Book 35 - EMS Field Manual - LAFD Training
Book 35 - EMS Field Manual - LAFD Training
Book 35 - EMS Field Manual - LAFD Training
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
I<br />
I<br />
Preface<br />
The <strong>EMS</strong> <strong>Field</strong> <strong>Manual</strong>, <strong>LAFD</strong> <strong>Book</strong> <strong>35</strong>, is intended to serve as a convenient<br />
reference for all Advanced Life Support (ALS) and Basic Life Support (BLS)<br />
Fire Department personnel.<br />
The condensed information contained herein was generated from existing<br />
policies and procedures that govern <strong>LAFD</strong> <strong>EMS</strong> operations. Members are<br />
required to maintain a thorough knowledge of Department of Health Services<br />
(DHS) and <strong>LAFD</strong> policies and procedures. To maintain a high standard of<br />
expertise, as qualified health care professionals, a periodic review of these<br />
writings is recommended.<br />
Excerpts from the (DHS) Prehospital Care Policy <strong>Manual</strong> (<strong>LAFD</strong> <strong>Book</strong> 33),<br />
DHS Medical Guidelines, <strong>LAFD</strong> <strong>Training</strong> Bulletins, Departmental Bulletins,<br />
<strong>LAFD</strong> <strong>Manual</strong> of Operation, and <strong>EMS</strong> Updates were utilized in the compilation<br />
of this manual.<br />
<strong>Book</strong> <strong>35</strong> is subject to periodic revisions as policy andlor procedures change.<br />
If field personnel identify areas that may require clarification or revision, please<br />
contact the Quality Improvement Section at (2 13) 485-7 153.
'<br />
<strong>EMS</strong> <strong>Field</strong> <strong>Manual</strong> (<strong>Book</strong> <strong>35</strong>)<br />
TABLE of CONTENTS<br />
FIELD PROCEDURES / PROTOCOLS<br />
<strong>LAFD</strong> Patient Assessment Guidelines<br />
Simple Triage and Rapid Treatment (START)<br />
Acute Life Threatening Event (ALTE)<br />
Broselow Pediatric Emergency Tape 1 PEDS Color Code<br />
Patient Resolution Guide (PRG)<br />
PRG Principles<br />
Level of Consciousness<br />
Glasgow Coma Scale<br />
Revised Trauma Score<br />
Patient Refusal of Treatment andlor Transportation (AMA) I In Custody<br />
Child I Elder I Dependent Adult Abuse Reporting<br />
Determination of Death<br />
Patients Determined to be Dead<br />
Medical Patients in Cardiopulmonary Arrest<br />
Crime ScenesIAccidental DeathsISuspected Suicides<br />
Procedures Following Pronouncement of Death<br />
Documentation for Reports<br />
Prehospital Do-Not-Resuscitate (DNR) Orders<br />
Honoring Advance Health Care Directives (AHCD)<br />
Task Oriented <strong>EMS</strong> Standard Operating Guidelines (SOGs) [TasksIEquipment]<br />
Size-Ups<br />
SOGs for <strong>EMS</strong> Incidents (e.g., Cardiac Arrest, Trauma, Medical Complaint)<br />
Patient Transfer of Care from ALS to BLS<br />
EMT-1 Expanded Scope of Practice<br />
Poison Control System<br />
System-wide Mental Assessment Response Team (SMART)<br />
City Volunteer Programs<br />
Miscellaneous I Communications During Emergencies<br />
Highest Ranking Medical Authority<br />
Body Armor Vests<br />
Medical Waste Disposal<br />
Management of Multiple Victim Incidents I MCI Short Form<br />
Revised: 512005<br />
PAGE 1 OF 3<br />
SECTION 1<br />
1.0<br />
1. 1<br />
1.2<br />
1. 2a<br />
1.3<br />
1. 3a<br />
1.4<br />
1.4a<br />
1.4b<br />
1.5<br />
1. 6<br />
1.7<br />
1. 7a<br />
1. 7b<br />
1.7~<br />
1. 7d<br />
1. 7e<br />
1. 8<br />
1. 8a<br />
1.9<br />
1. 9a<br />
1. 9b<br />
1.10<br />
1.11<br />
1. 12<br />
1.12a<br />
1. 13<br />
1. 14<br />
1.14a<br />
1.14b<br />
1.14~<br />
1. 15
<strong>EMS</strong> <strong>Field</strong> <strong>Manual</strong> (<strong>Book</strong> <strong>35</strong>)<br />
TABLE of CONTENTS<br />
PATIENT TRANSPORTATION 1 DESTINATION<br />
<strong>LAFD</strong> Patient Destination Guidelines /General Principles<br />
Patients Transported by BLS Personnel<br />
Patients Transported by ALS Personnel<br />
Transport to Specialty Care Centers: SART Centers, Trauma Centers, Trauma<br />
Triage CriteriaIGuidelines, Extremis Patients<br />
Trauma Catchment / Boundary Areas<br />
Pediatric Trauma Centers<br />
LA County Trauma Center Maps<br />
Trauma Center Diversion / EDAP I PMC / PTC / Perinatal<br />
Burn Patients / Decompression<br />
Patient Destination Guidelines / EDAP / Patient Requests / Hospital Diversion<br />
Transporting Patients in Custody<br />
Hospital Refusal to Accept Rescue Ambulance Patients<br />
Service Area Hospitals Specialties / Exceptions<br />
Service Area Hospital Maps<br />
Los Angeles County Emergency Medical Service Receiving Facilities<br />
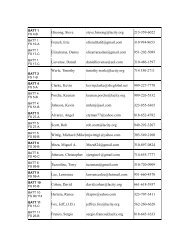
<strong>EMS</strong> and Battalion Offices<br />
Receiving Hospitals Sorted by <strong>EMS</strong> Battalion Captains<br />
Fire Station, Battalion, Division, <strong>EMS</strong> Battalion Chart<br />
<strong>LAFD</strong> Rescue Ambulance Locations<br />
APPARATUS 1 EQUIPMENT<br />
Apparatus Towing Apparatus Breakdown Procedures 1 Documentation<br />
Apparatus Maintenance<br />
CAV and NAV<br />
Obtaining a Spare Gurney<br />
Multi-Casualty Medical Supply Cache<br />
Disaster Cache Box (Amy1 Nitrite I Mark I Kit)<br />
Base Hospital Hailing and Working Channel Assignments<br />
Revised: 512005 PAGE 2 OF 3<br />
SECTION 2<br />
SECTION 3
Records and Documentation<br />
The Journal (F-2)<br />
<strong>EMS</strong> <strong>Field</strong> ~ akal (<strong>Book</strong> <strong>35</strong>)<br />
TABLE of CONTENTS<br />
RECORDS / DOCUMENTATION<br />
Hazardous Substance Exposure Report (F-3)<br />
Stores Requisition (F-80)<br />
Rescue Equipment Loan Slip (F-215M)<br />
<strong>EMS</strong> Report (F-902M)<br />
Controlled Medication Inventory (F-903)<br />
<strong>LAFD</strong> Situation Report (F-904)<br />
The Health Insurance Portability and Accountability Act (HIPAA)<br />
CAL I OSHA and FED I OSHA Notifications<br />
Communicable Disease Exposure (Contaminated Needle Puncture)<br />
Procedures I Exposure Categories<br />
, Communicable Disease Exposure and Notification Report (F-420)<br />
1<br />
' Communicable Disease Decontamination<br />
Suspected Child AbuseINeglect Reporting Guidelines<br />
Suspected Elder and Dependent Adult Abuse Reporting Guidelines<br />
Communication Failure Protocol<br />
Mnemonics<br />
Abbreviations<br />
Bibliography<br />
Record of Revisions<br />
Revised: 512005 PAGE 3 OF 3<br />
SECTION 4<br />
4. 0
\<br />
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
<strong>LAFD</strong> PATIENT ASSESSMENT GUIDELINES<br />
^ SCENE<br />
 Safety (BSI PrccautionsJPPE)<br />
+ Environment<br />
 Mechanism of Injury<br />
+ Number of Patients<br />
^ GENERAL IMPRESSION<br />
+ What you see!<br />
^ AIRWAY<br />
4 P U LS E (Rate, Rhythm, Quality)<br />
4 RESPIRATION (Rate, Rhythm, TV)<br />
4 B P (Systolic/Diastolic) [Orthostatic's PRN]<br />
^ BREATHING (AssistfOxygen)<br />
^ CIRCULATION (RadialICarotid)<br />
+ Pulses<br />
+ Capillary Refill<br />
+ Control Severe Bleeding (PRN)<br />
- j COMPLETE BODY CHECK<br />
/ SKIN SIGNS<br />
+ Color<br />
+ Temperature<br />
+ Moisture<br />
^ CHIEF COMPLAINT<br />
(SignsISymptoms)<br />
+ Objective Observation<br />
+ Subjective Findings<br />
(What they say!)<br />
FIRST- PERFORM FOCUSED BODY CHECK<br />
(Determined by LOG, Chief Complaint, and History)<br />
Glasgow Coma Scale (GCS)<br />
ASSESS BILATERAL BREATH SOUNDS<br />
for patients with chest injuries, difficulty<br />
breathing, and I or signs of shock<br />
LO 0 K for Tissue Damage, Scars, Deformities, Abnormal Behavior I Motion, Fluids<br />
F E EL for Tenderness, Instability, Crepitus<br />
4 HEAD 4 BREATHSOUNDS 4 NEUROLOGICAL<br />
4 NECK 4 ABDOMENIPELVIS 4 BACK<br />
4 CHEST 4 EXTREMITIES (UpperILower) 4 MEDICAL TAGS,<br />
TRACKS, TRAUMA<br />
DEFORMITY BURNS<br />
CONTUSION TENDERNESS<br />
ABRASION LACERATIONS<br />
PUNCTURE1 SWELLING<br />
PENETRATING<br />
PULSES<br />
MOTOR<br />
SENSORY<br />
Revised: 121200 1
Section I: <strong>Field</strong> Procedures 1 Protocols<br />
<strong>LAFD</strong> PATIENT ASSESSMENT GUIDELINES<br />
S SignsISymptoms<br />
A Allergies<br />
M Medications<br />
P Past History<br />
L Last AteIDrank<br />
E Events Preceding<br />
FOCUSED HISTORY<br />
0 Onset<br />
P Provokes<br />
Q Quality<br />
RegionIRadiationl<br />
Recurrence<br />
S Severity<br />
T Time<br />
Alcohol1 Apneal<br />
A Anaphylaxis1<br />
E EpilepsyIEnvironment<br />
/ Insulin<br />
0 Overdose<br />
U Uremialunderdose<br />
T Trauma<br />
1 Infection<br />
StrokeIShockl<br />
Seizure<br />
C Cardiovascular<br />
AIRWAY (OIP, Mask) SPINAL PRECAUTION<br />
BREATHING (Position I BVM 102) GLUCOSE<br />
CIRCULATION (Direct Pressure I Position Patient) OB ASSISTANCE<br />
CONTROL BLEEDING BANDAGING 1 SPLINTING<br />
REPEAT.<br />
Initial and Focused exam:<br />
Priority patients every 5 minutes<br />
Stable patients every 15 minutes<br />
Have a Plan! Route! Code 3?<br />
Treatment En Route?<br />
ONGOING ASSESSMENT<br />
à Motor Response<br />
1 Ã Verbal Response 1<br />
REVISED TRAUMA SCORE (RTS)<br />
,- . ... .<br />
(Uoded Values)<br />
SBP + RR + GCS<br />
Revised: 1212001
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
SIMPLE TRIAGE and RAPID TREATMENT<br />
-\ START<br />
,<br />
b -<br />
REPOSITION<br />
ASSESS<br />
RespiratiodRate ABSENT<br />
ASSESS<br />
Circulation<br />
0<br />
< 2 sec. /<br />
RADIAL PULSE<br />
PRESENT<br />
I Y<br />
ASSESS<br />
Mental Status<br />
*<br />
Airway and<br />
REASSESS<br />
Respiration<br />
Simple Triage and Rapid Treatment<br />
Revised: 121200 1
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
ACUTE LIFE-THREATENING EVENT (ALTE)<br />
An ALTE may occur during sleep, wakefulness, or feeding in the pediatric patient. It is described as an<br />
episode that is frightening to the observer and characterized by a COMBINATION of:<br />
* Transient Apnea<br />
* Color Change<br />
* Marked Muscle Tone Changes<br />
* Choking 1 Gagging<br />
Upon <strong>EMS</strong> arrival this pediatric patient may appear completely normal and asymptomatic. However,<br />
a complete and accurate history of the event is critical in determining ALTE.<br />
Base Hospital contact is required. If the circumstances surrounding the incident are vaguelunclear it<br />
is the base station MICNs responsibility to determine the appropriate destination for the patient.<br />
ALTE may be a symptom of many specific disorders including, but not limited to, gastrointestinal<br />
reflux, infection, seizures, airway abnormality, hypoglycemia, metabolic problems, or impaired<br />
regulation of breathing during sleep and feeding. ALTE was previously called a "Near-miss SIDS."<br />
THE MOST IMPORTANT DIAGNOSTIC STEP IS TO OBTAIN A CAREFUL HISTORY<br />
OF THE CURRENT COMPLAINT FROM THE PERSON WHO WITNESSED THE EVENT.<br />
The evaluation and history taking for ALTE patientsconsists of:<br />
* Color (red, pale, cyanotic)<br />
* Respiratory Effort (apnea, obstruction, irregular)<br />
* Sleep Status (awake, asleep)<br />
* PositionMotor (prone, supine, uprightllimpness)<br />
* Breathing PatternINoises (choking, stridor)<br />
* Eye Movement (closed, startled, rolled, fluttering)<br />
* Relationship to Feeding<br />
* Fluid in the Mouth<br />
* Duration<br />
* Need for Intervention<br />
* Age 1-3 years: Base Contact andor Transport is required.<br />
Age 0- 12 months: Transport regardless of chief complaint andor mechanism of injury.<br />
' ALTE patients age 12 months and under: BASE CONTACT g.mJ TRANSPORT to a PCCC is required.<br />
Revised: 121200 1<br />
PAGE 1 OF 2
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
BROSELOW PEDIATRIC EMERGENCY TAPE<br />
The Broselow Pediatric Emergency Tape is a mandatory piece of equipment carried on all ALS<br />
units in Los Angeles County. The Broselow Tape is used to estimate weight, drug dosages, and<br />
correct size of equipment for pediatric patients up to 74 pounds [34 kg]. It is mandatory to use<br />
the Broselow Tape on all ALS pediatric patients. [Refer to "<strong>EMS</strong> Update 2001 '7<br />
After determining the correct color code, document the three-digit color code in the Peds Color<br />
Code Box, Incident Info Section of the <strong>EMS</strong> Report [F-902Ml. For billing purposes, convert the<br />
kilograms to pounds and document in the weight box. Use only the color code when reporting to<br />
the Base Hospital.<br />
The color coding system is designed to reduce calculation errors associated with medication<br />
administration. If the infant's size falls into the "gray" area [first section of the tape: 3 kg.,<br />
4 kg., or 5 kg.] it is necessary to report the specific weight and color to the Base Hospital.<br />
For all other color coded sections it is only required to report the color code.<br />
GY3<br />
YEL<br />
GY4<br />
WHT<br />
Placement of the Broselow Tape for measuring from the<br />
standing or supine position is as follows :<br />
Place the RED end of the tape for.. ....<br />
STAND IN G : To the heel of the foot and measure to the<br />
top of the head.<br />
SUPINE: To the top of the head and measure to the<br />
heel of the foot [while extending the leg].<br />
Note:<br />
The pediatric drug dosages are only to be taken from the "Color Code Drug Doses<br />
LA County Kids" (laminated cards) that are carried on each ALS unit.<br />
THE BROSELOW TAPE IS ONLY TO BE USED TO DETERMINE THE COLOR CODE.<br />
Revised: 512005<br />
GY5<br />
BLU<br />
PAGE 2 OF 2<br />
PNK<br />
ORG<br />
RED<br />
GUN<br />
PUR<br />
-
LEVEL of CONSCIOUSNESS<br />
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
<strong>EMS</strong> personnel shall perform a patient assessment to determine orientation and level of consciousness<br />
an each patient they encounter. This assessment should determine patient's state of awareness and<br />
orientation to time, place, person, or purpose [A & 0 X 3 per LA County Medical Guidelines].<br />
Inappropriate aggressiveness or hostility should alert members to the possibility that the patient's<br />
thinking process may be impaired. EMT-Is shall access an EMT-P resource any time a patient is<br />
unable to reasonably answer one or more of the following questions:<br />
^ -<br />
+ Name<br />
+ Day of the week I year I time of day<br />
+ Where helshe lives I where they are now<br />
GLASGOW COMA SCALE (GCS)<br />
ADULT (% 14 year)<br />
Spontaneous<br />
To Voice<br />
To Pain<br />
None<br />
Obedient<br />
Purposeful<br />
Withdrawal<br />
Flexion<br />
Extension<br />
None<br />
Oriented<br />
Confusion<br />
Inappropriate<br />
Incomprehensible<br />
None<br />
21 HLD (12 months to 14 years)<br />
Spontaneous<br />
To Voice<br />
To Pain<br />
None<br />
-<br />
Obedient<br />
Localizes<br />
Withdrawal<br />
Flexion<br />
Extension<br />
None<br />
-<br />
5 Oriented<br />
4 I Confusion<br />
3 Inappropriate<br />
2 Incomprehensible<br />
1 1 None<br />
In addition to the numerical Glasgow Coma Scale (GCS), document a brief descriptive assessment<br />
on the <strong>EMS</strong> Report Form (F-902M) .<br />
The GCS is required to assess neurological status on all patients greater than twelve (12) months of<br />
age. This includes patients who do not have an altered level of consciousness.<br />
After consultation with the primary care giver, the patient examiner shall estimate the appropriate-<br />
ness of the response for the younger child that is not able to communicate (motor response-obedient<br />
and verbal response-oriented).<br />
Revised: 512005 PAGE 1 OF 2
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
REVISED TRAUMA SCORE (RTS)<br />
The Revised Trauma Score (RTS) is a physiological scoring system to determine the survival<br />
probability of trauma patients. If the patient (age one year and above) meets trauma center criteria<br />
and is transported to a Trauma Center or PTC the RTS shall be completed and documented on the<br />
<strong>EMS</strong> Report Form (F-902M).<br />
THREE assessment elements comprise the RTS:<br />
+ SYSTOLIC BLOOD PRESSURE (SBP)<br />
+ RESPIRATORY RATE (RR)<br />
+ GLASGOW COMA SCALE (GCS)<br />
ASSESSMENT ELEMENT IS GIVEN A "CODED VALUE" (CV).<br />
THE "CVS" ARE THEN TOTALED TO GIVE THE RTS ("0-12").<br />
The "coded value" (sum) of the: SBP + RR + GCS = R T S<br />
RTS = (2+2+3)<br />
CALCULATING<br />
Nx: If unable to auscultate or palpate a blood pressure due to hypo-perfusion7 enter a value of "1 ."<br />
(The lower the score the more critical the patient.)<br />
Document the rational for a palpated blood pressure in the F-902M Comments section .<br />
Revised: 512005<br />
The RTS is heavily weighted toward the GCS to compensate for major head injury<br />
without multi-system trauma or major physiological changes.
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
PATIENT REFUSAL of TREATMENT 1 TRANSPORTATION<br />
EMT-Is may allow a patient to refuse treatment I transport if glJ the following conditions are met:<br />
The patient's condition does not meet any criteria on the Patient Resolution Guide (PRG).<br />
* The patient does not meet altered level of consciousness criteria as described in DHS, Ref. No. 809.<br />
The patient understands the severity of their condition and has a plan for follow-up medical care.<br />
Patient understands and signs the F-902M in the space provided. Additionally, the patient receives<br />
the Patient After Care Instruction form [back of the F-902M Pink copy].<br />
Note: IF THE PATIENT DOES NOT MEET THE ABOVE CRITERIA, AN ALS RESOURCE SHALL<br />
BE REQUESTED TO DOCUMENT THE PATIENT'S REFUSAL (AMA). A PARAMEDIC<br />
WORKING ON A BLS RESOURCE MAY NOT HANDLE AMA'S IN LIEU OF AN ALS RESOURCE.<br />
* A BLS resource shall request a Paramedic RA.<br />
* EMT RA shall request the closest ALS resource e.g., Paramedic Engine, ALS RA.<br />
The ALS resource shall make base hospital contact while with the patient.<br />
Advise base hospital of all circumstances, patient's condition, and the reason for refusal.<br />
* Have the patient or legal guardian sign the AMA form [back of the F-902M White copy]. If the patient<br />
refuses to sign the AMA form, this shall be documented in the Comments section of the F-902M.<br />
.'\<br />
Refer to <strong>Book</strong> <strong>35</strong>, Section 2.0: "Patient Destination Guidelines".<br />
An <strong>EMS</strong> Battalion Captain shall be requested to respond to the incident if the Paramedics are<br />
uncomfortable with any aspect of the AMA. (Dept. Bulletin No. 01-10)<br />
, PATIENTS IN CUSTODY<br />
. Patients under the care or in custody of law enforcement often pose a challenge for pre-hospital care<br />
providers. These patients represent a very high degree of medical-legal risk. Patient care,<br />
documentation, and transportation must be in accordance with existing policies and procedures.<br />
Members are required to conduct a complete Initial and Focused assessment which includes vital signs,<br />
pertinent negative findings and a statement on the F-902M (<strong>EMS</strong> Report) which outlines the chief<br />
complaint and/or the reason for the 9- 1 - 1 call. Members must remember that the history on these<br />
patients should be suspect due to the possibility of the patient being under the influence of illicit drugs,<br />
may not have access to their prescription medications, or may have sustained trauma with no obvious<br />
signs or symptoms; and patient care should not be based solely upon the history obtained.<br />
All members are reminded that patients in custody may refuse care BUT cannot refuse transportation to an<br />
emergency department for evaluation. Patients who refuse treatmentltransport and whose chief complaints<br />
meet the PRO Section I and I1 or Reference 808 criteria require transport and/or base hospital contact.<br />
Transporting Restrained Patient's (Reference No. 838)<br />
Restraint equipment (handcuffs, plastic ties, or "hobble" restraints) applied by law enforcement officer:<br />
Must provide sufficient slack to allow patient to take full tidal volume breaths.<br />
Requires the officers continued presence (the officer shall accompany the patient in the ambulance)<br />
Must not compromise the patients respiratory/circulatory systems. (Transport patient in supine position.)<br />
Must not cause vascular, neurological, or respiratory compromise.<br />
Patient's restrained extremities shall be evaluated for pulse quality, capillary refill, color and temperature,<br />
nerve and motor function immediately following application and every 15 minutes thereafter.<br />
Documentation is necessary to justify actions done or not done if unable to perform the above.<br />
Restraints may be attached to the frame of the gurney but not to the movable side rails.<br />
Revised: 512005 PAGE 1 OF 1
CHILD / ELDER / DEPENDENT ADULT ABUSE<br />
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
EMT-Is and EMT-Ps are required to report all cases of suspected abuse and/or neglect as soon as possible.<br />
ABUSE<br />
NEGLECT<br />
CHILD<br />
ELDER<br />
, ,<br />
punishment, willful cruelty, unjustifiable<br />
punishment, or sexual assault.<br />
Failure of any person having the care and/<br />
or custody of a child, elder, or dependent<br />
adult to exercise that degree of care which<br />
a reasonable person in a like position<br />
would exercise.<br />
Any person between the ages of 18 and<br />
64 years that cannot fully care for<br />
DEPENDENT<br />
-<br />
himherself due to physical and/or<br />
ADULT mental limitations.<br />
1. Request OCD to notify and have the<br />
appropriate law enforcement agency<br />
report to the incident location or hospital<br />
if the patient is to be transported.<br />
2- The law enforcement agency will assign an<br />
investigator. If the patient does not require<br />
immediate transport wait for the responding<br />
law enforcement agency unless a responsible<br />
Any person under 18 years old. I1<br />
adult (other than the abuser) remains on scene.<br />
3. The member in charge of patient care shall<br />
Any person 65 years old or older.<br />
forward the completed Department of Social<br />
Services Report to the appropriate <strong>EMS</strong><br />
Battalion Captain within 36 hours.<br />
4. Make a Journal (F-2) entry, that shows the<br />
, report was completed and forwarded.<br />
NB: While on scene obtain names, addresses, and telephone numbers of witnesses, victims, siblings, parents,<br />
and law enforcement / investigating officer (s) involved with the incident,<br />
<strong>Field</strong> members may obtain copies of the Social Services (8572) form "Suspected ChildAbuse Report" from<br />
the concerned <strong>EMS</strong> Battalion Captain or find the form listed in the Prehospital Care Policy <strong>Manual</strong>, <strong>Book</strong> 33,<br />
Reference No. 822.2. The Social Services form "Suspected Dependent Adult/Elder Abuse " may also be found<br />
in <strong>Book</strong> 33, Reference No. 829.2.<br />
Revised: 712003<br />
\
DETERMINATION OF DEATH<br />
A patient may be determined dead if in addition to the absence of respiration, cardiac activity, and<br />
\ neurological reflexes, one or more of the following conditions exists (DHS, Reference # 814):<br />
)<br />
+ Decapitation.<br />
+ Massive crush injury.<br />
+ Penetrating or blunt injury with evisceration of the heart, lung, or brain.<br />
+ Decomposition.<br />
4 Incineration.<br />
+ Extrication time greater than 15 minutes, with no resuscitative measures performed prior to extrication.<br />
+ Pulseless, non-breathing victims of a multiple victim incident where insufficient medical resources<br />
precluded initiating resuscitative measures.<br />
+ Drowning victims, when it is reasonably determined that submersion has been greater than one hour.<br />
-<br />
+ Rigor mortis requires assessment (as described in Section 1.7a ).<br />
Patients Determined to be Dead<br />
If the initial assessment reveals rigor mortis andor post-mortem lividity &,<br />
<strong>EMS</strong> personnel shall perform the following assessments:<br />
(NN: Assessment steps may be performed concurrently.)<br />
RESPIRATORY<br />
* Assuring that the patient has an open airway<br />
* Look, listen, and feel for respiration<br />
(This includes auscultation of the lungs for a minimum of 30 seconds)<br />
CARDIAC<br />
* Auscultation of the apical pulse for a minimum of 60 seconds<br />
* Adults and children: Palpation of the carotid pulse for a minimum of 60 seconds<br />
Infants: Palpation of the brachial pulse for a minimum of 60 seconds<br />
NEUROLOGICAL<br />
* Assess pupil response with a penlight or flashlight<br />
* Check for a response to painful stimuli<br />
Resuscitative measures shall not be initiated on patients who have been determined dead (according<br />
A to this policy) or on patients who meet DHS, ~ ef. No. 815, "Honoring Prehospital DNR Orders"<br />
Medical Patients in Cardiopulmonary Arrest<br />
Initiate immediate resuscitation and ALS intervention for patients who do not meet<br />
conditions described in Section 1.7. In general, these patients shall be:<br />
* Treated in the field long enough for possible resuscitation to occur.<br />
, * Rapidly transported if an adequate airway or venous access cannot be established.<br />
* Treated and transported if the patient is: A suspected drug overdose, hypothermic,<br />
in refractory ventricular fibrillation or ventricular tachycardia.<br />
Revised: 1212001 PAGE 1 OF 2
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
Crime Scenes I Accidental Deaths I Suspected Suicides<br />
+ Responsibility for patient health care management rests with the most medically qualified<br />
person on scene.<br />
+ Authority for crime scene management shall be vested in law enforcement. It may be necessary<br />
to ask law enforcement officers for assistance to create a "safe path" into the scene to access the<br />
patient, while minimizing scene contamination.<br />
+ If law enforcement is not on scene, prehospital care personnel shall attempt to create a "safe path"<br />
and secure the scene until their arrival.<br />
Procedures Following Determination of Death<br />
All therapeutic modalities initiated during the resuscitation must be left in place.<br />
(This includes ET 1 ETC tubes, IV catheters, EKG electrodes, and oral 1 nasal pharayngeal airways.)<br />
The deceased shall not be moved without the Coroner's authorization.<br />
- 1<br />
NB: It may be necessary to move the deceased if the scene is unsafe or if the deceased is creating a ,'<br />
hazard. In such emergent situations, field personnel may relocate the deceased to a safer<br />
location or transport to the most accessible receiving facility.<br />
Documentation for Reports<br />
+ The criteria used to determine death. (Listed in Section 1.7a.)<br />
 The condition of the patient and what, if any, resuscitation interventions were initiated.<br />
+ If the deceased was moved, document the location and the reason why. If movement of the<br />
deceased was authorized by the Coroner document: The case number and the representative<br />
who authorized the movement.<br />
--<br />
Revised: 121200 1
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
PREHOSPITAL DO-NOT-RESUSCITATE (DNR) ORDERS<br />
' -\<br />
, FOR PULSELESS AND APNEIC PATIENTS WITH VALID DNR ORDERS:<br />
EMT-Is shall a begin CPR or attach defibrillator<br />
EMT-Ps shall a begin CPR or attempt ALS procedures (Combi-tube, ET, cardiotonic drugs, etc.)<br />
1. Identification by witness who can absolutely<br />
identify patient/ID bands; and<br />
2. Written physicians order in patient's chart,<br />
such as:<br />
 No Code<br />
 NoCPR<br />
+ Do-Not-Resuscitate; or<br />
3. Verbal physician's order (in person) which<br />
must be followed immediately in writing.<br />
1. Check the "DNR" box on the F-902M,<br />
(<strong>EMS</strong> Report form).<br />
2. Briefly describe in the Comments section:<br />
 Any care given<br />
 The physician's name and telephone<br />
number<br />
 The date the DNR order was originally<br />
signed<br />
3. Attach a photocopy of the facility's DNR<br />
order to the F-902M (White copy).<br />
1. Identification by witness who can absolutely<br />
identify patient1ID bands; and<br />
2. Presence of an original (or copy):<br />
 Los Angeles County Do-Not-Resuscitate<br />
(DNR) Form (Ref No. 81 5.1)<br />
 State Prehospital Do-Not-Resuscitate<br />
(DNR) Form (Ref No. 815.2)<br />
1. Check the "DNR" box on the F-902M<br />
(<strong>EMS</strong> Report form).<br />
2. Briefly describe in the Comments section:<br />
 Any care given<br />
 The physician's name and telephone<br />
number<br />
. Â The date the DNR order was originally<br />
signed<br />
3. If available, attach page 2 of the DNR form<br />
(provider agency copy) to the F-902M (White<br />
copy) prior to forwarding. If the provider<br />
agency copy or photocopy is not available,<br />
record all DNR information on the F-902M.<br />
Do a take the patient's copy if it is the only<br />
copy on scene.<br />
In the prehospital setting, a Living Will or Durable Power of Attorney are non-acceptable DNR forms.<br />
Revised: 121200 1 PAGE 1 OF 2
A Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
PREHOSPITAL DO-NOT-RESUSCITATE (DNR) ORD'ERS<br />
Resuscitation shall begin immediately and paramedics shall contact the base hospital for further<br />
direction if there is any objection or disagreement by family members or caretakers about withholding<br />
resuscitation; or if prehospital personnel have any reservations about the validity of the DNR order.<br />
For patients who are a pulseless and apneic with valid DNR orders, EMT-Is and EMT-Ps shall<br />
provide for their comfort, safety, and dignity by using the following appropriate supportive measures:<br />
EMT-IS:<br />
+ Maintain Airway (Oropharyngeal 1 Nasopharyngeal Airways) and Suctioning<br />
+ Administer Oxygen<br />
+ Control External Hemorrhage<br />
+ Apply Dressings, Bandages, and Slings<br />
+ Immobilize Skeletal Injuries<br />
+ Position of Comfort<br />
E M T - P s : (In addition to the above)<br />
+ Visualize airwaylremove foreign bodies by means of a laryngoscope and Magill forceps<br />
+ Contact base hospital if IV access andlor pain medication is necessary<br />
* In the event of deterioration of the patient's vital signs, level of consciousness, or of<br />
cardiopulmonary arrest, continue transporting to the designated receiving facility (even<br />
though it may not be the most accessible). Transport to the patient's requested treating<br />
facility.<br />
* If the patient's caretaker is unable to provide care, advise transport.<br />
(A private ambulance may be suggested.)<br />
* Generally, emergency transport is not necessary but left to the discretion of <strong>EMS</strong> personnel.<br />
(Emergency transportation may be necessary for such cases as hemorrhage, unmanaged<br />
airway, severe pain, etc.). (DHS, Reference # 8 15)<br />
Revised: 121200 1 PAGE 2 OF 2
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
ADVANCED HEALTH CARE DIRECTIVES (AHCD)<br />
California law on AHCDs recognizes that adults have the fundamental right to control the decisions<br />
relating to their own health care, including the decision to have life-sustaining treatment withheld or<br />
withdrawn. The AHCD enables patients (over the age of 18) who are unable to speak for themselves<br />
(e.g., coma, Alzheimer's, etc) to provide their health care instructions.<br />
A VALID AHCD MUST MEET THE FOLLOWING REQUIREMENTS:<br />
4 Patient is unable to make their own life decisions<br />
d Power-of-Attorney Health Care Agent is designated with effective DATE<br />
d End of Life Decision box is designated (checked)<br />
d Two witness signatures and DATED, or<br />
d Notary Public<br />
d Signed by a Patient Advocate or Ombudsman if the patient is in a skilled nursing facility<br />
Note: An AHCH has reciprocity between states and must be honored if all the above are completed.<br />
If the patient's caretaker is unable to provide care, advise transport. (A private ambulance may be suggested.)<br />
Generally, emergency transport is not necessary but left to the discretion of <strong>EMS</strong> personnel.<br />
Emergency transportation may be necessary for such cases as<br />
hemorrhage, unmanaged airway, severe pain, etc. (DHS, Reference # 81 8)<br />
GUIDELINES FOR PREHOSPITAL CARE PERSONNEL:<br />
Provide the level of care according to the patient's wishes and/or medical condition when<br />
dealing with Advanced Health Care Directives and bbDo-Not-Resuscitate (DNR)" orders.<br />
_ AJ-S and BLS shall provide for the patient's comfort, safety, and dignity by using<br />
(he following appropriate measures:<br />
+ ASSIST VENTILATIONS (via a bag-valve-mask device)<br />
+ CHEST COMPRESSIONS<br />
+ AUTOMATED EXTERNAL DEFIBRILLATOR (AED)<br />
(only ifBLS is on scene prior to the arrival of ALS)<br />
pulmonary resuscitation,<br />
defibrillation, drug therapy,<br />
and other life saving measures.<br />
+ ADVANCE AIRWAY + CARDIAC DRUGS:<br />
MANAGEMENT Adenosine Epinephrine<br />
+ DEFIBRILLATION Atropine Lidocaine<br />
+ CARDIOVERSION Dopamine<br />
+ AIRWAY MANEUVERS (including removal offoreign body) + HYDRATION 1 DIURESIS<br />
SUCTIONING + GLUCOSE ADMINISTRATION<br />
+ OXYGEN ADMINISTRATION + PAIN CONTROL (i. e., morphine)<br />
+ HEMORRHAGE CONTROL<br />
Revised: 812003 PAGE 1 OF 1
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
TASK ORIENTED <strong>EMS</strong> STANDARD OPERATING GUIDELINES<br />
<strong>EMS</strong> Standard Operating Guidelines (SOGs) are intended as guidelines to establish pre-determined<br />
, tasks for each member of the company. Company Commanders shall assign taskslresponsibilities<br />
based upon the expertise of each team member. Additionally, the tasks designated for each of the<br />
following four positions are not intended to supersede any pre-existing duties assigned to the member.<br />
The medical condition of the patient determines the work flow and sequencing of tasks.<br />
\<br />
. ./Â¥<br />
A-B<br />
Person<br />
c<br />
Person<br />
D<br />
Person<br />
E<br />
Person<br />
The "A-B" (Airway-Breathing) person who assesses the airway; applies oxygen;<br />
determines the respiratory rateltidal volume; and any signs of distress while<br />
checking breath sounds. In cases of cardiac or respiratory arrest, the "A-B" person<br />
inserts the airway and performs bag-valve-mask (BVM) ventilation.<br />
The "C" (Circulation) person is responsible for preserving the circulation by stopping<br />
any overt bleeding, and obtains the pulselrate and blood pressure. For pulseless patients:<br />
applies the automated external defibrillator (AED); attempts defibrillation; and provides<br />
chest compressions for CPR, as necessary.<br />
The "D" (Disability) person is responsible for preventing further patient disability by<br />
assessing the current degree of disability and applies splintslspinal immobilization as<br />
necessary. In cardiac arrest cases: assists with equipment needs (such as oxygen bottles,<br />
backboard, and gurney); assists the paramedics with IV line preparation and equipment<br />
needs. In many situations, the fourth member of the company is unavailable since the<br />
Engineer has apparatus responsibilities. However, the Engineer may assist the rescue<br />
as described above and may be able to assist when the patient is outside of a structure.<br />
The "E" (Executive) person ensures that all of the other team members are properly<br />
performing their tasks. In cardiac arrest cases, the "E" person assists the "C" person<br />
set up the automated external defibrillator (AED) to ensure rapid application. The "E"<br />
person assesses the scene for safety, initiates the F-902M, keeps records of interventions<br />
and their delivery times, interacts with family members to obtainlrecord patient<br />
information which includes: medical history, allergies, a current medications list,<br />
current address (include ZIP code), and (if available) Medi-Cal number.<br />
Even when dispatched simultaneously (with an ALS unit), fire company members<br />
shall perform the above tasks (including defibrillation) as a team.<br />
Suggested personnel for each <strong>EMS</strong> team assignment and equipment to be carried to the patient:<br />
A-B<br />
c<br />
D<br />
E<br />
FF or FF/PM<br />
Firefighter<br />
Engineer or A0<br />
Captain<br />
Revised: 121200 1 PAGE 1 OF 4<br />
Oxygen, BVM, and airway<br />
managementJsuction bag<br />
AED and medical box<br />
Flashlight, splints, backboard,<br />
gurney as needed<br />
F-902M and Radio<br />
tf
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
Note: ALL personnel shall exercise good judgment and follow Department policy regarding<br />
equipment and medical supplies carried to the patient(s) on initial approach.<br />
Medicallstarter Box Medicallstarter Box Medicallstarter Box MedicallTrauma Box<br />
Oxygen Oxygen Oxygen Oxygen<br />
(with respiratory supplies) (with respiratory supplies) (with respiratory supplies) (with respiratory supplies)<br />
Defibrillator Trauma Box Disposable OB Kit Defibrillator<br />
Additionally, for incidents occurring above the first floor , the gurney shall be brought in.<br />
SIZE-UPS<br />
Size-ups shall be given to additional resources responding with the fire company.<br />
In particular, a size-up for an <strong>EMS</strong> incident shall be provided under the following conditions:<br />
+ Requests for an ALS unit when a BLS unit is dispatched for an "A" or "B" category call.<br />
+ Additional resources requested beyond the original dispatch.<br />
When multiple resources are dispatched to a single incident, the first unit on scene shall provide a<br />
brief size-up and may cancel or down grade, to non-emergency, the additional resources when<br />
appropriate. It is not uncommon for a BLS Engine, a Paramedic Assessment Engine, and a<br />
Paramedic Rescue to be dispatched on a single incident. Exercise good judgment in terms of<br />
additional resources to proceed through, and if so, whether emergency or non-emergency.<br />
In addition, if the patient is stable but still requires transport or an ALS resource for documentation<br />
only, consideration shall be given to have that resource proceed through nun-emergency.<br />
Revised: 121200 1<br />
The "<strong>EMS</strong> size-up" (given on TAC 10) shall include the following information and<br />
be very brief (vital signs normally are not included):<br />
PAGE 2 OF 4
TEAM<br />
TEAM<br />
A-B<br />
Revised: 912003<br />
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
To further describe the tasks to be performed by each team member, the following<br />
examples of <strong>EMS</strong> incidents (with the SOGs for fire personnel) are listed:<br />
COMPANY PERSONNEL<br />
FF or<br />
FFPM<br />
Firefighter<br />
Engineer<br />
or<br />
A0<br />
Captain<br />
COMPANY PERSONNEL<br />
Firelighter<br />
Engineer<br />
or<br />
A0<br />
Captain<br />
TASKS<br />
Assess airway; suction as needed; basicladvanced airway, BVM;<br />
observe for chest rise and gastric distention. Announce 10-second<br />
time intervals when the paramedic performs intubation.<br />
Utilize the automated external defibrillator (AED) to<br />
analyze EKG rhythm; defibrillate as needed; chest<br />
compressions of CPR; carotid pulse checks; if applicable,<br />
obtain the AED Code Summary and initiate the F-901<br />
(Cardiac Arrest Outcome Data Sheet).<br />
Anticipate and provide necessary equipment; direct paramedics<br />
to the patient; assist with IV line preparation; gather and<br />
properly dispose of medical waste.<br />
Supervise team; assess scene safety; assist bbC" Person with<br />
AED rapid application; interact with familyhystanders. Initiate<br />
F-902M; record patient assessment data (and times); interventions<br />
(and times); patient's medical history and list of medications,<br />
and (if available) Medi-Cal number, address (include ZIP code).<br />
Give a brief size-up to the paramedics.<br />
TASKS<br />
Administer Oxygen at 15Llmin.; auscultate lungs to determine<br />
equal breath sounds; assess: airway, rate of respirations, and<br />
tidal volume. As needed: suction, BVM, provide and maintain<br />
cervical support.<br />
Check for: pulse and rate; blood pressure; perform total body<br />
check; control bleeding. Assess: LOC, skin signsleyes.<br />
Determine GCS I RTS, chief complaint, and obtain medical<br />
history. Apply dressings, bandages, splints, and spinal<br />
immobilization as needed.<br />
Anticipate and obtain necessary equipment. Provide lighting.<br />
Direct paramedics to the patient; obtain gurney; assist with IV<br />
line preparation; gather and properly dispose of medical waste.<br />
-<br />
Supervise team; assess scene safety; determine the need for<br />
additional resources; interact with farnilyhystanders; initiate<br />
F-902M. Record patient assessment data (and times); record<br />
interventions (and times); obtain patient's medical history and<br />
current medications list, and (if available) Medi-Cal number,<br />
address (include ZIP code). Give a brief size-up to the<br />
paramedics.
TEAM<br />
A-B<br />
c<br />
D<br />
E<br />
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
MEDICAL COMPLAINT CHEST PAIN SEIZURE DIABETIC PATIENT<br />
COMPANY PERSONNEL<br />
FIRE<br />
Engineer<br />
or<br />
A0<br />
Revised: 121200 1<br />
Captain<br />
-<br />
BLS & ALS<br />
ALS RA<br />
PM<br />
BLS RA<br />
FF<br />
BLS RA<br />
FF<br />
ALS RA<br />
PM<br />
TASKS<br />
Assess: airway, respiratory rateltidal volume.<br />
Auscultate lungs for breath sounds.<br />
As needed: administer Oxygen, suction, BVM.<br />
Assess: pulselrate, blood pressure, skin signs, eyes.<br />
Complete total body check.<br />
Determine LOCIGCS.<br />
Obtain chief complaint and medical history.<br />
Anticipate and obtain necessary equipment (gurney).<br />
Direct paramedics to the patient. Assist with IV line<br />
preparation. Gather and properly dispose of medical waste.<br />
Supervise team. Assess scene safety and additional<br />
resource needs. Interact with familyhystanders. Obtain<br />
the patient's correct address (include ZIP code), Medi-Cal<br />
number (if available), medical history, allergies and list of<br />
current medications. Initiate the F-902M, record patient<br />
assessment data (and times), interventions (and times).<br />
Give a brief size-up to the paramedics.
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
PATIENT TRANSFER OF CARE FROM ALS TO BLS UNIT<br />
) The decision to transport a patient is governed by:<br />
The patient's medical condition The patient's chosen receiving facility<br />
* DHS policies and guidelines Medical judgment of the on-scene medical authority<br />
<strong>LAFD</strong> policies<br />
If the patient does not require ALS level care, the patient may be transported by a BLS ambulance.<br />
Members shall include the following steps when transferring care from an ALS unit to a BLS unit:<br />
Base hospital approval is required if the patient meets base hospital contact criteria.<br />
Obtain agreement from the BLS receiving team to accept responsibility for the patient.<br />
Advise the BLS receiving team of the patient's condition, history, physical assessment,<br />
and all treatment rendered.<br />
The ALS unit initiates the F-902M <strong>EMS</strong> Report and completes the appropriate sections<br />
ensuring that the unit and team member numbers are clear and legible.<br />
* The Green copy of the F-902M report shall be retained by the ALS unit.<br />
All other F-902M report copies are given to and completed by the BLS [transporting] unit.<br />
Revised: 121200 1 PAGE 1 OF 1
EMT-1 EXPANDED SCOPE OF PRACTICE<br />
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
County of Los Angeles <strong>EMS</strong> Agency (Ref. No. 802) EMT-I Expanded Scope ofpractice 1<br />
- -<br />
(Treatment Protocols, Interfacility, andlor 9- 1 - 1 responses)<br />
Prior to arrival of paramedics or transport:<br />
 Place patient in position of comfort<br />
 High flow 02<br />
 Monitor vital signs<br />
 Shock position PRN<br />
Monitor, maintain, and adjust preset rate:<br />
+ Glucose solutions<br />
+ Isotonic salt solutions (e.g., Normal<br />
Saline or Ringer's Lactate)<br />
(May turn off if infiltrated)<br />
Adjusted to TKO rate by hospital personnel:<br />
 Folic acid-max 1 mg/1000 ml<br />
+ Multi-vitamins-ma. 1 vial/1000 ml<br />
 Thiaminemax 100 mg/1000 ml<br />
Require infusion pump at preset rate:<br />
+ KCL-max 20 mEq11000 ml<br />
+ Total Parenteral Nutrition<br />
+ Chemotheraputic agents with required<br />
precautions (Spill Kit)<br />
May be implanted or external:<br />
 Insulin<br />
+ Demerol (Meperidine)<br />
 Morphine<br />
revised: 121200 1 PAGE 1 OF 1<br />
Approved by transferring physician:<br />
 Nasogastric (NG) tubes<br />
 Gastrostomy tubes<br />
 Heparin locks<br />
+ Foley catheters<br />
 Tracheostomy tubes<br />
+ Indwelling vascular access lines<br />
+ CVP monitoring devices<br />
+ Arterial lines including Swan Ganz<br />
catheters<br />
If available and indicated, assist patient or<br />
allow self-administration if criteria is met:<br />
+ Sublingual nitroglycerine aerosol or tablets<br />
* Systolic BP greater than 100<br />
 Bronchodilator inhaler or nebulizer<br />
* Alert enough to use inhaler<br />
+ Epinephrine device (Auto-Injector)<br />
* Signs and symptoms of severe allergic<br />
reaction (Respiratory distress or<br />
hypoperfusion)<br />
+ If assistance is given, EMT-Is shall not<br />
cancel EMT-P response.<br />
+ An ALS resource shall be requested if<br />
one has not been dispatched.<br />
+ In life-threatening situations, consider<br />
BLS transport if ALS arrival is longer<br />
than BLS transport time.
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
POISON CONTROL CENTER<br />
The California Poison Control Center is a facility that provides information and advice<br />
regarding the management of individuals who have or may have ingested or otherwise<br />
been exposed to poisonous or possibly toxic substances.<br />
1 ACCESSING A POISON CONTROL CENTER: 1<br />
1 9-1-1 PROVIDERS I (800) 404- 4646 1<br />
Health Professionals (800) 41 1- 8080<br />
Public Hotline (800) 876- 4766<br />
SYSTEM-WIDE MENTAL ASSESSMENT RESPONSE TEAM<br />
In 1993 the Department of Health Services in cooperation with the Los Angeles Police Department<br />
committed resources to staff a system-wide mental assessment response team (SMART) in the City.<br />
SMART is designed to provide a cooperative, compassionate mental health 1 law enforcement<br />
response team to assist affected citizens in accessing available mental health services. The team is<br />
able to assist in providing quick resolutions without unnecessary incarceration or hospitalization.<br />
SMART consists of nine teams including a supervisory team. Each team will be composed of one<br />
police officer and one Department of Mental Health clinician.<br />
The SMART goals are to:<br />
* Prevent unnecessary incarceration andlor hospitalization of mentally ill individuals.<br />
* Provide alternate care in the least restrictive environment through a coordinated and<br />
comprehensive system-wide approach.<br />
* Prevent the duplication of mental health services.<br />
* Allow police patrol units to return to service sooner.<br />
1 SMART HOURS of OPERATION<br />
1 Telephone: (213) 485-4188 1 Day Watch: 1 0700 hours to 1530 hours 1<br />
1 PM Watch: 1 1530 hours to 2400 hours 1<br />
SMART personnel shall request an ambulance to transport a person when:<br />
* The person is in need of immediate medical attention requiring transportation by <strong>EMS</strong> personnel<br />
* The person is extremely violent and requires restraint to the extent that they must be transported<br />
in a recumbent position.<br />
* The violent person is injured or physically ill and is in need of immediate medical attention.<br />
NB: When a mentally disordered andor violent person is transported by ambulance,<br />
at least one police officer shall accompany the patient.<br />
Revised: 121200 1 PAGE 1 OF 1<br />
-
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
b CITY VOLUNTEER PROGRAMS<br />
CRISIS RESPONSE TEAM [CRT]<br />
On November 25, 1998, under the direction of the Mayor's Office, Volunteer Bureau, Crisis<br />
Response Teams began City-wide operation. Crisis Response Team (CRT) members are trained<br />
civilian volunteers who respond, on request, to FirelPolice emergencies to perform immediate<br />
andlor short term on-scene intervention to victims, families, witnesses, and survivors of traumatic<br />
events.<br />
These teams do not perform counseling functions and will not function in the capacity of<br />
Department Critical Incident Stress Debriefing Teams for Firefighters and/or Police Officers.<br />
CRT members may be requested for any incident which, in the judgment of the incident commander,<br />
necessitates rapid intervention and referrals for humanitarian services such as :<br />
Grief management Drownings<br />
Shelter Fires with displaced occupants<br />
Food acquisition Homicides<br />
Abused/neglected children Major traffic accidents<br />
Death Suicides<br />
Drive-by shootings<br />
The goal of the CRT is to allow emergency responders to complete operational duties while the \,<br />
CRT team provides humanitarian services. -. 9'<br />
Requests for CRT shall be made through Operations Control Dispatch Section [OCD]. OCD will<br />
coordinate notification with the appropriate Police Division. CRT members are identifiable by their<br />
jackets and picture identification. They are instructed to report to the incident commander upon<br />
their arrival.<br />
Any questions regarding the CRT may be directed to the Bureau of Human Resources,<br />
Bureau Liaison Officer, [2 1 31 485-3396.<br />
COMMUNITY EMERGENCY RESPONSE TEAM [CERT]<br />
The Community Emergency Response Team [CERT] are civilian volunteers [trained<br />
by the Fire Department] who assist their communities during the initial phase of a disaster,<br />
e.g., major earthquake. The purpose of the CERT Program is to improve community self-reliance<br />
and, therefore, survival in the event of a large disaster. It is known that emergency service<br />
resources will be depleted, to the extent that some individuals or neighborhoods will need to rely<br />
on themselves during the first 24 to 72 hours.<br />
Note:<br />
The management of City Volunteer Programs is delineated in <strong>LAFD</strong> <strong>Training</strong> Bulletin 71<br />
Revised: 0 112003 PAGE 1 OF 1<br />
/
I<br />
Section 1: <strong>Field</strong> Procedures 1 Protocols<br />
MISCELLANEOUS<br />
Members shall use the following terms to indicate the urgency of the situation when<br />
requesting police response through Operations Control Dispatch (OCD):<br />
Fire Department needs " H E L P I'<br />
Use this term when there is imminent grave danger to <strong>LAFD</strong> personnel e.g., members<br />
are being attacked, attack is imminent, or other immediate hazardldanger.<br />
Assigned to response:<br />
ALL AVAILABLE POLICE UNITS IN THE AREA<br />
(one unit dispatched Code 3 and other units ASAP)<br />
FIRE COMPANY<br />
BATTALION CHIEF AND/OR<br />
<strong>EMS</strong> BATTALION CAPTAIN (if <strong>EMS</strong> incident)<br />
Fire Department needs " A S S I S T A N C E "<br />
Use this term when there is a large hostile crowd and apparent danger to <strong>LAFD</strong><br />
personnel or apparatus.<br />
Assigned to response:<br />
ALL AVAILABLE POLICE UNITS IN THE AREA<br />
(one unit dispatched Code 2 and other units ASAP)<br />
BATTALION CHIEF AND/OR<br />
<strong>EMS</strong> BATTALION CAPTAIN (if <strong>EMS</strong> incident)<br />
" B A C K - U P " the Fire Department<br />
Use this term when there are belligerent individuals and a likelihood of physical<br />
altercation.<br />
Assigned to response:<br />
ONE POLICE UNIT ASSIGNED, CODE 2<br />
" M E E T " the Fire Department<br />
Use this term when requesting LAPD to accompany you to a known "trouble area" or<br />
when the Incident Commander requests LAPD for traffic or crowd control.<br />
Assigned to response:<br />
Revised: 512005<br />
ONE POLICE UNIT ASSIGNED, CODE 2
MISCELLANEOUS<br />
Section I: <strong>Field</strong> Procedures I Protocols<br />
+ THE HIGHEST RANKJNG MEDICAL AUTHORITY on scene (generally a<br />
paramedic) is responsible for the overall. medical care rendered to patients.<br />
+ The Incident Commander is responsible for scene management, this includes:<br />
Scene Safety<br />
Resource Allocation<br />
Communications<br />
+ In order to effectively supervise <strong>EMS</strong> incidents, officers are expected<br />
to have a clear understanding of-and the ability to apply-the following:<br />
Department of Health Services policies and procedures (Prehospital<br />
Care Policy <strong>Manual</strong>, <strong>LAFD</strong> <strong>Book</strong> 33):<br />
1 802 1 EMT- 1 Scope of Practice I<br />
1 806 1 Procedures Prior to Base Hospital Contact I<br />
1 808 1 Base Hospital Contact and Transport Criteria 1<br />
1 814 1 Deteminatioflronouncement of Death in the <strong>Field</strong> 1<br />
1 Patient Refbsal of Treatment or Transport<br />
1 834 1<br />
502, 508, 5 10,<br />
511, 512, 515,<br />
518,519,520<br />
822,829<br />
Patient Destination Policies<br />
Suspected Abuse Policies and Procedures<br />
BODY ARMOR VESTS<br />
The BODY ARMOR VEST shall be donned prior to entering a potentially hostile environment.<br />
Protection from an attack depends on concealment of the vest so the attacker cannot purposefblly<br />
aim at or attack the unprotected area of the body. The vest shall be covered by a brush jacket,<br />
<strong>EMS</strong> safety coat, or firefighting turnout coat.<br />
Members shall wear their vests to the following incidents:<br />
+ Assault with a Deadly Weapon (ADW) + Sniper Incident 1 Police Standby<br />
+ Domestic Violence 1 Family Dispute + Tactical Alert<br />
+ Shooting<br />
+ Incidents in Known "Trouble Area"<br />
+ Stabbing I Cutting<br />
+ Other Violent Crimes or Conditions<br />
Nd: A vest may be worn anytime a member feels it is necessary.<br />
Revised: 512005 PAGE 2 OF 3<br />
7
Section I: <strong>Field</strong> Procedures 1 Protocols<br />
MISCELLANEOUS<br />
MEDICAL WASTE DISPOSAL<br />
Before leaving the scene collect all usedcontaminated materials and place in zip-lock bags for<br />
discard in the biohazard containers at the hospital.<br />
Place the disposable sharp supplies into a puncture resistant container. Leave these containers at<br />
the receiving hospital when 314 fbll and secured properly.<br />
Revised: 512005<br />
PAGE 3 OF 3
Section I: <strong>Field</strong> Procedures I Protocols<br />
MANAGEMENT OF MULTIPLE VICTIM INCIDENTS<br />
Normally BLS resources will not have the responsibility of medical incident control of multiple<br />
victim incidents. However, they may be the first resource on the scene of such an incident.<br />
An ALS resource shall be requested for incidents involving the transport of five or more<br />
patients and for patients whose condition meets the Patient Resolution Guide (PRG) criteria.<br />
The BLS resource shall obtain the following assessment information and initiate patient triage<br />
tags prior to the arrival of the ALS resource. (Refer to <strong>Book</strong> <strong>35</strong>? Section 1.1, START; U FD<br />
<strong>Book</strong> 70, Multi-Casualty Incident Procedures; DHS, Reference No. 519.)<br />
ROLE OF THE PROVIDER AGENCY:<br />
+ Institute ICS as necessary.<br />
+ Implement START as necessary.<br />
t Establish communication with either the MAC or base hospital for the purpose of<br />
patient destination andor medical direction. In general, the Medical Alert Center (MAC)<br />
should be contacted for 10 or more patients and the base hospital for less than 10 patients.<br />
t Additional BLSIALS transporting units may be requested fi-om Operations Control Dispatch<br />
as necessary.<br />
+ Request? if necessary? the hospital based medical resources from the MAC? as outlined in<br />
DHSy Ref. No. 8 17? Hospital Emergency Response Team (HERT).<br />
1 t NATUm OF INCIDENT<br />
PROVIDE THE FOLLOWING SCENE INFORMATION TO<br />
THE MAC OR BASE HOSPITAL,:<br />
t SEVERITY STATUS: estimated number of immediate? delayed? minor, and<br />
deceased patients. If indicated? include total number and category of pediatric patients.<br />
t RECEIVING FACILITIES closest to location to include trauma centers? PTCs,<br />
PMCs, and EDAPs.<br />
v<br />
v<br />
'#<br />
v<br />
'#<br />
v<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
7.<br />
8.<br />
Patient number [e.g., patient # 3 of 81<br />
Chief complaint<br />
Age<br />
Gender<br />
Brief patient assessment<br />
Brief description of treatment provided<br />
Sequence number<br />
Transporting provider and unit number? destination, and ETA<br />
vvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvv.<br />
~*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A*A<br />
@ PROVIDE THE FOLLOWING PATIENT INFORMATION AS TIME PERMITS:<br />
Revised: 512005 PAGE 1 OF 2<br />
7
Section I: <strong>Field</strong> ProcedureslProtocols<br />
MCI <strong>EMS</strong> REPORT SHORT FORM<br />
The Multiple Casualty Incident (MCI) Short Form has been developed by the Los Angeles<br />
County <strong>EMS</strong> Agency as an optional form for use by providers in situations where multiple<br />
patients are encountered on scene. The form is a "shortened" version of the Los Angeles<br />
County <strong>EMS</strong> form that encompasses the essential data for the incident while providing a<br />
valuable timesaving tool to providers for multi-patient incidents. The MCI short form may<br />
be used in place of the standard <strong>EMS</strong> Report Form in MCl's.<br />
Page one Page one (back copy) Patient Release<br />
When more than ten (10) patients are encounteredl the provider has the option of using the<br />
MCI Short Form. When this form is usedl a standard <strong>EMS</strong> Report Form (F-902M) does not need<br />
to be filled out. During a mass casualty incidentl the MCI Short Form can be used as a stand-<br />
alone forml used along with a triage tagl or used in place of a triage tag (these options are at<br />
the discretion of the department or provider). (Refer to Departmental Bulletin No. 04-1 9)<br />
Each MCI <strong>EMS</strong> Report Short Form can accommodate up to four patients and is formatted in<br />
quadruplicate. The back of the first page allows the patient to release the Fire Department from<br />
liability. Use this section ONLY when patients that DO NOT meet the criteria of the <strong>LAFD</strong><br />
PRG or the <strong>LAFD</strong> <strong>Book</strong> 33, Ref. No. 808 * are released from the scene.<br />
The fourth page has an adhesive backing and could be placed on the patient for tracking.<br />
Once the patient is released from the scenel the patient can keep the adhesive copy for their<br />
records. This adhesive copy can also be used as a record for the receiving facility! if the patient<br />
seeks medical treatment on their own.<br />
The MCI <strong>EMS</strong> Report Short Form will be carried by all companies and<br />
will be included in the MCI packet.<br />
* Patients who meet the above criterial require an <strong>EMS</strong> Report Form F-902M<br />
completion and base hospital contact.<br />
Revised: 512005 PAGE 2 OF 2
Section 2: Patient Transportation 1 Destination<br />
<strong>LAFD</strong> PATIENT DESTINATION GUIDELINES<br />
prepared to receive emergency cases and administer emergency care appropriate to the needs of the<br />
patient, in the absence of "decisive factors to the contrary."<br />
4 ALS units utilizing Standing <strong>Field</strong> Treatment Protocols (SFTPs) shall transport patients in accordance<br />
with this policy.<br />
4 The most appropriate health facility for a patient may be that facility which is affiliated with the patient's<br />
health plan. Depending upon the patient's chief complaint and medical history, it may be advantageous<br />
for the patient to be transported to a facility where helshe may be treated by a personal physician and/or<br />
the individual's personal health plan where medical records are available.<br />
4 The MAR facility may or may not be the closest facility geographically. Transport personnel shall take<br />
into consideration traffic, weather conditions, or other similar factors which may influence transport time<br />
when identifying which hospital is most accessible.<br />
+ Patients shall @ be transported to a medical facility that has requested diversion due to "Internal Disaster."<br />
PATIENTS TRANSPORTED BY BLS PERSONNEL<br />
Stable patients requiring only basic life support (BLS) shall be transported to the MAR, regardless of its<br />
diversion status (Exception: Internal Disaster).<br />
For pediatric patients, the MAR is the most accessible Emergency Department Approved for Pediatrics.<br />
For perinatal patients, the MAR is to be the most accessible Perinatal Center.<br />
BLS personnel may honor patient requests provided that the patient is stable, requires basic life support<br />
measures only, and the ambulance is not unreasonably removed from its primary area of response.<br />
I<br />
- Transport patients to the MAR unless:<br />
* The base hospital determines that a more distant hospital is more appropriate to meet the needs of the patient.<br />
* The patient meets criteria or guidelines for transport to a specialty care center.<br />
* The patient requests a specific hospital [provided the patient's condition is considered stable to tolerate<br />
additional transport time, the receiving hospital agrees to accept the patient, and the <strong>EMS</strong> provider has<br />
determined that such a transport would not unreasonably remove the unit from its primary area of response].<br />
* If transport to the desired hospital involves an extended transport time [> 20 min.] notify OCD of the<br />
extended time and contact the receiving facility to determine if they will accept the patient.<br />
* If the desired hospital is unreasonably far, request the <strong>EMS</strong> Battalion Captain.<br />
NA: On an "as needed basis", the <strong>EMS</strong> agency may extend maximum transport time. grequests cannot be<br />
honored, the provider should attempt to arrange for alternate transportation i.e., private ambulance.<br />
ALS units may be directed to an alternate "open" facility when the medical facility has requested diversion<br />
of patients requiring ALS, if:<br />
* The patient does not exhibit an uncontrollable problem in the field (e.g., unmanageable airway,<br />
uncontrolled hemorrhage).<br />
* The ALS unit estimates that it can reach an alternate facility within 15 minutes (Code 3) from the<br />
incident location.<br />
* There are no "open" facilities within this time frame, ALS units shall be directed to the MAR<br />
regardless of its diversion status (Exception: Internal Disaster). N-: On an "as needed basis,''<br />
the maximum transport time may be extended.<br />
Revised: 512005<br />
PAGE 1 OF 1
CALIFORNIA<br />
CENTINEIA FREEMAN-<br />
MEMORIAL CAMPUS 1<br />
ADULT<br />
ADULT 1<br />
12 & OLDER<br />
16 & OLDER 1<br />
-- -<br />
COMMUNITY OF LONG BEACH ADULT PEDIATRIC<br />
IACIUSC<br />
1<br />
ADULT<br />
1<br />
PEDIATRIC<br />
1<br />
LITTLE COMPANY OF MARY-<br />
L I<br />
TORRANCE<br />
I 1 E COMPANY OF MARY ADULT<br />
SAN PEDRO<br />
PEDIATRIC 1<br />
1 SAN GABRIEL VALLEY I ADULT I 14 & OLDER 1<br />
1 SANTAMONICAIUCLA I ADULT I PEDIATRIC 1<br />
"Sexual Assault" refers to patients who state they were sexually assaulted or if <strong>EMS</strong> personnel<br />
suspect the patient was a victim of sexual assault. Prehospital personnel shall notify the local<br />
law enforcement agency of sexual assault victims regardless whether the patient complains of<br />
physical injuries. <strong>EMS</strong> personnel, in conjunction with law enforcement, are highly encouraged<br />
to transport suspected sexual assault patients, who deny physical injuries, to a designated SART<br />
Center. (DM Reference No. 508)<br />
Revised: 512005 PAGE 1 OF 2<br />
1
\<br />
Trauma patients shall be secured and transported from the scene as quickly as<br />
possible, consistent with optimal trauma care. EMT-Ps shall make base hospital<br />
contact with the area's trauma hospital, when it is also a base hospital, on all injured patients who<br />
meet Base Contact and Transport criteria, trauma triage criteria and/or guidelines, or in the paramedic's<br />
judgment it is in the patient's best interest to be transported to a trauma hospital. Hospital contact shall<br />
be accomplished in such a way as not to delay transport.<br />
Patients who fall into one or more of the following categories are to be transported directly to the area's<br />
designated trauma hospital, if transport time does not exceed 20 minutes. If existing field resources at<br />
the time of transport allow, patients may be transported an additional 10 minutes (to a maximum of 30<br />
minutes). Transport pediatric trauma patients to the designated PTC. (DHS, Reference No. 506)<br />
Systolic Blood Pressure: Adults < 90<br />
Children < 70<br />
Abnormal capillary refill<br />
1 No spontaneous eye opening<br />
Penetrating cranial injury<br />
Penetrating thoracic injury within<br />
Blunt injury to chest with unstable chest<br />
wall (Flail chest)<br />
Penetrating injury to neck<br />
Diffuse abdominal tenderness<br />
Patients surviving falls from heights > 15 feet<br />
Intrusion of motor vehicle into passenger space<br />
Cardiopulmonary arrest with penetrating torso trauma<br />
Blunt head injury associated with altered consciousness<br />
(GCS equal to or less than 14, excluding patients < 1 year<br />
IOpen<br />
old), seizures, unequal pupils, or focal neurological defecit<br />
or closed injury to the spinal column associated with<br />
sensory deficit or weakness of one or more extremities<br />
Mechanism of injury is the most effective method of selecting critically injured patients before<br />
unstable vital signs develop. Paramedics and base hospital personnel shall consider mechanism of<br />
injury when determining patient destination. Transportation to a trauma hospital is advisable for:<br />
* Survivors of vehicular accidents (in which fatalities occurred) who complain of injury<br />
* Pedestrians struck by automobiles<br />
* Patients ejected from vehicles<br />
* Patients requiring extrication<br />
* The very young, very old, and patients with precarious previous medical histories<br />
The following extremis patients require immediate transport to the most accessible receiving (MAR) facility:<br />
* Patients with an obstructed airway<br />
* Cardiac arrest from traumatic injuries (Exception: Transport a penetrating torso injury to a<br />
Trauma Center)<br />
* Patients whose lives would be jeopardized by transportation to any but the most accessible receiving<br />
(MAR) facility, as determined by the base hospital personnel<br />
Revised: 512005 PAGE 2 OF 2
Section 2: Patient Transportation 1 Destination<br />
When base hospital contact cannot be made, for any reason, paramedics shall<br />
decide the destination for trauma patients using the guidelines set forth.<br />
BLS personnel shall transport patients to the most accessible receiving (MAR) facility /<br />
trauma catchment/boundary area is a geographical area surrounding a trauma hospital in which the<br />
trauma hospital has agreed to accept trauma patients. The boundaries may either be defined by streets1<br />
freewaysllandmarks or transport time. (DHS, Reference # 504)<br />
* Secure Catchment Boundaries1 Area: A catchment area around a trauma hospital strictly defined<br />
by streetslfreeways or other physical landmarks. Hospitals with secure catchment areas will only<br />
accept trauma patients from incident locations within the defined area.<br />
* Open Catchment BoundariesIArea: A catchment area around a trauma hospital defined by<br />
transport time (i.e., a hospital will accept patients who can be transported to its facility within<br />
a 30-minute, Code-3 transport time). The boundaries of a trauma hospital with an open catchment<br />
area will vary throughout any given day due to variations in weather and traffic patterns.<br />
ALS personnel responsibilities include: (1) Maintaining current knowledge of which geographic areas are<br />
securelopen catchment areas or areas undesignated for trauma within the assigned area; (2) Advising the<br />
base hospital of the designated trauma hospital covering the incident location when making base contact<br />
on a trauma patient.<br />
SECURE Catchment 1 Boundaries for ADULT and PEDIATRIC Trauma Patients:<br />
Henry Mayo Newhall Memorial Huntington Memorial (PMC)<br />
St. Francis Medical Center St. Mary Medical Center (PMC)<br />
Northridge Medical Center-Roscoe Campus<br />
I SECURE Catchment 1 Boundaries for ADULT and 1<br />
OPEN Catchment I Boundaries for PEDIATRIC Trauma Patients:<br />
Cedars-Sinai Medical Center (PMC , PTC) UCLA Medical Center (PMC, PTC)<br />
Long Beach Memorial (PMC, PTC) California Medical Center<br />
F~~atchment I Boundaries for Trauma Patients:<br />
Childrens Hospital L. A. (PMC, PTC)<br />
HarborIUCLA Medical Center (F'MC, PTC) Providence Holy Cross<br />
LACAJSC Medical Center (PMC, PTC)<br />
Trauma patients from incidents occurring in an undesignated area shall be transported to:<br />
* The assigned Air Ambulance Trauma Transport Program hospital<br />
(Antelope ValleylEast County only); or<br />
* The closest/open County-operated trauma hospital within the 30-minute transport<br />
guidelines, by groundlair; or<br />
* The most accessible receiving hospital (Extremis) (EDAP for pediatric patients).<br />
Revised: 512005 PAGE 1 OF 2<br />
\
1 139 1 CEDARS SINAI 1 LA 1 PAGE632-J1<br />
1 145 1 CHILDRENS 1 1 PAGE 594-A4<br />
248<br />
438<br />
533<br />
81 8<br />
HARBOR / UCLA<br />
LAC~USC<br />
LONG BEACH MEMORIAL<br />
UCLA MEDICAL CENTER<br />
All Pediatric Trauma Centers (PTCs) have an<br />
OPEN trauma catchment area for pediatric trauma patients.<br />
Pediatric patients (14 years of age or younger), who meet Trauma Center Criteria and/or<br />
Guidelines, shall be transported to a designated PTC<br />
133 CALIFORNIA TRAUMA EDAP PERINATAL x<br />
139 CEDARS-SINAI TRAUMA PMC EDAP PERINATAL NICU PTC x<br />
145<br />
248<br />
270<br />
305<br />
CHILDRENS<br />
HARBOR /UCLA<br />
TORRANCE<br />
1<br />
HOLY CROSS<br />
324 1 HUNTINGTON MEM.<br />
TRAUMA<br />
1 TRAUMA 1 PMC 1<br />
EDAP<br />
EDAP<br />
PERINATAL NICU<br />
1 PERINATAL 1 NICU 1 1 X 1<br />
LONG BEACH MEM. TRAUMA PMC EDAP PERINATAL NICU PTC<br />
533<br />
571<br />
667<br />
134<br />
818<br />
Revised: 512005<br />
HENRY MAY0<br />
NORTHRIDGE<br />
ST. FRANCIS<br />
ST. MARY<br />
UCLA<br />
TRAUMA<br />
TRAUMA<br />
TRAUMA<br />
TRAUMA<br />
TRAUMA<br />
TRAUMA<br />
PMC<br />
PMC<br />
PMC<br />
PMC<br />
LA<br />
LONG BEACH<br />
LA<br />
EDAP<br />
EDAP<br />
EDAP<br />
EDAP<br />
EDAP<br />
EDAP<br />
EDAP<br />
PAGE 2 OF 2<br />
PERINATAL<br />
PERINATAL<br />
PERINATAL<br />
PERINATAL<br />
PERINATAL<br />
PERINATAL<br />
PAGE 764-A6<br />
PAGE 6<strong>35</strong>-B3<br />
PAGE 792-E2<br />
PAGE 632-B2<br />
1 438 1 USC 1 TRAUMA 1 PMC 1 EDAP 1 PERINATAL 1 NICU 1 PTC 1 I<br />
NICU<br />
NICU<br />
NICU<br />
NICU<br />
NICU<br />
NICU<br />
PTC<br />
PTC<br />
PTC<br />
x<br />
x<br />
x<br />
x<br />
x<br />
x<br />
J
- -<br />
1 CALIFORNIA MEDICAL CENTER [CALI<br />
CEDARS SINAI MEDICAL CENTER [CSM]<br />
CHILDRENS HOSPITAL OF LOS ANGELES [CHH]<br />
HARBOR I UCLA MEDICAL CENTER [HGH]<br />
HENRY MAY0 NEWHALL MEMORIAL [HMNI<br />
PROVIDENCE HOLY CROSS MEDICAL CENTER [HCHI<br />
1 HUNTINGTON MEMORIAL HOSPITAL [HMH]<br />
1<br />
LAC I USC MEDICAL CENTER [USC]<br />
LONG BEACH MEMORIAL MEDICAL CENTER [LBM]<br />
NORTHRIDGE HOSPITAL MEDICAL CENTER [NRHI<br />
ST. FRANCIS MEDICAL CENTER [SFM]<br />
ST. MARY MEDICAL CENTER [SMM]<br />
UCLA MEDICAL CENTER [UCL]<br />
Revised: 0512005 PAGE 1 of 26<br />
--<br />
ADULT<br />
ADULT PEDIATRIC<br />
ADULT<br />
ADULT<br />
ADULT<br />
ADULT<br />
ADULT<br />
ADULT<br />
ADULT<br />
ADULT<br />
ADULT<br />
PEDIATRIC<br />
PEDIATRIC<br />
PEDIATRIC<br />
PEDIATRIC<br />
ADULT PEDIATRIC
LA COUNTY<br />
TRAUMA CENTERS<br />
Revised: 512005 PAGE 2 of 26
1 LEGEND<br />
CAL<br />
Revised: 05/2005<br />
CALIFORNIA MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
DESTINATION CRITERIA<br />
OPEN catchmentl boundaries for PEDIATRIC trauma patients<br />
and<br />
SECURE catchmentl boundaries for ADULT trauma patients.<br />
PAGE 3 of 26<br />
THOMAS GUIDE MAP BOOK PAGE<br />
CALIFORNIA 133 EDAP, PERINATAL, TRAUMA, SART 634-D6<br />
-
CALIFORNIA MEDICAL CENTER<br />
" 1 TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0512005 PAGE 4 of 26<br />
California<br />
Medical Center<br />
Trauma Center<br />
Catchment Area<br />
PHASE 2<br />
Target Date: 02101105<br />
CAL California Medical Center<br />
- TRAUMA<br />
TRAUMA CENTER<br />
AREA<br />
BOUNDARIES<br />
Ñà FREEWAYS<br />
- MAJOR STREETS<br />
NORTHERNBOUNDARY<br />
Sanla Monica (10) Freeway<br />
Western Avenue<br />
EASTERNBOUNDARY<br />
Central Avenue<br />
SOUTHERNBOUNDARY<br />
Century Blvd (PHASE 2)<br />
WESTERNBOUNDARY<br />
Crenshaw Boulevard<br />
Crealed: 1110Z041PLN<br />
s
CEDARS-SINAI MEDICAL CENTER<br />
" 1 TRAUMA CENTER CATCHMENT AREA I<br />
CSM<br />
UCL<br />
CHH<br />
MULHOLLAND DR / CAHUENGA PASS / GRIFFITH PARK AREA<br />
(PARAMEDIC / BASE HOSPITAL JUDGEMENT)<br />
SANTA MONICA (1 0) FREEWAY<br />
MOTOR AVE 1 SANTA MONICA (1 0) FREEWAY<br />
1 DESTINATION CRITERIA<br />
OPEN catchment1 boundaries for PEDIATRIC trauma patients<br />
and<br />
SECURE catchment1 boundaries for ADULT trauma patients.<br />
CEDARS SINAI<br />
UCLA<br />
cH'LDRENs<br />
HOSPITAL<br />
139<br />
818<br />
145<br />
PMC, EDAP, PERINATAL, TRAUMA, PTC<br />
PMC, EDAP, PERINATAL, TRAUMA, PTC<br />
Revised: 0512005 PAGE 5 of 26<br />
PMC, EDAP, PEDIATRIC TRAUMA CENTER (PTC)<br />
THOMAS GUIDE MAP BOOK PAGE<br />
632-J 1<br />
632-B2<br />
5 94-A4
CEDARS-SINAI MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0712004 PAGE 6 of 26
UCLA HOSPITAL<br />
CENTER CATCHMENT AREA 1<br />
1 DESTINATION CRITERIA<br />
Harbor 1 UCLA Medical Center has an OPEN catchment area and will<br />
accept patients who can be transported to its facility within a 30-minute,<br />
Code-3 transport time.<br />
1 LEGEND<br />
The times may vary throughout any given day because<br />
of variations in weather and traffic patterns.<br />
THOMAS GUIDE MAP BOOK PAGE
HARBOR 1 UCLA HOSPITAL<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0512005 PAGE 8 of 26
HENRY MAY0 NEWHALL MEMORIAL HOSPITAL<br />
TRAUMA CENTER CATCHMENT AREA<br />
1 LEGEND<br />
1 DESTINATION CRITERIA<br />
SECURE catchment area for<br />
ADULT and PEDIATRIC trauma patients.<br />
1 HMN 1 HENRY MAY0 NEWHALL 1 270<br />
I I PROVIDENCE<br />
HcH HOLY CROSS<br />
1 NRH 1 NORTHRIDGE<br />
Revised: 0712004 PAGE 9 of 26<br />
EDAP, PERINATAL, TRAUMA<br />
EDAP, PERINATAL, TRAUMA<br />
THOMAS GUIDE MAP BOOK PAGE<br />
EDAP, PERINATAL, TRAUMA 1 530-J2<br />
I
HENRY MAY0 NEWHALL MEMORIAL HOSPITAL<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0312003 PAGE 10 of 26<br />
,-
6.b PROVIDENCE HOLY CROSS MEDICAL CENTER<br />
"1 TRAUMA CENTER CATCHMENT AREA<br />
1 DESTINATION CRITERIA<br />
Providence Holy Cross Medical Center has an OPEN catchment area and will accept<br />
patients who can be transported to its facility within a 30-minute, Code -3 transport time.<br />
1 LEGEND<br />
The boundaries will vary throughout any given day because<br />
of variations in weather and traffic patterns.<br />
I I HcH PROVIDENCE<br />
HOLY CROSS<br />
CHILDRENS HOSPITAL<br />
I cHH I<br />
NRH<br />
I HMN I<br />
Revised: 05/2005<br />
NORTHRIDGE<br />
HENRY MAY0<br />
NEWHALL<br />
THOMAS GUIDE MAP BOOK PAGE<br />
I I I<br />
I 1 501-HI I<br />
305 EDAP, PERINATAL, TRAUMA<br />
145<br />
PMC, EDAP, PTC<br />
571 1 EDAP, PERINATAL, TRAUMA 1 530-J2<br />
--<br />
EDAP, PERINATAL, TRAUMA I<br />
PAGE 11 of 26<br />
5 94-A4<br />
4554%
PROVIDENCE HOLY CROSS MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0312003 PAGE 12 of 26
1 LEGEND<br />
HMH<br />
USC<br />
HUNTINGTON MEMORIAL HOSPITAL<br />
TRAUMA CENTER CATCHMENT AREA<br />
DESTINATION CRITERIA<br />
SECURE catchment area for<br />
ADULT and PEDIATRIC trauma patients.<br />
A secure catchment area is strictly defined by streetdfree ways<br />
or other physical landmarks.<br />
HUNTINGTON<br />
MEMORIAL<br />
LAC/USC MEDICAL<br />
324<br />
438<br />
Revised: 0512005 PAGE 13 of 26<br />
PMC, EDAP, PERINATAL, TRAUMA<br />
PMC, EDAP, PERINATAL, TRAUMA, PTC,<br />
SART<br />
THOMAS GUIDE MAP BOOK PAGE<br />
565-H6<br />
6<strong>35</strong>-B3
HUNTINGTON MEMORIAL HOSPITAL<br />
TRAUMA CENTER CATCHMENT AREA<br />
COUNTY<br />
Revised: 0312003 PAGE 14 of 26
LEGEND<br />
USC<br />
HMH<br />
CHH<br />
LAC 1 USC MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
1 DESTINATION CRITERIA<br />
LAC/USC MEDICAL<br />
HUNTINGTON<br />
MEMORIAL<br />
OPEN catchment area for<br />
ADULT and PEDIATRIC trauma patients.<br />
CHILDRENS HOSPITAL<br />
438<br />
324<br />
145<br />
Revised: 0312003 PAGE 15 of 26<br />
PMC, EDAP, PERINATAL, TRAUMA, PTC,<br />
sART<br />
PMC, PERINATAL, EDAP, TRAUMA<br />
PMC, EDAP, PEDIATRIC TRAUMA CENTER<br />
THOMAS GUIDE MAP BOOK PAGE<br />
6<strong>35</strong>-B3<br />
565-H6<br />
594-A4
Revised: 0512005<br />
LAC 1 USC MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
PAGE 16 of 26
@<br />
LONG BEACH MEMORIAL HOSPITAL<br />
TRAUMA CENTER CATCHMENT AREA<br />
LEGEND<br />
ORANGE COUNTY LINE<br />
1 DESTINATION CRITERIA<br />
SECURE catchment area for ADULT trauma patients<br />
OPEN catchment area for PEDIATRIC trauma patients.<br />
THOMAS GUIDE MAP BOOK PAGE<br />
I I 1 1 1 LONG BEACH<br />
PMC, EDAP, PERINATAL, TRAUMA,<br />
795-E2<br />
LBM MEMORIAL 533 PTC<br />
1 SMM 1 ST. MARY MEDICAL 1 134 1 EDAP, PERINATAL, TRAUMA I 795-~6<br />
1 SFM 1 ST. FRANCIS MEDICAL 1 667 1 EDAP, PERINATAL, TRAUMA 1 705436<br />
Revised: 0512005 PAGE 17 of 26
LONG BEACH MEMORIAL HOSPITAL<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0712004 PAGE 18 of 26
NORTHRIDGE MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
DESTINATION CRITERIA<br />
SECURE catchment area for trauma patients and will accept patients who can<br />
be transported to its facility within a 30-minute, Code -3 transport time.<br />
LEGEND<br />
The times may vary throughout any given day<br />
because of variations in weather and traffic patterns.<br />
s<br />
THOMAS<br />
PROVIDENCE HOLY CROSS<br />
NRH NORTHRIDGE<br />
Revised: 0712004<br />
PAGE 19 of 26<br />
GUIDE MAP BOOK PAGE<br />
501 -HI<br />
530-J2
NORTHRIDGE MEDICAL CENTER ROSCOE<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0712004 PAGE 20 of 26
ST. FRANCIS MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
DESTINATION CRITERIA<br />
SECURE catchment area for trauma patients and will accept patients who can<br />
be transported to its facility within a 30-minute, Code -3 transport time.<br />
LEGEND<br />
SFM<br />
Revised: 0512005<br />
The times may vary throughout any given day<br />
because of variations in weather and traffic patterns.<br />
PAGE 2 1 of 26<br />
THOMAS GUIDE MAP BOOK PAGE<br />
ST. FRANCIS MEDICAL 667 EDAP, PERINATAL, TRAUMA 705-B6
ST. FRANCIS MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0512005 PAGE 22 of 26
ST. MARY MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
1 DESTINATION CRITERIA<br />
SECURE catchment area for trauma patients and will accept patients who can<br />
be transported to its facility within a 30-minute, Code -3 transport time.<br />
1 LEGEND<br />
The times may vary throughout any given day<br />
because of variations in weather and traffic patterns.<br />
THOMAS GUIDE MAP BOOK PAGE<br />
sMM 1 ST. MARY MEDICAL 1 134 1 EDAP, PERINATAL, TRAUMA 1 795-~6<br />
LBM<br />
Revised: 0512005<br />
LONG BEACH<br />
MEMORIAL<br />
533 PMC, EDAP, PERINATAL~TRAUMA, PTC 795-E2<br />
PAGE 23 of 26
ST. MARY MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
Revised: 0712004 PAGE 24 of 26
CSM<br />
NRH<br />
UCL<br />
LEGEND<br />
UCLA MEDICAL CENTER<br />
TRAUMA CENTER CATCHMENT AREA<br />
1 DESTINATION CRITERIA<br />
OPEN catchment area for PEDIATRIC trauma patients<br />
and<br />
SECURE catchment area for ADULT trauma patients.<br />
CEDARS-SINAI<br />
NORTHRIDGE<br />
UCLA<br />
139<br />
57 1<br />
8 1 8<br />
Revised: 0512005 PAGE 25 of 26<br />
PMC, EDAP, PERINATAL, TRAUMA, PTC<br />
EDAP, PERINATAL, TRAUMA,<br />
EDAP, PMC, PERINATAL, TRAUMA, PTC<br />
THOMAS GUIDE MAP BOOK PAGE<br />
632-J 1<br />
530-J2<br />
632-B2
I<br />
UCLA MEDICAL CENTER (UCL)<br />
TRAUMA CENTER CATCHMENT AREA<br />
Pacific Ocean<br />
Revised: 0512005 Page 26 of 26
Section 2: Transportation 1 Destination<br />
TRAUMA CENTER DIVERSION<br />
\ v When the designated trauma hospital requests diversion to trauma, transport the patient to:<br />
The closest open County-operated trauma hospital within the 30-minute transport guidelines,<br />
by ground or by air;<br />
The closest open trauma hospital with an open catchment area within the 30-minute transport<br />
guideline by ground (DHS Reference # 504)<br />
For multiple victim incidents (five or more patients), secure catchment boundaries shall be adhered<br />
to. It is understood that during a multiple victim incident, as a result of normal triage procedure,<br />
trauma patients may ultimately be transported to a trauma hospital as the next closest facility<br />
(crossing the catchment/ boundary) as receiving hospitals in the surrounding geographic area of the<br />
incident are utilized to their maximum capacity.<br />
EDAp / PMC / PTC Added to the guidelines for identifying critically ill or injured<br />
pediatric patients requiring transport to a PMC is ALTE (Acute<br />
Life Threatening Event). In 2003, the new category of Pediatric Trauma Center (PTC) was added<br />
to the list of Specialty Care Centers. Pediatric patients meeting Trauma Center CriteriaIGuidelines<br />
will be transported to the most accessible PTC that may be reached within 30 minutes. In cases<br />
when a PTC cannot be reached within this time frame, transport to an adult trauma center.<br />
Factors to consider prior<br />
\ transport to an EDAP,<br />
PMC, or a PTC:<br />
Does not meet PMCRTC transport<br />
Transport time to PMC is > 30-min.<br />
BLS transport when ALS unit is not<br />
available<br />
Uncontrollable, life threatening<br />
situation ( e.g., unmanageable airway or<br />
uncontrollable hemorrhage, respiratory<br />
or cardiac arrest)<br />
(Refer to the PRG, Principle)<br />
* Severity of illness or injury and stability of the child's condition<br />
* Current status of the pediatric receiving facility<br />
* Anticipated transport time<br />
* Destination request by family or physician if patient's condition allows<br />
Critically ill (MEDICAL)<br />
Severe respiratory distress<br />
Cyanosis<br />
ALTE 21 2 months of age<br />
Persistent altered mental status<br />
Status epilepticus<br />
Cardiac dysrhythmia<br />
Critically injured (TRAUMA)<br />
Trauma criteria and1<br />
or guidelines *<br />
Transport time does not<br />
exceed 30 minutes *<br />
* For patients who meet<br />
DHS Ref.# 506<br />
Transport to the most accessible Perinatal Center: Patients who are at least 20 weeks<br />
pregnant and who appear to be in active labor or have perinatal complications, chief<br />
complaint is related to the pregnancy, and injured perinatal patients who do not meet trauma criteria or<br />
guidelines. For patients who have made previous arrangements for OB care, honor patient destination<br />
request if: Patient condition permits such transport, transport to requested OB facility would not exceed<br />
20 minutes, and would not unreasonably remove the transporting unit from its area of primary response.<br />
(DHS, Reference # 5 1 1)<br />
Revised: 0512005 PAGE 1 OF 1
BURN PATIENTS<br />
Destination for patients sustaining bum injuries shall be determined as follows:<br />
Section 2: Patient Transportation 1 Destination<br />
* Patients who meet trauma or PTC criteria and/or guidelines shall be transported to<br />
the appropriate trauma hospital or PTC.<br />
* Patients who do not meet trauma or PTC criteria and/or guidelines shall be transported to the<br />
most accessible receiving (MAR) appropriate for their age. (DHS, Reference 5 12)<br />
Note: Firelighter's, who sustain bum injuries, that do not meet base station contact<br />
criteria, shall be TAKEN DIRECTLY to either the Grossman Burn Center at<br />
Sherman Oaks Hospital or Torrance Memorial Hospital Burn Center.<br />
To expedite the appropriate care associated with the complexities of bums when<br />
a firelighter sustains a bum injury, no matter how slight, the following shall be<br />
adhered to :<br />
+ Firelighter medically evaluated by paramedics.<br />
4 Request for the concerned <strong>EMS</strong> Battalion Captain shall be made<br />
through OCDS.<br />
4 Transport consistent with DHS, Reference 512. However, when the bum injury does not<br />
meet base contact criteria, the member shall be transported directly to one of the above<br />
bum centers.<br />
This is particularly directed at minor bums that are recognized as a first-degree with high probability<br />
of progressing to a second-degree and any second-degree bum. Serious bums require base contact 1<br />
as noted in DHS Reference No 808. Bums secondary to or associated with injuries meeting trauma<br />
center criteria shall be transported to a trauma center prior to a bum center.<br />
1 DECOMPRESSION<br />
Paramedics should simultaneously establish base hospital contact with LACIUSC Medical Center and<br />
the Medical Alert Center (MAC) via the Hospital Emergency Administrative Radio (HEAR)<br />
for any patient suspected of having a decompression emergency.<br />
LAC/USC Medical Center will provide medical orders for patient care and determine if the<br />
patient should be transported directly from the incident location to a hyperbaric chamber.<br />
MAC will determine which hyperbaric chamber is most appropriate to the needs of the patient and<br />
coordinate transportation to the chamber for the patient and medical personnel. (Factors considered include:<br />
patient condition, distance, altitude, ETA of available transportation, and limitations of various aircraft.)<br />
*Obtain dive incident history of the patient and dive partner, if able.<br />
'Coordinate patient transportation to the appropriate receiving facility.<br />
*Retrieve patient's dive equipment (e.g., regulator, tank, gauges, weight belt,<br />
etc.) and transport with patient.<br />
As a general rule, the integrity of the dive equipment should be maintained and not<br />
tampered with except by investigating authorities. (Refer to DHS, Reference No. 518.)<br />
NA: If MAC cannot be accessed directly fi-om the field and another base hospital is contacted,<br />
that base hospital should contact MAC for coordination of treatment and transport.<br />
Revised: 512005<br />
PAGE 1 OF 2
,)<br />
Section 2: Patient Transportation 1 Destination<br />
DECOMPRESSION 1<br />
Paramedics should simultaneously establish base hospital contact with LAC/USC Medical Center<br />
and the Medical Alert Center (MAC) via the Hospital Emergency Administrative Radio (HEAR)<br />
for any patient suspected of having a decompression emergency.<br />
LACNSC Medical Center will provide medical orders for patient care and determine if the<br />
patient should be transported directly from the incident location to a hyperbaric chamber.<br />
MAC will determine which hyperbaric chamber is most appropriate to the needs of the patient and<br />
coordinate transportation to the chamber for the patient and medical personnel. (Factors considered<br />
include: patient condition, distance, altitude, ETA of available transportation, and limitations of<br />
various aircraft.)<br />
* Obtain dive incident history of the patient and dive partner, if able.<br />
* Coordinate patient transportation to the appropriate receiving facility.<br />
Retrieve patient's dive equipment (e.g., regulator, tank, gauges, weight belt,<br />
etc.) and transport with patient.<br />
As a general rule, the integrity of the dive equipment should be maintained and not<br />
tampered with except by investigating authorities. (Refer to DHS, Reference No. 518.)<br />
NA: If MAC cannot be accessed directly from the field and another base hospital is contacted,<br />
that base hospital should contact MAC for coordination of treatment and transport.<br />
Revised: 121200 1<br />
PAGE 2 OF 2
Section 2: Patient Transportation 1 Destination<br />
PATIENT DESTINATION GUIDELINES<br />
a'- <strong>EMS</strong> personnel shall use the following guidelines when making patient destination decisions: -V<br />
, 1<br />
PATIENTS 0-14 YEARS OLD: Transport to themost accessible EDAP I PMC I PTC<br />
1 PATIENTS 15 YEARS or OLDER: Transport to the most accessible receiving (MAR) facility 1<br />
Emergency Departments Approved for Pediatrics (EDAP)<br />
Brotman<br />
California<br />
Cedars Sinai ** +<br />
Centinela Freeman-Centinela<br />
Centinela Freeman-Memorial<br />
Childrens Hospital LA * * +<br />
Columbia - West Hills<br />
Downey Regional<br />
East LA Doctors<br />
Encino Tarzana - Tarzana<br />
Gardena Memorial<br />
Glendale Adventist<br />
Glendale Memorial<br />
Harbor/UCLA Medical Center * * +<br />
Henry Mayo Newhall Memorial<br />
Huntington Memorial * *<br />
Kaiser - Woodland Hills<br />
KingIDrew<br />
LAC/USC Medical Center ** +<br />
Little Company of Mary-San Pedro<br />
Little Company of Mary-Torrance<br />
Long Beach Memorial ** +<br />
Northridge - Roscoe Campus<br />
Pacifica of the Valley<br />
Providence Holy Cross<br />
Providence St. Joseph<br />
Robert F. Kennedy<br />
St. Francis<br />
St. John's<br />
St. Mary Medical Center<br />
San Gabriel Valley<br />
Santa Monica - UCLA<br />
Simi Valley<br />
Torrance Memorial<br />
UCLA Medical Center * * +<br />
Valley Presbyterian<br />
Verdugo Hills<br />
White Memorial<br />
** PMC + PTC Italics denotes "Trauma Center"<br />
If the patient is stable, honor the patient's or physician's request. Normally, the transportation time shall<br />
not exceed 20 minutes (non-emergency). Extended transport times require authorization from OCD.<br />
Internal Disaster: No BLS or ALS Transport<br />
Emergency Room (ER) Saturation: No ALS Transport<br />
Neuro, CT Scan, Trauma, PTC: No ALS Transport (for patients requiring these specialties)<br />
"Service Area" hospitals may @ divert except for INTERNAL, DISASTER. Diversion<br />
transportation time is 15 minutes (Code 3) to an open emergency room (ER). If ER is open, within<br />
the 15 minute transport time, transport to the most accessible ER.<br />
Revised: 512005<br />
PAGE 1 OF 1<br />
1'
Section 2: Patient Transportation 1 Destination<br />
TRANSPORTING PATIENTS IN CUSTODY<br />
Utilize the following procedural guidelines when requested by LAPD<br />
(or other law enforcement agencies) to transport a patient in custody:<br />
+ A law enforcement officer shall ride in the back of the rescue ambulance with the patient<br />
at all times.<br />
+ Patients shall be transported to the most accessible medical facility. (Patient's from the<br />
Central Jail or Parker Center shall be transported to LACAJSC's 13th floor Jail Ward, unless<br />
in extremis).<br />
+ Restrained patients shall not be transported in the prone (facelchest downward) position.<br />
Such patients shall be transported in the left lateral position.<br />
+ Restraint equipment, applied by <strong>EMS</strong> personnel, must be either padded leather or soft<br />
restraints. Restraint methods must allow for quick release. (DHS Reference # 838)<br />
+ Restrained extremities shall be evaluated for pulse quality, capillary refill, color, nerve,<br />
and motor status every 15 minutes or less.<br />
REQUIRED DOCUMENTATION ON THE <strong>EMS</strong> REPORT FORM (F-902M)<br />
SHALL INCLUDE:<br />
The type of and reason restraints were needed.<br />
2 Identity of agencylmedical facility applying restraints.<br />
Assessment of the circulatory and neurological status of the restrained extremities.<br />
Any abnormal findings require the restraints to be removed and reapplied or<br />
supporting documentation.<br />
Assessment of the cardiac and respiratory status of the restrained patient.<br />
HOSPITAL REFUSAL TO ACCEPT RESCUE AMBULANCE PATIENTS<br />
Personnel encountering serious problems at a hospital emergency room (i.e., refusing patient) shall<br />
contact OCD and request an <strong>EMS</strong> Battalion Captain to respond to their location. It shall be the<br />
responsibility of the <strong>EMS</strong> Battalion Captain to investigate the circumstances and ensure that proper<br />
base hospital notification/docurnentation is made. Journal entries of the incident shall be made and<br />
the Station Commander notified. Once a patient arrives inside the intended emergency room, the<br />
patient shall remain.<br />
Revised: 512005<br />
PAGE 1 OF 1
hospitals have an agreement with the <strong>EMS</strong> Agency that only those patients within a given boundary<br />
will be transported to their facility. Service area hospitals may honor patient requests from outside<br />
of their service area; however, they are not obligated to do so.<br />
All <strong>LAFD</strong> ambulances with any ALS or BLS patient, within a defined service area, will transport<br />
to the service area hospital, maintaining the service area hospital agreement.<br />
(In most instances the service area hospital is also the MAR.)<br />
Patients who meet criteria or guideline for a specialty care center (e.g., EDAP, PMC, Trauma,<br />
Perinatal) not provided by the service area hospital, shall be transported to the appropriate<br />
specialty care center.<br />
Patients exhibiting uncontrollableproblems in the field will be transported to the most accessible<br />
medical facility regardless of incident location.<br />
Patients from multiple casualty incidents may have to cross boundaries, depending on incident<br />
location or direction from the base hospital or Medical Alert Center.<br />
N-: Service area hospitals shall not be on diversion for any categories other than Internal Disaster.<br />
It is the responsibility of BLS and ALS personnel to recognize the appropriate receiving hospital<br />
based on the patient's condition and incident location.<br />
CALIFORNIA MEDICAL CENTER<br />
CENTINELA FREEMAN-CENTINELA<br />
CENTINELA FREEMAN-MEMORIAL<br />
EAST LA DOCTORS<br />
GOOD SAMARITAN<br />
EDAP<br />
EDAP<br />
EDAP<br />
EDAP<br />
PERINATAL<br />
PERINATAL<br />
PERINATAL<br />
PERINATAL<br />
PERINATAL<br />
I I I<br />
1 MEMORIAL HOSP. OF GARDENA 1 ED AP 1 PERINATAL 1 1<br />
WHITE MEMORIAL MED. CENTER<br />
Patient requests for transport to a service area hospital when the incident location is outside the<br />
hospital's defined service area or inside the service area of another hospital may be honored by:<br />
1 BLS Resource (For BLS patients):<br />
EDAP<br />
PERINATAL<br />
NICU<br />
NICU-<br />
NICU<br />
The receiving hospital agrees to accept the patient.<br />
The transporting unit is not unreasonably removed from its primary response area.<br />
1 ALS Resource:<br />
Base Hospital concurs that the patient's condition is stable to permit the estimated transpoi -t time.<br />
The requested hospital agrees to accept the patient.<br />
The transporting unit is not unreasonably removed from its primary response area.<br />
NICU<br />
NICU<br />
N*: The receiving hospital may be contacted directly if the ALS unit is transporting a BLS patient.<br />
Revised: 512005<br />
PAGE 1 OF 1<br />
/-^<br />
1
Section 2: Trans~ortation 1 Destination<br />
Good Samaritan Hospital & California Hospital<br />
Good Samaritan Hospital and California Hospital have the above service<br />
area boundaries and are divided by Olympic Blvd.<br />
If BOTH hospitals are listed as emergency department "SATURATED,"<br />
adult patients from incident locations:<br />
NORTH of Olympic B1vd.-transport to Good Samaritan Hospital.<br />
SOUTH of Olympic B1vd.- transport to California Hospital.<br />
1 DESTINATION CRITERIA<br />
Rescue ambulance personnel shall access the Mobile Data Terminal (MDT) to<br />
determine the hospital emergency department status prior to initiating transport.<br />
If either hospital is listed as an emergency department "SATURATED," service<br />
area patients shall be taken to the other hospital.<br />
CAI, California Medical Center 133 EDAP, PERINATAL, NICU Thomas Guide Pg. 634-D6<br />
1<br />
I I I<br />
GSH 1 Good Samaritan Hospital 1 220 [PERINATAL, NICU<br />
I<br />
1 Thomas Guide Pg. 634-D3 1<br />
Revised: 512005
HOSPITAL OF THE GOOD SAMARITAN<br />
&<br />
CALIFORNIA MEDICAL CENTER<br />
Service Area<br />
Revised: 512005 PAGE 2 OF 8
Section 2: Transportation I Destination<br />
Centinela Freeman-Centinela & Centinela Freeman-Memorial<br />
Patients fiom incident locations:<br />
4 Within the "Secondary Service Area'' may be transported to Centinela Freeman-<br />
MEMORIAL (DFH) or CENTINELA FREEMAN-CENTINELA (CNT).<br />
4 West of the 405 Freeway, may be transported to Centinela Freeman- MARINA (DFM).<br />
BMC<br />
CNT<br />
DFM<br />
DFH<br />
kl?W<br />
4 All PEDIATRIC patientsy age 14 or less not meeting pediatric trauma or PMC criteria,<br />
shall be transported to Centinela Freeman- MEMOFUAL Hospital.<br />
4 All adult patients, age <strong>35</strong>2, with the chief complaint of CHEST PAIN or<br />
SYMPTOMATIC DYSRHYTHMIAy shall have ALS transport to CENTINELA FREEMAN-<br />
CENTINELA<br />
Permissible EXCEPTIONS to transporting patients to this destination are:<br />
d Incidents involving patients requiring transport to a specialty care facility<br />
(trauma center or pediatric critical care center).<br />
4 When honoring a patient request in accordance with Department customer service guidelines.<br />
d When facility is closed due to internal disaster.<br />
Brotman Medical Center<br />
Centinela Freeman-CENTINELA<br />
Centinela Freeman MARINA<br />
Centinela Freeman MEMORIAL<br />
Kaiser-West LA<br />
172<br />
141<br />
457<br />
153<br />
362<br />
EDAP<br />
Revised: 512005 PAGE 3 OF 8<br />
EDAPy PERINATAL, NICU<br />
EDAP, PERINATAL, NICU<br />
PERINATAL<br />
Thomas Guide Pg. 672-Gl<br />
Thomas Guide Pg. 703-D4<br />
Thomas Guide Pg. 762-B6<br />
Thomas Guide Pg. 703-D2<br />
Thomas Guide Pg. 632-J6
Secondary Service Area:<br />
The Secondary Service Area will become effective when all receiving hospitals within<br />
15 minutes from the incident location7 in the Secondary Service Area7 have requested<br />
diversion to ED saturation. In this instance, patients may be transported to DFH or CNT.<br />
I<br />
Manchester Ave. Boundary:<br />
When both DFH and CNT have requested diversion due to ED saturation7 patients<br />
will be transported as follows:<br />
Patients NORTH of MANCHESTER Ave. will be transported to DFH.<br />
Patients SOUTH of MANCHESTER Ave. will be transported to CNT.<br />
Revised: 512005
MHG<br />
CNT<br />
MLK<br />
SFM<br />
HGH<br />
Section 2: Transportation I Destination<br />
Memorial Hospital of Gardena<br />
LEGEND 1<br />
Memorial Hospital of Gardena<br />
Centinela Hospital-CENTINELA<br />
KingDrew<br />
St. Francis<br />
HarborRJCLA<br />
EDAP, PERINATAL<br />
EDAP, PERINATAL, NICU<br />
EDAP, PERINATAL<br />
Revised: 512005 PAGE 5 OF 8<br />
EDAP, PERINATAL, TFUUMA<br />
PMC, EDAP, PERINATAL,<br />
TRAUMA, PTC<br />
Thomas Guide Pg. 734-A5<br />
Thomas Guide Pg. 703-D4<br />
Thomas Guide Pg. 704-G7<br />
Thomas Guide Pg. 705-B6<br />
Thomas Guide Pg. 764-A6
Revised: 512005<br />
MEMORIAL HOSPITAL OF GARDENA<br />
Service Area<br />
PAGE 6 OF 8
Section 2: Transportation 1 Destination<br />
White Memorial Medical Center<br />
(Including East LA Doctors)<br />
DESTINATION CRITERIA k<br />
While in the White Memorial Service Area, rescue ambulance personnel shall transport to the most<br />
accessible, open hospital within the Service Area, e.g., White Memorial Medical Center, East Los<br />
Angeles Doctors, or LACAJSC Medical Center..<br />
LEGEND<br />
WMH White Memorial Med.Cent.<br />
970<br />
Thomas Guide Pg. 6<strong>35</strong>-A4<br />
EDAP, PERINATAL, NICU<br />
1 ELA l~ast Los Angeles Doctors 1 157 1 EDAP, PERINATAL 1 Thomas Guide Pg. 6<strong>35</strong>-D7 1<br />
1 I PMC, PERINATAL, NICU,<br />
LAC/USC Medical Center 438 TMw, pTc (USE) 1 Thomas Guide Pg. 6<strong>35</strong>-B3<br />
Revised: 512005 PAGE 7 OF 8
WHITE MEMORIAL MEDICAL CENTER<br />
Service Area<br />
Revised: 512005<br />
PAGE 8 OF 8
Section 2: Patient Trans~ortation 1 Destination<br />
LOS ANGELES COUNTY <strong>EMS</strong> RECEIVING FACILITIES 1<br />
/Al hambra Hospital 1 (626) 570-1606 1 100 S. Raymond Ave., Alhambra, 91801 1<br />
Beverly Hospital * A (323) 726-1222 309 W. Beverly Blvd., Montebello, 90640<br />
Brotman Medical Center * (310) 836-7000 3828 Delmas Terrace, Culver City, 90231<br />
1 . California Hospital Medical Center * A I (213) 748-2411 1 1338 S. Hope St, Los Angels, 90015 1<br />
1 Cedars-Sinai Medical Center ** A I (310) 855-5000 1 8700 Beverly Blvd., Los Angeles, 90048<br />
1 Centinela Airport Medical Center 1 1 9601 S. Sepulveda, Los Angeles, 90045<br />
1 Centinela Freeman-Centinela * A 1 (310) 673-4660 1 555 E. ~ardy~t., Inglewood, 90301<br />
Centinela Freeman-Marina (310) 823-891 1 4650 Lincoln Blvd., Marina Del Rey, 90291<br />
Centinela Freeman- Memorial * A (310) 674-7050 333 N. Prairie Ave., Inglewood, 90301<br />
Century City Hospital (ER CLOSED 4/04)<br />
Children's Hospital of Los Angeles * ** (323) 660-2450 4650 Sunset Blvd., Los Angeles, 90027<br />
Coast Plaza Doctors (562) 868-3751 13100 Studebaker Road, Norwalk, 90650<br />
Columbia West Hills Medical Center * A (818) 676-4000 7300 Medical Center Dr., West Hills, 91307<br />
Downey Regional * A (562) 904-5000 11 500 Brookshire Ave., Downey, 90241<br />
1 East Los Anaeles Doctors * A 1 (323) 268-5514 1 4060 E. Whittier Blvd., Los Angles,90023<br />
JEncino Tarzana Regional -Encino 1 (818) 995-5000 1 16237 Venture Blvd., Encino, 91436<br />
1 Encino Tarzana Regional -Tarzana * A 1 (818) 881-0800 1 18321 Clark St., Tarzana, 91<strong>35</strong>6> 1<br />
Garfield Medical Center * A (626) 573-2222 525 N. Garfield Ave., Monterey Park, 91754<br />
Glendale Adventist Medical Center * A (818) 409-8111 . 1509 Wilson Terrace, ~lendal'e,91206 -<br />
Glendale Memorial * A (81 8) 502-1 900 1420 S. Central Ave., Glendale, 91225-7036<br />
I ,<br />
Good Samaritan A 1 (213) 977-21 21 1 616 S. Witmer St., Los ~n~eles,~~fl017<br />
' , ' -<br />
Harbor/UCLA Medical Center * ** A .<br />
(310)<br />
222-2345 1000 W. Carson St., Torrance, 90509<br />
Henry Mayo Newhall Memorial * (661) 253-8000 23845 W. McBean Parkway, ~alencia, 91<strong>35</strong>5<br />
Huntington Memorial * ** A (626) 397-5000 100 W. California Blvd., Pasadena, 91109<br />
1 Kaiser Hospital - Baldwin Park A 1 (626) 851 -1 01 1 1 1011 Baldwin Park Blvd., Baldwin Park, 91706 1<br />
Kaiser Hospital - Bellflower A (562) 461 -3000 9400 E. Rosecrans Ave., Bellflower, 90706<br />
1 Kaiser Hospital - South Bay A<br />
I<br />
1 (310) 325-51 11<br />
t<br />
1 25825 S. Vermont Ave., Harbor City, 90710 1<br />
Kaiser Hospital - Sunset (LA) A (323) 783-401 1 4867 Sunset Blvd., Los Angels, 96027<br />
a?<br />
1 Kaiser Hospital - Panorama City A 1 (818) 375-2000 1 13652 Cantara St., Panorama City, 91402 1<br />
1 Kaiser Hospital - West Los Angeles A 1 I (323) 857-2000 1 I 6041 Cadillac Ave., Los ~ngeIe~9.Qw .<br />
Kaiser Hospital -Woodland Hills * A (818) 719-3800 5601 De Soto Ave., Woodland Hills, 91367<br />
Little Company of MayTorrance * A (310) 540-7676 4101 Torrance Blvd.,Torrance, 90503<br />
Revised: 512005<br />
PAGE 1 OF 2<br />
I
^<br />
Section 2: Patient Transportation 1 Destination<br />
1 Little Company of Mary-San Pedro * A<br />
1 Long Beach Community * A<br />
(31 0) 832-331 1<br />
(562) 498-1000<br />
1300 W. 7th St, San Pedro, 90732<br />
1720 Terrnino Ave., Long Beach, 90804<br />
Long Beach MemorialMedical Center * ** A (562) 933-231 1 2801 Atlantic Ave., Long Beach, 90806<br />
LA County Olive View Medical Center A (81 8) 364-1 555 14445 Olive View Dr., Sylrnar, 91342-1495<br />
LAC/USC Medical Center ** * A<br />
Martin Luther King JrDrew Medical Center * A<br />
Memorial Hospital of Gardena * A<br />
(323) 226-2622<br />
(310) 668-4321<br />
(310) 532-4200<br />
1200 N. State St, Los Angeles, 90033<br />
12021 S. Wilmington Ave., Los Angeles, 90059<br />
1145 W. Redondo Beach Blvd., Gardena,<br />
I I<br />
Mission Community Hospital I (818) 787-2222 I 14850 Roscoe Blvd., Panorama City, 91402<br />
Monterey Park Hospital A (626) 570-9000 900 S. Atlantic Blvd., Monterey Park, 91754<br />
Olympia Medical Center<br />
Pacific Hospital of Long Beach A<br />
Pacifica Hospital of the Valley * A<br />
Providence Holy Cross Medical Center * A<br />
Providence Saint Joseph Medical Center * A<br />
Saint Francis Medical Center * A<br />
Saint John's Hospital and Medical Center *<br />
Saint Mary Medical Center * A<br />
San Gabriel Valley Medical Center * A<br />
Santa Monica - UCLA Medical Center * A<br />
Sherman Oaks Community Hospital<br />
(323) 938-3161<br />
(562) 595-191 1<br />
(81 8) 767-3310<br />
(818) 365-8051<br />
(81 8) 843-51 11<br />
(310) 603-6000<br />
(310) 829-5511<br />
(562) 491-9000<br />
(626) 289-5454<br />
(310) 319-4000<br />
(81 8) 981 -71 11<br />
5925 San Vicente Blvd., Los Angeles, 90019<br />
2776 Pacific Ave., Long Beach, 90806<br />
9449 San Fernando Road, Sun Valley, 91<strong>35</strong>2<br />
15031 Rinaldi St, Mission Hills, 91345<br />
501 S. Buena Vista St, Burbank, 91505<br />
3630 Imperial Highway, Lynwood, 90262: ,<br />
2103 Santa Monica Blvd., Santa Monica, 90404<br />
1050 Linden Ave., Long Beach, 90813<br />
218 S. Santa Anita St, San ~~bri$l,91776> .<br />
1250 Sixteenth St, Santa Monica, 90404<br />
4929 Van Nuys Blvd., Shennan OW, 91403<br />
1 UCLA Medical Center * ** A 1 (310) 825-91 11 1 10833 Le Conte Ave., Los Angeles, 9@24 1<br />
1 Valley Presbyterian Hospital * A 1 (818) 782-6600 1 15107 Vanowen St, Van Nuys, 91405 1<br />
1 Verdugo Hills Hospital * A I (81 8) 790-71 00 1 1812 Verdugo Blvd., Glendale, 91208,<br />
1 White Memorial Medical Center * A I (323) 268-5000 1 1720 Cesar Chavez Ave., Lo8 Angeles, 90033 1<br />
Revised: 512005<br />
"Italics" Denotes TRAUMA CENTER<br />
* EDAP<br />
** PMC<br />
PAGE 2 OF 2<br />
PTC<br />
A PERINATAL<br />
"1
Section 2: Patient Transportation 1 Destination<br />
Revised: 712004<br />
BATTALION OFFICES<br />
PAGE 1 OF 1
RECEIVING HOSPITALS SORTED BY <strong>EMS</strong> BATTALION OFFICE<br />
Section 2: Patient Transportation 1 Destination<br />
California, Orthopaedic<br />
Glendale Adventist, Glendale Memorial,<br />
Huntina ton Memorial<br />
Hudson Clinic<br />
Centinela Airport Clinic, Centinela Freeman-<br />
Centinela, Centinela Freeman-Marina,<br />
Centinela Freeman-Memorial<br />
Children's, Kaiser Los Angeles,<br />
Queen of AngelsIHollywood Presbyterian<br />
HarborIUCLA, Kaiser South Bay,<br />
Little Company of Mary-San Pedro,<br />
Little Company of Mary-Torrance,<br />
Long - Beach Memorial, Pacific of Long Beach,<br />
St. Mary, Torrance Memorial<br />
Alhambra, Beverly, East Los Angeles Doctors,<br />
Garfield, ~aiser Baldwin park; LACIUSC,<br />
Monterey Park, San Gabriel Valley,<br />
White Memorial<br />
St. John's, Santa MonicaIUCLA,<br />
UCLA, Veterans Administration Wadsworth<br />
Encino Tarzana-Encino,<br />
Sherman Oaks, Valley Presbyterian<br />
Good Samaritan<br />
Henry Mayo, Kaiser Panorama City,<br />
Mission Community, Olive View, Pacifica,<br />
Providence Holy Cross, Verdugo Hills<br />
Coast Plaza Doctors, Downey Regional,<br />
Gardens Memorial, Humphrey Clinic,<br />
Kaiser Bellflower, KingIDrew, St. Francis<br />
Providence St. Joseph<br />
Northridge-Roscoe, Simi Valley<br />
Columbia West Hills, Encino Tarzana-Tarzana<br />
Kaiser Woodland Hills<br />
Brotman, Cedars-Sinai, Century City,<br />
Kaiser West Los Angeles, Olympia<br />
PAGE 1 OF 1
3 9 1 3 1 10 78 1 14 14 114 1<br />
PAGE 1 OF 1<br />
Section 2: Patient Transportation 1 Destination
A Section<br />
1 1<br />
2: Patient Transportation 1 Destination<br />
<strong>LAFD</strong> RESCUE AMBULANCE LOCATIONS<br />
1 1 1 7 1 2230 N. Pasadena Ave. 1 Lincoln Heights 1 pg. 595 A-7 1 (21 3) 485-6201 , '<br />
1 3 I 3 1 803 1 1 1 108 N.FremontAve. 1 Bunker Hill 1 634 F-3 1 (213) 485-6203 1<br />
5 1<br />
5 1 1 4 I 6621 W. Manchester Ave. 1 Westchester 1 702 F-3 l(213) 485-6205 1<br />
1 1 1 430 E. Seventh St. 1 Civic Center 1 634 F-5 1(213)485-6209 1<br />
1 11 I 11 I811 1 11 11819 W.SeventhSt. 1 Westlake 1 634 C-3 1(213)485-6211 1<br />
1 11 I 1206 S. Vermont Ave. 1 Pico Heights 1 634 A-4 l(213) 485-6213 1<br />
1 3 I 915 W. JeffersonBlvd. 1 USC Campus 1 634 B-7 (213) 485-6215 1<br />
1 1 1 1601 S. Santa Fe Ave. 1 Industrial Eastside 1 634 H-7 1 (2 13) 485-621 7<br />
1 9 1 12229 W. Sunset Blvd. 1 Brentwood 1 631 G-3 (310)575-8519 1<br />
1 21 1 21 1 1 3 11187 E.52ndSt. 1 South Los Angeles 1 674 E-4 1 (213) 485-6221 1<br />
1 V824 1 12 I 9411 Wentworth St. 1 SunlandlShadow His 1 503 D-3 1 (8 18) 756-8624 1<br />
1 26 I 26 I 826 I 3 I 2009 S. Western Ave. 1 West Adams 1 633 H-6 1 (2 13) 485-6226 1<br />
1 828 1 15 1 11641 Corbin Ave. 1 Porter Ranch 1 500 E-1 1 (818) 756-9728 1<br />
1 n I 33 18% I 13 I6406 S.MainSt. 1 South Los Angeles 1 674 C-6 1 (2 13) 485-6233 1<br />
<strong>35</strong>1- I 8<strong>35</strong> I 5 I 1601 N. Hillhurst Ave. 1 Los Feliz 1 594 A-4 l(213) 485-62<strong>35</strong> 1<br />
Revised: 512005 PAGE 1 OF 3
A Section 2: Patient Trans~ortation 1 Destination<br />
1 44 1 1 844 I 2 1 1410 Cypress Ave. I Cypress Park 1 595 H-4 (213) 485-6244 1<br />
1 47 1 47 1 1 7 1 4575 E. Huntington Dr. S. 1 Monterey Hills 1 595 D-6 l(213) 485-6247 1<br />
1 49 1 1 V849 I 6 1 400 Yacht St.,Berth 194 1 Wilmington 1 824 F-1 1(310)548-7549 1<br />
I 51 I 51 I 1 4 1 104<strong>35</strong> Sepulveda I LAX 1 702 0-5 ] (213) 485-6251 1<br />
1 55 1 55 1 1 2 I 4455 E. York Blvd. I Eagle Rock 1 594 J-1 l(213) 485-6255 1<br />
1 57 1 57 1257 1 V857 1 13 1 7800 S. Vermont Ave. 1 South Los Angeles 1 704 A-1 1(213)485-6257 1<br />
1 59 1 59 1 1 9 1 11505 W. Olympic Blvd. 1 West Los Angeles I 632 B-6 I(310) 575-8559 1<br />
\ 161 1 61 1 861 1 18 15821 W.ThirdSt. 1 Park LaBrea 1 633 D-1 1(213)485-6261 1<br />
1 4 1 1930 Shell Ave. 1 Venice 1 671 J-5 l(310) 575-8563 1<br />
1 65 16512651 1 13 11525. E.103rdSt. 1 watts 1 704 F-5 l(213) 485-6265 1<br />
1 68 I 68 1 868 1 18 I 5023 W. Washington Bl. 1 Mid-City 1 633 D-5 1(213)485-6268 1<br />
Il-70 1 1 15 1 9861 Reseda Blvd. 1 Northridge 1 500 J-5 1(818)756-8670 1<br />
1 17 1 681 1 De Soto Ave. 1 Canoga Park 1 530 C-6 l(818) 756-8672 1<br />
- - - - - -<br />
I 74 I 74 I 1 12 1 7777 Foothill Blvd. 1 Tujunga 1 503 H-3 l(818) 756-8674 1<br />
1 V876 I 5 I 31 11 N. Cahuenga Bl. 1 Cahuenga Pass 1 593 D-1 l(213) 485-6276 1<br />
1 V878 I 14 1 4230 Coldwater Cyn. Av 1 Studio City 1 562 E-5 l(818) 756-8678 1<br />
80 1 1 691 1 World Way West 1 LAX Crash Rescue 1 702 E-5 l(213) 485-6280 1<br />
Revised: 512005<br />
PAGE 2 OF 3
Section 2: Patient Trans~ortation / Destination<br />
1 81 1 81 1 881 1 12 114123 Nordhoff St. 1 Arleta I P ~ . 502 B-7 1 (818) 756-8681 1<br />
1 83 1 83 1 1 10 I 5001 BalboaBlvd. 1 Encino 1 561 D-3 1(818)756-8683 1<br />
1 6 I 1331 W. 253rd St. 1 Harbor City 1 794 A-4 l(310) 548-7585 1<br />
1 87 1 87 1 1 15 1 10241 Balboa Blvd. 1 Granada Hills 1 501 C-4 l(818) 756-8687 1<br />
1 89 1 89 1 889 1 14 1 7063 Laurel Canyon Blvd. 1 North Hollywood 1 532 G-5 l(818) 756-8689 1<br />
1 91 1 91 1 V891 1 12 1 14430 Polk St. 1 482 A-4 l(818) 756-8691 1<br />
1 95 1 95 1 1 4 1 10010 International Rd. 1 LA Airport 1 702 J-5 l(213) 485-6295 1<br />
1 97 1 1 V897 1 14 1 8021 Mulholland Drive 1 Laurel Canyon 1 592 J-1 l(818) 756-8697 1 . !<br />
--<br />
9 9 199 10 1 14145 Mulholland Drive 1 Beverly Glen I 562 A-7 l(818) 756-8699 1<br />
1 103 1 103 1 1 15 1 18143 Parthenia St. 1 Northridge 1 531 A-1 l(818) 756-8603 1<br />
1 109 I I V909 1 10 I 16500 Mulholland Drive I Encino Hills 1 561 E-7 l(818) 756-8609 1<br />
1 Ill ] I I 6 I 1444 S. Seaside, Berth 256 1 Fish HarborlTenn Is. 1 824 D-5 l(310) 548-7541 1<br />
114 I 8060 Balboa Place-Air Ops Van Nuys Airport<br />
Legend: "V" = Variable Staffing<br />
Revised: 512005<br />
PAGE 3 OF 3<br />
,
Section 3: Apparatus 1 Equipment<br />
. . . .<br />
APPARATUS TOWING / BREAKDOWN PROCEDURES<br />
1 0630-2300 HOURS 1<br />
1. Notify OCD and Battalion Commander of status.<br />
2. OCD shall contact the Shops or mechanic to<br />
determine: tow, repair, or if a relief apparatus is<br />
required.<br />
3- Battalion Commander shall arrange transportation.<br />
4. OCD shall report time towing contractor was<br />
notified.<br />
5. Tow to nearest S&M facility; if accident, tow to<br />
Central Shops.<br />
6- A member shall accompany the apparatus or<br />
meet the contractor at the Shops for security<br />
and to validate the tow invoice.<br />
2300-0630 HOURS<br />
1- Notify OCD and Battalion Commander of<br />
status.<br />
-<br />
\<br />
'<br />
Company Commander shall determine if<br />
repairs may be made by members or Heavy<br />
Rescue; and if a relief apparatus is required.<br />
3, Update OCD of status.<br />
4. Tow utilizing procedures 5 and 6 above.<br />
1. Notify OCD and Battalion Commander of status.<br />
2. Company Commander shall determine if field<br />
repair or towing is required.<br />
3- Company Commander shall arrange for a relief<br />
apparatus and change over.<br />
4. After change over, notify OCD that a tow<br />
is needed.<br />
5- A member shall accompany the apparatus or<br />
meet the contractor at the Shops for security and<br />
to validate the tow invoice.<br />
2300-0630 HOURS<br />
1. Notify OCD and Battalion Commander of status.<br />
2. Company Commander shall arrange for repair<br />
or change over to a relief apparatus.<br />
3. Update OCD of status.<br />
4. Store apparatus in quarters overnight and tow<br />
utilizing towing procedures above.<br />
If the Shops are closed and Rescue Maintenance is not in quarters, contact OCD on the telephone<br />
outside of the office for entry. Use the gate keys in the lock box to open the yard and leave apparatus.<br />
Leave a note to briefly describe the apparatus type, problems, and status. Secure yard before leaving.<br />
The following information is needed for the tow invoice:<br />
1. Name of towing service<br />
2. Make, year, and Shop No. of apparatus<br />
3. Address where towing was initiated<br />
4. Date and time tow contractor was notified<br />
5. Time towing service arrived on scene<br />
6. Time towing was completed<br />
Sign the receipt, include your assignment and telephone number, then forward to S&M at:<br />
Mail Stop 253. An F-80 is required for the repairs, but not for the towing.<br />
Revised: 121200 1 PAGE 1 OF 1
Section 3: Apparatus 1 Equipment<br />
APPARATUS MAINTENANCE<br />
Maintenance procedures are performed periodically based on the pre-described maintenance<br />
schedules set forth in Volume 3-710 and Department Log <strong>Book</strong>s. The Station Commander is<br />
ultimately responsible for the condition of apparatus under hislher command, but each<br />
member shares equally in the responsibility of maintaining Department apparatus.<br />
To increase the performance and life of Department apparatus, daily, weekly, monthly, and<br />
bi-monthly preventive maintenance checks are preformed. Certain basic procedures in daily<br />
maintenance pre-checks on all apparatus shall be accomplished at the beginning of each shift or<br />
at any time a change of relief occurs. Refer to <strong>LAFD</strong>, <strong>Book</strong> 8, Drivers <strong>Training</strong> <strong>Manual</strong>, Module 4.<br />
The Preventive Maintenance form [F-3 771 RA applies to all Rescue Ambulances (active, reserve,<br />
and standby) that are serviced by field personnel. It is used to record the preventive maintenance<br />
performed and problems discovered. Refer to MOP, Volume 3- 711-48.32.<br />
The form is:<br />
+ Completed monthly by the responsible member.<br />
+ Original forwarded to Battalion Commander within the first two weeks of each month<br />
(prior to Battalion inspection).<br />
+ Copy retained in Apparatus Log <strong>Book</strong> until replaced by original from Battalion.<br />
+ Original retained in Log <strong>Book</strong> for one year.<br />
All needed repairs will be reported as directed in MOP, Volume 4,813-40.40 and 40.50 (this includes<br />
brake adjustment, emergency lighting, steering, warning devices, etc.). - 1<br />
Revised: 12/2001 PAGE 1 OF 1
CAV / NAV<br />
Section 3: Apparatus / Equipment<br />
AVI 1 Available within 60 seconds (1 minute)<br />
Available within 180 seconds (3 minutes) Fire Resources<br />
Available within 60 seconds (1 minute) ALS 1 BLS Rescue Ambulance<br />
k<br />
NAV<br />
Not available for dispatch<br />
Mobile Data Terminal (MDT) unit status shall be updated and correct at all times while<br />
AVI (Available), CAV (Conditionally Available), or NAV (Not Available).<br />
A Journal (F-2) entry shall be made for CAV / NAV status (include times and reason).<br />
Resources that are CAV shall maintain radio watch at all times.<br />
CHANNEL 4: METRO (RESCUE ONLY) CHANNEL 18: FRANK HOTCHKIN<br />
MEMORIAL TRAINING<br />
CHANNEL 7: METRO<br />
CENTER [FHMTC]<br />
CHANNEL 8: VALLEY<br />
Provide the following information to OCD when requesting CAV status:<br />
e The amount of time (before the resource will be available to respond - within 1-3 minutes).<br />
+ The CAV status reason:<br />
Routine <strong>Training</strong> 43<br />
, I<br />
37 1 Required <strong>Training</strong> 1 44<br />
38 1 Mechanical<br />
39 r~eturnin~ From Move-up<br />
-- 1 45<br />
I 46<br />
40 Returning From Incident<br />
47<br />
4 1 Community Relations<br />
48<br />
#<br />
42 1 Equipment1 Supplies Restock 1 49<br />
- -- -<br />
StafFing<br />
CAV Other - Must Specify<br />
Fire Prevention<br />
Non-Emergency Move-up<br />
Continuing Education<br />
Oil Change<br />
EMT <strong>Training</strong><br />
Provide the following information to OCD when requesting NAV status:<br />
+ The location where the resource will be NAV. (This may be a fire stations first-in district or a location code.)<br />
+ The NAV status reason:<br />
Revised: 912003 PAGE 1 OF 1<br />
26 1 Routine <strong>Training</strong><br />
27 EMT Re-certification<br />
I<br />
29 Decontamination<br />
30 Annual Apparatus Testing<br />
3 1 NAV Other - Must Snecifi<br />
- -<br />
32 1 Change Over<br />
33 1 No Hospital Beds<br />
34 1 Oil Change<br />
m<br />
1<br />
1<br />
I<br />
<strong>35</strong> 1 Required <strong>Training</strong> 1
. Section 3: Apparatus 1 Equipment<br />
- . . .<br />
OBTAINING A SPARE GURNEY<br />
A cache of spare gurneys is maintained at each <strong>EMS</strong> Battalion Office.<br />
The procedure to obtain a spare gurney is as follows:<br />
* Notify the Station Commander and <strong>EMS</strong> Battalion office.<br />
* Ascertain the availability of spare gurneys at the <strong>EMS</strong> Battalion office.<br />
* Take the defective gurney to the <strong>EMS</strong> Battalion office and attach an F-175 tag stating the problem.<br />
* Label the new gurney with your RA designation, using 2%'' red decals.<br />
Place decals on each side panel of the gurney.<br />
* Make appropriate journal entry when you return to quarters.<br />
Use Extreme Caution at all times when operating gurneys to prevent patient injury<br />
andlor private property damage. Particular attention shall be given when:<br />
Repositioning into a chair position, moving through confined areas and doorways,<br />
transporting combative andlor altered mental status patients, and loading patients<br />
inlout of an ambulance. Active measures are required by members to assure the<br />
safe position of the patients hands and extremities to prevent injuries.<br />
Revised: 912003 PAGE 1 OF 1
tion 3: Apparatus 1 Equipment<br />
MULTI-CASUALTY MEDICAL SUPPLY CACHE<br />
caches are designed for rapid deployment of emergency medical supplies to a multi-casualty incident,<br />
, \ major catastrophe, or at the Incident Commander's discretion. Each cache weighs approximately three-<br />
1 hundred pounds and consists of six plastic boxes, 12 wooden backboards, and a full complement of<br />
dressing and bandaging material; and each cache is designed to provide basic first-aid and EMT-I level<br />
treatment for 15 to 50 patients. They are transportable inside Department helicopters, heavy apparatus,<br />
plug buggies, and rescue ambulances. The following deployment locations provide for geographic<br />
coverage, potential need, and transport considerations:<br />
, HAZARDOUS MATERIALS CACHE<br />
)V<br />
HAZARADOUS CHEMICAL AGENT EMERGENCY<br />
- For signs and symptoms of Cyanide<br />
: poisoning administer Amyl Nitrite in<br />
conjunction with decontamination.<br />
+ CYANIDE POISONING EXPOSURE:<br />
Special considerations:<br />
Wear PPE and ensure decon procedures are completed<br />
prior to treatment and transpod.<br />
Apply high flow oxygen via mask, observe for deterioration,<br />
monitor respirations and LOC. Cardiac monitor and venous<br />
access. MAKE BASE CONTACT.<br />
Decontaminate if indicated. Administer antidote, if indicated.<br />
d Crush ampule<br />
d Place in a 4x4 Gauze I (tape inside MasWBVM)<br />
d Allow victim to hold antidote and inhale vapor for 60 sec.<br />
(ventilate for 60 seconds)<br />
d Remove ampule 1 ventilate for 15 sec.<br />
d Admin. a new ampule every 2-3 min.<br />
The Medical Supply Trailer<br />
is available for immediate<br />
response to disasters,<br />
MCI's, or at IC discretion.<br />
Can be deployed for<br />
"Special Event" venues.<br />
They can be towed by any<br />
pick-up or larger vehicle with<br />
a tow package.<br />
CONTENTS:<br />
Mark I Kit - 30<br />
Amyl Nitrite - 36<br />
(3 boxes of 12)<br />
Contact MAC: 7-323-722-8073<br />
whencacheboxisopenedandused.<br />
Inventory documentation includes<br />
recording the disaster cache lock<br />
number on the F-903 and F-2. (7-03)<br />
Repeat all steps until IV antidote is available in the ED. Treat cardiac dysrhythmias,<br />
seizures, and hypotension as indicated per LA Co. Treatment Care Guidelines and Ref # 806.<br />
Revised: 0312004 PAGE 1 OF 2
Section 3: Apparatus 1 Equipment<br />
v<br />
HAZARDOUS MATERIALS CACHE<br />
+ MARK I KIT: FOR NERVE AGENTS<br />
Indications for use include poisoning with<br />
organophosphate nerve agents with at least<br />
one sigdsymptom listed:<br />
Respiratory distresslmesty SOB<br />
Muscle twitchinglseizure<br />
Generalized weaknesslparalysis<br />
Copious secretions (SLUDGE)<br />
Hold auto-injector by the plastic clip<br />
with non-dominant hand.<br />
The larger auto-injector is on top<br />
and held at eye level.<br />
With the other handy check your<br />
injection site for any obstacles such<br />
as buttons or objects in the pocketsy<br />
which may interfere with the injections.<br />
PULL THE SMALL GREEN-TIPPED AUTO-INJECTOR (ATROPINE) OUT OF THE CLIP.<br />
REMOVE THE SAFETY CAP (yellow on Atropine; gray on 2PAM-DO NOT TOUCH THE<br />
COLOWD END OF THE INJECTOR after removing the safety cap, since it will inject into<br />
the &ngers or hand if any pressure is applied).<br />
HOLD IT LIKE A PEN OR PENCIL, BETWEEN THE THUMB AND FIRST TWO FINGERS.<br />
POSITION THE GREEN TIP OF THE AUTO-INJECTOR AGAINST THE INJECTION SITE<br />
(ANTEROLATERAL THIGH).<br />
APPLY FIRM, EVEN PRESSURE (not a jabbing motion) TO THE INJECTOR until it pushes<br />
the needle into the thigh or buttock.<br />
HOLD THE INJECTOR FIRMLY IN PLACE FOR AT LEAST 10 SECONDS. Carehlly<br />
remove and then massage the area.<br />
PULL THE BLACK-TIPPED 2-PAM AUTO-INJECTOR OUT OF THE CLIP AND INJECT IN<br />
THE SAME MANNER.<br />
Revised: 0 112003 PAGE 2 OF 2
BASE HOSPITAL HAILING AND CHANNEL ASSIGNMENTS<br />
Beverly (Closed) 1 # 9 5 I 5E 1 4 E 1<br />
, , ,<br />
Cedars-Sinai 1 #94 1 1 B 1 6 B 1<br />
- - - --<br />
Glendale Adventist #I7 8 C * NA<br />
HarborIUCLA #64 4 D 7 D<br />
Henry Mayo Newhall #81 4A 5A<br />
Holy Cross #42 6 A 2A<br />
Huntington Memorial #92 5 F 2A<br />
LACIUSC #28 4 C 6 C<br />
Little Co. of Mary-Torrance 1 #I6 2 D 1<br />
Methodist Hosp. of So. Cal. #49 8 F 3 F<br />
Northridge (NRH) #29 1 A 8A<br />
Pomona Valley # 2 5 7 F 5A<br />
I I<br />
Presbyterian Intercomm. #84 3 E 8 E<br />
Q of A I Hwd. Pres. (Closed 04/04) #75 3 C 7 C<br />
Citrus Valley 1 #I 8 1 4F 1 * NA I<br />
Robert F. Kennedy (Closed W04) 1 #71 I 85 1 3 5 1<br />
St. Francis #53<br />
St. Joseph<br />
St. Mary<br />
Torrance Memorial<br />
I I I<br />
UCLA 1 #59 1 2B -1. 3 B<br />
Revised: 512005<br />
#<strong>35</strong><br />
#24 on 7<br />
#79<br />
PAGE 1 OF 1<br />
1 E<br />
5 A<br />
7 E<br />
3 D<br />
8E<br />
3A<br />
4E<br />
3A
Section 4: Records 1 Documentation<br />
RECORDS AND DOCUMENTATION<br />
THE JOURNAL (F-2) is maintained by each company and is used to record a history of all pertinent<br />
.iformation relative to the daily operation of the command. Entries will appear in a chronological order.<br />
Accuracy, clarity, and completeness of entries are essential on all emergency and non-emergency incidents.<br />
Incidents where unusual circumstances exist (e.g., crime fatalities, patient refusal of treatment and/or<br />
transport, etc.) require a more thorough Journal entry. Members making entries in the Rescue Ambulance<br />
Journal shall adhere to the instructions outlined in the <strong>Manual</strong> of Operation, Volume 5, 917-00.00.<br />
FORMAT<br />
COLOR OF INK: The following entries shall be made in RED ink:<br />
+ Date (centered at the top of each page and the first available line when a new calendar day begins<br />
* Move-up (resulting from an alarm),<br />
+ Alarm information (emergency and non-emergency).<br />
All other entries shall be made in BLUE or BLACK ink.<br />
PLATOON CHANGE ENTRIES:<br />
+ Time, members on duty (include member ID # and assignment),<br />
+ The status of equipment (cell phone, 800 MHz radio, LAPD ASTRO radio), fuel card,<br />
and controlled medications.<br />
INCIDENT ENTRIES:<br />
+ Incident type (e.g., traffic, chest pain, shooting, etc.) and the F-902M sequence number<br />
(entered in the margin).<br />
+ Time of alarm.<br />
Underline "Location of Incident."<br />
1 Patient Information: Patient number (in cases of multiple patients), name, age, sex, chief complaint,<br />
complete vital signs, and treatment rendered.<br />
+ Disposition: Transport destination, time complete, time in quarters.<br />
Documentation may include ride-a-longs, interns, drills, training sessions, equipment loans<br />
and repair, change of rescue staffing during the shift, apparatus placed out of service, injuries,<br />
illness, exposure, patient in custody (include LAPD unit number) or any other occurrences<br />
incidental to the tour of duty.<br />
PHYSICAL SECURITY OF ALL REPORTS, RECORDS, OR DOCUMENTS CONTAINING<br />
PATIENT HEALTH INFORMATION (PHI) SHALL BE SECURED AND NOT LEFT<br />
UNATTENDED ON DESKS OR TABLES AT ANY TIME,<br />
THIS INCLUDES THE JOURNAL (F-2).<br />
Refer to <strong>LAFD</strong> Departmental Bulletin No. 03-1 1<br />
THE HAZARDOUS SUBSTANCE EXPOSURE REPORT (F-3) is generated when a<br />
member has been or is suspected of being exposed to a hazardous substance. An F-3 is available<br />
on the Station Network Staffing System. Instructions are outlined in the <strong>Manual</strong> of Operation,<br />
Volume 5,917-00.00.<br />
STORES REQUISITION (F-80)<br />
1s per Department policy, the F-80 is used to request services or supplies as shown in Volume 4,817<br />
Service and Supplies /Requisition and Delivery. Four copies of the F-80 are initiated by concerned<br />
member. Forward part 1 (white), part 2 (canary) and part 3 (pink) to concerned Department subdivision.<br />
Retain part 4 (goldenrod) until delivery is received. EXCEPTION: Copies of the F-80 Medical Supply<br />
order shall be maintained in the combined file at the fire station for a period of three years.<br />
Revised: 512005<br />
PAGE 1 OF 3
Section 4: Records 1 Documentation<br />
THE RESCUE EQUIPMENT LOAN SLIP (F-215M)<br />
As per Department policy, all <strong>LAFD</strong> equipment is to be clearly marked. Complete a "Rescue<br />
Equipment Loan Slip" (F-215M) in duplicate when equipment is left at a receiving facility.<br />
Clearly document on the F-2J5M the following information:<br />
d The incident date and number d Patient's name (or hospital patient file number)<br />
dHospital arrival time d FD member's name/assignment<br />
A responsible person, from the receiving facility, shall sign and retain a copy of the F-2 15M (loan receipt).<br />
The original copy, containing the initiating member's name and assignment clearly printed, is to be<br />
retained by the rescue ambulance until the equipment is retrieved. A Journal (F-2) entry is also required.<br />
RECORDS AND DOCUMENTATION<br />
THE EMERGENCY MEDICAL SERVICE REPORT (F-902M) is a subpoenable legal, medical,<br />
and billing document that becomes a permanent part of the patient's medical records. First on scene<br />
prehospital care providers shall initiate an F-902M for ALL calls dispatched, except "returned by<br />
radio." Refer to <strong>LAFD</strong>, <strong>Book</strong> 5 (F-902M Instruction <strong>Manual</strong>).<br />
MEDICAL SUPPLIES AND PHARMACEUTICALS procedures are outlined in Departmental<br />
Bulletin No. 01 -1 3. Refer to DHS, Ref. No. 702.2 and Ref. No. 703 for inventory requirements.<br />
ONNEL SHAL.L:<br />
Perform a daily inventory check.<br />
Document entries of the controlled medications (on hand) on the Controlled Medication<br />
Inventory [F-9031 form and in the Journal (F-2), any time there is a change in personnel<br />
or controlled medication.<br />
Following an incident, all units shall replenish their apparatus inventory of medical supplies and<br />
pharmaceuticals immediately upon returning to quarters.<br />
Individual paramedic units are provided with a minimum inventory list of <strong>EMS</strong> supplies to be<br />
maintained onboard and intended to supply a resource for an average 24-hour shift.<br />
However, to meet specific needs, it may be necessary to increase the established minimums<br />
of certain medications andlor supplies.<br />
Each fire station shall order <strong>EMS</strong> supplies and medications (other than controlled medication) on a<br />
monthly basis. Attach the monthly use summary to the F-80 cover sheet and forwarded to Supply and<br />
Maintenance for processing.<br />
Revised: 512005<br />
PAGE 2 OF 3
Section 4: Records 1 Documentation<br />
HE CONTROLLED MEDICATION INVENTORY (F-903) form shall be maintained on the<br />
apparatus until completed. Completed forms shall be retained on file, at the assigned location of<br />
the ALS unit, for a minimum of THREE YEARS. m: A copy of the com~leted Controlled<br />
Medication Inventory form shall be forwarded monthly to the concerned <strong>EMS</strong> Battalion Office .)<br />
A Journal (F-2) entry will be made of the amount of controlled drugs on hand at shift change;<br />
whenever controlled drugs are received and/or delivered; and any time there is a change of responsible<br />
personnel. Notify the <strong>EMS</strong> Battalion Captain between the hours of 0630-0800 of the need for re-supply<br />
of controlled medication and report the current levels of each controlled medication.<br />
When a controlled medication is used, provide the original F-902M BLUE to the <strong>EMS</strong> Battalion<br />
Captain in exchange for the replacement medication. When the medication is issued, the paramedic<br />
receiving the medication will sign in places: The <strong>EMS</strong> Battalion Captain's (controlled medication)<br />
log and the "Receiving Personnel" column of their individual unit copy of the Controlled Medication<br />
Inventory form. (Refer to the Departmental Bulletin No. 0 1 - 13 .)<br />
THE LOS ANGELES FIRE DEPARTMENT SITUATION REPORT (F-904) is used to<br />
facilitate resolution and feedback to inquiries regarding the emergency medical service and/or<br />
other Department related critical issues. The data gathered will assist in identifying areas of<br />
concern relative to performance, patient care issues, and Department training needs. Refer to<br />
<strong>LAFD</strong> Departmental Bulletin No. 01 -06.<br />
THE HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA)<br />
is a federal legislation for the protection and security of personally identifiable health care<br />
information. Members are to take reasonable and prudent measures to secure patients'<br />
protected health information (PHI).<br />
The Department has implemented policies and procedures regarding "Notice of Privacy Practices" (NPP).<br />
Members shall provide each patient with a written NPP utilized by the <strong>LAFD</strong>. Acknowledgement of the<br />
NPP shall be accomplished by obtaining the patient's signature on the back of the F-902M White copy.<br />
Enter NPP given in "Comments" or Transfer of Care" section. If patients are unable to acknowledge<br />
receiving the NPP, the NPP shall be left with the patient at the receiving facility. Exception, when the<br />
patient is unable, due to altered mental status, age, or in police custody. Document the reason why the<br />
patient was unable to sign and that the NPP was provided. (Refer to: <strong>LAFD</strong> Department Bulletin<br />
No. 03-1 1 and <strong>Book</strong> 5.)<br />
Revised: 512005<br />
PAGE 3 OF 3
Section 4: Records 1 Documentation<br />
CALIOSHA and FEDIOSHA NOTIFICATIONS<br />
The senior ranking (<strong>EMS</strong>) member on the rescue ambulance shall make a CallOSHA notification of<br />
serious industrial injuries, illness, or death (other than a traffic accident). If no Department<br />
ambulance has responded, the Incident Commander shall make the notification. If the patient is a<br />
Los Angeles Fire Department member, the station commander (where the member is regularly<br />
assigned) is responsible for making the CallOSHA notification.<br />
A serious injury or illness is any injury or illness that may require admission to a hospital for<br />
24 hours or more (for other than observation), treatment for the loss of any body part, or serious<br />
permanent disfigurement (i.e., serious bums).<br />
The reporting member shall journalize (F-2) the CallOSHA notification including the name of the<br />
person notified and the time of notification.<br />
Revised: 0212003<br />
CALIOSHA<br />
Metro/West/South LA<br />
DowntownIEast LA<br />
Harbor Area<br />
San Fernando Valley Area<br />
Additionally, AS SOON AS POSSIBLE,<br />
(2 13) 576-745 1<br />
(562) 949-7827<br />
(3 10) 5 16-3734<br />
(818) 901-5403<br />
Nx: For Federal Employees contact:<br />
FEDIOSHA (800) 475-4020 or (619) 557-2909<br />
Contact the District Attorney's Office for all incidents involving:<br />
Industrial Related Death or Near Death<br />
1 District Attorney 1<br />
1 Command Post telephone number 1 (2 13) 974-3607 1<br />
The following information will be required for all notifications:<br />
Incident Date and Time<br />
Patient's Name and Age<br />
Patient's Home Address<br />
Patient's Occupation<br />
Name of Employer<br />
Employer's Address<br />
On-site Supervisor's Name and Telephone Number<br />
Incident Address<br />
Patient Destination (Receiving facility)<br />
Extent of Injury<br />
Description of Incident<br />
PAGE 1 OF 1
Section 4: Records 1 Documentation<br />
LEVEL I<br />
Contact limited to merely being in the presence of a person suspected of having<br />
a communicable disease.<br />
1 LEVEL I1 1 Contamination of clothing or equipment by blood and/or body fluids.<br />
LEVEL I11<br />
Exposure of skidmucus or conjunctival membranes to blood and/or body<br />
fluids (e.g., vomitus, urine, feces). This category includes ingestion of<br />
"possible" contaminated food, needle puncture, and human bites.<br />
(Refer to <strong>LAFD</strong>, <strong>Training</strong> Bulletin No. 82.)<br />
For known or suspected exposure to an infectious/cornrnunicable disease, blood and/or body fluids,<br />
or if the member sustains a contaminated needle wound, do the following:<br />
1 1. 1 Immediately cleanse the affected area. 1<br />
1 2. 1 Notify your Station Commander. 1<br />
3.<br />
4.<br />
Notify the appropriate <strong>EMS</strong> Battalion Captain of all "Level 111" exposures.<br />
On the F-902M, check "Inquiry Requested" box and document in the Comments section.<br />
5.<br />
1 6. 1<br />
Complete and forward an F-420; complete an F-225 or F-166A; and D WC Form 1 for all<br />
"Level I1 and 111" exposures.<br />
Ensure a detailed entry in the Journal (F-2) and the member's Personal Record <strong>Book</strong>.<br />
Members shall not seek or receive "first care" until consultation and direction has been<br />
received from the Medical Liaison Unit and/or the <strong>EMS</strong> Battalion Captain.<br />
1<br />
COMMUNICABLE DISEASE EXPOSURE AND NOTIFICATION REPORT (F-420)<br />
The F-420 shall be carried on all <strong>LAFD</strong> apparatus and shall be completed by the concerned<br />
member who may have been exposed to a "Reportable Communicable Disease" and/or received<br />
a contaminated needle wound. The F-420 original copy is given to the hospital.<br />
Reportable Communicable Diseases Include:<br />
+ AIDS<br />
+ Hepatitis<br />
+ Meningitis<br />
+ Syphilis<br />
+ Tuberculosis<br />
Revised: 512005 PAGE 1 OF 2<br />
-
Section 4: Records 1 Documentation<br />
Department equipment which has been contaminated with blood or other body fluids, shall be<br />
decontaminated by members wearing disposable rubber protective gloves as follows:<br />
+ Rescue equipment such as traction splints, backboards, KED boards, blood pressure cuffs,<br />
bag-valve-mask device, airway management instruments, etc., shall be washed with a<br />
disinfectant-detergent solution and hot water then air dried.<br />
+ Delicate electronic equipment such as scope/defibrillators, radios, etc., shall be wiped<br />
down with a 1 : 10 bleachlwater solution (1 part bleach to 10 parts of water) as soon as<br />
possible post incident.<br />
t The rescue ambulance patient area should be scrubbed with a 1 : 10 bleachlwater solution,<br />
rinsed with clear water and air dried.<br />
Needles are to be handled with extreme care. The Department supplies sharp containers<br />
that are to be used for all dirty needle disposal. If self-covering IV catheters are not being<br />
used, the contaminated needles shall be recapped for safety of personnel. Place the cap<br />
on a flat surface and replace the needle in the cap using a "one-handed method."<br />
Note: Do not stick needles in RA seat cushions.<br />
Revised: 121200 1 PAGE 2 OF 2
'<br />
Section 4: Records I Documentation<br />
SUSPECTED CHILD ABUSE I NEGLECT REPORTING GUIDELINES<br />
The primary purpose of the Department of Justice Suspected Child Abuse Report form SS 8572<br />
(DHS, Ref. No 822.2) is to make all agencies aware of possible abuselneglect. In order to<br />
facilitate this process in Los Angeles County, it is recommended that a prompt verbal report be<br />
made to both the Department of Children and Family Services (DCFS) and local law edorcement.<br />
However if the child is in imminent danger, local law enforcement should be notified immediately.<br />
To make a verbal report to DCFS, call the<br />
CHILD ABUSE HOTLINE at: (800) 540- 4000<br />
This should be done as soon as possible. It is recommended that the Child Abuse<br />
Report form be completed prior to making verbal notification. The Suspected Child Abuse1<br />
Neglect report is to be completed according to the instructions on the back of the form<br />
DCFS<br />
3075 Wilshire Blvd.<br />
Los Angeles, California 9001 0<br />
SUSPECTEDELDERAND DEPENDENTADULTABUSE<br />
REPORTING GUIDELINES<br />
Paramedics and EMTs, as health care practitioners, are mandated reporters and have a legal<br />
obligation to report known or suspected elder and dependent adult abuse.<br />
An elder is a person 65 years of age or older. A dependent adult is a person 18-64.years old, who<br />
have physical or mental limitations that restrict their ability to protect their own rights or carry out<br />
normal activities.<br />
DEPARTMENT MEMBERS SHALL MAKE A REPORT WHENEVER:<br />
+ The member observes or has knowledge of an incident that reasonably appears to be abuse, or<br />
+ The member is told of an incident by the victim, or<br />
+ The member reasonably suspects abuse.<br />
Mandated reports of physical abuse, sexual abuse, isolation, abandonment, financial abuse, neglect, and<br />
self-neglect are to be made immediately or as soon as practically possible by telephone. The follow-up<br />
written report must be SENT WITHIN TWO WORKING DAYS to the agency to which the telephone<br />
report was made.<br />
Voluntary reports of other types of abuse, such as mental abuse or abduction, may be made either<br />
!by telephone or by means of the written report mailed or faxed to the appropriate agency.<br />
Revised: 0912003<br />
PAGE 1 OF 3
Section 4: Records I Documentation<br />
SUSPECTEDELDERAND DEPENDENTADULTABUSE<br />
REPORTING GUIDELINES<br />
When the abuse or neglect is suspected to have occurred in a LONG-TERM CARE FACILITY *<br />
report either to the local law enforcement agency or to:<br />
Long Term Care Ombudsman<br />
1527 Fourth Street, Suite 250<br />
Santa Monica, CA 90401<br />
Telephone: (800) 334-WISE (8001 334-9473)<br />
Fax: (3 10) 395-4090<br />
Afler hours telephone: (800) 23 1-4024 (State Crisis Line)<br />
* LONG-TERM CARE FACILITY : Includes, but is not limited to, the following facilities:<br />
1. Any long-term health care facility, such as a nursing facility, a skilled nursing<br />
facility, a congregate living health facility, a licensed respite care facility, or an<br />
intermediate care facility, including habilitative and nursing intermediate care<br />
facilities for the developmentally disabled.<br />
2. A community care facility, such as an adult day care facility, an adult day<br />
support center, an adult residential facility, or a social rehabilitation facility,<br />
whether licensed or unlicensed.<br />
3. A swing bed in an acute care facility, or any extended care facility*<br />
4. A licensed residential care facility for the elderly.<br />
When abuse, neglect, or self-neglect is suspected to have occurred ANYWHERE ELSE,<br />
report either to the local law enforcement agency or to: ,<br />
Los Angeles County Adult Protective Services Centralized Intake Unit<br />
3333 Wilshire Blvd., Suite 400<br />
Los Angeles, CA 90010<br />
Telephone: (888) 202-4-CIU (888) 202-4248<br />
Fax: (213) 738-6485<br />
Afler hours telephone: (877) 4-R-SENIORS (877) 477-3646<br />
TELEPHONE REPORT: Reports are to include as much of the following information, as possible:<br />
1. The name, address, telephone number, and occupation of the person making the report.<br />
2. The name, address, and age of the elder or dependent adult.<br />
3. The names and addresses of family members or any other person responsible for the elder or<br />
dependent adult's care.<br />
4. The nature and extent of the elder or dependent adult's condition.<br />
5. The date and place of the abuse incident.<br />
6. Any other information requested by the receiving agency, including information that led the<br />
reporter to suspect elder or dependent adult abuse.<br />
7. Information about the suspected perpetrator.<br />
Revised: 09D003 PAGE 2 0 ~ 3<br />
'\<br />
J
Section 4: Records I Documentation<br />
SUSPECTED ELDER AND DEPENDENT ADULT ABUSE<br />
REPORTING GUIDELINES<br />
#i WRITTEN REPORT: The Report of Suspected Dependent AdultElder Abuse (Ref. No. 829.1)<br />
must be completed and submitted to the agency initially contacted. Upon completion, immediately<br />
forward the report to the involved <strong>EMS</strong> Battalion Captain. The <strong>EMS</strong> Battalion Captain shall review<br />
and Fax the report to the appropriate agency.<br />
THIS PROCESS SlULL NOT EXCEED TWO (2) . . WORKING DAYS (48 HOURS) OF THE<br />
TELEPHONE REPORK<br />
0<br />
WITHIN 48 HOURS<br />
PARAMEDICS AND EMTS ARE MANDATED REPORTERS. IF YOU SUSPECT ABUSE, NEGLECT, OR<br />
SELF-MGLECT, YOU AFU3 REQUIRED BY STATE LAW TO WPORT IT.<br />
RECORD YOUR OBSERVATIONS OF ELDER DUSE AS YOU DO FOR CHILD ABUSE.<br />
LOS ANGELES COUNTY ELDER ABUSE HOTLINE: (877) 4- R-SENIORS (877) 477-3646<br />
Shortage of food Unkempt, odorous Unemployed<br />
Excessive trash Passive or afraid Substance abuser<br />
Utilities are turned off 1 Bruises, scratches, cuts 1 Mental disorder 1<br />
How reeks of urinelfoul odors 1 Confhed 1 Uncooperative 1<br />
Insect and vermin infestation 1 Calls 91 1 fiequently Speaks for dependent person<br />
Broken whdowslcode<br />
vioIations, etc.<br />
I I<br />
Tells you there is neglect or abuse Aggressive or controlling I<br />
NPES OF ABUSE:<br />
Physical<br />
Sexual<br />
ADULT PROTECTIVE SERVICES (APS) Social Workers investigate reports of suspected abuse<br />
and neglect (24-hours a day in life-threatening situations).<br />
Revised: 912003<br />
Financial<br />
Abandonment<br />
Isolation<br />
Abduction<br />
YOUR OBSERVATIONS HELP WITH THE INVESTIGATION.<br />
ELDERS: 65 years of age or older<br />
DEPENDENT ADULTS: 18-64 year olds who have physical or mental limitations<br />
that restrict their ability to protect their o m rights or carry out normal activities.<br />
PAGE 3 OF 3<br />
Neglect others<br />
Neglect by self<br />
Psychological I<br />
A
Section 4: Records 1 Documentation<br />
COMMUNICATION FAILURE PROTOCOL<br />
Communication Failure Protocols (DHS, Ref. No. 81 0) are followed when paramedics are<br />
unable to establish andor maintain base hospital communications and a delay in treatment may<br />
jeopardize the life of a patient. In those cases the following procedures will be adhered to:<br />
Perform a thorough patient assessment and record all findings on the F-902M.<br />
Initiate the appropriate treatment protocol(s) for the patient's presenting signs1symptoms as<br />
per the EMT-P Communication Failure Protocol Quick Reference.<br />
Transport to a general acute care hospital in accordance with LA County Policies.<br />
Transport as quickly as possible consistent with optimal patient care (may occur at any point<br />
in the standing orders).<br />
Make vigorous attempts to establisldmaintain voice contact with physician or MICN while en<br />
route to the receiving hospital.<br />
IMMEDIATELY make a VERBAL REPORT to the on-duty emergency room physician or<br />
MICN at the assigned base hospital.<br />
Complete the ALS Communication Failure Report Form as described in DHS, Ref. No. 8 10.<br />
Non compliance with this policy may be construed as hctioning outside the supervision<br />
(scope) of medical control under the Health and Sdety Code l798.2OO(c)(lO).<br />
WRITTEN REPORT : Within 24 hours of the incident, involved paramedics shall complete<br />
Section A and forward the form to the Base Hospital Medical Director at the assigned base hospital. y, , ><br />
Revised: 912003<br />
PAGE 1 OF 1<br />
WITHIN 24 HOURS
/<br />
Section 4: Records I Documentation<br />
COMMUNICATION FAILURE PROTOCOL<br />
Communication Failure Protocols (DHS, Ref. No. 81 0) are followed when paramedics are<br />
unable to establish andor maintain base hospital communications and a delay in treatment may<br />
jeopardize the life of a patient. In those cases the following procedures will be adhered to:<br />
1. Pedorm a thorough patient assessment and record all findings on the F-902M.<br />
2. Initiate the appropriate treatment protocol(s) for the patient's presenting signs/symptoms as<br />
per the EMT-P Communication Failure Protocol Quick Reference.<br />
3. Transport to a general acute care hospital in accordance with LA County Policies.<br />
4. Transport as quickly as possible consistent with optimal patient care (may occur at any point<br />
in the standing orders).<br />
5. Make vigorous attempts to establishlmaintain voice contact with physician or MICN while en<br />
route to the receiving hospital.<br />
6. IMMEDIATELY make a VERBAL REPORT to the on-duty emergency room physician or<br />
MICN at the assigned base hospital.<br />
7. Complete the ALS Communication Failure Report Form as described in DHS, Ref. No. 8 10.<br />
8. Non compliance with this policy may be construed as hctioning outside the supervision<br />
(scope) of medical control under the Health and Safety Code 1798.200(~)(10).<br />
\ WRITTEN REPORT : Within 24 hours of the incident, involved paramedics shall complete<br />
-4 Section A and forward the form to the Base Hospital Medical Director at the assigned base hospital.<br />
Revised: I212001<br />
PAGE 1 OF 1<br />
WITHIN 24 HOURS
Section 4: Records 1 Documentation<br />
, Mnemonics (memory joggers) are effective tools used to assist <strong>EMS</strong> personnel in conducting<br />
more thorough assessments. The following are a few examples to assist with patient assessments.<br />
1 SECONDARY (FOCUSED) 'SURVEY 1 BURN INJURY I<br />
(SAMPLE / 3 "T's")<br />
S -Signs/Symptoms<br />
A -Allergies<br />
M -Medications<br />
P -Past medical history<br />
L -Last oral intake.<br />
E -Event preceding.<br />
T -Tags (Medical)<br />
T -Tracks<br />
T -Trauma<br />
(DCAPP-BTLS)<br />
D -Deformities<br />
C -Contusions<br />
A -Abrasions<br />
P -Penetration<br />
P -Paradoxical movement<br />
1 NEUROLOGICAL I 1 LEVEL OF RESPONSIVENESS 1<br />
-<br />
-Depth of coma<br />
E -Eyes<br />
R -Respiratory status<br />
M -Motor response<br />
INJURED EXTREMITY (Distal to Injury)<br />
(PMS)<br />
BONY AREA EXAM<br />
Revised: 121200 1 PAGE 1 OF 2<br />
(AVPU)<br />
A -Alert<br />
V -Responds to Verbal stimulus<br />
P -Responds to Painful stimulus<br />
U -Unresponsive<br />
1 TO ELICIT PERSONAL HISTORY I<br />
W -Weight<br />
H -History of medical problem<br />
A -Age, allergies<br />
M -Under D's care<br />
-- -<br />
1 SIGNS OF A TENSION PNEUMOTHORAX 1<br />
(PUNT)<br />
P -Progressive Dyspnea<br />
U -Unilateral Breath Sounds<br />
N -Neck Vein Distension<br />
T -Tracheal Deviation
Section 4: Records 1 Documentation<br />
CAUSES OF ASYSTOLE<br />
(4-H Police Department)<br />
H -Hypoxia<br />
H -Hyperkalemia<br />
H -Hypokalemia<br />
H -Hypotherrnia<br />
P -Pre-existing Acidosis<br />
D -Drug Overdose<br />
NARCOTICS INHIBITED BY NARCAN h<br />
Many Doctors Practice Tender Loving<br />
Care Many Hours Daily<br />
1 POSSIBLE CAUSES OF PEA<br />
(MATCH (X4) ED)<br />
M -Myocardial Infarction (massive acute)<br />
A -Acidosis<br />
T -Tension Pneurnothorax<br />
C -Cardiac Tamponade<br />
H -Hypoxia, Hypovolemia,<br />
Hyperkalemia, Hypotherrnia<br />
E -Pulmonary Embolus<br />
D -Drug Overdose<br />
1 COMMON CAUSES OF<br />
PEDIATRIC SEIZURES<br />
F -Fever<br />
H -HeadTrauma<br />
E -Epilepsy<br />
(medically diagnosed)<br />
L -Low blood sugar1<br />
chemical disturbances<br />
P -Poison/overdose<br />
Revised: 912001 PAGE 2 OF 2<br />
1 ET DRUG ADMINISTRATION 1<br />
-<br />
-<br />
DRUG CHECK PRIOR TO<br />
ADMINISTRATION<br />
(DICCE)<br />
D -Drug/Dose<br />
I -1ntegritylIndications<br />
C -Clarity<br />
C -Concentration/Contraindications<br />
E -Expiration date<br />
1 ABDOMINALPAIN 1<br />
(DR. GERM)<br />
D -Distention<br />
R -Rigidity<br />
G -Guarding<br />
E -Ecchymosis<br />
R -Referred Pain<br />
M -Masses<br />
ASSESSMENT TOOL<br />
(SOAP)<br />
NEUROVASCULAR COMPROMISE<br />
("5 P's")<br />
Pain Where, what's causing it?<br />
Pulse Is there a distal pulse in the injured extremity?<br />
Paresthesia Any abnormal sensation at the site?<br />
Paralysis Indicates peripheral nerve damage or<br />
circulatory impairment.<br />
Pallor Check color, temperature, and capillary refill.
Abdomen ABD<br />
Abortion AB<br />
Apical Pulse<br />
Abrasion<br />
-<br />
Accelerated Junctional Rhythm<br />
Section 4: Records 1 Documentation<br />
Anterior 1 ANT<br />
ABR Appointment ~ P T<br />
-- --<br />
AJ R Approximately I APPRO:<br />
Accelerated Ventricular Rhythm AVR Arterial Blood Gases<br />
Accident ACC<br />
Acquired Immune Deficiency<br />
Syndrome<br />
Acute Life Threatening Event ALTE<br />
Acute Myocardial Infarction<br />
Artery<br />
AIDS As Needed<br />
As Soon as Possible ASAP<br />
Aspirin 1 ASA<br />
Adult Respiratory Distress Syndrome ARDS Assault 1 AST<br />
Advanced Health Care Directive<br />
Advanced Life Support<br />
AHCD<br />
ALS<br />
Advised ADV<br />
After Care Instructions<br />
Assaulted with a Deadly Weapon 1 ADW<br />
Asystole ASY<br />
At Once STAT<br />
ACI Atrial Fibrillation AF I<br />
After I Past I Post<br />
Against Medical Advice<br />
Agonal<br />
AMA<br />
AGO<br />
Atrial Flutter<br />
Atrioventricular<br />
Attempted Suicide<br />
AFL<br />
k-<br />
Airway 1 Breathing I Circulation ABC Auscultation<br />
Alcohol On Breath AOB<br />
- -<br />
Alert & Oriented times 3 Parameters<br />
(Purpose, Time, Place)<br />
Allergies ALG<br />
Altered<br />
Altered Level of Consciousness<br />
Ambulance / Ambulatory<br />
Amount<br />
ALT<br />
Automated External Defibrillator<br />
Axillary<br />
Backboard BBD<br />
Bag of Waters BOW<br />
ALOC Bag-Valve-Mask BVM<br />
AMB<br />
AMT<br />
Ampule AMP Before<br />
Antecu bital<br />
Revised: 512005<br />
PAGE 1 OF 9<br />
Base Hospital Medical Director BHMD<br />
Basic Life Support 1 BLS
Section 4: Records / Documentation<br />
Carbon Dioxide<br />
Cardioversion<br />
Catheter<br />
Centigrade / Celsius<br />
Central Nervous System<br />
Cerebrospinal Fluid<br />
Cerebrovascular Accident<br />
Certified Nurse Assistant<br />
Cervical Spine<br />
Revised: 512005<br />
CAR<br />
CATH<br />
C<br />
CNS<br />
CSF<br />
CVA<br />
CNA<br />
C-SP<br />
Cervical Vertebrae<br />
Chest Pain<br />
Chief Complaint<br />
-<br />
Chronic Obstructive Pulmonary<br />
Disease<br />
-<br />
---.-<br />
C-1, C-2,<br />
etc.<br />
COPD<br />
Chronic Renal Failure<br />
-<br />
CRF<br />
Circulation, Sensation, Movement<br />
-<br />
Clean and Dress<br />
-<br />
CSM<br />
Clear<br />
-<br />
CLR<br />
Communication Failure Protocol<br />
-<br />
Complains Of<br />
CFP<br />
Complete Blood Count CBC<br />
Complete Heart Block<br />
Congestive Heart Failure<br />
Contact Not Attempted<br />
Contagious Disease<br />
Contusion<br />
Coronary Artery Bypass Surgery<br />
Coronary Artery Disease<br />
Coronary Care Unit<br />
Corrected To<br />
Cubic Centimeter<br />
Date of Birth<br />
Dead on Arrival<br />
CHB<br />
CHF<br />
CNA<br />
CONT<br />
CABS<br />
CAD<br />
ccu<br />
C/T<br />
DOB<br />
DOA<br />
Decrease DECR<br />
Defibrillation DEF
--<br />
Section 4: Records I Documentation<br />
ABBREVIATIONS<br />
Delirium Tremens 1 DT9s Equal and Reactive<br />
E&R<br />
Dextrose 5 Percent in Water<br />
Esophageal Gastric Tube Airway EGTA<br />
Diabetes Mellitus<br />
Esophageal Obturator Airway EOA<br />
Diabetic Ketoacidosis<br />
Estimated<br />
EST<br />
Diagnosis<br />
DX Estimated Blood Loss<br />
Dilation and Curettage<br />
D&C Estimated Time of Arrival ,*<br />
Discontinue<br />
Ethyl Alcohol<br />
ETOH<br />
Distal<br />
DIST Evaluation<br />
EVAL<br />
Do-Not-Resuscitate<br />
DNR Examination<br />
EXAM<br />
Drop<br />
gtt Expected Date of Confinement EDC<br />
Dry Sterile Dressing<br />
DSD<br />
Expected Date of Delivery 1 EDD<br />
Duodenal Ulcer<br />
Expiratory<br />
EXP<br />
Dyspnea on Exertion<br />
External<br />
EXT<br />
Each, Every<br />
Eyes, Ears, Nose, and Throat EENT<br />
Electrocardiogram<br />
1 ECG (EKG]<br />
Fahrenheit<br />
F<br />
Electroencephalogram<br />
EEG<br />
Family History<br />
F H<br />
Emergency Department<br />
ED<br />
Fetal Heart Tones<br />
FHT<br />
Emergency Department Approved<br />
EDAP<br />
for Pediatrics<br />
Fever of Unknown Origin<br />
FUO<br />
Emergency Medical Service (System) <strong>EMS</strong> Fixed and Dilated<br />
F&D<br />
Emergency Medical Technician-<br />
Fluid<br />
Advanced Airway<br />
Emergency Medical Technician<br />
Emergency Medical Technician-Paramedic EMT-P<br />
Follow Up<br />
Emergency Room<br />
Foreign Body<br />
FB<br />
Esophageal Tracheal Combitube<br />
Four Times a Day<br />
QID<br />
Endotracheal Tube<br />
ET<br />
Fracture<br />
FX<br />
Revised: 512005<br />
PAGE 3 OF 9
Section 4: Records 1 Documentation<br />
ABBREVIATIONS<br />
Frequent FREQ Hypertension 1 HTN<br />
Gallbladder GB Hyperventilation I<br />
Gastroenteritis 1 GE 1 ldioventricular Rhythm<br />
Gastrointestinal<br />
Genitourinary<br />
Glasgow Coma Scale GCS<br />
Immediate Danger to Life & Health IDLH<br />
Increase INCR<br />
Inhaled I IN<br />
Grain Injury 1 INJ<br />
Gram ~"-"<br />
Gravida G<br />
Gunshot Wound 1 GSW<br />
Has Been Drinking 1 HBD<br />
Headache<br />
Inspiration INSP<br />
Insulin Dependent Diabetes IDD<br />
--- -<br />
Intake and Output<br />
Intensive Care Unit ICU<br />
International Unit I U<br />
Intramuscular IM<br />
Heart Block<br />
Heart Block- (1st 1 2nd 1 3rd )<br />
Intrauterine Pregnancy IUP<br />
Degree Intravenous IV<br />
Heart Rate I Hour HR<br />
I<br />
Intravenous Piggyback IVPB<br />
Heart Sounds 1 Intravenous Push IVP<br />
Height<br />
-<br />
Hemorrhage HEM0<br />
History HX<br />
History of Present Illness 1 HPI I<br />
Hospital<br />
Hospital Emergency<br />
Administrative Radio<br />
Hospital Emergency<br />
Response Team<br />
1 HOSP 1<br />
HEAR<br />
Human Immunodeficiency Virus 1 HIV I<br />
Revised: 512005<br />
HERT<br />
PAGE 4 OF 9<br />
Involuntary INVOL<br />
Irrigation<br />
Joint JT<br />
Jugular Vein Distention<br />
Junctional Rhythm<br />
Keep Vein Open<br />
Kilogram<br />
Knock Out<br />
-- -<br />
Laboratory<br />
JVD<br />
JR<br />
KVO<br />
kg<br />
KO<br />
1 LAB
Laceration<br />
Large<br />
Middle<br />
Midline<br />
Section 4: Records / Documentation<br />
-- - -<br />
Last Normal Menstrual Period LNMP Military Anti-Shock Trousers<br />
Lateral<br />
I<br />
LAT<br />
@<br />
Milliequivalent<br />
Left / Liter Milligram<br />
m!3<br />
Left Bundle Branch Block LBBB<br />
Milliliter<br />
Left Lower Extremity 1 LLE Minimal Blood Loss<br />
Left Lower Quadrant<br />
Left Upper Extremity 1 LUE<br />
Left Upper Quadrant<br />
Level / Loss of Consciousness<br />
Licensed Vocational Nurse<br />
Liquid<br />
LLQ<br />
LUQ<br />
LOC<br />
Liters per Minute LIMIN<br />
Long Backboard<br />
Lumbar Spine<br />
Lumbar Vertebrae L-I , L-2, etc.<br />
Meconium<br />
Medical<br />
Medical Doctor<br />
Medications<br />
Mental Retardation<br />
--- --<br />
Mentally Disordered Person MDP<br />
Microdrop<br />
Midclavicular Line<br />
Revised: 512005<br />
MCIGlT<br />
MCL<br />
PAGE 5 OF 9<br />
Mobile lntensive Care Nurse<br />
Mobile lntensive Care Unit<br />
Moderate<br />
Month<br />
Morning<br />
Morphine Sulfate /Multiple<br />
Sclerosis<br />
Most Accessible Receiving (facility)<br />
Motor Vehicle Accident<br />
Motorcycie Accident<br />
Moves All Extremities<br />
Multifocal<br />
Multiple<br />
Myocardial Infarction<br />
Nasal Cannula<br />
Nasogastric Tube<br />
Nasopharyngeal<br />
Nausea 1 Vomiting 1 Diarrhea<br />
Negative<br />
MAST 1<br />
mL<br />
MBL<br />
MICN<br />
MICU<br />
MOD<br />
MO<br />
AM<br />
MAR '<br />
MVA
Neonatal Intensive Care Unit NICU<br />
Newborn 1 NB<br />
Nitroglycerine<br />
No Apparent Distress<br />
No Known Allergies<br />
Non-breathing, Unconscious, Pulseless, Nupu<br />
Unresponsive<br />
Normal I N<br />
Normal Saline 1 NS<br />
Normal Sinus Rhythm 1 NSR<br />
Normal Spontaneous Vaginal<br />
Delivery<br />
Not Applicable I Not Available NIA<br />
Nothing by Mouth 1 NPO<br />
Notice of Privacy Practices 1 NPP<br />
Object I Objective 1 OBJ<br />
Obstetrical I Gynecological 1 OBIGYN<br />
Occasional OCC<br />
Organic Brain Syndrome OBS<br />
Oropharyngeal OP<br />
Ounce OZ<br />
Overdose OD<br />
Oxygen 02<br />
Pacemaker Rhythm PMR<br />
Palpation 1 PALP<br />
Para I Pulse P<br />
I<br />
Paroxysmal Supraventricular Tachycardia<br />
Partial Pressure of Carbon Dioxide<br />
Partial Pressure of Oxygen<br />
Past Medical History<br />
Patient 1 Physical Therapy<br />
Pedal Edema<br />
Pediatric<br />
Pediatric Medical Center<br />
Pediatric Trauma Center<br />
PSVT<br />
PO2<br />
PMH<br />
PED ED<br />
PED<br />
PMC<br />
PTC<br />
Pelvic Inflammatory Disease PID<br />
Penicillin<br />
Percussion<br />
-<br />
PCN<br />
PERC<br />
Per Rectal PR<br />
Personal Protective Equipment<br />
Possible<br />
PPE<br />
POSS<br />
Posterior POST<br />
Postoperative<br />
Postpartum<br />
Paramedic I Afternoon 1 Evening PM Private<br />
Prehospital Care Coordinator<br />
Premature Atrial Contraction<br />
Premature Junctional Contraction<br />
Premature Ventricular Contraction<br />
POST OP<br />
PCC<br />
PAC<br />
PJC<br />
PVC<br />
Prenatal Care PNC<br />
Prior To Arrival<br />
Paroxysmal Nocturnal Dyspnea PND Private Medical Doctor PMD<br />
Revised: 512005<br />
PTA<br />
PVT
[ Protocol PRO<br />
ABBREVIATIONS<br />
Proximal PROX<br />
Public Access Defibrillator PAD<br />
Pulmonary Edema PUL ED<br />
Pulmonary Embolus<br />
Pulseless Electrical Activity<br />
PEA<br />
Section 4: Records 1 Documentation<br />
Sacral Spine S-S P<br />
Saline Lock I Sublingual SL<br />
seizure -ffD<br />
----.....-- --<br />
Sexually Transmitted Disease<br />
Short Backboard SBB<br />
Shortness of Breath 1 SOB<br />
Pulses 1 Movement 1 Sensation PMS<br />
Pupils Equal and Reactive to<br />
Light<br />
Radial<br />
Range of Motion<br />
Red Blood Cell<br />
Refused Medical Assistance<br />
PERL<br />
RAD<br />
ROM<br />
RBC<br />
RMA<br />
Sinus Arrhythmia<br />
Sinus Bradycardia<br />
Sinus Tachycardia<br />
small<br />
Small Bowel Obstruction -+<br />
SA<br />
SB<br />
1 SBO<br />
Registered Nurse<br />
Resident Of 1 Rule Out<br />
Respiration<br />
Respiration Rate<br />
wo<br />
RESP<br />
solution 1 SOL<br />
Specialty Center<br />
Standing <strong>Field</strong> Treatment Protocol<br />
Stab Wound<br />
Returned by Radio RxR Subcutaneous<br />
Revised Trauma Score<br />
Rheumatic Heart Disease<br />
Right<br />
RTS<br />
RHD<br />
Right Bundle Branch Block RBBB<br />
Right Lower Extremity<br />
Right Lower Quadrant<br />
Right Upper Extremity<br />
Right Upper Quadrant<br />
RLE<br />
RLQ<br />
RUE<br />
RUQ<br />
Revised: 512005 PAGE 7 OF 9<br />
Subjective<br />
Substernal Chest Pain<br />
Sudden Infant Death Syndrome<br />
Suppository<br />
SQ<br />
SUBJ<br />
SSCP<br />
SIDS<br />
SUPP<br />
-
Section 4: Records I Documentation<br />
--<br />
Supraventricular Tachycardia SVT Unconscious<br />
UNC<br />
Symptom<br />
Syrup<br />
Tablet<br />
Tachycardia<br />
Temperature<br />
Tender Loving Care<br />
Tetanus Toxoid<br />
SYR<br />
TAB<br />
TACH<br />
Thoracic Spine T-SP<br />
Thoracic Vertebrae<br />
Three Times a Day<br />
Times / By<br />
To Keep Open<br />
(Total) Body Surface Area<br />
Traffic Accident<br />
Traffic Collision<br />
Transient Ischemic Attack<br />
Transport<br />
Treatment<br />
Tuberculosis<br />
Twice a Day<br />
Tylenol<br />
Unable to Locate<br />
Revised: 512005<br />
T<br />
Unifocal<br />
Upon Our Arrival<br />
Upper Gastrointestinal<br />
Upper Respiratory Infection<br />
Urinary Tract Infection<br />
TLC Venereal Disease<br />
T-1. T-2. etc.<br />
TID<br />
x<br />
TKO<br />
Ventricular Fibrillation<br />
Ventricular Tachycardia<br />
Verbal Order<br />
Vital Signs / Versus<br />
Volume<br />
Water<br />
(T) BSA Watt-Second<br />
TIA<br />
TRANS<br />
Weak<br />
Weight<br />
---<br />
Well Developed / Well Nourished<br />
White Blood Cell<br />
Wide Open<br />
With<br />
---<br />
UOA<br />
UGI<br />
URI<br />
UTI<br />
VOL<br />
H20<br />
WDIWN<br />
WBC<br />
BID Within Normal Limits WNL<br />
TY L<br />
UTL<br />
Without<br />
YearIOld Female<br />
YearIOld Male
0<br />
Year I Old Male<br />
Decrease I Negative 1 Minus 1 -<br />
Equals<br />
Female<br />
Greater Than<br />
Increase I Positive I Plus<br />
c<br />
.No<br />
Less Than<br />
Change<br />
Number<br />
Percent 1 %<br />
Secondary To<br />
Revised: 512005 PAGE 9 OF 9<br />
Section 4: Records 1 Documentation
Section 4: Records & Documentation<br />
BIBLIOGRAPHY<br />
M-S Unit Inventory 1 <strong>LAFD</strong> <strong>Book</strong> 33 1 Ref. No. 702<br />
'advance Health Care Directives (AHCD)<br />
<strong>EMS</strong> UPDATE 2003<br />
UTE (Apparent Life Threatening Event)<br />
<strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 808.1<br />
'aMA/Patient Refusal of Treatment or Transport<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
Dept. Bulletin<br />
Ref. No. 834<br />
No. 01-10<br />
'application of Patient Restraints<br />
<strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 838<br />
'aspirin Administration to Chest Pain Patients<br />
Dept. Bulletin No. 99-20<br />
'assessment of Altered Level of Consciousness<br />
<strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 809<br />
Glasqow Coma Scale (GCS)<br />
<strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 809<br />
Revised Trauma Score (RTS)<br />
<strong>EMS</strong> UPDATE 1999<br />
ksessment Unit Inventow<br />
apparatus Maintenance<br />
1 I<br />
1<br />
<strong>LAFD</strong> <strong>Book</strong> 33 1 Ref. No. 703<br />
I<br />
<strong>LAFD</strong> <strong>Book</strong> 8 1 Module 4<br />
1 I<br />
'automated External Defibrillators<br />
Base Hospital ContactlTransportation Criteria<br />
Body Armor Vests<br />
Bomb Scene Incidents<br />
Burn Patient Destination<br />
CAUOSHA and FEDIOSHA Notifications<br />
Cellular Telephone Procedures 1 Dept. Bulletin 1 No. 98-17<br />
I I<br />
Communicable Disease Decontamination<br />
Communicable Disease Exposure and Notification (F-420)<br />
Source Patient HIV Status<br />
Source Patient HIV Status Flowchart<br />
Petition for Order to Test Blood (Accused)<br />
Infectious Disease Protocols<br />
Communication Failure Protocol<br />
Conditionally Available (CAV) & Non-Available (NAV)<br />
Decompression EmergenciesIPatient Destination<br />
Determination I Pronouncement of Death in the <strong>Field</strong><br />
<strong>Training</strong> Bulletin No. 64<br />
Dept. Bulletin No.98-14, 99-11, 99-14<br />
<strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 808<br />
<strong>Training</strong> Bulletin No. 81<br />
<strong>Training</strong> Bulletin No. 75<br />
<strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 512<br />
Dept. Bulletin No. 99-09<br />
MOP, Vol. 1 2/1-4234 & 2/1-56.01<br />
Dept. Bulletin No. 96.29<br />
<strong>LAFD</strong> <strong>Book</strong> 75<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
<strong>Training</strong> Bulletin<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
Dept. Bulletin<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
<strong>Training</strong> Bulletin<br />
Ref. No. 836.2<br />
Ref. No. 836<br />
Ref. No. 836.1<br />
Ref. No. 836.3<br />
No. 82<br />
Ref. No. 810<br />
No. 98-20<br />
Ref. No. 518<br />
Ref. No. 814<br />
No. 100<br />
Disposing of Medical Waste 1 MOP, Vol. 1 1 211-84.60<br />
I I<br />
<strong>EMS</strong> Report Short Form for Multi Casualty Incidents (MCI)<br />
<strong>EMS</strong> UPDATES 1996-1997,1999,2000,2001,2002,2003<br />
<strong>EMS</strong> Safety Eye Shield and Face Masks<br />
EMT-1 Scope of Practice<br />
Revised: 512005<br />
PAGE 1 OF 3<br />
Dept. Bulletin<br />
Dept. Bulletin<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
No. 03-19<br />
No. 92-7<br />
Ref. No. 802
BIBLIOGRAPHY<br />
Section 4: Records 1 Documentation<br />
Eaui~ment Retrieval Procedure<br />
Firelighter Burn Injuries<br />
Health Insurance Portability and Accountability Act (HIPAA)<br />
1<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
Dept. Bulletin<br />
Dept. Bulletin<br />
I Ref. No. 708<br />
I No. 99-09<br />
1 No. 03-1 1<br />
Honoring Prehospital Do-Not-Resuscitate (DNR) Orders <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 815<br />
Hospital Directory <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 501<br />
Hospitals Requesting Diversion of ALS Units (Guidelines) <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 503<br />
Hospital Status Information via Mobile Data Terminals (MDTs) Dept. Bulletin No. 98-21<br />
Infectious Disease Protocols<br />
<strong>LAFD</strong> EMT Re-certification <strong>Training</strong> Course<br />
<strong>Training</strong> Bulletin No. 82<br />
Lifepak 12 Cardiac MonitorIDelibrillator Use Dept. Bulletin No. 0506<br />
Management of Multiple Victim Incidents <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 519<br />
Medical Guidelines (DHS) <strong>LAFD</strong> <strong>Book</strong> 32<br />
Medical Supplies and Pharmaceuticals Dept. Bulletin No. 04-08<br />
Minimum Equipment Used on Incidents <strong>LAFD</strong> <strong>Book</strong> 63 Pg. 54-55<br />
Multi-Casualty Incident Procedures <strong>LAFD</strong> <strong>Book</strong> 70<br />
Multi-Casualty Medical Supply Cache<br />
Notice of Privacy Practices (NPP) 1<br />
Dept. Bulletin<br />
Dept. Bulletin<br />
Dept. Bulletin<br />
No. 89-8<br />
No. 04-03<br />
I No. 03-1 1<br />
Paramedic Emergency Care, Third Edition, Brady,<br />
1997 Paramedic <strong>Training</strong> Institute, January 1997<br />
Syllabus 1 Syllabus 6<br />
Prehospital Emergency Care, 6th Edition, Brady, 2000<br />
Patient Destination Guidelines <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 502<br />
Decompression Emergencies <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 518<br />
Sexual Assault Patient Destination <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 508<br />
Pediatric Patient Destination <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 510<br />
Perinatal Patient Destination <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 51 1<br />
Patient Resolution Guide (PRG) <strong>Training</strong> Bulletin No. 18<br />
Patient Transportation Policy 1 Dept. Bulletin 1 No. 04-22<br />
I ,<br />
Police Custody (Patient Care Policy for Patients in Custody) 1 Dept. Bulletin 1 No. 04-17<br />
I ,<br />
Reporting of AbuseINeglect-Child, Elder, Dependent Adult<br />
Dept. Bulletin No. 92-5<br />
<strong>LAFD</strong> <strong>Book</strong> 33 No. 822,829<br />
Rescue Ambulance Preventative Maintenance 1 MOP, Vol. 5 !<br />
,<br />
Rescue Equipment Loan Slip (F-215M) MOP, Vol. 5 917-00.00 (1 -89)<br />
Safety Precautions While Using RA Gurneys<br />
Service Areas<br />
Situation Report (F-904)<br />
'<br />
1 I<br />
1<br />
Dept. Bulletin<br />
Dept. Bulletin<br />
Dept. Bulletin<br />
No. 96-1 1<br />
1 No. 94-21<br />
I<br />
1 No. 01-06<br />
Spinal Immobilization<br />
I I<br />
<strong>Training</strong> Bulletin No. 87<br />
START (Simple Triage and Rapid Treatment) <strong>LAFD</strong> <strong>Book</strong> 70<br />
Suspected Child Abuse Reporting Guidelines <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 822<br />
Suspected Elder and Dependent Adult Abuse Reportinq <strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 829<br />
Revised: 512005<br />
PAGE 2 OF 3
BIBLIOGRAPHY<br />
Section 4: Records 1 Documentation<br />
Towing Apparatus Procedures 1 MOP, Vol. 4 p~/3-44.01<br />
Trauma Catchment Areas 1 <strong>LAFD</strong> <strong>Book</strong> 33 I Ref. No. 504<br />
1<br />
I I<br />
Trauma Hospital Temp. ClosureIDiversion<br />
<strong>LAFD</strong> <strong>Book</strong> 33 Ref. No. 505<br />
of Trauma Patients<br />
Trauma Triage<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
Transporting Patients in Custody 1 Dept. Bulletin 1 No. 93-12<br />
I I<br />
Trans. Pre-paid Health Plan Members to Kaiser Facilities<br />
Treatment 1 Transport of Minors<br />
Trial Program-Emergency Medical Service Areas for California<br />
& Good Samaritan Hospitals<br />
Trial Program, Hospital Transportation Service Areas<br />
Dept. Bulletin<br />
<strong>LAFD</strong> <strong>Book</strong> 33<br />
Dept,<br />
Ref. No. 506<br />
Ref. No. 838<br />
No. 03-12<br />
Ref. No. 832<br />
V-Vac Hand Powered Suction Unit 1 <strong>Training</strong> Bulletin 1 No. 72<br />
I I<br />
Variable Staffed BLS Ambulance Program 1 Dept. Bulletin 1 No. 04-22<br />
Revised: 512005<br />
PAGE 3 OF 3<br />
Dept. Bulletin<br />
No. 92-3<br />
No. 90-17
I<br />
Los Angeles Fire Department<br />
<strong>EMS</strong> FIELD MANUAL<br />
<strong>Book</strong> <strong>35</strong><br />
Record of Revisions<br />
Keep your manual current. After receiving and filing additional or revised pages, initial and date<br />
the appropriate columns following the change number.<br />
No blanks should appear between initialed blocks. If you have failed to record a revision notice or<br />
have not received one, notify the Quality Improvement Section at (21 3) 485-71 53.<br />
CHANGE INITIAL DATE CHANGE INITIAL DATE<br />
NOTICE # NOTICE #<br />
*** Revisions incorporated into manual PAGE I OF 2 Revised: 512005