90 – Pneumonias of horses Glanders (farcy, malleus)
90 – Pneumonias of horses Glanders (farcy, malleus)
90 – Pneumonias of horses Glanders (farcy, malleus)
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>90</strong> <strong>–</strong> <strong>Pneumonias</strong> <strong>of</strong> <strong>horses</strong><br />
<strong>Glanders</strong> (<strong>farcy</strong>, <strong>malleus</strong>)<br />
2010.<br />
(Broncho)interstitial pneumonia<br />
• Equine influenza<br />
<strong>–</strong> Type A virus, two subtypes<br />
• A/equi/2 <strong>–</strong> H3N8; A/equi/1 <strong>–</strong> H7N7<br />
<strong>–</strong> Clinical signs<br />
• Coughing, serous to purulent oculonasal discharge,<br />
fever, weakness<br />
• Rarely sytemic involvement and death<br />
<strong>–</strong> Lesions<br />
• Hyperemia, focal erosions in the upper respiratory tract<br />
• Bronchointerstitial pneumonia<br />
<strong>–</strong> edema<br />
<strong>–</strong> necrosis <strong>of</strong> bronchiolar epithelium<br />
<strong>–</strong> secondary bacterial pneumonia<br />
(Broncho)interstitial pneumonia<br />
• Equine herpesviruses (EHV-4, EHV-1)<br />
<strong>–</strong> Mild upper respiratory signs<br />
<strong>–</strong> Secondary bacterial bronchopneumonia<br />
<strong>–</strong> Systemic lesions in neonates!<br />
• Rhinovirus, reovirus, equine arteritis virus, adenovirus<br />
<strong>–</strong> similar clinical signs and lesions<br />
<strong>–</strong> predisposing factors for heaves (COPD)?<br />
• African horse sickness<br />
<strong>–</strong> severe edema, vascular damage (Reoviridae, Orbivirus)<br />
• Hendra virus<br />
<strong>–</strong> syntitial giant cells (Paramyxoviridae, Morbillivirus)<br />
• Clamydophila psittaci<br />
• Idiopathic proliferative interstitial pneumonia<br />
<strong>–</strong> sequel: pulmonary fibrosis, toxicosis / viral infection?<br />
Topics <strong>–</strong> morphological categorization<br />
• (Broncho)interstitial pneumonia<br />
<strong>–</strong> equine influenza, EHV-1, EHV-4 infection<br />
• Bronchopneumonia<br />
<strong>–</strong> catarrhal-purulent bronchopneumonia<br />
<strong>–</strong> fibrinous bronchopneumonia, pleuropneumonia<br />
• Streptococcus equi ssp. equi, ~ zooepidemicus; Bordetella<br />
bronchiseptica, Klebsiella pneumoniae, Staphylococcus sp.<br />
<strong>–</strong> necrotic/gangraneous bronchopneumonia<br />
• aspiration pneumonia<br />
• Focal/multifocal pneumonia<br />
<strong>–</strong> septic thromboembolism related pneumonia<br />
• (Pyo)granulomatous pneumonia<br />
<strong>–</strong> Rhodococcus equi infection<br />
<strong>–</strong> glanders (Burkholderia mallei infection)<br />
<strong>–</strong> fungal pneumonias<br />
• aspergillosis, pneumocystosis<br />
Interstitial pneumonia<br />
EIV infection, donkey<br />
Pulmonary fibrosis, horse<br />
1
Bronchopneumonia<br />
• Catarrhal-purulent pneumonia<br />
• Fibrinous (pleuro)pneumonia<br />
<strong>–</strong> cranioventral consolidation<br />
<strong>–</strong> predisposing factors<br />
• stress, viral infections etc.<br />
<strong>–</strong> secondary bacterial infection<br />
• Streptococcus equi ssp. equi, ~ zooepidemicus;<br />
Bordetella bronchiseptica, Klebsiella pneumoniae,<br />
Staphylococcus sp.<br />
Bronchopneumonia<br />
• Necrotic/gangrenous pneumonia<br />
<strong>–</strong> aspiration pneumonia<br />
• anatomical predisposition<br />
<strong>–</strong> „tracheal puddle”<br />
• iatrogenic<br />
<strong>–</strong> nasogastric tubing<br />
• CNS involvement!!!!!!!!<br />
<strong>–</strong> rabies, WNV or other viral encephalitides, lead<br />
poisoning, fumonisin toxicosis etc.<br />
<strong>–</strong> usually unilateral, foul smell, rapid autolysis,<br />
necrosis predominates, mixed bacterial flora<br />
Aspiration pneumonia, horse<br />
Chronic purulent bronchopneumonia, horse<br />
Aspiration pneumonia<br />
Pyogranulomatous pneumonia<br />
• Rhodococcus equi infection<br />
<strong>–</strong> Rhodococcus equi<br />
• Facultatively intracellular bacterium, complex lipids<br />
in its cell wall<br />
• Normal inhabitant <strong>of</strong> soil and intestinal tract <strong>of</strong><br />
different species<br />
• Disease in foals <strong>of</strong> 1-6 months <strong>of</strong> age<br />
• Pathogenesis is incompletely understood<br />
<strong>–</strong> Clinical signs<br />
• Fever, cough, nasal discharge, increased<br />
respiratory rate<br />
• High mortality<br />
2
Pyogranulomatous pneumonia<br />
• Rhodococcus equi infection<br />
<strong>–</strong> Lesions<br />
• Lungs and tracheobroncial lymphonodes<br />
<strong>–</strong> Multiple large, firm nodules <strong>of</strong> various size<br />
<strong>–</strong> Caseation necrosis without fibrous capsule formation<br />
(not a proper abscess!)<br />
<strong>–</strong> Predominantly pyogranulomatous inflammation<br />
• Intestinal tract<br />
<strong>–</strong> Ulcerative enterocolitis, involvement <strong>of</strong> mesentarial<br />
lymphonodes<br />
• Arthritis, dermatitis, hepatitis, vertebral<br />
osteomyelitis, ulcerative lymphangitis<br />
Rhodococcus equi pneumonia, horse<br />
Rhodococcus equi pneumonia, horse Rhodococcus equi pneumonia, horse<br />
Granulomatous pneumonia<br />
• Mycobacteriosis<br />
<strong>–</strong>Mycobacterium avium complex<br />
<strong>–</strong>Mycobacterium tuberculosis<br />
<strong>–</strong>Mycobacterium bovis<br />
• Predominantly proliferative<br />
tuberculosis<br />
Granulomatous pneumonia<br />
• Fungal pneumonias<br />
<strong>–</strong>Pulmonary aspergillosis<br />
• secondary to mucosal damage<br />
<strong>–</strong>intestines! ulcerative fungal colitis<br />
• systemic lesions<br />
<strong>–</strong>brain, lungs, skin<br />
• severe disseminated fibrinonecrotic to<br />
granulomatous pneumonia<br />
3
Pulmonary aspergillosis, horse<br />
Pneumocystosis, GMS stain →<br />
Pulmonary aspergillosis, horse Pulmonary aspergillosis, horse<br />
← Pneumocystosis, H-E stain<br />
Granulomatous pneumonia<br />
• Fungal pneumonias<br />
<strong>–</strong>Pneumocystosis<br />
• Pneumocystis carinii fungus<br />
• Secondary to immunosuppressive agents /<br />
immunodeficiencies<br />
<strong>–</strong> SCID<br />
<strong>–</strong> Viral infections, Rhodococcus equi inf.<br />
• Histological diagnosis<br />
<strong>–</strong> foamy structure within alveoli<br />
<strong>–</strong> Gömöri’s Methenamine Silver stain (GMS)<br />
<strong>–</strong> minimal inflammatory changes<br />
Pyogranulomatous pneumonia<br />
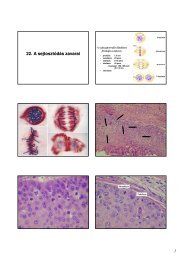
• <strong>Glanders</strong> (<strong>malleus</strong>, <strong>farcy</strong>)<br />
• Burkholderia mallei<br />
<strong>–</strong> Gram-negative, obligate aerobic, nonmotile,<br />
obligate pathogen<br />
<strong>–</strong> Zoonotic agent, bioterrorism!<br />
• Occurrence<br />
<strong>–</strong> Asia, North-Africa, (far-far) East-Europe (?),<br />
South-and Central America<br />
• Susceptible species<br />
<strong>–</strong> Equidae (solipeds), carnivores, guinea-pig,<br />
hamster, goat, man<br />
4
<strong>Glanders</strong> - history<br />
• 3 rd Century BC<br />
<strong>–</strong>Described by Aristotle<br />
• 1664: Contagious nature recognized<br />
• 1830: Zoonotic nature suspected<br />
• 1891: Mallein test developed<br />
• 1<strong>90</strong>0: Control programs implemented<br />
<strong>Glanders</strong> - history<br />
• World War II<br />
<strong>–</strong> Japanese infected <strong>horses</strong>, civilians and POW’s<br />
<strong>–</strong> U.S. and Russia investigated use as biological<br />
weapon<br />
<strong>Glanders</strong><br />
• Pathogenesis<br />
<strong>–</strong> the disease develops through several<br />
successive stages, each is characterised<br />
by distinctive clinical signs and lesions<br />
<strong>–</strong> outcome depends on the immunological<br />
status <strong>of</strong> the host<br />
<strong>–</strong> p. os uptake: primary complex in the<br />
alimentary tract<br />
• early generalisation: lungs, spleen, liver etc.<br />
• late generalisation: septicaemia, nasal mucosa,<br />
skin<br />
<strong>Glanders</strong> - history<br />
• World War I<br />
<strong>–</strong> Suspected use as biological agent to infect<br />
Russian <strong>horses</strong> and mules<br />
• Affected troops and supply convoys<br />
<strong>–</strong> Large number <strong>of</strong> human cases in Russia<br />
during and after WWI<br />
<strong>Glanders</strong><br />
• Way <strong>of</strong> infection<br />
<strong>–</strong>per os<br />
• contaminated feed, water, carcasses <strong>of</strong><br />
infected dead animals<br />
<strong>–</strong>percutaneous or conjunctival, aerogenical<br />
<strong>–</strong>asymptomatic carriers<br />
<strong>Glanders</strong><br />
• Incubation time<br />
<strong>–</strong> Few days to several months<br />
• Clinical forms and signs<br />
<strong>–</strong> Acute form<br />
• donkeys, mules, certain <strong>horses</strong>, carnivores, (man)<br />
• coughing, fever, nasal discharge<br />
• septicaemia, (pyemia), bronchopneumonia, death in<br />
days<br />
<strong>–</strong> Chronic form<br />
• certain <strong>horses</strong>, mules, (man)<br />
• granulomatous changes in the lungs, in the nasal<br />
mucosa, in the skin<br />
• subclinical infection does occur (mallein-test)<br />
5
Draining fistulous tracts<br />
in the skin<br />
<strong>Glanders</strong><br />
<strong>Glanders</strong>,<br />
intradermo-palpebral test<br />
• Lesions<br />
<strong>–</strong> Different lesions might be present in the<br />
same animal<br />
• Lungs<br />
• Nasal mucosa, paranasal sinuses, lips<br />
• Skin (lymphatics)<br />
• Lymphonodes<br />
• Testicles, liver, spleen<br />
• Basic forms <strong>of</strong> lesions<br />
<strong>–</strong> Malleotic nodule (granuloma)<br />
<strong>–</strong> Predominantly exsudative form<br />
<strong>–</strong> Predominantly proliferative form<br />
<strong>Glanders</strong>, nasal and dermal lesions<br />
Malleotic nodule<br />
<strong>Glanders</strong>,<br />
Strauss reaction,<br />
male guinea-pig<br />
• Exsudative development<br />
<strong>–</strong> pathogen in the centre, surrounded by PMNs,<br />
exsudation and hyperemic ring around<br />
<strong>–</strong> later histiocytes and giant cells appear<br />
<strong>–</strong> the center becomes necrotized, fibroblasts<br />
appear on the perimeter<br />
• Proliferative development<br />
<strong>–</strong> pathogen in the centre, surrounded by<br />
epitheloid cells and giant cells<br />
<strong>–</strong> more epitheloid cells accumulate<br />
<strong>–</strong> the center becomes necrotized, fibroblasts<br />
appear on the perimeter...<br />
6
Malleotic nodule<br />
• Developed malleotic nodule<br />
<strong>–</strong>pyogranuloma with narrow demarcation<br />
zone<br />
• colliquated or caseous centre with<br />
occassional calcium salt deposition,<br />
surrounded by epitheloid cells, giant cells<br />
and granulation tissue<br />
• poppy seed to pea sized nodules with<br />
greyish-yellow dry or liquid centre<br />
Malleotic nodules, nasal septum, horse<br />
„Farcy”,<br />
ulcerative lymphangitis<br />
Malleotic nodule, lung<br />
Malleotic ulcer<br />
• Malleotic ulcer<br />
<strong>–</strong> nodules close to the surface<br />
• mucous membranes, skin<br />
<strong>–</strong> nasal cavity, trachea, larynx<br />
<strong>–</strong> necrosis, shedding <strong>of</strong> the necrotized part<br />
<strong>–</strong> shallow to deep erosions <strong>–</strong> ulcers<br />
• uneven margin<br />
• undermined edge<br />
• covered with egg-white like material<br />
<strong>–</strong> healing with scar formation<br />
Different stages <strong>of</strong> malleotic nodules and ulcers, nasal septum, horse<br />
7
Malleotic ulcer on the lip,<br />
donkey<br />
Malleotic nodules and ulcers, nasal septum, horse<br />
Chronic malleotic ulcers, nasal septum, horse Chronic malleotic ulcers, nasal septum, horse<br />
Predominantly exsudative glanders<br />
• Lungs, other tissues<br />
<strong>–</strong>ser<strong>of</strong>ibrinous inflammation around the<br />
pathogen<br />
• bronchopneumonia<br />
<strong>–</strong>necrosis with caryorhexis, colliquation<br />
<strong>–</strong>healing with proliferation <strong>of</strong> malleotic<br />
granulation tissue<br />
• may contain dry areas with calcium<br />
deposits<br />
Disseminated pyogranulomas, bronchopneumonia<br />
8
Thrombosis, necrotizing rhinitis<br />
(„Zahn-lines” in the thrombus)<br />
Predominantly proliferative glanders<br />
• Mucous membranes<br />
<strong>–</strong>proliferation <strong>of</strong> malleotic granulation<br />
tissue<br />
• fibroblasts<br />
• histiocytes, giant cells<br />
<strong>–</strong>barley seed sized greyish-white firm<br />
nodules on mucous membranes<br />
<strong>Glanders</strong><br />
• Differential diagnosis<br />
<strong>–</strong> Strangles<br />
• Streptococcus equi ssp. equi<br />
<strong>–</strong> Epizootic lymphangiitis<br />
• Histoplasma sp.<br />
<strong>–</strong> Ulcerative lymphangiitis<br />
• Corynebacterium pseudotuberculosis<br />
<strong>–</strong> Melioidosis<br />
• Burkholderia pseudomallei<br />
<strong>–</strong> Blastomycosis, cryptococcosis<br />
• Blastomyces sp., Cryptococcus sp.<br />
Fibrinous vasculitis<br />
Proliferative malleotic nodules, trachea, horse<br />
9