July 2010 - AOGD
July 2010 - AOGD
July 2010 - AOGD
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 10 <strong>July</strong> <strong>2010</strong> Monthly Issue 3<br />
<strong>AOGD</strong> Bulletin<br />
M inimise<br />
aternal<br />
ortality<br />
Safe<br />
Mother<br />
Nation<br />
<strong>AOGD</strong> Secretariat<br />
Department of Obstetrics & Gynecology<br />
Room No. 112, Ward 1, Block A, First Floor, New Surgical Block, Lok Nayak Hospital & MAMC, New Delhi<br />
Tel.: 011-23232400 Ext. 4545, 4222 • E-mail : asmita.rathore@yahoo.com • website : www.aogd.org
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
Editor<br />
Dr Vijay Zutshi<br />
9818319110<br />
Co-Editor<br />
Dr sarita s Kale<br />
9868392748<br />
Dr K agarwal<br />
9968604350<br />
Dr shaKun tyagi<br />
9013447287<br />
<strong>AOGD</strong> Bulletin<br />
Volume 10 <strong>July</strong> <strong>2010</strong> Monthly Issue 3<br />
<strong>AOGD</strong> Office BeArers <strong>2010</strong>-11<br />
Patrons<br />
Dr anusuya Das<br />
9868511137<br />
Dr sn MuKerjee<br />
011-22523178<br />
Dr s Batra<br />
9968604338<br />
HosPitality sECrEtary<br />
Dr suDha prasaD<br />
9968604341<br />
Jt HosPitality sECrEtary<br />
Dr gauri ganDhi<br />
9968604344<br />
Dr MuMtaZ Khan<br />
9868392797<br />
Dr Deepti goswaMi<br />
9968604348<br />
PrEsidEnt<br />
Dr usha ManaKtala<br />
9968604339<br />
Joint sECrEtary<br />
Dr sangeeta gupta<br />
9968604349<br />
Dr DeVenDer<br />
9650520360<br />
Hon sECrEtary<br />
Dr asMita rathore<br />
9968604345<br />
WEb-Editor<br />
Dr ashoK KuMar<br />
9810261473<br />
Co-WEb Editor<br />
Dr latiKa sahu<br />
9968604400<br />
Dr renu tanwar<br />
9968604352<br />
Dr shiKha sharMa<br />
9868392747<br />
Ex-offiCio mEmbErs<br />
Dr. s prateeK Dr. renuKa sinha<br />
ExECutiVE mEmbErs<br />
ViCE-PrEsidEnt<br />
Dr reVa tripathi<br />
9968604340<br />
trEasurEr<br />
Dr y M Mala<br />
9968604347<br />
Joint trEasurEr<br />
Dr MaDhaVi gupta<br />
9968604351<br />
Dr ChanDan DuBey<br />
9871489719<br />
aCadEmiC sECrEtary<br />
Dr raKsha arora<br />
9968604342<br />
Jt aCadEmiC sECrEtary<br />
Dr sangeeta Bhasin<br />
9868392788<br />
Dr leena waDhwa<br />
Pub rElations sECrEtary<br />
Dr anjali teMpe<br />
9868604343<br />
Jt Pub rElations sECrEtary<br />
Dr poonaM sChDeVa<br />
9811515144<br />
Dr raChna sharMa<br />
9868830202<br />
Dr pushpa panDey<br />
Dr. a KuMar Dr. s Bhasin Col. B s Duggal<br />
Dr. s Bathla Dr. r Chitra Dr. s FoteDar<br />
Dr. i ganguli Dr. sangeeta gupta Dr. t gupta<br />
Dr. M gouri DeVi Dr. shiVlata gupta Dr. up jha<br />
Dr. s B Khanna Dr. s MaliK Dr. r Mehra<br />
Dr. a Kriplani Dr. s Mittal Dr. s salhan<br />
Dr. p singh Dr. s s triVeDi Dr. n B VaiD<br />
Contents<br />
• From the Editor’s Pen ..............................................................04<br />
• Secretary’s Message .................................................................05<br />
• Rational use of Oral Iron Therapy in Pregnancy ..............06<br />
• Journal Scan ..................................................................................11<br />
• Proceedings of the <strong>AOGD</strong> Clinical Meeting<br />
at Indraprastha Apollo Hospitals, Sarita Vihar,<br />
New Delhi on 25th June, <strong>2010</strong> ...............................................17<br />
• Next Clinical Meeting ...............................................................18<br />
• RCOG Green-top Guideline Summarized by<br />
RCOG- AICC, North Zone-Management<br />
of Monochorionic Twin Pregnancy ....................................19<br />
Disclaimer<br />
The advertisements in this bulletin are not a warranty, endorsement or approval of the products<br />
or services. The statements and opinions contained in the articles of the <strong>AOGD</strong> Bulletin are solely<br />
those of the individual authors and contributors, and do not necessarily reflect the opinions or<br />
recommendations of the publisher. The publisher disclaims responsibility of any injury to persons<br />
or property resulting from any ideas or products referred to in the articles or advertisements.<br />
Printed, Published & Edited by<br />
Dr Vijay Zutshi, Editor <strong>AOGD</strong> on behalf of Association of Obstetricians and Gynaecologists of Delhi.<br />
Published at <strong>AOGD</strong> Secretariat, Department of Obstetrics & Gynaecology, Maulana Azad Medical<br />
College, New Delhi 110 002, India,<br />
Tel.: 011-23232400 Ext. 4405.<br />
Printed at<br />
Process & Spot C-112/3, Naraina Industrial Area, Phase - 1, New Delhi 110 028<br />
3
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
4<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
Dear Friends,<br />
Despite the National programmes anemia is one of the leading indirect causes of maternal<br />
mortality in India. We all know iron supplements are available in various forms. How to<br />
choose the correct form for your patient, when to take, what to avoid with iron supplements<br />
has been beautifully highlighted in the review article by Dr. Goswami. If you recommend an<br />
iron supplement, consider the type of iron and pill, as well as the cost. The guidelines on the<br />
dilemma of managing monochorionic twin has been summarised for our members. Journal<br />
scan as usual gives you the abstracts of situations faced by all of us in day to day practice.<br />
Suggestions and contributions are invited from the members.<br />
Dr. Vijay Zutshi<br />
From the Editors Pen<br />
“Knowledge is of no value unless you put it into practice.”<br />
Anton Chekhov quotes (Russian playwright and master of the modern short story, 1860-1904)<br />
Dr. Bharti Minocha MD, FICMCH, FICOG<br />
Formerly Consultant, Associate Professor, Safdarjung Hospital & VMMC, New Delhi<br />
Presently Consultant at:<br />
Rockland Hospital<br />
Institutional Area<br />
Katwaria Sarai, New Delhi<br />
Tel.: 011-41222222, 41688756/765 Time: 9.00am-11.00am, Tue. - Sat.<br />
Aakash Hospital<br />
90/43, Malviya Nagar, New Delhi<br />
Tel.: 011-40504111 Time: 11:00am - 12:00am, Mon., Wed., Sat.<br />
Paras Hospital<br />
Sushant Lok 1, Gurgaon<br />
Tel.: 0124-4585555 Time: 5:00pm - 7:00pm, Tue., Thur., Fri.<br />
Appointment Requests<br />
Mob.: 9811473626 E-mail: minochab@yahoo.com
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
Dear Friends,<br />
Greetings from <strong>AOGD</strong>.<br />
Environment Day was celebrated on 5th of June. Significance of environment in women’s’<br />
health is vital. Physical environment in terms of pollution free air, hygienic surroundings<br />
are generally important and family environment with focus on nutrition, status in family,<br />
access to healthcare have direct impact. We all should use this opportunity to sensitize<br />
ourselves and our clients regarding importance of healthy environment.<br />
Brief account of activities for month of June is given below. Many activities are planned<br />
for future apart from monthly clinical meeting. Please participate in them in large numbers.<br />
Your suggestions are valuable to us.<br />
Best regards<br />
Dr. Asmita Rathore<br />
Secretary’s Message<br />
Forthcoming Events<br />
1. “Symposium on Evidence to Action” for reducing maternal and neonatal morbidity and mortality on 17th-18th <strong>July</strong>, <strong>2010</strong><br />
at JLN Auditorium, AIIMS. Organized by Deptt of Obst. & Gynae., AIIMS in collaboration with MOHFW and WHO.<br />
2. Workshop on “Endoscopy Upadate <strong>2010</strong>” on 18th <strong>July</strong>, <strong>2010</strong> at P.S.K., Laxminagar district centre, under aegis of <strong>AOGD</strong> &<br />
IFS, KJIVF & Laparoscopy Centre, Delhi.<br />
3. Next Clinical Monthly meeting of <strong>AOGD</strong> will be held on 30th <strong>July</strong>, <strong>2010</strong> at Army Hospital, New Delhi.<br />
4. Thirteenth Practical course & CME in Obstetrics & Gynaecology is being held from 6th to 8th August, <strong>2010</strong>. for details<br />
contact Dr. Y. M. Mala, M.: 9968604347.<br />
5. National CME on Obstetrics & Gynecology Module 3 on 28-29th August, <strong>2010</strong> at AIIMS. For registration, please contact<br />
Dr. Neeta Singh, M.: 9868397311.<br />
6. 32nd Annual Conference of <strong>AOGD</strong> will be held on from 30th & 31st October, <strong>2010</strong> at Maulana Azad Medical College, N, D.<br />
7. Colposcopy Worskhop will be held on 31st <strong>July</strong>, <strong>2010</strong> at Sir Gangaram Hospital, New Delhi. For details contact: Dr Harsha<br />
Khullar, M.: 09414170555, Email: azadanita@rediffmail.com<br />
Thirteenth Practical Course & CME for Post Graduates from 6th - 8th Augest, <strong>2010</strong> at MAMC, New Delhi for details<br />
contact Dr. Y. M. Mala M.: 09968604347 or Dr. Madhavi M.: 09968604351<br />
Events Held<br />
1. IMA JANAKPURI GYNAE CLUB organised CME on 3rd June at Medico House Janakpuri under the aegis of <strong>AOGD</strong>.<br />
Dr Narender Malhotra & Dr Jaideep Malhotra delivered a talk on IUGR & CONGENITAL ANOMALIES.<br />
2. Live Workshop on Pelvic Surgery on 12th June, <strong>2010</strong> at Artemis Hospital, Gurgaon, Organized by Sunrise Keyhole<br />
Surgery Foundation & <strong>AOGD</strong>.<br />
3. South Delhi Gynae Forum & SJH conducted CME on DUB on 24th June, <strong>2010</strong>.<br />
4. <strong>AOGD</strong> Clinical meeting was held on 25th June, <strong>2010</strong> at Apollo Hospital.<br />
5. Part I MRCOG Course was held at RCOG NZ Centre, CR Park on 20th June, <strong>2010</strong>.<br />
5
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
6<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
REVIEW ARTICLE<br />
Rational use of Oral Iron Therapy in Pregnancy<br />
Dr Deepti Goswami, Professor, Obst. & Gynae., Maulana Azad Medical College, New Delhi<br />
BURDEN OF IRON DEFICIENCY ANEMIA _______<br />
In a study of pregnant womne in urbam Delhi slums, it was<br />
found that 85.4% pregnant women had hemoglobin levels<br />
below 11.0 g/dl. The prevalence of mild (Hb level 10-10.9<br />
g/dl)), moderate (Hb level 7.0-9.9 g/dl) and severe anemia<br />
(Hb level 6.9 g/dl and below) was 30.4%,53.5% and 1.5%,<br />
respectively 1 .<br />
Iron metabolism is controlled by absorption rather than<br />
excretion 2 .<br />
Iron absorption<br />
• Occurs mostly in the duodenum and proximal jejunum.<br />
• Only 5 to 10 percent of dietary intake of iron gets<br />
absorbed.<br />
• The amount of elemental iron absorbed in the gut<br />
can vary significantly depending on several factors,<br />
including hemoglobin level and body iron stores.<br />
• In states of overload, absorption decreases.<br />
• Absorption can increase three- to fivefold in states<br />
of depletion. The decline in iron status that normally<br />
accompanies pregnancy results in an increase in the<br />
efficiency of absorption of dietary or supplemental iron.<br />
Dietary iron is available in two forms<br />
• Heme iron (meat) - its absorption is minimally affected<br />
by dietary factors.<br />
• Nonheme iron (plants, dairy foods)- requires acid<br />
digestion and its bioavailability varies depending on<br />
the concentration of enhancers (e.g., ascorbate, meat)<br />
and inhibitors (e.g., calcium, fiber, tea, coffee, wine) in<br />
the diet.<br />
Iron deficiency state<br />
• Iron stores are depleted before iron deficient<br />
erythropoiesis occurs.<br />
• Three years of a severely iron deficient diet (less than<br />
1-2 mg/d) or acute hemorrhage of two liters (0.4 mg<br />
elemental iron per ml whole blood) will both cause a<br />
complete loss of iron stores.<br />
• The loss of iron stores is reflected in the blood by a<br />
reduction in serum ferritin and reduced levels / of iron<br />
bound to transferrin. Serum ferritin levels
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
It has a pleasant taste and does not cause prominent<br />
gastrointestinal irritation. However most clinical<br />
studies have shown that it has variable and generally<br />
poor bioavailability.<br />
• Carbonyl iron is elemental iron, not an iron salt. It is<br />
a small particle preparation of highly purified metallic<br />
iron. Its rate of absorption depends on the production<br />
of gastric acid (which is required to make carbonyl<br />
iron soluble). Thus it enters the body much more<br />
gradually than other types of iron that can dissolve<br />
rapidly. Bioavailability is approximately 70% of<br />
a similar dose of ferrous sulfate. This slow rate of<br />
solubilization minimizes the toxicity of carbonyl<br />
iron.<br />
• Delayed release and enteric-coated iron<br />
preparations are better tolerated than the nonenteric<br />
coated tablets. However, they are less effective<br />
since they may contain less iron and their iron may not<br />
be released in the duodenum, where iron is absorbed.<br />
In fact, patients who have been treated unsuccessfully<br />
with enteric-coated and prolonged-release iron<br />
preparations may respond well to the administration<br />
of nonenteric-coated ferrous salts.<br />
b. Other ingredients in iron preparations<br />
Indian market is flooded with preparations containing iron,<br />
vitamins, minerals, and other micronutrients.<br />
Only preparations containing iron and folic acid (in appropriate<br />
amounts) are rational and recommended by the WHO.<br />
• Zinc salts act as competitors of iron absorption and<br />
thus decrease its absorption.<br />
• When present in an amount of 200mg or more,<br />
ascorbic acid (vitamin C) increases the absorption of<br />
medicinal iron by at least 30%. However, the increased<br />
uptake is associated with a significant increase in<br />
the incidence of side effects including destruction of<br />
the intestinal mucous membrane when put to over<br />
work. Therefore, the addition of ascorbic acid seems<br />
to have little advantage over increasing the amount<br />
of iron administered. (Goodman & Gilman, The<br />
Pharmacological Basis of Therapeutics, 11th edition)<br />
• Copper deficiency is extremely rare in human beings.<br />
• Oral treatment with pyridoxine is of benefit in<br />
correcting anemia associated with consumption of<br />
anti-tuberculosis drugs.<br />
• Haemoglobin per se is a poor source of elemental<br />
iron absorbed by the body. The source of haemoglobin<br />
is blood of animals killed in slaughter houses. No<br />
standard textbooks of medical sciences or medical<br />
journals mention the use of haemoglobin as a drug.<br />
Haemoglobin containing iron preparations are banned<br />
since year 2000.<br />
• Some preparations contain liver extract and even<br />
alcohol. Government notifications have banned<br />
combinations containing liver extract.<br />
c. Administering oral iron 3<br />
• Aim is to provide a daily dose of 150-200 mg of<br />
elemental iron. This would require prescribing one<br />
ferrous sulfate tablet 3 times daily. Since each tablet<br />
contains approximately 60 mg of elemental iron.<br />
Assuming that 10% of the iron is absorbed, the<br />
hemoglobin concentration may fully correct after 4<br />
weeks in patients with moderate, uncomplicated iron<br />
deficiency (about 500–800 mg of iron, enough for 500<br />
to 800 ml of packed red blood cells, or enough to raise<br />
the whole blood hemoglobin 2–3 g/dl).<br />
• Iron tablets are recommended between meals or at<br />
bedtime to avoid the alkalinizing effect of food and to<br />
take advantage of the peak gastric acid production late<br />
at night.<br />
• Although iron absorption occurs more readily when<br />
taken on an empty stomach, this increases the<br />
likelihood of stomach upset because of iron therapy.<br />
Increased patient adherence should be weighed against<br />
the inferior absorption.<br />
• Foods rich in tannates (e.g., tea) or phytates (e.g.,<br />
bran, cereal), or medications that raise the gastric pH<br />
(e.g., antacids, proton pump inhibitors, histamine H2<br />
blockers) reduce absorption and should be avoided if<br />
possible.<br />
• Iron absorption can be increased by addition of citrus<br />
fruits. In contrast, tea inhibits iron absorption so one<br />
should wait 1-2 hours after the meal before drinking<br />
tea or alternatively, remove tea from their diet.<br />
• Absorption is also delayed with tetracyclines, milk,<br />
and phosphate-containing, carbonated beverages<br />
such as soft drinks. Even the calcium, phosphorus<br />
and magnesium salts contained in iron-containing<br />
multivitamin pills impair absorption of elemental<br />
iron. Hence multivitamin preparations should not be<br />
recommended as a sole therapy for iron deficient anemia.<br />
• The effect of calcium and milk is similar. When calcium<br />
carbonate is taken concurrently with ferrous<br />
sulphate; the iron absorption can be reduced by<br />
two-thirds.<br />
• Some persons have difficulty absorbing the iron<br />
because of poor dissolution of the coating. A liquid iron<br />
preparation would be a better choice for these patients.<br />
d. Side effects of oral iron and their management<br />
• Side effects of oral iron are directly related to the<br />
amount of elemental iron, administered. Hence side<br />
effects are much less with preparations which have<br />
much lower elemental iron content than anhydrous<br />
ferrous sulphate.<br />
• Laxatives, stool softeners, and adequate intake of<br />
liquids can alleviate the constipating effects of oral iron<br />
therapy.<br />
• If a patient is intolerant to the recommended dose of<br />
150-200mg of daily elemental iron, dose reductions<br />
are applied. Changes in iron salts (and hence elemental<br />
7
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
8<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
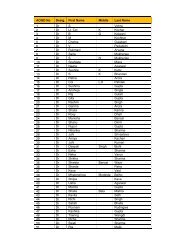
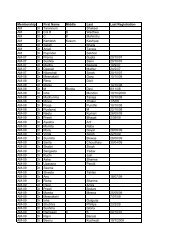
Table 1: Ferrous sulphate preparations (Elemental iron 37% in anhydrous/ dried ferrous sulphate, 20% in regular ferrous sulphate):<br />
S. No. Drug Pharma Co. Ferrous<br />
sulphate<br />
1. Conviron TR<br />
[cap]<br />
2. Elferri TR<br />
[cap]<br />
3. Fefol<br />
[spansule]<br />
4. Fefol-Z<br />
[spansule]<br />
Carbonyl iron<br />
5. Fesovit<br />
spansule<br />
[cap]<br />
6. J.P. tone TR<br />
[TR tab]<br />
Ranbaxy<br />
(Pharma)<br />
Swizera<br />
(ACE)<br />
Glaxo Smith<br />
Kline<br />
Glaxo Smith-<br />
Kline<br />
Glaxo Smith<br />
Kline<br />
Folic acid Vit B12 Other content Packing/<br />
Price<br />
(Dried) 60mg 1.5 mg 15 µg Vit B6, Vit C 15’s<br />
(Rs. 55.35)<br />
(Dried) 60 mg 1.5 mg 15 µg Vit B6, Vit C 15’s<br />
(Rs.54)<br />
150 mg 0.5 mg x x 15’s (Rs.<br />
46.5)<br />
150 mg 0.5 mg x zinc 15’s<br />
(Rs.65.90)<br />
150 mg 1 mg 15 µg vit B6,<br />
nicotinamide<br />
30’s<br />
(Rs. 87.7)<br />
Jagsonpal (Dried) 150 mg 0.5 mg x zinc 1x15<br />
(Rs. 48)<br />
Table 2: Ferrous fumarate preparations (Elemental iron 33%):<br />
S. No. Drug Pharma<br />
Co.<br />
Ferrous<br />
fumarate<br />
Apprx<br />
cost / tab<br />
Rs. 3.6<br />
Rs. 3.6<br />
Rs. 3<br />
Rs. 4.4<br />
Rs. 3<br />
Rs. 3.2<br />
Folic acid Vit B12 Other content Packing/ Price Approx cost<br />
/ tablet<br />
1. Autrin [cap] Wyeth 300mg 1.5 mg 15 µg x 30’s (Rs 36.60) Rs. 1.3<br />
2. Dumasules<br />
[cap]<br />
3. Elferri Z [cap] Swizera<br />
(ACE)<br />
Unimed 300mg 0.75 mg 7.5 µg vit C, Vit B1, Vit<br />
B, Niacinamide<br />
10’s (Rs. 11.56) Rs.1.1<br />
200mg 1.5mg 15 µg zinc 30’s (Rs. 35.65) Rs.1.1<br />
4. Hemsi [cap] Serum Intl 300 mg 1.5mg 5µg zinc, copper,<br />
manganese,<br />
lysine<br />
5. Globac Z [sg<br />
cap]<br />
6. Haem Up<br />
Gems [cap]<br />
7. Hembran plus<br />
[cap]<br />
Zydus<br />
Nutriva<br />
15’s (Rs. 31.50) Rs.2<br />
152 mg 1.5mg 15µg zinc 30’s (Rs 77.20) Rs.2.5<br />
Cadila 200mg 1.5mg x Copper,<br />
manganese<br />
30’s (Rs 67.07) Rs 2.2<br />
Brawn 300 mg 1.5mg 15µg vit C, vit B6 10’s (Rs. 20) Rs.2<br />
8. Hemsi [cap] Serum Intl 300 mg 1.5mg 5µg zinc, copper,<br />
manganese,<br />
lysine<br />
9. Livogen FC<br />
[captab]<br />
15’s (Rs. 31.50) Rs.2<br />
Merck 152 mg 1.5 mg x x 10’s (Rs 18.33) Rs.1.8<br />
10. Softeron [cap] Aristo 165mg 0.75 mg x Docusate sodium 15’s Rs. (17.20) Rs.1.1<br />
11. Vitcofol [cap] FDC<br />
(Select)<br />
12. Ziferrin TR<br />
[cap]<br />
300 mg 0.75 mg 7.5 µg zinc, vit B6 15’s (Rs 24.3) Rs.1.6<br />
Zydus cadila 200mg 1mg 10µg zinc 10’s (Rs. 20.44) Rs.2<br />
Table 3: Ferrous gluconate preparations (Elemental iron 12%):<br />
S. No. Drug Pharma Co. Ferrous<br />
gluconate<br />
1. J.P. tone<br />
[syr]<br />
2. Mulmin<br />
plus<br />
3. R.B.tone<br />
[cap]<br />
Jagsonpal 200 mg<br />
/10ml<br />
Folic acid Vit B12 Other content Packing/Price Approx cost /<br />
tablet<br />
x 2.5 µg Multivitamins,<br />
D-panthenol<br />
Juggat 50 mg 0.25 mg 5 µg Multivitamins, vit<br />
A,D,E,C<br />
Medley<br />
Nutrakare<br />
200 ml (Rs. 75) Rs 3.7/10ml<br />
10 (Rs. 40) Rs. 4<br />
259 mg 2.5 mg 2.5 mg zinc, calcium 15’s (Rs. 36) Rs. 2.4
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
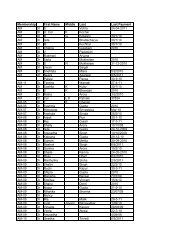
Table 4: Ferrous glycine sulfate preparations (Elemental iron 23%):<br />
S.<br />
No.<br />
1. Fecontin-F<br />
[CR- tab]<br />
2. Fecontin-Z<br />
[CR- tab]<br />
3. Hemfer<br />
[cap]<br />
Drug Pharma<br />
Co.<br />
Modi<br />
Mundi<br />
Modi<br />
Mundi<br />
Ferrous glycine<br />
sulfate<br />
Folic acid Vit B12 Other<br />
content<br />
Packing/Price Approx cost /<br />
tablet<br />
100 mg 0.5 mg x x 120’s (Rs. 558.6) Rs. 4.6<br />
100 mg 0.5 mg x zinc 10’s (Rs. 62.9) Rs. 6.3<br />
Alkem 50 mg 0.5 mg 7.5 µg zinc, vit C<br />
75 mg<br />
Table 5: Ferric ammonium citrate (Elemental iron 18%):<br />
S. No. Drug Pharma<br />
Co.<br />
1. Dexorange<br />
[cap]<br />
2. Dexorange<br />
[syr]<br />
Franco-<br />
Indian<br />
Franco-<br />
Indian<br />
3. Globac liq Zydus<br />
Alidac<br />
4. Haem Up<br />
liquid<br />
Ferric ammonium<br />
citrate<br />
Folic acid Vit B12 Other<br />
content<br />
10’s (Rs. 22) Rs. 2.2<br />
Packing/<br />
Price<br />
160 mg 0.5 mg 7.5 µg zinc 30’s (Rs.<br />
54.42)<br />
160 mg/15ml 0.5 mg 7.5 µg x 200 ml<br />
(Rs. 59.90)<br />
60 mg/15 ml 1 mg 12.5 µg zinc 200 ml (Rs.<br />
43.86)<br />
Cadila 160 mg /15ml 0.5 mg 7.5 µg copper,<br />
manganese<br />
Table 7: Iron (III) hydroxide polymaltose complex (iron 46%):<br />
S. No. Drug Pharma Co. Iron (III) hydroxide<br />
polymaltose<br />
1. Globac-PM<br />
[tab]<br />
Zydus<br />
(Alidac)<br />
2. Fegem [tab] Torrent 50 mg 100<br />
mg<br />
Folic acid Vit B12 Other<br />
content<br />
200ml (Rs<br />
50.95)<br />
Packing/<br />
Price<br />
100 mg 1.5 mg x x 10’s<br />
(Rs. 39.78)<br />
0.175 mg<br />
0.35 mg<br />
x x 10’s<br />
(Rs. 26.5) 10’s<br />
(Rs. 49)<br />
Approx cost /<br />
tablet<br />
Rs. 1.8<br />
Rs. 4.5/15 ml<br />
Rs. 3.3/15 ml<br />
Rs 3.75/ 15ml<br />
Approx cost/<br />
tablet<br />
3. Femed [tab] Comed 100 mg 1 mg x x 10’s (Rs. 42) Rs. 4.2<br />
4. Fericip chew<br />
tab<br />
Cipla 100 mg 0.35 mg x x 10’s (Rs. 45) Rs. 4.5<br />
5. Ferium [cap] Emcure 100 mg 1 mg x x 10’s (Rs. 45) Rs. 4.5<br />
6. Ferose [cap] CFL 50 mg 0.35 mg x x 10’s (Rs. 42) Rs. 4.2<br />
7. Mumfer [chw<br />
tab]<br />
Table 8: Other iron preparations in the market:<br />
S. No. Drug Pharma<br />
Co.<br />
1. Anofer Sun pharma Carbonyl<br />
iron 120<br />
mg<br />
Glenmark 100 mg 0.5 mg x 30’s<br />
(Rs.148.8)<br />
2. Safiron [cap] Khandelwal Carbonyl<br />
iron 100mg<br />
3. FeriumXT<br />
[cap]<br />
Emcure<br />
Schweiz<br />
Rs. 5<br />
Rs. 4<br />
Rs. 5<br />
Iron Folic acid Vit B12 Other content Packing/Price Approx cost<br />
/tablet<br />
Ferrous<br />
ascorbate<br />
100 mg<br />
iron per tablet) and formulations are commonly tried.<br />
One may also try dose reductions by lengthening the<br />
dose interval. This may permit iron-intolerant patients<br />
to continue oral therapy, and avoid parenteral therapy.<br />
However lowering the daily iron dose would require a<br />
longer duration of therapy.<br />
1.5mg 12µg Multivitamin,<br />
Sodium Docusate<br />
10’s 47 Rs 4.7<br />
1.5mg 10µg Zinc, selenium, vit E 3x10 (Rs. 400) Rs 13.3<br />
1.5 mg x x 10’s (Rs.72.95) Rs 7.3<br />
e. Response to therapy<br />
• Patients with iron deficient anemia should manifest a<br />
response to iron with reticulocytosis in three to seven<br />
days.<br />
• An increase in the hemoglobin level of 1 g per dl should<br />
9
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
10<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
occur every two to three weeks on iron therapy.<br />
• Theoretically, 500 mg of absorbed iron should produce<br />
500 cc of packed cells, or enough to raise the hemoglobin<br />
by about 2 g/dl.<br />
An insufficient response may be due to:<br />
• ongoing blood loss<br />
• malabsorption due to anatomical or inhibiting factors<br />
e.g. antacids or tea<br />
• incorrect diagnosis<br />
• noncompliance<br />
TR-timed release CR-controlled release<br />
• There are hundreds of products listed in drug formularies.<br />
In this article an effort has been made to include some of<br />
the marketed drugs in Delhi.<br />
• The prices are what are available on the website www.<br />
mims.com<br />
It is worthwhile to note that:<br />
• Similar names may have different iron preparations<br />
e.g.:<br />
FORTIS BLOOM IVF CENTRE<br />
Fortis La Femme Hospital, New Delhi<br />
• Globac PM (Iron (III) hydroxide polymaltose), Globac<br />
Z (ferrous fumarate) & Globac liq (ferric ammonium<br />
citrate).<br />
• Ferium (Iron (III) hydroxide polymaltose) & Ferium XT<br />
(Ferrous ascorbate)<br />
• Haem up gems (ferrous fumarate) & Haem Up liq<br />
(ferric ammonium citrate)<br />
• JP tone syrup (ferrous gluconate) & JP tone TR tablet<br />
(ferrous sulphate).<br />
• Different brands containing same iron preparation may<br />
contain different amount of iron, so when calculating<br />
the cost of daily therapy due consideration should be<br />
given to the amount of iron in the tablet and number<br />
of tablets required in a day.<br />
REFERENCES _______________________________<br />
1. Killip S, Bennett JM, Chambers MD. Iron deficiency anemia. Am<br />
Fam Physician. 2007; 75:671-8.<br />
2. Mukherji J. Iron deficiency anemia in pregnancy. Rational Drug<br />
Bull. 2002; 12:2-5.<br />
3. Brise H, Hallberg L. Absorbability of different iron compounds.<br />
Acta Med Scand Suppl. 1962; 376:23-37.<br />
Proudly announces for 1st time in North India IMSI. Initiated the technique of IMSI (Intracytoplasmic<br />
Morphologically selected Sperm Injection) for enhancing ICSI results.<br />
Other Services<br />
• IVF for Blocked tube.<br />
• ICSI, PESA, TESE for males with low counts or no count.<br />
• Egg donation for women more than 40 years of age.<br />
• Surrogacy for those who can’t carry their pregnancy.<br />
• Laser hatching, cumulus assisted transfer (CAT) &<br />
blastocyst culture for women who fail repeatedly with<br />
IVF/ICSI.<br />
• Oocyte freezing for women who want to bank their<br />
eggs for future use.<br />
• Ovarian tissue freezing for young cancer patients;<br />
semen donation for men with no sperms.<br />
• Semen bank for patients undergoing chemotherapy /<br />
radiation. Embryo freezing with the latest technique of<br />
Vitrification, for women with extra embryos following IVF.<br />
• Intracytoplasmic Morphologically selected sperm<br />
transfer (IMSI) to improve pregnancy rates following<br />
ICSI for male factor infertility.<br />
FOR APPOINTMENTS:<br />
Fortis La Femme Hospital<br />
S-549, G.K. - II, New Delhi 110 048<br />
Our Success Rates<br />
We are happy to inform you that our clinical pregnancy<br />
rates in women less than 35 years of age have reached<br />
40% to 45% per attempt. Our live baby rates are in the<br />
range of 25 to 30% per patient, which is similar to the<br />
rates in the west. The success goes down with advancing<br />
age. Hence early recourse to IVF/ICSI is essential.<br />
IVF Consultant - Mumbai<br />
Dr. Hrishikesh Pai Dr. Nandita Palshetkar<br />
09820057722 09820032315<br />
hdpai@hotmail.com nanditapalshetkar@hotmail.com<br />
Dr. Rishma Pai Dr. Jaya Gogate<br />
09821016005 09820723682<br />
IVF Consultant - Delhi<br />
Dr. Parul Katiyar Dr Seema Bajaj<br />
9313328177 9810577494<br />
Ms. Anchal, Ms Navneet, # 9350887858, 29220125 40579493, 40579400<br />
Email: ivflafemme@fortishealthcare.com<br />
Web site: www.infertilityindia.com, www.1to9months.com
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
Journal Scan<br />
Dr Shakun Tyagi, Dr Neha Singh, Dr Ayesha Arif, Dr Seema Beniwal<br />
WHAT MEASURED BLOOD LOSS TELLS US<br />
ABOUT POSTPARTUM BLEEDING: A SYSTEMATIC<br />
REVIEW. (BJOG <strong>2010</strong>;117:788–800) ___________<br />
Sloan NL, Durocher J, Aldrich T, Blum J, Winikoff B<br />
Objectives: Systematic review of measured postpartum<br />
blood loss with and without prophylactic uterotonics for<br />
prevention of postpartum hemorrhage (PPH).<br />
Methods: 29 studies with objective measurement of blood<br />
loss after delivery were evaluated. Most of the studies<br />
measured blood loss by placing a bedpan underneath the<br />
parturient woman. The collected blood was poured into a jar<br />
for volume measurement, and all soaked gauze pads were<br />
counted and weighed. A few studies used the fairly new<br />
blood collection sheet or delivery drape to calculate blood loss.<br />
Results: The distribution of average blood loss is similar<br />
with any prophylactic uterotonic, and is lower than without<br />
prophylaxis. Compared with no uterotonic, oxytocin and<br />
misoprostol have lower PPH (≥500 ml) and severe PPH<br />
(≥1000 ml) rates. Oxytocin has lower PPH and severe PPH<br />
rates than misoprostol.<br />
Conclusion: Oxytocin is superior to misoprostol in<br />
hospitals. Although oxytocin is superior, misoprostol<br />
substantially lowers PPH and severe PPH. A sound<br />
assessment of the relative merits of the two drugs is needed<br />
in rural areas, where most PPH deaths occur.<br />
RISK OF UTERINE RUPTURE ASSOCIATED WITH<br />
AN INTERDELIVERY INTERVAL BETWEEN 18 AND<br />
24 MONTHS (OBSTETRICS & GYNECOLOGY, MAY<br />
<strong>2010</strong>;115,( 5): 1003-6) _______________________<br />
Bujol E, Gauthier R<br />
Objective: To estimate the association between interdelivery<br />
interval and uterine rupture in women with a<br />
previous cesarean delivery<br />
Methods: Secondary analysis was performed in a<br />
retrospective cohort study of women who underwent a trial<br />
of labor after undergoing a previous cesarean delivery. Only<br />
singleton pregnancies with a trial of labor at term were<br />
included. The rates of uterine rupture were compared among<br />
women with interdelivery intervals 24 months or longer<br />
(controls), 18–24 months, and fewer than 18 months. The<br />
student t test and multivariable logistic regression analysis<br />
were conducted. A P value of less than .05 was considered<br />
significant.<br />
Results: Of the 1,768 women analyzed, 1,323 (74.8%)<br />
had an interdelivery interval of 24 months or longer, 257<br />
(14.5%) had an interval between 18 and 24 months, and 188<br />
(10.6%) had an interval of less than 18 months. The rate of<br />
successful VBAC (70%, 74%, and 73%, respectively; P=0.28)<br />
not different across the three groups. After adjustment for<br />
confounding variables, an interdelivery interval less than 18<br />
months was associated with a significant increase of uterine<br />
rupture (odds ratio [OR], 3.0; 95% confidence interval [CI],<br />
1.3–7.2), whereas an interdelivery interval between 18 and<br />
24 months was not (OR, 1.1; 95% CI, 0.4 –3.2)<br />
Conclusion: The risk of uterine rupture was significantly<br />
higher in women with an interdelivery interval less than 18<br />
months than in women with an interval of 24 months or<br />
longer, but not in women with an interval between 18 and<br />
23 months. An interdelivery interval less than 18 months<br />
was an independent and an important factor associated<br />
with uterine scar defect, after adjustment for a uterine<br />
scar thickness less than 2.3 mm and a previous single-layer<br />
closure of the uterus.<br />
PROGESTOGEN TREATMENT OPTIONS FOR<br />
EARLY ENDOMETRIAL CANCER (BR J OBSTET<br />
GYNAECOL <strong>2010</strong>;117:879–84) ________________<br />
Cade TJ, Quinn MA, Rome RM, Neeshama D<br />
Objective: Analysis of cancer-free outcome and fertility<br />
potential with progestogen therapy for early endometrial<br />
cancer.<br />
Methods: Sixteen patients receiving progestogen therapy<br />
for stage-1 grade-1 endometrial cancer were retrospectively<br />
reviewed and their response to treatment, duration of<br />
response and fertility outcome in a specialist gynaecological<br />
oncology unit at a tertiary hospital was evaluated.<br />
Results: Of the 16 patients, four received an oral<br />
progestogen, three received levonorgestrel-releasing<br />
intrauterine system (Mirena), and nine received both forms<br />
of treatment. Response to therapy was assessed by disease<br />
regression on serial endometrial curettage. Ten patients<br />
(63%) responded to treatment, with a median time to<br />
response of 5.5 months. Six patients did not respond, but<br />
they were either early in treatment or opted for surgical<br />
management before the average time of response. No<br />
patient who responded had a later recurrence. The mean<br />
follow-up time was 27 months (range 3–134 months),<br />
with no patient deaths. Three patients had successful<br />
pregnancies.<br />
11
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
12<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
Conclusions: Progestogen therapy appears to be a realistic<br />
treatment option in selected patients in the closely<br />
supervised environment of a specialist gynecological<br />
10:00 – 10:20am Registration<br />
10:20 – 10:30am Welcome Address<br />
Chairpersons: Prof. Neera Aggarwal,<br />
Prof. Usha Manaktala, Prof. Sudha Prasad<br />
10:30 – 10:50am Video Hysteroscopy - a underused Modality<br />
Dr.(Prof.) Kuldeep Jain<br />
10:50 – 11:00am Audience Interaction<br />
11:00 – 11:20am Understanding energy applications in<br />
Endoscopy – Dr. (Prof.) Renu Mishra<br />
11:20 – 11:30am Audience Interaction<br />
Chair: Dr Nalini Mahajan,<br />
Dr. Asmita Rathor, Dr. Vijay Zutshi<br />
11:30 – 11:50am Nuiences of endoscopic suturing<br />
Dr. Nutan Jain<br />
MEMORIAL HOSPITAL<br />
HEALTHCARE PERSONALISED<br />
KJIVF & Laparoscopy Centre, Delhi<br />
in association with <strong>AOGD</strong> & IFS Organizes<br />
“Endoscopy Update <strong>2010</strong>”<br />
on 18th <strong>July</strong> <strong>2010</strong>, Sunday 10am to 2pm<br />
at P.S.K Laxminagar District Centre<br />
DR. (MS) S. K. DAS<br />
MD, FICOG, FIAMS<br />
HOD, Dept. of Gynae- Oncology<br />
Former HOD, Safdarjung Hospital<br />
Former Senior consultant, RGCI & RC and<br />
Sri Balaji Action Medical Institute<br />
Available for Consultantion at:<br />
B L Kapur Memorial Hospital, Pusa Road<br />
Clinic cum Residence<br />
B-202, Welcome Apts, Rohini Delhi<br />
Tel.: 9810059380, 27552151<br />
oncology unit, with a safe cancer outcome for most women<br />
and with successful pregnancy in some.<br />
11:50 – 12noon Audience Interaction<br />
12:00 – 12:20pm Endoscopic Myomectomy-when, How &<br />
by Whom? – Dr. (Prof.) Alka Kriplani<br />
12:20 – 12:30pm Audience Interaction<br />
12:30 – 01:30pm Current trends & Challenges in<br />
endometriosis – Panel Discussion<br />
Moderator : Dr. Kuldeep Jain<br />
Panelist : Dr. Sonia Malik,<br />
Dr. Sohani Verma, Dr. Neera Agarwal,<br />
Dr. Usha Manaktala, Dr. Sudha Prasad,<br />
Dr. Renu Mishra, Dr. Nutan Jain,<br />
Dr. Alka Kriplani<br />
01:30 – 02:30pm Lunch<br />
Registration Fees – Rs. 100/- only. For registration contact: Mr. Shyam 9811233711 & Ms. Anu 65253282, 22503927<br />
SPONSERED BY --- INCA (SUN PHARMA)<br />
Ultrasound & Whole Body Color Doppler Chinic<br />
Transabdominal, Transvaginal, Transrectal<br />
Sector, Concex Sector, Linear,<br />
3-D, 4-D, TUI, etc.<br />
Dr. Varun Dugal MBBS, MD (Radio-Diagnosis)<br />
Mon to Sat -9 am to 1 pm Mon to Fri - 4 pm to 6 pm<br />
C - 27, Green Park Extn., New Delhi - 110 016<br />
Tel: 011-26865531, 26967125, 26867508<br />
Help Mobile: 9958228448<br />
(Closed on Sunday - Saturday Half Day)<br />
Gynaecology Oncology Surgeon & Colposcopist<br />
DR. SHRUTI BHATIA<br />
MD, DNB, MNAMS<br />
Consultant<br />
Dept. of Gynae-Oncology<br />
Clinic<br />
I-217, Ashok Vihar, Delhi<br />
Tel.: 9811471545
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
<strong>AOGD</strong> Activities<br />
Live Pelvic Surgery Workshop jointly organized by Sunrise Keyhole Surgery Foundation and <strong>AOGD</strong><br />
on 12th June, <strong>2010</strong> at Artemis Hospital, Gurgaon.<br />
Shri Ghulam Nabi Azadji lighting the inaugural lamp. Dr Usha Manaktala, President <strong>AOGD</strong> lighting the inaugural lamp.<br />
April, <strong>2010</strong> MAMC<br />
<strong>AOGD</strong> Clinical Meeting Calendar for the year <strong>2010</strong>-2011<br />
May, <strong>2010</strong> Max Super Specialty Hospital<br />
June, <strong>2010</strong> Apollo Hospital<br />
<strong>July</strong>, <strong>2010</strong> Army Hospital (R & R)<br />
August, <strong>2010</strong> AIIMS<br />
September, <strong>2010</strong> LHMC<br />
October, <strong>2010</strong> Moolchand Hospital<br />
November, <strong>2010</strong> GTB Hospital<br />
December, <strong>2010</strong> RML Hospital<br />
January, 2011 Sir Ganga Ram Hospital<br />
February, 2011 DDU Hospital<br />
March, 2011 Safdarjung Hospital<br />
April, 2011 MAMC<br />
13
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
Proceedings of the <strong>AOGD</strong> Clinical Meeting at Indraprastha<br />
Apollo Hospitals, Sarita Vihar, New Delhi on 25th June, <strong>2010</strong><br />
UTERINE ARTERIOVENOUS MALFORMATIONS-<br />
REPORT OF TWO CASES _____________________<br />
SB Khanna, Harsh Rastogi, Kiranbala Dash, Saba<br />
Uterine AV malformation is a rare cause of uterine bleeding.<br />
Clinical presentation varies from no signs over various<br />
degrees of menorrhagia to massive life -threatening vaginal<br />
bleeding. Clinical findings in such cases are unreliable and<br />
uterine curettage is not therapeutic and even aggravates<br />
at times. Therefore high index of clinical suspension is<br />
required to diagnose this condition. With availability of<br />
newer diagnostic modalities like Doppler flow USG, MRI &<br />
Pelvic angiography it has become easier to diagnose such<br />
cases. Two cases of uterine arteriovenous malformation are<br />
being presented.<br />
Case - 1: Mrs. U.S a 30years old P1A2 presented with<br />
complaints of continuous bleeding P/V for 3 months<br />
not responding to hemostats & estrogen progesterone<br />
combinations. She also had D&C done one month back<br />
(HPE: proliferative endometrium). On examination she<br />
had moderate pallor. Pelvic examination revealed a normal<br />
sized uterus. Her haemoglobin was 7gm/dl. Her USG Pelvis<br />
reaveled a 7.3cm x 4cm with hypoechoic area in posterior<br />
myometrium with internal vascularity. On color flow florid<br />
colour pattern with mosaic aliasing color flow was seen<br />
which was continuing with Right adnexal vessels and right<br />
uterine artery. She was admitted, transfused with one<br />
unit of packed red cells. After discussing all possibilities of<br />
treatment with the patient she wanted to conserve uterus<br />
for fertility. Her pelvic angiography revealed high flow AVM<br />
in right posterior part of body & fundus fed by both uterine<br />
arteries and right ovarian artery.<br />
Case-2: Mrs. H. a 45year old female P0A4 presented with<br />
pain in lower abdomen and irregular periods with heavy<br />
bleeding for 5-6 years. Her cycles were of 4-5/30-60 days but<br />
very heavy. She had 4 spontaneous early pregnancy losses<br />
followed by D&E each time. On examination uterus was of<br />
16 week size, soft and pulsations were felt in both fornices.<br />
She also had blood transfusion twice. Her USG abdomen<br />
revealed a bulky uterus with markedly tortuous and dilated<br />
vessels in myometrium and B/L adnexa suggestive of<br />
uterine arteriovenous malformation. MRI pelvis revealed a<br />
bulky uterus with multiple tortous flow voids seen involving<br />
uterus, b/L adnexal region, perivesical region in pelvic<br />
cavity with large venous pouch noted in left adnexal region.<br />
Left ovarian artery also appeared dilated and tortuous. B/L<br />
uterines appeared tortuous dilated. Pelvic angiogram was<br />
suggestive of fistulous communication noted on the left<br />
side fed by branches of left ovarian artery and draining<br />
into pelvic veins. Fistulous side was noted near the inferior<br />
aspect of left SI joints. Multiple fistulous communications<br />
noted from both uterine arteries and draining into pelvic<br />
veins. Both these cases were managed successfully with<br />
uterine artery embolization.<br />
A RARE CASE OF VAGINAL OBSTRUCTION<br />
ASSOCIATED WITH MENSTRUAL PROBLEM AND<br />
IN FERTILITY _______________________________<br />
Sushma Sinha, Jyoti Gupta<br />
Introduction<br />
Birth trauma, chemical vaginitis, carcinoma and<br />
radiotherapy are known to cause vaginal stenosis, leading<br />
to difficult sexual intercourse or scanty periods. Rarely,<br />
vaginal obstruction may be due to postmenopausal atrophy,<br />
endometriosis, or vaginitis, leading to scarring or adhesions.<br />
We report a rare case of vaginal obstruction associated with<br />
menstrual problem and infertility.<br />
Case Report<br />
A 26 year old nullipara, married for 4 years presented<br />
with inability to conceive and cyclical spotting for 2 years<br />
along with pain lower abdomen off and on specially during<br />
spotting. Abdomen was soft and non-tender. Per speculum,<br />
no projecting cervix was visualized. A small pit was seen at<br />
vault with a spot of blood and the pit could not be negotiated.<br />
Per vaginum, pelvis felt empty. Per rectum, a doubtful<br />
boggy mass was felt anterior to rectum. All investigations<br />
pertaining to infertility were normal. USG pelvis revealed<br />
a normal size uterus with short cervix. Vagina could not be<br />
clearly differentiated from fluid in anterior and posterior<br />
fornix. MRI revealed a well defined peripherally enhancing<br />
collection in posterior fornix and vagina with normal uterus<br />
and cervix. Laparoscopy was done. Uterus was normal<br />
size. No evidence of infection or endometriosis seen. No<br />
significant collection was seen in pouch of douglous. Bulge<br />
seen in posterior fornix. Speculum examination under<br />
anaesthesia revealed vault like appearance. Colpotomy<br />
was done and cream coloured pus was drained both from<br />
anterior and posterior forniceal sites. Pus was sent for AFB<br />
culture, PCR aerobic and anaerobic culture Aerobic culture<br />
revealed coagulase negative staphylococcus. Patient was<br />
sent home on antibiotics. On follow up 3 months later,<br />
she was relived of pain. Menstrual pattern was same. On<br />
speculum examination, vault was still closed and no orifice<br />
17
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
18<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
was seen. On EUA, Small opening at vault seen. No pus or<br />
blood seen. A lacrimal probe guided dissection was done<br />
around the opening at vault. Cervix was seen and held with<br />
vulsellum. A circumferential incision was given over cervix<br />
and vaginal wall stitched circumferentially over cervix. After<br />
2 months, cycles were regular without pain. Intercourse has<br />
not resumed. Speculum examination revealed a healthy<br />
looking cervix. Uterus was normal sized, mobile, nontender<br />
with free fornices, on vaginal examination.<br />
Discussion<br />
Case of vaginal stenosis are largely seen in old women<br />
resulting from carcinoma or radiotherapy. In younger<br />
women, causes are largely pertaining to trauma or pelvic<br />
surgery. Such a case of vaginal obstruction is a rare<br />
observation in literature. Infectious and anatomical<br />
etiologies have good prognosis in infertile patients provided<br />
the treatment is prompt and adequate.<br />
CHALLENGES IN DISCORDANT TWIN<br />
PREGNANCIES _______________________________<br />
Sohani Verma, Anita Kaul, Chinmayee Ratha<br />
The prevalence of multifetal pregnancies continues to rise all<br />
over the world. Despite the improved standards of antenatal<br />
care and diagnostics, at times we are still faced with some<br />
rather tricky clinical scenarios. Severe discordance among<br />
both fetuses in terms of either a structural or genetic<br />
abnormality or a severe growth restriction leading to<br />
imminent or actual intrauterine demise of one of the twins,<br />
is one of the greatest challenges in the management of twin<br />
pregnancy. Such discordance is certainly much more lethal<br />
in fortunately less prevalent monochorionic pregnancies,<br />
However, even in more common dichorionic diamniotic<br />
(DCDA) twin pregnancies, one may have to face these<br />
problems with significant medical and ethical dilemmas.<br />
We are presenting here two such cases to highlight these<br />
challenges.<br />
Case 1: The first case is about a DCDA twin pregnancy<br />
with one fetus anencephalic and the other normal cotwin.<br />
Unfortunately the anencephaly was detected only<br />
at 26 weeks of gestation due to delayed attendance for<br />
antenatal care. Since the option of selective feticide was<br />
not plausible at that gestation, a conservative approach<br />
was opted for. However the sac with the anencephalic twin<br />
developed severe polyhydramnios and caused maternal<br />
respiratory distress. After detailed counselling of the<br />
couple about the maternal and fetal risks, they opted for<br />
amnioreduction with the aim to reduce maternal distress.<br />
She was given prophylactic antenatal corticosteroids and<br />
about 2 litres of amniotic fluid was aspirated from the<br />
sac of the anencephalic twin. The mother felt relieved.<br />
The amniodrainage was repeated after three weeks due to<br />
recurrence of maternal respiratory distress. The normal<br />
twin developed signs of intrauterine growth restriction.<br />
The pregnancy continued till 34 weeks when she set into<br />
preterm labour. She had an uneventful vaginal delivery on<br />
14.06.<strong>2010</strong> with no immediate postpartum complications.<br />
The normal twin weighed 1.3kg, female, required minimal<br />
neonatal resuscitation and is presently doing well in the nursery.<br />
This case highlights the merits of conservative approach in<br />
the interest of the normal co-twin. Had the case presented<br />
earlier, selective feticide could be considered.<br />
Case 2: A 29 year old female with history of for unexplained<br />
primary infertility of 4 years duration and several failed<br />
ovarian stimulation (OS) cycles outside, was treated with<br />
OS +IUI. She conceived with a triplet pregnancy. Multifetal<br />
pregnancy reduction was performed at 8 weeks gestation<br />
and she continued with DCDA twin pregnancy normally<br />
till 22 weeks gestation. Further course of pregnancy was<br />
complicated by obstetric cholestasis, threatened preterm<br />
labour at 29 weeks, mild PIH and severe intrauterine<br />
growth restriction (IUGR) of twin II. Pregnancy was closely<br />
monitored by serial ultrasounds with colour Doppler<br />
studies. Despite being aware of the imminent death of twin<br />
II, a conscious informed decision was taken by the parents to<br />
continue the pregnancy in the interest of the comparatively<br />
healthier twin I. Twin II suffered intrauterine demise at 31<br />
weeks gestation. Pregnancy continued for further 12 days,<br />
when due to non-reassuring CTG, reduced fetal movements<br />
and moderate IUGR on ultrasound of the surviving twin,<br />
an elective LSCS was performed at 33 weeks gestation.<br />
Both mother and female baby (birth weight 1.9 kg, Apgar<br />
9/1,9/5) are healthy at the follow ups at 3 and 6 months.<br />
This case highlights the turbulent course of post infertility<br />
treatment multiple gestation. Apart from the medical<br />
problems it also addresses the difficult and controversial<br />
ethical and emotional decision making challenges faced by<br />
the parents as well as the Obstetric team.<br />
A multidisciplinary approach in a tertiary level centre with<br />
counselling and sufficient neonatal support is essential for<br />
optimizing the outcome in twin pregnancies with single<br />
fetus demise.<br />
Next Clinical Meeting<br />
Date: 30th <strong>July</strong>, <strong>2010</strong>, Time: 04.00 – 05.00pm<br />
Venue: Army Hospital, New Delhi<br />
Topics<br />
1. Pregnancy with acute pulmonary edema 3. Embryo reduction<br />
2. Two cases of ipsilateral absence of tube and ovary 4. A case of Intersex state
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
RCOG Green-top Guideline Summarized by RCOG-AICC, North Zone<br />
Management of Monochorionic Twin Pregnancy<br />
Compiled by Dr Neema Sharma MD, MRCOG and Dr Nirmala Agarwal MD, FRCOG<br />
The particular challenges of monochorionic (MC)<br />
pregnancies arise from the vascular placental anastomoses<br />
that are almost universal and connect the umbilical<br />
circulations of both twins: twin–twin transfusion syndrome<br />
(TTTS), the consequences to the co-twin of fetal death and<br />
the management of discordant malformations. In addition,<br />
monochorionic, monoamniotic (MCMA) pregnancies<br />
(1% of twin pregnancies) carry a very high risk of cord<br />
entanglement.<br />
Diagnosis of monochorionic twin pregnancy<br />
All women with a twin pregnancy should be offered an<br />
ultrasound examination at 10–13 weeks of gestation to<br />
assess viability, chorionicity, major congenital malformation<br />
and nuchal translucency. (Grade B recommendation)<br />
If there is uncertainty about the diagnosis of chorionicity,<br />
a photographic record of the ultrasound appearance of the<br />
membrane attachment to the placenta should be retained<br />
in the case notes and a second opinion should be sought. [√]<br />
Chorionicity is better assessed by ultrasound before 14<br />
weeks than after 14 weeks. (Grade C recommendation)<br />
Ultrasound diagnosis was based on demonstration of the<br />
‘lambda’ or ‘twin peak’ sign (dichorionic) (DC)or ‘T-sign’<br />
(monochorionic) at the membrane–placenta interface 1 .<br />
(Evidence level 2+)<br />
The diagnosis of TTTS is based on ultrasound criteria:<br />
• the presence of a single placental mass<br />
• concordant gender<br />
• oligohydramnios with maximum vertical pocket [MVP]<br />
less than 2 cm in one sac and polyhydramnios in other<br />
sac (MVP ≥ 8 cm) (some would say ≥ 8 cm at ≤ 20 weeks<br />
and ≥ 10 cm over 20 weeks)<br />
• discordant bladder appearances – severe TTTS<br />
• haemodynamic and cardiac compromise – severe TTTS<br />
What is the Outcome of MC compared to dichorionic<br />
(DC) twin pregnancies ?<br />
Clinicians and women should be aware that MC twin<br />
pregnancies have higher fetal loss rates than DC twin<br />
pregnancies, mainly due to second trimester loss and,<br />
overall, may have a propensity to excess neurodevelopmental<br />
morbidity. (Grade C recommendation)<br />
A prospective Scandinavian study of 495 pregnancies<br />
diagnosed before 15 weeks found fetal loss at less than 24<br />
weeks of gestation to be 14.2% MC compared with 2.6% DC<br />
(P < 0.05) 2 . (Evidence Level 2+)<br />
Sebire and colleagues have suggested that the main risk<br />
of fetal death in MC pregnancies is before 24 weeks of<br />
gestation and after this time the rate of perinatal loss is<br />
only slightly higher in MC than DC pregnancies (4.9%<br />
versus 2.8%, respectively) 3 .<br />
Ultrasound scanning<br />
Nuchal translucency measurements should be offered<br />
to women with MC pregnancies who wish to have fetal<br />
aneuploidy screening. [√]<br />
All MC twins should have a detailed ultrasound scan which<br />
includes extended views of the fetal heart.<br />
(Grade B recommendation)<br />
A fetal echocardiographic assessment should be considered<br />
in the assessment of severe TTTS.<br />
(Grade D recommendation)<br />
Fetal ultrasound assessment should take place every 2–3<br />
weeks in uncomplicated MC pregnancies from 16 weeks. [√]<br />
After 24 weeks, when first presentation of TTTS is<br />
uncommon, the main purpose is to detect fetal growth<br />
restriction, which may be concordant or discordant.<br />
Grading/staging system for severity of TTTS<br />
Women with monochorionic twin pregnancies should<br />
be asked to report sudden increases in abdominal size or<br />
breathlessness, as this may be a manifestation of TTTS. [√]<br />
How useful are grading systems for severity of TTTS in<br />
establishing prognosis?<br />
The Quintero system of staging TTTS (Table 1) has<br />
some prognostic value but the course of the condition<br />
is unpredictable and may involve improvement or rapid<br />
deterioration.<br />
The Quintero classification system 4<br />
i. There is a discrepancy in amniotic fluid volume with<br />
oligohydramnios of a maximum vertical pocket (MVP)<br />
≤ 2 cm in one sac and polyhydramnios in other sac<br />
(MVP ≥ 8 cm). The bladder of the donor twin is visible<br />
and Doppler studies are normal<br />
ii. The bladder of the donor twin is not visible (during<br />
19
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
20<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
length of examination, usually around 1 hour) but<br />
Doppler studies are not critically abnormal<br />
iii. Doppler studies are critically abnormal in either twin<br />
and are characterised as abnormal or reversed enddiastolic<br />
velocities in the umbilical artery, reverse flow<br />
in the Ductus venosus or pulsatile umbilical venous<br />
flow<br />
iv. Ascites, pericardial or pleural effusion, scalp oedema<br />
or overt hydrops present<br />
v. One or both babies are dead.<br />
What is (are) the Optimal treatment(s) of TTTS and<br />
their outcomes?<br />
Twin–twin transfusion syndrome should be managed<br />
in conjunction with regional fetal medicine centres with<br />
recourse to specialist expertise. [√]<br />
Severe twin–twin transfusion syndrome presenting before<br />
26 weeks of gestation should be treated by laser ablation<br />
rather than by amnioreduction or septostomy.<br />
(Grade A recommendation)<br />
In a Cochrane review, for laser ablation versus<br />
amnioreduction, there were fewer deaths of both babies<br />
(RR 0.33, 95%CI 0.16–0,67), fewer neonatal deaths (RR<br />
0.29, 95% CI 0.14–0.61, adjusted for clustering) and fewer<br />
perinatal deaths (RR 0.59, 95% CI 0.40–0.87, adjusted for<br />
clustering). More babies were alive without neurological<br />
abnormality at 6 months of age after laser ablation (RR<br />
1.66, 95% CI1.17–2.35, adjusted for clustering). Long-term<br />
outcomes are awaited 5 . (Evidence level 1+)<br />
Some women request termination of pregnancy when<br />
severe TTTS is diagnosed and this should be discussed as<br />
an option. (Evidence level 3)<br />
What is the optimal timing and method of delivery for<br />
otherwise uncomplicated MC pregnancies ?<br />
It is appropriate to aim for vaginal birth of monochorionic<br />
twins unless there are accepted, specific clinical indications<br />
for caesarean section, such as twin one lying breech or<br />
previous caesarean section. [√]<br />
Delivery should be planned for 36–37 weeks of gestation,<br />
unless there is an indication to deliver earlier. [√]<br />
For uncomplicated MCDC pregnancies (without TTTS<br />
or fetal growth restriction), there may be a higher risk<br />
of unexplained fetal demise despite intensive fetal<br />
surveillance. The management of multiple pregnancies in<br />
general is controversial, as are the timing of induction and<br />
the proposed mode of delivery.<br />
An RCOG Study Group 6 suggested that, in DC twin<br />
pregnancies, discussion should take place as to the mode<br />
of delivery and intrapartum management at 34–36 weeks.<br />
Delivery should be planned at 37–38 weeks. In MC twin<br />
pregnancies, discussion should take place as to the mode<br />
of delivery and intrapartum management at 32–34 weeks.<br />
Delivery should be planned at 36–37 weeks.<br />
What are the consequences for the surviving twin<br />
after fetal death of the co-twin in a MC twin pregnancy<br />
and what is optimal clinical managment ?<br />
After the single fetal death in a monochorionic pregnancy,<br />
the risk to the surviving twin of death or neurological<br />
abnormality is of the order of 12% and 18%, respectively.<br />
Clinicians should be aware that the risks are much higher<br />
than in dichorionic pregnancies and that management of<br />
such pregnancies is complex. (Grade B recommendation)<br />
Damage to MC twins after the death of a co-twin is now<br />
thought to be caused by acute haemodynamic changes<br />
around the time of death, with the survivor essentially<br />
haemorrhaging part of its circulating volume into the<br />
circulation of the dying twin. This may cause transient or<br />
persistent hypotension and low perfusion,leading to the<br />
risk of ischaemic organ damage, notably but not exclusively,<br />
to the brain.<br />
Clinical management is complex and is best overseen by<br />
fetal medicine experts with the knowledge and experience to<br />
advise about the advantages and disadvantages of different<br />
approaches. Rapid delivery is usually unwise, unless there<br />
are significant cardiotocographic abnormalities or evidence<br />
of anaemia in the survivor, as evidenced by abnormal middle<br />
cerebral artery Doppler waveforms or if fetal death occurs<br />
late in pregnancy. Detailed counselling is essential and<br />
should be recorded in the case records. Serious compromise<br />
in the surviving fetus may be anticipated and this should<br />
be discussed with parents, including the significant risk of<br />
long-term morbidity. Evidence of fetal compromise (such<br />
as abnormal cardiotocography) could represent continuing<br />
damage to the brain and other organs, as well as already<br />
existing damage. A conservative policy is often appropriate,<br />
with brain imaging planned by 4 weeks to establish (if the<br />
baby has survived) whether serious cerebral morbidity<br />
has occurred. The appearances of such manifestations on<br />
ultrasound examination of the fetal central nervous system<br />
are variable and may take up to 4 weeks to occur. Fetal<br />
magnetic resonance imaging provides earlier and more<br />
detailed information about brain lesions in the surviving<br />
fetus than does ultrasound and its use is recommended.<br />
(Evidence level 3)<br />
In such circumstances, termination of pregnancy would<br />
then be an option. The gestational age at the time of<br />
diagnosis will have an important influence on management<br />
options. The views of the parent or parents will be critical.<br />
REFERENCE ________________________________<br />
1. Sepulveda W, Sebire NJ, Hughes K, Odibo A, Nicolaides KH.<br />
The lambda sign at 10–14 weeks of gestation as a predictor of<br />
chorionicity in twin pregnancies. Ultrasound Obstet Gynecol<br />
1996;7:421–3.<br />
2. Sperling L. Detection of chromosomal abnormalities, congenital
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
abnormalities and transfusion syndrome in twins. Ultrasound<br />
Obstet Gynecol 2007;29:517–26.<br />
3. Sebire NJ, Snijders RJ, Hughes K, Sepulveda W, Nicolaides KH.<br />
The hidden mortality of monochorionic twin pregnancies. Br J<br />
Obstet Gynaecol 1997;104:1203–7.<br />
4. Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK,<br />
Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol<br />
1999;19:550–5.<br />
5. Roberts D, Neilson JP, Kilby MD, Gates S. Interventions for the<br />
treatment of twin-twin transfusion syndrome. Cochrane Database<br />
Sys Rev 2008;CD002073.<br />
6. Consensus views arising from the 50th Study Group: Multiple<br />
Pregnancy. In: Kilby M, Baker P, Critchley H, Field D, editors.<br />
Multiple pregnancy. London: RCOG Press; 2006. p. 283–6.<br />
GRADES OF RECOMMENDATIONS ____________<br />
A - At least one meta-analysis, systematic reviews or<br />
randomised controlled trial rated as 1++ and directly<br />
applicable to the target population; or A systematic review<br />
of randomised controlled trials or a body of evidence<br />
consisting principally of studies rated as 1+, directly<br />
applicable to the target population and demonstrating<br />
overall consistency of results<br />
B - A body of evidence including studies rated as 2++ directly<br />
applicable to the target population and demonstrating<br />
overall consistency of results; or Extrapolated evidence<br />
from studies rated as 1++ or 1+<br />
C - A body of evidence including studies rated as 2+ directly<br />
applicable to the target population and demonstrating<br />
overall consistency of results; or Extrapolated evidence<br />
from studies rated as 2++<br />
D - Evidence level 3 or 4; or Extrapolated evidence from<br />
studies rated as 2+<br />
[√] Good practice point - Recommended best practice based<br />
on the clinical experience of the guideline development group<br />
CLASSIFICATION OF EVIDENCE LEVELS _______<br />
1++ High-quality meta-analyses, systematic reviews of<br />
randomised controlled trials or randomised controlled<br />
trials with a very low risk of bias<br />
1+ Well-conducted meta-analyses, systematic reviews of<br />
randomised controlled trials or randomised controlled<br />
trials with a low risk of bias<br />
1- Meta-analyses, systematic reviews of randomised<br />
controlled trials or randomised controlled trials with a high<br />
risk of bias<br />
2++ High-quality systematic reviews of case–control or<br />
cohort studies or high quality case–control or cohort<br />
studies with a very low risk of confounding, bias or chance<br />
and a high probability that the relationship is causal<br />
2+ Well-conducted case–control or cohort studies with<br />
a low risk of confounding, bias or chance and a moderate<br />
probability that the relationship is causal<br />
2- Case–control or cohort studies with a high risk of<br />
confounding, bias or chance and a significant risk that the<br />
relationship is not causal<br />
3 Non-analytical studies; e.g. case reports, case series<br />
4 Expert opinion<br />
SRIVASTAVA MRI & IMAGING CENTRE<br />
(An ISO 9001:2008 CERTIFIED DIAGNOSTIC CENTRE)<br />
• MRI 1.5 TESLA (SIEMENS)<br />
• USG with Obstetrics color Doppler<br />
• LAB collection centre<br />
Disclaimer ‘ The RCOG takes no responsibility for the<br />
accuracy of the summary or any consequences that follows<br />
by following the summary Guidelines’. View full guideline on<br />
www.rcog.org.uk/womens-health/clinical-guideline<br />
*One of the few centres equipped with dedicated breast coil for MRI mammography<br />
with added advantage of:<br />
No radiation<br />
No compressive pain<br />
Can be done for young patients also<br />
Dr Sanjay Srivastava, M.B.B.S, D.M.R.D., D.N.B.<br />
Sr Consultant Radiologist<br />
1,2,3, Purvanchal Plaza, Pocket–B, Market, Mayur Vihar, Phase-2, Delhi 110 091<br />
Tel.: 011-22779009, 9811157069, 9811892896<br />
On Panel: CGHS, ESI, BSES<br />
21
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
22<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
23
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
Website: www.aiccrcognzindia.com<br />
24<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
RCOG-NZ India Advanced Laparoscopy & Hysteroscopy Workshop<br />
Dates: 26th & 27th <strong>July</strong> <strong>2010</strong> Venue: Max Hospital Saket<br />
Organising Chairperson: Dr. U.P. Jha<br />
Organising Secretaries & Contact Persons: Dr. Anjila Aneja, Dr. Meena Naik<br />
Invited National Faculty: Dr. Shailesh Puntambekar, Dr. Praveen Patel<br />
Day 1 Monday, 26th <strong>July</strong>, <strong>2010</strong><br />
Lectures<br />
09:00 - 09:10 am Laparoscopic ergonomy and port placement- Dr. U.P.Jha<br />
09:10 - 09:20 am Avoiding laparoscopic complications- Dr. Anjila Aneja<br />
09:20 - 09:30 am Avoiding complications with electrocautery and energy sources<br />
- Dr. Meena Naik<br />
Video Sessions - Unedited & edited videos<br />
09:30 - 11:30 am Management of Endometriosis<br />
Management of endometriomas, Dissection of obliterated<br />
pouch of Douglas, Excision of rectovaginal septum, Ureteric &<br />
etroperitoneal dissection in endometriosis, Repeat surgery<br />
in endometriosis, Uteroscacral nerve ablation.<br />
Bowel adhesiolysis, Unusual sites of endometriosis<br />
11:45 - 01:00 pm Advanced Hysteroscopy<br />
Myomectomy, Septal resection, Asherman’s syndrome,<br />
Tubal cannulation, Use of Versascope & Versapoint<br />
01:30 - 03:30 pm Laparoscopic Myomectomy<br />
Subserous fibroids, Cervical fibroids, Intramural fibroids,<br />
Large fibroids, Intracorporeal suturing, LAM – Laparoscopic<br />
assisted myomectomy, Vaginal removal of fibroids & vaginal<br />
suturing<br />
03:30 - 04:30 pm Laparoscopy in Infertility<br />
Laparoscopic salpingostomy/fimbrioplasty, Laparoscopic<br />
tubal anastomosis, Restoring tubo - ovarian relationship<br />
Free Videos Session<br />
04:30 - 05:30 pm Competitive video presentations<br />
Day 2 Tuesday, 27th <strong>July</strong>, <strong>2010</strong><br />
Video Sessions (edited & unedited)<br />
08:30 - 10:30 am Laparoscopic management of adnexal masses<br />
Ovarian dermoid cysts, Multicystic ovarian lesions, Large ovarian<br />
masses, Suspicious adnexal masses, Solid ovarian tumours<br />
10:45 - 12:30 pm Laparoscopic hysterectomy TLH, LAVH<br />
Hysterectomy for large uterus, Hysterectomy for severe<br />
endometriosis, NDVH<br />
01:00 - 04:00 pm Laparoscopic Onco Surgery<br />
Laparoscopic surgery for endometrial cancer, Radical<br />
hysterectomy for carcinoma cervix, Laparoscopic pelvic<br />
lymphadenectomy, Laparoscopic para-aortic lymphadenectomy<br />
Laparoscpic omentectomy<br />
04:00 - 05 :00 pm Pelvic floor repair<br />
Vault suspension, Anterior & posterior compartment repair<br />
Repair of nulliparous prolapse<br />
Royal College of Obstetricians &<br />
Gynaecologists North Zone India<br />
(A Registered Society Under the Registrar of Societies)<br />
RCOG Office & Centre for Activities: B-235, CR Park, New Delhi<br />
Forthcoming Activities in <strong>2010</strong> under aegis of <strong>AOGD</strong><br />
RCOG-NZ India Advanced Obstetric Skills Course<br />
Date: 25th <strong>July</strong>, <strong>2010</strong><br />
Venue: RCOG-NZ Office & Centre, B-235, Chitranjan Park, New Delhi<br />
Workshop Convenors: Dr. Urvashi P Jha, Dr. Sanjeev Sharma (UK)<br />
Workshop Coordinators & Contact Persons: Dr. Anjila Aneja, Dr. Jayasree Sundar<br />
Overview: This hands on training course will be of great value to postgraduates<br />
and practicing obstetricians. Expert faculty will give hands-on training on<br />
various techniques.<br />
Course Programme - Training module stations & groups:<br />
• Management of pregnant patient with fits<br />
• Management of massive obstetric hemorrhage<br />
• Shoulder dystocia<br />
• Twins and breech delivery<br />
• Post partum collapse<br />
• CTG and its clinical implications<br />
• Partogram and management of labour<br />
Limited seats only<br />
Registration Fee: Rs. 700/- (For PG students Rs. 500/-)<br />
Free Video Session<br />
04:30 - 05:00 pm Competitive video presentation<br />
Limited seats only<br />
Registration Fee: Rs. 1500/- (For PG students Rs. 700/-)<br />
The Complete RCOG-NZ MRCOG Part 1 Revision Course<br />
Date: 23rd-25th <strong>July</strong>, <strong>2010</strong><br />
Venue: RCOGNZ Centre, CR Park(Basement), New Delhi<br />
Course Organiser & Contact Persons: Dr Neema Sharma, Dr Mamta Mishra<br />
Overview: Three day refresher course in basic sciences relevant to MRCOG, 12<br />
important tips to clear the exam, EMQ & MCQ practice tests<br />
Course Fee: Rs. 5,000/-<br />
The Complete RCOG Franchised MRCOG Part 2 Revision Course<br />
(Written and OSCE) New Delhi, India<br />
Date: 28th-30th <strong>July</strong>, <strong>2010</strong><br />
Course Organiser & Contact Persons: Dr Saritha S. Kale, Dr Jayasree Sundar<br />
Overview: The course reflects the current MRCOG Part 2 examination and<br />
will be conducted by experienced consultants from the Royal College of<br />
Obstetricians and Gynaecologists. The emphasis will be on key topics.<br />
Candidates will have the opportunity to experience ALL the current formats of<br />
testing, namely: MCQ, EMQ, SAQ and OSCE.<br />
Success Rate : 75% in Sept. 2009 exams.<br />
Course Convenors: Dr David Redford (UK) & Dr A. Hollingworth (UK)<br />
Course Organiser: Dr Sanjeev Sharma (UK)<br />
The course will be limited to 20 candidates.<br />
The intensive nature of this course reflects the fact that it is specifically designed<br />
for examination candidates requiring revision only - it is not a teaching course.<br />
There will be 10 OSCE stations.<br />
Programme<br />
Day 1<br />
08:15 am Registration<br />
08:30 am Introduction Mr Sanjeev Sharma<br />
08:45 am Extended Matching Questions-Lecture Mr Sanjeev Sharma<br />
09:00 am EMQ’s Test<br />
09:30 am MCQ’s Lecture Mr Sanjeev Sharma<br />
09:45 am MCQ’s Test<br />
10:30 am Clinical Governance and Mr Sanjeev Sharma<br />
the NHS health system<br />
11:00 am Uro - Gynaecology Dr Sonu Agarwal<br />
11:40 am Foetal Medicine Dr Anita Kaul<br />
12:10 pm SAQ’s Lecture Mr Sanjeev Sharma<br />
12:10 pm SAQ’s 1 & 2 Test Mr Sanjeev Sharma<br />
13:00 pm LUNCH and briefing to local examiners Mr Sanjeev Sharma<br />
13:30 pm OSCE Lecture Mr Sanjeev Sharma<br />
13:30 pm Prioritization Dr Neema, Dr Jayasree<br />
14:30 pm Demonstration OSCE’s<br />
15:30 pm Role Play 1.Good Role, 2.Bad Role<br />
17:00 pm OSCE Discussion General Discussion/Feedback<br />
Home Work- SAQ’S 3,4,5,6<br />
Day 2<br />
08:15 am Feedback-MCQs and EMQs Mr Sanjeev Sharma<br />
09:30 am Risk management in obstetrics Mr Sanjeev Sharma<br />
and gynaecology with sample questions<br />
10:00 am Audit with practice audits Mr Sanjeev Sharma<br />
11:45 am Feedback- SAQs 1-2 Mr Sanjeev Sharma<br />
12:15 pm Screening in the UK-Antenatal and cervical Dr Jayasree/Dr Sarita<br />
12:45 pm MCQ Test<br />
13:15 pm LUNCH and briefing to local examiners<br />
14:00 pm OSCE All Examiners<br />
16:30 pm Discussion & feedback with candidates<br />
Home work SAQ’s 7 & 8<br />
Day 3<br />
08:30 am Feedback–SAQ’s 3,4,5 & 6 Mr Sanjeev Sharma
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bull <strong>AOGD</strong> Bulletin<br />
09:00 am NHS Assisted conception, MDT Mr Sanjeev Sharma<br />
09:45 am MCQ’s Test Mr Sanjeev Sharma<br />
10:30 am Critical Appraisal with practice Dr Sarita Kale<br />
11:30 am Feedback SAQ’s 7 & 8 Mr Sanjeev Sharma<br />
12:00 pm Feedback MCQ & General discussion Mr Sanjeev Sharma<br />
13:00 pm Briefing to local examiners Mr Sanjeev Sharma<br />
13:30 pm OSCE All Examiners<br />
16:00 pm Discussion/Feedback with candidates<br />
Course Fee: Rs. 15,000/-<br />
RCOG-UK Certified & Franchised<br />
Basic Practical Skills Course in Obstetrics & Gynaecology<br />
Organised by North Zone India<br />
Dates: 31th <strong>July</strong> & 1st August, <strong>2010</strong><br />
Venue: Ethicon Institute of Surgical Education, Kirtinagar, New Delhi<br />
Course Conveners: Dr. Urvashi P Jha, Dr Sanjeev Sharma (UK)<br />
Course co-ordinators & Contact Persons: Dr. Jasmine Chawla, Dr. Mamta Dagar<br />
Course Contents: Hands on Franchise Course for Trainees & Practising<br />
Gynaecologists Certified by RCOG London on the following topics with one<br />
to one interaction<br />
Principles of Safe & Effective Surgery Principles of Gynae Examination<br />
Knotting & Suturing Episiotomy repair<br />
Tissue Handling Mx of normal & breech delivery<br />
Handling Instruments Fetal blood sampling<br />
Surgical Documentation Ventouse & forceps delivery<br />
Anatomy of Pelvic Floor Caesarean section<br />
Management of Massive Obstetric Management of shoulder dystocia<br />
Haemorrhage Principles of safe endoscopy<br />
Endoscopic Equipment Principles of haemostasis & dissection<br />
Principles of Electro Surgery Evacuation of uterus<br />
Limited seats only<br />
Course Fee: Rs. 5,000/- (for manual £ 36 additional and optional)<br />
RCOG-NZ India Annual Conference<br />
(All India Co-ordinating Committee-Royal College of Obstetricians & Gynaecologists UK)<br />
Conference Theme:<br />
“Changing Clinical Practice in Changing Times”<br />
Date: Saturday, 4th September, <strong>2010</strong><br />
Time: 08.00 am - 05.00 pm<br />
Venue: Indraprastha Apollo Hospitals, Auditorium, Sarita Vihar, New Delhi 110076<br />
Organizing Chairperson: Dr Urvashi Prasad Jha<br />
Organizing Secretaries: Dr Sohani Verma, Dr. Sarita S. Kale, Dr Anita Kaul<br />
Invited International Faculty<br />
Dr Richard Charles (Rick) Warren (UK), Dr Theresa Freeman Wang (UK)<br />
Others to be announced soon<br />
Planned Topics<br />
One Stop Clinics, Day Care Major Gynae Surgeries, Managing HPV Positive<br />
Women, Interventional Radiology in Obs & Gynae, Ambulatory Obstetrics,<br />
Changing trends in HRT and Menopause, Fertility preservation in Gynaecology,<br />
Changing pattern in Prolapse Management, The 12 Week Fetal Clinic, Minimal<br />
Invasive Perinatal Autopsy, Contraception in Changing Times, Caesarean<br />
Sections-Changing Indications and technique, Predicting Preterm Labour,<br />
Peripartum Mental Health Issues, Challenges of Obesity in Obs & Gynae, The<br />
Latest Trend- Revirgination and Cosmetic Surgery of the Female Genitalia<br />
• Those registering only for the “Ultrasound Workshop” on 5th September,<br />
may send their registration request and cheque in favour of “Delhi<br />
Ultrasound Update” payable at New Delhi to Dr Kuldeep Singh, Secretary-<br />
IFUMB, D-80, East of Kailash, New Delhi 110065<br />
For details and registration form log on to: www.aiccrcognzindia.com<br />
Mailing Address: Dr. Sohani Verma, IVF Unit, 1st Floor, Gate No. 6, Indraprastha<br />
Apollo Hospitals, Sarita Vihar, New Delhi 110 076<br />
Email: sohaniverma@hotmail.com, shamsundersaritha@gmail.com,<br />
anitagkaul@gmail.com, Tel.: 011-29872146/99, M.: 09810116623<br />
Inauguration of<br />
RCOG-NZ Centre, CR Park, New Delhi<br />
on Saturday, 4th September, <strong>2010</strong> at 7pm<br />
by Mr Richard Charles (Rick) Warren<br />
Honorary Secretary, RCOG (London)<br />
All RCOG-NZ Courses & CMEs are being conducted in association with<br />
<strong>AOGD</strong>. Last date of registration 20th <strong>July</strong>, <strong>2010</strong>. PG students must<br />
enclose certificate form HOD. To register for any of the courses, please<br />
download the Registration Form from: www.aiccrcognzindia.com.<br />
Payments to be made by cheque/demand draft (only) in favour of “CME-<br />
NZ-RCOG2007 Plus”. Please post the form & the cheque/demand draft<br />
to Dr. Saritha Shamsunder Kale, Hon Secretary RCOG-NZ India, E-99,<br />
Ansari Nagar (East), AIIMS Campus, New Delhi 110029, India<br />
Contacts<br />
Dr Sarita Shamsunder Kale<br />
shamsundersaritha@gmail.com<br />
M: 09868392748<br />
Dr Sohani Verma<br />
sohaniverma@hotmail.com<br />
M: 09810116623<br />
Dr. Jasmine Chawla<br />
drjasminechawla@gmail.com<br />
M: 09310009321<br />
Dr Mamta Mishra<br />
shreeja11@yahoo.co.in<br />
M: 09868078855<br />
Dr Kuldeep Singh<br />
singhdrkuldeep@rediffmail.com<br />
ifumbdelhichapter@gmail.com<br />
M: 09811196613<br />
Dr Mala Arora<br />
narindermala@gmail.com<br />
M: 09818676801<br />
Dr Anjila Aneja<br />
anjilaaneja@yahoo.co.in<br />
M: 09810059519<br />
Dr Anita Kaul<br />
anitagkaul@gmail.com<br />
M: 09811100511<br />
Dr Payal Singhal<br />
payal_sgh@yahoo.co.in<br />
M: 09312277293<br />
Dr Neema Sharma<br />
nimavijay@yahoo.co.in<br />
M: 09582500310<br />
Dr Meena Naik<br />
m.naik1971@yahoo.com<br />
M: 09818258503<br />
Dr Jayasree Sundar<br />
jayasreesundar@yahoo.co.in<br />
M: 09810297461<br />
Dr Mamta Dagar<br />
mamtadagar2004@yahoo.co.in<br />
M: 09811437782<br />
RCOG-NZ, India Pre-conference Workshop<br />
Annual Hands-On Colposcopy Course<br />
(Under Aegis of INDIAN SOCIETY OF COLPOSCOPY & CERVICAL PATHOLOGY)<br />
Approved by International Federation of Cervical Pathology & Colposcopy (IFCPC)<br />
Date: 2nd & 3rd September, <strong>2010</strong><br />
Venue: Day-1- RCOGNZ Center, CR Park, New Delhi<br />
Day-2- Max Super Specialty Hospital, Saket, New Delhi<br />
Course Convenors: Dr. Urvashi P Jha, Dr. Vijay Zutshi<br />
Course Coordinators: Dr. Sarita Shamsunder Kale, Dr. Meena Naik<br />
Invited International Faculty: Dr Theresa Freeman Wang(London, UK)<br />
Limited seats only<br />
RCOG-NZ India Post Conference Workshops<br />
Post Conference Workshop I-Ultrasound Workshop<br />
In association with International Federation of Ultrasound in Medicine & Biology (Delhi Chapter)<br />
Theme: Woman’s Imaging- Meeting The Needs of the Modern Woman<br />
Date: Sunday, 5th September, <strong>2010</strong><br />
Venue: Indraprastha Apollo Hospitals, Sarita Vihar New Delhi 110076<br />
Organizing Secretaries: Dr Kuldeep Singh, Dr Anita Kaul<br />
Post Conference Workshop II- Life Skills for Doctors<br />
Date: Sunday, 5th September, <strong>2010</strong><br />
Venue: RCOG- NZ Center, B-235, CR Park, New Delhi<br />
Organizing Secretary & Contact Person: Dr Mala Arora<br />
This workshop aims to develop the necessary Life Skills required by Practising<br />
Gynecologists to cope with the demands of their profession. Emphasis will be on:<br />
Self Awareness - Identifying ones strengths and weaknesses, Problem<br />
Solving, Decision Making, Critical Thinking, Creative Thinking, Effective<br />
Communication, Doctor Patient Relationships, Coping with Emotions, Stress<br />
Management<br />
Post Confrence Workshop III- Certified AICC RCOG-NZ<br />
Practical Training Course for OT Staff<br />
(Doctors, Nurses & Technicians)<br />
(Open, Vaginal & Minimal Access Gynae Surgeries)<br />
Essential for effective functioning & maintenance of OT<br />
Dates: 5th September <strong>2010</strong><br />
Venue: Max Hospital, 1 Press Enclave Road, Saket)<br />
Organizing Chairperson: Dr. U. P.Jha<br />
Organizing Secretaries & Contact Persons: Dr. Anjila Aneja, Dr. Jayasree<br />
Sundar, Dr. Payal Singhal, Dr. Meena Naik<br />
25
<strong>AOGD</strong> BulletinA<br />
Bulletin<br />
26<br />
Team Gynae<br />
Dr Sonia Malik<br />
Dr Kavita Katoch<br />
Dr Vinita Sherwal<br />
Dr.Vandana Bhatia<br />
Anaesthesia<br />
Dr Avtar Krishan<br />
Embryology<br />
Dr Ved Prakash<br />
<strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin <strong>AOGD</strong> Bulletin<br />
Facilities<br />
IUI,IVF, ICSI, Oocyte & Embryo, Donation, Surrogacy<br />
Semen Banking Embryo freezing, Fetal Reduction, Interventional Ultrasound<br />
LOCATION-1<br />
Holy Angels Hospital<br />
1st Floor, Community Centre, Basant Lok<br />
Vasant Vihar, New Delhi-110057<br />
Tel.: 65416928, 26153635, 26141229, 26143411<br />
Email:southendr@rediffmail.com<br />
Specialty Clinics:<br />
Infertility<br />
Recurrent pregnancy loss<br />
Andrology<br />
Sexual Medicine<br />
Immunology<br />
LOCATION-2<br />
PARAS Hospital<br />
PARAS Southend Fertility & IVF Centre<br />
C-1Block, Phase 1, Sushant Lok, Sector 43, Gurgaon<br />
Tel.: 01244585555
Name: _______________________________________________________________________________________<br />
Address for Correspondence: ____________________________________________________________________<br />
_______________________________________________________________________________________________<br />
Telephone Numbers:<br />
Residence STD Code ________________________ Tel. No. ________________________________________<br />
Clinical/Hospital STD Code ________________________ Tel. No. ________________________________________<br />
Mobile _________________________________________ Fax. No. ________________________________________<br />
E-mail: _______________________________________________________________________________________<br />
Tittle of free paper / poster (if appricable): ________________________________________________________<br />
Registration Fee<br />
32 nd Annual Conference of <strong>AOGD</strong><br />
30th-31st October, <strong>2010</strong><br />
Auditorium, Maulana Azad Medical College, New Delhi<br />
REGISTRATION FORM<br />
Conference Registration Details<br />
Delegate Members Non- members Postgraduates*<br />
Before 30.09.10 1800/- 2000/- 1500/-<br />
Till 15.10.10 2500/- 3000/- 2000/-<br />
After 15.10.10 (Spot) 3500/- 4000/- 2500/-<br />
Cancellation Charges<br />
Before 30th August, <strong>2010</strong> 25%<br />
After 30th August, <strong>2010</strong> 75%<br />
After 30th September, <strong>2010</strong> No Refund<br />
Spot Registration does not guarantee a Conference Kit<br />
Payment Details<br />
Cheque / DDs payable at Delhi drawn in favour of “<strong>AOGD</strong> Conference <strong>2010</strong>”<br />
Cash Amount __________________ Cheque/ Demand Draft No. __________________ Dt. _____________<br />
Amount __________________________________________ Drawn on bank _______________________________<br />
________________________________________________ Signature ___________________________________<br />
*Post graduates should attach a certificate from HOD.<br />
Send Completed Registraction Form along with cheque to:<br />
Dr. Asmita M. Rathore, Organizing Secretary<br />
<strong>AOGD</strong> Secretariat, Deptt. of Obstetrics & Gynaecology<br />
Room No. 112, Ward 1, Block A, First Floor, New Surgical Blcok<br />
Lok Nayak Hospital (Opp. Delhi Gate), Jawaharlal Nehru Marg, New Delhi 110 002<br />
Tel.: 011-23232400 Ext.: 4545<br />
Abstract Form at the back of this page
<strong>AOGD</strong> Conference - <strong>2010</strong><br />
Abstract Form<br />
Type of Presentation: Oral Poster Competition Paper<br />
Topic of paper / poster: ...................................................................................................................................................................<br />
Theme<br />
Minimizing Maternal Mortality Endometrium and it’s related problems Miscellaneous<br />
Name: …………………………….......................................………………………….......………………..…............……........………<br />
Mailing Address: ……………………………....................................................................................................................................<br />
................................................................………………………….......................................…………...……....................…........…<br />
Telephone (R): ………………............................... (O): ………………............................... (M):………….....……...........................<br />
Fax: .................................................................................. Email: .................................................................................................<br />
Registration Fee Details: DD / Cheque / Receipt No. ....................................................................................................................<br />
Title: ..............................................................................................................................................................................................<br />
Rules for paper submission :<br />
1. Free Papers : Presenting author’s name to be first and underlined. Structured abstract (with a soft copy in a CD) not more than 250 words along with<br />
Abstract Form to reach <strong>AOGD</strong> Secretariat by 30th Sept., <strong>2010</strong>.<br />
2. Competition Paper : Abstract form with full text & CD in 4 copies should reach <strong>AOGD</strong> Secretariat by 15th Sept., <strong>2010</strong>.<br />
The competition paper should not carry the name of institution and co-authors.<br />
Only best 8 papers will be selected for presentation in oral session.<br />
Structured Abstract with title:<br />
Type your abstract of 250 words in this box and e-mail to asmita.rathore@yahoo.com.