ADCS-ADL Scale, Scoring and Manual - Dementia Outcomes ...
ADCS-ADL Scale, Scoring and Manual - Dementia Outcomes ...
ADCS-ADL Scale, Scoring and Manual - Dementia Outcomes ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
@]<br />
Alzheimer's Disease<br />
Cooperative Study<br />
~@mJl]~~@ (g@~@ ~@~@[J11 [P@[JmJl]<br />
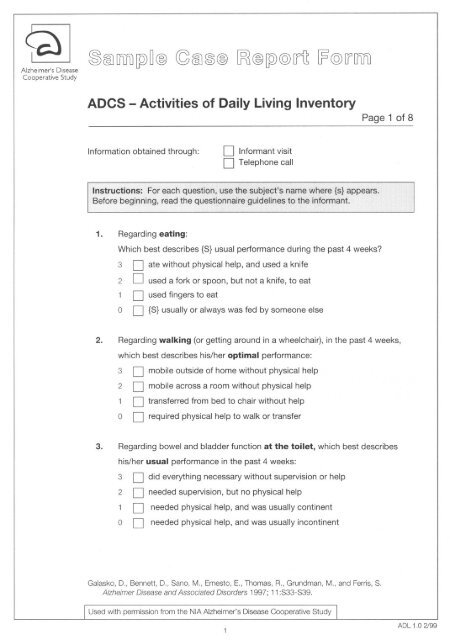
<strong>ADCS</strong> - Activities of Daily Living Inventory Page 1 of 8<br />
Informationobtained through: 0 Informant visit<br />
0 Telephone call<br />
1. Regardingeating:<br />
Which best describes {S} usual performanceduring the past 4 weeks?<br />
3 0 ate without physical help, <strong>and</strong> used a knife<br />
20 used a fork or spoon, but not a knife, to eat<br />
10<br />
00<br />
used fingers to eat<br />
{S} usually or always was fed by someone else<br />
2. Regardingwalking (or getting around in a wheelchair), in the past 4 weeks,<br />
which best describes his/her optimal performance:<br />
3 0 mobile outside of home without physical help<br />
2 0 mobile across a room without physical help<br />
1 0 transferred from bed to chair without help<br />
0 0 required physical help to walk or transfer<br />
3. Regarding bowel <strong>and</strong> bladder function at the toilet, which best describes<br />
his/her usual performance in the past 4 weeks:<br />
3 0 did everything necessary without supervision or help<br />
2 0 needed supervision, but no physical help<br />
1 0 needed physical help, <strong>and</strong> was usually continent<br />
0 0 needed physical help, <strong>and</strong> was usually incontinent<br />
Galasko, D., Bennett, D., Sano, M., Ernesto, E., Thomas, R., Grundman, M., <strong>and</strong> Ferris, S.<br />
Alzheimer Disease <strong>and</strong> Associated Disorders 1997; 11:S33-S39.<br />
Used with permission from the NIA Alzheimer's Disease Cooperative Study<br />
<strong>ADL</strong> 1 .0 2/99
@] .@CID [j[Jj) [j2) ~ @ ~ CID<br />
Alzheimer's Disease<br />
Cooperative Study<br />
Yes No<br />
Don't<br />
Know 6.<br />
l<br />
D<br />
0<br />
D<br />
0<br />
~<br />
@ !JB @ [j2) @ [f It [F @ [f [j[Jj)<br />
<strong>ADCS</strong> - Activities of Daily Living Inventory Page 2 of 8<br />
4. Regardingbathing, in the past 4 weeks, which best describes his/her usual<br />
performance:<br />
3 D bathed without reminding or physical help<br />
2 D no physical help, but needed supervision/reminders to bathe completely<br />
1 D needed minor physical help (e.g., with washing hair) to bathe completely<br />
0 D needed to be bathed completely<br />
5. Regardinggrooming£ in the past 4 weeks, which best describes his/her optimal<br />
performance:<br />
3<br />
2<br />
1<br />
0<br />
D cleaned <strong>and</strong> cut fingernails without physical help<br />
D brushed or combed hair without physical help<br />
D kept face <strong>and</strong> h<strong>and</strong>s clean without physical help<br />
D needed help for grooming of hair, face, h<strong>and</strong>s, <strong>and</strong> fingernails<br />
Regarding dressing, in the past 4 weeks:<br />
A) Did {S} select his/her first set of clothes for the day?<br />
If yes, which best describes his/her usual performance:<br />
~ 3 D without supervision or help<br />
2 D with supervision<br />
1 D with physical help<br />
B) Regarding physically getting dressed, which best describes his/her usual<br />
performance in the past 4 weeks:<br />
4 D dressed completely without supervision or physical help<br />
3 D dressed completely with supervision, but without help<br />
2 D needed physical help only for buttons, clasps, or shoelaces<br />
1 D dressed without help if clothes needed no fastening or buttoning<br />
0 D always needed help, regardless of the type of clothing<br />
2<br />
<strong>ADL</strong> 1.0 2/99
@]<br />
Alzheimer's Disease<br />
Cooperative Study<br />
Yes<br />
L<br />
Yes<br />
L<br />
No<br />
Don't<br />
Know<br />
0<br />
0<br />
0<br />
0<br />
Don't<br />
Yes No Know<br />
1<br />
0 0<br />
0 0<br />
01 01 0<br />
0<br />
0<br />
0<br />
01 0 0<br />
No<br />
Don't<br />
Know<br />
0<br />
0<br />
0<br />
0<br />
~@)ITlfl)~~@(G@)~@ [pJ@~@[f11[P@[fITlfl)<br />
<strong>ADCS</strong> - Activities of Daily Living Inventory<br />
7. In the past 4 weeks, did {8} use a telephone?<br />
8.<br />
Don't<br />
Yes No Know 9.<br />
0 0<br />
0 0<br />
If yes, which best describes his/her highest level of performance:<br />
Page 3 of 8<br />
;:. 5 D made calls after looking up numbers in white or yellow pages, or by<br />
4<br />
3<br />
2<br />
1<br />
dialing directory assistance<br />
D made calls only to well-known numbers, without referring to a directory<br />
or list<br />
D made calls only to well-known numbers, by using a directory or list<br />
D answered the phone; did not make calls<br />
D did not answer the phone, but spoke when put on the line<br />
In the past 4 weeks, did {8} watch television?<br />
If yes, ask all questions:<br />
Did (8):<br />
a) usually select or ask for different programs or his/her favorite show?<br />
b) usually talk about the content of a program while watching it?<br />
c) talk about the content of a program within a day (24 hours) after watching it?<br />
In the past 4 weeks, did {8} ever appear to pay attention to conversation or small<br />
talk for at least 5 minutes?<br />
Note: {5} did not need to initiate the conversation.<br />
If yes, which best describes his/her usual degree of participation:<br />
3 D usually said things that were related to the topic<br />
2 D usually said things that were not related to the topic<br />
1 D rarely or never spoke<br />
10. Did {8} clear the dishes from the table after a meal or snack?<br />
If yes, which best describes how he/she usually performed:<br />
;:. 3 D without supervision or help<br />
2 D with supervision<br />
1 D with physical help<br />
3<br />
<strong>ADL</strong> 1.0 2/99
~<br />
Alzheimer's Disease<br />
Cooperative Study<br />
Yes<br />
Yes<br />
Yes<br />
Don't<br />
~@mru[9)~@ (g@~@ [g1@[9)@[{lt ~@[{mru<br />
<strong>ADCS</strong> - Activities of Daily Living Inventory Page 4 of 8<br />
No<br />
D<br />
0<br />
Know<br />
D<br />
0<br />
11. In the past 4 weeks, did {S} usually manage to find his/her personal belongings at<br />
home?<br />
If yes, which best describes how he/she usually performed:<br />
Don't<br />
No Know<br />
D D 12.<br />
0<br />
~ 0<br />
Yes<br />
Don't<br />
No Know 13.<br />
D D<br />
Don't<br />
No Know 14<br />
D D .<br />
0<br />
0<br />
0<br />
0<br />
3 D without supervision or help<br />
2 D with supervision<br />
1 D with physical help<br />
In the past 4 weeks, did {S} obtain a hot or cold beverage for him/herself?<br />
(A cold beverage includes a glass of water.)<br />
If yes, which describes his/her highest level of performance<br />
3 D made a hot beverage, usually without physical help<br />
2 D made a hot beverage, usually if someone else heated the water<br />
1 D obtained a cold beverage, usually without physical help<br />
In the past 4 weeks, did {S} make him/herself a meal or snack at home?<br />
If yes, which best describes his/her highest level of food preparation:<br />
~ 4 D cooked or microwavedfood, with little or no help<br />
3 D cooked or microwaved food, with extensive help<br />
2 D mixed or combined food items for a meal or snack, without cooking or<br />
microwaving (e.g., made a s<strong>and</strong>wich)<br />
1 D obtained food on his/her own, without mixing or cooking it<br />
In the past 4 weeks, did {S} dispose of garbage or litter in an appropriate place<br />
or container at home?<br />
If yes, which best describes how he/she usually<br />
3 D without supervision or help<br />
2 D with supervision<br />
1 D with physical help<br />
4<br />
performed:<br />
<strong>ADL</strong> 1.0 2/99
@]<br />
Alzheimer's Disease<br />
Cooperative Study<br />
Yes<br />
L<br />
Yes<br />
D 1<br />
Yes<br />
Don't<br />
No Know 15.<br />
D D<br />
0 0<br />
Don't<br />
No Know 16.<br />
D D<br />
0 0<br />
D 0<br />
D 0<br />
Don't<br />
No Know 17.<br />
D D<br />
0 0<br />
~@lmru~~@(g@l~@ [Ri@~@[fli ~@[fmru<br />
<strong>ADCS</strong> - Activities of Daily Living Inventory Page 5 of 8<br />
In the past 4 weeks, did {S} get around (or travel) outside of his/her home?<br />
If yes, which best describes his/her optimal performance:<br />
;.. 4 D alone, went at least 1 mile away from home<br />
3 D alone, but remained within 1 mile of home<br />
2 D only when accompanied <strong>and</strong> supervised, regardless of the trip<br />
1 D only with physical help, regardlessof the trip<br />
In the past 4 weeks, did {S} ever go shopping?<br />
If yes, ask A <strong>and</strong> B:<br />
A) Which one best describes how {S} usually selects items:<br />
3 D without supervision or physical help?<br />
2 D with some supervision or physical help?<br />
1 D not at all, or selected mainly r<strong>and</strong>om or inappropriate items?<br />
B) Did {S} usually ~ for items without supervision or physical help?<br />
In the past 4 weeks, did {S} keep appointments or meetings with other people,<br />
such as relatives, a doctor, the hairdresser, etc.?<br />
If yes, which best describes his/her awareness of the meeting ahead of time:<br />
3 D usually remembered, may have needed written reminders<br />
e.g. notes, a diary, or calendar<br />
2 D only remembered the appointment after verbal reminders on the day<br />
1 D usually did not remember, in spite of verbal reminders on the day<br />
5<br />
<strong>ADL</strong> 1.0 2/99
@]<br />
Alzheimer's Disease<br />
Cooperative Study<br />
Yes No<br />
Don't<br />
Know 18.<br />
0 0<br />
? D D<br />
D D D<br />
1 0 0<br />
D D D<br />
1 0 0<br />
D D D<br />
1 0 0<br />
D 1 D 0 D 0<br />
D 1 D 0 D 0<br />
Don't<br />
Yes No Know 19.<br />
D D<br />
0 0<br />
D D D<br />
1 0 0<br />
D D D<br />
1 0 0<br />
D D D<br />
1 0 0<br />
Don't<br />
Yes No Know<br />
D D 20.<br />
0 0<br />
~@QVi)~~@ (Q;@~@ ~@~@[f11 ~@[fQVi)<br />
<strong>ADCS</strong> - Activities of Daily Living Inventory Page 6 of 8<br />
In the past 4 weeks, was {S} ever left on his/her own?<br />
If yes, ask all questions:<br />
Was {S} left:<br />
a) away from home, for 15 minutes or longer, during the day?<br />
b) at home, for an hour or longer, during the day?<br />
c) at home, for less than 1 hour, during the day?<br />
In the past 4 weeks, did {S} talk about current events? (This means events or<br />
incidents that occurred during the past month.)<br />
If yes, ask all questions:<br />
Did {S} talk about events that...:<br />
a) he/she heard or read about or saw on TV but did not take part in?<br />
b) he/she took part in outside home involving family, friends, or neighbors?<br />
c) events that occurred at home that he/she took part in or watched?<br />
In the past 4 weeks, did {S} read a magazine. newspaper or book for more than 5<br />
minutes at a time?<br />
If yes, ask all questions:<br />
Did {S} usually:<br />
a) talk about details of what he/she read while or shortly<br />
« than 1 hour) after reading?<br />
b) talk about what he/she read 1 hour or longer after reading?<br />
6<br />
<strong>ADL</strong> 1.0 2/99
~ ~@J[ffi1)~~@(g@J~@ [Ri@~@[flt[P@[f[ffi1)<br />
Alzheimer's Disease<br />
Cooperative Study<br />
Yes<br />
Yes<br />
No<br />
Don't<br />
Know<br />
D<br />
0<br />
D<br />
0<br />
Don't<br />
No Know 22.<br />
D D<br />
0 0<br />
<strong>ADCS</strong> - Activities of Daily Living Inventory Page 7 of 8<br />
21. In the past 4 weeks, did {S} ever write things down?<br />
Note: If {S} wrote things only after encouragement or with help, the response<br />
should still be 'yes.'<br />
If yes, which best describes the most complicated things that he/she wrote:<br />
3 D letters or long notes that other people understood<br />
2 D short notes or messages that other people understood<br />
1 D his/her signature or name<br />
In the past 4 weeks, did {S} perform a pastime. hobby or game?<br />
If yes, which pastimes did he/she perform:<br />
Ask about all of the following, check all that apply:<br />
D card or board games (including bridge, chess, checkers)<br />
D bingo D crosswords Dart<br />
D musical instrument D knitting D sewing<br />
Dreading D gardening D golf<br />
D tennis<br />
D other<br />
D workshop D fishing<br />
Note: Walking does NOT count as a hobby/pastime for this scale.<br />
D If {S} performs hobbies/pastimes only at day care, check here.<br />
If yes, how did {S} usually perform his/her most common pastimes:<br />
3 D without supervision or help<br />
2 D with supervision<br />
1 D with help<br />
7<br />
<strong>ADL</strong> 1 .0 2/99
@I ~@)M~~@ ~@)~@ [Ri@~@[f1t [F@[fM<br />
Alzheimer's Disease<br />
Cooperative Study<br />
Yes No<br />
Don't<br />
Know<br />
D<br />
0<br />
D<br />
0<br />
L<br />
<strong>ADCS</strong> - Activities of Daily Living Inventory Page 8 of 8<br />
23. In the past 4 weeks, did {S} use a household appliance to do chores?<br />
~ Ask about all of the following, <strong>and</strong> check those that were used:<br />
D washer D dryer D vacuum<br />
D dishwasher D toaster D toaster oven<br />
D range D microwave D food processor<br />
D other<br />
If yes, for the most commonly used appliances, which best describes how {S}<br />
usually used them:<br />
4 D without help, operating more than on-off controls if needed<br />
3 D without help, but operated only on/off controls<br />
2 D with supervision, but no physical help<br />
1 D with physical help<br />
LU Total Score (0-78)<br />
LU Number of "Don't Know" Responses<br />
8<br />
<strong>ADL</strong>1.0 2/99
1.1-'<br />
<strong>ADCS</strong> - ACTIVITIES OF DAILY LIVING (<strong>ADL</strong>) INVENTORY<br />
NOTES: (1) {P} refers to the participant <strong>and</strong> should be replaced by the participant's<br />
name or relationship to the study partner each time an <strong>ADL</strong> question<br />
is asked of the study partner.<br />
(2) This <strong>ADL</strong> inventory must be given in the format of an interview of the<br />
study partner, either directly or by telephone. The form should NOT be<br />
given to a study partner to complete on his/her own.<br />
READ THE FOllOWING INSTRUCTIONS TO THE STUDY PARTNER:<br />
I am goingto ask you about a numberof daily activitiesthat {P} may have performed<br />
duringthe past4 weeks. Pleasetell me about{P}'s actual performance,not aboutwhat<br />
he/shecould havedone if an opportunityhad arisen. For each activitythat {P}<br />
attempted,I'm going to ask you to chooseone out of a numberof descriptionsthat best<br />
fits his/her most usual performance.<br />
For some activities, I'll ask about whether {P} performed independently, or with<br />
supervision or help. Let me explain how we are defining these words:<br />
Independently means that {P} completed the activity without being helped. We still<br />
consider it independent if {P} was reminded or prompted to get started, or<br />
received a little prompting while performing the activity.<br />
With supervision means that {P} required verbal reminders <strong>and</strong> instructions while<br />
doing the activity.<br />
With help means that {P} was given some degree of ~ assistance by another<br />
person to perform the activity.<br />
INSTRUCTIONS FOR THE RATER:<br />
If the study partner states that {P} had no opportunity to perform the task during the past<br />
four weeks (e.g., {P} did not have access to a telephone, therefore could not possibly<br />
make phone calls), the response should be recorded as 'no.'<br />
If either the study partner's answer or the questionnaire are unclear, please make notes<br />
on the case report form detailing the problem.<br />
For questions regarding specific <strong>ADL</strong> items, please refer to the <strong>ADL</strong> Response Card.<br />
I-I
<strong>ADCS</strong> - Activitiesof Daily Living<br />
(<strong>ADL</strong>) Inventory<br />
A. General Remarks<br />
There are widely varying ways to carry<br />
out <strong>ADL</strong>, especially Instrumental <strong>ADL</strong>.<br />
This leads to difficulty when trying to<br />
obtain <strong>ADL</strong> ratings from an informant in a<br />
st<strong>and</strong>ardized way for a clinical trial. The<br />
<strong>ADCS</strong> - <strong>ADL</strong> Inventory approaches the<br />
problem by offering detailed descriptions<br />
of each activity, <strong>and</strong> by asking the<br />
informant to describe observed actions or<br />
behaviors. The informant is asked to<br />
focus on the past 4 weeks. The informant<br />
must not estimate what the patient might<br />
be able to do had an opportunity arisen,<br />
but on what the patient actually did. The<br />
informant should not try to interpret the<br />
patient's thought processes or intentions.<br />
To help the informant to remain focused<br />
on observed actions <strong>and</strong> behavior during<br />
the past 4 weeks, it may be useful to ask<br />
him/her for examples of what the patient<br />
did regarding the <strong>ADL</strong> in question.<br />
B. Administering the <strong>ADCS</strong> - <strong>ADL</strong><br />
Inventory<br />
The <strong>ADCS</strong> - <strong>ADL</strong> Inventory was developed<br />
<strong>and</strong> tested as an interview administered<br />
by a rater in person or by telephone.<br />
It should not be filled out by the<br />
informant.<br />
C. Format of Questions<br />
. For each basic<strong>ADL</strong> (questions 1-5,<br />
6A), there is a forced choice of best<br />
response.<br />
. All other <strong>ADL</strong> consist of a main<br />
.<br />
question followed by subquestions<br />
(descriptors) .<br />
Subquestions are arranged in<br />
hierarchical fashion, starting with the<br />
highest (most independent) level of<br />
.<br />
.<br />
.<br />
<strong>ADL</strong> performance <strong>and</strong> ending with<br />
the lowest.<br />
For each <strong>ADL</strong>, the initial response to<br />
the main questions is "yes", "no" or<br />
"don't know". If an informant gives 4<br />
or more "don't know" responses, it is<br />
worth trying to identify an alternative<br />
informant.<br />
After a "no" or "don't know" response,<br />
the subquestions are<br />
disregarded unless specific instructions<br />
indicate otherwise. "No" or<br />
"don't know" act as fast forward cues<br />
to proceed to the next <strong>ADL</strong>.<br />
After a "yes" response, there are 2<br />
possible paths:<br />
1. From several descriptors, the<br />
informant chooses the one that best<br />
matches the patient's performance<br />
(e.g., question 6A). The informant<br />
should be offered as many descriptors<br />
as necessary to describe the<br />
patient's <strong>ADL</strong> ability, starting from the<br />
highest level <strong>and</strong> proceeding downwards<br />
or<br />
2. The informant makes a "yes" or<br />
"no" choice for each subquestion.<br />
There is a reminder in these cases to<br />
ask every question after an initial<br />
"yes" (e.g., question 8).<br />
D. St<strong>and</strong>ardizing "independently",<br />
"with supervision",<br />
<strong>and</strong> "with help"<br />
For many <strong>ADL</strong>, the hierarchy depends on<br />
how much intervention is needed by the<br />
informant or others to enable the patient<br />
to perform the <strong>ADL</strong>.<br />
Independently = the patient completed<br />
the <strong>ADL</strong> without physical help, <strong>and</strong> at<br />
most with reminders to do the task, or a<br />
brief prompt during the <strong>ADL</strong>.
<strong>ADL</strong><br />
With supervision = the patient required<br />
verbal reminders <strong>and</strong> instructions while<br />
doing the <strong>ADL</strong>; this occupied the<br />
caregiver's (or informant's) time.<br />
With help = the patient was given some<br />
degree of physical assistance by another<br />
person to perform the <strong>ADL</strong>.<br />
E. "Usual" performance of <strong>ADL</strong><br />
Patients may vary from day to day in their<br />
<strong>ADL</strong> performance. If an informant<br />
responds that a patient sometimes<br />
performs <strong>ADL</strong> at one level <strong>and</strong> sometimes<br />
at another, the interviewer should<br />
ask him/her to choose the most com-<br />
monly applicable level/descriptor.<br />
When In doubt about a higher or lower<br />
level of ability, rate the higher one if the<br />
patient does manage to perform at that<br />
level fairly consistently.<br />
F. Comments on specific questions<br />
in the Inventory<br />
1. Eating: self-explanatory<br />
2. Walking: we are interested in mobility,<br />
not specifically walking. If the patient<br />
used a walker or wheelchair, but was<br />
mobile outside of home without help, he/<br />
she is independent.<br />
3. Toileting: self-explanatory<br />
4. Bathing: minor physical help includes<br />
actions such as washing hair, help with<br />
drying, running the water or adjusting its<br />
temperature. More extensive help should<br />
be scored as needing to be bathed.<br />
5. Grooming: toenail cutting is not rated<br />
since physical difficulty may impede this<br />
aspect of grooming, even in cognitively<br />
normal elderly.<br />
6A. "Selecting" clothes impliesactive<br />
participationbythe patient.This may<br />
involve physically selecting clothes, or<br />
providing input to the caregiver about<br />
wishes or preferences. It is rated separately<br />
from physically getting dressed.<br />
68. Dressing: the 3rd <strong>and</strong> 4th levels are<br />
similar. The intention is that "help only for<br />
buttons, clasps or shoelaces" implies<br />
only a minor contribution from the<br />
caregiver, i.e., the patient performs some<br />
degree of fastening, zipping or tying.<br />
Using "clothes needing no fastening or<br />
buttoning" implies that these have been<br />
completely ab<strong>and</strong>oned. Velcro counts as<br />
a fastener.<br />
7. Telephone: reminders or supervision<br />
are allowable but not help, e.g., a patient<br />
can be prompted to dial directory assistance,<br />
or told the number <strong>and</strong> still score<br />
at the highest level. If the patient makes<br />
calls only if the numbers are dictated by<br />
the caregiver, or if the telephone is set up<br />
to automatically dial one of a preselected<br />
group of numbers on pressing a single<br />
button, the patient scores 2 points.<br />
8. Television: if the patient sits in front<br />
of a television screen without demon-<br />
strating awareness or recollection of<br />
something he/she sees, then all<br />
subquestions will be answered as "no".<br />
"Talk about the content of a program"<br />
should be interpreted fairly broadly; the<br />
patient does not need to initiate the<br />
conversation, but should require more<br />
than a "yes" or "no" answer to a question<br />
like "Did vou enjoy the program?"<br />
9. Conversation: "paid attention"<br />
implies more than being present <strong>and</strong><br />
seemingly alert during a conversation.<br />
The patient must participate verbally.<br />
Since it is difficult to judge whether<br />
nonverbal participation in a conversation<br />
is meaningful, it is not an option among<br />
the descriptors.<br />
10. Clear dishes from a table: the<br />
patient does not have to clear the table<br />
entirely, but should participate enouQ,hto
<strong>ADL</strong><br />
make a useful contribution. Clearing<br />
items other than dishes e.g., glasses or<br />
utensils are acceptable as alternatives.<br />
11. Finds personal belongings: it may<br />
be helpfulto give examplessuch as<br />
clothing,glasses,wallet, keys,etc.<br />
12. Beverage: gettingor preparinga<br />
beverageafter instructionsor a remindercounts<br />
as no physical help.<br />
13. Mealor snack: if the patient<br />
required supervision to cook or microwave,<br />
but functioned without physical<br />
help, score as the highest level. Mixing<br />
or combining items without cooking can<br />
also include supervision. An example of<br />
the lowest level of a "yes" response is<br />
the patient who finds <strong>and</strong> eats food preprepared<br />
by someone else.<br />
14. Dispose of garbage or litter: does<br />
not only refer to major household<br />
garbage produced in a kitchen. Disposing<br />
of any trash in an appropriate<br />
container qualifies for a "yes" response.<br />
15. Travel: intended to cover the<br />
patient's ability to remain oriented, not<br />
get lost <strong>and</strong> be able to venture beyond<br />
home. It does not matter whether the<br />
patient walked, drove, took public<br />
transport or was a passenger in a car.<br />
The distance of 1 mile is arbitrary <strong>and</strong><br />
implies travel beyond sight of home.<br />
16. Shopping: shopping is a complex<br />
activity. We have focused on the two<br />
most essential aspects (after getting to<br />
the shop, covered by question 15),<br />
choosing items <strong>and</strong> paying. If the patient<br />
goes shopping with a prewritten list <strong>and</strong><br />
a sum of money provided by someone<br />
else, that should be scored as without<br />
supervision, provided the patient<br />
selected the items on the list. Paying for<br />
items could involve cash, check or<br />
credit; the issue is whether supervision<br />
or help is needed.<br />
17. Keep appointments or meetings:<br />
mainly aimed at monitoring memory. An<br />
"appointment/meeting" may be liberally<br />
interpreted to include almost any kind of<br />
preplanned meeting, outing or excursion.<br />
It does not matter who made the appointment<br />
or whether the patient traveled<br />
alone or with somebody else. The highest<br />
level implies the patient remembered the<br />
appointment on his/her own, memory<br />
aids are acceptable.<br />
18. Left alone: if the patient was left<br />
alone for an hour or longer at home, then<br />
they automatically will score a "yes" for<br />
descriptor c, "less than 1 hour at home."<br />
19. Talk about current events: the<br />
patient does not need to initiate conversation<br />
about current events, but must<br />
demonstrate awareness or recollection<br />
by providing details of the event(s).<br />
Merely agreeing or disagreeing with other<br />
people by saying "yes or "no" is not<br />
sufficient to display knowledge/recall of<br />
current events. Patients who are severely<br />
aphasic will score "no" for talking about<br />
current events.<br />
20. Reading: looking at a book, magazine<br />
or newspaper <strong>and</strong> turning the pages<br />
for more than 5 minutes on end may<br />
equal reading. Unless the patient communicates<br />
the content of what he/she<br />
reads to someone else, it is not possible<br />
to judge whether he/she actually reads or<br />
not, in a way that shows elements of<br />
comprehension <strong>and</strong> retention of information.<br />
The informant should be encouraged<br />
to interact with the patient to be<br />
able to make an accurate judgment.<br />
21. Writing: short notes or messages<br />
can be either spontaneous or written to<br />
dictation. A shopping list, "to do" list, or<br />
taking an intelligible telephone message<br />
would qualify.<br />
22. Pastime, hobbl.2!.Same: the
<strong>ADL</strong><br />
menu of hobbies or games is to help the<br />
informant <strong>and</strong> may provide us with<br />
secondary information if complex hobbies<br />
are lost <strong>and</strong> replaced by simpler ones. A<br />
hobby should involve element(s) of<br />
concentration, knowledge <strong>and</strong> memory,<br />
<strong>and</strong> manual skills. If hobbies other than<br />
those in the menu are offered, try to<br />
describe what the patient does in some<br />
detail so that we can monitor this.<br />
23. Household appliance: an appliance<br />
is defined as a device with one or<br />
more switches or controls, usually<br />
(though not necessarily) with an electrical<br />
or other power source, used to do<br />
chores. For men, tools with controls or<br />
switches would qualify, but not a screwdriver,<br />
hammer or saw. Again, if the<br />
patient needs only minimal verbal<br />
prompting to operate the appliance,<br />
press a switch, or operate a control, the<br />
highest level is scored.
Alzheimer Disease <strong>and</strong> Associated Disorders<br />
Vol. 11, Suppl. 2, S33-S39<br />
@ 1997 Lippincott-Raven Publishers, Philadelphia<br />
An Inventory to Assess Activities of Daily Living for Clinical<br />
Trials in Alzheimer's Disease<br />
)<br />
Douglas Galasko, *David Bennett, tMary Sano, Chris Emesto, Ronald Thomas,<br />
Michael Grundman, :j:Steven Ferris, <strong>and</strong> the Alzheimer's Disease Cooperative Study<br />
Department of Neurosciences (Neurology), University of California, San Diego, California; *Rush Alzheimer's Disease Center<br />
<strong>and</strong> Department of Neurological Sciences, Rush-Presbyterian-St. Lukes Medical Center, Chicago, Illinois; tDepartment of<br />
Neurology, Columbia University <strong>and</strong> the Sergievsky Center, New York, New York; <strong>and</strong> :j:Departmentof Psychiatry, New York<br />
University Medical Center, New York, New York, u.S.A.<br />
Summary: We developed a set of infonnant-based items describing perfonnance of<br />
activities of daily living (<strong>ADL</strong>) by patients with Alzheimer's disease (AD) to identify<br />
which <strong>ADL</strong> are useful for assessment of patients in clinical trials. Evaluation of <strong>ADL</strong><br />
is an important outcome measure in AD clinical trials. For clinical trial measurement,<br />
<strong>ADL</strong> should have broad applicability, good test-retest reliability, scaling to cover a<br />
range of perfonnance, <strong>and</strong> sensitivy to detect change in disease progression. A total of<br />
45 <strong>ADL</strong> items developed from literature review <strong>and</strong> clinical experience were administered<br />
to informants of 242 AD patients <strong>and</strong> 64 elderly controls as part of the multicenter<br />
Alzheimer's Disease Cooperative Study Instrument protocol. Half of the subjects<br />
were re-evaluated at 1 <strong>and</strong> 2 months <strong>and</strong> all at 6 <strong>and</strong> 12 months. Controls<br />
performed virtually all <strong>ADL</strong> items optimally at baseline <strong>and</strong> at 12 months. Among<br />
subjects with AD, 27 of the 45 <strong>ADL</strong> were widely applicable, i.e., performed at baseline<br />
or premorbidly by >90% of subjects; showed good test-retest reliability between<br />
baseline <strong>and</strong> 1 <strong>and</strong> 2 months; correlated with MMSE scores of AD patients crosssectionally;<br />
<strong>and</strong> showed a decline in performance from baseline to 12months in at least<br />
20% of AD patients. <strong>ADL</strong> could be identified that capture change in functional ability<br />
in patients across the entire range of the MMSE. The remaining 18 <strong>ADL</strong> included<br />
several that may be useful for trials that target specific populations, e.g., women with<br />
AD. Because change on specific items depends on baseline MMSE, <strong>ADL</strong> evaluation<br />
should include items relevant to the severity of dementia of patients enrolled in a<br />
clinical trial. Key Words: Alzheimer's disease-Activities of daily living-Clinical<br />
trials-Patient assessment.<br />
Functional assessment of patients with Alzheimer's<br />
disease (AD), in terms of performance of activities of<br />
daily living (<strong>ADL</strong>), is a critical element in patient care.<br />
For investigational drug studies, changes in <strong>ADL</strong> performance<br />
can be used as a secondary outcome measure to<br />
document that cognitive or other effects of an anti-AD<br />
Address correspondence <strong>and</strong> reprint requests to Dr. D. Galasko at<br />
Neurology V127, VA Medical Center, 3350 La Jolla Village Drive, San<br />
Diego CA 92161, U.S.A. (The Inventory of <strong>ADL</strong> <strong>and</strong> an accompanying<br />
manual are available on request from Dr. Galasko.)<br />
drug are clinically relevant. Treatment that enhances<br />
cognitive function should lead to improvement in performance<br />
of <strong>ADL</strong>, whereas treatment that slows the progression<br />
or delays the onset of AD should be associated<br />
with preservation or slower deterioration of <strong>ADL</strong> performance.<br />
Although scores of <strong>ADL</strong> scales <strong>and</strong> cognitive tests are<br />
correlated in patients with AD (Pfeffer et aI., 1982; Vitaliano<br />
et aI., 1984), <strong>ADL</strong> performance also depends on<br />
factors such as sustained attention, motivation, <strong>and</strong> motor<br />
performance. It is difficult to predict from overall
S34 D. GALASKO ET AL.<br />
cognitive test scores or even from tests of specific cognitive<br />
domains which <strong>ADL</strong> are likely to be impaired or<br />
how severe the impairment will be (Loewenstein et aI.,<br />
1992). The amount of cognitive change needed to produce<br />
a change in <strong>ADL</strong> performance is unknown.<br />
<strong>ADL</strong> evaluation for clinical trials is an understudied<br />
area. Most <strong>ADL</strong> scales were developed for general geriatric<br />
assessment <strong>and</strong> to help determine the need for<br />
services, <strong>and</strong> focus on basic activities such as walking,<br />
feeding, <strong>and</strong> toileting (Katz et aI., 1963; Lawton et aI.,<br />
1969). A few scales, such as those of Blessed (Blessed et<br />
aI., 1968), Lawton (Lawton et aI., 1969), Pfeffer (Pfeffer<br />
et aI., 1982), Weintraub (Weintraub, 1986), <strong>and</strong> the<br />
NOSGER (Spiegel et aI., 1991) were introduced for geriatric<br />
assessment or for clinical evaluation of patients<br />
with AD, <strong>and</strong> include items that assess more complicated<br />
activities (instrumental <strong>ADL</strong>, I<strong>ADL</strong>). Some of these<br />
scales contain gender-specific items or items performed<br />
at infrequent intervals, such as filling out forms or documents.<br />
Others ask whether a subject "can" perform an<br />
<strong>ADL</strong> rather than relying on purely observed activities,<br />
which introduces judgment or opinion into the informant's<br />
report. Several scales combine both <strong>ADL</strong> <strong>and</strong><br />
behavioral information (Blessed et aI., 1968; Spiegel et<br />
aI., 1991). Many I<strong>ADL</strong> show a floor effect in AD, i.e.,<br />
patients lose I<strong>ADL</strong> very early in the course of dementia,<br />
whereas basic <strong>ADL</strong> show a ceiling effect, with normal<br />
performance until late in the course of AD (Spector et aI.,<br />
1978). The approach of using loss of <strong>ADL</strong> or I<strong>ADL</strong> as<br />
milestones (Galasko et aI., 1995) is similar to that of the<br />
Functional Assessment <strong>Scale</strong> (Reisberg, 1988) <strong>and</strong> is<br />
best suited to clinical studies with long follow-up periods.<br />
Performance <strong>ADL</strong> (P<strong>ADL</strong>) scales require subjects to<br />
perform <strong>ADL</strong> tasks in a structured setting using props<br />
(Loewenstein et aI., 1992). <strong>Scoring</strong> is st<strong>and</strong>ardized <strong>and</strong><br />
can capture elements of performance such as sequencing,<br />
initiation, <strong>and</strong> motivation. However, P<strong>ADL</strong> scales cover<br />
a relatively small number of activities, are timeconsuming,<br />
<strong>and</strong> do not evaluate performance in the subjects'<br />
own home environments. In view of the limitations<br />
of existing instruments for use in clinical trials, the Alzheimer's<br />
Disease Cooperative Study (<strong>ADCS</strong>) developed<br />
a set of informant-based <strong>ADL</strong>.<br />
METHODS<br />
Development of the Inventory<br />
A subcommittee of the <strong>ADCS</strong>, composed of clinicians<br />
with expertise in dementia assessment <strong>and</strong> clinical trials,<br />
developed an inventory comprising a wide range of<br />
<strong>ADL</strong>. The initial item pool consisted of activities that<br />
Alzheimer Disease <strong>and</strong> Associated Disorders, Vol. 11, Suppl. 2, 1997<br />
normal elderly individuals regularly perform <strong>and</strong> that<br />
were likely to be relevant to patients with AD over a<br />
broad range of severity of dementia. The inventory included<br />
<strong>ADL</strong> from existing scales <strong>and</strong> novel items based<br />
on clinical experience, i.e., <strong>ADL</strong> necessary for personal<br />
care, communicating <strong>and</strong> interacting with other people,<br />
maintaining a household, conducting hobbies <strong>and</strong> interests,<br />
<strong>and</strong> making judgments <strong>and</strong> decisions.<br />
For each <strong>ADL</strong>, an informant is first asked whether or<br />
not the patient attempted the activity during the past 4<br />
weeks. If a patient did attempt the <strong>ADL</strong>, the informant is<br />
asked to choose the single most accurate definition of the<br />
patient's level of performance from a set of descriptions<br />
of alternative methods of carrying out the <strong>ADL</strong>. For<br />
<strong>ADL</strong> in which different methods of performance do not<br />
apply, the informant is asked whether the subject usually<br />
carried out the <strong>ADL</strong> "independently" (the highest<br />
level), "with supervision" (needing verbal instructions<br />
during <strong>ADL</strong> performance, an intermediate level of ability),<br />
or "with physical help" (a lower level of performance).<br />
If a subject needed reminders to get started but<br />
then performed an <strong>ADL</strong> independently <strong>and</strong> successfully,<br />
that is rated as independently. These definitions of levels<br />
of independence are explained to informants before the<br />
inventory is administered. To verify that nonperformance<br />
of <strong>ADL</strong> was due to loss of ability, for each <strong>ADL</strong> that was<br />
not attempted during the 4-week period, informants were<br />
asked whether or not patients performed the activity<br />
premorbidly.<br />
The <strong>ADL</strong> questions were pretested at three sites,<br />
modified where necessary to enhance their clarity,<br />
<strong>and</strong> an inventory of 45 <strong>ADL</strong> was administered to AD<br />
patients <strong>and</strong> controls as part of an <strong>ADCS</strong> multicenter<br />
study.<br />
Subjects<br />
The <strong>ADCS</strong> study of instrument development for AD<br />
clinical trials enrolled elderly controls (n = 64; 24 men<br />
<strong>and</strong> 40 women) <strong>and</strong> subjects with AD (242 AD patients;<br />
94 men <strong>and</strong> 148 women) as described (Ferris et aI., this<br />
issue). Recruitment of subjects with AD was stratified by<br />
Mini-Mental State Examination (MMSE; Folstein et aI.,<br />
1975) scores at baseline, <strong>and</strong> all were communitydwelling<br />
at the time of enrollment in the study. All subjects<br />
were evaluated at baseline <strong>and</strong> at 6 <strong>and</strong> 12 months,<br />
<strong>and</strong> half of the subjects were evaluated at 1 <strong>and</strong> 2<br />
months. The present study made use of data at baseline,<br />
1, 2, <strong>and</strong> 12 months.<br />
Procedures<br />
For each AD patient, an informant who spent at least<br />
2 days per week with the patient was identified <strong>and</strong> in-
terviewed with the <strong>ADL</strong> Inventory. Controls acted as<br />
their own informants. <strong>ADL</strong> interviews were conducted in<br />
person at baseline. To increase follow-up participation, if<br />
informants were unable to travel to a center's clinic site,<br />
interviews were conducted by telephone. A representative<br />
from each participating center attended a training<br />
se~sion at which use of the inventory was described, <strong>and</strong><br />
ea~h site received a procedural manual describing each<br />
question in the <strong>ADL</strong> Inventory. The personnel who carried<br />
out <strong>ADL</strong> interviews were psychometrists or clinicians<br />
with experience in assessment of patients with AD.<br />
The <strong>ADL</strong> Inventory took from 30 to 45 min to administer.<br />
Data Analysis<br />
Data were analyzed using SPSS (version 6.1). We<br />
used several criteria to determine which <strong>ADL</strong> in the inventory<br />
were likely to be best suited for use in monitoring<br />
patients in clinical trials. These included wide applicability,<br />
good test-retest reliability, ability of the <strong>ADL</strong> to<br />
show stepwise scaling <strong>and</strong> to correlate with dementia<br />
severity, <strong>and</strong> decline of <strong>ADL</strong> performance in an appreciable<br />
percentage of patients with AD over 12 months<br />
(Feinstein et aI., 1986; Streiner <strong>and</strong> Norman, 1995). Applicability<br />
was measured as the percentage of subjects<br />
who attempted each <strong>ADL</strong> at baseline, or premorbidly in<br />
the case of AD patients who did not attempt specific<br />
<strong>ADL</strong>. As an index of short-term (test-retest) reliability<br />
for each <strong>ADL</strong>, the extent of agreement between ratings at<br />
baseline, one <strong>and</strong> two months was calculated using a K<br />
statistic (O'Connell <strong>and</strong> Dobson, 1984). To determine<br />
whether the levels of performing each <strong>ADL</strong> related to<br />
dementia severity, we compared MMSE scores between<br />
patients who carried out the <strong>ADL</strong> in each specified manner<br />
at baseline by ANOVA. If MMSE scores of patients<br />
performing an <strong>ADL</strong> at different descriptors or "levels"<br />
of <strong>ADL</strong> performance did not differ significantly (p<br />
S36 D. GALASKO ET AL.<br />
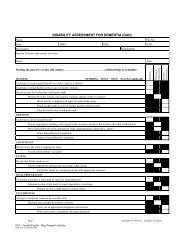
TABLE 1. Metric properties of selected <strong>ADL</strong> Inventory questions in patients with AD<br />
Applicability: % of subjects Change at 12 months:<br />
attempting <strong>ADL</strong> at baseline<br />
Test-retest Correlation<br />
% of subjects who declined on <strong>ADL</strong><br />
<strong>ADL</strong> question<br />
(number of levelst Overall<br />
By MMSE stratab<br />
>20 16 10 5 0<br />
reliability<br />
(K)<br />
with MMSE<br />
(Spearman R) Overall >20<br />
By MMSE stratab<br />
16 10 5 0<br />
H<strong>and</strong>les mail (3) 30 1 1 I 0.41* 0.50** 22 .. .. 0 0<br />
Discusses current events (4) 44 . 1 1 0.51* 0.48** 30 .. .. . 0<br />
Makes a snack or meal (5) 50 . 1 1 I 0.62* 0.55** 30 0 .. .. 0<br />
Writes note/letter/name (4) 51 . 1 1 I 0.59* 0.57** 33 0 .. .. .. 0<br />
Uses household appliance (4)C 53 . 1 1 1 0.62* 0.61** 34 0 .. .. .. 0<br />
Reads(4) 54 . 1 1 1 0.45* 0.56** 30 .. .. .. .. 0<br />
Hobby/pastime/game (3r 56 . 1 1 1 I 0.59* 0.44** 29 0 0 .. .. 0<br />
Chooses clothes to wear (3Y 56 . 1 1 I 0.59* 0.54** 36 0 .. .. .. 0<br />
Turns off lights (2) 60 . 1 1 1 I 0.61* 0.44** 24 0 0 .. .. 0<br />
Puts away belongings (4)C 61 . 1 1 1 I 0.45* 0.46** 35 0 .. .. .. 0<br />
Can be left alone (4) 62 . 1 . 1 0.52* 0.55** 35 .. .. . .. 0<br />
Goes shopping (3) 63 . 1 . 1 I 0.48* 0.47** 36 .. .. .. .. ..<br />
Keeps appointments (4) 70 . 1 . 1 1 0.46* 0.44** 35 0 0 .. .. .<br />
Obtainsa beverage(5) 70 . . . 1 I 0.54* 0.61** 40 .. . . .. 0<br />
Finds belongings (3)C 71 . . 1 1 I 0.40* 0.42** 37 0 .. .. .. ..<br />
Clears a table (4)C 71 . 1 . 1 1 0.60* 0.45** 32 0 0 .. .. ..<br />
Disposes of litter (4)C 73 . . . 1 1 0.43* 0.49** 35 0 .. .. .. ..<br />
Makes conversation (4) 75 . 1 1 1 1 0.41* 0.40** 35 0 0 .. .. ..<br />
Grooms(5) 75 . . . 1 I 0.55* 0.64** 35 0 .. . 0<br />
Gets dressed (5) 75 . . . 1 I 0.55* 0.66** 42 0 . . . 0<br />
Bathes(5) 77 . . . 1 I 0.73* 0.66** 40 0 .. .. . ..<br />
Uses a telephone (4) 80 . . . 1 1 0.50* 0.70** 47 .. . . . ..<br />
Travelsoutsidehome(5) 90 . . . . . 0.59* 0.50** 44 .. 0 .. .. ..<br />
Watches TV (5) 92 . . . . . 0.45* 0.44** 34 .. .. .. . ..<br />
Toileting(4) 92 . . . . . 0.66* 0.61** 37 0 .. . .<br />
Walking(5) 97 . . . . . 0.45* 0.28** 14 0 0 0<br />
Eating(5) 97 . . . . . 0.60* 0.55** 30 0 .. . .<br />
a <strong>ADL</strong> are arranged in ascending order according to the overall percentage of patients with AD who attempted the <strong>ADL</strong> at baseline.<br />
b MMSE strata are as follows: >20, 20-28 points; 16,16-20; 10, 10-15; 5, 5-9; 0, 0-4. Symbols indicate the percentage of subjects in MMSE strata<br />
who attempted each <strong>ADL</strong> at baseline: . >80%; 161-80%; 141-60%; 121-40%; blank 0-20%. Symbols for the percentage of subjects who declined<br />
at 12 months are as follows: . 50%; .. 30-49%; 0 10-29%; blank 0-9%.<br />
C <strong>ADL</strong> descriptorshad the format "independently,""with supervision,"or "with physicalhelp." All other <strong>ADL</strong> had specificallyworded<br />
descriptors of different levels of <strong>ADL</strong> performance.<br />
* p < 0.01; **p < 0.001.<br />
baseline, a floor effect that renders it unsuitable for a<br />
general-purpose <strong>ADL</strong> scale.<br />
We next examined short-term (test-retest) reliability,<br />
using K statistics to assess the extent to which ratings of<br />
performance of each <strong>ADL</strong> item agreed at baseline <strong>and</strong> at<br />
I <strong>and</strong> 2 months. Over 2 months, the progression of AD<br />
should not be great enough to lead to a change in <strong>ADL</strong><br />
performance. In general, KSfell into the 0.4-0.75 range,<br />
indicating moderate to very good agreement. Among<br />
<strong>ADL</strong> with the highest KS were activities whose ratings<br />
were dichotomous (yes or no) <strong>and</strong> the traditional basic<br />
<strong>ADL</strong>. Several items, i.e., cleaning up spills, being aware<br />
of toileting needs, <strong>and</strong> participating in a group event had<br />
low KS «0.4, indicating only fair agreement) <strong>and</strong> were<br />
eliminated from contention.<br />
Stepwise scaling of levels of <strong>ADL</strong> performance <strong>and</strong><br />
correlation with dementia severity was the next criterion.<br />
Tables I <strong>and</strong> 2 include the number of levels specified for<br />
Alzheimer Disease <strong>and</strong> Associated Disorders, Vol. 11, Suppl. 2, 1997<br />
each <strong>ADL</strong> in the inventory; an <strong>ADL</strong> question with a<br />
dichotomous (yes or no) response has two levels, while<br />
one that can be performed independently, with supervision,<br />
with some physical help, or not at all has four. To<br />
determine whether these levels have hierarchical properties,<br />
we first examined the MMSE scores of patients who<br />
performed each <strong>ADL</strong> at each specified level at baseline.<br />
As an example, MMSE scores for levels of using a telephone<br />
are displayed in Fig. 1. For most <strong>ADL</strong>, as each<br />
level indicated less independent or less complex <strong>ADL</strong><br />
performance, the MMSE scores showed a pattern of progressive<br />
decrease. If two descriptors of an <strong>ADL</strong> corresponded<br />
to a similar range <strong>and</strong> distribution of MMSE<br />
scores, then the descriptors were assumed to represent<br />
cognitively equivalent levels of the <strong>ADL</strong>. This suggested<br />
that the pair of descriptors could be merged <strong>and</strong> performance<br />
of that <strong>ADL</strong> could be adequately described using<br />
one level less. This situation arose very infrequently,
<strong>ADL</strong> INVENTORY S37<br />
a <strong>ADL</strong> descriptors had the format "independently," "with supervision," or "with physical help." All other <strong>ADL</strong> had specifically worded<br />
descriptors of different levels of <strong>ADL</strong> performance.<br />
b Sev: impaired performance was noted only in severely demented patients.<br />
almost exclusively for the descriptors that indicated<br />
minimal performance of the <strong>ADL</strong> (e.g., "with help<br />
only") <strong>and</strong> complete loss of the <strong>ADL</strong>.<br />
To analyze scaling further, we calculated the Spearman<br />
rank-order correlation coefficients between levels of<br />
<strong>ADL</strong> performance <strong>and</strong> dementia severity, as indexed by<br />
30<br />
20<br />
~<br />
(IJ<br />
::E<br />
::E 10<br />
TABLE 2. <strong>ADL</strong> with properties that did not meet specified criteria for assessment of <strong>ADL</strong> in clinical trials<br />
Not attempted<br />
S38 D. GALASKO ET AL.<br />
patients with mild dementia (MMSE >20), to ensure that<br />
change was adequately captured in that subgroup of patients.<br />
Among the AD cohort overall, 12 <strong>ADL</strong> were relatively<br />
insensitive to decline at 12 months, as listed in<br />
Table 2. Although the rating of walking ability did not<br />
meet this criterion, it is included in Table 1 because of its<br />
traditional use as a fundamental basic <strong>ADL</strong>.<br />
We next examined the relationship between baseline<br />
MMSE severity stratum <strong>and</strong> the number of <strong>ADL</strong> items<br />
(from the 27 in Table 1) on which subjects showed decline<br />
of performance at 12 months (Fig. 2). Note that<br />
subjects with AD in every MMSE stratum showed decline<br />
on <strong>ADL</strong>, but subjects with moderate cognitive impairment<br />
at baseline (MMSE 5-20) declined on more<br />
<strong>ADL</strong> than did those with mild or very severe impairment.<br />
Items Less Suited for <strong>ADL</strong> Assessment in a<br />
Clinical Trial<br />
Table 2 lists the <strong>ADL</strong> that failed to meet one or more<br />
criteria. The most common problems with <strong>ADL</strong> in this<br />
group were lack of wide applicability (usually due to a<br />
gender effect), poor scaling, e.g., low correlation with<br />
dementia severity, little change over 12 months, <strong>and</strong><br />
change restricted to severely demented patients only.<br />
Most of these <strong>ADL</strong> had good reliability, <strong>and</strong> several of<br />
the items in Table 2 would be suitable for use in customized<br />
<strong>ADL</strong> scales for a clinical trial that targets<br />
women, or for a study of severely impaired patients.<br />
DISCUSSION<br />
Many <strong>ADL</strong> items were widely applicable, had good<br />
test-retest reliability, correlated significantly with the extent<br />
of cognitive impairment in AD as measured by the<br />
MMSE, <strong>and</strong> showed decline in performance in a significant<br />
percentage of AD subjects at 12 months. These<br />
properties indicate that they should prove valuable for<br />
rating functional ability in AD clinical trials. The finding<br />
that over one-third of the <strong>ADL</strong> failed to meet one or more<br />
of these criteria illustrates the problems inherent in mea-<br />
'" 0)<br />
.S<br />
U<br />
0)<br />
'"<br />
25<br />
20<br />
-B<br />
is<br />
15<br />
....<br />
0....<br />
10<br />
0)<br />
Z<br />
5<br />
0<br />
Controls 21 - 30 16- 20 10- 15 5-9<br />
Baseline MMSE group for subjects with AD<br />
Alzheimer Disease <strong>and</strong> Associated Disorders, Vol. 11, Suppl. 2, 1997<br />
0-4<br />
suring <strong>ADL</strong> in a spectrum of patients with AD who are<br />
typically the subject of clinical trials.<br />
Most of the items showed good test-retest reliability<br />
over 1-2 months, which presumably was aided by pretesting<br />
the items to improve their clarity, conducting a<br />
brief training session, distributing a procedures manual,<br />
<strong>and</strong> specifying the amount of contact an informant had to<br />
have with the patient. It is difficult to obtain consistent<br />
ratings of intermediate levels of <strong>ADL</strong> performance, especially<br />
when <strong>ADL</strong> have many potential levels or methods<br />
of performance, even when these are specified as<br />
carefully as possible. To improve test-retest reliability, it<br />
may be necessary to improve the specific descriptors of<br />
levels of performance, to collapse levels of performance<br />
on some <strong>ADL</strong>, <strong>and</strong> to provide additional training to raters.<br />
The validity of informant-derived descriptions of <strong>ADL</strong><br />
ability is difficult to establish directly. Observation of<br />
subjects at home or in the community would be ideal but<br />
is not practical. As a substitute, we estimated concurrent<br />
validity of <strong>ADL</strong> reports by comparing <strong>ADL</strong> ability with<br />
cognitive performance <strong>and</strong> found a substantial crosssectional<br />
correlation between <strong>ADL</strong> performance <strong>and</strong><br />
MMSE scores for most items. Longitudinal decline on<br />
many <strong>ADL</strong> items over 1 year among subjects with AD is<br />
consistent with decline on cognitive <strong>and</strong> global measures<br />
(Ferris et aI., 1997, this issue) <strong>and</strong> provides a further<br />
indication of validity.<br />
The optimal <strong>ADL</strong> performance by controls in this<br />
study needs to be qualified. Among an elderly control<br />
population, one would typically expect some degree of<br />
<strong>ADL</strong> impairment as a result of physical disability, impaired<br />
special senses, or medical illness. The controls in<br />
this study were judged to be cognitively normal, <strong>and</strong><br />
represent high-functioning individuals living independently<br />
in the community. Their results are therefore consistent<br />
with expectations for a group of very healthy<br />
elderly individuals but do not necessarily extrapolate to<br />
the elderly in general, or to the "oldest old."<br />
The large number of items in the <strong>ADL</strong> Inventory al-<br />
FIG. 2. Number of <strong>ADL</strong> items in the Inventory (from<br />
the 27 listed in Table 1) on which subjects with AD<br />
showed decline in performance at 12 months. The box<br />
plot shows the 25th, 50th (median), <strong>and</strong> 75th percentiles<br />
as well as 95% limits for the total number of <strong>ADL</strong> on<br />
which subjects in each MSE stratum declined.