Newsletter Newsletter - Society for Obstetric Anesthesia and ...
Newsletter Newsletter - Society for Obstetric Anesthesia and ...
Newsletter Newsletter - Society for Obstetric Anesthesia and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Society</strong> <strong>for</strong> <strong>Obstetric</strong> <strong>Anesthesia</strong> <strong>and</strong> Perinatology<br />
David J. Wlody, MD<br />
Greetings to the members of SOAP, <strong>and</strong> to<br />
all those who are interested in the anesthetic<br />
care of the pregnant woman. As the New<br />
Year begins, there is ample evidence that<br />
both our <strong>Society</strong> <strong>and</strong> the subspecialty of<br />
<strong>Obstetric</strong> Anesthesiology are healthy, <strong>and</strong><br />
poised <strong>for</strong> what I believe will be a period of<br />
unprecedented growth.<br />
The <strong>Obstetric</strong> Anesthesiology program at<br />
this year’s ASA Annual Meeting in Chicago<br />
was, once again, extremely successful. The<br />
SOAP-Sol Shnider Breakfast Panel, entitled<br />
“Can obstetric anesthesia affect long-term<br />
maternal <strong>and</strong> newborn outcome?”, was very<br />
well attended. Dr. Barbara Leighton of<br />
Washington University, Dr. William<br />
Grobman of the Department of OB-GYN at<br />
Northwestern University, <strong>and</strong> Dr. Patricia<br />
Lav<strong>and</strong>’homme of the Université Catholique<br />
in Brussels delivered comprehensive<br />
presentations on the effects of anesthetic<br />
technique on breastfeeding success, pelvic<br />
floor dysfunction, <strong>and</strong> the development of<br />
chronic post-Cesarean pain, respectively.<br />
The SOAP/Anesthesiology scientific paper<br />
special session showcased six outst<strong>and</strong>ing<br />
papers in the field of OB anesthesia. These<br />
sessions, as well as the refresher course<br />
lectures, pro-con debates, <strong>and</strong> all of our<br />
other offerings made this year’s Annual<br />
Meeting a showcase <strong>for</strong> our subspecialty.<br />
The political activities of the ASA were<br />
equally important to <strong>Obstetric</strong> Anesthesiology.<br />
www.soap.org<br />
The ASA House of Delegates approved a<br />
revision of the Practice Guidelines <strong>for</strong><br />
<strong>Obstetric</strong> <strong>Anesthesia</strong>, marking the first<br />
change in this document since 1998. This<br />
revision incorporates almost ten years of<br />
obstetric anesthesia research, <strong>and</strong> represents<br />
the state of the art <strong>for</strong> the anesthetic care of<br />
the pregnant woman. It can be downloaded<br />
at the ASA website:<br />
http://www2.asahq.org/publications/<br />
Many thanks to the members of the ASA<br />
Task Force on <strong>Obstetric</strong> <strong>Anesthesia</strong>, <strong>and</strong> to<br />
the Task Force chair, Joy Hawkins, <strong>for</strong> all<br />
their hard work.<br />
Many of you are familiar with Anne<br />
Maggiore <strong>and</strong> her team at the International<br />
<strong>Anesthesia</strong> Research <strong>Society</strong>, who have<br />
provided management services to SOAP<br />
since 2003. SOAP has been very pleased<br />
with the service provided by IARS, <strong>and</strong><br />
wished to continue this relationship.<br />
Un<strong>for</strong>tunately, we have been notified by<br />
IARS that they will no longer be able to<br />
provide management services to SOAP<br />
effective December 31, 2007. SOAP sent out<br />
a Request <strong>for</strong> Proposal in August, <strong>and</strong> <strong>for</strong> the<br />
past several months, the Board of Directors<br />
has been evaluating management proposals<br />
that have been submitted to us. It is the<br />
Board’s goal to select a firm that is<br />
experienced with the management of an<br />
anesthesiology society, <strong>and</strong> that can provide<br />
excellent service within fiscally responsible<br />
constraints. The Board hopes to make a<br />
selection prior to the Annual Meeting in<br />
Banff, in order to permit our new team to<br />
observe the meeting firsth<strong>and</strong>.<br />
I am sure that many of you are interested in<br />
the status of our application to the<br />
Accreditation Council on Graduate Medical<br />
Education (ACGME) <strong>for</strong> accreditation of<br />
<strong>Newsletter</strong><br />
President’s Message<br />
January 2007<br />
training in <strong>Obstetric</strong> Anesthesiology. The<br />
<strong>for</strong>mal application has been submitted to<br />
ACGME, <strong>and</strong> as of this writing, plans are<br />
being finalized <strong>for</strong> representatives of SOAP<br />
to meet with ACGME within the next<br />
several months. For reasons I recounted in<br />
my last President’s message, the success of<br />
this ef<strong>for</strong>t is of critical importance to our<br />
subspecialty. SOAP leadership will keep you<br />
in<strong>for</strong>med of the progress of our application.<br />
It seems that a constant during my career in<br />
obstetric anesthesiology has been the<br />
publication, <strong>and</strong> subsequent wide dissemination<br />
to the general public, of articles<br />
suggesting a causal relationship between<br />
epidural analgesia <strong>and</strong> various adverse<br />
effects on the mother or her newborn—a<br />
relationship which is often eventually<br />
disproved, with much less fanfare than the<br />
original report. From long-term effects on<br />
the intellectual development of the newborn,<br />
to the development of chronic headache, to<br />
an increased incidence of cesarean section,<br />
we spend much continued on page 2<br />
Inside<br />
OAPEF Contribution Listing . . . . . . . . . . . 2<br />
39th Annual Meeting<br />
Scientific Program . . . . . . . . . . . . . . . . . . 3<br />
Syllabus . . . . . . . . . . . . . . . . . . . . . . . . . .4<br />
PRO/CON Debate . . . . . . . . . . . . . . . . . . . .6<br />
SOAP Future Meetings . . . . . . . . . . . . . . . .9<br />
SOAP Membership Committee Report . . . 10
President’s Message–continued from page 1 OAPEF Contributions<br />
of our time responding to concerns that are<br />
unsubstantiated by the medical literature, but which<br />
are nevertheless highly disturbing to our patients.<br />
The most recent of these was a study, widely<br />
reported in the news media in mid-December, that<br />
claimed to demonstrate that women who received<br />
epidural analgesia were more likely to have<br />
difficulty breastfeeding in the first week after<br />
delivery, <strong>and</strong> were twice as likely to have given up<br />
breastfeeding at six months after delivery. The study,<br />
by Torvaldsen et al., entitled “Intrapartum epidural<br />
analgesia <strong>and</strong> breastfeeding: a prospective cohort<br />
study” can be found at in an online-only journal at:<br />
http://www.internationalbreastfeedingjournal.com<br />
The findings comprise a secondary analysis of a<br />
database collected <strong>for</strong> a different study in Australia in<br />
1997. In an interview with Reuters news service, the<br />
lead author was quoted that the most important<br />
message is that women who receive epidurals should<br />
receive additional help with breastfeeding, but also<br />
that the results of this study should be used to enable<br />
women to make in<strong>for</strong>med decisions about analgesia<br />
during labor. There are methodologic problems with<br />
this study that, in my view, render the results<br />
completely unreliable (Table 1). Un<strong>for</strong>tunately, none<br />
of the news articles that I have read were written with<br />
enough scientific rigor to address any of these<br />
shortcomings, <strong>and</strong> presented the study as gospel truth.<br />
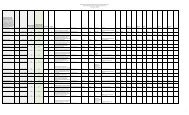
TABLE 1<br />
Methodologic Shortcomings-Torvaldsen et al.<br />
1. Non-r<strong>and</strong>omized study—selection bias is likely.<br />
2. Mixed vaginal <strong>and</strong> cesarean deliveries—when<br />
vaginal deliveries were analyzed separately, NO<br />
association between analgesia <strong>and</strong> breastfeeding<br />
3. All women receiving an epidural also received<br />
parenteral meperidine<br />
4. No dose-response relationship demonstrated<br />
5. Despite the alarming tone of many of the media<br />
reports, both the study author <strong>and</strong> an accompanying<br />
editorial clearly state that a causal relationship<br />
cannot be demonstrated by these findings.<br />
Comments courtesy of William Camann, MD<br />
It is easy enough to become disheartened by such<br />
episodes, but the world is not necessarily a fair<br />
place, <strong>and</strong> on the scale of injustice this is a small<br />
one. It is our task to be familiar with the<br />
(mis)in<strong>for</strong>mation that is circulating among our<br />
patients, to be able to address, accurately <strong>and</strong><br />
dispassionately, the merits or lack thereof of these<br />
studies, <strong>and</strong> to support our colleagues who per<strong>for</strong>m<br />
the research that provides the basis <strong>for</strong> what we do<br />
every day. It is in this fashion that we can truly be<br />
advocates <strong>for</strong> our patients, their newborns, <strong>and</strong> the<br />
generations to come.<br />
Good luck, <strong>and</strong> best wishes <strong>for</strong> the coming year.<br />
November 1, 2005 – December 15, 2006<br />
Donors
SOAP 39th Annual Meeting – Scientific Program<br />
Wednesday, May 16, 2007<br />
7:00 - 2 pm Simulation Workshops<br />
1:00 - 5:15 pm Japanese <strong>Society</strong> of Anesthesiology<br />
SOAP Symposium (Simultaneous Japanese<br />
Translation)<br />
Gurinder M. S. Vasdev, MD; et al.<br />
1:00 - 5:00 pm American Academy of Pediatric Neonatal<br />
Resuscitation Certification Program<br />
6:00 - 8:00 pm Reception<br />
Thursday, May 17, 2007<br />
6:00 am-5:00 pm Registration<br />
6:45 - 8:00 am Breakfast with Exhibitors <strong>and</strong> Poster Review<br />
8:00 - 10:00 am Spouse <strong>and</strong> Guest Hospitality<br />
7:45 - 8:00 am General Assembly<br />
Welcome to the 39th Annual SOAP Meeting:<br />
David J. Wlody, MD, President; Raouf Wahba, MD,<br />
FRCPC, Host; Gurinder M.S. Vasdev, MD, FRCA,<br />
Chair<br />
8:00 - 9:30 am Gertie Marx: Research Competition<br />
Moderator: Alan C. Santos, MD<br />
Judges: William R. Camann, MD; Andrew Harris,<br />
MD; Gordon Lyons, FRCA; Linda S. Polley, MD;<br />
Maya S. Suresh, MD<br />
9:30 - 9:45 am Distinguished Service Award<br />
Presented to Frank James, MD by SOAP President<br />
David J. Wlody, MD<br />
9:45 - 10:15 am Coffee with Exhibitors/Posters<br />
10:15 - 11:00 am PRO/CON Debate: Neuraxial Techniques<br />
<strong>for</strong> Labor Analgesia Should be Placed in<br />
the Lateral Position<br />
Moderator: John Thomas, MD<br />
Pro: Lawrence C. Tsen, MD<br />
Con: Linda S. Polley, MD<br />
11:00-12:00 pm Oral Presentations #1<br />
Moderator: Mark Rosen, MD<br />
12:00 - 1:00 pm Lunch with Exhibitors <strong>and</strong> Poster Review<br />
1:00 - 2:00 pm What’s New in <strong>Obstetric</strong>s?<br />
Introduction: Raouf Wahba, MD, FRCPC;<br />
Presenter: Michael Helewa, MD, FRCPC<br />
2:00 - 3:00 pm Zuspan Award: Research Competition<br />
Moderator: Vernon Ross, MD<br />
Judges: Linda Barbour, MD, MSPH; Michael<br />
Helewa, MD, FRCPC; Edward T. Riley, MD; Junzo<br />
Takeda, MD; Kathryn Zuspan, MD<br />
3:00 - 3:30 pm Coffee Break with Exhibitors <strong>and</strong> Poster Review<br />
3:30 - 6:00 pm SOAP Business Meeting – Awards Presentations<br />
David J. Wlody, MD<br />
_______________<br />
6:00 - 9:00 pm Residents/Fellows/Students Only Forum<br />
(Trainees & Mentors)<br />
Session Chair: Gurinder M.S. Vasdev, MD<br />
6:00 - 7:00 pm Welcome Reception <strong>for</strong> Trainees<br />
David J. Wlody, MD, President, SOAP<br />
7:00 - 7:30 pm Poster Review<br />
— 3—<br />
7:30 - 8:00 pm Oral Presentations<br />
Judges: Terrance Breen, MD; M. Joanne Douglas,<br />
MD, FRCPC; Helene Finegold, MD;<br />
Joanne C. Hudson, MD; Linda S. Polley, MD;<br />
Monica Riesner, MD; Barbara Scavone, MD<br />
8:00 - 8:45 pm Resident Lecture: Professionalism in<br />
Anesthesiology through SOAP<br />
Joanne Hudson, MD<br />
Friday, May 18, 2007<br />
6:00 am-12 noon Registration<br />
6:45 - 8:00 am Breakfast with Exhibits <strong>and</strong> Poster Review<br />
8:00 - 10:00 am Spouse <strong>and</strong> Guest Hospitality<br />
6:45 - 7:45 am Breakfast with the Experts<br />
Co-Chairs: David Campbell, MD, MSc, FRCPC;<br />
Michael Paech, MD<br />
Experts: Brendan Carvalho, MB, BCh; Jose Carvalho,<br />
MD, PhD, FRCPC; Sheila E. Cohen, MB, ChB,<br />
FRCA; Lesley-Ann Crone, MD, FRCPC; M. Joanne<br />
Douglas, MD, FRCPC; Roshan Fern<strong>and</strong>o, FRCA;<br />
David Gambling, MD, FRCPC; Stephen Halpern,<br />
MD, FRCPC; David Hepner, MD; Robert S.<br />
McKay, MD; Dolores McKeen, MD, FRCPC; Jill<br />
Mhyre, MD; Pam Morgan, MD, FRCPC; Holly Muir,<br />
MD, FRCPC; Kenneth E. Nelson, MD; Toshiyuki<br />
Okutomi, MD; Quisqueya Palacios, MD; Craig<br />
Palmer, MD; Donald H. Penning, MD, MSc, FRCP;<br />
Roanne Preston, MD, FRCPC; Maya S. Suresh, MD;<br />
Katsuo Terui, MD; Ashu Wali, MD, FFARCSI;<br />
Cynthia Wong, MD<br />
8:00 - 9:00 am Poster Review #1<br />
Moderator: Yaakov Beilin, MD<br />
9:00 - 10:00 am What’s New in <strong>Obstetric</strong> Medicine?<br />
Introduction: William R. Camann, MD<br />
Speaker: Linda Barbour, MD, MSPH<br />
10:00 - 10:30 am Coffee with Exhibitors <strong>and</strong> Poster Review<br />
10:30 - 1:00 pm Patient Safety Session<br />
Chair: Stephen Pratt, MD<br />
10:30 - 11:15 am Role of Simulation in Teaching <strong>Obstetric</strong> <strong>Anesthesia</strong><br />
Speaker: John Sullivan, MD<br />
11:15 - 12:15 pm Pro-Con Debate #2: Crew Resource<br />
Management in Medicine is a Fad<br />
Moderator: May Pian-Smith, MD, MS<br />
Pro: Richard N. Wissler, MD, PhD<br />
Con: John Pawlowski, MD<br />
12:15 - 1:00 pm The Impact of National Patient Safety Goals<br />
from the Joint Commission on the Accreditation<br />
of Healthcare Organization <strong>for</strong> <strong>Obstetric</strong>s <strong>and</strong><br />
<strong>Obstetric</strong> <strong>Anesthesia</strong><br />
Speaker: Edward Molina-Lamas, MD, FACA<br />
1:30 pm Golf Tournament : Fairmont Banff Springs Golf<br />
Course (includes lunch)<br />
2:00 - 6:00 pm Social Afternoon (lunch on your own)<br />
Fun Run/Walk; Horseback Riding; Nature Trails; SPA<br />
7:00 - 11:00 pm The SOAP Ball (Party attire)
SOAP 39th Annual Meeting – Scientific Program<br />
Regional Workshop in <strong>Obstetric</strong> <strong>Anesthesia</strong> - Optional<br />
2:00 - 4:45 p.m. Regional Workshop in <strong>Obstetric</strong> <strong>Anesthesia</strong><br />
(By Ticket Only - Limited Registration)<br />
Director: Jose Carvalho, MD, PhD, FRCPC<br />
Faculty: Cristian Arzola, MD; Mirinalini Balki,<br />
MD; Jose Carvalho, MD, PhD, FRCPC;<br />
Barry Harrison, MD, FANZCA; James Hebl, MD;<br />
Shreeniwas Jawalekar, MD; S<strong>and</strong>ra Kopp, MD;<br />
Krzysztof M. Kuczkowski, MD; Hugh Smith, MD,<br />
PhD; Jack Wilson, MD<br />
Program<br />
2:00 - 2:45 p.m. Introduction to Ultrasound <strong>and</strong> Case Examples<br />
(participants divided into two groups)<br />
2:45 - 3:30 p.m. Group 1: Ultrasound with models<br />
Group 2: Glass spine demonstration, CSE<br />
Simulator, Tsui Test Simulator<br />
3:30 - 4:00 p.m. Break (re-set stations)<br />
4:00 - 4:45 p.m. Group 1: Glass spine demonstration, CSE<br />
Simulator, Tsui Test Simulator<br />
Group 2: Ultrasound with models<br />
Saturday, May 19, 2007<br />
6:00 am-12 noon Registration<br />
8:00 - 10:00 am Spouse <strong>and</strong> Guest Hospitality<br />
6:30 - 7:45 am Breakfast Panel: Genomics in <strong>Obstetric</strong> <strong>Anesthesia</strong><br />
Chair: Richard Smiley, MD, PhD<br />
Speakers: William Hartman, MD, PhD;<br />
Ruth L<strong>and</strong>au, MD<br />
8:00 - 9:00 am OB <strong>Anesthesia</strong> Research:<br />
The Unanswered Questions<br />
Speakers: Robert D’Angelo, MD; Philip Hess, MD;<br />
Barbara Leighton, MD; Edward Riley, MD;<br />
Scott Segal, MD; Richard Smiley, MD, PhD<br />
9:00 - 10:00 am Gerard W. Ostheimer Lecture:<br />
What’s New in OB <strong>Anesthesia</strong>?<br />
Introduction: Roshan Fern<strong>and</strong>o, FRCA<br />
Speaker: Alison Macarthur, MD, MSc, FRCPC<br />
10:00 - 10:15 am Break<br />
10:15 - 11:15 am Oral Presentation #2<br />
Moderator: Michael Froelich, MD<br />
11:15 - 12:15 pm Fred Hehre Lecture: Malpractice or<br />
Miscommunication? The Importance of Improved<br />
Communication between Anesthesiologists,<br />
Patients <strong>and</strong> our Colleagues<br />
Introduction: David J. Wlody, MD<br />
Speaker: David J. Birnbach, MD, MPH<br />
12:15 - 1:00 pm Lunch (on your own)<br />
1:00 - 2:00 pm Best Paper Presentations<br />
Moderator: Gordon Lyons, FRCA<br />
Judges: Theodore Cheek, MD; McCallum Hoyt, MD;<br />
Geraldine O’Sullivan, FRCA; Alex Pue, MD;<br />
Michael P. Smith, MD, MS Ed;<br />
Rakesh Vadhera, FRCA<br />
2:00 - 3:00 pm Best Case Reports: You Did What?<br />
Moderator: Robert Gaiser, MD<br />
3:00 - 3:15 pm Break<br />
3:15 - 4:00 pm Poster Review #2<br />
Moderator: Moeen K. Panni, MD<br />
— 4—<br />
4:00 - 5:30 pm Panel on Infection after Neuraxial <strong>Anesthesia</strong><br />
Chair: Peter H. Pan, MD<br />
Panelists: Joy Hawkins, MD; Terese T. Horlocker,<br />
MD; Samuel Hughes, MD; Ruth L<strong>and</strong>au, MD<br />
6:00 pm Transportation to Mountain View Barbeque<br />
6:00 - 10:30 pm Mountain View Barbeque - Optional Event<br />
A place where the starry mountain views are<br />
breathtaking <strong>and</strong> the western hospitality abounds!<br />
Mosey on in to the famous “Donut Tent,” a round<br />
log building with a hole in the center - built<br />
specifically <strong>for</strong> blazing bonfires. Please sign up <strong>for</strong><br />
this event at www.roadwest.com/soap.<br />
SOAP 39th Annual Meeting<br />
May 16-19, 2007<br />
FAIRMONT BANFF SPRINGS, ALBERTA, CANADA<br />
SOAP had an excellent year in 2006, thanks to the outst<strong>and</strong>ing ef<strong>for</strong>ts<br />
of Bill Camann <strong>and</strong> David Wlody. We achieved many of our goals at<br />
the 38th annual meeting in Hollywood, Florida with a large attendance<br />
<strong>and</strong> an outst<strong>and</strong>ing program. Our excellent financial per<strong>for</strong>mance in<br />
2006 is helping us build a stronger SOAP <strong>for</strong> the future. Setting our<br />
course <strong>for</strong> 2007 is actually quite simple: Concentrate on what we do<br />
best—<strong>and</strong> make it even better! We ensure that the quality of research<br />
<strong>and</strong> education presented at SOAP are so unique <strong>and</strong> valuable that they<br />
will always be in dem<strong>and</strong>. As program chair <strong>and</strong> host <strong>for</strong> SOAP 2007,<br />
it is our honor to invite you to attend the 39th Annual Meeting in Banff,<br />
Alberta, Canada. This meeting will feature some of the brightest <strong>and</strong><br />
most talented physicians who will share recent advances in obstetric<br />
anesthesia. This is a strong <strong>for</strong>um <strong>for</strong> obstetric anesthesia; not only<br />
highlighted by the scientific program but by the social events as well:<br />
All this in a picture postcard setting.<br />
The Scientific Program<br />
This starts with pre-meeting workshops. We are proud to introduce<br />
2.25-hour h<strong>and</strong>s on simulation session. There will be real-time<br />
simulated OB disasters, which the participants must manage (please<br />
wear com<strong>for</strong>table clothing). We have invited simulation education<br />
experts from the Mayo Clinic <strong>and</strong> Magee Women’s Hospital with<br />
the current state of the art medical simulators to teach this course.<br />
Please register early, as there is limited space.<br />
We are also pleased to offer re-certification in Neonatal Resuscitation<br />
(NRP). As you all know the American Academy of Pediatrics recently<br />
revised the NRP. Our course will highlight these changes <strong>and</strong> review<br />
the pertinent details <strong>for</strong> re-certification. Pre-registration is<br />
m<strong>and</strong>ated, so we can mail the required reading materials to you.<br />
Satisfactory completion of this course will result in a 2-year<br />
certification from the American Academy of Pediatrics. Space is<br />
limited <strong>and</strong> registration is on a first come first served bases.<br />
SOAP extends a warm welcome to the Japanese <strong>Society</strong> of Anesthesiology<br />
(JSA). A joint Pre-meeting symposium represents an<br />
important link <strong>for</strong> our society <strong>and</strong> the emerging subspecialty<br />
continued on page 5
continued from page 4<br />
SOAP 39th Annual Meeting – May 16-19, 2007<br />
of <strong>Obstetric</strong> <strong>Anesthesia</strong> in Japan. We are confident both SOAP <strong>and</strong><br />
JSA members will enjoy this <strong>for</strong>um of international exchange<br />
creating an environment to foster collaborative research, education<br />
<strong>and</strong> clinical practice.<br />
We encourage you not to miss the SOAP reception on Wednesday<br />
evening. It is a great chance to mingle with other SOAP members in<br />
a wonderful atmosphere in the “Castle in the Rockies.”<br />
Thursday, May 17, 2007, our <strong>for</strong>mal meeting opens with the Gertie<br />
Marx: Research Competition. For those coming to SOAP <strong>for</strong> the first<br />
time, this is a great opportunity to win a prize at SOAP. The papers<br />
selected <strong>for</strong> the award are judged on the day. The Zuspan Award <strong>and</strong><br />
Best Paper awards are other prizes that encourage academic contributions<br />
from our obstetrician <strong>and</strong> obstetric medicine colleagues.<br />
One of the most enjoyable portions of our meeting is the debates. In<br />
calling the first question, Laurence Tsen <strong>and</strong> Linda Polley will debate<br />
“the correct position <strong>for</strong> initiation of neuraxial blocks.” For our second<br />
question, Richard Wissler will go head to head with John Pawlowski<br />
debating whether “crew resource management in medicine is a fad.”<br />
We are privileged to have Dr. Michael Elias Helewa, Past<br />
President/Président sortant of The <strong>Society</strong> of <strong>Obstetric</strong>ians <strong>and</strong><br />
Gynaecologists of Canada, deliver the “What’s New in <strong>Obstetric</strong>s?”<br />
lecture. Our next invited speaker is Dr. Linda Barbour from Denver,<br />
Colorado. She is Past President of the North American <strong>Society</strong> of<br />
<strong>Obstetric</strong> Medicine, has served on the Pregnancy Council <strong>for</strong> the<br />
American Diabetes Association, <strong>and</strong> chaired the Colorado Clinical<br />
Guidelines Collaborative <strong>for</strong> Management of Gestational Diabetes<br />
<strong>for</strong> the state health department. She will present the “What’s New in<br />
<strong>Obstetric</strong> Medicine” lecture.<br />
Dr. Alison Macarthur from Toronto, Ontario, Canada is the chair of<br />
the <strong>Obstetric</strong> Section of the Canadian Anesthesiologists’ <strong>Society</strong>.<br />
She has graciously offered to present the Gerard Ostheimer Lecture:<br />
“What’s new in <strong>Obstetric</strong> <strong>Anesthesia</strong>?”.<br />
Professor David Birnbach, from Miami, Florida will deliver the honored<br />
Fred Hehre Lecture. He will discuss the problems associated with<br />
miscommunications. We believe there will be many eloquent surprises<br />
in his outst<strong>and</strong>ing presentation. This is truly a “do not miss lecture.”<br />
What’s new <strong>for</strong> SOAP in 2007?<br />
• We have introduced a trainee <strong>for</strong>um: An opportunity <strong>for</strong><br />
residents, fellows, students <strong>and</strong> mentors to become more<br />
involved in SOAP. Our future lies within the young curious<br />
minds that promote our mission.<br />
• A primer in genomics has been added to the research hour to<br />
introduce members to the huge potential <strong>for</strong> obstetric anesthesia of<br />
the human genomic project. Just think – one day we will be able<br />
plan a parturients anesthetic based on a blood test or buccal smear.<br />
• The Impact of National Patient Safety Goals from the Joint<br />
Commission on the Accreditation of Healthcare Organization <strong>for</strong><br />
<strong>Obstetric</strong>s <strong>and</strong> <strong>Obstetric</strong> <strong>Anesthesia</strong>. Much of the dem<strong>and</strong>s of<br />
— 5—<br />
JCAHO affect us directly or indirectly. Dr. Edward Molina-Lamas<br />
will unravel the reasons why such m<strong>and</strong>ates have come about <strong>and</strong><br />
he will be open <strong>for</strong> a question <strong>and</strong> answer session.<br />
• The Regional Workshop is an optional event <strong>for</strong> Friday afternoon<br />
<strong>for</strong> those who are unable to join in the social events. The highlights<br />
include the use of ultrasound <strong>for</strong> placement of neuraxial block,<br />
h<strong>and</strong>s-on demonstration of the spinal anesthesia (including microcatheters)<br />
with the glass spine, CSE simulator <strong>and</strong> the Tsui test <strong>for</strong><br />
epidural placement.<br />
• To answer many of the questions regarding neuraxial infection we<br />
present a panel discussion on “infection after neuraxial<br />
anesthesia”. This <strong>for</strong>um will discuss many of the issues<br />
surrounding anti-sepsis <strong>and</strong> higlight some of the challenges facing<br />
the ASA in developing practice advisories.<br />
Social Events<br />
No SOAP will ever be complete without memorable social events.<br />
The following will be offered on our website (www.soap.org). Please<br />
register early so we can better allocate resources <strong>for</strong> these events.<br />
• Welcome to Banff Reception • SOAP Ball (party attire)<br />
• Golf Tournament • Mountain View Barbecue<br />
• Fun Run/Walk • Tours of Area Attractions<br />
• Horseback Riding • SOAP dine around<br />
Getting to Banff<br />
Air travel to Banff is via Calgary’s International Airport, which is<br />
located approximately 80 miles east of the resort. SOAP has made<br />
special arrangements <strong>for</strong> discounted round-trip ground<br />
transportation from the Calgary Airport to Banff. This timesaving<br />
service is exclusively <strong>for</strong> SOAP participants. Registrants are<br />
encouraged to take advantage of this convenient transportation.<br />
In<strong>for</strong>mation is available on the SOAP website <strong>and</strong> includes a link to<br />
Road West, here you can make your reservation:<br />
www.roadwest.com/soap<br />
The Fairmount Banff Springs is truly a “Castle in the Rockies”. It is<br />
one of a kind hotel. SOAP has negotiated great rates <strong>for</strong> SOAP<br />
participants. Great rates <strong>and</strong> low Alberta tax structure provide great<br />
opportunity to enjoy this unique atmosphere. SOAP also arranged<br />
<strong>for</strong> a convenient transportation directly from the Fairmont Banff<br />
Spring Hotel to Calgary International Airport <strong>for</strong> those who have<br />
early Sunday departures flights. Please make your reservation<br />
through Road West link <strong>and</strong> indicate your departure time.<br />
Weather everywhere can be unpredictable; Banff in May will<br />
experience late spring or early summer temperatures. As with all<br />
mountain climates the evenings will be cool. Those of you who wish<br />
to travel to the glaciers you should bring appropriate clothes. Banff<br />
is rated as one of the world’s most beautiful parks by National<br />
Geographic. Please consider spending a little extra time <strong>and</strong> enjoy<br />
great spring skiing at Sunshine Village, golf <strong>and</strong> horseback riding.<br />
Do not miss this exceptional opportunity; make plans today to attend<br />
SOAP’s 39th Annual Meeting at the “Castle in the Rockies”.<br />
We look <strong>for</strong>ward to seeing you in Banff.
PRO CON<br />
PRO<br />
Supplemental Oxygen Should Routinely Be Used<br />
During Cesarean Section<br />
Scott Segal, MD<br />
Brigham <strong>and</strong> Women’s Hospital<br />
Harvard Medical School<br />
Boston, MA<br />
Am I really defending oxygen?! Anesthesiologists’ use of supplemental<br />
oxygen during surgical procedures is one of the oldest, most<br />
fundamental <strong>and</strong> widely accepted interventions in the specialty.<br />
However, tradition is not a valid argument <strong>and</strong> I will attempt to make<br />
a logical case <strong>for</strong> the routine use of oxygen.<br />
To begin, let me propose a syllogism:<br />
• If an intervention offers significant benefit to all patients, or<br />
benefits some patients <strong>and</strong> has neutral effects on all others, <strong>and</strong><br />
• If this intervention does not produce significant adverse effects,<br />
then<br />
• The intervention should be routinely used.<br />
To illustrate this reasoning, consider pulse oximetry or capnography,<br />
both interventions that truly help very few patients but do so at no<br />
appreciable risk <strong>and</strong> so are routinely employed.<br />
Beneficial effects of oxygen<br />
There are several direct benefits of oxygen to the mother <strong>and</strong><br />
perhaps the baby:<br />
1. During maternal anesthetic mishap. Contrary to our wishes,<br />
regional anesthesia sometimes fails, <strong>and</strong> general anesthesia is<br />
needed. A large study showed this occurs 4.3% of the time during<br />
epidural anesthesia, <strong>and</strong> 1.2% during spinal anesthesia 1 . If the<br />
procedure has started, it is a big head start on being able to quickly<br />
induce general anesthesia. More ominously, unexpected high or<br />
total spinal occurs often enough to justify precautionary oxygen.<br />
After epidural block, 1/1400 to 1/4500 patients develop high or<br />
total spinal bloc. 2,3 Even after routine spinal block, 1/3200 to<br />
1/30,000 will develop a total spinal. 1,4 Otherwise unexplained<br />
bradyasystolic cardiac arrest under spinal anesthesia occurs even<br />
more frequently, 1/1600-1/3700. 5-7 Taking some liberties in my<br />
estimation of our readership, that means this will happen to<br />
someone reading this article at least several times a year!<br />
Does oxygen help when things go wrong? Yes! Half a century ago<br />
when intravenous anesthetics <strong>and</strong> controlled ventilation were just<br />
coming of age, investigators showed that desaturation during apnea<br />
was much faster in patients breathing room air than in those<br />
receiving supplemental oxygen. Dillon 8 gave thiopental to induce<br />
apnea <strong>and</strong> showed a 50% decrease in PO2 in 4 minutes when<br />
breathing room air, but only 5% when breathing oxygen. Similarly,<br />
Weitzner 9 showed SaO2 decreased to 60% in just 1.5 minutes of<br />
apnea after air ventilation but did not change after oxygen<br />
ventilation. And even a little oxygen helps vs. none at all. Heller 10<br />
— 6—<br />
compared room air to different FiO2’s <strong>and</strong> showed desaturation in<br />
just 1 minute on room air vs. 2.5 minutes on 33% O2, <strong>and</strong><br />
supranormal PO2 after 4 minutes when breathing 50 or 100%. Of<br />
course, all of us appreciate that obesity <strong>and</strong> pregnancy both lead to<br />
even more rapid desaturation than in the healthy males studied<br />
decades ago.<br />
2. During obstetric mishaps. Rarely <strong>and</strong> unexpectedly, amniotic<br />
fluid embolism (AFE) or air embolism can complicate cesarean<br />
section, leading to sudden cardiopulmonary decompensation. The<br />
situation would be analogous to that of a total spinal or<br />
bradyasystolic arrest, in that a longer time be<strong>for</strong>e desaturation<br />
might be expected if the patient were breathing oxygen. Of<br />
course, no good data exists comparing AFE with or without<br />
oxygen! More commonly, sudden brisk hemorrhage sometimes<br />
complicates cesarean section. Oxygen has been shown to<br />
ameliorate the cognitive dysfunction <strong>and</strong> tachycardia which<br />
accompanies severe isovolemic anemia 11 .<br />
3. Reducing maternal wound infection. Two well-per<strong>for</strong>med<br />
r<strong>and</strong>omized trials have shown that supplemental oxygen reduced<br />
wound infection rates after abdominal surgery. 12,13 This remains to<br />
be demonstrated in cesarean section, but wound infection is<br />
relatively common in this operation, particularly in the case of<br />
obesity or ruptured membranes.<br />
4. Reducing maternal nausea. Some evidence supports a role <strong>for</strong><br />
oxygen in reducing nausea in women receiving spinal anesthesia. 14<br />
It remains to be demonstrated in cesarean section, but the baseline<br />
incidence is so high that even a modest effect would be<br />
welcomed.<br />
5. The baby. Although the placenta insulates the fetus from<br />
hyperoxia, increasing maternal FiO2 increases the PO2 in the<br />
umbilical vein <strong>and</strong> artery. 15 Using fetal pulse oximetry, Simpson<br />
<strong>and</strong> James 16 demonstrated that among common methods <strong>for</strong> in<br />
utero resuscitation of the baby (also including fluid bolus <strong>and</strong><br />
position changes), maternal oxygen was the most effective <strong>and</strong><br />
had the greatest effect on fetal oxygenation when the baseline was<br />
lowest. Although neither proponents nor opponents of oxygen<br />
have shown any effect on global indices of neonatal well-being, it<br />
is instructive to note that when the fetus is most vulnerable (low<br />
SpO2), oxygen has its greatest possible beneficial effect.<br />
Adverse effects of oxygen are trivial<br />
Oxygen is one of the best tolerated drugs in our arsenal. In modern<br />
medicine, cost is not an issue (about a hundredth of a cent per liter,<br />
or less than a nickel a case!). Some women will complain of<br />
discom<strong>for</strong>t or claustrophobia while wearing a mask, but gentle<br />
reassurance, trimming the mask slightly, or substituting nasal prongs<br />
are effective ways to improve acceptance.<br />
Potentially more importantly, oxygen during cesarean section has<br />
been associated with increased levels of lipid peroxidation in the<br />
baby. 17-19 This work, done primarily by my opponent, has also<br />
demonstrated no improvement but also no deleterious effects on the<br />
fetus or neonate from maternal oxygen administration. This includes<br />
uterine artery <strong>and</strong> vein blood gases <strong>and</strong> Apgar scores. It has also<br />
been observed that babies resuscitated after birth with room air have<br />
continued on page 7
continued from page 6<br />
PRO CON<br />
better outcomes than those receiving oxygen. However, in this<br />
clinical situation, the fragile neonatal cardiorespiratory system is<br />
exposed to much higher concentrations of oxygen (<strong>and</strong> postive<br />
pressure ventilation) than the situation of the fetus exposed<br />
indirectly in utero.<br />
Conclusions<br />
Returning to the original syllogism, oxygen has been shown to have<br />
real benefits to some mothers <strong>and</strong> negligible risk to all mothers. The<br />
risks to the baby, if any, are largely theoretical. There<strong>for</strong>e, I argue<br />
that it should be routine in all cesarean sections.<br />
References<br />
1. Pan PH, Bogard TD, Owen MD. Incidence <strong>and</strong> characteristics<br />
of failures in obstetric neuraxial analgesia <strong>and</strong> anesthesia: a<br />
retrospective analysis of 19,259 deliveries. Int J Obstet Anesth<br />
2004;13:227-33.<br />
2. Craw<strong>for</strong>d JS. Some maternal complications of epidural<br />
analgesia <strong>for</strong> labour. Anaesthesia 1985;40:1219-25.<br />
3. Paech MJ, Godkin R, Webster S. Complications of obstetric<br />
epidural analgesia <strong>and</strong> anaesthesia: a prospective analysis of<br />
10,995 cases. Int J Obstet Anesth 1998;7:5-11.<br />
4. Irita K, Tsuzaki K, Sawa T et al. [Critical incidents due to drug<br />
administration error in the operating room: an analysis of<br />
4,291,925 anesthetics over a 4 year period]. Masui<br />
2004;53:577-84.<br />
5. Auroy Y, Benhamou D, Bargues L et al. Major complications of<br />
regional anesthesia in France: The SOS Regional <strong>Anesthesia</strong><br />
Hotline Service. Anesthesiology 2002;97:1274-80.<br />
6. Auroy Y, Narchi P, Messiah A et al. Serious complications<br />
related to regional anesthesia: results of a prospective survey in<br />
France. Anesthesiology 1997;87:479-86.<br />
7. Caplan RA, Ward RJ, Posner K, Cheney FW. Unexpected<br />
cardiac arrest during spinal anesthesia: a closed claims analysis<br />
of predisposing factors. Anesthesiology 1988;68:5-11.<br />
8. Dillon JB, Darsie ML. Oxygen <strong>for</strong> acute respiratory depression<br />
due to administration of thiopental sodium. J Am Med Assoc<br />
1955;159:1114-6.<br />
9. Weitzner SW, King BD, Ikezono E. The rate of arterial oxygen<br />
desaturation during apnea in humans. Anesthesiology<br />
1959;20:624-7.<br />
10. Heller ML, Watson TR, Jr. Polarographic study of arterial oxygenation<br />
during apnea in man. N Engl J Med 1961;264:326-30.<br />
11. Weiskopf RB, Feiner J, Hopf HW et al. Oxygen reverses<br />
deficits of cognitive function <strong>and</strong> memory <strong>and</strong> increased heart<br />
rate induced by acute severe isovolemic anemia.<br />
Anesthesiology 2002;96:871-7.<br />
12. Belda FJ, Aguilera L, Garcia de la Asuncion J et al.<br />
Supplemental perioperative oxygen <strong>and</strong> the risk of surgical<br />
wound infection: a r<strong>and</strong>omized controlled trial. Jama<br />
2005;294:2035-42.<br />
13. Greif R, Akca O, Horn EP et al. Supplemental perioperative<br />
oxygen to reduce the incidence of surgical-wound infection.<br />
Outcomes Research Group. N Engl J Med 2000;342:161-7.<br />
— 7—<br />
14. Ratra CK, Badola RP, Bhargava KP. A study of factors concerned<br />
in emesis during spinal anaesthesia. Br JAnaesth 1972;44:1208-11.<br />
15. Ramanathan S, G<strong>and</strong>hi S, Arismendy J et al. Oxygen transfer<br />
from mother to fetus during cesarean section under epidural<br />
anesthesia. Anesth Analg 1982;61:576-81.<br />
16. Simpson KR, James DC. Efficacy of intrauterine resuscitation<br />
techniques in improving fetal oxygen status during labor. Obstet<br />
Gynecol 2005;105:1362-8.<br />
17. Khaw KS, Ngan Kee WD, Lee A et al. Supplementary oxygen<br />
<strong>for</strong> elective Caesarean section under spinal anaesthesia: useful<br />
in prolonged uterine incision-to-delivery interval? Br J Anaesth<br />
2004;92:518-22.<br />
18. Khaw KS, Wang CC, Ngan Kee WD et al. Effects of high<br />
inspired oxygen fraction during elective caesarean section<br />
under spinal anaesthesia on maternal <strong>and</strong> fetal oxygenation <strong>and</strong><br />
lipid peroxidation. Br J Anaesth 2002;88:18-23.<br />
19. Ngan Kee WD, Khaw KS, Ma KC et al. R<strong>and</strong>omized, doubleblind<br />
comparison of different inspired oxygen fractions during<br />
general anaesthesia <strong>for</strong> Caesarean section. Br J Anaesth<br />
2002;89:556-61.<br />
CON<br />
Supplemental Oxygen Should Not Routinely Be Used<br />
During Cesarean Section<br />
Warwick D. Ngan Kee<br />
BHB, MBChB, MD. FANZCA, FHKCA, FHKAM<br />
Professor<br />
Department of Anaesthesia <strong>and</strong> Intensive Care<br />
The Chinese University of Hong Kong<br />
Hong Kong, China<br />
Introduction<br />
Based on historical recommendations, it is common <strong>for</strong> anesthesiologists<br />
to give supplemental oxygen to patients having cesarean<br />
section. However, after reviewing the evidence <strong>for</strong> its use, I stopped<br />
routinely giving supplemental oxygen during regional anesthesia<br />
many years ago. Here are the reasons why.<br />
Physiological considerations<br />
The human placenta is thought to function as a concurrent exchange<br />
system. Although this is relatively inefficient, many physiological<br />
adaptations have evolved to ensure adequate oxygen delivery to <strong>and</strong><br />
within the fetus. On the maternal side, unloading of oxygen in the<br />
placenta is facilitated by a rightward shift of the oxyhemoglobin<br />
dissociation curve secondary to increased levels of 2,3-DPG <strong>and</strong><br />
inward diffusion of fetal waste. On the fetal side, although umbilical<br />
venous (UV) PO2 values (typically around 28-30 mm Hg) are much<br />
lower than maternal arterial values, the fetus is well adapted to this.<br />
Adaptations include a high fetal hematocrit comprising mainly fetal<br />
hemoglobin which has high oxygen affinity, <strong>and</strong> a high fetal cardiac<br />
output. This ensures that the fetus is well oxygenated <strong>and</strong> thus<br />
attempts to increase fetal PO2 values above the normal physiological<br />
range are unnecessary.<br />
continued on page 8
continued from page 7<br />
PRO CON<br />
The rationale <strong>for</strong> giving supplemental oxygen<br />
Common reasons given <strong>for</strong> giving oxygen are to increase fetal<br />
oxygenation <strong>and</strong> to increase maternal safety in the event of<br />
hypotension or hypoventilation. In an early study of patients having<br />
epidural anesthesia it was demonstrated that administering<br />
increasing supplemental concentrations of oxygen to the mother<br />
(21%, 47%, 74% <strong>and</strong> 100%) resulted in proportional increases in<br />
UV <strong>and</strong> umbilical arterial (UA) PO2. 1 However, careful examination<br />
of the study methodology reveals that: 1) the oxygen was delivered<br />
at 10L/min via a circle system <strong>and</strong> an anesthesia facemask, a method<br />
unlikely to be used in clinical practice; 2) the UA <strong>and</strong> UV values<br />
attained were supranormal <strong>and</strong> thus of doubtful physiological<br />
benefit; <strong>and</strong> 3) there was no difference in clinical outcome between<br />
groups. More recently, Cogliano <strong>and</strong> colleagues evaluated<br />
supplemental oxygen during spinal anesthesia. Patients received<br />
either air by simple facemask, 4 L/min oxygen by simple facemask<br />
or 2 L/min oxygen by nasal cannulae. 2 They found no difference<br />
between groups in UA or UV PO2 suggesting that giving oxygen<br />
using methods that are most likely to be used in actual clinical<br />
practice have no significant impact on fetal oxygenation.<br />
It has been suggested that supplemental oxygen should be used<br />
because hypotension is common during spinal anesthesia. 3 However,<br />
it is more rational to treat hypotension directly; my recent work<br />
shows that this is achievable. 4<br />
Another suggested reason <strong>for</strong> giving supplemental oxygen is to<br />
mitigate the effects of spinal anesthesia on respiratory function.<br />
Kelly et al showed that spinal anesthesia decreased several measures<br />
of respiration function. 5 However, giving 35% oxygen versus air had<br />
no beneficial effect on UV PO2 or clinical outcome. Use of a pulse<br />
oximeter will readily identify patients who require oxygen because<br />
of impaired ventilatory function, obviating the need to take the<br />
“shotgun” approach of giving oxygen to every patient.<br />
A review article published more that 10 years ago suggested that<br />
increasing maternal oxygenation was useful to build up fetal PO2 as<br />
there is no oxygen transmission to the fetus after uterine incision. 6<br />
However, in a r<strong>and</strong>omized controlled trial, we were unable to shown<br />
any benefit of supplemental oxygen when the uterine-incision to<br />
delivery time was prolonged. 7 We have found that giving 60%<br />
oxygen during spinal anesthesia was effective in increasing UV<br />
PO2, 8 but values attained are greater than those measured in<br />
vigorous infant delivered vaginally. 9<br />
It may be thought useful to give oxygen during regional anesthesia<br />
to prepare <strong>for</strong> the (rare) event that urgent conversion to general<br />
anesthesia is required. However, time to achieve adequate<br />
denitrogenation of the lungs is unlikely to be significantly decreased<br />
by giving oxygen by simple facemask or nasal cannulae be<strong>for</strong>eh<strong>and</strong>.<br />
The potential benefit of supplemental oxygen during emergency<br />
cesarean section is less clear. Previously, we have found that<br />
administration of 60% oxygen using a tight fitting venturi mask<br />
during emergency spinal anesthesia did increase UV PO2 which<br />
— 8—<br />
provided a potentially useful increase in oxygen content in patients<br />
classified as urgent. 10 However, it should be pointed out that a<br />
concentration of 60% is unlikely to be achieved using simple masks<br />
<strong>and</strong> nasal cannulae <strong>and</strong> in our study there was no difference in<br />
clinical outcome, including Apgar scores <strong>and</strong> fetal acidosis between<br />
patients who received air or oxygen.<br />
Potential adverse effects of giving oxygen<br />
It is often intuitively assumed that giving oxygen might do some<br />
good but will not do harm. However, giving oxygen is not<br />
necessarily as innocuous as is commonly assumed.<br />
Application of an oxygen mask or nasal cannulae may be uncom<strong>for</strong>table<br />
<strong>and</strong> interfere with patient communication. Oxygen <strong>and</strong> the<br />
apparatus used to deliver it cost money. Hyperoxygenation has been<br />
shown to increase markers of oxygen free radical activity in both<br />
mother <strong>and</strong> fetus. 8 Although the clinical significance of this is<br />
undetermined, free radicals have been implicated in a number of<br />
important pathological processes. Use of the fresh gas flow outlet to<br />
administer supplemental oxygen during regional anesthesia has the<br />
potential risk of accidental volatile anesthetic administration <strong>and</strong><br />
failure of preoxygenation in a subsequent urgent case has been<br />
described because of failure to reconnect the fresh gas tubing. 11 Other<br />
evidence <strong>for</strong> potential harm of oxygen include a study that found lower<br />
fetal pH occurred when oxygen was given to mothers during the second<br />
stage of labor 12 <strong>and</strong> data suggesting that outcome during neonatal<br />
resuscitation may be better when air is used instead of oxygen. 13<br />
Conclusion<br />
There is no evidence <strong>for</strong> a clinically important benefit from giving<br />
routine supplemental oxygen to healthy patients during cesarean<br />
section. It should not be assumed that routine administration of<br />
oxygen is harmless. Use your clinical judgement – <strong>and</strong> your pulse<br />
oximeter – to identify the occasional patient who may benefit from<br />
oxygen. For the others, there is clearly no need.<br />
References<br />
1. Ramanathan S, G<strong>and</strong>hi S, Arismendy J, Chalon J, Turndorf H.<br />
Oxygen transfer from mother to fetus during cesarean section<br />
under epidural anesthesia. Anesth Analg 1982; 61: 576-81.<br />
2. Cogliano MS, Graham AC, Clark VA. Supplementary oxygen<br />
administration <strong>for</strong> elective Caesarean section under spinal<br />
anaesthesia. Anaesthesia 2002; 57: 66-9.<br />
3. M<strong>and</strong>al NG, Gulati A, Khaw KS, Ngan KW. Oxygen<br />
supplementation during Caesarean delivery. Br J Anaesth 2004;<br />
93: 469-70.<br />
4. Ngan Kee WD, Khaw KS, Ng FF. Prevention of hypotension<br />
during spinal anesthesia <strong>for</strong> cesarean delivery: an effective<br />
technique using combination phenylephrine infusion <strong>and</strong><br />
crystalloid cohydration. Anesthesiology 2005; 103: 744-50.<br />
5. Kelly MC, Fitzpatrick KT, Hill DA. Respiratory effects of spinal<br />
anaesthesia <strong>for</strong> caesarean section. Anaesthesia 1996; 51: 1120-2.<br />
6. Bassell GM, Marx GF. Optimization of fetal oxygenation. Int J<br />
Obstet Anesth 1995; 4: 238-43.<br />
continued on page 9
PRO CON<br />
continued from page 8<br />
7. Khaw KS, Ngan Kee WD, Lee A et al. Supplementary oxygen<br />
<strong>for</strong> elective Caesarean section under spinal anaesthesia: useful<br />
in prolonged uterine incision-to-delivery interval? Br J Anaesth<br />
2004; 92: 518-22.<br />
8. Khaw KS, Wang CC, Ngan Kee WD, Pang CP, Roger MS. Effects<br />
of high inspired oxygen fraction during elective Caesarean section<br />
under spinal anaesthesia on maternal <strong>and</strong> fetal oxygenation <strong>and</strong><br />
lipid peroxidation. Br J Anaesth 2002; 88: 18-23.<br />
9. Arikan GM, Scholz HS, Petru E, Haeusler MC, Haas J, Weiss<br />
PA. Cord blood oxygen saturation in vigorous infants at birth:<br />
what is normal? BJOG 2000; 107: 987-94.<br />
10. Khaw KS, Ngan Kee WD, Wang CC, Ng FF, Rogers MS.<br />
Supplementary oxygen <strong>for</strong> emergency cesarean section under<br />
regional anesthesia. Anesthesiology 2004; 101: A1229.<br />
11. Stone AG, Howell PR. Use of the common gas outlet <strong>for</strong> the<br />
administration of supplemental oxygen during Caesarean<br />
section under regional anaesthesia. Anaesthesia 2002; 57: 690-2.<br />
12. Thorp JA, Trobough T, Evans R, Hedrick J, Yeast JD. The effect<br />
of maternal oxygen administration during the second stage of<br />
labor on umbilical cord blood gas values: a r<strong>and</strong>omized<br />
controlled prospective trial. Am J Obstet Gynecol 1995; 172:<br />
465-74.<br />
13. Saugstad OD, Rootwelt T, Aalen O. Resuscitation of<br />
asphyxiated newborn infants with room air or oxygen: an<br />
international controlled trial: the Resair 2 study. Pediatrics<br />
1998; 102: e1.<br />
SOAP Future Meetings<br />
SOAP 39th Annual Meeting<br />
Fairmont Banff Springs<br />
“Castle in the Rockies”<br />
Alberta, Canada<br />
May 16 - 19, 2007<br />
SOAP 40th Annual Meeting<br />
Renaissance Chicago Hotel<br />
Chicago, IL<br />
April 30 - May 4, 2008<br />
SOAP 41st Annual Meeting<br />
Renaissance Washington DC Hotel<br />
Washington, DC<br />
April 29 - May 3, 2009<br />
SOAP 42nd Annual Meeting<br />
San Antonio, TX<br />
— 9—<br />
10 Reasons Why You Should Come to<br />
The 39th Annual Meeting in Banff<br />
1. To participate in a h<strong>and</strong>s-on state-of-the-art<br />
simulation session.<br />
2. To become certified in Neonatal Resuscitation <strong>and</strong><br />
learn about the new guidelines from AAP.<br />
3. To learn about what's going on in obstetric<br />
anesthesia in Japan.<br />
4. To discuss whether the seated position is optimal <strong>for</strong><br />
labor analgesia via neuraxial techniques.<br />
5. To discuss whether crew resource management is<br />
just a fad.<br />
6. To find out what JCAHO means <strong>for</strong> obstetric<br />
anesthesia.<br />
7. To debate whether ultrasound technologies should<br />
be used <strong>for</strong> neuraxial technique placements.<br />
8. To discuss if we can rationalize practice parameters<br />
to prevent neuraxial infection associated with<br />
regional anesthesia.<br />
9. To visit the not to be missed, one-of-a-kind, picture<br />
post card setting of Banff.<br />
10. To attend the many Social Events (details at<br />
www.soap.org)<br />
Getting to Banff:<br />
Air travel to Banff is via Calgary’s International Airport. SOAP has<br />
made special arrangements <strong>for</strong> discounted round-trip ground<br />
transportation from the Calgary Airport to Banff. This timesaving<br />
service is exclusively <strong>for</strong> SOAP participants. Registrants are<br />
encouraged to take advantage of this convenient transportation.<br />
In<strong>for</strong>mation is available on the SOAP web site <strong>and</strong> includes a link to<br />
Road West, here you can make your reservation:<br />
www.roadwest.com/soap<br />
Please inquire with the SOAP office<br />
to place your OB <strong>Anesthesia</strong><br />
job offerings on the SOAP website.<br />
Email: soaphq@soap.org
Make plans to attend the SOAP 39th<br />
Annual Meeting in Banff.<br />
Banff is truly a<br />
breathtaking location.<br />
Visit the hotel web site to view<br />
the slideshow <strong>and</strong> the hotel<br />
recreational activities.<br />
http://www.fairmont.com/banffsprings/<br />
• Bowling Center – Canadian 5-pin bowling<br />
• Pool Area – indoor <strong>and</strong> outdoor pools,<br />
whirlpool, children’s wading pool.<br />
• Mountain Biking – various tours available<br />
depending on your stamina - remember to<br />
bring your camera <strong>and</strong> binoculars.<br />
• Water Sports – canoeing, boat tours, boat<br />
rentals, chartered fishing trips, river float<br />
trips, whitewater rafting<br />
• Tennis – five supreme turf courts available<br />
• Coach Tours – four-hour bus tour of<br />
Banff to Lake Louise with stops along the<br />
way, Gondola rides atop Lake Sulphur,<br />
coach/boat combination tours,<br />
mountain/lake/waterfall tour<br />
• Horseback Riding – western-style trail rides<br />
depart from the Fairmont Banff Springs<br />
Corral (one <strong>and</strong> three-hour rides available)<br />
• Hiking - nature walks<br />
• Lake Louise Panorama Gondola - one<br />
hour west of Banff - spectacular views of<br />
Bow Valley from atop Lake Louise ski hill.<br />
Gondola ride available to Whitehorn Lodge<br />
Banff Surrounding Attractions:<br />
• Lake Louise<br />
• Johnston Canyon<br />
• Castle Mountain<br />
• Tunnel Mountain<br />
• Valley of the Ten Peaks<br />
• Mount Rundle, Vermillion Lake<br />
TOUR PACKAGE INFORMATION<br />
http://www.roadwest.com/soap<br />
Airport Transportation to <strong>and</strong> from<br />
Calgary International Airport to the<br />
Fairmont Banff Springs Hotel (round<br />
trip $60.00 USD) – info available at<br />
http://www.soap.org/meetings.htm<br />
SOAP Membership Committee Report<br />
SOAP is blessed with a remarkable membership. Annual meetings are a time not only<br />
to find out what’s new in obstetric anesthesia, but to catch up with colleagues <strong>and</strong><br />
friends. The Membership Committee is dedicated to pursue the issues that will improve<br />
<strong>and</strong> nurture our society.<br />
In the summer edition of our newsletter, Mike Smith wrote a summary of our<br />
membership survey. The majority of members were very satisfied with the<br />
organization. However, there was a relative paucity in “young” members. The<br />
Membership Committee decided its first priority to address the relatively low number<br />
of young <strong>and</strong> new graduate members. While there may be several factors hypothesized<br />
that may contribute to this discrepancy in SOAP, there was unanimous agreement that<br />
anesthesia residents should play a prominent role within our organization.<br />
The Membership Committee proposed an Ad hoc Residents Committee, which was<br />
approved by the Board of Directors. Dr. Joanne Hudson was elected chair <strong>and</strong> given<br />
the charge to organize the resident component of the <strong>Society</strong>. The mission of her<br />
committee is to promote resident interest in SOAP with the ultimate goal of retention<br />
of members in life <strong>and</strong> promotion of advanced training in obstetric anesthesia. Dr.<br />
Hudson is very dedicated to the cause <strong>and</strong> I believe there will be a substantial increase<br />
in resident members at SOAP. At the Annual Meeting we will identify residents with a<br />
designated name tag so that all members can make them feel welcome <strong>and</strong> included.<br />
The Membership Committee’s next goal was to identify resources which could be used<br />
to help <strong>and</strong> support SOAPers in their everyday practice. There was a wide range of<br />
requests from web based promotions; e.g. web blogs, bulletin boards, interesting case<br />
log, to more specific member benefits such as a journal. As with all requests financial<br />
considerations need to be assessed. Currently, the requests are being evaluated on a<br />
value <strong>for</strong> money basis. The membership committee members welcome your thoughts<br />
<strong>and</strong> ideas, either in person at Banff or via email vasdev.gurinder@mayo.edu.<br />
2006 has been a challenging year <strong>for</strong> funding <strong>for</strong> all physicians. For example, funding<br />
from the NIH has become increasingly difficult to obtain, with seasoned<br />
anesthesiologists either not receiving funding or requiring several revisions to achieve<br />
this goal. Looking at the NIH CRISP database <strong>for</strong> December 2006, there is a significant<br />
decrease in NIH funded studies <strong>for</strong> obstetrics <strong>and</strong> anesthesia. This may be a reflection<br />
of the research funding focused on basic sciences <strong>and</strong> genomics. FAER <strong>and</strong> OAPEF<br />
have supported obstetric anesthesia research <strong>and</strong> have provided starting <strong>and</strong> supporting<br />
grants <strong>for</strong> many. However, with the NIH decrease in funding, a rather discouraging<br />
environment <strong>for</strong> long-term academic support has been created. SOAP advocates<br />
excellence in research, <strong>and</strong> <strong>for</strong> those academics who will endure the hard times, I hope<br />
that SOAP will explore ways of supporting research until new funding opportunities<br />
arise. Attrition of seasoned investigators takes a considerable time to replace <strong>and</strong><br />
obstetric anesthesiologists run the risk of loosing new innovative ideas that will<br />
enhance patient care <strong>and</strong> safety.<br />
Sadly, my term as Chair of the Membership Committee comes to an end in 2007.<br />
SOAP Bylaws require the President to select the new committee chair. To avoid any<br />
conflict of interest, I have asked David Wlody to review potential c<strong>and</strong>idates <strong>and</strong> make<br />
a recommendation at the next board meeting. I have enjoyed my time as chair <strong>and</strong> look<br />
<strong>for</strong>ward to supporting the next chair enthusiastically.<br />
Gurinder M. Vasdev, MD<br />
Chair, Membership Committee<br />
SOAP<br />
— 10 —
SOAP Media Award<br />
The Publications Committee is soliciting nominations<br />
<strong>for</strong> the SOAP Media Award. The award will be given<br />
to a piece from the print or broadcast media that best<br />
represents the specialty of obstetric anesthesia to the<br />
general public. This award will be presented at the<br />
Annual Meeting. Please send your nominations via<br />
email to soaphq@soap.org.<br />
ASA/SOAP Abstract Submission<br />
The deadline to submit your abstracts <strong>for</strong> the ASA <strong>and</strong> SOAP Jointly<br />
Sponsored ASA 2007 Abstract Session is April 2, 2007.<br />
Additional in<strong>for</strong>mation available at: http://www.call4abstracts.com/asa<br />
Distinguished Service Award<br />
Nominations <strong>for</strong> the 2008 Distinguished Service Award<br />
are being solicited by the SOAP Board of Directors. The<br />
Board selects the recipient(s) based on the following<br />
criteria:<br />
• Has been a long-st<strong>and</strong>ing <strong>Society</strong> member<br />
• Has made numerous contributions to the <strong>Society</strong><br />
(i.e., served on the BOD, presented at Annual<br />
Meetings, served on <strong>Society</strong> committees)<br />
• Has provided exceptional service to the OB<br />
anesthesia specialty<br />
Nominations should be sent to soaphq@soap.org. The<br />
Board of Directors will select a recipient(s) during the<br />
next Board Meeting in Banff, Canada.<br />
Past Recipients:<br />
2000 - Gertie Marx 2003 - Brett Gutsche<br />
2001 - Mieczyslaw Finster 2004 - Sheila Cohen<br />
2002 - Robert Bauer 2005 - Frederick Zuspan<br />
Richard Clark, 2006 - Felicity Reynolds<br />
James Elam 2007 - Frank James<br />
James Evans<br />
Robert Hustead<br />
<strong>and</strong> Bradley Smith<br />
Miscellaneous Items<br />
— 11 —<br />
Use of SOAP Mailing List <strong>for</strong><br />
Surveys/Research<br />
Because of an increasing number of requests <strong>for</strong> the SOAP<br />
mailing list, the Board of Directors has established a<br />
protocol <strong>for</strong> requesting the official mailing list. As a<br />
benefit of SOAP membership, those conducting surveys<br />
or research studies may request the SOAP mailing list.<br />
Requirements are:<br />
1. Offered to SOAP Members in good st<strong>and</strong>ing.<br />
2. Mailing list <strong>for</strong> research use only.<br />
3. The research survey must be IRB approved at the<br />
primary investigator's institution.<br />
4. The survey <strong>and</strong> IRB approval letter must be<br />
submitted to SOAP Headquarters.<br />
5. The survey will then be reviewed by the SOAP<br />
Research Committee.<br />
A fee of $100 will be charged <strong>for</strong> this one-time<br />
distribution/use of the mailing list. Requests <strong>for</strong> followup<br />
surveys will be h<strong>and</strong>led on a case-by-case basis.<br />
(Note: No email addresses will be provided but, if<br />
preferred, the survey can be emailed from SOAP<br />
headquarters.)<br />
For additional in<strong>for</strong>mation contact:<br />
Robert D’Angelo, MD<br />
Chair, SOAP Research Committee<br />
rdangelo@wfubmc.edu<br />
or<br />
Submit your request to:<br />
Via Email: soaphq@soap.org<br />
Via Fax: 216-642-1127<br />
Via Mail: SOAP<br />
2 Summit Park Drive, Suite 140<br />
Clevel<strong>and</strong>, OH 44131
<strong>Society</strong> <strong>for</strong> <strong>Obstetric</strong> <strong>Anesthesia</strong> <strong>and</strong> Perinatology<br />
2006-2007 Board of Directors<br />
President<br />
David J. Wlody, MD<br />
New York, NY<br />
President-Elect<br />
Gurinder M. S. Vasdev, MD<br />
Rochester, MN<br />
First Vice President<br />
Linda S. Polley, MD<br />
Ann Arbor, MI<br />
Second Vice President<br />
Lawrence C. Tsen, MD<br />
Boston, MA<br />
Treasurer<br />
McCallum R. Hoyt, MD, MBA<br />
Greene, ME<br />
Secretary<br />
Brenda Bucklin, MD<br />
Denver, CO<br />
<strong>Society</strong> <strong>for</strong> <strong>Obstetric</strong> <strong>Anesthesia</strong> <strong>and</strong> Perinatology<br />
2 Summit Park Drive, Suite 140<br />
Clevel<strong>and</strong>, Ohio 44131<br />
Immediate Past President &<br />
Journal Liaison<br />
William R. Camann, MD<br />
Boston, MA<br />
Chair, ASA Committee on<br />
<strong>Obstetric</strong> <strong>Anesthesia</strong><br />
Samuel Hughes, MD<br />
San Francisco, CA<br />
<strong>Newsletter</strong> & Website Editor<br />
Michael P. Smith, MD, MS Ed.<br />
Clevel<strong>and</strong>, OH<br />
Meeting Hosts 2006<br />
David J. Birnbach, MD<br />
Miami, FL<br />
Jose Carvalho, MD, PhD, FRCPC<br />
Toronto, ON, Canada<br />
Meeting Host 2007<br />
Raouf Wahba, MD, FRCPC<br />
Calgary, AB, Canada<br />
— 12 —<br />
Meeting Host 2008<br />
Barbara Scavone, MD<br />
Chicago, IL<br />
Director at Large<br />
Rakesh B. Vadhera, MD, FRCA,<br />
FFARCSI<br />
Galveston, TX<br />
Representative,<br />
ASA House of Delegates<br />
Andrew P. Harris, MD, MHS<br />
Baltimore, MD<br />
ASA Alternate Delegate<br />
Richard N. Wissler, MD, PhD<br />
Rochester, NY