review on common root canal irrigants - Dharmsinh Desai University
review on common root canal irrigants - Dharmsinh Desai University
review on common root canal irrigants - Dharmsinh Desai University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
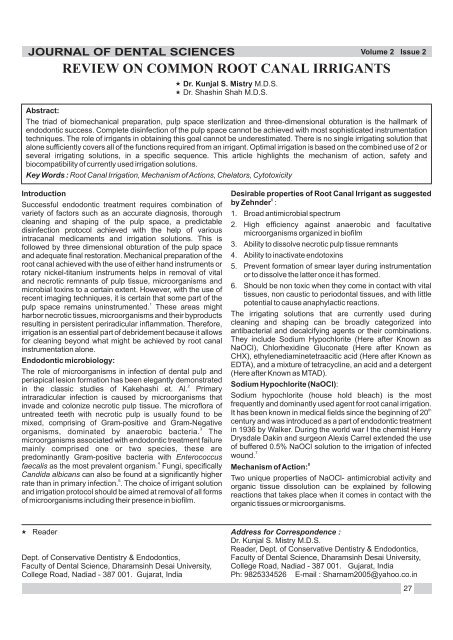
JOURNAL OF DENTAL SCIENCES<br />
Abstract:<br />
Reader<br />
REVIEW ON COMMON ROOT CANAL IRRIGANTS<br />
Dept. of C<strong>on</strong>servative Dentistry & Endod<strong>on</strong>tics,<br />
Faculty of Dental Science, Dharamsinh <strong>Desai</strong> <strong>University</strong>,<br />
College Road, Nadiad - 387 001. Gujarat, India<br />
Dr. Kunjal S. Mistry M.D.S.<br />
Dr. Shashin Shah M.D.S.<br />
Volume 2 Issue 2<br />
The triad of biomechanical preparati<strong>on</strong>, pulp space sterilizati<strong>on</strong> and three-dimensi<strong>on</strong>al obturati<strong>on</strong> is the hallmark of<br />
endod<strong>on</strong>tic success. Complete disinfecti<strong>on</strong> of the pulp space cannot be achieved with most sophisticated instrumentati<strong>on</strong><br />
techniques. The role of <strong>irrigants</strong> in obtaining this goal cannot be underestimated. There is no single irrigating soluti<strong>on</strong> that<br />
al<strong>on</strong>e sufficiently covers all of the functi<strong>on</strong>s required from an irrigant. Optimal irrigati<strong>on</strong> is based <strong>on</strong> the combined use of 2 or<br />
several irrigating soluti<strong>on</strong>s, in a specific sequence. This article highlights the mechanism of acti<strong>on</strong>, safety and<br />
biocompatibility of currently used irrigati<strong>on</strong> soluti<strong>on</strong>s.<br />
Key Words : Root Canal Irrigati<strong>on</strong>, Mechanism of Acti<strong>on</strong>s, Chelators, Cytotoxicity<br />
Introducti<strong>on</strong><br />
Successful endod<strong>on</strong>tic treatment requires combinati<strong>on</strong> of<br />
variety of factors such as an accurate diagnosis, thorough<br />
cleaning and shaping of the pulp space, a predictable<br />
disinfecti<strong>on</strong> protocol achieved with the help of various<br />
intra<strong>canal</strong> medicaments and irrigati<strong>on</strong> soluti<strong>on</strong>s. This is<br />
followed by three dimensi<strong>on</strong>al obturati<strong>on</strong> of the pulp space<br />
and adequate final restorati<strong>on</strong>. Mechanical preparati<strong>on</strong> of the<br />
<strong>root</strong> <strong>canal</strong> achieved with the use of either hand instruments or<br />
rotary nickel-titanium instruments helps in removal of vital<br />
and necrotic remnants of pulp tissue, microorganisms and<br />
microbial toxins to a certain extent. However, with the use of<br />
recent imaging techniques, it is certain that some part of the<br />
1<br />
pulp space remains uninstrumented. These areas might<br />
harbor necrotic tissues, microorganisms and their byproducts<br />
resulting in persistent periradicular inflammati<strong>on</strong>. Therefore,<br />
irrigati<strong>on</strong> is an essential part of debridement because it allows<br />
for cleaning bey<strong>on</strong>d what might be achieved by <strong>root</strong> <strong>canal</strong><br />
instrumentati<strong>on</strong> al<strong>on</strong>e.<br />
Endod<strong>on</strong>tic microbiology:<br />
The role of microorganisms in infecti<strong>on</strong> of dental pulp and<br />
periapical lesi<strong>on</strong> formati<strong>on</strong> has been elegantly dem<strong>on</strong>strated<br />
2<br />
in the classic studies of Kakehashi et. Al. Primary<br />
intraradicular infecti<strong>on</strong> is caused by microorganisms that<br />
invade and col<strong>on</strong>ize necrotic pulp tissue. The microflora of<br />
untreated teeth with necrotic pulp is usually found to be<br />
mixed, comprising of Gram-positive and Gram-Negative<br />
3<br />
organisms, dominated by anaerobic bacteria. The<br />
microorganisms associated with endod<strong>on</strong>tic treatment failure<br />
mainly comprised <strong>on</strong>e or two species, these are<br />
predominantly Gram-positive bacteria with Enterococcus<br />
4<br />
faecalis as the most prevalent organism. Fungi, specifically<br />
Candida albicans can also be found at a significantly higher<br />
5<br />
rate than in primary infecti<strong>on</strong>. . The choice of irrigant soluti<strong>on</strong><br />
and irrigati<strong>on</strong> protocol should be aimed at removal of all forms<br />
of microorganisms including their presence in biofilm.<br />
Desirable properties of Root Canal Irrigant as suggested<br />
6<br />
by Zehnder :<br />
1. Broad antimicrobial spectrum<br />
2. High efficiency against anaerobic and facultative<br />
microorganisms organized in biofilm<br />
3. Ability to dissolve necrotic pulp tissue remnants<br />
4. Ability to inactivate endotoxins<br />
5. Prevent formati<strong>on</strong> of smear layer during instrumentati<strong>on</strong><br />
or to dissolve the latter <strong>on</strong>ce it has formed.<br />
6. Should be n<strong>on</strong> toxic when they come in c<strong>on</strong>tact with vital<br />
tissues, n<strong>on</strong> caustic to period<strong>on</strong>tal tissues, and with little<br />
potential to cause anaphylactic reacti<strong>on</strong>s.<br />
The irrigating soluti<strong>on</strong>s that are currently used during<br />
cleaning and shaping can be broadly categorized into<br />
antibacterial and decalcifying agents or their combinati<strong>on</strong>s.<br />
They include Sodium Hypochlorite (Here after Known as<br />
NaOCl), Chlorhexidine Gluc<strong>on</strong>ate (Here after Known as<br />
CHX), ethylenediaminetetraacitic acid (Here after Known as<br />
EDTA), and a mixture of tetracycline, an acid and a detergent<br />
(Here after Known as MTAD).<br />
Sodium Hypochlorite (NaOCl):<br />
Sodium hypochlorite (house hold bleach) is the most<br />
frequently and dominantly used agent for <strong>root</strong> <strong>canal</strong> irrigati<strong>on</strong>.<br />
th<br />
It has been known in medical fields since the beginning of 20<br />
century and was introduced as a part of endod<strong>on</strong>tic treatment<br />
in 1936 by Walker. During the world war I the chemist Henry<br />
Drysdale Dakin and surge<strong>on</strong> Alexis Carrel extended the use<br />
of buffered 0.5% NaOCl soluti<strong>on</strong> to the irrigati<strong>on</strong> of infected<br />
7<br />
wound.<br />
8<br />
Mechanism of Acti<strong>on</strong>:<br />
Two unique properties of NaOCl- antimicrobial activity and<br />
organic tissue dissoluti<strong>on</strong> can be explained by following<br />
reacti<strong>on</strong>s that takes place when it comes in c<strong>on</strong>tact with the<br />
organic tissues or microorganisms.<br />
Address for Corresp<strong>on</strong>dence :<br />
Dr. Kunjal S. Mistry M.D.S.<br />
Reader, Dept. of C<strong>on</strong>servative Dentistry & Endod<strong>on</strong>tics,<br />
Faculty of Dental Science, Dharamsinh <strong>Desai</strong> <strong>University</strong>,<br />
College Road, Nadiad - 387 001. Gujarat, India<br />
Ph: 9825334526 E-mail : Sharnam2005@yahoo.co.in<br />
27
JOURNAL OF DENTAL SCIENCES<br />
NaOCl acts as an organic and fat solvent, degrading fatty<br />
acids and transforming them into fatty acid salts (soap) and<br />
glycerol (alcohol) which reduces the surface tensi<strong>on</strong> of the<br />
remaining soluti<strong>on</strong>.<br />
NaOCl neutralizes amino acids forming water and salt. With<br />
the exit of hydroxyl i<strong>on</strong>s, there is reducti<strong>on</strong> of pH.<br />
Hypochlorus acid, a substance present in sodium<br />
hypochlorite soluti<strong>on</strong>, when in c<strong>on</strong>tact with organic tissue acts<br />
as a solvent and releases chlorine, which combines with<br />
protein amino groups to form chloramines. The<br />
chloraminati<strong>on</strong> reacti<strong>on</strong> between chlorine and the amino<br />
group (NH) forms chloramines that interfere in cell<br />
metabolism. Chlorine has an antimicrobial acti<strong>on</strong>, inhibiting<br />
bacterial enzymes and leading to an irreversible oxidati<strong>on</strong> of<br />
SH groups (sulphydryl groups) of essential bacterial<br />
enzymes.<br />
C<strong>on</strong>centrati<strong>on</strong> of NaOCl:<br />
Various c<strong>on</strong>centrati<strong>on</strong>s of NaOCl from 0.5% to 5.25% have<br />
9,10<br />
been tried out. Higher the c<strong>on</strong>centrati<strong>on</strong> better will be<br />
antimicrobial effect and tissue dissolving capacity. At the<br />
same time higher c<strong>on</strong>centrati<strong>on</strong> also carries the risk of toxicity<br />
and tissue reacti<strong>on</strong>. Literature is full of studies showing<br />
severe irritati<strong>on</strong>s when c<strong>on</strong>centrated soluti<strong>on</strong> were<br />
inadvertently forced into the periapical tissues bey<strong>on</strong>d apex<br />
11,12<br />
of the tooth under endod<strong>on</strong>tic treatment. 5.25% NaOCl<br />
has an unpleasant odour and this odour decreases as the<br />
c<strong>on</strong>centrati<strong>on</strong> decreases. From in vitro observati<strong>on</strong>s, it has<br />
been shown that 1% NaOCl is sufficient to dissolve the pulp<br />
13<br />
tissue. Although less c<strong>on</strong>centrated soluti<strong>on</strong>s have shown<br />
14<br />
antimicrobial efficacy higher c<strong>on</strong>centrati<strong>on</strong>s of NaOCl<br />
present faster and greater bactericidal effect. However, the<br />
Volume 2 Issue 2<br />
higher the c<strong>on</strong>centrati<strong>on</strong> of this substance the greater is its<br />
9<br />
cytotoxic effects . Hence based <strong>on</strong> these studies, there is no<br />
rati<strong>on</strong>ale for using hypochlorite soluti<strong>on</strong>s at c<strong>on</strong>centrati<strong>on</strong>s<br />
higher than 1%.<br />
Increasing the efficacy of NaOCl:<br />
1. Heating<br />
An increase in temperature of low c<strong>on</strong>centrati<strong>on</strong> NaOCL<br />
soluti<strong>on</strong> increases its tissue dissoluti<strong>on</strong> and antimicrobial<br />
properties. This is supported by a recent study where a<br />
temperature rise of 25ºc. increased NaOCl efficacy by a<br />
factor of 100. The capacity of 1% NaOCl at 45ºc. to dissolve<br />
human dental pulp is found to be equal to that of a 5.25%<br />
15<br />
soluti<strong>on</strong> at 20ºc.<br />
Ultras<strong>on</strong>ics:<br />
Ultras<strong>on</strong>ic activati<strong>on</strong> of sodium hypochlorite has also been<br />
suggested to accelerate the chemical reacti<strong>on</strong>, create<br />
cavitati<strong>on</strong>al effects and achieve superior cleansing acti<strong>on</strong>.<br />
When a small file (mostly ISO no. 15) is held free in an<br />
enlarged <strong>canal</strong> filled with NaOCl and ultras<strong>on</strong>ically activated,<br />
the ultras<strong>on</strong>ic energy warms the soluti<strong>on</strong> in the <strong>canal</strong> and the<br />
res<strong>on</strong>ant vibrati<strong>on</strong>s cause movement of aqueous NaOCl into<br />
the difficult to reach ramificati<strong>on</strong>s in the <strong>canal</strong>, an effect called<br />
16<br />
“Acoustic streaming”. However, it appears important to<br />
apply the instrument after the <strong>canal</strong> preparati<strong>on</strong> has been<br />
completed. An instrument that oscillates freely in the <strong>canal</strong><br />
gives more ultrasound effects in the irrigating soluti<strong>on</strong> than<br />
the instrument that binds to <strong>canal</strong> wall. Therefore, to use a No.<br />
15 file in an ultras<strong>on</strong>ic hand piece 1 mm. short of working<br />
length, the <strong>canal</strong> should be enlarged apically at least to a size<br />
25.<br />
Chlorhexidine:<br />
Chlorhexidine was developed in the late 1940s in the<br />
6<br />
research laboratories of Imperial Chemical Industries Ltd.<br />
CHX is a cati<strong>on</strong>ic biguanide that possesses broad<br />
antibacterial activity in combinati<strong>on</strong> with relatively low<br />
toxicity and the ability to bind to skin and mucous<br />
membranes.<br />
Mechanism of Acti<strong>on</strong>:<br />
The CHX molecule reacts with negatively charged groups <strong>on</strong><br />
the cell surface, causing an irreversible loss of cytoplasmic<br />
c<strong>on</strong>stituents, membrane damage, and enzyme inhibiti<strong>on</strong>. At<br />
high c<strong>on</strong>centrati<strong>on</strong>s, CHX results in extensive cell damage,<br />
coagulati<strong>on</strong> of cytoplasm, and precipitati<strong>on</strong> of proteins and<br />
17<br />
nucleic acids. CHX is a positively charged hydrophobic and<br />
lipophilic molecule that interacts with phospholipids <strong>on</strong> the<br />
cell membrane of bacteria and then enters the cell through<br />
some type of active or passive transport mechanism. Its<br />
efficacy is based <strong>on</strong> interacti<strong>on</strong> between positive charge of<br />
the molecule and negatively charged phosphate groups <strong>on</strong><br />
the bacterial cell wall that increases the permeability of cell<br />
wall and allows it to penetrate into bacteria with intracellular<br />
toxic effects. CHX at low c<strong>on</strong>centrati<strong>on</strong> will result in<br />
bacteriostatic effect but at higher c<strong>on</strong>centrati<strong>on</strong>s, it is<br />
bactericidal due to precipitati<strong>on</strong> and/or coagulati<strong>on</strong> of the<br />
cytoplasm which is probably caused by protein cross-<br />
18<br />
linking.<br />
28
JOURNAL OF DENTAL SCIENCES<br />
Antibacterial activity:<br />
CHX is active against a wide range of microorganisms, such<br />
as Gram-positive and Gram-negative bacteria, bacterial<br />
spores, lipophilic virus, yeast, and dermatophytes, being<br />
bacteriostatic at low c<strong>on</strong>centrati<strong>on</strong>s and bactericidal at high<br />
19<br />
c<strong>on</strong>centrati<strong>on</strong>s. CHX shows a substantial antimicrobial<br />
activity against comm<strong>on</strong> endod<strong>on</strong>tic pathogens like<br />
staphylococcus aureus, Porphyrom<strong>on</strong>as endod<strong>on</strong>talis,<br />
foreign body granuloma formati<strong>on</strong> at 2 weeks, which resolved<br />
24<br />
over time. To help evaluate the inflammatory resp<strong>on</strong>se of 2%<br />
Chlorhexidine, Tanamaru Filho et al. separately injected<br />
0.5% NaOCl, 2% Chlorhexidine digluc<strong>on</strong>ate, and phosphatebuffered<br />
saline into the perit<strong>on</strong>eal cavity of mice. This study<br />
found the number of inflammatory cells resulting from 2%<br />
CHX injecti<strong>on</strong> was similar to the phosphate-buffered saline<br />
c<strong>on</strong>trol at all times tested, while the 0.5% NaOCl injecti<strong>on</strong><br />
25<br />
resulted in significantly larger number of inflammatory cells.<br />
Ribeiro et al. evaluated the genotoxiciy of formocresol,<br />
param<strong>on</strong>ochlorophenol, calcium hydroxide, and CHX against<br />
Chinese hamster Ovary cells. Results showed that n<strong>on</strong>e of<br />
26<br />
the menti<strong>on</strong>ed agents c<strong>on</strong>tributed to DNA damage. Thus, in<br />
the clinically used c<strong>on</strong>centrati<strong>on</strong>s, the biocompatibility of<br />
CHX is acceptable.<br />
While CHX has so many positive qualities, it lacks tissue<br />
dissoluti<strong>on</strong> property. Naenni et al. used full thickness palatal<br />
mucosa from pigs incubated in 10ml of 10% Chlorhexidine for<br />
2 hours. At the end of 2 hours, the pig mucosa retained 90% of<br />
its initial weight while 1% NaOCl caused the pig mucosa to<br />
27<br />
retain <strong>on</strong>ly 7% of the initial weight. Khademi et al. treated<br />
fifty pieces of bovine pulp tissue with normal saline, MTAD,<br />
2% Chlorhexidine digluc<strong>on</strong>ate and 2.5% NaOCl and<br />
c<strong>on</strong>cluded that Chlorhexidine has the weakest tissue<br />
28<br />
dissoluti<strong>on</strong> capacity.<br />
Chelator soluti<strong>on</strong>s:<br />
Volume 2 Issue 2<br />
Chelating agents were introduced into endod<strong>on</strong>tics as an aid<br />
in preparati<strong>on</strong> of narrow and decalcified <strong>canal</strong>s by Nygaard<br />
–Ostby in 1957 who recommended the use of 15% EDTA at<br />
pH 7.3.<br />
EDTA and citric acid<br />
Sodium Hypochlorite has a limited acti<strong>on</strong> of removing <strong>on</strong>ly the<br />
Porphyrom<strong>on</strong>as gingivalis, Prevotella intermedia,<br />
organic c<strong>on</strong>tents from the smear layer, therefore<br />
1 0 demineralizing agents such as ehylenediamine tetra acetic<br />
Enterococcus faecalis, candida albicans. and<br />
20<br />
acid (EDTA) and citric acid have been recommended for<br />
Streptococcus mutans. The antimicrobial acti<strong>on</strong> is related to<br />
complete eliminati<strong>on</strong> of smear layer during <strong>root</strong> <strong>canal</strong><br />
type, c<strong>on</strong>centrati<strong>on</strong>, and presentati<strong>on</strong> form of the <strong>irrigants</strong> as<br />
therapy. Chelating agents are available in both liquid and<br />
well as the microbial susceptibility. The c<strong>on</strong>centrati<strong>on</strong> often<br />
paste forms. EDTA is used in 17% c<strong>on</strong>centrati<strong>on</strong> and citric<br />
used in endod<strong>on</strong>tic therapy is 2% Chlorhexidine. This has<br />
acid is used in the c<strong>on</strong>centrati<strong>on</strong> of 10 to 20%. In vitro studies<br />
been found to be more effective in the least time when<br />
have shown their cytotoxicity, and 10% citric acid has proven<br />
compared with other c<strong>on</strong>centrati<strong>on</strong>s of Chlorhexidine ranging<br />
20<br />
to be more biocompatible than 17% EDTA-T and 17%<br />
from 0.002% to 2%. CHX can be used in liquid or gel<br />
29<br />
EDTA.<br />
formulati<strong>on</strong>s. The CHX gel makes instrumentati<strong>on</strong> easier,<br />
21<br />
thus increasing the mechanical removal of tissues. MTAD<br />
Furthermore it also decreases the smear layer formati<strong>on</strong> It was introduced as an alternative to EDTA to remove the<br />
22<br />
which does not happen with liquid formulati<strong>on</strong>.<br />
smear layer by Torabinejad et al. It is a mixture of 3%<br />
Cytotoxicity:<br />
doxycycline, 4.25% citric acid and detergent-Tween 80. It has<br />
30<br />
a combined chelating and antibacterial properties. In the<br />
Results from a laboratory study <strong>on</strong> the toxicity of CHX to<br />
MTAD preparati<strong>on</strong>, citric acid may serve to remove the smear<br />
human gingival cells showed that the toxic potency of CHX is<br />
layer allowing the doxycycline to enter the dentinal tubules<br />
dependent <strong>on</strong> the length of exposure and the compositi<strong>on</strong> of<br />
23<br />
and exert an antibacterial effect. The effectiveness of the<br />
the exposure medium. While Chlorhexidine does not appear<br />
MTAD to completely remove the smear layer is enhanced<br />
to cause any l<strong>on</strong>g-term damage to host tissues, it may still<br />
when a low c<strong>on</strong>centrati<strong>on</strong> of NaOCl (1.3%) is used as an<br />
cause an inflammatory resp<strong>on</strong>se in these tissues if<br />
intra<strong>canal</strong> irrigant before placing 1 ml of MTAD in a <strong>canal</strong> for<br />
expressed bey<strong>on</strong>d <strong>root</strong> <strong>canal</strong>. Yesilsoy et al. injected 0.12%<br />
five minutes and rinsing it with an additi<strong>on</strong>al 4 ml of MTAD as<br />
Chlorhexidine into the subcutaneous tissues of the backs of<br />
31<br />
the final rinse. However, a final rinse with MTAD might have<br />
pigs to help asses short term toxic effects. After histological<br />
a negative effect <strong>on</strong> the b<strong>on</strong>ding ability of both resin based<br />
examinati<strong>on</strong>, they found a mild inflammatory resp<strong>on</strong>se after 2<br />
and calcium hydroxide based sealers due to the precipitate<br />
hours, moderate inflammatory resp<strong>on</strong>se after 2 days, and a<br />
32<br />
formati<strong>on</strong>. MTAD also has been shown to adversely affect<br />
the b<strong>on</strong>d strength of Gutta-perch and AH plus filling material<br />
33<br />
to <strong>root</strong> dentin when used as final rinse.<br />
Maleic Acid:<br />
Maleic acid is a mild organic acid used as an acid c<strong>on</strong>diti<strong>on</strong>er<br />
in adhesive dentistry. It efficiently removes the smear layer at<br />
5% and 7% c<strong>on</strong>centrati<strong>on</strong>. However, at 10% or more<br />
c<strong>on</strong>centrati<strong>on</strong> it can result in demineralizati<strong>on</strong> and damage to<br />
34<br />
<strong>root</strong> <strong>canal</strong> wall. Final irrigati<strong>on</strong> with 7% Maleic acid is more<br />
efficient than 17% EDTA in removal of smear layer from apical<br />
third of the <strong>root</strong> <strong>canal</strong> system, which is a crucial area for<br />
35<br />
disinfecti<strong>on</strong>. Also 7% Maleic acid produces maximum<br />
surface roughness <strong>on</strong> <strong>root</strong> <strong>canal</strong> walls as compared to 17%<br />
EDTA. This surface roughness produces an important role in<br />
36<br />
micromechanical b<strong>on</strong>ding of resin sealers. However, the<br />
technique of use and biologic effects of Maleic acid <strong>on</strong><br />
periapical tissues needs evaluati<strong>on</strong>, before it is routinely<br />
employed for clinical use.<br />
Tetraclean:<br />
Tetraclean (Ogna Laboratori Farmaceutici, Muggiò (Mi),<br />
Italy), like MTAD, is mixture of an antibiotic, an acid and a<br />
detergent. However, the c<strong>on</strong>centrati<strong>on</strong> of the antibiotic<br />
(doxycycline-50 mg/ml), and the type of detergent<br />
37<br />
(polypropylene glycol) differ from those of MTAD. It shows<br />
a high acti<strong>on</strong> against both, strictly anaerobic and facultative<br />
29
JOURNAL OF DENTAL SCIENCES<br />
38<br />
anaerobic bacteria. It removes the smear layer and opens<br />
up the dentinal tubule orifices. It has low surface tensi<strong>on</strong><br />
which enables a better adaptati<strong>on</strong> of the mixtures to the<br />
37<br />
dentinal walls. It is also more effective than MTAD against E.<br />
faecalis in plankt<strong>on</strong>ic culture and in mixed species in vitro<br />
39<br />
biofilm. In another study, they compared the antimicrobial<br />
efficacy of 5.25% NaOCl, MTAD, and Tetraclean against an<br />
E. faecalis biofilm generated <strong>on</strong> cellulose nitrate membrane<br />
filters. Only the NaOCl could disaggregate and remove the<br />
biofilm at every time interval tested although treatment with<br />
Tetraclean caused a high degree of biofilm disaggregati<strong>on</strong> at<br />
40<br />
each time interval when compared with MTAD.<br />
Interacti<strong>on</strong> between comm<strong>on</strong>ly used <strong>irrigants</strong><br />
It is important to note here that both EDTA and citric acid<br />
41<br />
str<strong>on</strong>gly interact with NaOCl. They immediately reduce the<br />
available chlorine in the soluti<strong>on</strong>, rendering the sodium<br />
hypochlorite irrigant ineffective <strong>on</strong> bacteria and necrotic<br />
42<br />
tissues. Hence, it has been suggested that citric acid or<br />
EDTA should never be mixed with sodium hypochlorite. Once<br />
irrigati<strong>on</strong> has been completed with NaOCl, the remaining<br />
NaOCl should be removed and <strong>on</strong>ly then should the irrigati<strong>on</strong><br />
with EDTA begin.<br />
CHX has no tissue-dissolving activity and there have been<br />
efforts to combine CHX with hypochlorite for added benefits<br />
from the two soluti<strong>on</strong>s. However, CHX and NaOCl are not<br />
soluble in each other; a brownish-orange precipitate is<br />
formed when they are mixed. Atomic absorpti<strong>on</strong><br />
spectrophotometry has indicated that the precipitate c<strong>on</strong>tains<br />
43<br />
ir<strong>on</strong>, which may be the reas<strong>on</strong> for the orange development.<br />
Presence of parachloroaniline, which may have mutagenic<br />
potential, has also been dem<strong>on</strong>strated in the precipitate. Until<br />
this precipitate is studied further, its formati<strong>on</strong> should be<br />
avoided by removing the NaOCl before placing CHX into the<br />
44<br />
<strong>canal</strong>.<br />
C<strong>on</strong>clusi<strong>on</strong><br />
Irrigati<strong>on</strong> has a key role in successful endod<strong>on</strong>tic treatment.<br />
Although NaOCl is the most important irrigating soluti<strong>on</strong>, no<br />
single irrigant can accomplish all the tasks required by<br />
irrigati<strong>on</strong>. Detailed understanding of the mode of acti<strong>on</strong> of<br />
various available and comm<strong>on</strong>ly used soluti<strong>on</strong>s is important<br />
for optimal irrigati<strong>on</strong>. New developments in the compositi<strong>on</strong><br />
of the irrigating soluti<strong>on</strong>s and mechanical devices used for<br />
effective delivery of the soluti<strong>on</strong> in intricate areas of the <strong>root</strong><br />
<strong>canal</strong> system willhelp to advance safe and effective irrigati<strong>on</strong>.<br />
Reference:<br />
1. Peters OA, Scho¨nenberger K, Laib A. Effects of four Ni-<br />
Ti preparati<strong>on</strong> techniques <strong>on</strong> <strong>root</strong> <strong>canal</strong> geometry<br />
assessed by micro computed tomography. Int Endod J<br />
2001; 34:221–30.<br />
2. Kakehashi S., Stanley H R, Fitzgerald R J. The effects of<br />
surgical exposures of dental pulps in germ-free and<br />
c<strong>on</strong>venti<strong>on</strong>al laboratory rats. J Oral Surgery 1963;<br />
20:340-349.<br />
3. Siqueira J F, Rocas I N. Exploiting molecular methods to<br />
explore endod<strong>on</strong>tic infecti<strong>on</strong>s Part-II: Redefining<br />
endod<strong>on</strong>tic Microbiota. J Endod 2005; 31(7): 488-498.<br />
4. Pinheiro E T, Gomes BPFA, Ferraz C.C.R., Sousa E L R.<br />
Volume 2 Issue 2<br />
Microorganisms from <strong>canal</strong>s of <strong>root</strong>-filled teeth with peri<br />
apical lesi<strong>on</strong>s.Int endod J.2003; 36(1): 1-11.<br />
5. Peciuliene V, Reynaud A H, Haapasalo M. Isolati<strong>on</strong> of<br />
Yeasts and enteric bacteria in <strong>root</strong>-filled teeth with chr<strong>on</strong>ic<br />
apical period<strong>on</strong>titis. Int Endod J. 2001; 34(6):429-434.<br />
6. M.Zehnder, Root Canal Irrigants; JOE May 2006, 32 (5):<br />
389-398.<br />
7. Dakin HD. On the use of certain antiseptic substances in<br />
treatment of wounds, Br. Med J 1915; 2; 318-20.<br />
8. Estrela C. E L Barbin, E. Spano, A. Marchesan, D. Pecora<br />
Mechanism of acti<strong>on</strong> of Sodium Hypochlorite . Braz Dent<br />
J 2002: 13(2): 113-117.<br />
9 Gomes BPFA, Ferraz CCR, Vianna MEVB, Berber FB. In<br />
vitro antimicrobial activity of several c<strong>on</strong>centrati<strong>on</strong>s of<br />
sodium hypochlorite and Chlorhexidine Gluc<strong>on</strong>ate in the<br />
eliminati<strong>on</strong> of Enterococcus Faecalis. Int Endod J,<br />
2001;34: (6): 24-8.<br />
10 M E Vianna, BPFA Gomes. In vitro evaluati<strong>on</strong> of the<br />
antimicrobial activity of Chlorhexidine and sodium<br />
hypochlorite: Oral surgery Oral Medicine Oral Pathology;<br />
January 2004; 97(1): 79-84.<br />
11 Witt<strong>on</strong> R, Henthorn K, Ethunandan M, et al. Neurological<br />
complicati<strong>on</strong>s following extrusi<strong>on</strong> of sodium hypochlorite<br />
soluti<strong>on</strong> during <strong>root</strong> <strong>canal</strong> treatment. Int Endod J. 2005;<br />
38:843-848.<br />
12 Gursoy UK, Bostanci V, Kosger HH. Palatal mucosa<br />
necrosis because of accidental sodium hypochlorite<br />
injecti<strong>on</strong> instead of anesthetic soluti<strong>on</strong>. Int Endod J.<br />
2006;39:157-161.<br />
13 Sirtes G, Waltimo T, Schaetzle M, Zehnder M,. The effect<br />
of temperature <strong>on</strong> sodium hypochlorite short-term<br />
stability, pulp dissoluti<strong>on</strong> capacity, and antimicrobial<br />
efficacy. J Endod 2005; 31:669-71.<br />
14 Siqueira J F, I N Rocas, Lima KC, Favieri A. Chemo<br />
mechanical reducti<strong>on</strong> of the bacterial populati<strong>on</strong> in the<br />
<strong>root</strong> <strong>canal</strong> after instrumentati<strong>on</strong> and irrigati<strong>on</strong> with 1%,<br />
2.5% and 5.25% sodium hypochlorite. J Endod.2000;<br />
26(6):331-4.<br />
15 Sirtes G, Waltimo T, Schaetzle M, Zehnder M. The effects<br />
of temperature <strong>on</strong> sodium hypochlorite short-term<br />
stability, pulp dissoluti<strong>on</strong> capacity, and antimicrobial<br />
efficacy. J Endod 2005; 31:669-71.<br />
16 Majina Ahmad, T.R.Pitt Ford, LLawrence A. Crum.<br />
Ultras<strong>on</strong>ic debridement of <strong>root</strong> <strong>canal</strong>s- Acoustic<br />
streaming and its possible role. JOE October 1987;<br />
13(10): 490-499.<br />
17 J<strong>on</strong>es, C. G. 1997. Chlorhexidine: is it still the gold<br />
standard? Period<strong>on</strong>tology 2000 15:55–62.<br />
18 Gomes BPFA, Souza SFC, Ferraz CCR. Effectiveness of<br />
2% CHX gel and calcium Hydroxide against<br />
Enterococcus faecalis in bovine <strong>root</strong> dentin in vitro. Int<br />
Endo Journal 2003; 36: 267-275.<br />
19 Dent<strong>on</strong> GW. Chlorhexidine. In: Block SS. Disinfecti<strong>on</strong>,<br />
sterilizati<strong>on</strong> and preservati<strong>on</strong>. 4th ed. Philadelphia: Lea &<br />
Febiger, 1991:274-89.<br />
30
JOURNAL OF DENTAL SCIENCES<br />
20 Lessa, F C Rosetti, Nogueira,F Silveira Direct and<br />
transdentinal antibacterial activity of chlorhexidine<br />
:American J of Dentistry; Oct 2010:25( 5): 255-259.<br />
21 Vivacqua-Gomes N, Ferraz CCR, Gomes BPFA, Zaia<br />
AA, Teixeira FB, Souza-Filho FJ. Influence of <strong>irrigants</strong> <strong>on</strong><br />
the cor<strong>on</strong>al microleakage of laterally c<strong>on</strong>densed guttapercha<br />
<strong>root</strong> fillings. Int Endod J 2002; 35:1-5.<br />
22 Ferraz CCR, Gomes BPFA, Zaia AA, Teixeira F, Souza-<br />
Filho FJ. In vitro assessment of the antimicrobial acti<strong>on</strong><br />
and the mechanical ability of Chlorhexidine gel as an<br />
endod<strong>on</strong>tic irrigant. J Endod 2001;27:452-5.<br />
23 Babich H, Wurzburger BJ, Rubin Y L, Sinensky MC, Blau<br />
L, An in Vitro study <strong>on</strong> the cytotoxicity of Chlorhexidine<br />
digluc<strong>on</strong>ate to human gingival cells, Cell biology and<br />
Toxicology 11, 79-88.<br />
24 Yesilsoy C, Whitake E, Cleveland D. Antimicrobial and<br />
toxic effects of established and potential <strong>root</strong> <strong>canal</strong><br />
<strong>irrigants</strong>. J endod. 1995;(10):513-515.<br />
25 Tanamaru Filho M, Le<strong>on</strong>ardo MR, Silva LA. Inflammatory<br />
resp<strong>on</strong>se to different endod<strong>on</strong>tic irrigating soluti<strong>on</strong>s Int<br />
Endod J. 2002; 35(9): 735-739.<br />
26 Ribeiro DA, Scolastici C, Marques PLA, Marques MEA,<br />
Salvadori MF : Genotoxicity of antimicrobial endod<strong>on</strong>tic<br />
compounds by single cell gel assay in Chinese hamster<br />
ovary cells. Oral surgery Oral Medicine, Oral Pathology,<br />
Oral radiology and Endod<strong>on</strong>tics 2005, 99: 637-40.<br />
27 Naenni N, Thoma K, Zehnder M. Soft tissue dissoluti<strong>on</strong><br />
capacity of currently used and potential endod<strong>on</strong>tic<br />
<strong>irrigants</strong> J Endod. 2004; 30(11): 785-787.<br />
28 Abbasali Khademi, Ehsan usefian, Mahboobe F. Tissue<br />
dissolving ability of several endod<strong>on</strong>tic <strong>irrigants</strong> <strong>on</strong><br />
bovine pulp tissue Iranian Endod<strong>on</strong>tic journal 2007; 2 ( 2):<br />
65-67.<br />
29 Sceiza MF, Daniel RL, Santos EM, Jaeger MM, Cytotoxic<br />
effects of 10% citric acid and EDTA-T used as <strong>root</strong> <strong>canal</strong><br />
<strong>irrigants</strong>. An in Vitro Analysis. J Endod 2001; 7: 741-3.<br />
30 Torabinejad M, Khademi A A, Babagoli j, Cho Y, Johns<strong>on</strong><br />
W B, Bozhilov K, A new soluti<strong>on</strong> for removal of smear<br />
layer.J Endod 2003;29:170-5.<br />
31 Torabinejad M, Khademi A A, Cho Y, Bakland L K,<br />
Shabanhang S, The effect of various c<strong>on</strong>centrati<strong>on</strong>s of<br />
sodium hypochlorite <strong>on</strong> the ability of MTAD to remove the<br />
smear layer. J Endod 2003; 29:233-9.<br />
32 Gopikirishna V, Venkateshbabu N, Datta k,<br />
Kandaswamy D. Evaluati<strong>on</strong> of the effect of MTAD in<br />
comparis<strong>on</strong> with EDTA when employed as the final rinse<br />
<strong>on</strong> the shear b<strong>on</strong>d strength of three endod<strong>on</strong>tic sealers to<br />
dentin. Aus Endod Journal Aprill 2011.37(1):12-17.<br />
33 Ahmed Abdel Rahman Hashem, Angie G. Gh<strong>on</strong>eim,<br />
Reem A. Lutfy, and Manar Y. Fouda, The effect of<br />
different irrigating soluti<strong>on</strong>s <strong>on</strong> b<strong>on</strong>d strength of Two <strong>root</strong><br />
<strong>canal</strong> filling systems. J Endod April 2009; 35(4):537-<br />
540.<br />
Volume 2 Issue 2<br />
34 Prabhu SG, Rahim N Bhat KS ,Mathew J. Comparis<strong>on</strong> of<br />
removal of endod<strong>on</strong>tic smear layer using NaOCl, EDTA,<br />
and different c<strong>on</strong>centrati<strong>on</strong>s of Maleic acid –A SEM study.<br />
Endod<strong>on</strong>tology: June 2003; 15: 20-25.<br />
35 NV Ballal, S. Kandian, Kundabala Mala, K S Bhat,<br />
Shashirashmi Acharya. Comparis<strong>on</strong> of the Efficacy of<br />
Maleic Acid and Ethylenediaminetetraacetic Acid in<br />
Smear Layer Removal from Instrumented Human Root<br />
Canal: A Scanning Electr<strong>on</strong> Microscopic Study J Endod<br />
Nov. 2009;35 (1573-1576.<br />
36 NV Ballal, S. Kandian, Kundabala Mala, K S<br />
Bhat.Evaluati<strong>on</strong> of the effect of Maleic acid and EDTA <strong>on</strong><br />
Micro hardness and surface roughness of Human <strong>root</strong><br />
<strong>canal</strong> dentin. J Endod; August 2010:36(8): 1385-1388.<br />
37 Giardino L, Ambu E, Becce C, Rim<strong>on</strong>dini L, Morra M.<br />
Surface tensi<strong>on</strong> comparis<strong>on</strong> of four comm<strong>on</strong> <strong>root</strong> <strong>canal</strong><br />
<strong>irrigants</strong> and two new <strong>irrigants</strong> c<strong>on</strong>taining antibiotic. J<br />
Endod 2006; 32:1091-3.<br />
38 Luciano Giardino, Enrico Savoldi, E. Ambu, Roberto<br />
Rim<strong>on</strong>dini, Alberto Palez<strong>on</strong>a, E A Debbia, Antimicrobial<br />
effect of MTAD, tetraclean, Cloreximid and sodium<br />
hypochlorite against three comm<strong>on</strong> endod<strong>on</strong>tic<br />
pathogens. Indian Journal of Dental research 2009;<br />
20(3): 391-395.<br />
39 F G Pappen, Y. Shen, W. Gian, M R Le<strong>on</strong>ardo, L Giardino,<br />
M Haapasalo.In vitro antibacterial acti<strong>on</strong> of Tetraclean,<br />
MTAD and Five experimental irrigati<strong>on</strong> soluti<strong>on</strong>s Int<br />
Endod J. June 2010:43 (6): 528-535.<br />
40 Giardino L, Ambu E, Savoldi E, Rim<strong>on</strong>dini L, Cassanelli<br />
C, Debbia EA. Comparative evaluati<strong>on</strong> of antimicrobial<br />
efficacy of sodium hypochlorite, MTAD, and Tetraclean<br />
against Enterococcus faecalis biofilm. J Endod 2007;<br />
33:852-5.<br />
41 Baumgartner JC, Ibay AC, The chemical reacti<strong>on</strong>s of<br />
<strong>irrigants</strong> used for <strong>root</strong> <strong>canal</strong> debridement. J Endod<br />
1987;13: 47-51.<br />
42 Zehnder M, Schmidlin P, Sener B, Waltimo T, Chelati<strong>on</strong> in<br />
<strong>root</strong> <strong>canal</strong> therapy rec<strong>on</strong>sidered. J Endod 2005; 31:817-<br />
20.<br />
43 Marchesan MA, Pasternak Junior B, Af<strong>on</strong>so MM, et al.<br />
Chemical analysis of the flocculate formed by the<br />
associati<strong>on</strong> of sodium hypochlorite and chlorhexidine.<br />
Oral Surg Oral Med Oral Pathol Oral Radiol Endod<br />
2007;103:103–5.<br />
44 Basrani BR, Manek S, Sodhi RN, et al. Interacti<strong>on</strong><br />
between sodium hypochlorite and chlorhexidine<br />
gluc<strong>on</strong>ate. J Endod 2007; 33:966–9.<br />
31