Ultrasonographic Cervical Length Assessment in Predicting ... - SOGC
Ultrasonographic Cervical Length Assessment in Predicting ... - SOGC
Ultrasonographic Cervical Length Assessment in Predicting ... - SOGC
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>SOGC</strong> CLINICAL PRACTICE GUIDELINE<br />
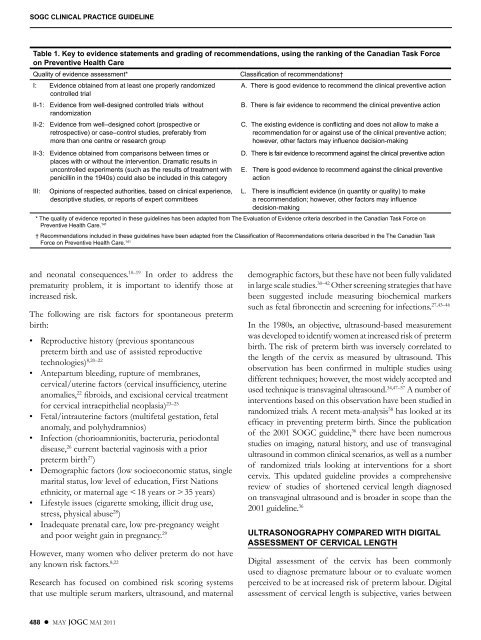
Table 1. Key to evidence statements and grad<strong>in</strong>g of recommendations, us<strong>in</strong>g the rank<strong>in</strong>g of the Canadian Task Force<br />
on Preventive Health Care<br />
Quality of evidence assessment* Classification of recommendations†<br />
I: Evidence obta<strong>in</strong>ed from at least one properly randomized A . There is good evidence to recommend the cl<strong>in</strong>ical preventive action<br />
controlled trial<br />
II-1: Evidence from well-designed controlled trials without<br />
B . There is fair evidence to recommend the cl<strong>in</strong>ical preventive action<br />
randomization<br />
II-2: Evidence from well–designed cohort (prospective or<br />
retrospective) or case–control studies, preferably from<br />
more than one centre or research group<br />
II-3: Evidence obta<strong>in</strong>ed from comparisons between times or<br />
places with or without the <strong>in</strong>tervention . Dramatic results <strong>in</strong><br />
uncontrolled experiments (such as the results of treatment with<br />
penicill<strong>in</strong> <strong>in</strong> the 1940s) could also be <strong>in</strong>cluded <strong>in</strong> this category<br />
III: Op<strong>in</strong>ions of respected authorities, based on cl<strong>in</strong>ical experience,<br />
descriptive studies, or reports of expert committees<br />
and neonatal consequences. 10–19 In order to address the<br />
prematurity problem, it is important to identify those at<br />
<strong>in</strong>creased risk.<br />
The follow<strong>in</strong>g are risk factors for spontaneous preterm<br />
birth:<br />
• Reproductive history (previous spontaneous<br />
preterm birth and use of assisted reproductive<br />
technologies) 8,20–22<br />
• Antepartum bleed<strong>in</strong>g, rupture of membranes,<br />
cervical/uter<strong>in</strong>e factors (cervical <strong>in</strong>sufficiency, uter<strong>in</strong>e<br />
anomalies, 22 fibroids, and excisional cervical treatment<br />
for cervical <strong>in</strong>traepithelial neoplasia) 23–25<br />
• Fetal/<strong>in</strong>trauter<strong>in</strong>e factors (multifetal gestation, fetal<br />
anomaly, and polyhydramnios)<br />
• Infection (chorioamnionitis, bacteruria, periodontal<br />
disease, 26 current bacterial vag<strong>in</strong>osis with a prior<br />
preterm birth27 )<br />
• Demographic factors (low socioeconomic status, s<strong>in</strong>gle<br />
marital status, low level of education, First Nations<br />
ethnicity, or maternal age < 18 years or > 35 years)<br />
• Lifestyle issues (cigarette smok<strong>in</strong>g, illicit drug use,<br />
stress, physical abuse28 )<br />
• Inadequate prenatal care, low pre-pregnancy weight<br />
and poor weight ga<strong>in</strong> <strong>in</strong> pregnancy. 29<br />
However, many women who deliver preterm do not have<br />
any known risk factors. 8,22<br />
Research has focused on comb<strong>in</strong>ed risk scor<strong>in</strong>g systems<br />
that use multiple serum markers, ultrasound, and maternal<br />
488 l MAY JOGC MAI 2011<br />
C . The exist<strong>in</strong>g evidence is conflict<strong>in</strong>g and does not allow to make a<br />
recommendation for or aga<strong>in</strong>st use of the cl<strong>in</strong>ical preventive action;<br />
however, other factors may <strong>in</strong>fluence decision-mak<strong>in</strong>g<br />
D . There is fair evidence to recommend aga<strong>in</strong>st the cl<strong>in</strong>ical preventive action<br />
E . There is good evidence to recommend aga<strong>in</strong>st the cl<strong>in</strong>ical preventive<br />
action<br />
L . There is <strong>in</strong>sufficient evidence (<strong>in</strong> quantity or quality) to make<br />
a recommendation; however, other factors may <strong>in</strong>fluence<br />
decision-mak<strong>in</strong>g<br />
* The quality of evidence reported <strong>in</strong> these guidel<strong>in</strong>es has been adapted from The Evaluation of Evidence criteria described <strong>in</strong> the Canadian Task Force on<br />
Preventive Health Care . 141<br />
† Recommendations <strong>in</strong>cluded <strong>in</strong> these guidel<strong>in</strong>es have been adapted from the Classification of Recommendations criteria described <strong>in</strong> the The Canadian Task<br />
Force on Preventive Health Care . 141<br />
demographic factors, but these have not been fully validated<br />
<strong>in</strong> large scale studies. 30–42 Other screen<strong>in</strong>g strategies that have<br />
been suggested <strong>in</strong>clude measur<strong>in</strong>g biochemical markers<br />
such as fetal fibronect<strong>in</strong> and screen<strong>in</strong>g for <strong>in</strong>fections. 27,43–46<br />
In the 1980s, an objective, ultrasound-based measurement<br />
was developed to identify women at <strong>in</strong>creased risk of preterm<br />
birth. The risk of preterm birth was <strong>in</strong>versely correlated to<br />
the length of the cervix as measured by ultrasound. This<br />
observation has been confirmed <strong>in</strong> multiple studies us<strong>in</strong>g<br />
different techniques; however, the most widely accepted and<br />
used technique is transvag<strong>in</strong>al ultrasound. 34,47–57 A number of<br />
<strong>in</strong>terventions based on this observation have been studied <strong>in</strong><br />
randomized trials. A recent meta-analysis 58 has looked at its<br />
efficacy <strong>in</strong> prevent<strong>in</strong>g preterm birth. S<strong>in</strong>ce the publication<br />
of the 2001 <strong>SOGC</strong> guidel<strong>in</strong>e, 36 there have been numerous<br />
studies on imag<strong>in</strong>g, natural history, and use of transvag<strong>in</strong>al<br />
ultrasound <strong>in</strong> common cl<strong>in</strong>ical scenarios, as well as a number<br />
of randomized trials look<strong>in</strong>g at <strong>in</strong>terventions for a short<br />
cervix. This updated guidel<strong>in</strong>e provides a comprehensive<br />
review of studies of shortened cervical length diagnosed<br />
on transvag<strong>in</strong>al ultrasound and is broader <strong>in</strong> scope than the<br />
2001 guidel<strong>in</strong>e. 36<br />
ULTRASONOGRAPHY COMPARED WITH DIGITAL<br />
ASSESSMENT OF CERVICAL LENGTH<br />
Digital assessment of the cervix has been commonly<br />
used to diagnose premature labour or to evaluate women<br />
perceived to be at <strong>in</strong>creased risk of preterm labour. Digital<br />
assessment of cervical length is subjective, varies between