strong>in</strong>g a second op<strong>in</strong>ion as<br />
they had previously seen physicians who<br />
diagnosed another pathology (generally capsulitis or a second <strong>in</strong>terspace neuroma) that was resistant to<br />
treatment.
weil4feet.com<br />
(847) 390.7666<br />
Interest<strong>in</strong>gly, while conduct<strong>in</strong>g a cadaveric study earlier this year aimed at elucidat<strong>in</strong>g the cross-sectional<br />
anatomy of the metatarsal neck and the proximal attachment of the plantar plate, researchers found 80<br />
percent (16 of 20) of these randomly selected specimens had one of four types of plantar plate tears 12 .<br />
HOW TO DETERMINE PLANTAR PLATE PATHOLOGY<br />
A thorough cl<strong>in</strong>ical exam<strong>in</strong>ation can isolate the possibility of plantar plate pathology. Patients will typically<br />
present with pa<strong>in</strong> to the ball of the foot that is progressive <strong>in</strong> nature. They may compla<strong>in</strong> of some<br />
numbness <strong>in</strong>to the area, which is likely due to swell<strong>in</strong>g putt<strong>in</strong>g pressure on the nerves <strong>in</strong> the area. The toe<br />
may be chang<strong>in</strong>g position over time by becom<strong>in</strong>g more dorsally aligned or with lateral or, more commonly,<br />
medial deviation. There can be concomitant first ray pathology (hallux valgus or hallux rigidus), but this is<br />
not always present.<br />
In the most severe cases, there may be a crossover toe deformity or MPJ dislocation. Hammertoe<br />
deformities may or may not be present. In early manifestations of disease, swell<strong>in</strong>g at the plantar aspect<br />
of the MPJ may be present. However, <strong>in</strong> the situation of complete tear, this may be absent. There will be
weil4feet.com<br />
(847) 390.7666<br />
pa<strong>in</strong> at the plantar aspect of the MPJ or distal aspect of the metatarsal head. A modified drawer test may<br />
yield <strong>in</strong>stability <strong>in</strong> comparison to the contralateral foot or <strong>in</strong> comparison to the “expected normal” when<br />
bilateral disease is present. A drawer test will be pa<strong>in</strong>ful <strong>in</strong> the patient with an <strong>in</strong>complete tear but often<br />
pa<strong>in</strong>less with complete tear. There may be weakness of plantarflexion of the affected toe.<br />
X-ray f<strong>in</strong>d<strong>in</strong>gs of bilateral weightbear<strong>in</strong>g films will often show an altered metatarsal pattern with the<br />
second metatarsal be<strong>in</strong>g slightly longer <strong>in</strong> comparison to the contralateral foot, transverse plane deviation<br />
of the digits, splay<strong>in</strong>g of the digits and a subtly <strong>in</strong>creased metatarsus adductus angle. Interest<strong>in</strong>gly, 60<br />
percent of our patients had splay<strong>in</strong>g of the second and third digits, and did not have an <strong>in</strong>terdigital<br />
neuroma. In the past, advanced diagnostics were <strong>in</strong>consistent at best. Magnetic resonance images (MRI)<br />
of a MPJ would rarely provide more than one or two slices through the jo<strong>in</strong>t and visualization of the<br />
plantar plate was <strong>in</strong>adequate. More recently, MRI techniques have allowed a much higher level of<br />
appreciation of the MPJ.<br />
The plantar plate (black arrow) is completely detached<br />
from the proximal phalanx with flexor tendons <strong>in</strong> close<br />
plantar proximity (green arrow). Note the thickness of<br />
the plantar plate.<br />
Our previous Fellow, Wenjay Sung, DPM, led our<br />
ACFAS Research Grant Award to determ<strong>in</strong>e MRI<br />
correlation to <strong>in</strong>traoperative f<strong>in</strong>d<strong>in</strong>gs of plantar plate<br />
pathology. The overall accuracy of MRI <strong>in</strong><br />
determ<strong>in</strong><strong>in</strong>g if plantar plate pathology was present<br />
was 96 percent. This study also revealed a<br />
sensitivity of 95 percent, a specificity of 100<br />
percent, a positive predictive value of 100 percent<br />
and a negative predictive value of 67 percent. This<br />
MRI study occurred without IV contrast and without<br />
<strong>in</strong>tra-articular contrast, as had been done previously<br />
<strong>in</strong> the literature 13,14 . Sung’s MRI study was the 2011<br />
poster award w<strong>in</strong>ner at the American Orthopedic<br />
<strong>Foot</strong> and <strong>Ankle</strong> Surgeons Annual Summer Meet<strong>in</strong>g,<br />
and will be published <strong>in</strong> the Journal of <strong>Foot</strong> and<br />
<strong>Ankle</strong> Surgery <strong>in</strong> 2012 15 .<br />
We also have an ongo<strong>in</strong>g study look<strong>in</strong>g at<br />
diagnostic ultrasound <strong>in</strong> comparison to MRI f<strong>in</strong>d<strong>in</strong>gs<br />
and <strong>in</strong>traoperative f<strong>in</strong>d<strong>in</strong>gs. The early results from this study suggest that ultrasound evaluation of the<br />
plantar plate is highly technician dependent. Although the ability of the ultrasound and technician to detect<br />
the presence of plantar plate pathology is relatively high (75 percent), the ability to accurately detect the<br />
location of the plantar plate pathology is very low (31 percent).<br />
A GUIDE TO PERFORMING THE COMBINED PLANTAR PLATE REPAIR AND WEIL<br />
OSTEOTOMY<br />
To rectify plantar plate pathology and metatarsal deformity, we have developed a comb<strong>in</strong>ed procedure to<br />
perform a dorsal approach anatomic plantar plate repair and a <strong>Weil</strong> osteotomy.<br />
Make a l<strong>in</strong>ear <strong>in</strong>cision overly<strong>in</strong>g the extensor apparatus extend<strong>in</strong>g from the distal third of the metatarsal<br />
shaft to the midshaft of the proximal phalanx center<strong>in</strong>g over the MPJ. After perform<strong>in</strong>g dissection down to<br />
the extensor apparatus, create an <strong>in</strong>cision between the extensor digitorum longus and brevis to the level<br />
of bone from the distal metatarsal to the proximal phalanx shaft. Place a self-reta<strong>in</strong><strong>in</strong>g retractor deep to<br />
the extensor tendons and expose the MPJ. Reflect the medial and lateral collaterals off the proximal<br />
phalanx base, mak<strong>in</strong>g sure to preserve their metatarsal head attachments.
weil4feet.com<br />
(847) 390.7666<br />
Then carefully place a small or medium McGlamry type elevator <strong>in</strong>to the MPJ and advance it proximally<br />
(hugg<strong>in</strong>g the bone) to release adhesions and mobilize the proximal plantar plate attachment at the<br />
metatarsal neck. This allows improved exposure to the plantar plate <strong>in</strong> later steps. Only use the elevator<br />
plantarly and do not carry it to the medial or lateral side of the metatarsal head. This helps ma<strong>in</strong>ta<strong>in</strong><br />
collateral attachments as these attachments provide the most important blood supply to the metatarsal<br />
head.<br />
The M<strong>in</strong>i‐Scorpion (Arthrex) grasps the plantar plate and<br />
engages the suture.<br />
Perform a <strong>Weil</strong> osteotomy <strong>in</strong> the affected<br />
metatarsal. The osteotomy starts <strong>in</strong> the dorsal (2 to<br />
3 mm) articular surface of the metatarsal. The<br />
angle of the osteotomy is as close to parallel to the<br />
weightbear<strong>in</strong>g surface as possible. This angle is<br />
important to prevent plantar displacement of the<br />
metatarsal head as one creates shorten<strong>in</strong>g.<br />
After complet<strong>in</strong>g the osteotomy, use a metatarsal<br />
push<strong>in</strong>g device to push the metatarsal head<br />
proximally 7 to 15 mm and temporarily fixate it with<br />
a 1.6-mm threaded K-wire.<br />
Place a m<strong>in</strong>i-jo<strong>in</strong>t distraction device over the p<strong>in</strong> to<br />
fixate the metatarsal head and then place a second<br />
p<strong>in</strong> from dorsal to plantar, 5 mm distal to the base<br />
of the proximal phalanx. After plac<strong>in</strong>g the<br />
distractor, open it to ga<strong>in</strong> dorsal access to the MPJ and visualize the plantar plate.<br />
This photo shows the plantar plate with a mattress<br />
suture <strong>in</strong> place.<br />
One can confirm plantar plate pathology with direct<br />
visualization of this structure. We have observed<br />
several different types of plantar plate <strong>in</strong>juries.<br />
These <strong>in</strong>juries <strong>in</strong>clude attenuation/attrition,<br />
longitud<strong>in</strong>al buttonhole tears, partial transverse<br />
tears or complete ruptures. The most common<br />
pattern, <strong>in</strong> cadavers and our patients alike, is the<br />
<strong>in</strong>complete transverse tears at the attachment <strong>in</strong>to<br />
the proximal phalanx. These tears can be visible at<br />
the medial plantar plate attachment or, more<br />
commonly, the lateral plantar plate attachment.<br />
With more advanced disease, the entire plantar<br />
plate will be torn. Coughl<strong>in</strong> published an anatomic<br />
study of plantar plate tears and a modified version<br />
of our grad<strong>in</strong>g scale 12,16 .<br />
If the plantar plate has pathology, one must<br />
carefully dissect the entirety of the plantar plate off the base of the proximal phalanx. The flexor tendons<br />
run <strong>in</strong> close plantar (deep) proximity to the plantar plate at this level and one must take care not to cut<br />
them. After resect<strong>in</strong>g the plantar plate off the phalanx, carry dissection proximally to create a full<br />
thickness flap of the plantar plate for advancement. A Freer elevator may be helpful to ma<strong>in</strong>ta<strong>in</strong> a<br />
consistent level of tissue dur<strong>in</strong>g this dissection.<br />
After completely mobiliz<strong>in</strong>g the plantar plate, utilize a M<strong>in</strong>i-Scorpion device from the Complete <strong>Plate</strong><br />
<strong>Repair</strong> Kit (Arthrex) to create a wide three-stitch mattress. Remove the distraction device and place a<br />
right angle towel clamp around the sides of the proximal phalanx. Perform manual<br />
distraction/plantarflexion to expose the base of the proximal phalanx. Remove any soft tissue
weil4feet.com<br />
(847) 390.7666<br />
attachments on the plantar surface of the proximal phalanx base. Us<strong>in</strong>g a small curette, roughen the<br />
plantar bony surface to facilitate plantar plate reattachment.<br />
Here one can see an oblique bone tunnel with a suture<br />
passer <strong>in</strong> place to pass the suture, secur<strong>in</strong>g the plantar<br />
plate <strong>in</strong>to the proximal phalanx.<br />
Create crossed bone tunnels <strong>in</strong> the proximal<br />
phalanx from distal dorsal medial to proximal<br />
plantar lateral. Create a second tunnel by drill<strong>in</strong>g<br />
from distal dorsal lateral to proximal plantar medial.<br />
Then pass the sutures attached to the plantar plate<br />
from plantar to dorsal through the bone tunnels <strong>in</strong><br />
the phalanx.<br />
Proceed to remove the temporary fixation for the<br />
metatarsal head and pull the metatarsal head to its<br />
desired length. It is rare to shorten more than 3<br />
mm. After achiev<strong>in</strong>g accurate alignment, fixate the<br />
osteotomy with one or two Snap-Off screws.<br />
<strong>Plantar</strong>flex the phalanx to approximately 15 to 20<br />
degrees. Then pull the sutures tightly to advance<br />
the plantar plate <strong>in</strong>to the base of the proximal<br />
phalanx. Tie the sutures dorsally to secure the<br />
plantar plate position. The toe will appear plantarflexed. Then reapproximate deep tissue and sk<strong>in</strong>, and<br />
apply a bulky compressive bandage hold<strong>in</strong>g the second toe <strong>in</strong> plantarflexion. This bandage should rema<strong>in</strong><br />
<strong>in</strong> place for seven to 10 days with guarded partial weightbear<strong>in</strong>g <strong>in</strong> a surgical shoe.<br />
Secure the sutures <strong>in</strong> place through bone tunnels, pull<strong>in</strong>g<br />
the plantar plate <strong>in</strong>to the proximal phalanx.<br />
Here one can see the proper position of the toe after<br />
fixation of the osteotomy and secur<strong>in</strong>g the sutures<br />
dorsally.<br />
After remov<strong>in</strong>g the bandages, <strong>in</strong>struct the patient to<br />
return to a supportive athletic shoe with guarded<br />
weightbear<strong>in</strong>g. The patient receives a night brace<br />
to reduce swell<strong>in</strong>g. This brace (AFTR DC brace<br />
with osteotomy strap, BioSk<strong>in</strong>) will serve as a night<br />
spl<strong>in</strong>t to hold the toe <strong>in</strong> plantarflexion. This night<br />
spl<strong>in</strong>t<strong>in</strong>g technique helps prevent dorsal<br />
contracture and scar tissue formation that can lead<br />
to limited postoperative plantarflexion.<br />
Aggressive physical therapy beg<strong>in</strong>s at seven to 10<br />
days postoperatively with particular emphasis on<br />
plantarflexion strength. Passive and active range of<br />
motion of the short and long flexor tendons —<br />
often under the direction of a physical therapist —<br />
two to three times a week is often <strong>in</strong>cluded <strong>in</strong> the<br />
postoperative regimen.<br />
Patients are able to return to normal shoe gear six<br />
to eight weeks postoperatively and beg<strong>in</strong><br />
aggressive weightbear<strong>in</strong>g activities.<br />
HOW PATIENTS HAVE FARED<br />
FOLLOWING THE PROCEDURE<br />
Our early results of this procedure were published<br />
<strong>in</strong> <strong>Foot</strong> and <strong>Ankle</strong> Specialist <strong>in</strong> 2011.17<br />
Postoperative Visual Analogue Scale scores
weil4feet.com<br />
(847) 390.7666<br />
decreased from 7.3 + 1.6 to 1.7 + 1.8. Eighty-five percent of patients reported improved function and 77<br />
percent of patients were satisfied or very<br />
satisfied with the outcome of the procedure. For this group of patients, there were two complications:<br />
pa<strong>in</strong>ful hardware and cont<strong>in</strong>ued metatarsalgia. There were no <strong>in</strong>cidences of dehiscence, malunion, nonunion<br />
or recurrent MPJ subluxation or dislocation.<br />
S<strong>in</strong>ce the time of that study’s publication, we have performed many more procedures, all with similar and<br />
significant reduction <strong>in</strong> pa<strong>in</strong> level postoperatively. There have been a few patients who have susta<strong>in</strong>ed<br />
significantly pa<strong>in</strong>ful post-op stiffness that has resolved after a jo<strong>in</strong>t manipulation with the patient under<br />
anesthesia. Further results will be available with longer follow-up of this larger cohort of patients.<br />
IN CONCLUSION<br />
Through our research, we conclude that the <strong>in</strong>cidence of plantar plate pathology is far more prevalent<br />
than commonly appreciated. In a randomized group of 20 cadavers, 80 percent of specimens had plantar<br />
plate tears 12 . Anytime we see a pa<strong>in</strong>ful metatarsalgia with plantar swell<strong>in</strong>g at the MPJ, we suspect a<br />
plantar plate tear.<br />
This is the postoperative brace with a strap hold<strong>in</strong>g the<br />
toe <strong>in</strong> a plantarflexed position.<br />
An appropriate cl<strong>in</strong>ical exam and radiographs can<br />
help detect plantar plate problems. Magnetic<br />
resonance imag<strong>in</strong>g and ultrasound can help<br />
accurately def<strong>in</strong>e the presence and location of<br />
plantar plate deficits.<br />
Previously, surgeons would have to choose<br />
whether to realign the metatarsal position or repair<br />
the plantar plate. Both procedures provide<br />
successful outcomes but have limitations as<br />
neither addresses the entire pathology <strong>in</strong>volved.<br />
The dorsal approach for anatomic plantar plate<br />
repair provides a comb<strong>in</strong>ed alternative to fully<br />
correct the complex nature of both a plantar plate<br />
repair and metatarsal deformity. The dorsal<br />
approach of this procedure allows the surgeon<br />
appreciation of both severe and subtler plantar<br />
plate <strong>in</strong>juries that may not be clearly evident from a<br />
plantar approach. This approach also allows for<br />
metatarsal realignment and prevention of a plantar<br />
scar.<br />
We believe that with further attention and research,<br />
we can better understand, diagnose and treat<br />
plantar plate problems to provide surgeons and<br />
patients alike with the most optimal results.<br />
Dr. <strong>Weil</strong> is the President and Fellowship Director of<br />
the <strong>Weil</strong> <strong>Foot</strong>, <strong>Ankle</strong> and Orthopedic <strong>Institute</strong>. He<br />
also serves as the Editor of <strong>Foot</strong> and <strong>Ankle</strong> Specialist. Dr. <strong>Weil</strong> is a Fellow of the American College of<br />
<strong>Foot</strong> and <strong>Ankle</strong> Surgeons.<br />
Dr. Kle<strong>in</strong> is the Reconstructive <strong>Foot</strong> and <strong>Ankle</strong> Surgical Fellow at the <strong>Weil</strong> <strong>Foot</strong>, <strong>Ankle</strong> and Orthopedic<br />
<strong>Institute</strong>.
REFERENCES<br />
weil4feet.com<br />
(847) 390.7666<br />
1. Highlander P, VonHerbulis E, Gonzalez A, Britt J, Buchman J. Complications of the <strong>Weil</strong> Osteotomy.<br />
<strong>Foot</strong> <strong>Ankle</strong> Spec. 2011;4(3):165-70.<br />
2. Garg R, Thordarson DB, Schrumpf M, Castaneda D. Slid<strong>in</strong>g oblique versus segmental resection<br />
osteotomies for lesser metatarsophalangeal jo<strong>in</strong>t pathology. <strong>Foot</strong> <strong>Ankle</strong> Int. 2008; 29(10):1009-14.<br />
3. Migues A, Slullitel G, Bilbao F, Carrasco M, Solari G. Float<strong>in</strong>g-toe deformity as a complication of the<br />
<strong>Weil</strong> osteotomy. <strong>Foot</strong> <strong>Ankle</strong> Int. 2004; 25(9):609-13.<br />
4. Joseph R, Schroeder K, Greenberg M. A retrospective analysis of lesser metatarsophalangeal jo<strong>in</strong>t<br />
fusion as a treatment option for hammertoe patholiogy associated with metatarsophalangeal jo<strong>in</strong>t<br />
<strong>in</strong>stability. J <strong>Foot</strong> <strong>Ankle</strong> Surg. 2012; 51: 57–62.<br />
5. Baravarian B, Thompson J, Nazarian D. <strong>Plantar</strong> plate tears: a review of the modified flexor tendon<br />
transfer repair of stabilization. Cl<strong>in</strong> Pod Med Surg. 2011; 28: 57–58.<br />
6. Bouche RT, Heit EJ. Comb<strong>in</strong>ed plantar plate and hammertoe repair with flexor digitorum longus tendon<br />
transfer for chronic, severe sagittal plane <strong>in</strong>stability of the lesser metatarsophalangeal jo<strong>in</strong>ts: prelim<strong>in</strong>ary<br />
observations. J <strong>Foot</strong> <strong>Ankle</strong> Surg. 2008; 47(2):125-137.<br />
7. Klammer G, Baumann G, Kaspar Moor B, Farshad M, Esp<strong>in</strong>osa N. Early complication and recurrence<br />
rates after kirschner wire transfixation <strong>in</strong> lesser toe surgery: a prospective randomized study. <strong>Foot</strong> <strong>Ankle</strong><br />
Int. 2012; 33(2):105-112.<br />
8. Coughl<strong>in</strong> MJ. Second metatarsophalangeal jo<strong>in</strong>t <strong>in</strong>stability <strong>in</strong> the athlete. <strong>Foot</strong> <strong>Ankle</strong>. 1993; 14:309-319.<br />
9. Cruveilhier J. The Anatomy of the Human Body. Harper & Bros, New York, 1844, pp. 176.<br />
10. Sta<strong>in</strong>sby GD. Pathological anatomy and dynamic offect of the displaced paltnar plate and the<br />
importance of the <strong>in</strong>tegrity of the plantar plate-deep transverse <strong>in</strong>termetatarsal ligament tie-bar. Ann R<br />
Coll Surg Engl. 1997; 79:58-68.<br />
11. Bhatia D, Myerson MS, Curtis MJ, Cunn<strong>in</strong>gham BW, J<strong>in</strong>nah RH. Anatomical restra<strong>in</strong>ts to dislocation<br />
of the second metatarsophalangeal jo<strong>in</strong>t and assessment for repair technique. JBJS. 1994; 76A(9):1371-<br />
1375.<br />
12. Coughl<strong>in</strong> M, Schutt SA, Hirose CB, et al. Metatarsophalangeal jo<strong>in</strong>t pathology <strong>in</strong> crossover second toe<br />
deformity: a cadaveric study. <strong>Foot</strong> <strong>Ankle</strong> Int. 2012; 33(2):133-140.<br />
13. Kier R, Abrahamian H, Cam<strong>in</strong>ear D, et al. MR arthrography of the second and third<br />
metatarsophalangeal jo<strong>in</strong>ts for the detection of tears of the plantar plate and jo<strong>in</strong>t capsule. AJR Am J<br />
Roentgenol. 2010; 194(4):1079-81.<br />
14. Gregg J, Silberste<strong>in</strong> M, Schneider T, Marks P. Sonographic and MRI evaluation of the plantar plate: A<br />
prospective study. Eur Radiol. 2006; 16(12):2661-9. Epub 2006 Jul 4.<br />
15. Sung W, Burns P, Wukich D. Radiographic outcomes of primary first metatarsophalangeal jo<strong>in</strong>t<br />
arthrodesis for hallux abductovalgus deformities. E-Poster Competition, 26th Annual Summer Meet<strong>in</strong>g of<br />
the American Orthopaedic <strong>Foot</strong> & <strong>Ankle</strong> Society, July 7-10, 2010
weil4feet.com<br />
(847) 390.7666<br />
16. Coughl<strong>in</strong> MJ, Baumfeld DS, Nery C. Second MTP jo<strong>in</strong>t <strong>in</strong>stability: grad<strong>in</strong>g of the deformity and<br />
description of surgical repair of capsular <strong>in</strong>sufficiency. Phys Sportsmed. 2011; 39(3):132-41.<br />
17. <strong>Weil</strong> L Jr, Sung W, <strong>Weil</strong> LS Sr, Mal<strong>in</strong>oski K. Anatomic plantar plate repair us<strong>in</strong>g the <strong>Weil</strong> metatarsal<br />
osteotomy approach. <strong>Foot</strong> <strong>Ankle</strong> Spec. 2011; 4(3):145-50.