entire issue. - The Royal New Zealand College of General ...
entire issue. - The Royal New Zealand College of General ...
entire issue. - The Royal New Zealand College of General ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
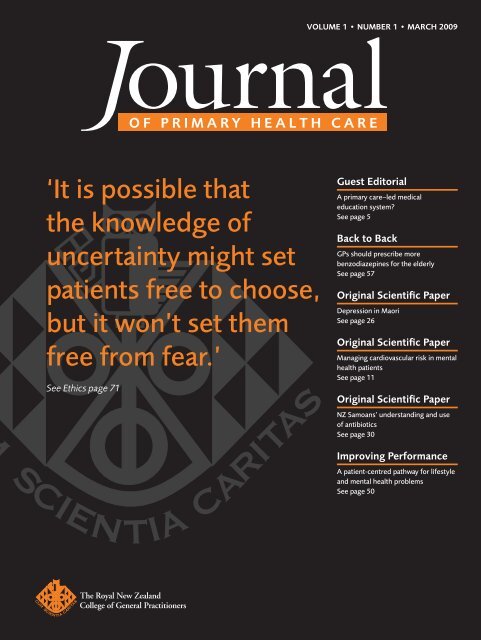
OF PRIMARY HEALTH CARE<br />
‘It is possible that<br />
the knowledge <strong>of</strong><br />
uncertainty might set<br />
patients free to choose,<br />
but it won’t set them<br />
free from fear.’<br />
See Ethics page 71<br />
VOLUME 1 • NUMBER 1 • MaRch 2009<br />
Guest Editorial<br />
A primary care–led medical<br />
education system?<br />
See page 5<br />
Back to Back<br />
GPs should prescribe more<br />
benzodiazepines for the elderly<br />
See page 57<br />
Original Scientific Paper<br />
Depression in Maori<br />
See page 26<br />
Original Scientific Paper<br />
Managing cardiovascular risk in mental<br />
health patients<br />
See page 11<br />
Original Scientific Paper<br />
NZ Samoans’ understanding and use<br />
<strong>of</strong> antibiotics<br />
See page 30<br />
Improving Performance<br />
A patient-centred pathway for lifestyle<br />
and mental health problems<br />
See page 50
OF PRIMARY HEALTH CARE<br />
2 Editorials<br />
From the Editor<br />
2 Simple, fresh, tasty and local<br />
Felicity Goodyear-Smith<br />
Guest Editorials<br />
5 A primary care–led medical education system?<br />
Peter Crampton<br />
6 Using psychoactive medication to intervene in children’s<br />
behaviour: An evidence-based practice?<br />
Barry Parsonson<br />
11 Original scientific Papers<br />
Quantitative Research<br />
11 Cardiovascular risk assessment and management in mental<br />
health clients: Perceptions <strong>of</strong> mental health and general<br />
practitioners in <strong>New</strong> <strong>Zealand</strong><br />
Amanda Wheeler, Jeff Harrison, Zara Homes<br />
20 Prevalence <strong>of</strong> acne and its impact on the quality <strong>of</strong> life in<br />
school-aged adolescents in Malaysia<br />
Arshad Hanisah, Khairani Omar, Shamsul Azhar Shah<br />
26 <strong>The</strong> prevalence <strong>of</strong> depression among Maori patients in<br />
Auckland general practice<br />
Bruce Arroll, Felicity Goodyear-Smith, Ngaire Kerse et al.<br />
Mixed Method Research<br />
30 Understanding and use <strong>of</strong> antibiotics amongst Samoan<br />
people in <strong>New</strong> <strong>Zealand</strong><br />
Pauline Norris, Marianna Churchward, Fuafiva Fa’alau et al.<br />
Systematic Reviews<br />
36 Summary <strong>of</strong> an evidence-based guideline on s<strong>of</strong>t t<strong>issue</strong><br />
shoulder injuries and related disorders—Part 1: Assessment<br />
Gillian Robb, Bruce Arroll, Duncan Reid et al.<br />
42 Summary <strong>of</strong> an evidence-based guideline on s<strong>of</strong>t t<strong>issue</strong><br />
shoulder injuries and related disorders—Part 2: Management<br />
Gillian Robb, Bruce Arroll, Duncan Reid et al.<br />
50 Improving Performance<br />
A patient-centred referral pathway for mild to moderate<br />
lifestyle and mental health problems: Does this model work<br />
in practice?<br />
Jill Calveley, Angela Verhoeven, David Hopcr<strong>of</strong>t<br />
57 Back to Back<br />
GPs should prescribe more benzodiazepines for the elderly<br />
Yes Bruce Arroll; No Ngaire Kerse<br />
61 Continuing Pr<strong>of</strong>essional Development<br />
61 POEMS: Patient Oriented Evidence that Matters<br />
62 String <strong>of</strong> PEaRLS<br />
COnTEnTs<br />
VOLUME 1 • NUMBER 1 • MaRch 2009<br />
issn 1172-6164 (Print)<br />
issn 1172-6156 (Online)<br />
62 cochrane corner: Benzodiazepines may hasten improvement<br />
in major depression for up to six weeks<br />
Bruce Arroll<br />
63 Pounamu: Bridging two worlds in the interview process<br />
—the psychiatric assessment and Maori in primary care<br />
Pamela Ara Bennett<br />
65 charms & harms: St John’s wort (Hypericum perforatum)<br />
Joanne Barnes<br />
66 Resource Summary: Destination: Recovery<br />
Te Unga Ki Uta:Te Oranga; Future responses to mental<br />
distress and loss <strong>of</strong> well-being—discussion paper from the<br />
Mental Health Advocacy Coalition<br />
Helen Rodenburg<br />
67 Practical Pointers: Effective communication strategies to<br />
enhance patient self-care<br />
Fiona Moir, Renske van den Brink, Richard Fox et al.<br />
71 Ethics<br />
Uncertainty, fear and whistling happy tunes<br />
Katherine Wallis<br />
74 Essays<br />
74 Sub-threshold mental health syndromes: Finding an<br />
alternative to the medication <strong>of</strong> unhappiness<br />
Fiona Mathieson, Sunny Collings, Anthony Dowell<br />
77 Mind over matter—implications for general practice<br />
Andrew Corin<br />
80 Letters to the Editor<br />
82 Book Reviews<br />
82 <strong>The</strong> Baby Business: What’s happened to maternity care in <strong>New</strong><br />
<strong>Zealand</strong>—Lynda Exton<br />
Reviewers: William Fergusson and Joan Carll<br />
83 <strong>The</strong> <strong>New</strong> <strong>Zealand</strong> Pregnancy Book: A guide to pregnancy, birth<br />
and a baby’s first three months<br />
3rd ed.—Sue Pullon and Cheryl Benn<br />
Reviewers: Jon Wilcox and Helen Ride<br />
84 Ideological Debates in Family Medicine<br />
—Stephen Buetow and Tim Kenealy<br />
Reviewer: Marjan Kljakovic<br />
85 Integrating mental health into primary care:<br />
A global perspective<br />
86 Gems <strong>of</strong> nZ Primary Health Care Research<br />
88 About the Journal <strong>of</strong> Primary Health Care<br />
VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE 1
EDITORIALs<br />
FROM THE EDiTOR<br />
Felicity Goodyear-<br />
Smith MBChB MGP<br />
FRnZCGP, Editor<br />
CORREsPOnDEnCE TO:<br />
Felicity Goodyear-smith<br />
Department <strong>of</strong> <strong>General</strong><br />
Practice and Primary<br />
Health Care, Faculty<br />
<strong>of</strong> Medical and Health<br />
sciences, <strong>The</strong> University<br />
<strong>of</strong> Auckland, PB 92109,<br />
Auckland, new <strong>Zealand</strong><br />
f.goodyear-smith@<br />
auckland.ac.nz<br />
simple, fresh, tasty and local<br />
campbell Murdoch rightfully mourns the<br />
passing <strong>of</strong> the NZFP. Although he suspects<br />
foul play, hers was not an untimely<br />
death. 1 While we may grieve her loss, we can<br />
also welcome the Journal <strong>of</strong> Primary Health Care<br />
(JPHC), whose time has come. Like Campbell, I<br />
remember nostalgically when, as a GP, I was ‘a<br />
clinician, physician, [minor] surgeon, obstetrician<br />
and paediatrician’. My work day routinely<br />
included family planning, palliative care, ‘VD’<br />
(now called sexual health), numerous cervical<br />
smears and dealing with patients with addictions.<br />
<strong>The</strong>re were also opportunities when my resuscitation<br />
skills were required, and I was frequently up<br />
all night attending patients in their homes when<br />
I was on-call. Except possibly for a few rural colleagues,<br />
those days have passed.<br />
<strong>The</strong> content <strong>of</strong> general practice has fragmented,<br />
with roles played not only by other doctors,<br />
but also by colleagues from other disciplines,<br />
including nursing and pharmacy. <strong>The</strong> Primary<br />
Health Care Strategy was introduced in 2001. 2<br />
Its mission was to shift from traditional general<br />
practice to ‘a new direction for primary health<br />
care with a greater emphasis on population health<br />
and the role <strong>of</strong> the community, health promotion<br />
and preventive care, the need to involve a range<br />
<strong>of</strong> pr<strong>of</strong>essionals’. This is the model under which<br />
now we work. What still requires greater clarity<br />
is the role <strong>of</strong> these different pr<strong>of</strong>essionals, how<br />
they work together and how care is integrated.<br />
Campbell is right—we still need our own doctor.<br />
GPs are pivotal to health care. We know our patients<br />
and their families. <strong>The</strong> relationship is the<br />
key. We need communication and integration—<br />
to be informed if our patients are on the pill,<br />
pregnant, taking complementary and alternative<br />
medicines, receiving methadone maintenance<br />
therapy, in the hospice for respite care.<br />
<strong>The</strong> final <strong>issue</strong> <strong>of</strong> NZFP included editorials from<br />
its distinguished line-up <strong>of</strong> previous editors<br />
with advice and support to me as the incoming<br />
editor <strong>of</strong> the new journal. Rae West can be<br />
reassured that the JPHC remains the academic<br />
publication <strong>of</strong> the RNZCGP, ‘by and for doctors’,<br />
3 although with considerable contribution<br />
from colleagues from numerous other disciplines,<br />
and <strong>of</strong> significant relevance and interest<br />
to their practices.<br />
JPHC aims both to move research into practice<br />
and practice into research. Latest evidence is<br />
provided in a distilled form for rapid and easy<br />
assimilation by busy practitioners. <strong>The</strong>se will<br />
be pithy and succinct, hopefully avoiding one<br />
<strong>of</strong> the challenges articulated by Ian St George,<br />
<strong>of</strong> ‘information smothering’. 4 As well as the<br />
POEMs (‘Patient Oriented Evidence that Matters’)<br />
lauded by Rae, 3 you will find the Cochrane<br />
Corner, a String <strong>of</strong> PEARLS (‘Practical Evidence<br />
About Real Life Situations’), Gems (short précis)<br />
<strong>of</strong> NZ Primary Health Care Research, Charms and<br />
Harms (evidence on the effectiveness and safety<br />
<strong>of</strong> herbal and other complementary remedies),<br />
Pounamu (precious Maori research, essays and<br />
items for practitioners) and brief synopses <strong>of</strong><br />
guidelines and bulletins.<br />
This first <strong>issue</strong> focuses on mental health. Many<br />
<strong>of</strong> the contributions are by GPs. Bruce Arroll and<br />
Ngaire Kerse go Back to Back on giving benzodiazepines<br />
to the elderly. 5 Katherine Wallis, our<br />
guest ethicist, writes elegantly about the possible<br />
effects <strong>of</strong> the knowledge <strong>of</strong> uncertainty. 6 Fiona<br />
Moir, Richard Fox, Renske van den Brink and<br />
Susan Hawken discuss communication strategies<br />
to enhance patient self-care. 7 Helen Rodenberg<br />
presents a discussion paper on responses to mental<br />
distress and loss <strong>of</strong> well-being; Andrew Corin<br />
ponders on mind over matter. 8<br />
This <strong>issue</strong> also contains valuable contributions<br />
from a diverse range <strong>of</strong> other disciplines, including<br />
pharmacy, public health, physiotherapy,<br />
psychology, psychiatry, nursing and midwifery.<br />
2 VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE
Our Pounamu (Maori primary health care<br />
treasure) this month is provided by psychiatrist<br />
Pamela Bennett, who discusses how to bridge<br />
the Maori and Pakeha worlds when assessing and<br />
managing Maori with psychiatric illness. 9<br />
Read the challenge <strong>issue</strong>d by our editorial board<br />
member Peter Crampton, public health physician<br />
and Dean <strong>of</strong> the Wellington School <strong>of</strong> Medicine,<br />
on a primary care–led medical education system, 10<br />
and the thought-provoking article by another<br />
board member, psychologist Barry Parsonson, on<br />
whether giving psychoactive drugs to control children’s<br />
behaviour is evidence-based. 11 Psychologist<br />
Fiona Mathieson and psychiatrist Sunny Collings,<br />
joined by Tony Dowell (GP and editorial board<br />
member), consider ultra-brief interventions as<br />
alternatives to drugs in treating unhappiness. 12<br />
PHO initiative she championed to provide an<br />
intervention pathway for patients with mild and<br />
moderate mental health and lifestyle problems. 15<br />
Sadly, Jill died suddenly and unexpectedly in<br />
December. Her paper was under revision and we<br />
have published her final version as she left it.<br />
Amanda Wheeler et al. explore the challenge <strong>of</strong><br />
assessing and managing cardiovascular risk in<br />
patients with mental health problems and the difficulties<br />
<strong>of</strong> the primary/secondary care interface. 16<br />
A study finds that facial acne has a significant<br />
emotional and social impact on Malaysian high<br />
school students, and is likely to be generalisable<br />
to our NZ adolescents. 17<br />
A study on Samoan perception <strong>of</strong> the purpose <strong>of</strong><br />
antibiotics reveals just how important communi-<br />
<strong>The</strong> content <strong>of</strong> general practice has fragmented, with roles played<br />
not only by other doctors, but also by colleagues from other<br />
disciplines, including nursing and pharmacy… What still requires<br />
greater clarity is the role <strong>of</strong> these different pr<strong>of</strong>essionals, how they<br />
work together and how care is integrated.<br />
Moving practice into research requires collaboration.<br />
Guest editor <strong>of</strong> the final NZFP, Susan<br />
Dovey, expressed concerns ‘about leaving research<br />
to university-based researchers’. 13 Just as today’s<br />
GPs do not practise in isolation, so too they<br />
cannot be expected to conduct research on their<br />
own. Preparing research proposals and ethics<br />
applications and following proscribed protocols<br />
for specific methodologies takes both time and<br />
expertise. JPHC will regularly publish studies<br />
conducted by GPs and other primary health care<br />
practitioners under the mentorship and support<br />
<strong>of</strong> their university colleagues.<br />
<strong>The</strong> original studies in this <strong>issue</strong> are diverse, but<br />
all address practical <strong>issue</strong>s for practitioners on<br />
the ground. Bruce Arroll and colleagues present<br />
results from a large study on the prevalence <strong>of</strong><br />
depression in Maori. 14 Jill Calveley describes the<br />
cation with our patients is, and that it cannot be<br />
assumed that patients share a Western scientific<br />
understanding <strong>of</strong> what antibiotics are or do. 18<br />
Finally, on a very practical level, the systematic<br />
reviews <strong>of</strong> shoulder injury assessment 19 and<br />
management 20 provide summary tips on diagnosis<br />
and treatment.<br />
Campbell Murdoch points out that NZ leads<br />
the world in general practice and primary health<br />
care publications per head <strong>of</strong> population, 1 which<br />
are now accessible to you in our Gems section. A<br />
surprising number <strong>of</strong> NZ books <strong>of</strong> interest and<br />
relevance to family medicine are also published,<br />
which are critiqued by local reviewers.<br />
JPHC provides a forum for discussion and debate.<br />
As well as Back to Back, essays, the guest Ethics<br />
column and editorials, we welcome letters to the<br />
EDITORIALs<br />
FROM THE EDiTOR<br />
VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE 3
EDITORIALs<br />
FROM THE EDiTOR<br />
editor. <strong>The</strong> electronic version <strong>of</strong> JPHC is available<br />
free; we aim to publish ‘in press’ papers online<br />
prior to release <strong>of</strong> the hard copy, and electronic<br />
discussion will come as soon as the IT capacity is<br />
available.<br />
<strong>The</strong> mission for JPHC reflects that <strong>of</strong> NZFP—publish<br />
original relevant research, provide educational<br />
updates, stimulate critical thinking and debate and<br />
reflect on changes in modern general practice. 21<br />
<strong>The</strong> mission for JPhc reflects that <strong>of</strong><br />
NZFP—publish original relevant research,<br />
provide educational updates, stimulate<br />
critical thinking and debate and reflect on<br />
changes in modern general practice<br />
To follow through on Ian St George’s culinary<br />
metaphor, 4 JPHC <strong>of</strong>fers a smörgåsbord <strong>of</strong> wholesome<br />
dishes. Continuing pr<strong>of</strong>essional education is<br />
served as simple, fresh and local morsels. Essays<br />
and editorials <strong>of</strong>fer more meaty fare—tasty but<br />
easily digestible. Original scientific papers have<br />
pride <strong>of</strong> place at every table, presented in a palatable<br />
fashion. Readers either may merely pick at the<br />
abstract and summary box, or devour the studies<br />
in their <strong>entire</strong>ty.<br />
You may choose to graze from time to time or to<br />
sit down for the full meal. Either way, I wish you<br />
bon appétit.<br />
References<br />
1. Murdoch C. What’s in a name? nZ Fam Physician<br />
2008;35(6):12–15.<br />
2. Ministry <strong>of</strong> Health. <strong>The</strong> Primary Health Care strategy. Wellington;<br />
2001 Feb.<br />
3. West R. Regarding my editorship. nZ Fam Physician<br />
2008;35(6):7–8.<br />
4. st George i. A bright future for the journal. nZ Fam Physician<br />
2008;35(6):5–6.<br />
5. Arroll B, Kerse n. Back to Back: GPs should prescribe more<br />
benzodiazepines for the elderly. J Primary Health Care<br />
2009;1(1):57–60.<br />
6. Wallis K. Uncertainty, fear and whistling happy tunes. J<br />
Primary Health Care 2009;1(1):71–73.<br />
7. Moir F, van den Brink R, Fox R, Hawken s. Effective communication<br />
strategies to enhance patient self-care. J Primary Health<br />
Care 2009;1(1):67–70.<br />
8. Corin A. Mind over matter—implications for general practice.<br />
J Primary Health Care 2009;1(1):77–79.<br />
9. Bennett P. Bridging two worlds in the interview process—the<br />
psychiatric assessment and Maori in primary care. J Primary<br />
Health Care 2009;1(1):63–65.<br />
10. Crampton P. A primary care-led medical education system? J<br />
Primary Health Care 2009;1(1):5–6.<br />
11. Parsonson B. Using psychoactive medication to intervene in<br />
children’s behaviour: An evidence-based practice? J Primary<br />
Health Care 2009;1(1):6–10.<br />
12. Mathieson F, Collings s, Dowell A. sub-threshold mental<br />
health syndromes: Finding an alternative to the medication <strong>of</strong><br />
unhappiness. J Primary Health Care 2009;1(1):74–77.<br />
13. Dovey s. Transitions. nZ Fam Physician 2008;35(6).<br />
14. Arroll B, Goodyear-smith F, Kerse n, Hwang M, Crengle s,<br />
Gunn J, et al. <strong>The</strong> prevalence <strong>of</strong> depression among Maori<br />
patients in Auckland general practice. J Primary Health Care<br />
2009;1(1):26–29.<br />
15. Calveley J, Verhoeven A, Hopcr<strong>of</strong>t D. A patient-centred referral<br />
pathway for mild to moderate lifestyle and mental health<br />
problems: does this model work in practice? J Primary Health<br />
Care 2009;1(1):50–56.<br />
16. Wheeler A, Harrison J, Homes Z. Cardiovascular risk assessment<br />
and management in mental health clients: perceptions<br />
<strong>of</strong> mental health and general practitioners in new <strong>Zealand</strong>. J<br />
Primary Health Care 2009;1(1):11–19.<br />
17. Hanisah A, Khairani Os, A. Prevalence <strong>of</strong> acne and its impact<br />
on the quality <strong>of</strong> life in school-aged adolescents in Malaysia. J<br />
Primary Health Care 2009;1(1):20–25.<br />
18. norris P, Churchward M, Fa’alau F, Va’ai C. Understanding and<br />
use <strong>of</strong> antibiotics amongst samoan people in new <strong>Zealand</strong> J<br />
Primary Health Care 2009;1(1):30–35.<br />
19. Robb G, Arroll B, Reid D, Goodyear-smith F. summary <strong>of</strong> an<br />
evidence-based guideline on s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and<br />
related disorders—Part 1: Assessment. J Primary Health Care.<br />
2009;1(1):36–41.<br />
20. Robb G, Arroll B, Reid D, Goodyear-smith F. summary <strong>of</strong> an<br />
evidence-based guideline on s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and<br />
related disorders—Part 2: Management. J Primary Health<br />
Care 2009;1(1):42–49.<br />
21. Townsend T. Editing the nZFP. nZ Fam Physician.<br />
2008;35(6):16–18.<br />
4 VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE
A primary care–led medical<br />
education system?<br />
<strong>The</strong> primary health care sector is an underutilised<br />
resource for medical education.<br />
<strong>The</strong> combined forces <strong>of</strong> ageing demographics,<br />
advances in community-based medical<br />
treatments for chronic diseases, a commitment<br />
to reducing health inequalities, and cost pressures<br />
increasingly conspire to push health care<br />
into primary care settings. Medical education<br />
must mirror this trend—if for no other reason<br />
than the practical imperative that medical<br />
education needs to occur where the bulk <strong>of</strong><br />
treatment occurs. <strong>The</strong> numbers are compelling:<br />
four out <strong>of</strong> five children and adults visit their<br />
GP at least once in a 12-month period, and with<br />
a mean number <strong>of</strong> visits being 3.2 this accounts<br />
for millions <strong>of</strong> individual contacts. 1 About one<br />
quarter <strong>of</strong> children and adults use a public<br />
hospital service in a 12-month period (counting<br />
emergency department use, outpatient, day case<br />
and inpatient episodes). 1 Our medical graduates<br />
must be prepared to meet the treatment patterns<br />
reflected in these numbers.<br />
<strong>The</strong> shift <strong>of</strong> medical education into community<br />
settings is happening in many countries, and is<br />
readily evident in <strong>New</strong> <strong>Zealand</strong> with the setting<br />
up <strong>of</strong> rural programmes at both our medical<br />
schools, the increasing use <strong>of</strong> general practice in<br />
undergraduate medical education, and government<br />
funding support for increased numbers <strong>of</strong><br />
vocational training places for general practice.<br />
But the barriers to increasing primary care–based<br />
medical education are numerous. Not least is the<br />
lack <strong>of</strong> a long-established tradition <strong>of</strong> widespread,<br />
routine, undergraduate medical education in<br />
primary care, resulting in weak or absent basic<br />
physical infrastructure for teaching, the absence<br />
<strong>of</strong> a well-established pattern <strong>of</strong> GP registrars<br />
teaching undergraduate medical students as occurs<br />
in hospitals, and poor career structure for primary<br />
care–based teachers. Added to this is the relatively<br />
low level <strong>of</strong> government support for specialist GP<br />
vocational training compared with other specialist<br />
training programmes, notwithstanding the strong<br />
policy emphasis this decade on <strong>New</strong> <strong>Zealand</strong>’s<br />
‘primary care–led health system’. <strong>The</strong>n there is<br />
the sticky problem <strong>of</strong> ownership; we need to find<br />
mechanisms for government to invest in basic infrastructure<br />
for primary care–based education in<br />
a way that secures and protects public investment<br />
and simultaneously meets the needs <strong>of</strong> trainers.<br />
A head <strong>of</strong> steam is rapidly building to see these<br />
problems addressed, fuelled by recognition not<br />
only <strong>of</strong> the above <strong>issue</strong>s, but also that the current<br />
training system is not especially orientated towards<br />
equipping graduates for a career in primary<br />
care. This point is well made in a recent report <strong>of</strong><br />
the Workforce Taskforce: 2<br />
<strong>The</strong> traditional model <strong>of</strong> training doctors and<br />
nurses focuses on preparing them to work in hospital<br />
environments. This model does not meet the<br />
demands <strong>of</strong> an aging population, the rise in chronic<br />
disease and co-morbidities, and the emphasis on<br />
treatment in the community.<br />
Primary health care requires a workforce with skills<br />
and competencies to implement primary and population<br />
health services in the community. Practitioners<br />
need to be flexible, contextually responsive, innovative<br />
and engaged in a process <strong>of</strong> life-long learning.<br />
A new and exciting development is the recent<br />
establishment <strong>of</strong> a project by the Universities<br />
<strong>of</strong> Auckland and Otago and the RNZCGP.<br />
<strong>The</strong>y have jointly funded the establishment <strong>of</strong><br />
a National <strong>General</strong> Practice Clinical Placement<br />
Coordination position. <strong>The</strong> first-year objectives <strong>of</strong><br />
this project are to:<br />
• coordinate student and registrar placements<br />
in general practice settings;<br />
EDITORIALs<br />
GUEsT EDiTORiAL<br />
Peter Crampton<br />
MBChB, PhD, FAFPHM,<br />
MRnZCGP, Dean and<br />
Head <strong>of</strong> Campus,<br />
University <strong>of</strong> Otago<br />
Wellington<br />
CORREsPOnDEnCE TO:<br />
Peter Crampton<br />
school <strong>of</strong> Medicine<br />
and Health science,<br />
University <strong>of</strong> Otago,<br />
Wellington, PO Box 7343,<br />
Wellington, new <strong>Zealand</strong><br />
peter.crampton@<br />
otago.ac.nz<br />
VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE 5
EDITORIALs<br />
GUEsT EDiTORiAL<br />
Barry S Parsonson<br />
MA(Hons),<br />
PGDipClinPsych, PhD,<br />
FnZPss,<br />
Registered Psychologist,<br />
special Education Group,<br />
Ministry <strong>of</strong> Education,<br />
new <strong>Zealand</strong><br />
CORREsPOnDEnCE TO:<br />
Barry Parsonson<br />
PO Box 829, napier,<br />
new <strong>Zealand</strong><br />
drp@appliedpsych.co.nz<br />
• establish a common database <strong>of</strong><br />
teaching practices;<br />
• develop and implement a joint communications<br />
plan to promote GP teaching;<br />
• initiate liaison with DHBs to link with<br />
second-year house surgeon placements; and<br />
• provide project management support<br />
for combined University and<br />
<strong>College</strong> policy development.<br />
This project is a coordinated attempt to plan and<br />
build basic infrastructure for primary care-based<br />
medical education in the hope <strong>of</strong> meeting the<br />
medical needs <strong>of</strong> <strong>New</strong> <strong>Zealand</strong>’s population in 20<br />
and 30 years’ time. It will require the support <strong>of</strong><br />
the Ministry <strong>of</strong> Health and the Tertiary Education<br />
Commission to promote and fund some <strong>of</strong><br />
the vital elements such as quality standards for<br />
teaching practices and student consulting rooms.<br />
I am hopeful that the Journal will keep abreast <strong>of</strong><br />
medical education <strong>issue</strong>s and play an important<br />
role in disseminating research papers related to<br />
primary care–based teaching and learning. While<br />
this editorial has focused on medical education,<br />
needless to say similar attention must be paid<br />
to the future <strong>of</strong> primary care–based nursing<br />
education. In the meantime, the challenge for the<br />
sector is to translate the vision <strong>of</strong> a primary care–<br />
led health system into a primary care–led medical<br />
education system. <strong>The</strong>re is much work to be done.<br />
Using psychoactive medication to<br />
intervene in children’s behaviour:<br />
An evidence-based practice?<br />
Introduction<br />
This paper arose out <strong>of</strong> concern that many child<br />
clients with behaviour <strong>issue</strong>s also are clients <strong>of</strong><br />
paediatric and child and adolescent health services<br />
which prescribe medication as a means <strong>of</strong> behaviour<br />
management. In addition, concerns arose over<br />
the increasing moves to ‘pathologise’ children’s<br />
behaviour. For example, in an editorial preceding<br />
a series <strong>of</strong> research articles on ‘preschool<br />
pathology’, Angold and Egger 1 state ‘We can now<br />
confidently assert that we have the wherewithal<br />
to assess the psychiatric status <strong>of</strong> children down<br />
to age two [years]’. While admitting perfection<br />
was not yet attained, they added that, as a<br />
consequence, there was no reason to exclude such<br />
young children from studies <strong>of</strong> specific psychiatric<br />
disorders. <strong>The</strong>y describe studies <strong>of</strong> parental,<br />
teacher and self assessments <strong>of</strong> preschoolers<br />
which predict subsequent behavioural and emotional<br />
disorders at school age without questioning<br />
References<br />
1. Ministry <strong>of</strong> Health. A Portrait <strong>of</strong> Health, Key Results <strong>of</strong> the<br />
2006/07 new <strong>Zealand</strong> Health survey. Wellington: Ministry <strong>of</strong><br />
Health; 2008.<br />
2. Workforce Taskforce. Working Together for Better Primary<br />
Health Care, Overcoming barriers to workforce change and innovation,<br />
Report to the Minister <strong>of</strong> Health from the Workforce<br />
Taskforce. Wellington Workforce Taskforce; 2008.<br />
the validity or reliability <strong>of</strong> such instruments.<br />
Even more troubling is their opinion that if these<br />
emergent disorders are not treated by age two to<br />
three years, it may be too late to produce effective<br />
change via primary prevention interventions.<br />
Sterba, Egger, and Angold 2 claim that the rates <strong>of</strong><br />
DSM-IV disorders 3 in preschoolers are similar to<br />
those for children and adolescents and that DSM-<br />
IV diagnoses are relevant for children in the<br />
two- to five-year-old range, even though the DSM<br />
manual itself does not make such provision.<br />
Angold and Egger do not comment on what they<br />
consider to be ‘primary prevention’ for preschoolers,<br />
nor do they consider the possibility that<br />
predictions made in toddlerhood that then are<br />
confirmed in childhood may well be a result<br />
<strong>of</strong> constant environmental factors (e.g. parenting,<br />
parental depression or poverty), rather than<br />
products <strong>of</strong> a child’s ‘psychopathology’. 1 One<br />
6 VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE
further obvious consequence <strong>of</strong> the focus on<br />
early childhood psychopathology is the introduction<br />
<strong>of</strong> psychotropic medications as interventions.<br />
Recent publicity concerning the prescription <strong>of</strong><br />
antidepressants to two-year-olds in <strong>New</strong> <strong>Zealand</strong><br />
is one exemplar. <strong>The</strong> reported 40-fold increases in<br />
bipolar diagnosis and medication <strong>of</strong> children and<br />
adolescents in the USA between 1994 and 2003<br />
represents another. 4 Both reports raise concerns.<br />
Parents and teachers <strong>of</strong> children with problem<br />
behaviours appear to demand medication as a<br />
‘quick fix’. Parents and school personnel praising<br />
the effects <strong>of</strong> medication who were quoted in<br />
some reports were found to focus primarily on<br />
reductions in these behaviours. Only a few <strong>of</strong> the<br />
parents cited were troubled by associated weight<br />
gains and dyskinesia. Those promoting early diagnosis<br />
and medication are expressing no concerns<br />
about any long-term neuro-developmental risks or<br />
potential learning deficits resulting from medication<br />
during early childhood or administration on<br />
a long-term basis, which suggests that these are<br />
not yet important considerations in their view.<br />
This is not to say that concerns about the pathologisation<br />
<strong>of</strong> childhood are not being expressed<br />
from within psychiatry, as recent articles 5 and<br />
books 6 attest. <strong>The</strong> question remains as to whether<br />
these critics are being heard over the evident blare<br />
<strong>of</strong> publicity from protagonists <strong>of</strong> early identification<br />
and treatment, including the reported<br />
pressures from the pharmaceutical industry for<br />
psychiatrists, paediatricians and parents to identify<br />
and treat ‘disorders’ in early childhood with<br />
medications that rarely have been researched in<br />
terms <strong>of</strong> their impacts on children’s development.<br />
One problem for those working with children in<br />
the school environment is a lack <strong>of</strong> knowledge<br />
by teachers, Resource Teachers Learning and<br />
Behaviour (RTLB) and educational psychologists<br />
about medications prescribed for children. <strong>The</strong>re<br />
is evidence that, despite 25% <strong>of</strong> children referred<br />
to them being medicated, many psychologists<br />
working in schools in the USA lacked adequate<br />
knowledge <strong>of</strong> psycho-pharmaceutical agents. 7<br />
Parents and teachers <strong>of</strong>ten report expectations<br />
that the medication will effect positive changes<br />
in behaviour, but <strong>of</strong>ten seem completely uninformed<br />
about the efficacy, suitability or potentially<br />
harmful side effects <strong>of</strong> the adult psycho-<br />
pharmaceutical agents typically prescribed for<br />
these children. <strong>The</strong>re is also evidence <strong>of</strong> a lack<br />
<strong>of</strong> consultation between those providing psychosocial<br />
interventions within schools and those prescribing<br />
medication to the same children, despite<br />
widespread advice that pharmaceutical interventions<br />
should be accompanied by psychosocial<br />
ones. 8-10 In many instances any evidence-based rationale<br />
for prescribing some <strong>of</strong> these medications,<br />
especially to children and adolescents (e.g. 11, 12 ),<br />
is reliant on small sample studies, <strong>of</strong>ten comprising<br />
diverse groups and only a few <strong>of</strong> which use<br />
double-blind case controlled designs. In an age<br />
in which evidence-based practice and informed<br />
consent are deemed to be requirements <strong>of</strong> good<br />
practice, the data need to be examined.<br />
Attention Deficit Hyperactivity<br />
Disorder (ADHD)<br />
<strong>The</strong> most widely used and, probably, the best<br />
researched medication for child behaviour<br />
management is Ritalin (methylphenidate) which<br />
is widely prescribed for ADHD. 8 Some children<br />
do appear to respond well to Ritalin, although<br />
not all diagnosed with ADHD do so and caution<br />
is advised in assessing and regularly reviewing<br />
medication. 8,12 <strong>The</strong>re are clearly some common<br />
CNS and physical side effects which are likely<br />
to impact on school performance, including<br />
headache, drowsiness, dizziness and dyskinesia. 12<br />
<strong>The</strong>re are concerns about the long-term effects <strong>of</strong><br />
Ritalin on children, including stunted growth,<br />
hypertension and increased risk <strong>of</strong> stroke, as<br />
well as questions about the actual benefits <strong>of</strong> its<br />
long-term use in managing hyperactivity. Some<br />
<strong>of</strong> the major <strong>issue</strong>s <strong>of</strong> conflict around ADHD,<br />
apart from concerns about the use <strong>of</strong> medication,<br />
are those <strong>of</strong> whether or not it is a ‘disorder’, how<br />
valid the DSM-IV 3 criteria are, 13,14 and to what<br />
extent the ‘disorder’ model <strong>of</strong> ADHD is driven<br />
by the pharmaceutical industry itself. 14,15<br />
In their major review <strong>of</strong> the literature, Fonagy et<br />
al. 9 conclude that stimulant medication is most<br />
effective. For the 25% <strong>of</strong> children diagnosed as<br />
ADHD and not responding well to stimulants<br />
they suggest that antidepressants may represent<br />
an option, although there are cautions relating to<br />
their use with children. While acknowledging<br />
benefits <strong>of</strong> combining medication with psychoso-<br />
EDITORIALs<br />
GUEsT EDiTORiAL<br />
VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE 7
EDITORIALs<br />
GUEsT EDiTORiAL<br />
cial interventions, their review suggests that few<br />
<strong>of</strong> the latter, on their own, have as much impact as<br />
medication on core symptoms, such as inattention<br />
and hyperkinesis. <strong>The</strong>re is evidence that behaviour<br />
modification is <strong>of</strong> some assistance with reducing<br />
<strong>of</strong>f-task and disruptive behaviours and then can<br />
lead to reductions in medication. CBT enhanced effective<br />
coping and choice making and multi-modal<br />
interventions were still being evaluated at the time<br />
(i.e. 2000). Systemic and psychodynamic interventions<br />
lacked empirical data for or against their use.<br />
Concerns about the high degree <strong>of</strong> co-morbity<br />
between ADHD and conduct and mood disorders<br />
and specific learning deficits, and the reliability<br />
and validity <strong>of</strong> ADHD diagnosis 14 may be supported<br />
by the large variations between studies in<br />
terms <strong>of</strong> the efficacy <strong>of</strong> various medications and<br />
psychosocial interventions. Questions also have<br />
been raised about the validity <strong>of</strong> the neuro-imaging<br />
studies used to support claims that ADHD<br />
has a neurological basis. 16 It seems the jury is still<br />
out on just what ADHD is and whether or not it<br />
is a ‘disorder’.<br />
Anxiety<br />
Wolpert et al. concluded that the front line interventions<br />
for anxiety disorders in children were the<br />
behavioural therapies, including Cognitive Behaviour<br />
<strong>The</strong>rapy (CBT). 10 <strong>The</strong>y suggested that only if<br />
these failed to produce effects should the addition<br />
<strong>of</strong> anti-depressant medication be considered as an<br />
option. It was noted that medication alone was less<br />
effective than medication in combination with<br />
behavioural interventions. A meta-analysis <strong>of</strong><br />
CBT interventions with children and adolescents<br />
diagnosed with anxiety disorders concluded that<br />
both individual and group CBT interventions were<br />
more effective than placebo; that brief interventions<br />
were as effective as longer ones; and that<br />
CBT showed that beneficial treatment effects were<br />
maintained in long-term follow-up.<br />
Autism spectrum Disorders (AsD)<br />
Medications ranging from atypical antipsychotics<br />
and SSRIs are <strong>of</strong>ten prescribed for ASD symptoms<br />
such as ‘Obsessive Compulsive Disorder<br />
(OCD)’, ‘depression’, ‘aggression’ and ‘withdrawal’<br />
in children and adolescents diagnosed<br />
with ASD. A review <strong>of</strong> almost 1700 medication<br />
studies by Broadstock et al., which included<br />
adolescents but not children, found only five that<br />
met criteria for randomised placebo-controlled<br />
investigations. 11 <strong>The</strong> medications included risperidone<br />
(2), naltrexone (1), fluvoxamine (1), and<br />
clomipramine and haloperidol (1). Most trials<br />
were comprised <strong>of</strong> small numbers <strong>of</strong> participants,<br />
included older children and adults and were<br />
short-term (e.g. six weeks), which raised questions<br />
about the generality <strong>of</strong> the findings, especially<br />
in respect <strong>of</strong> long-term drug administration. <strong>The</strong><br />
authors concluded that while some <strong>of</strong> the medications<br />
showed some benefit for some participants,<br />
no conclusions could be reached about relative<br />
efficacy other than that haloperidol might have<br />
some advantage over clomipramine and that naltrexone<br />
was found to be ineffective. Further, no<br />
differentiation between efficacy for pre-pubertal<br />
vs post-pubertal individuals was possible and<br />
no useful information relating to treatment <strong>of</strong><br />
co-morbid disorders was able to be identified.<br />
Fonagy et al. concluded from their extensive<br />
review that, while some medications produced<br />
some symptom reduction, there was little justification<br />
for medication <strong>of</strong> children with ASD<br />
except where there was co-morbid ADHD, when<br />
stimulant medication might <strong>of</strong>fer some benefit. 9<br />
<strong>The</strong>y recommended behavioural intervention as<br />
the first order intervention, with medication being<br />
trialled if the former proved ineffective.<br />
Questions need to be asked about the validity<br />
<strong>of</strong> applying separate DSM-IV diagnostic labels<br />
to behaviours typical <strong>of</strong> ASD and treating them<br />
specifically. For example, when narrow, specific<br />
interests are relabelled as OCD and then medicated<br />
as such it may be inappropriate, given that the<br />
mechanisms and functions <strong>of</strong> such behaviours in<br />
autism are possibly very different from those in<br />
OCD. In addition, while there are relatively few<br />
adequate studies <strong>of</strong> the efficacy <strong>of</strong> medications,<br />
there are many hundreds which demonstrate<br />
the efficacy <strong>of</strong> psychosocial interventions for a<br />
wide range <strong>of</strong> ASD behaviours, such as Applied<br />
Behaviour Analysis (cf. Maurice et al. 17 ).<br />
In summary, Fonagy et al. 9 concluded that there<br />
were no adequate studies <strong>of</strong> children with Asperger’s<br />
Syndrome and that for ASD in general,<br />
behavioural programmes should be tried first,<br />
8 VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE
with ADHD being managed by medication and<br />
that ‘there is no evidence to support the routine<br />
use <strong>of</strong> other medications’.<br />
Attachment disorders<br />
Diagnosis <strong>of</strong> children as having these seems to be<br />
fashionable at present. Reviews <strong>of</strong> assessment <strong>of</strong><br />
attachment ‘disorders’ 18 and <strong>of</strong> attachment theory,<br />
research and treatment 19 point to concerns over<br />
assessment, diagnosis and treatment strategies. For<br />
example O’Connor and Byrne noted that clinicians<br />
rarely use attachment measures in the process<br />
<strong>of</strong> diagnosis and <strong>of</strong>ten have limited knowledge<br />
<strong>of</strong> attachment theory or training in its application.<br />
Equally, they note, attachment measures are not<br />
designed to be diagnostic <strong>of</strong> attachment disorder,<br />
which has no established assessment protocol.<br />
Slater comments that so-called ‘attachment disorder’,<br />
as set out in diagnostic manuals is more about<br />
child maltreatment than attachment. She states<br />
that the research underpinning diagnosis owes<br />
little, if anything, to attachment theory as promulgated<br />
by Bowlby and Ainsworth and is more<br />
grounded in research concerned with the social<br />
behaviour <strong>of</strong> maltreated children. Similarly, Slater<br />
notes, interventions focus on introducing a consistent<br />
and available caregiver or improving the<br />
relationship with the current caregiver without<br />
directly addressing the child’s own attachment<br />
<strong>issue</strong>s or models. She concludes that the current<br />
definitions <strong>of</strong> reactive attachment disorder are<br />
not helpful in meeting children’s needs because<br />
they owe so little to developmental research in<br />
attachment and that, regardless, it seems inappropriate<br />
to pathologise children for having had such<br />
a disruptive start to life. One has to wonder if the<br />
‘pathology’ in attachment disorders does not relate<br />
more to the inadequacies <strong>of</strong> the children’s caregivers<br />
than to the children who are so labelled!<br />
<strong>The</strong> American Academy <strong>of</strong> Child and Adolescent<br />
Psychiatry (AACAP) has recently published a<br />
practice parameter relating to assessment and<br />
treatment <strong>of</strong> children and adolescents with Reactive<br />
Attachment Disorder that raises concerns<br />
about the potential harm to young children’s<br />
developing brains from psychopharmacological<br />
medication, the need to try medication-free<br />
interventions first and the risks that any interventions<br />
pose if they have not been derived from<br />
appropriate studies. 20 This is one ray <strong>of</strong> light<br />
in a field in which many medical practitioners,<br />
including paediatricians and child psychiatrists,<br />
seem comfortable with prescribing psychoactive<br />
medications for young children without trying,<br />
or necessarily being aware <strong>of</strong>, any other modes <strong>of</strong><br />
intervention, such as behavioural therapies.<br />
Mood disorders<br />
Medication <strong>of</strong> childhood ‘mood disorders’ (depression<br />
and bipolar disorders) has, as noted earlier,<br />
become increasingly popular in recent times.<br />
Healy and Le Noury 5 are highly critical <strong>of</strong> the<br />
emergence <strong>of</strong> paediatric bipolar disorder as a condition.<br />
<strong>The</strong>y argue that the ‘disorder’ is primarily<br />
a creation <strong>of</strong> the pharmaceutical industry and are<br />
critical <strong>of</strong> the apparent lack <strong>of</strong> academic scepticism<br />
accompanying the promotion <strong>of</strong> the ‘disorder’ and<br />
the capture <strong>of</strong> psychiatrists by that industry. <strong>The</strong>y<br />
are concerned at the consequences for children <strong>of</strong><br />
exposure to ‘cocktails <strong>of</strong> potent drugs without any<br />
evidence <strong>of</strong> benefit’. 5 <strong>The</strong> drugs listed in the article<br />
include Depakote, olanzapine, risperidone, and<br />
quetiapine and it is reported that some children<br />
receive more than one <strong>of</strong> these medications.<br />
Prevalence <strong>of</strong> depression in children aged between<br />
nine and 16 years is reported as estimated to<br />
be about 9.5%. In the UK, the NICE guidelines<br />
relating to childhood depression advise that the<br />
treatment <strong>of</strong> choice for the first three months<br />
should be psychological (CBT, Family <strong>The</strong>rapy or<br />
Interpersonal <strong>The</strong>rapy). 10 Only if this intervention<br />
does not produce symptomatic improvement<br />
by six weeks is anti-depressant medication recommended<br />
for adolescents only, and then only in<br />
conjunction with either CBT or Family <strong>The</strong>rapy.<br />
Medication is not recommended for younger children.<br />
In other words, the first line <strong>of</strong> treatment<br />
is psychological and the second, for adolescents<br />
only, is the addition <strong>of</strong> medication, preferably<br />
fluoxitine. 10 Perera et al. found that in their South<br />
London CAMHS setting, 28% <strong>of</strong> 25 children and<br />
adolescents being treated for depression were medicated<br />
without any psychological therapy and 72%<br />
were receiving both, with most being prescribed<br />
fluoxitine, despite known enhanced risk <strong>of</strong> suicide<br />
in adolescents taking this medication. <strong>The</strong>y provided<br />
no data on whether psychological interventions<br />
were tried alone at first, on the severity <strong>of</strong><br />
EDITORIALs<br />
GUEsT EDiTORiAL<br />
VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE 9
EDITORIALs<br />
GUEsT EDiTORiAL<br />
depression or age range <strong>of</strong> the participants, except<br />
that seven (28%) were under age 15 years.<br />
Conclusions<br />
This overview makes no pretence <strong>of</strong> being<br />
comprehensive, but even a brief review <strong>of</strong> the<br />
literature raises questions about the direction that<br />
psychiatric diagnosis and treatment <strong>of</strong> children<br />
is taking, along with concerns about the increasing<br />
tendency to pathologise and medicate what<br />
are represented as ‘disorders’ <strong>of</strong> childhood. It<br />
appears that little cognizance has been taken <strong>of</strong><br />
the changes in society that could lead to what are<br />
essentially adaptive and functional human behaviours<br />
in evolutionary terms being increasingly<br />
deemed pathological as we change living styles.<br />
In earlier times children were given the freedom<br />
or opportunity to help adults in a range <strong>of</strong> activities<br />
and/or to play and roam outdoors. Nowadays,<br />
they are more likely to be required to stay within<br />
the bounds <strong>of</strong> small sections or to be indoors<br />
where play involves a video game console or computer<br />
games. <strong>The</strong>y also are typically transported<br />
to and from school each weekday, where they<br />
spend still more time in an environment in which<br />
they <strong>of</strong>ten are expected to sit relatively still,<br />
to concentrate, and generally to be fairly quiet.<br />
Expectations <strong>of</strong> children that they will moderate<br />
their behaviour and not disturb adults in such<br />
environments may fuel demands for medication<br />
to achieve the tolerable states <strong>of</strong> child behaviour<br />
which parents and teachers appear to be failing to<br />
obtain without it.<br />
<strong>The</strong> irony <strong>of</strong> providing children with prescription<br />
medications to manage their behaviours and<br />
moods while simultaneously warning them <strong>of</strong><br />
the dangers <strong>of</strong> so-called recreational drugs seems<br />
to be lost on our society. Societal changes over<br />
time are, in part, the focus <strong>of</strong> the anthropological<br />
study <strong>of</strong> ADHD by Neufeld and Foy 15 which is<br />
instructive and suggests similar cautions should<br />
apply to other so-called disorders <strong>of</strong> childhood<br />
that now are increasingly being identified earlier<br />
and treated with psychotrophic medications. We<br />
ignore the contextual circumstances and functional<br />
purposes <strong>of</strong> ‘problem’ behaviour at our<br />
peril. We medicate children without yet being<br />
aware <strong>of</strong> the possible long-term risks and costs,<br />
both for them and us, even if life is more peace-<br />
ful when they are medicated. <strong>The</strong> concerns and<br />
cautions expressed by the AACAP 20 in respect <strong>of</strong><br />
treatment <strong>of</strong> Attachment Disorder should more<br />
generally be voiced as applicable to the whole<br />
spectrum <strong>of</strong> childhood ‘disorders’ <strong>of</strong> behaviour,<br />
given that the underlying developmental risks are<br />
the same.<br />
References<br />
1. Angold A, Egger HL. Preschool psychopathology: lessons for<br />
the lifespan. J Child Psychol Psychiatry Oct 2007;48(10):961–<br />
966.<br />
2. sterba s, Egger HL, Angold A. Diagnostic specificity and nonspecificity<br />
in the dimensions <strong>of</strong> preschool psychopathology. J<br />
Child Psychol Psychiatry Oct 2007;48(10):1005–1013.<br />
3. American Psychiatric Association, ed. Diagnostic and statistical<br />
Manual iV. 4th ed. Washington DC; 2004.<br />
4. Cary B. Bipolar illness soars as a diagnosis for the young. new<br />
York Times. september 4, 2007.<br />
5. Healy D, Le noury J. Pediatric bipolar disorder: An object <strong>of</strong><br />
study in the creation <strong>of</strong> an illness (Cited in sharav, V. H., 2007).<br />
int J Risk safety Med 2007;19:209–221.<br />
6. Timimi s, ed. Pathological child psychiatry and the medicalization<br />
<strong>of</strong> childhood. Hove, UK: Brunner-Routledge; 2002.<br />
7. Carlson Js, Demaray MK, Hunter-Oehmk s. A survey <strong>of</strong> school<br />
psychologists’ knowledge and training in child psychopharmacology.<br />
Psych sch 2006;43(5):623–633.<br />
8. Abrams L, Flood J, Phelps L. Psychopharmacology in schools.<br />
Psych sch 2006;43(4):493–501.<br />
9. Fonagy P, Target M, Cottrell D, Phillips J, Kurtz Z. A review <strong>of</strong><br />
the outcomes <strong>of</strong> all treatments <strong>of</strong> psychiatric disorder in childhood:<br />
MCH 17-33. Final Report to the national Health service<br />
Executive. London: national Health service; July 2000.<br />
10. Wolpert M, Fuggle P, Cottrell D, Fonagy P, eds. Drawing on<br />
Evidence: Advice for mental health pr<strong>of</strong>essionals working with<br />
children and adolescents. 2nd ed. London: CAMHs Publications;<br />
2006.<br />
11. Broadstock M, Doughty C, Eggleston M. systematic review<br />
<strong>of</strong> the effectiveness <strong>of</strong> pharmacological treatments for adolescents<br />
and adults with autism spectrum disorder. Autism Jul<br />
2007;11(4):335–348.<br />
12. Curel P, Kumar n, Robinson B, editors. new Ethicals. 8th ed.<br />
Auckland: Adis international Ltd; 2004.<br />
13. Barkley RA. international Consensus statement on ADHD. J<br />
Am Acad Child Adolesc Psychiatry Dec 2002;41(12):1389.<br />
14. Timimi s, Moncrieff J, Jureidini J, et al. A critique <strong>of</strong> the<br />
international consensus statement on ADHD. Clin Child Fam<br />
Psychol Rev Mar 2004;7(1):59–63.<br />
15. neufield P, Foy M. Historical reflections on the ascendancy<br />
<strong>of</strong> ADHD in north America c. 1980 – c. 2005. Br J Ed studies<br />
2006;54(4):449–470.<br />
16. Leo J, Cohen D. Broken brains or flawed studies? A critical<br />
review <strong>of</strong> ADHD neuroimaging research. J Mind Behav Win<br />
2003;24(1):29–56.<br />
17. Maurice C, Green G, Foxx RM, eds. Making a difference: Behavioral<br />
interventions for Autism. Austin; 2001. TX: PRO-ED.<br />
18. O’Connor TG, Byrne J. Attachment measures for research and<br />
practice. Child Adolesc Mental Health nov 2007;12(4):187–192.<br />
19. slater R. Attachment: <strong>The</strong>oretical development and critique.<br />
Educ Psychol Pract sep 2007;23(3):205–219.<br />
20. Boris nW, Zeanah CH, Work Group on Quality i. Practice<br />
parameter for the assessment and treatment <strong>of</strong> children and<br />
adolescents with reactive attachment disorder <strong>of</strong> infancy and<br />
early childhood. J Am Acad Child Adolesc Psychiatry nov<br />
2005;44(11):1206–1219.<br />
10 VOLUME 1 • nUMBER 1 • MARCH 2009 J OURnAL OF PRiMARY HEALTH CARE
Cardiovascular risk assessment and<br />
management in mental health clients:<br />
Perceptions <strong>of</strong> mental health and general<br />
practitioners in <strong>New</strong> <strong>Zealand</strong><br />
Amanda Wheeler PGDipPsychPharm, BPharm, BSc, MRPharmS, RegPharmNZ; 1,2 Jeff Harrison PhD,<br />
DipClinPharm, GradCertClinEd, BSc (Hons), MRPharmS, RegPharmNZ, BCPS; 1,2 Zara Homes BPharm 2<br />
ABSTRACT<br />
INTRODUCTION: People with mental illness have higher rates <strong>of</strong> morbidity and mortality, largely due<br />
to increased rates <strong>of</strong> cardiovascular disease (CVD). Metabolic syndrome is well recognised but rarely<br />
expressed as a need to assess and manage cardiovascular risk factors; furthermore there is confusion<br />
about whose role this is. This study explores health practitioners’ knowledge, attitudes, barriers/solutions<br />
towards cardiovascular risk assessment and management in mental health patients.<br />
METHOD: A survey <strong>of</strong> mental health practitioners (MHPs n=421) and general practitioners (GPs n=232)<br />
was undertaken in a health service in Auckland.<br />
RESULTS: Three-quarters <strong>of</strong> respondents agreed mental illness predisposes to CVD. Fifty-five percent<br />
<strong>of</strong> MH doctors agreed they could effectively assess CVD risk compared to 67% <strong>of</strong> GPs. Only 21% <strong>of</strong> MH<br />
doctors agreed they could effectively manage CVD risk compared to 57% <strong>of</strong> GPs. Seventy-nine percent<br />
<strong>of</strong> MHPs believed that assessing CVD risk was a joint responsibility between GP and MHP, compared<br />
to 33% <strong>of</strong> GPs; 62% <strong>of</strong> GPs believed it was their sole responsibility. Forty-six percent <strong>of</strong> MHPs believed<br />
managing CVD risk was a joint responsibility compared with 29% <strong>of</strong> GPs; 58% <strong>of</strong> GPs saw this as their<br />
role. Only 13% <strong>of</strong> MHPs and fewer than 4% <strong>of</strong> GPs agreed that MH services were effectively assessing<br />
and managing CVD risk. MHPs identified lack <strong>of</strong> knowledge and skills (58%) and poor communication between<br />
primary–secondary care (53%) as the main barriers. GPs identified barriers <strong>of</strong> poor communication<br />
(64%) and patient compliance with health care management (71%). <strong>The</strong> top two solutions proposed by<br />
MHPs were provision <strong>of</strong> GP subsidies (47%) and training (43%). GPs also identified provision <strong>of</strong> a subsidy<br />
(66%) and collaborative management between GPs and MH (44%) as solutions.<br />
CONCLUSION: <strong>The</strong>re is widespread recognition <strong>of</strong> increased risk <strong>of</strong> CVD in MH patients. MHPs do not<br />
believe they have the knowledge and skills to manage this risk. GPs believe this is their responsibility.<br />
Both groups recognise communication with, and access to, primary care for MH patients as key barriers.<br />
KEyWORDS: Mental health, cardiovascular risk, risk reduction<br />
Introduction<br />
People with serious mental illness have increased<br />
rates <strong>of</strong> a variety <strong>of</strong> comorbid physical illness. 1-3<br />
<strong>The</strong> NZ Mental Health Survey found that people<br />
with mental disorder had higher prevalence rates<br />
<strong>of</strong> chronic physical conditions, including chronic<br />
ORIGINAL SCIENTIFIC PAPERS<br />
pain, cardiovascular disease, hypertension and<br />
respiratory illness; 68% with a mental disorder<br />
had at least one chronic physical condition compared<br />
with 53% without mental disorder. 3<br />
Serious mental illness is associated with excess<br />
mortality. 4-6 This excess mortality cannot<br />
qUANTITATIVE RESEARCH<br />
1 Waitemata District Health<br />
Board, Auckland<br />
2 School <strong>of</strong> Pharmacy, Faculty<br />
<strong>of</strong> Medical and Health<br />
Sciences, <strong>The</strong> University <strong>of</strong><br />
Auckland, Auckland<br />
J PRIMARY HEALTH CARE<br />
2009;1(1):11–19.<br />
CORRESPONDENCE TO<br />
Amanda Wheeler<br />
Director, Clinical<br />
Research & Resource<br />
Centre, Waitemata<br />
District Health Board,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
amanda.wheeler@<br />
waitematadhb.govt.nz<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 11
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
be explained by self-harm or other injury. 7 A<br />
meta-analysis demonstrated a 1.5–fold increase in<br />
age-adjusted mortality for people with schizophrenia;<br />
8 similar increases have been found in<br />
cohorts with bipolar and major depression. 4 Cardiovascular<br />
disease (CVD) is one <strong>of</strong> the dominant<br />
factors in this excess mortality 9-12 and there is<br />
evidence <strong>of</strong> an excess <strong>of</strong> obesity, hypertension,<br />
metabolic syndrome and type II diabetes that<br />
underpins this greater cardiovascular morbidity<br />
and mortality. 13-18<br />
Compounding this increased prevalence <strong>of</strong> CVD<br />
risk factors are the medications for mental illness,<br />
particularly second-generation antipsychotics and<br />
mood stabilisers. <strong>The</strong>se agents are associated with<br />
the development <strong>of</strong> insulin resistance, abdominal<br />
obesity, the metabolic syndrome and overt diabetes.<br />
19-26 Such metabolic changes translate directly<br />
into an atherogenic risk factor pr<strong>of</strong>ile. 10,27<br />
<strong>The</strong> NZ Health Strategy has highlighted significant<br />
health inequalities and the need to improve<br />
the health status <strong>of</strong> people with mental illness as<br />
one <strong>of</strong> its 13 goals for improvement. 28 A document<br />
that recognises the importance <strong>of</strong> effectively<br />
assessing and managing risk factors for metabolic<br />
syndrome in people with mental illness has been<br />
developed and disseminated by a national mental<br />
health (MH) metabolic working group. However,<br />
there is incomplete linkage <strong>of</strong> this to CVD risk<br />
and inconsistent implementation <strong>of</strong> the recommendations<br />
<strong>of</strong> this initiative throughout the<br />
country. 29 <strong>The</strong>re also appears to be confusion over<br />
role boundaries, with health pr<strong>of</strong>essionals being<br />
unsure <strong>of</strong> whose responsibility it is to assess and<br />
manage the physical health <strong>of</strong> patients with a serious<br />
mental illness. This is particularly a problem<br />
for people whose only access to the health system<br />
is through their psychiatrist or MH provider.<br />
This study aimed firstly to determine health practitioners’<br />
attitudes and knowledge about the assessment<br />
and management <strong>of</strong> cardiovascular risk<br />
in patients with a mental illness and, secondly,<br />
to identify the barriers and possible solutions to<br />
addressing this <strong>issue</strong>. <strong>The</strong>re is a particular focus<br />
on whom health pr<strong>of</strong>essionals believe should be<br />
responsible for monitoring and managing the<br />
physical health <strong>of</strong> secondary care MH patients.<br />
Methods<br />
Questionnaire development<br />
A semi-structured interview was conducted with<br />
eight key informants to explore knowledge, experience,<br />
current practice and attitudes in assessing<br />
and managing cardiovascular risk in people with<br />
a serious mental illness. <strong>The</strong> key informants<br />
included MH practitioners, GPs and a consumer<br />
advisor. Based on the preliminary findings, a<br />
questionnaire was developed addressing the important<br />
areas <strong>of</strong> the study. A draft questionnaire<br />
was piloted with another eight MH and primary<br />
care practitioners, who provided feedback on the<br />
questionnaire’s content and format; changes were<br />
made accordingly.<br />
Two final questionnaires were developed. One,<br />
for MH practitioners, consisting <strong>of</strong> 35 questions<br />
and the other, for GPs, omitted three questions<br />
and some questions were amended slightly to<br />
ensure audience relevancy. Each questionnaire<br />
took five to 10 minutes to complete. <strong>The</strong> first<br />
section collected demographic data (years <strong>of</strong><br />
experience, age, ethnicity) as well as information<br />
pr<strong>of</strong>iling the patients the participant provided<br />
care for. <strong>The</strong> second section consisted <strong>of</strong> attitudinal<br />
questions. Participants were asked if they<br />
were concerned about psychotropic medications<br />
increasing cardiovascular risk and to indicate (using<br />
a 6-point Likert scale) whether they agreed or<br />
disagreed with statements ranging from strongly<br />
agree to strongly disagree, or how <strong>of</strong>ten they<br />
referred patients to particular interventions, ranging<br />
from always to never. <strong>The</strong>re was also a series<br />
<strong>of</strong> questions assessing the practitioner’s level <strong>of</strong><br />
knowledge <strong>of</strong> cardiovascular risk assessment.<br />
<strong>The</strong> final part <strong>of</strong> the survey asked participants to<br />
identify (from a list generated from key informant<br />
interviews and pilot) the three most important<br />
barriers and solutions to assessment and<br />
management <strong>of</strong> cardiovascular risk in people with<br />
a serious mental illness. Further comments could<br />
be made at the end <strong>of</strong> the survey. (A copy <strong>of</strong> the<br />
questionnaire can be requested from corresponding<br />
author).<br />
Ethics approval was obtained from the University<br />
<strong>of</strong> Auckland Human Participants Ethics Committee<br />
(2006/L/020).<br />
12 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Participants<br />
<strong>The</strong> anonymous questionnaire was distributed to<br />
MH practitioners and GPs providing care within<br />
the Waitemata District Health Board catchment<br />
area. This service is the largest in NZ and provides<br />
both primary and secondary health care to north<br />
and west Auckland [2006 population <strong>of</strong> 481 611<br />
making up 12% <strong>of</strong> total population 30 ] and includes<br />
forensic, acute and community MH services. <strong>The</strong><br />
questionnaire was distributed by email to 421 MH<br />
practitioners (83 senior medical <strong>of</strong>ficers [psychiatrists<br />
and medical <strong>of</strong>ficers], 93 psychiatric trainees,<br />
seven house <strong>of</strong>ficers, six MH pharmacists and<br />
231 MH nursing staff). An email reminder was<br />
sent two weeks later; the researchers also attended<br />
medical education and team meetings to encourage<br />
participation. Participants were asked to return<br />
anonymous questionnaires in the internal mail.<br />
Questionnaires were also disseminated to 232<br />
GPs across six Primary Health Organisations<br />
Table 1. Participant demographics<br />
Pr<strong>of</strong>essional role<br />
Response rate<br />
Years experience<br />
0–5<br />
SMO<br />
n (%)<br />
22/83<br />
(27)<br />
Nil<br />
5–10 2/22<br />
(9.1)<br />
10–15 4/22<br />
(18.2)<br />
15+ 16/22<br />
(72.7)<br />
Ethnicity<br />
NZ<br />
European<br />
12/22<br />
(54.5)<br />
Other** 10/22<br />
(45.5)<br />
MH<br />
nurse<br />
n (%)<br />
52/231<br />
(22.5)<br />
5/52<br />
(9.6)<br />
7/52<br />
(13.5)<br />
10/52<br />
(19.2)<br />
30/52<br />
(57.7)<br />
32/52<br />
(61.5)<br />
20/52<br />
(38.5)<br />
MH<br />
pharmacist<br />
n (%)<br />
6/6<br />
(100)<br />
1/6<br />
(16.7)<br />
2/6<br />
(33.3)<br />
3/6<br />
(50)<br />
House<br />
<strong>of</strong>ficer<br />
n (%)<br />
3/7<br />
(43)<br />
2/3<br />
(66.7)<br />
Nil<br />
1/3<br />
(33.3)<br />
Nil Nil<br />
5/6<br />
(83.3)<br />
1/6<br />
(16.7)<br />
1/3<br />
(33.3)<br />
2/3<br />
(66.6)<br />
Psychiatric<br />
trainee<br />
n (%)<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 13<br />
23/93<br />
(25)<br />
6/23<br />
(26.1)<br />
9/23<br />
(39.1)<br />
3/23<br />
(13.0)<br />
5/23<br />
(21.7)<br />
9/23<br />
(39.1)<br />
14/23<br />
(60.9)<br />
GP<br />
n (%)<br />
90/232<br />
(38.8)<br />
5/90<br />
(5.5)<br />
7/90<br />
(7.8)<br />
16/90<br />
(17.8)<br />
62/90<br />
(68.9)<br />
72/90<br />
(80.0)<br />
18/90<br />
(20.0)<br />
Total*<br />
n (%)<br />
203/611<br />
(33.2)<br />
19/198<br />
(9.6)<br />
27/198<br />
(13.6)<br />
37/198<br />
(18.7)<br />
115/198<br />
(58.1)<br />
132/198<br />
(66.7)<br />
66/198<br />
(33.3)<br />
* Seven MH participants did not disclose their pr<strong>of</strong>essional role and five participants did not disclose their ethnicity or<br />
answer the clinical experience question.<br />
** Other ethnicities included Other European, Maori, Pacific, Asian, African, Middle Eastern, North American, and not<br />
specified. <strong>The</strong>se were grouped to protect participants’ identity within small health pr<strong>of</strong>essional groups.<br />
SMO = Senior Medical Officer (psychiatrists and medical <strong>of</strong>ficers)<br />
WHAT GAP THIS FILLS<br />
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
What we already know: People with serious mental health disorders<br />
have an excess <strong>of</strong> morbidity and mortality due to physical health problems,<br />
including cardiovascular disease. Mental health medicines increase the risk<br />
<strong>of</strong> metabolic syndrome contributing to the excess cardiovascular disease<br />
seen in this group.<br />
What this study adds: <strong>The</strong>re is a gap between knowledge and action in<br />
cardiovascular disease (CVD) risk assessment and management for mental<br />
health patients. Primary health care providers are best placed to manage<br />
CVD risk, but shared care between primary care and specialist mental health<br />
services, and mechanisms to improve access to primary care for this vulnerable<br />
group, are needed.<br />
(PHOs) located in the health service catchment<br />
area. This was done using methods chosen at the<br />
discretion <strong>of</strong> the PHO and included emailing the<br />
questionnaire to a central contact who distributed<br />
the questionnaire to GPs; posting the question-
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
Table 2. Practitioners’ views about psychotropic treatments increasing cardiovascular risk<br />
Schizophrenia<br />
Table 3. Proportion <strong>of</strong> respondents identifying cardiovascular risk management targets<br />
correctly<br />
MH practitioner<br />
n (%)<br />
<strong>General</strong> practitioner<br />
n (%)<br />
BP (< 140/85mmHg) 2 /111(1.8) 7/89 (7.9)<br />
FPG (< 6mmol/L) 25/108 (23.1) 29/89 (32.6)<br />
Total Cholesterol<br />
(
or strongly agreed that they could accurately and<br />
effectively manage CVD risk compared to 54.4%<br />
<strong>of</strong> GPs.<br />
Knowledge<br />
Most participants were unable to correctly answer<br />
the target blood pressure, fasting plasma glucose,<br />
total cholesterol and low-density lipoprotein levels<br />
for a non-diabetic patient required to achieve<br />
a reduction in the five-year cardiovascular risk<br />
(Table 3).<br />
Responsibility for cardiovascular risk<br />
assessment and management<br />
Respondents’ views on whose role it was to assess<br />
and manage cardiovascular risk were explored<br />
next, along with questions about their own<br />
current practice in such activities. Most MH practitioners<br />
(79.1%) believed that assessing cardiovascular<br />
risk was a joint responsibility between the<br />
GP and the MH practitioner, whereas only 31.8%<br />
<strong>of</strong> GPs agreed. In contrast, GPs were far more<br />
likely to believe it was their sole responsibility<br />
compared with MH practitioners (62.5% vs 17.3%).<br />
Just less than half <strong>of</strong> MH practitioners (46.4%)<br />
believed that managing a patient’s cardiovascular<br />
risk was the joint responsibility <strong>of</strong> the GP and<br />
MH practitioner compared with 28.4% <strong>of</strong> GPs.<br />
Again, GPs were more likely to see this as their<br />
role (56.8% vs 33.6%).<br />
Finally, only 12.8% <strong>of</strong> MH practitioners and 6.9%<br />
<strong>of</strong> GPs agreed or strongly agreed that MH services<br />
effectively assess and manage cardiovascular<br />
risk in patients with serious mental illness.<br />
Respondents considered dietary advice the most<br />
required service; most respondents agreed or<br />
strongly agreed their patients required referral<br />
for dietary advice (93.6% MH practitioners; 82.2%<br />
GPs). However, fewer than half <strong>of</strong> both practitioner<br />
groups (39.5% MH practitioners; 31.5%<br />
GPs) stated that they referred patients for dietary<br />
advice either always or most <strong>of</strong> the time.<br />
Most participants agreed or strongly agreed<br />
that their patients required referral to exercise<br />
programmes (83.7% and 78.9% respectively), about<br />
ORIGINAL SCIENTIFIC PAPERS<br />
a third <strong>of</strong> practitioners stating they referred<br />
patients to these services either always or most <strong>of</strong><br />
the time (36.9% compared with 36.4%). Exercise<br />
referrals included the Green Prescription,<br />
to gyms in the local community or to secondary<br />
care facilities. Just over 80% <strong>of</strong> participants<br />
believed that their patients required referral to<br />
smoking cessation programmes, such as Quitline,<br />
or for nicotine replacement therapy. GPs were<br />
more likely to refer patients to appropriate smoking<br />
cessation services (44.3% vs 27.8%; chi 2 =3.07,<br />
df=1, p=0.08).<br />
qUANTITATIVE RESEARCH<br />
Figure 1. Barriers to cardiovascular risk assessment and management in mental health<br />
patients<br />
Figure 2. Solutions for cardiovascular risk assessment and management for mental health<br />
patients<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 15
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
Barriers and solutions to cardiovascular<br />
risk assessment and management<br />
Respondents were asked to indicate the three<br />
most important barriers and solutions to effectively<br />
assessing and managing CVD for patients<br />
with a serious mental illness (Figures 1 and 2).<br />
For MH practitioners the top two barriers were<br />
secondary care providers’ knowledge and skills<br />
(57.6%) and lack <strong>of</strong> communication between MH<br />
provider and GP (52.9%). Lack <strong>of</strong> time in secondary<br />
care to complete assessment and follow-up<br />
(41.2%) and patients’ financial status to accessing<br />
primary care and medications (41.2%) were jointly<br />
the third most frequently rated barrier.<br />
<strong>The</strong> top three solutions to overcome barriers<br />
were (in decreasing importance) subsidising GP<br />
visits (47.4%), training or continued education<br />
on cardiovascular screening for MH practitioners<br />
(43.2%), establishing cardiovascular screening<br />
guidelines and interventions, and improving<br />
communication between primary and secondary<br />
care (both 37.9%).<br />
This question was presented slightly differently<br />
to GPs and three options were omitted. GPs rated<br />
the most important barrier as patient factors; that<br />
is, compliance with medication and follow-up<br />
appointments (71.6%). Consistent with MH practitioners,<br />
lack <strong>of</strong> communication between MH<br />
provider and GP and a patient’s financial ability<br />
to access primary care and medications were both<br />
rated as second most important barrier (59.5%).<br />
GPs agreed with MH practitioners that subsidising<br />
primary care visits would be the most effective<br />
solution to overcoming these barriers (62.3%).<br />
<strong>The</strong> next two important solutions for GPs were<br />
collaborative management between MH and GP<br />
(45.5%), and provision <strong>of</strong> proactive programmes/<br />
interventions for cardiovascular risk assessment/<br />
management (42.1%).<br />
Other comments<br />
Participants were given the opportunity to write<br />
comments at the end <strong>of</strong> the survey. Most MH<br />
practitioners focussed on the fact that they believed<br />
that they should be involved in the assessment<br />
<strong>of</strong> cardiovascular risk and helping patients<br />
to access primary health care, but that it was not<br />
their responsibility to manage this risk. Some<br />
respondents expressed concern about time and<br />
resource constraints that might restrict their ability<br />
to comprehensively manage these risk factors.<br />
<strong>The</strong>re was some personal anxiety and concern<br />
expressed at the poor level <strong>of</strong> knowledge <strong>of</strong> MH<br />
practitioners in this area <strong>of</strong> health care.<br />
Most <strong>of</strong> the comments from GPs focussed on<br />
funding, both in terms <strong>of</strong> a patient’s inability to<br />
pay for services and in terms <strong>of</strong> the limitations<br />
placed on the resources available to GPs. GPs also<br />
commented, but to a lesser extent, that the expertise<br />
and therefore the responsibility for managing<br />
cardiovascular risk lay with GPs. Some respondents<br />
from this group felt that the restrictions on<br />
time in primary care for consultations (average 10<br />
minutes) prevented discussions about anything<br />
more than acute <strong>issue</strong>s with patients. Lack <strong>of</strong><br />
communication between providers and paucity <strong>of</strong><br />
MH practitioners well-trained in the cardiovascular<br />
risk area was also <strong>of</strong> concern.<br />
Discussion<br />
This was the first NZ study to explore MH<br />
practitioners’ and GPs’ views on assessment and<br />
management <strong>of</strong> cardiovascular risk in people<br />
with serious mental illness. Most practitioners<br />
were aware <strong>of</strong> MH patients’ increased cardiovascular<br />
risk. Interestingly, practitioners appeared<br />
to associate the increased risk with the MH<br />
treatments they were most used to prescribing in<br />
everyday practice; treatments for schizophrenia<br />
and bipolar disorder for MH practitioners and<br />
treatments for depression in GPs. MH practitioners<br />
rated second-generation antipsychotics as the<br />
medications they were most concerned about<br />
for increasing cardiovascular risk. However, it<br />
was surprising that other medications, such as<br />
lithium and sodium valproate were not associated<br />
with increased risk by MH practitioners; there<br />
is a well-described relationship between these<br />
medications and appetite increase, weight gain,<br />
and metabolic syndrome. 31,32<br />
Whilst approximately half <strong>of</strong> MH doctors had<br />
confidence in their ability to assess patients’<br />
CVD risk, only one-fifth had faith in their own<br />
ability to effectively manage cardiovascular risk.<br />
16 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
In comparison, equal numbers <strong>of</strong> GPs reported<br />
confidence in cardiovascular assessment and<br />
management. Given the recent high pr<strong>of</strong>ile <strong>of</strong><br />
CVD risk assessment and management both<br />
nationally and amongst PHOs in the Auckland<br />
area, it is perhaps surprising that fewer than<br />
two-thirds <strong>of</strong> GPs agreed that they could do this<br />
effectively. Furthermore, respondents reported<br />
confidence with assessment and management was<br />
somewhat at odds with the finding that their<br />
knowledge <strong>of</strong> current guideline screening targets<br />
was poor; fewer than one-tenth <strong>of</strong> MH practitioners<br />
and GPs could correctly identify the<br />
NZGG target blood pressure and total cholesterol<br />
level for a non-diabetic patient with a five-year<br />
CVD risk >15%.<br />
<strong>The</strong> survey found respondents had little faith in<br />
the current ability <strong>of</strong> MH services to accurately<br />
and effectively assess and manage cardiovascular<br />
risk—overall only 10% <strong>of</strong> practitioners agreed<br />
that this was being done effectively at present.<br />
MH practitioners suggested that they relied on<br />
the primary care sector (via joint mechanisms)<br />
for physical health screening and solely on the<br />
primary care sector for management. Most GPs<br />
believed that both screening and management<br />
were their sole responsibility. Written comments<br />
provided further evidence <strong>of</strong> this belief,<br />
with some MH practitioners stating it was their<br />
responsibility to identify risks, but that they<br />
referred patients to the GP for risk management,<br />
and some GPs commented that they had the<br />
knowledge and expertise in this area.<br />
Whilst most practitioners believed that MH<br />
patients needed to be able to access assistance<br />
and programmes for dietary advice, exercise and<br />
smoking cessation, only about a third <strong>of</strong> practitioners<br />
surveyed actually completed referrals for<br />
patients as part <strong>of</strong> their clinical role. This may<br />
indicate a lack <strong>of</strong> knowledge about the services<br />
available and how to access them or may reflect<br />
the uncertainty about the boundaries <strong>of</strong> care<br />
between MH and primary care services.<br />
Despite suggestions that MH practitioners feel<br />
partly responsible for assessing cardiovascular<br />
risk, they were aware <strong>of</strong> their lack <strong>of</strong> knowledge<br />
and skill in this area and believe that they would<br />
benefit from both further training and guidance.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
<strong>The</strong>y identified that provision <strong>of</strong> guidelines for<br />
assessment and management interventions would<br />
be useful to improve this lack <strong>of</strong> knowledge. <strong>The</strong><br />
<strong>New</strong> <strong>Zealand</strong> Mental Health Metabolic Working<br />
Group <strong>issue</strong>d guidance on monitoring for the<br />
metabolic syndrome in patients with mental illness<br />
in 2006. 33 However, this guidance does not<br />
make specific links to assessment and management<br />
<strong>of</strong> cardiovascular risk, nor do the NZGG<br />
guidelines 34 identify people with serious mental<br />
illness as a risk group to be targeted for risk assessment.<br />
Whilst there is evidence describing the<br />
effect <strong>of</strong> MH treatments on some indices <strong>of</strong> CVD<br />
risk, there is little data describing their effect<br />
on global CVD risk. Because the existing risk<br />
prediction models are based on population data,<br />
they may underestimate risk in this relatively<br />
young patient group; further work needs to be<br />
undertaken in this area.<br />
Financial factors were identified as an important<br />
barrier to physical health screening and management<br />
by both practitioner groups. Traditionally,<br />
screening has been managed by the primary care<br />
sector, where a co-payment has been required to<br />
visit a GP and co-payment is <strong>of</strong>ten required for<br />
prescriptions. <strong>The</strong> subsidy <strong>of</strong> regular and longer<br />
duration primary care visits and long-term treatments<br />
for this at-risk group potentially removes<br />
one <strong>of</strong> the barriers to accessing primary health<br />
care and treatment. Respondents also identified<br />
the need for better communication between the<br />
two services as vital in order to improve physical<br />
health outcomes. This is particularly important<br />
if the patient has been prescribed psychotropic<br />
medications that are essential in the treatment<br />
<strong>of</strong> mental illness but which may further increase<br />
the patient’s cardiovascular risk. Collaborative<br />
management may be needed to assist patients attend<br />
follow-up appointments in primary care and<br />
adhere to additional medication.<br />
Also <strong>of</strong> note is the particular significance <strong>of</strong> some<br />
<strong>of</strong> the <strong>issue</strong>s, highlighted in this research, to<br />
cohorts <strong>of</strong> mental health clients from Maori and<br />
Pacific backgrounds. Maori and Pacific ethnicities<br />
appear to be at increased risk <strong>of</strong> CVD; Maori are<br />
known to have a higher incidence <strong>of</strong> cardiovascular<br />
events (both fatal and non-fatal) and have<br />
them earlier than non-Maori. 34 CVD contributes<br />
significantly to earlier mortality and significant<br />
qUANTITATIVE RESEARCH<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 17
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
morbidity in Pacific people compared to European.<br />
34 Diabetes and obesity also affect Maori<br />
and Pacific peoples disproportionately compared<br />
to Europeans; this is reflected in an increased<br />
morbidity and mortality due to diabetes. 35<br />
This inequitable burden <strong>of</strong> disease is exacerbated<br />
further where CVD, diabetes and serious mental<br />
illness intersect. Maori were found to have a<br />
higher prevalence <strong>of</strong> mental illness, both serious<br />
and in general, compared to the NZ general<br />
population. 36 For serious mental illness requiring<br />
inpatient treatment, admissions for Maori have<br />
been found to be higher than non-Maori. 37,38<br />
<strong>The</strong> relationship between socioeconomic position,<br />
CVD, diabetes and mental illness is strong<br />
and, in NZ, over half the Maori population and<br />
an even greater proportion <strong>of</strong> Pacific people live<br />
in the most deprived areas. 34 However, the NZ<br />
Mental Health Survey found that Maori and<br />
Pacific people with mental illness were less likely<br />
to access health services <strong>of</strong> any type, regardless<br />
<strong>of</strong> sociodemographic factors such as age and<br />
household income. 39 This could partially be due<br />
the fact that, although secondary services are free<br />
at the point <strong>of</strong> care, primary care services where<br />
physical health is traditionally managed are only<br />
partially subsidised and the two systems function<br />
independently <strong>of</strong> each other. All <strong>of</strong> these factors<br />
may collectively put Maori and Pacific people<br />
at further risk <strong>of</strong> cardiovascular mortality. <strong>The</strong><br />
<strong>issue</strong>s raised by both MH practitioners and GPs<br />
with regard to access and subsidy for primary<br />
care services may be <strong>of</strong> particular significance to<br />
Maori and Pacific people, and those in the lowest<br />
socioeconomic groups.<br />
We are not aware <strong>of</strong> any published studies exploring<br />
the views <strong>of</strong> both MH practitioners and<br />
GPs, nor any focussing on cardiovascular risk.<br />
However, our findings, in terms <strong>of</strong> the concerns<br />
<strong>of</strong> MH practitioners, are reflected by two papers<br />
examining US psychiatrists’ awareness <strong>of</strong> and<br />
concerns about the impact <strong>of</strong> therapies for bipolar<br />
disorder 40 and schizophrenia 41 on metabolic<br />
syndrome. <strong>The</strong>se surveys highlighted that US<br />
psychiatrists recognise metabolic syndrome as<br />
a significant health risk and screen for metabolic<br />
effects, primarily weight gain and glucose<br />
intolerance. Psychiatrists treating bipolar disorder<br />
indicated that they also measure lipids and, to a<br />
lesser degree, blood pressure and waist circumference.<br />
40 Suppes et al. reported that three-quarters<br />
<strong>of</strong> respondents reported having diagnosed metabolic<br />
syndrome, but only 28% correctly identified<br />
the five variables used to diagnose metabolic syndrome;<br />
this has parallels with our own findings<br />
about CVD risk factor targets. Finally, Suppes<br />
et al. reported that 92% <strong>of</strong> respondents referred<br />
patients to primary care for management <strong>of</strong><br />
metabolic risk factors; this reflects the views <strong>of</strong><br />
our respondents that this is the most appropriate<br />
setting for management <strong>of</strong> CVD risk.<br />
<strong>The</strong> main limitation <strong>of</strong> this study is the poor<br />
response rate, particularly from nursing staff.<br />
Whilst the response rate is disappointing, the<br />
possible implication is that non-responders were<br />
less knowledgeable or, perhaps, less concerned<br />
about the risks <strong>of</strong> CVD in MH patients. <strong>The</strong><br />
assumption that lack <strong>of</strong> knowledge about the<br />
area resulted in a poorer response is somewhat<br />
supported by comments made at the end <strong>of</strong> the<br />
survey and to the facilitators who presented the<br />
survey to potential participants at journal club<br />
and CME meetings. If this assumption is correct,<br />
then the scale <strong>of</strong> inaction and unmet need may be<br />
greater even than highlighted in this study.<br />
In conclusion, this survey found that there is<br />
widespread recognition <strong>of</strong> the increased risk <strong>of</strong><br />
CVD in patients with a serious mental illness.<br />
MH practitioners do not currently have the<br />
knowledge and skills to assume responsibility for<br />
assessing or managing this risk. GPs believe that<br />
this is primarily their responsibility. Both groups<br />
recognise the barriers presented by communication<br />
with, and access to, primary care services<br />
for, MH patients. <strong>The</strong> survey highlights potential<br />
concerns about the management <strong>of</strong> physical<br />
health in this high-risk group; further research is<br />
required to both identify the burden <strong>of</strong> physical<br />
ill health in this group, and to describe their engagement<br />
with physical and preventative health<br />
services, including CVD risk assessment and<br />
management.<br />
References<br />
1. Dickey B, Normand SL, Weiss RD, Drake RE, Azeni H. Medical<br />
morbidity, mental illness, and substance use disorders. Psychiatr<br />
Serv 2002;53(7):861–7.<br />
2. Sokal J, Messias E, Dickerson FB, Kreyenbuhl J, Brown CH,<br />
Goldberg RW, et al. Comorbidity <strong>of</strong> medical illnesses among<br />
18 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
adults with serious mental illness who are receiving community<br />
psychiatric services. J Nerv Ment Dis 2004;192(6):421–7.<br />
3. Scott KM, Oakley Browne MA, McGee MA, Wells JE. Mentalphysical<br />
comorbidity in Te Rau Hinengaro: <strong>The</strong> <strong>New</strong> <strong>Zealand</strong><br />
Mental Health Survey. Aust NZ J Psychiatry 2006;40(10):882–8.<br />
4. Harris EC, Barraclough B. Excess mortality <strong>of</strong> mental disorder.<br />
Br J Psychiatry 1998;173:11–53.<br />
5. Osby U, Brandt L, Correia N, Ekbom A, Sparen P. Excess mortality<br />
in bipolar and unipolar disorder in Sweden. Arch Gen<br />
Psychiatry 2001;58(9):844–50.<br />
6. Weeke A, Juel K, Vaeth M. Cardiovascular death and manicdepressive<br />
psychosis. J Affect Disord 1987;13(3):287–92.<br />
7. Osby U, Correia N, Brandt L, Ekbom A, Sparen P. Mortality<br />
and causes <strong>of</strong> death in schizophrenia in Stockholm county,<br />
Sweden. Schizophr Res 2000;45(1-2):21–8.<br />
8. Brown S. Excess mortality <strong>of</strong> schizophrenia. A meta-analysis.<br />
British Journal <strong>of</strong> Psychiatry 1997;171:502–8.<br />
9. Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King<br />
MB. Relative risk <strong>of</strong> cardiovascular and cancer mortality in<br />
people with severe mental illness from the United Kingdom’s<br />
<strong>General</strong> Practice Rsearch Database. Arch Gen Psychiatry<br />
2007;64(2):242–9.<br />
10. Enger C, Weatherby L, Reynolds RF, Glasser DB, Walker AM.<br />
Serious cardiovascular events and mortality among patients<br />
with schizophrenia. J Nerv Ment Dis 2004;192(1):19–27.<br />
11. Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia<br />
and increased risks <strong>of</strong> cardiovascular disease. Am<br />
Heart J 2005;150(6):1115–21.<br />
12. Lambert TJR, Velakoulis D, Pantelis C. Medical comorbidity in<br />
schizophrenia. Med J Aust 2003;178(9 (Suppl)):s67–s70.<br />
13. Kendrick T. Cardiovascular and respiratory risk factors and<br />
symptoms among general practice patients with long-term<br />
mental illness. Br J Psychiatry 1996;169(6):733–9.<br />
14. Davidson S, Judd F, Jolley D, Hocking B, Thompson S, Hyland<br />
B. Cardiovascular risk factors for people with mental illness.<br />
Aust N Z J Psychiatry 2001;35(2):196–202.<br />
15. Ryan MCM, Thakore JH. Physical consequences <strong>of</strong> schizophrenia<br />
and its treatment: the metabolic syndrome. Life Sci<br />
2002;71(3):239–57.<br />
16. Basu R, Brar JS, Chengappa KNR, John V, Parepally H,<br />
Gershon S, et al. <strong>The</strong> prevalence <strong>of</strong> the metabolic syndrome<br />
in patients with schizoaffective disorder—bipolar subtype.<br />
Bipolar Disord 2004;6(4):314–8.<br />
17. Morriss R, Mohammed FA. Metabolism, lifestyle and bipolar<br />
affective disorder. J Psychopharmacol 2005;19(6_suppl):94–101.<br />
18. Tirupati S, Chua LE. Obesity and metabolic syndrome in<br />
a psychiatric rehabilitation service. Aust NZ J Psychiatry<br />
2007;41(7):606–10.<br />
19. Mackin P, Watkinson HM, Young AH. Prevalence <strong>of</strong> obesity,<br />
glucose homeostasis disorders and metabolic syndrome in psychiatric<br />
patients taking typical or atypical antipsychotic drugs: a<br />
cross-sectional study. Diabetologia 2005;48(2):215–21.<br />
20. Meyer JM, Koro CE. <strong>The</strong> effects <strong>of</strong> antipsychotic therapy<br />
on serum lipids: a comprehensive review. Schizophr Res<br />
20 04;70(1):1–17.<br />
21. <strong>New</strong>comer JW. Second-generation (atypical) antipsychotics<br />
and metabolic effects: A comprehensive literature review.<br />
CNS Drugs 2005;19(SUPPL. 1):1–93.<br />
22. Ryan MCM, Flanagan S, Kinsella U, Keeling F, Thakore JH. <strong>The</strong><br />
effects <strong>of</strong> atypical antipsychotics on visceral fat distribution in<br />
first episode, drug-naive patients with schizophrenia. Life Sci<br />
2004;74(16):1999–2008.<br />
23. Sacchetti E, Turrina C, Parrinello G, Brignoli O, Stefanini<br />
G, Mazzaglia G. Incidence <strong>of</strong> diabetes in a general practice<br />
population: a database cohort study on the relationship with<br />
haloperidol, olanzapine, risperidone or quetiapine exposure.<br />
Int J Clin Psychopharmacol 2005;20(1):33–7.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
24. Wang C-j, Zhang Z-j, Sun J, Zhang X-b, Mou X-d, Zhang X-r,<br />
et al. Serum free fatty acids and glucose metabolism, insulin<br />
resistance in schizophrenia with chronic antipsychotics. Biol<br />
Psychiatry 2006;60(12):1309–13.<br />
25. Wirshing DA, Boyd JA, Meng LR, Ballon JS, Marder SR, Wirshing<br />
WC. <strong>The</strong> effects <strong>of</strong> novel antipsychotics on glucose and<br />
lipid levels. J Clin Psychiatry 2002;63(10):856–65.<br />
26. Zipursky RB, Gu H, Green AI, Perkins DO, Tohen MF, McEvoy<br />
JP, et al. Course and predictors <strong>of</strong> weight gain in people with<br />
first-episode psychosis treated with olanzapine or haloperidol.<br />
Br J Psychiatry 2005;187:537–43.<br />
27. Almeras N, Despres J-P, Villeneuve J, Demers M-F, Roy M-A,<br />
Cadrin C, et al. Development <strong>of</strong> an atherogenic metabolic risk<br />
factor pr<strong>of</strong>ile associated with the use <strong>of</strong> atypical antipsychotics.<br />
J Clin Psychiatry 2004;65(4):557–64.<br />
28. Ministry <strong>of</strong> Health. <strong>The</strong> <strong>New</strong> <strong>Zealand</strong> Health Strategy. Wellington,<br />
<strong>New</strong> <strong>Zealand</strong>: Ministry <strong>of</strong> Health; 2000.<br />
29. <strong>New</strong> <strong>Zealand</strong> Mental Health Metabolic Working<br />
Group. Intervention Guide for Mental Health Service Users on<br />
Antipsychotic <strong>The</strong>rapy. Auckland: Janssen<br />
Cilag NZ Ltd; 2006.<br />
30. Walker RA, Martin S. Demographic Pr<strong>of</strong>ile for Waitemata<br />
District Health Board: An Analysis <strong>of</strong> 2006 Census. Auckland:<br />
Watemata District Health Board; 2007.<br />
31. Breum L, Astrup A, Gram L, Andersen T, Stokholm KH, Christensen<br />
NJ, et al. Metabolic changes during treatment with<br />
valproate in humans: implication for untoward weight gain.<br />
Metabolism 1992;41(6):666–70.<br />
32. Vendsborg PB, Bech P, Rafaelsen OJ. Lithium treatment and<br />
weight gain. Acta Psychiatr Scand 1976;53(2):139–47.<br />
33. <strong>New</strong> <strong>Zealand</strong> Mental Health Metabolic Working Group. A<br />
<strong>New</strong> <strong>Zealand</strong> Mental Health Metabolic Working Group Initiative.<br />
Auckland: Janssen Cilag Ltd; 2006.<br />
34. <strong>New</strong> <strong>Zealand</strong> Guidelines Group. <strong>The</strong> assessment and management<br />
<strong>of</strong> cardiovascular risk: Evidence-based best practice<br />
guideline. Wellington: <strong>New</strong> <strong>Zealand</strong> Guidelines Group<br />
(NZGG); 2003.<br />
35. <strong>New</strong> <strong>Zealand</strong> Guidelines Group. Management <strong>of</strong> Type 2<br />
Diabetes: Evidence-based best practice guideline. Wellington:<br />
<strong>New</strong> <strong>Zealand</strong> Guidelines Group (NZGG); 2003.<br />
36. Wells JE, Browne MAO, Scott KM, McGee MA, Baxter J, Kokaua<br />
J. Te Rau Hinengaro: <strong>The</strong> <strong>New</strong> <strong>Zealand</strong> Mental Health Survey:<br />
Overview <strong>of</strong> methods and findings. 2006;40(10):835–44.<br />
37. Wheeler A, Robinson E, Robinson G. Admissions to acute<br />
psychiatric inpatient services in Auckland, <strong>New</strong> <strong>Zealand</strong>:<br />
a demographic and diagnostic review. N Z Med J<br />
2005;118(1226):U1752.<br />
38. Edmonds LK, Williams S, Walsh AE. Trends in Maori mental<br />
health in Otago. Aust N Z J Psychiatry 2000;34(4):677–83.<br />
39. Baxter J, Kokaua J, Wells JE, McGee MA, Browne MAO. Ethnic<br />
comparisons <strong>of</strong> the 12 month prevalence <strong>of</strong> mental disorders<br />
and treatment contact in Te Rau Hinengaro: <strong>The</strong> <strong>New</strong> <strong>Zealand</strong><br />
Mental Health Survey. 2006;40(10):905–13.<br />
40. Suppes T, McElroy SL, Hirschfeld RMA. Awareness <strong>of</strong> Metabolic<br />
Concerns and Perceived Impact <strong>of</strong> Pharmacotherapy in<br />
Patients with Bipolar Disorder: A Survey <strong>of</strong> 500 US Psychiatrists.<br />
Psychopharmacol Bull 2007;40(2):22–37.<br />
41. <strong>New</strong>comer JW, Nasrallah HA, Loebel AD. <strong>The</strong> Atypical<br />
Antipsychotic <strong>The</strong>rapy and Metabolic Issues National Survey:<br />
practice patterns and knowledge <strong>of</strong> psychiatrists. 2004;24(5<br />
Suppl 1):S1–6.<br />
qUANTITATIVE RESEARCH<br />
ACKNOWLEDGMENTS<br />
We would like to<br />
acknowledge the<br />
support <strong>of</strong> the MH<br />
practitioners and consumer<br />
representatives who were<br />
interviewed, piloted and<br />
who provided feedback<br />
in the development<br />
<strong>of</strong> the survey. We<br />
also acknowledge the<br />
support <strong>of</strong> the DHBs<br />
and PHOs in distributing<br />
the survey. Finally, we<br />
are very grateful to the<br />
respondents for their time<br />
participating in the survey.<br />
COMPETING INTERESTS<br />
None declared.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 19
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
1 Muar District <strong>of</strong> Health,<br />
Muar, Johor, Malaysia<br />
2 Department <strong>of</strong> Family<br />
Medicine, Faculty <strong>of</strong><br />
Medicine, Universiti<br />
Kebangsaan Malaysia,<br />
Malaysia<br />
3 Department <strong>of</strong> Public<br />
Health, Faculty <strong>of</strong> Medicine,<br />
Universiti Kebangsaan<br />
Malaysia, Malaysia<br />
J PRIMARY HEALTH CARE<br />
2009;1(1):20–25.<br />
CORRESPONDENCE TO:<br />
Arshad Hanisah<br />
Family Medicine Specialist,<br />
Muar District <strong>of</strong> Health,<br />
Jalan Othman, 84000<br />
Muar, Johor, Malaysia<br />
ihanisah@hotmail.com<br />
Prevalence <strong>of</strong> acne and its impact on the<br />
quality <strong>of</strong> life in school-aged adolescents<br />
in Malaysia<br />
Arshad Hanisah MMed (FamMed UKM); 1 Khairani Omar MMed (FamMed UKM); 2 Shamsul Azhar Shah 3<br />
ABSTRACT<br />
AIM: <strong>The</strong> objective <strong>of</strong> this study was to determine the prevalence <strong>of</strong> facial acne and its impact on the<br />
quality <strong>of</strong> life among adolescents attending secondary schools in Muar, Malaysia.<br />
METHODS: A cross-sectional study was conducted where 409 samples were selected using stratified<br />
cluster random sampling from two secondary schools in Muar, involving Form 1 to Form 5 students.<br />
Students were diagnosed clinically and the severity <strong>of</strong> facial acne was assessed using Global Acne Grading<br />
System. A self-reported Cardiff Acne Disability Index was used to assess the quality <strong>of</strong> life among<br />
adolescents who had acne.<br />
RESULTS: <strong>The</strong> prevalence <strong>of</strong> facial acne among the adolescents was 67.5% (n=276). Facial acne increased<br />
with increasing age (p=0.001). It was more common among males (71.1%) than females (64.6%),<br />
p=0.165. <strong>The</strong> males also had a higher prevalence <strong>of</strong> severe acne (p=0.001). <strong>The</strong> quality <strong>of</strong> life was<br />
affected by the severity <strong>of</strong> acne. Students with severe acne had higher levels <strong>of</strong> Cardiff Acne Disability<br />
Index (rho=0.521).<br />
CONCLUSION: Facial acne is a common disorder and appears to have a considerable impact on quality<br />
<strong>of</strong> life among adolescents. <strong>The</strong> above findings should alert health care pr<strong>of</strong>essionals and the school<br />
authorities to actively identify, manage and educate adolescents with facial acne.<br />
KEyWORDS: Facial acne, adolescents, Cardiff Acne Disability Index, quality <strong>of</strong> life<br />
Introduction<br />
Acne vulgaris is the most common dermatological<br />
condition encountered in adolescents. It affects<br />
almost 85% <strong>of</strong> people 12–24 years <strong>of</strong> age. 1 It<br />
commonly affects young people during the time<br />
when they are undergoing maximum psychological,<br />
social and physical changes.<br />
Acne commonly involves the face. Facial appearance<br />
represents important aspects <strong>of</strong> one’s<br />
perception <strong>of</strong> body image. <strong>The</strong>refore, it is not<br />
surprising that a susceptible individual with<br />
facial acne may develop significant psychosocial<br />
disability. Emotional stress can also exacerbate<br />
acne, and patients with acne may develop<br />
psychiatric problems as a consequence <strong>of</strong> their<br />
problem. 2<br />
Skin disease can have a major impact on one’s<br />
quality <strong>of</strong> life. Overall quality <strong>of</strong> life is an all<br />
inclusive concept incorporating all factors that<br />
impact upon an individual life. <strong>The</strong> concept<br />
can be divided into several components, including<br />
psychological, social and physical domains. 3<br />
<strong>The</strong> impact <strong>of</strong> acne on a particular patient is not<br />
always easy to judge clinically. It was found that<br />
both women and men find the effects <strong>of</strong> acne<br />
on appearance to be the most bothersome aspect<br />
<strong>of</strong> their disease and the negative effects <strong>of</strong> acne<br />
occur in both older and younger patients. 4 Even<br />
mild acne can pose a significant problem for some<br />
patients, diminishing their quality <strong>of</strong> life and in<br />
some cases their social functioning. 5,6<br />
Acne may also be associated with decreased selfesteem/self-confidence,<br />
interpersonal difficulties,<br />
20 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
unemployment and increased prevalence <strong>of</strong> anxiety<br />
and depression. 7,8 A study <strong>of</strong> 111 acne patients<br />
aged 16 years and over attending a United Kingdom<br />
dermatology outpatient clinic found levels<br />
<strong>of</strong> social and emotional problems are comparable<br />
with those in people with severe chronic disabling<br />
disease such as arthritis and epilepsy. 9<br />
However, the relationship between the severity<br />
<strong>of</strong> acne and emotional distress is poorly understood<br />
although it is known that acne is a source<br />
<strong>of</strong> distress and embarrassment. 10 <strong>The</strong>refore there<br />
is a need to study the psychosocial impact and<br />
the quality <strong>of</strong> life <strong>of</strong> young people with acne<br />
using validated and age appropriate measures and<br />
an objective assessment <strong>of</strong> acne status. Thus the<br />
aim <strong>of</strong> this study is to determine the prevalence<br />
<strong>of</strong> acne and its impact on the quality <strong>of</strong> life in<br />
adolescents.<br />
Materials and methods<br />
This was a cross-sectional study conducted in two<br />
secondary schools in Muar, Malaysia. Muar is a<br />
district in one <strong>of</strong> the states in Malaysia. It has a<br />
multiethnic population. <strong>The</strong>re are about 17 secondary<br />
schools in the district. <strong>The</strong> two secondary<br />
schools were selected randomly. <strong>The</strong>se schools are<br />
co-educational schools which comprise Form 1 to<br />
Form 5 students.<br />
<strong>The</strong> calculation <strong>of</strong> sample size was performed<br />
using Epi info Statistical Package, using the formula<br />
n=[ z / s ] 2 x p [ 1-p ], where n is a sample<br />
size, z is the confidence interval taken as 1.96, s<br />
is taken as 0.05 and p is the probability in this<br />
study and taken as prevalence <strong>of</strong> acne vulgaris in<br />
Malaysia which is about 85%. 11 Considering the<br />
drop <strong>of</strong>f rate as 10%, the minimum sample size<br />
calculated was 196. <strong>The</strong> sample size was then<br />
doubled to 400 due to stratified cluster sampling<br />
method.<br />
With the approval <strong>of</strong> the headmasters <strong>of</strong> the<br />
two secondary schools, the lists <strong>of</strong> students were<br />
obtained from the school registration books. <strong>The</strong><br />
study population was stratified into five strata<br />
based on their forms; Form 1 to Form 5. In each<br />
stratum, the samples were selected randomly. <strong>The</strong><br />
informed consent letter describing the research<br />
was given to the selected students and their par-<br />
WHAT GAP THIS FILLS<br />
ORIGINAL SCIENTIFIC PAPERS<br />
What we already know: Acne vulgaris is the most common dermatological<br />
condition encountered in adolescents, affecting them at a time when they<br />
are undergoing maximum psychological, social and physical changes. Acne<br />
can pose a significant problem for some patients, diminishing their social<br />
functioning and may be associated with decreased self-esteem/self-confidence,<br />
interpersonal difficulties, unemployment and increased prevalence <strong>of</strong><br />
anxiety and depression.<br />
What this study adds: Facial acne is a common disorder and appears to<br />
have a considerable impact on quality <strong>of</strong> life among adolescents attending<br />
secondary schools, particularly in severe cases. Primary health care pr<strong>of</strong>essionals<br />
and school authorities should actively identify, manage and educate<br />
adolescents on facial acne.<br />
ents. <strong>The</strong> students were excluded from the study<br />
if they or their parents refused to give consent.<br />
Absentees during the data collection day were<br />
also excluded from the study.<br />
On the data collection day, schools were visited<br />
by the researcher and school health nurse. Each<br />
student was examined for acne. In this study, the<br />
examination for acne included the head and neck<br />
only. All the manifestations <strong>of</strong> acne from comedone<br />
to nodules, not only by its presence but also<br />
number was reported. <strong>The</strong> acne severity was then<br />
graded using Global Acne Grading System. <strong>The</strong><br />
students with acne were then given self-reported<br />
Cardiff Acne Disability Index questionnaire.<br />
Clinical diagnosis was used to determine presence<br />
<strong>of</strong> acne. Facial acne was graded using<br />
the Global Acne Grading System (GAGS). 12<br />
<strong>The</strong> GAGS consider five locations on the face,<br />
with a factor at each location based roughly<br />
on surface area, distribution, and density <strong>of</strong><br />
pilosebaceous units. <strong>The</strong> borders on the face are<br />
delineated by the hairline, jaw line and ears.<br />
No magnifying glass or skin stretching was<br />
allowed, and good lighting was suggested. In<br />
this study all the manifestations <strong>of</strong> acne from<br />
comedones to nodules, not only by its presence<br />
but also number, were reported. Each <strong>of</strong> the<br />
location was graded separately on 0–4 scale,<br />
with the most severe lesion within that location<br />
determining the local score. <strong>The</strong> researcher<br />
then graded acne severity according to the<br />
qUANTITATIVE RESEARCH<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 21
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
Table 1. Prevalence <strong>of</strong> acne among the adolescents<br />
Gender<br />
global score which is the summation <strong>of</strong> all local<br />
scores. <strong>The</strong> maximum score was 32.<br />
Cardiff Acne Disability Index (CADI) is a wellvalidated<br />
self-reported questionnaire consisting<br />
<strong>of</strong> five questions with a Likert scale, four<br />
response categories (0–3). 13 <strong>The</strong> final score ranges<br />
from 0–15. <strong>The</strong> Cardiff Acne Disability Index is<br />
designed for use in teenagers and young adults<br />
with acne. <strong>The</strong> five questions relate to feeling <strong>of</strong><br />
aggression, frustration, interference with social<br />
life, avoidance <strong>of</strong> public changing facilities and<br />
appearance <strong>of</strong> the skin—all over the last month—<br />
and an indication <strong>of</strong> how bad the acne was now.<br />
<strong>The</strong> CADI score was calculated by summing<br />
the score <strong>of</strong> each question resulting in a possible<br />
maximum <strong>of</strong> 15 and minimum <strong>of</strong> 0. CADI scores<br />
were graded as low (0–4), medium (5–9) and high<br />
(10–15). <strong>The</strong> lower the cumulative CADI score,<br />
the lower the level <strong>of</strong> disability experienced<br />
by the student while a higher score indicated<br />
a higher level <strong>of</strong> disability. <strong>The</strong> CADI identifies<br />
area <strong>of</strong> concern in patients with acne. <strong>The</strong><br />
patients’ response to the questionnaire is significantly<br />
correlated with the clinicians’ assessment<br />
<strong>of</strong> acne severity.<br />
Presence <strong>of</strong> acne No acne Total p value<br />
n % n % n %<br />
Male 128 71.1 52 28.9 180 100 0.165<br />
Female 148 64.6 81 36.4 229 100<br />
Age (years)<br />
13 31 44.2 39 55.7 70 100 0.001<br />
14 57 64.0 32 36.0 89 100<br />
15 54 66.7 27 33.3 81 100<br />
16 65 76.5 20 23.5 85 100<br />
17 60 81.0 14 19 74 100<br />
18 9 90.0 1 10 10 100<br />
Ethnicity<br />
Malay 155 64.3 86 35.7 241 100 0.084<br />
Chinese 121 72.5 46 27.5 167 100<br />
Total 276 67.5 133 32.5 409 100<br />
<strong>The</strong> majority <strong>of</strong> students from age 13 to 18 years old had mild facial acne (90.2%)<br />
(refer table 2)<br />
Data was analysed using SPSS (Statistical Package<br />
for Social Studies) programme (version 11; SPSS<br />
Inc., Chicago). <strong>The</strong> level <strong>of</strong> significance was set at<br />
p
<strong>The</strong>re was a significant difference between acne<br />
severity and gender (c 2 = 16.47, p=0.001). However,<br />
there was no significant difference between<br />
facial acne severity and ethnicity (c 2 = 1.56,<br />
p>0.05) (refer to Tables 4 and 5).<br />
<strong>The</strong>re was a moderately strong correlation<br />
between facial acne severity and Cardiff Acne<br />
Disability Index (rho=0.521) at p=0.01 (Figure 1).<br />
(Correlation coefficient, rho0.8 very strong).<br />
<strong>The</strong> impact on quality <strong>of</strong> life increased with the<br />
facial acne severity.<br />
<strong>The</strong>re was no association between CADI score<br />
and gender: Mann–Whitney test (z score=0.046,<br />
p=0.964). It is an important finding, as there may<br />
be a perception among some health pr<strong>of</strong>essional<br />
that facial acne will have less impact on males. It<br />
showed that males were also aware <strong>of</strong> their skin<br />
problems.<br />
Discussion<br />
This study showed that facial acne is a common<br />
problem among adolescents in Muar, affecting<br />
71.1% <strong>of</strong> boys and 64.6% <strong>of</strong> girls. A study done<br />
in Turkey using Global Acne Grading System,<br />
reported that the prevalence <strong>of</strong> acne among high<br />
school students was 23.1%. 14 <strong>The</strong> difference in<br />
prevalence rates between these two studies may<br />
reflect ethnic differences or the involvement <strong>of</strong><br />
trunk examination which may limit participation<br />
<strong>of</strong> the adolescents. An Australian study showed<br />
that overall prevalence <strong>of</strong> acne was 36.1%. 15 In<br />
another study using Leeds Acne Grading Scale,<br />
reported the prevalence <strong>of</strong> acne in UK teenagers<br />
as 50%. 16 Comparisons <strong>of</strong> prevalence rate between<br />
studies are hampered by the varied methods <strong>of</strong><br />
acne grading used by different studies and the<br />
wide range <strong>of</strong> diagnostic criteria used. For this<br />
reason, in this study it was best to report all the<br />
manifestations <strong>of</strong> acne from comedone to nodules,<br />
not only by its presence but also number.<br />
<strong>The</strong> researcher then graded acne severity according<br />
to the global score which is the summation <strong>of</strong><br />
all local scores. Again, there is no internationally<br />
agreed system for reporting severity, although<br />
various systems have been recommended. Nevertheless,<br />
Global Acne Grading System has been<br />
Table 2. Severity <strong>of</strong> facial acne by age, gender and ethnicity<br />
Age (years)<br />
Acne Severity Total<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 23<br />
Mild<br />
n (%)<br />
Moderate<br />
n (%)<br />
Severe<br />
n (%) n (%)<br />
13 29 (93.5) 2 (6.5) 0 (0) 31 (100)<br />
14 53 (93.0) 4 (7.0) 0 (0) 57 (100)<br />
15 47 (87.0) 4 (7.4) 3 (5.6) 54 (100)<br />
16 57 (87.7) 6 (9.2) 2 (3.1) 65 (100)<br />
17 55 (91.7) 3 (5.0) 2 (3.3) 60 (100)<br />
18 8 (88.9) 1 (11.1) 0 (0) 9 (100)<br />
Overall 249 (90.2) 20 (7.3) 7 (2.5) 276 (100)<br />
Gender<br />
Males 106 (82.8) 15 (11.7) 7 (5.5) 128 (100)<br />
Females 143 (96.6) 5 (3.4) 0 (0) 148 (100)<br />
Ethnicity<br />
ORIGINAL SCIENTIFIC PAPERS<br />
Malay 136 (87.7) 13 (8.4) 6 (3.7) 155 (100)<br />
Chinese 113 (93.4) 7 (5.8) 19 (0.8) 139 (100)<br />
Table 3. Specific responses <strong>of</strong> Cardiff Acne Disability Index<br />
Specific responses <strong>of</strong> CADI<br />
(N = 276)<br />
Frequency<br />
(n )<br />
Percentage<br />
(%)<br />
Felt aggressive, frustrated 196 71.0<br />
Social interference 162 58.7<br />
Avoidance <strong>of</strong> public changing 49 17.8<br />
Patient psychological state 225 81.9<br />
Subjective assessment <strong>of</strong> acne severity<br />
(perceived as problem)<br />
Table 4. Relationship between acne severity and gender<br />
251 90.9<br />
Acne severity Male (n) Female (n ) Test p value<br />
Mild acne 106 143 c2 = 16.47 0.001<br />
Moderate to severe acne 22 5<br />
TOTAL 128 148<br />
Table 5. Relationship between facial acne severity and ethnicity<br />
Acne severity Malay (n) Non-Malay (n) Test p value<br />
Mild acne 136 113 c2 = 1.56 0.21<br />
Moderate to severe acne 19 26<br />
TOTAL 155 139<br />
qUANTITATIVE RESEARCH
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
found to be accurate and have minimal inter- and<br />
intra-rater variability. 11<br />
<strong>The</strong> findings in this study showed that acne prevalence<br />
increased with increasing age. This finding<br />
is similar to a previous study done in Australia. 14<br />
In this study, the male students were found to<br />
have more moderately severe acne compared to<br />
female students. <strong>The</strong> findings are consistent with<br />
previous studies done in other countries. 14,15,16,17<br />
Males tend to have more severe acne compared to<br />
females because they have oilier complexion and<br />
their androgen levels are higher. 18,19<br />
Cardiff Acne Disability Index helps to assess<br />
the quality <strong>of</strong> life in students with acne. <strong>The</strong><br />
subscales include feeling <strong>of</strong> aggression, frustration,<br />
interference with social life, avoidance <strong>of</strong><br />
public changing facilities and appearance <strong>of</strong> the<br />
skin. In this study, analysis <strong>of</strong> the subscales<br />
showed that the adolescents had particular<br />
difficulties in the areas <strong>of</strong> emotion (felt aggressive,<br />
frustrated), social interference/difficulties<br />
and psychological state disturbance. A study<br />
among teenage Scottish schoolchildren reported<br />
that 50% <strong>of</strong> pupils were emotionally affected by<br />
their acne. Twenty percent <strong>of</strong> pupils were affected<br />
in their personal and social lives because<br />
Figure 1. Spearman’s rho coefficient demonstrating correlation between Global Acne<br />
Grading Score and Cardiff Acne Disability Index.<br />
<strong>of</strong> their acne and 10% avoided swimming and<br />
other sports because <strong>of</strong> embarrassment. 20 In<br />
this study, five students (1.8%) scored 13 in Cardiff<br />
Acne Disability Index which was equal to<br />
severely impaired. It implied that the students<br />
had severe psychological impact from facial acne<br />
problem. However, the median score <strong>of</strong> CADI<br />
was 4, which was low. This implied that overall<br />
the students were mildly affected psychologically.<br />
This could be due to the higher prevalence<br />
<strong>of</strong> mild acne among the students. It also showed<br />
that the impact <strong>of</strong> acne on the students was<br />
influenced by the acne severity.<br />
This study demonstrated a moderately strong correlation<br />
between the total score <strong>of</strong> Cardiff Acne<br />
Disability Index and acne severity. <strong>The</strong> impact<br />
on quality <strong>of</strong> life increased with the facial acne<br />
severity. This result is consistent with previous<br />
studies which also demonstrated a fairly good<br />
correlation between facial acne severity and<br />
Cardiff Acne Disability Index. 15,20,21 This implies<br />
that impact <strong>of</strong> acne on quality <strong>of</strong> life must be<br />
considered in the management <strong>of</strong> facial acne.<br />
Overall, there was no significant difference in<br />
the CADI score between the genders (Mann–<br />
Whitney test, p>0.5). <strong>The</strong> impact <strong>of</strong> acne on<br />
quality <strong>of</strong> life was similar between genders.<br />
However, this contradicts results from previous<br />
studies which found that girls generally experience<br />
more psychological morbidity than boys. 22<br />
<strong>The</strong> finding in this study is important as there<br />
may be perception among some health pr<strong>of</strong>essionals<br />
that facial acne will have less impact on males.<br />
This study showed that male adolescents were<br />
also aware <strong>of</strong> their skin problems.<br />
<strong>The</strong> major limitation <strong>of</strong> this study is its crosssectional<br />
design. A prospective study would be<br />
better to demonstrate a direct causal link between<br />
acne and quality <strong>of</strong> life. Although we obtained<br />
a good response rate, it is possible that students<br />
who either refused to take part or who were<br />
absent represent more vulnerable adolescents or<br />
those most embarrassed by their skin. <strong>The</strong> study<br />
is likely therefore to have underestimated the<br />
impact <strong>of</strong> acne on quality <strong>of</strong> life. In this study,<br />
the CADI and GAG scores (especially the CADI)<br />
were quite skewed. Dichotomising the scores<br />
would perhaps demonstrate better results.<br />
24 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Conclusion<br />
Facial acne is common among adolescents and can<br />
cause major impact on their quality <strong>of</strong> life. It is important<br />
for the health pr<strong>of</strong>essionals to incorporate<br />
quality <strong>of</strong> life measurements when managing adolescents<br />
with acne. Cardiff Acne Disability Index<br />
is a useful tool to identify individual with facial<br />
acne who had poor quality <strong>of</strong> life. Health education<br />
is needed in our secondary schools to ensure<br />
that adolescents understand their disease, know<br />
what treatments are available and from whom they<br />
should seek advice. Health pr<strong>of</strong>essionals should<br />
be aware that early acne treatment can prevent<br />
progression <strong>of</strong> the disease and its complication.<br />
References<br />
1. Krowchuck DP. Managing Acne in Adolescent. Pediatr Clin<br />
North Am 2000;47(4):841–857.<br />
2. Koo JYM, Smith LL. Psychological aspects <strong>of</strong> acne. Pediatr J<br />
Dermatol 1991;8:185–188.<br />
3. Price P, Harding KG. Delining quality <strong>of</strong> life. J Wound Care<br />
1993;2:304–306.<br />
4. Jowett S, Ryan T. Skin disease and handicap: Analysis <strong>of</strong> the<br />
impact <strong>of</strong> skin condition. Soc Sci Med 1985;20:425–429.<br />
5. Lasek RJ, Chren MM. Acne vulgaris and the quality <strong>of</strong> life <strong>of</strong><br />
adult dermatology patients. Arch Dermatol 1998;134:454–458.<br />
6. Picardi A, Abeni D, Melchi CF, Puddu P, Pasquini P. Psychiatri<br />
morbidity in dermatological outpatients: an <strong>issue</strong> to be recognized.<br />
Br J Dermatol 2000;143:983–991.<br />
7. Koo J. <strong>The</strong> psychosocial impact <strong>of</strong> acne: Patient’s perceptions.<br />
J Am Acad Dermatol 1995;32:26–30.<br />
8. Wu SF, Kinder BN. Role <strong>of</strong> anxiety and anger in acne patients:<br />
a relationship with severity <strong>of</strong> the disorder. J Am Acad Dermatol<br />
1988;18:325–332.<br />
9. Mallon E, <strong>New</strong>ton JN. <strong>The</strong> quality <strong>of</strong> life in acne. J Am Acad<br />
Dermatol 1999;140:672–676.<br />
10. Lowe JG. <strong>The</strong> stigma <strong>of</strong> acne. Br J Hosp Med 1993;49:809–812.<br />
11. Khairani O, Zaiton S, Faridah MN. Do adolescents attending<br />
Bandar Mas Primary Care Clinic consult health pr<strong>of</strong>essional<br />
for their common health problems? Med J Malaysia<br />
2005;60(2):134–139.<br />
12. Doshi A, Zaheer A, Stiller MJ. A comparison <strong>of</strong> current acne<br />
grading systems and proposal <strong>of</strong> novel system. Int J Dermatol<br />
1997;36:416–418.<br />
13. Motley RJ, Finlay AY. Practical use <strong>of</strong> disability index in the<br />
routine management <strong>of</strong> acne. Clin Exp Dermatol 1992;17:1–3.<br />
14. Atkan S, Ozmen E, Sanli B. Anxiety, depression and nature <strong>of</strong><br />
acne vulgaris in adolescents. Int J Dermatol 2000;39:354–357.<br />
15. Killkenny M, Merlin K. Prevalence <strong>of</strong> common skin condition<br />
in Australia school student: Acne vulgaris. Br J Dermatol 1998;<br />
139:840–845.<br />
16. Smithard A, Glazebrook C, Williams HC. Acne prevalence,<br />
knowledge about acne and psychological morbidity in mid<br />
adolescence: A community base study. Br J Dermatol 2001;<br />
145:274–279.<br />
17. Stathakis V, Kilkenny M, Marks R. Descriptive epidemiology<br />
<strong>of</strong> acne vulgaris in the community. Australas J Dermatol<br />
1997;38:115–123.<br />
18. Lucky AW, Biro FM. Acne vulgaris in early adolescent boys<br />
correlation with pubertal maturation and age. Arch Dermatol<br />
1991;172:210–216.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
19. Burton JL, Cunliffe WJ, Stafford I, Shuster S. <strong>The</strong> prevalence <strong>of</strong><br />
acne vulgaris in adolescence. Br J Dermatol 1971;85:119–126.<br />
20. Walker N, Lewis Jones MS. quality <strong>of</strong> life and acne in Scottish<br />
adolescent children: use <strong>of</strong> the Children’s Dermatology Life<br />
quality Index (CDLqI) and the Cardiff Acne Disability Index<br />
(CADI). J Eur Acad Dermatol Venereol 2006;20:45–50.<br />
21. Motley RJ, Finlay AY. How much disability cause by acne. Clin<br />
Exp Dermatol 1989;14:194–198.<br />
22. Cotteril JA, Cunliffe WJ. Suicide in dermatological patients. Br<br />
J Dermatol 1997;137:246–250.<br />
qUANTITATIVE RESEARCH<br />
AKNOWLEDGEMENTS<br />
Permission to use the Cardiff<br />
Acne Disability Index was<br />
obtained from Pr<strong>of</strong> Andrew<br />
Finlay, Department <strong>of</strong><br />
Dermatology, University <strong>of</strong><br />
Wales <strong>College</strong> <strong>of</strong> Medicine,<br />
Cardiff, UK and permission<br />
to use the Acne Management<br />
questionnaire was obtained<br />
from Dr Cris Glazebrook,<br />
Behavioural Section, Division<br />
<strong>of</strong> Psychiatry, queens Medical<br />
Centre, Nottingham, UK.<br />
COMPETING INTERESTS<br />
None declared.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 25
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
1 Department <strong>of</strong> <strong>General</strong><br />
Practice & Primary Health<br />
Care, Faculty <strong>of</strong> Medical<br />
and Health Science, <strong>The</strong><br />
University <strong>of</strong> Auckland,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
2 Department <strong>of</strong> Maori Health<br />
(Te Kupenga Hauora Maori),<br />
Faculty <strong>of</strong> Medical and Health<br />
Science, <strong>The</strong> University <strong>of</strong><br />
Auckland<br />
3 Department <strong>of</strong> <strong>General</strong><br />
Practice, University <strong>of</strong><br />
Melbourne, Victoria, Australia<br />
4 Department <strong>of</strong> Psychological<br />
Medicine, University <strong>of</strong><br />
Auckland<br />
5 Department <strong>of</strong> Statistics,<br />
University <strong>of</strong> Auckland<br />
J PRIMARY HEALTH CARE<br />
2009;1(1):26–29.<br />
CORRESPONDENCE TO:<br />
Bruce Arroll<br />
Head <strong>of</strong> the Department<br />
<strong>of</strong> <strong>General</strong> Practice and<br />
Primary Health Care,<br />
Faculty <strong>of</strong> Medical and<br />
Health Sciences, <strong>The</strong><br />
University <strong>of</strong> Auckland,<br />
PB 92019, Auckland,<br />
<strong>New</strong> <strong>Zealand</strong><br />
b.arroll@auckland.ac.nz<br />
<strong>The</strong> prevalence <strong>of</strong> depression among Maori<br />
patients in Auckland general practice<br />
Bruce Arroll MBChB, PhD, FRNZCGP; 1 Felicity Goodyear-Smith MBChB, MGP, FRNZCGP; 1 Ngaire Kerse<br />
MBChB, PhD, FRNZCGP; 1 Melanie Hwang; 1 Susan Crengle MBChB FAFPHM (RACP); 2 Jane Gunn MBBS,<br />
PHD; 3 Tana Fishman DO, Am Osteo Bd Cert Fam Prac, FRNZCGP; 1 Simon Hatcher MBBS, MRCPsych,<br />
FRANZCP; 4 Sanat Pradhan MSc; 5 Karishma Sidhu MSc 5<br />
ABSTRACT<br />
INTRODUCTION: <strong>The</strong>re has been concern over high rates <strong>of</strong> mental illness in Maori. Previous studies in<br />
general practice have had small sample sizes.<br />
AIM: To determine the prevalence <strong>of</strong> major depression among Maori patients in Auckland general practice<br />
using the CIDI and the PHq as measurement tools.<br />
METHODS: This prevalence study is part <strong>of</strong> a larger randomised trial. <strong>The</strong> patients were recruited from<br />
77 general practitioners from around Auckland who could provide a private room for interviewing. <strong>The</strong><br />
patients were invited to participate in the waiting room and all consecutive patients were approached. For<br />
this study all patients received a computerised CIDI examination and one third received a PHq assessment<br />
prior to getting the CIDI. <strong>The</strong> interviewer was blind to the questionnaire results when the patient<br />
did the CIDI.<br />
RESULTS: <strong>The</strong>re were 7994 patients approached from whom there were data on 7432. <strong>The</strong> prevalence<br />
<strong>of</strong> Maori in the study was 9.7%. <strong>The</strong> overall 12-month prevalence <strong>of</strong> major depression based on the CIDI<br />
was 10.1% 95%CI (8.8 to 11.4). For Maori the prevalence was 11.5% 95%CI (8.8 to 14.2) and for non-<br />
Maori 10.1% 95%CI (8.6 to 11.3). For Maori men and Maori women the prevalence was 8.5% and 13.4%<br />
and for non-Maori men and non-Maori women it was 8.3% and 11.1%. <strong>The</strong> prevalence <strong>of</strong> depression over<br />
at least the previous two weeks on the PHq ≥9 for all participants was 12.9% 95%CI (11.2 to 14.5).<br />
DISCUSSION: <strong>The</strong> prevalence <strong>of</strong> depression among Maori is high, but not as high as earlier studies. This<br />
may be due to the bigger sample size <strong>of</strong> this study.<br />
KEyWORDS: Maori, prevalence, depression, primary care, general practice, <strong>New</strong> <strong>Zealand</strong><br />
Introduction<br />
Maori have had poorer mental health for decades<br />
while clear evidence has been collected in the<br />
last 20 years. 1,2 In particular, a concern about<br />
high rates <strong>of</strong> depression among Maori has been<br />
suggested, with few confirming studies. Increasingly,<br />
differences in mental health service use<br />
and clinical characteristics between different<br />
ethnic groups have been reflected in the <strong>of</strong>ficial<br />
statistics, while recent studies have found<br />
positive evidence <strong>of</strong> disparities between Maori<br />
and non-Maori populations at both primary and<br />
secondary levels <strong>of</strong> care. 3,4<br />
<strong>The</strong> most recent investigation on mental health<br />
in general practice found higher rates <strong>of</strong> major<br />
depression among Maori general practice attenders<br />
(46.4% in Maori while 15.4% in non-Maori<br />
in the last 12 months) 5 with the highest rates <strong>of</strong><br />
depression in female Maori patients (55.2%) and<br />
the greatest ethnological disparity between Maori<br />
and non-Maori women. However, these findings<br />
26 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
were based on a small number (n=81) <strong>of</strong> Maori<br />
respondents; therefore it is not clear how generalisable<br />
this information is. <strong>The</strong> <strong>New</strong> <strong>Zealand</strong><br />
Mental Health survey was a national study which<br />
included 2595 Maori. <strong>The</strong> results from this community<br />
sample reported a mood disorder in Maori<br />
<strong>of</strong> 11.4% (12-month prevalence) versus 7.4% in the<br />
general population. 6<br />
Our study looks at the prevalence <strong>of</strong> depression<br />
among Maori patients in Auckland general<br />
practices in participants recruited as part <strong>of</strong> a<br />
randomised trial.<br />
Methods<br />
This paper uses data from a randomised control<br />
trial <strong>of</strong> the Patient Health Questionnaire (PHQ), 7<br />
the Two Question With Help Questionnaire<br />
(TQWHQ) 8 and no screening in general practice.<br />
<strong>The</strong> PHQ has nine questions based on the DSM-<br />
IV. <strong>The</strong> TQWHQ is a three-question screening<br />
tool. This paper reports the prevalence <strong>of</strong> depression<br />
as detected in recruited participants. All<br />
participants completed the computerised CIDI<br />
(Composite International Diagnostic Interview)<br />
to evaluate the presence <strong>of</strong> depression as a gold<br />
standard. 9,10 <strong>The</strong> PHQ was administered to one<br />
third <strong>of</strong> the sample. RCT methodology and<br />
results will be reported in mid-2009.<br />
Recruitment <strong>of</strong> general practitioners<br />
All general practitioners in Auckland who<br />
worked greater than four-tenths in practice were<br />
eligible for the study. All eligible patients who<br />
gave informed consent were enrolled. A fee <strong>of</strong> $9<br />
per patient was paid to each GP to compensate for<br />
time spent asking the patient to meet with the<br />
interviewer, and reassessing patients found to be<br />
suicidal on the questionnaires. <strong>General</strong> practices<br />
in Auckland had to be able to provide a separate<br />
room for patient interviews. <strong>The</strong> study took place<br />
from 2006 to 2009.<br />
Recruitment <strong>of</strong> patients/index consultation<br />
Patients were eligible for the study if they were<br />
able to communicate in English, were aged over<br />
16 years, and were not suffering from any brain<br />
injury, dementia, terminal illness or intoxication.<br />
WHAT GAP THIS FILLS<br />
What we already know: Based on small studies, the prevalence <strong>of</strong> depression<br />
in Maori patients is high compared to non-Maori.<br />
What this study adds: <strong>The</strong> rates <strong>of</strong> depression in a larger group <strong>of</strong> Maori<br />
are high, but lower than previously estimated.<br />
Consecutive patients were approached in the waiting<br />
room and asked to participate in the study.<br />
Patients were recruited consecutively in order to<br />
obtain an adequate spectrum <strong>of</strong> disease as part <strong>of</strong><br />
screening and diagnostic test studies. After providing<br />
written informed consent they were asked<br />
to go to a private room to complete the study<br />
procedures. <strong>The</strong> interviewer was blind to the<br />
screening questionnaire results when the patients<br />
did the CIDI. <strong>The</strong> study was conducted according<br />
the principles <strong>of</strong> the STARD statement. 11<br />
Ethnicity was determined by self-selection as part<br />
<strong>of</strong> the screening questionnaire based on the 2006<br />
<strong>New</strong> <strong>Zealand</strong> census. Individuals could pick more<br />
than one ethnicity. Those who chose Maori only<br />
or Maori in addition to other ethnicities were<br />
considered Maori and those who did not chose<br />
Maori at all were considered to be non-Maori. A<br />
subgroup analysis was conducted <strong>of</strong> those who<br />
chose only Maori.<br />
Ethics approval<br />
<strong>The</strong> methods and procedures used in this study<br />
were approved by the Northern Y Regional<br />
Ethics Committee, Ministry <strong>of</strong> Health. (Ethics<br />
approval number NTY/06/09/080).<br />
Statistical methods<br />
All statistical analyses were carried out using<br />
STATA data analysis and statistical s<strong>of</strong>tware version.<br />
<strong>The</strong> analysis was done using STATA v3 to<br />
take into account the effect <strong>of</strong> clustering by GP.<br />
Results<br />
ORIGINAL SCIENTIFIC PAPERS<br />
<strong>The</strong> number <strong>of</strong> patients approached was 7994<br />
from whom there were 337 refusals (4.2%) and<br />
225 incomplete interviews (either patients did not<br />
complete the screening questionnaire or did not<br />
qUANTITATIVE RESEARCH<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 27
ORIGINAL SCIENTIFIC PAPERS<br />
qUANTITATIVE RESEARCH<br />
get the CIDI). On average, 96 participants (range<br />
4–228) were recruited from each <strong>of</strong> 77 general<br />
practitioners and 67 <strong>of</strong> the GPs contributed Maori<br />
patients (average <strong>of</strong> 11 Maori per GP, range 1–48).<br />
<strong>The</strong> demographics are shown in Table 1 which<br />
shows that 9.7% <strong>of</strong> the sample were Maori and<br />
Maori patients were younger than non-Maori patients.<br />
Table 2 shows the major depression in the<br />
previous 12 months in terms <strong>of</strong> a Diagnostic and<br />
Statistical Manual (DSM) IV diagnosis reported<br />
on the CIDI computer and for PHQ score ≥ 9, 12<br />
and 14 (available on one third <strong>of</strong> participants). 12<br />
<strong>The</strong> prevalence <strong>of</strong> depression as recorded by the<br />
PHQ for more than two weeks is higher than<br />
the CIDI for the previous 12 months. A PHQ<br />
score ≥ 9 indicates major depression. A sensitivity<br />
analysis was conducted using those who chose<br />
Maori as their only ethnic group. This resulted<br />
Table 1. Demographic characteristics <strong>of</strong> general practice attenders by ethnicity<br />
Overall<br />
n = 7432<br />
Maori<br />
n = 721<br />
Non-Maori<br />
n = 6711<br />
Mean age 49 39 50<br />
Median age 48 37 49<br />
Age range 16–99 16–82 16–99<br />
Gender<br />
Female 4460 (60%) 449 (62%) 4208 (63%)<br />
Male 2973 (40%) 272 (38%) 2504 (37%)<br />
in a slightly lower prevalence for only Maori (on<br />
CIDI) 9.6% versus 11.5% for all Maori for overall<br />
depression; 11.9% versus 13.4% for Maori women<br />
and 5.9% versus 8.4% for Maori men respectively.<br />
Discussion<br />
Our results show that depression is a significant <strong>issue</strong><br />
for Maori and consistent with the <strong>New</strong> <strong>Zealand</strong><br />
Mental Health survey and the MaGPIe study,<br />
although the differences between Maori and non-<br />
Maori were not significantly different in our study.<br />
Qualitatively our results were lower than those<br />
reported in the MaGPIe study. A sensitivity<br />
analysis using those who chose Maori as their<br />
only ethnicity had a slightly lower prevalence <strong>of</strong><br />
depression than with those who chose Maori and<br />
at least one other. <strong>The</strong> numbers are too small for<br />
interpretation to be made.<br />
<strong>The</strong> strengths <strong>of</strong> this study include the high<br />
response rate and the large number <strong>of</strong> Maori<br />
recruited from general practice. <strong>The</strong> methodology<br />
was simple with recruitment followed immediately<br />
by a computerised gold standard CIDI<br />
interview. Thus the PHQ findings and the CIDI<br />
findings are from the same day.<br />
A weakness <strong>of</strong> this study is that the GPs were<br />
not chosen randomly. However it was necessary<br />
Table 2. Prevalence <strong>of</strong> depression according to CIDI-DSM-IV major depressive disorder and PHQ scores among general practice attenders by gender<br />
and ethnicity. Proportion (95% confidence interval)<br />
Overall All non-Maori All Maori Non-Maori<br />
men<br />
28 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE<br />
Maori<br />
men<br />
Non-Maori<br />
women<br />
Maori<br />
women<br />
CIDI N = 7432 N = 6711 N = 721 N = 2697 N = 272 N = 4014 N = 449<br />
CIDI +ve* 10.1%<br />
(8.8, 11.4)<br />
10.1%<br />
(8.6, 11.3)<br />
11.5%<br />
(8.8,14.2)<br />
8.3%<br />
(6.9, 9.8)<br />
8.5%<br />
(4.7, 12.2)<br />
11.1%<br />
(9.5, 12.7)<br />
13.4%<br />
(10.2, 16.5)<br />
PHQ** N = 2497 N = 2240 N = 257 N = 903 N = 84 N = 1337 N = 173<br />
> 9 12.9%<br />
(11.2, 14.5)<br />
≥ 12 9.2%<br />
(7.7, 10.7)<br />
>14 5.2%<br />
(4.2, 6.2)<br />
12.6%<br />
(10.9, 14.2)<br />
9.0%<br />
(7.5, 10.5)<br />
* Positive for major depression in the last 12 months.<br />
15.2%<br />
(10.3, 20.0)<br />
11.3%<br />
(6.6, 15.9)<br />
10.2%<br />
(8.3, 12.1)<br />
** Sub-sample assessed with the PHq depression screen—relates to at least the past two weeks.<br />
( ) = 95% confidence interval adjusted for clustering by GP.<br />
11.9%<br />
(5.9, 17.9)<br />
12.7%<br />
(9.2, 16.2)<br />
16.8%<br />
(10.7, 22.7)
to have practices with a spare room available to<br />
conduct the gold standard interviews. <strong>The</strong> other<br />
weakness is that this study may be underpowered<br />
to find true differences. <strong>The</strong> CIDI has been criticised<br />
for use in surveys other than those wanting<br />
an epidemiological estimate. In one review <strong>of</strong> the<br />
PHQ it was thought that a cut point <strong>of</strong> ≥ 12 for<br />
the PHQ may give a closer estimate to the CIDI. 13<br />
In our study a cut point <strong>of</strong> ≥ 12 would make a<br />
prevalence <strong>of</strong> 9.2% (on PHQ) versus 10.1% (CIDI)<br />
versus 12.9% with a cut point <strong>of</strong> ≥ 9. <strong>The</strong> PHQ<br />
relates to at least the previous two weeks while<br />
the CIDI can be the previous month to the previous<br />
year. It is not clear which is the better gold<br />
standard and further work may be required.<br />
<strong>The</strong> other NZ general practice study is the<br />
MaGPIe study. 5 It reported 12-month major<br />
depression prevalence rates for Maori women as<br />
55.2% (95%CI 33%–77.4%) and for Maori men as<br />
21.3% (95% CI 2.3%–40.3%). While the confidence<br />
interval estimates for Maori men in the MaGPIe<br />
study include our point estimate, the rate for<br />
women does not. <strong>The</strong> difference may lie in the<br />
different location (Wellington versus Auckland)<br />
or in the different sample sizes (MaGPIe n=81)<br />
and our study (721). <strong>The</strong>re have also been a<br />
number <strong>of</strong> national depression initiatives which<br />
may have reduced the burden <strong>of</strong> depression and<br />
the national unemployment rate was dropping<br />
until the final quarter <strong>of</strong> 2008. <strong>The</strong> other <strong>issue</strong><br />
is that <strong>of</strong> the methodology. <strong>The</strong> MaGPIe study<br />
screened patients with the GHQ (<strong>General</strong> Health<br />
Questionnaire) and then required the patient to<br />
return for a second interview. This more complicated<br />
methodology may have biased the results<br />
toward a higher prevalence estimate.<br />
<strong>The</strong>se findings on prevalence <strong>of</strong> depression<br />
were consistent with other studies investigating<br />
similar <strong>issue</strong>s overseas, as minority populations<br />
in other countries, including native Americans<br />
and US Hispanics, have higher rates <strong>of</strong> mental<br />
disorders 14,15 and the disparities were also shown<br />
in migrant populations in the United Kingdom. 16<br />
<strong>The</strong> picture <strong>of</strong> depression among Maori patients<br />
in general practice suggests that it is at least as<br />
high as that in non-Maori and most likely to be<br />
higher, particularly for women. <strong>The</strong> previous<br />
estimates may have overestimated the prevalence<br />
but it may be better to research interventions<br />
acceptable to and effective for Maori rather than<br />
obtaining a more precise estimate <strong>of</strong> the problem.<br />
References<br />
ORIGINAL SCIENTIFIC PAPERS<br />
1. Durie M. Mental health and Maori development. ANZ J Psychiatry<br />
1999;33:5–12.<br />
2. Edmonds LK, Williams S, Walsh AES. Trends in Maori mental<br />
health in Otago. ANZ J Psychiatry 2000;36:677–683.<br />
3. Trauer T, Eagar K , GM. Ethnicity, deprivation and mental<br />
health outcomes. Aust Health Rev 2006;30(3):310–321.<br />
4. Bushnell J. Mental disorders among Maori attending their<br />
general practitioner. ANZ J Psychiatry 2005;39:401–406.<br />
5. <strong>The</strong> MaGPIe Research Group UoOaWSoMaHS. Mental disorders<br />
among Maori attending their general practitioner. ANZ J<br />
Psychiatry 2005;39:401–406.<br />
6. Oakley-Browne MA, Wells EJ, Scott KMe. Te Rau Hinengaro:<br />
<strong>The</strong> <strong>New</strong> <strong>Zealand</strong> mental health survey. Wellington, <strong>New</strong><br />
<strong>Zealand</strong>: Ministry <strong>of</strong> Health; 2006.<br />
7. Nease DE, Malouin JM. Depression screening:a practical<br />
strategy. J Fam Pract 2003;52:118–26.<br />
8. Arroll B, Goodyear-Smith F, Kerse N, Fishman T, Gunn J. Effect<br />
<strong>of</strong> the addition <strong>of</strong> a ‘help’ question to two screening questions<br />
on specificity for diagnosis <strong>of</strong> depression in general practice:<br />
diagnostic validity study. BMJ 2005;15 Sept 2005(http://bmj.<br />
com/cgi/content/abstract/bmj.38607.464537.7Cv1?ecoll).<br />
9. Andrews G, Peters L, Guzman AM, Bird K. A comparison <strong>of</strong><br />
two structured diagnostic interviews: CIDI and SCAN. Aust<br />
NZ J Psychiatry 1995;29:124–32.<br />
10. Peters L, Andrews G. Procedural validity <strong>of</strong> the computerised<br />
version <strong>of</strong> the Composite International Diagnostic<br />
Interview (CIDI-Auto) in the anxiety disorders. Psychol Med<br />
1995;25:1269–80.<br />
11. Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou<br />
PP, Irwig LM, et al. Towards complete and accurate reporting<br />
<strong>of</strong> studies <strong>of</strong> diagnostic accuracy: the STARD initiative. BMJ<br />
2003;326:41–4.<br />
12. American Psychiatric Association. Diagnostic and statistical<br />
manual <strong>of</strong> mental disorders (fourth edition) DSM-IV-TR. APA<br />
Washington, DC; 2000.<br />
13. Gilbody S, Richards D, Brealey S, Hewitt C. Screening for<br />
depression in medical settings with the Patient Health questionnaire<br />
(PHq): a diagnostic meta-analysis. J Genl Intl Med<br />
2007;22(11):1596–602.<br />
14. Lewis-Fernandez R, Das AK, Alfonso C, Weissman MM, Olfson<br />
M. Depression in US Hispanics: Diagnostic and Management<br />
Considerations in Family Practice. J Am Board Fam Pract<br />
2005;18:282–296.<br />
15. Office SGs. Mental Health: A Report <strong>of</strong> <strong>The</strong> Surgeon <strong>General</strong>.<br />
Washington, DC: Office <strong>of</strong> the Surgeon <strong>General</strong>; 1999.<br />
16. Bhugra D. Migration and depression. Acta Psychiatrica Scandinavica<br />
2003;Suppl 418:67–72.<br />
qUANTITATIVE RESEARCH<br />
ACKNOWLEDGEMENTS<br />
This study was funded<br />
by a grant from the<br />
Health Research Council<br />
<strong>of</strong> <strong>New</strong> <strong>Zealand</strong>.<br />
COMPETING INTERESTS<br />
None declared.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 29
ORIGINAL SCIENTIFIC PAPERS<br />
MIXED METHOD RESEARCH<br />
1 School <strong>of</strong> Pharmacy,<br />
University <strong>of</strong> Otago, Dunedin,<br />
<strong>New</strong> <strong>Zealand</strong><br />
2 Health Services Research<br />
Centre, Victoria University,<br />
Wellington<br />
3 Massey University, Albany,<br />
Auckland<br />
4 Maria’s HealthCare<br />
Pharmacy, Apia, Samoa<br />
J PRIMARY HEALTH CARE<br />
2009;1(1):30–35.<br />
CORRESPONDENCE TO:<br />
Pauline Norris<br />
School <strong>of</strong> Pharmacy,<br />
University <strong>of</strong> Otago,<br />
Box 913, Dunedin<br />
pauline.norris@otago.ac.nz<br />
Understanding and use <strong>of</strong> antibiotics<br />
amongst Samoan people in <strong>New</strong> <strong>Zealand</strong><br />
Pauline Norris MA, PhD; 1 Marianna Churchward; 2 Fuafiva Fa’alau; 3 Cecilia Va’ai 4<br />
ABSTRACT<br />
INTRODUCTION: Use <strong>of</strong> antibiotics is high in Samoa and this may affect the expectations and patterns<br />
<strong>of</strong> antibiotic use <strong>of</strong> Samoans in <strong>New</strong> <strong>Zealand</strong>.<br />
AIM: This study examined the understanding and reported use <strong>of</strong> antibiotics amongst Samoans in <strong>New</strong><br />
<strong>Zealand</strong>.<br />
METHODS: In-depth interviews were held with 13 Samoans in <strong>New</strong> <strong>Zealand</strong>. <strong>The</strong>se interviews were<br />
analysed and used to develop a questionnaire that was administered to 112 Samoans attending health<br />
care facilities in <strong>New</strong> <strong>Zealand</strong>.<br />
RESULTS: Many participants had little understanding <strong>of</strong> antibiotics. Less than 2% identified the correct<br />
purpose for antibiotics, and 66% thought they were used to relieve pain. Respondents regarded a wide<br />
range <strong>of</strong> medicines (including some which they regularly took) as antibiotics. <strong>The</strong>y frequently attributed<br />
colds and flu to environmental conditions (96%), and regarded antibiotics as a useful treatment for them<br />
(81%). <strong>The</strong>y reported stopping taking antibiotics before finishing the course. Very few (8%) were aware <strong>of</strong><br />
antibiotic resistance.<br />
DISCUSSION: Health care practitioners cannot assume that patients share a Western scientific understanding<br />
<strong>of</strong> which illnesses are caused by microbes, or what antibiotics are or do. People may have<br />
significant confusion about the medicines they take. Samoans, whether they are born in <strong>New</strong> <strong>Zealand</strong> or<br />
not, may hold traditional Samoan views about health and illness.<br />
KEyWORDS: Antibiotics, lay knowledge, URTI (upper respiratory tract infections), Samoa, <strong>New</strong> <strong>Zealand</strong><br />
Introduction<br />
Antibiotic resistance is a serious and growing<br />
problem. 1-3 This is due to high overall use, but<br />
sub-optimal patterns <strong>of</strong> use, such as incomplete<br />
treatment courses, may also be important. 2<br />
<strong>The</strong>re are approximately 130 000 Samoans in<br />
<strong>New</strong> <strong>Zealand</strong>, <strong>of</strong> whom 60% were born in <strong>New</strong><br />
<strong>Zealand</strong>. 4 Pacific people in general, <strong>of</strong> whom 49%<br />
are Samoan, have shorter life expectancy, poorer<br />
health, higher rates <strong>of</strong> diabetes, higher mortality<br />
rates from cardiovascular disease and stroke than<br />
the general population. 5 <strong>The</strong>re are several reasons<br />
to assume that antibiotic use might be high<br />
amongst Samoans in <strong>New</strong> <strong>Zealand</strong>. Pacific people<br />
have lower socioeconomic and health status and<br />
higher rates <strong>of</strong> infectious diseases than other<br />
<strong>New</strong> <strong>Zealand</strong>ers. 6 In the general population lower<br />
socioeconomic status is linked to higher rates <strong>of</strong><br />
infectious diseases 7,8 and higher use <strong>of</strong> antibiotics.<br />
9 In Samoa the use <strong>of</strong> antibiotics is high, and<br />
antibiotics are available without prescription from<br />
pharmacies. 10 This may affect Samoan people’s expectations<br />
<strong>of</strong> treatment and patterns <strong>of</strong> antibiotic<br />
use in <strong>New</strong> <strong>Zealand</strong>. One clone <strong>of</strong> community-acquired<br />
methicillin-resistant Staphloccocus aureus<br />
has been labelled Western Samoan Phage Pattern<br />
(WSPP) MRSA, because its prevalence amongst<br />
Samoans and other Pacific Islanders suggests that<br />
it may have emerged in Samoa. 1 In addition, the<br />
prevalence <strong>of</strong> traditional beliefs about health<br />
and illness may mean that Samoan people use<br />
antibiotics in ways that are not consistent with<br />
Western scientific beliefs.<br />
30 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Misunderstandings about antibiotics are common<br />
in a wide range <strong>of</strong> populations studied. 12-15 This<br />
study aimed to investigate understandings and use<br />
<strong>of</strong> antibiotics amongst Samoans in <strong>New</strong> <strong>Zealand</strong>.<br />
It did not aim to compare the level <strong>of</strong> knowledge<br />
<strong>of</strong> Samoans and non-Samoans in <strong>New</strong> <strong>Zealand</strong>,<br />
nor does it assume that Samoans have lower levels<br />
<strong>of</strong> knowledge than other <strong>New</strong> <strong>Zealand</strong>ers.<br />
Methods<br />
In-depth interviews were held with 13 Samoans<br />
in <strong>New</strong> <strong>Zealand</strong> in 2005–2006. <strong>The</strong>se interviews<br />
were audio-taped, transcribed, and those<br />
in Samoan were translated into English. <strong>The</strong>y<br />
were coded and analysed using nVivo. <strong>The</strong>mes<br />
were developed from the aims <strong>of</strong> the project,<br />
the results <strong>of</strong> previous studies, and inductively<br />
from the interviews. Analysis was discussed<br />
amongst team members, and the material from<br />
the interviews was used to develop a questionnaire<br />
exploring knowledge and use <strong>of</strong> antibiotics.<br />
This questionnaire was administered to 112<br />
Samoans. All interviews (in-depth and questionnaire)<br />
were carried out by Samoan members <strong>of</strong><br />
the research team.<br />
Respondents for the in-depth interviews were<br />
identified through the researchers’ informal<br />
networks in Auckland and Wellington. Respondents<br />
for the questionnaire were identified<br />
through health services catering primarily to<br />
Pacific people in Auckland and Wellington. All<br />
Samoan patients using the clinic during the times<br />
when the researcher was present were invited to<br />
participate.<br />
Both in-depth interviews and the survey were<br />
carried out either in Samoan or English. <strong>The</strong> seven<br />
in-depth interviews in Samoan were translated<br />
into English. An identical questionnaire layout in<br />
Samoan and English was used, so that translation<br />
was not necessary for the questionnaire analysis.<br />
Ethical approval for the study was granted by<br />
Wellington and Auckland ethics committees<br />
(AKX/04/07/194). Informed consent was<br />
obtained from all participants. Information<br />
sheets and consent forms were provided in<br />
English or Samoan.<br />
WHAT GAP THIS FILLS<br />
What we already know: Many studies have shown gaps in public knowledge<br />
about antibiotics, but none have looked specifically at Samoans.<br />
What this study adds: Significant misunderstandings by Samoans living<br />
in <strong>New</strong> <strong>Zealand</strong> are common. Primary health care practitioners should not<br />
assume that patients share their understandings <strong>of</strong> antibiotics or microbial<br />
illness.<br />
Results<br />
Semi-structured interviews<br />
Most <strong>of</strong> the participants (11/13) were female<br />
and their ages ranged from 29 to 82 years <strong>of</strong><br />
age. Eight were born in Samoa, and five in <strong>New</strong><br />
<strong>Zealand</strong>. <strong>The</strong> semi-structured interviews revealed<br />
significant misunderstandings and lack <strong>of</strong> knowledge<br />
<strong>of</strong> antibiotics. Some respondents consistently<br />
confused antibiotics with painkillers, while<br />
others had inconsistent understandings, which<br />
changed throughout the interview.<br />
Interviewer: What do you think antibiotics do?<br />
Participant: <strong>The</strong>y do—they heal don’t they?<br />
<strong>The</strong>y’re supposed to relieve the pain I guess.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
<strong>The</strong>re were frequent confusions between antibiotics<br />
and other medication. One respondent,<br />
speaking <strong>of</strong> her nephew with epilepsy:<br />
Interviewer: Do you remember what medication<br />
he was on?<br />
Participant: He was definitely on some sort <strong>of</strong><br />
antibiotics but I have no idea what they were, I<br />
will have to ask my sister. I think it was two lots<br />
<strong>of</strong> different ones.<br />
Antibiotics were frequently confused with paracetamol<br />
and other analgesics. However, during<br />
the interviews they were also confused with allopurinol,<br />
epilepsy medication, topical NSAIDs,<br />
asthma inhalers, Indocid, fluoxetine, and a<br />
urinary alkaliniser. This sort <strong>of</strong> confusion was<br />
common even in respondents who told us that<br />
antibiotics were medicines to kill bacteria.<br />
MIXED METHOD RESEARCH<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 31
ORIGINAL SCIENTIFIC PAPERS<br />
MIXED METHOD RESEARCH<br />
Figure 1. What do antibiotics do?<br />
Many respondents reported use <strong>of</strong> incomplete<br />
courses, and storing <strong>of</strong> leftover antibiotics.<br />
Respondent: I think the way my family uses<br />
antibiotics is typical.<br />
Interviewer: What do you mean by that?<br />
Respondent: <strong>The</strong>y use it and when they feel<br />
better they stop using them. And they will keep<br />
them for later use.<br />
A small number <strong>of</strong> respondents reported receiving<br />
advice about appropriate use <strong>of</strong> antibiotics<br />
from health pr<strong>of</strong>essionals, which sometimes appeared<br />
to have changed their attitudes or behaviour.<br />
Some perceived that doctors in <strong>New</strong> <strong>Zealand</strong><br />
had become less likely to prescribe antibiotics:<br />
Interviewer: So who suggested that you take<br />
these…who decided that you should use them?<br />
Respondent: Usually the doctor, but that was in<br />
the time when they gave them out pretty freely,<br />
nowadays they’re not as generous with antibiotics<br />
I find…you even have to ask ‘could we have an<br />
antibiotic?’ and they would generally say ‘no, let<br />
your own system fight it’ and they will tell you<br />
to go home and drink lots <strong>of</strong> water and fluids.<br />
Respondents could select more than one option. If they selected both a correct option<br />
(‘kill bacteria’) and an incorrect one such as ‘relieve pain’, their answer was counted as<br />
incorrect. Respondents who chose the answer ‘kill bacteria’ with no other option, or ‘kill<br />
bacteria’ and ‘heal illnesses’ with no other option were classified as correct.<br />
A minority <strong>of</strong> respondents remembered being<br />
told to complete courses <strong>of</strong> antibiotics, and one<br />
knew from reading medicine labels:<br />
Respondent: I remember when I was given antibiotics<br />
I make sure I take them all before.<br />
Interviewer: Do you?<br />
Respondent: It always says on the thing that you<br />
make sure you take all your antibiotic until you<br />
finish it <strong>of</strong>f, yeah.<br />
Interviewer: And you do?<br />
Respondent: Yeah.<br />
Survey<br />
One hundred and twelve people completed the<br />
questionnaire; an approximate response rate<br />
<strong>of</strong> 84%. Fifty-three percent <strong>of</strong> the sample were<br />
female. Nine percent were under 20 years old,<br />
31% were between 20 and 40 years old, 36% were<br />
40 and 60, and 24% were over 60 years old. Most<br />
(83%) were born in Samoa, with the others born in<br />
<strong>New</strong> <strong>Zealand</strong> (17%). For those born in Samoa, the<br />
average length <strong>of</strong> residence in <strong>New</strong> <strong>Zealand</strong> was<br />
14 years, with a range from six months to 40 years.<br />
Of those born in <strong>New</strong> <strong>Zealand</strong>, only one had lived<br />
in Samoa for a short time. <strong>The</strong> others had either<br />
not been to Samoa, or only been for holidays.<br />
Only two <strong>of</strong> the 112 people interviewed gave a<br />
correct answer to the question ‘What do antibiotics<br />
do?’ Responses were categorised as correct<br />
if they were ‘kill bacteria’ or ‘kill bacteria’ and<br />
‘heal illness’, but no other responses. Although<br />
half the sample (49%) correctly stated that antibiotics<br />
kill bacteria, this was a less popular answer<br />
than ‘kill viruses’ (65%), ‘relieve pain’ (66%), and<br />
‘strengthen the immune system’ (54%). (Figure 1)<br />
Just over half the sample (54%) correctly identified<br />
antibiotics from a list <strong>of</strong> medicines. Amoxycillin<br />
was correctly identified as an antibiotic<br />
by 81% <strong>of</strong> the sample, and Augmentin by 80%.<br />
However, the other medicines listed: ‘metformin<br />
for diabetes’, ‘allopurinol for gout’, paracetamol,<br />
coldral/coldrex, asthma inhalers, were also identified<br />
as antibiotics (Figure 2).<br />
32 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Colds were more commonly attributed to environmental<br />
rather than microbial causes (96% vs 42%).<br />
Environmental causes were changes in the weather<br />
(92% <strong>of</strong> respondents), dust (57%) and getting cold<br />
(50%). Thirteen (20%) <strong>of</strong> those who thought that<br />
dust caused colds were born in <strong>New</strong> <strong>Zealand</strong>.<br />
Respondents were asked, ‘If you had a cold/<br />
fulu* for three days, with coughing, heavy nose,<br />
and headache, what would you do?’ Almost all<br />
respondents (99%) said they would see a doctor<br />
or nurse, and over half reported that they would<br />
take medicines (46%). Panadol or paracetamol<br />
was by far the most common medicine reported<br />
(51/56 medicines listed). Hot drinks (35%), rest<br />
(28%), and traditional Samoan f<strong>of</strong>o (29%) were<br />
also commonly reported responses.<br />
Participants were asked what medicines they had<br />
taken in the last month, and what for. Sixteen<br />
people identified antibiotics (amoxicillin, augmentin,<br />
doxycycline, penicillin) which they reported<br />
that they had taken for flu, lung infections,<br />
infected chest, sore throat, throat infections, fissures,<br />
‘bad flu’, knee injury, chest pain/infection,<br />
eczema, boils, and tonsillitis.<br />
Of the two people who reported taking allopurinol<br />
in the last month, one had earlier indicated<br />
that allopurinol was an antibiotic. Of the 11<br />
people who reported taking metformin, eight had<br />
earlier indicated that metformin was an antibiotic.<br />
All but one <strong>of</strong> these people gave very wide interpretations<br />
<strong>of</strong> what antibiotics did, saying that they<br />
relieved pain, strengthened the immune system,<br />
killed viruses and bacteria, and healed illness.<br />
Of the 57 people who reported taking paracetamol<br />
in the last month, three thought this was an<br />
antibiotic. None <strong>of</strong> these three thought antibiotics<br />
relieved pain. Two thought they killed bacteria,<br />
and two thought they killed viruses. Two took the<br />
paracetamol for flu and one for a headache.<br />
Eighty-one percent <strong>of</strong> the sample believed antibiotics<br />
were useful for colds and flu, and four<br />
percent were not sure. Antibiotics were believed<br />
to prevent colds and flu getting worse (68%), help<br />
people get better sooner (62%), relieve symptoms<br />
(57%), and prevent serious illness (35%).<br />
* ‘Fulu’ is Samoan for cold or flu.<br />
Figure 2. Which medicines are antibiotics?<br />
Forty-six percent <strong>of</strong> people said they would stop<br />
taking antibiotics when they got better (rather<br />
than when the course was finished). When asked<br />
what they would do with leftover antibiotics,<br />
54% said they would keep them, 46% said they<br />
would throw them out, and 3% said they would<br />
give them to someone else. No one said they<br />
would return them to a pharmacy.<br />
When asked if antibiotics have any bad effects,<br />
half <strong>of</strong> the sample were unsure, and 39% thought<br />
they did. <strong>The</strong> ‘bad effects’ identified were allergy<br />
(34% <strong>of</strong> the whole sample), diarrhoea (31%),<br />
thrush (14%), damaging the immune system<br />
(13%), germs getting used to antibiotics (8%),<br />
‘people start to dependent on them’ (3%), inability<br />
to drink alcohol (1%), and overdose (1%).<br />
Discussion<br />
ORIGINAL SCIENTIFIC PAPERS<br />
Respondents could select more than one option. Respondents’ answers were classified<br />
as correct if they chose ‘Amoxil/amoxycillin’ with no other option, or ‘Augmentin’ with<br />
no other option, or ‘Amoxil/amoxycillin’ and ‘Augmentin’ with no other option. If, for<br />
example, a respondent said panadol and amoxil were antibiotics, their answer was<br />
counted as ‘incorrect’.<br />
Both the in-depth interviews and the questionnaire<br />
suggest that many Samoan people have<br />
little understanding <strong>of</strong> antibiotics, and regard<br />
a wide range <strong>of</strong> medicines as antibiotics (even<br />
medicines they have personal experience <strong>of</strong>). <strong>The</strong><br />
responses suggest that Samoan people frequently<br />
MIXED METHOD RESEARCH<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 33
ORIGINAL SCIENTIFIC PAPERS<br />
MIXED METHOD RESEARCH<br />
attribute colds and flu to environmental conditions,<br />
rather than microbes. <strong>The</strong>y regard antibiotics<br />
as a useful treatment for colds and flu,<br />
frequently stop taking them before finishing<br />
the course, and very few are aware <strong>of</strong> antibiotic<br />
resistance. Ironically, stopping taking antibiotics<br />
‘prematurely’ for those with a common cold will<br />
probably reduce resistance while such behaviour<br />
could be harmful for diseases with serious consequences<br />
such as streptococcal tonsillitis (and its<br />
relation to rheumatic fever).<br />
<strong>The</strong> survey involved a small sample <strong>of</strong> people<br />
who were visiting health care practitioners. <strong>The</strong><br />
interview process was very time-consuming and<br />
so the sample size <strong>of</strong> 112 was decided by practical<br />
constraints rather than a power calculation. Thus<br />
caution should be used when extrapolating to the<br />
general Samoan population, and further research<br />
is needed. However, this is the first information<br />
available on Samoan knowledge and understanding<br />
<strong>of</strong> antibiotics. <strong>The</strong>re were some difficulties<br />
in translating the terms ‘bacteria’ and ‘virus’ into<br />
It cannot be assumed that patients share Western<br />
scientific understandings about which illnesses are<br />
caused by microbes, which illnesses are viral, and<br />
which are bacterial, or what antibiotics are or do<br />
Samoan, so caution should also be used in interpreting<br />
results concerning these.<br />
Studies overseas have also found misconceptions<br />
and lack <strong>of</strong> knowledge about antibiotics. For example,<br />
8% <strong>of</strong> people interviewed in 1976 thought<br />
aspirin was an antibiotic 12 and only half <strong>of</strong> the<br />
respondents in another knew that codeine was<br />
not an antibiotic and some thought Robitussin<br />
was an antibiotic. 13<br />
<strong>The</strong> interviews reported here are part <strong>of</strong> a larger<br />
study looking at knowledge and use <strong>of</strong> antibiotics<br />
amongst Samoan people in Samoa and <strong>New</strong><br />
<strong>Zealand</strong>. In Samoa itself, participants reported<br />
routine use <strong>of</strong> antibiotics for colds and flu. This<br />
seems to be encouraged by prescribing patterns.<br />
Antibiotics are also available without prescription<br />
from pharmacies. 10<br />
<strong>The</strong> belief that exposure to cold and changes in<br />
weather can cause colds may also be common in<br />
Western cultures. 16 However, to our knowledge,<br />
the belief that dust causes colds and flu has not<br />
been reported elsewhere, although it may have<br />
been part <strong>of</strong> medical orthodoxy some time ago. 17<br />
In this study, Samoans born in <strong>New</strong> <strong>Zealand</strong><br />
were just as likely to report this belief as those<br />
born in Samoa. This suggests that health care<br />
pr<strong>of</strong>essionals cannot assume that <strong>New</strong> <strong>Zealand</strong>–<br />
born Samoans completely share Western ideas<br />
about health.<br />
A previous study found that 42% <strong>of</strong> the population<br />
<strong>of</strong> a <strong>New</strong> <strong>Zealand</strong> town had taken antibiotics<br />
in the last year. 9 In this study, 14% reported<br />
taking antibiotics in the last month. It is difficult<br />
to compare these numbers because the survey<br />
was administered with a sample <strong>of</strong> those visiting<br />
health care providers, rather than a general<br />
population sample.<br />
Curry et al. found that most people taking<br />
antibiotics for URTI believe that they help<br />
symptoms (85%) and shorten the course <strong>of</strong> URTI<br />
(80%). 14 Respondents in our study <strong>of</strong> Samoan<br />
people also commonly believe that antibiotics<br />
have these effects, and they also believe antibiotics<br />
prevent URTIs getting worse, and prevent<br />
serious illness.<br />
Respondents in our study <strong>of</strong> Samoan people<br />
reported a very high level <strong>of</strong> use <strong>of</strong> health care<br />
providers for colds/flu (99% said they would see<br />
a doctor or nurse for a cold lasting three days). In<br />
contrast, Curry et al. reported that only 15% <strong>of</strong><br />
their general population–based sample said they<br />
would usually see a doctor about an URTI. 14<br />
This study provides several messages for health<br />
care pr<strong>of</strong>essionals. It cannot be assumed that<br />
patients share Western scientific understandings<br />
about which illnesses are caused by microbes,<br />
which illnesses are viral, and which are bacterial,<br />
or what antibiotics are or do. People may have<br />
significant confusions about what the medicines<br />
they take actually do. Even Samoans who are<br />
34 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
orn in <strong>New</strong> <strong>Zealand</strong> may hold traditional Samoan<br />
views about health and illness, rather than<br />
Western ones. However there is some evidence<br />
that explanations about appropriate use <strong>of</strong> antibiotics<br />
given by individual doctors and pharmacists<br />
make a difference.<br />
While the results show the need for targeted<br />
health promotion about antibiotics in the Samoan<br />
community, they also suggest that caution is<br />
needed. Because many Samoan people were unable<br />
to distinguish antibiotics from other medicines,<br />
there is a risk that they may reduce use <strong>of</strong><br />
other essential medicines, such as metformin if<br />
they are warned about the dangers <strong>of</strong> antibiotic<br />
use. Messages about appropriate (non-antibiotic)<br />
management <strong>of</strong> colds and flu, building on existing<br />
culturally-based practices, would be safest<br />
strategy in this context.<br />
References<br />
1. Standing Medical Advisory Committee Sub-Group on Antimicrobial<br />
Resistance. <strong>The</strong> Path <strong>of</strong> Least Resistance. Department<br />
<strong>of</strong> Health (UK); 1998.<br />
2. World Health Organization. WHO Global Strategy for Containment<br />
<strong>of</strong> Antimicrobial Resistance. WHO; 2001.<br />
3. Ellis-Pegler R. Editorial: Antimicrobial resistance—can we,<br />
should we do anything about it? NZ Med J 1999;112:249–351.<br />
4. Ministry <strong>of</strong> Health NZ. Tagata Pasifika—Pacific Health. <strong>New</strong><br />
<strong>Zealand</strong>: Ministry <strong>of</strong> Health; 2007.<br />
5. Ministry <strong>of</strong> Health NZ. Pacific People’s Health. <strong>New</strong> <strong>Zealand</strong>:<br />
Ministry <strong>of</strong> Health; 2007.<br />
6. Ministry <strong>of</strong> Health NZ. Pacific Health: Pacific People’s Health.<br />
7. Davey Smith G, Neaton J, Wentworth D, Stamler R, Stamler<br />
J. Socioeconomic differentials in mortality risk among men<br />
screened for the Multiple Risk Factor Intervention Trial:<br />
Part 1—results for 300,685 white men. Am J Public Health<br />
1996;86:486–96.<br />
8. Salmond C, Crampton P. Deprivation and health. In: Howden-<br />
Chapman P, Tobias M, editors. Social inequalities in health:<br />
<strong>New</strong> <strong>Zealand</strong> 1999. Wellington: Ministry <strong>of</strong> Health; 2000.<br />
9. Norris P, Ecke D, Becket G. Demographic Variation in the use<br />
<strong>of</strong> antibiotics in a <strong>New</strong> <strong>Zealand</strong> town. NZ Med J 2005;118.<br />
10. Norris P, Nguyen H. Consumption <strong>of</strong> antibiotics in a small Pacific<br />
Island nation: Samoa. Pharmacy Practice 2007. 5: http://<br />
www.pharmacypractice.org/vol05/01/toc.htm.<br />
11. Smith S, Cook G. A decade <strong>of</strong> community MRSA in <strong>New</strong><br />
<strong>Zealand</strong>. Epidemiol Infect 2005;1–6.<br />
12. Chandler D, Dougdale A. What do patients know about antibiotics?<br />
Lancet 1976;2:422.<br />
13. Hong J, Philbrick J, Schorling J. Treatment <strong>of</strong> upper respiratory<br />
infections: do patients really want antibiotics? Am J Med<br />
1999;107:511–515.<br />
14. Curry M, Sung L, Arroll B, Goodyear-Smith F, Kerse N, Norris<br />
P. Public views and use <strong>of</strong> antibiotics for the common cold<br />
before and after an education campaign in <strong>New</strong> <strong>Zealand</strong>. NZ<br />
Med J 2006;119.<br />
15. Eng JV, Marcus R, Hadler JL, Imh<strong>of</strong>f B, Vugia DJ, Cieslak PR,<br />
Zell E, Deneen V, McCombs KG, Zansky SM, Hawkins MA,<br />
Besser RE. Consumer attitudes and use <strong>of</strong> antibiotics. Emerg<br />
Infect Dis 2003;9:1128–1135.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
16. Lee GM, Friedman JF, Ross-Degnan D, Hibberd PL,Goldmann<br />
DA. Misconceptions about colds and predictors <strong>of</strong> health<br />
service utilization 10.1542/peds.111.2.231. Pediatrics 2003;<br />
111:231–236.<br />
17. Neuwelt L. How to avoid colds. Am J Nurs 1918;18:371–373.<br />
MIXED METHOD RESEARCH<br />
ACKNOWLEDGEMENTS<br />
We wish to thank the<br />
Health Research Council <strong>of</strong><br />
<strong>New</strong> <strong>Zealand</strong> for funding<br />
the study, the health care<br />
providers who allowed us<br />
to interview their patients,<br />
and the participants.<br />
COMPETING INTERESTS<br />
None declared.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 35
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
1 Section <strong>of</strong> Epidemiology<br />
& Biostatistics, School <strong>of</strong><br />
Population Health, Faculty <strong>of</strong><br />
Medical and Health Science,<br />
<strong>The</strong> University <strong>of</strong> Auckland,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
2 Department <strong>of</strong> <strong>General</strong><br />
Practice and Primary Health<br />
Care, School <strong>of</strong> Population<br />
Health, Faculty <strong>of</strong> Medical<br />
and Health Science, <strong>The</strong><br />
University <strong>of</strong> Auckland,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
3 School <strong>of</strong> Rehabilitation and<br />
Occupation Studies, AUT<br />
University, Auckland<br />
J PRIMARY HEALTH CARE<br />
2009;1(1):36–41.<br />
CORRESPONDENCE TO:<br />
Gillian Robb<br />
Section <strong>of</strong> Epidemiology<br />
& Biostatistics, School<br />
<strong>of</strong> Population Health,<br />
University <strong>of</strong> Auckland<br />
Private Bag 92019,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
g.robb@auckland.ac.nz<br />
Summary <strong>of</strong> an evidence-based guideline<br />
on s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and related<br />
disorders—Part 1: Assessment<br />
Gillian Robb MPH (Hons), Dip Physiotherapy, Dip Ergonomics; 1 Bruce Arroll MBChB, PhD, FRNZCGP; 2 Duncan<br />
Reid MHSc (Hons), PGD (Manip Physiotherapy), MNZCP; 3 Felicity Goodyear-Smith MBChB, MGP, FRNZCGP 2<br />
ABSTRACT<br />
AIM: To provide a succinct summary <strong>of</strong> the diagnosis <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> injuries to the shoulder for primary<br />
health care practitioners based on the <strong>New</strong> <strong>Zealand</strong> guideline.<br />
METHODS: A multidisciplinary team developed the guideline by critically appraising and grading<br />
retrieved literature using the Graphic Appraisal Tool for Epidemiology (GATE). Recommendations were<br />
derived from resulting evidence tables.<br />
RESULTS: Diagnostic ultrasound is a valid tool for the diagnosis <strong>of</strong> a full thickness rotator cuff tear. If<br />
a significant tear is suspected, referral for diagnostic ultrasound is recommended. <strong>The</strong>re is a paucity <strong>of</strong><br />
evidence for the diagnosis <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and most recommendations are based on the<br />
consensus <strong>of</strong> the guideline team.<br />
CONCLUSION: Assessment relies on thorough history-taking and physician examination with appropriate<br />
referral where there is evidence <strong>of</strong> serious damage or the diagnosis remains unclear.<br />
KEyWORDS: Shoulder, shoulder pain, diagnosis, s<strong>of</strong>t t<strong>issue</strong> injuries<br />
Introduction<br />
S<strong>of</strong>t t<strong>issue</strong> shoulder injuries rank within the top<br />
three injury sites for nearly all major sport and<br />
recreational activities. 1 Not only do they represent<br />
a significant cost to the Accident Compensation<br />
Corporation (ACC), if poorly managed they can<br />
result in significant disability and loss <strong>of</strong> quality<br />
<strong>of</strong> life. In 2003 ACC commissioned a guideline<br />
for the diagnosis and management <strong>of</strong> common<br />
s<strong>of</strong>t t<strong>issue</strong> shoulder injuries to reduce identified<br />
variation in diagnosis and management and to<br />
improve outcomes for claimants. 2<br />
<strong>The</strong> diagnosis and management <strong>of</strong> shoulder<br />
injuries is one <strong>of</strong> the most challenging areas <strong>of</strong><br />
musculoskeletal medicine. Pathologies and their<br />
clinical manifestations vary widely from person<br />
to person and pathologies <strong>of</strong>ten co-exist, further<br />
compounding the diagnostic complexity.<br />
This paper is the first <strong>of</strong> a two-part series which<br />
summarises the evidence for the diagnosis <strong>of</strong> s<strong>of</strong>t<br />
t<strong>issue</strong> shoulder injuries based on the evidencebased<br />
guideline <strong>The</strong> diagnosis and management <strong>of</strong><br />
s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and related disorders. 2<br />
This guideline was developed in <strong>New</strong> <strong>Zealand</strong><br />
(NZ), led by Effective Practice, Informatics &<br />
Quality improvement (EPIQ), University <strong>of</strong><br />
Auckland under the auspices <strong>of</strong> the <strong>New</strong> <strong>Zealand</strong><br />
Guidelines Group (NZGG). <strong>The</strong> guideline was<br />
endorsed by the <strong>Royal</strong> <strong>New</strong> <strong>Zealand</strong> <strong>College</strong> <strong>of</strong><br />
<strong>General</strong> Practitioners, the NZ Orthopaedic Asso-<br />
36 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
ciation, the NZ Society <strong>of</strong> Physiotherapists Inc.,<br />
the NZ Association <strong>of</strong> Musculoskeletal Medicine,<br />
Sports Medicine NZ and the <strong>Royal</strong> Australasian<br />
and <strong>New</strong> <strong>Zealand</strong> <strong>College</strong> <strong>of</strong> Radiologists.<br />
<strong>The</strong> aim <strong>of</strong> this paper is to provide a succinct<br />
summary <strong>of</strong> the assessment <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> injuries<br />
to the shoulder in a form that is readily accessible<br />
to primary health care practitioners.<br />
Method<br />
<strong>The</strong> target group for the guideline is primary<br />
care practitioners. In NZ this group includes<br />
primary care medical practitioners, physiotherapists<br />
and osteopaths who are able to assess s<strong>of</strong>t<br />
t<strong>issue</strong> injuries <strong>of</strong> the shoulder and decide initial<br />
management.<br />
A broad-based multidisciplinary team (orthopaedic<br />
surgery, general practice, musculoskeletal<br />
radiology, musculoskeletal medicine, sports<br />
medicine, emergency medicine, physiotherapy,<br />
osteopathy) was convened in 2003, including<br />
nominated pr<strong>of</strong>essionals and representatives for<br />
Maori, Pacific people and consumers.<br />
<strong>The</strong> team met on two occasions over a 12-month<br />
period. <strong>The</strong>re were numerous consultations<br />
between members <strong>of</strong> the group throughout the<br />
guideline process, including several additional<br />
small group meetings to discuss various aspects<br />
<strong>of</strong> the guideline.<br />
This guideline summary addresses the diagnosis<br />
and referral <strong>of</strong> adults with the following<br />
shoulder injuries. Adolescents were also included<br />
for shoulder instabilities given that dislocation<br />
and recurrent dislocation are more common in<br />
this age group. Five pathological groupings were<br />
considered as reflective <strong>of</strong> the main s<strong>of</strong>t t<strong>issue</strong><br />
disorders seen in primary care. <strong>The</strong>se were:<br />
1. Rotator cuff disorders (including<br />
impingement, subacromial bursitis, tendinosis,<br />
painful arc syndrome, partial, full thickness<br />
and massive tears <strong>of</strong> the rotator cuff, long<br />
head <strong>of</strong> biceps rupture and calcific tendonitis)<br />
2. Frozen shoulder (also known as adhesive<br />
capsulitis)<br />
WHAT GAP THIS FILLS<br />
What we already know: Shoulder injuries are both common and difficult<br />
to diagnose.<br />
What this study adds: <strong>The</strong> evidence base to diagnosis <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong><br />
injuries to the shoulder is limited. This review <strong>of</strong>fers recommendations largely<br />
based on expert consensus. Assessment relies on thorough history-taking<br />
and physician examination, with appropriate referral where there is evidence<br />
<strong>of</strong> serious damage or the diagnosis remains unclear.<br />
3. Glenohumeral instabilities (acute and<br />
recurrent dislocation, labral injuries and other<br />
instabilities)<br />
4. Acromioclavicular (AC) joint injuries<br />
(including stress osteolysis, osteoarthritis and<br />
dislocation)<br />
5. Sternoclavicular (SC) joint injuries (including<br />
sprains, dislocation and arthritis and related<br />
conditions).<br />
<strong>The</strong> guideline specifically excluded fractures, inflammatory<br />
conditions, degenerative conditions,<br />
endocrinological and neurological conditions,<br />
hemiplegic shoulder and chronic shoulder pain<br />
including occupational overuse disorders.<br />
<strong>The</strong> following diagnostic and referral questions<br />
were considered by the team:<br />
• What aspects <strong>of</strong> the history are<br />
diagnostic—e.g. mechanisms <strong>of</strong> injury;<br />
a sensation <strong>of</strong> ‘popping out’?<br />
• What symptoms are diagnostic, e.g.<br />
location <strong>of</strong> pain; dead arm?<br />
• What aspects <strong>of</strong> the clinical examination /<br />
specific tests are valid and reliable for the<br />
diagnosis <strong>of</strong> the included shoulder conditions?<br />
• What are the red flags?<br />
• What imaging is appropriate to<br />
use in making the diagnosis?<br />
• What are the appropriate plain films to use<br />
in the diagnosis <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> injuries?<br />
• What is the place <strong>of</strong> diagnostic ultrasound?<br />
• What are the indications for referral<br />
for further evaluation?<br />
For each question a comprehensive literature<br />
search was undertaken in all major electronic<br />
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 37
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
data bases (Medline, CINAHL, EMBASE,<br />
AMED, SPORTdiscus and Current Contents).<br />
Relevant Internet sites were searched, including<br />
PEDro, NHS clinical trials, Health Technology<br />
Assessments for NHS, Bandolier and National<br />
Guideline Clearing House. Reference lists <strong>of</strong><br />
included studies were checked for additional<br />
studies. Only published studies in the English<br />
language were considered for inclusion.<br />
Quality was assessed using the Generic Appraisal<br />
Tool for Epidemiology (GATE) available at: http://<br />
www.epiq.co.nz (modified since this guideline<br />
was developed).<br />
Diagnostic studies were included only if they had<br />
at least 35 or more participants which represented<br />
an appropriate spectrum or defined clinical group,<br />
included blind independent assessment <strong>of</strong> the<br />
new test and reference standard and compared the<br />
reference test with the new test in at least 90% <strong>of</strong><br />
people.<br />
Evidence from the relevant studies was summarised<br />
into evidence tables (http://www.nzgg.<br />
org.nz/guidelines/0083/040610_Final_Guideline_methodology_and_evidence_tables_<br />
dia%E2%80%A6.pdf ). Recommendations were developed<br />
using the SIGN ‘Considered Judgement’<br />
process. (SIGN Guideline development process:<br />
http://www.sign.ac.uk/guidelines/fulltext/50/<br />
compjudgement.html).<br />
Table 1. Evidence summary—diagnosis<br />
Evidence summary<br />
Grading is based on the strength <strong>of</strong> the evidence<br />
and does not indicate the relative importance <strong>of</strong><br />
the recommendations.<br />
Results<br />
<strong>The</strong>re is a paucity <strong>of</strong> evidence for the diagnosis <strong>of</strong><br />
s<strong>of</strong>t t<strong>issue</strong> shoulder injuries. Recommendations<br />
have therefore been based primarily on the<br />
consensus <strong>of</strong> the guideline development team<br />
(Table 1).<br />
Routine x-rays and diagnostic ultrasound are<br />
the imaging techniques available to NZ primary<br />
health care practitioners. Referral to a specialist is<br />
required for other diagnostic imaging procedures<br />
including MRI and MR arthrography, which<br />
are the additional diagnostic imaging techniques<br />
most commonly used for s<strong>of</strong>t t<strong>issue</strong> injuries <strong>of</strong><br />
the shoulder. <strong>The</strong> evidence for these modalities<br />
has therefore not been included for this summary.<br />
‘A’ recommendation for the diagnosis<br />
<strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder injuries<br />
Diagnostic ultrasound<br />
If a significant rotator cuff tear is suspected, refer<br />
for diagnostic ultrasound. Diagnostic ultrasound<br />
should be undertaken by a radiologist with appropriate<br />
expertise using equipment with sufficient<br />
resolution.<br />
History <strong>The</strong>re is no evidence that any particular aspect <strong>of</strong> the history is both reliable and valid for<br />
the diagnosis <strong>of</strong> any shoulder injury.<br />
Physical examination <strong>The</strong>re is no evidence that any specific diagnostic test is both valid and reliable for the<br />
diagnosis <strong>of</strong> any s<strong>of</strong>t t<strong>issue</strong> shoulder injury.<br />
<strong>The</strong>re is no evidence that any particular combination <strong>of</strong> tests is useful in the diagnosis <strong>of</strong><br />
shoulder disorders.<br />
Radiography No validated clinical decisions rules were located for the use <strong>of</strong> plain radiography for s<strong>of</strong>t<br />
t<strong>issue</strong> shoulder injuries.<br />
Diagnostic ultrasound <strong>The</strong>re is good evidence that diagnostic ultrasound is a valid diagnostic tool in the diagnosis<br />
<strong>of</strong> full thickness rotator cuff tears in a secondary care setting with a likelihood ratio <strong>of</strong> 13.6<br />
(95% CI 9.13-18.95). 5<br />
Its ability to rule out rotator cuff disease is yet to be determined and there is no conclusive<br />
evidence for the validity <strong>of</strong> diagnostic ultrasound in the diagnosis <strong>of</strong> partial tears. 5<br />
<strong>The</strong>re is insufficient evidence to determine the validity <strong>of</strong> diagnostic ultrasound for rotator<br />
cuff tears in a primary care setting.<br />
38 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Consensus recommendations for the<br />
diagnosis <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder injuries<br />
1. Carry out a full clinical assessment, including<br />
a neurological examination if required<br />
<strong>The</strong> clinical manifestations <strong>of</strong> shoulder disorders<br />
are many and varied. A thorough clinical<br />
examination will help establish an accurate and<br />
definitive diagnosis (Table 2).<br />
2. Exclude red flags and other significant<br />
structural damage<br />
People with red flags and other significant structural<br />
damage require urgent referral to a specialist<br />
(Table 3).<br />
3. Screen for extrinsic causes <strong>of</strong> shoulder pain<br />
<strong>The</strong> site <strong>of</strong> pain may not be the source <strong>of</strong> the<br />
problem. Noting the onset, periodicity, site, character,<br />
radiation, associated symptoms and relieving<br />
and aggravating factors will alert the clinician<br />
to the severity <strong>of</strong> the disorder and the possible<br />
source <strong>of</strong> pain (Table 4). Provide appropriate treatment<br />
or refer to a specialist for further evaluation<br />
and management.<br />
4. Establish a provisional diagnosis<br />
<strong>The</strong> clinical diagnosis <strong>of</strong> shoulder disorders is<br />
difficult. <strong>The</strong>re is <strong>of</strong>ten overlap between commonly<br />
described conditions and variation in<br />
presentation <strong>of</strong> symptoms. <strong>The</strong> following key<br />
points should be kept in mind when diagnosing<br />
acute s<strong>of</strong>t t<strong>issue</strong> shoulder disorders:<br />
• Rotator cuff disorders:<br />
– Age >35 years<br />
– Upper arm pain/night pain<br />
– Painful arc<br />
– Limited active range <strong>of</strong> movement (ROM)<br />
– Full passive ROM<br />
– Possible weakness<br />
– +ve impingement sign.<br />
• Frozen shoulder<br />
– Gradual onset<br />
– Increasing severity <strong>of</strong> pain<br />
– Global limitation active and passive ROM<br />
– Possible diabetic<br />
Table 2. Clinical assessment <strong>of</strong> the shoulder<br />
History<br />
Inquiry Key Features Consider<br />
Age >35 year<br />
< 35 years<br />
Mechanism <strong>of</strong> injury Fall/direct trauma<br />
Fall onto point <strong>of</strong> shoulder<br />
Abduction/external<br />
rotation<br />
Head away (traction)<br />
Pain location/<br />
radiation<br />
Physical examination<br />
Above shoulder joint<br />
Upper arm/deltoid<br />
Anterior upper arm<br />
Below elbow (shooting)<br />
Night Pain<br />
Rotator cuff<br />
Instability<br />
Clavicle fracture<br />
AC joint<br />
Rotator cuff/dislocation<br />
Brachial Plexus<br />
AC Joint<br />
Rotator cuff<br />
Biceps tendonitis<br />
Nerve/neck<br />
Rotator cuff tendon<br />
Action Key features Consider<br />
Look Asymmetry/deformity<br />
Wasting<br />
Bruising<br />
Scars<br />
Feel SC joint/clavicle/AC joint<br />
Long head biceps<br />
Greater tuberosity<br />
Spine <strong>of</strong> scapula<br />
Test active ROM Limited active/full passive<br />
Painful arc<br />
Test passive ROM Limited active and passive<br />
Hypermobile/positive<br />
apprehension<br />
Test strength Weak abduction/wasting<br />
deltoid<br />
Weak abduction/external<br />
rotation<br />
Weak internal rotation<br />
Dislocation/fracture/AC joint<br />
dislocation<br />
Rotator cuff tear/nerve injury<br />
Dislocation/fracture<br />
Previous injury/surgery<br />
Local tenderness/prominence<br />
Local tenderness bicipital<br />
groove<br />
Local tenderness/fracture<br />
Local tenderness/fracture<br />
Rotator cuff disorder<br />
(impingement/tear)<br />
Rotator cuff disorder<br />
Frozen shoulder<br />
Instability<br />
Axillary nerve injury<br />
(dislocation)<br />
Rotator cuff tear<br />
Subscapularis/pectoralis<br />
major tear<br />
Special tests <strong>The</strong>re is no evidence that any specific test is both valid and<br />
reliable for the diagnosis <strong>of</strong> shoulder injuries.<br />
Neurological examination<br />
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
Level Motor Sensory Reflex<br />
C5 Deltoid/biceps Upper arm Biceps<br />
C6 Wrist extension Thumb Brachioradialis<br />
C7 Wrist extension/finger extension Middle finger Triceps<br />
C8 Finger grip Fifth finger None<br />
T1 Hand intrinsics Medial elbow None<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 39
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
• Anterior/recurrent dislocation<br />
– History <strong>of</strong> trauma<br />
– Pain and muscle spasm<br />
– Empty space below acromion<br />
– Humeral head anterior<br />
– Limited movement<br />
– Plus/minus +ve x-ray confirmation.<br />
• Instability disorders<br />
– Age 40 years<br />
Table 4. Possible extrinsic causes <strong>of</strong> shoulder pain<br />
Screen for the following:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Cervical spine disorders<br />
Nerve disorders<br />
Nerve root irritation<br />
Nerve compression/entrapment<br />
Brachial plexus injuries<br />
Neuralgic amyotrophy<br />
Inflammatory disorders<br />
Rheumatoid arthritis<br />
Polymyalgia rheumatica<br />
Complex regional pain syndrome<br />
My<strong>of</strong>ascial pain syndrome<br />
Scapulothoracic articulation<br />
Thoracic and rib injuries<br />
Visceral disorders<br />
Table 3. People requiring urgent referral for specialist<br />
evaluation<br />
Red flags (signs or symptoms which alert the clinician<br />
to serious pathology)<br />
Unexplained deformity or swelling<br />
• Consideration <strong>of</strong> surgery as management<br />
option (plain films are best requested by<br />
a specialist where surgery is being considered<br />
as a management option.<br />
Recommended views<br />
• AP glenoid fossa (Grashey View)<br />
• Either outlet or lateral scapular<br />
• Axial.<br />
Indications for diagnostic ultrasound<br />
Refer for diagnostic ultrasound where the clinical<br />
diagnosis is uncertain and it is important to<br />
exclude a significant rotator cuff tear.<br />
6. Refer for specialist referral where appropriate<br />
Appropriate and timely referral for a specialist<br />
evaluation is important where indicated to<br />
achieve optimal outcomes.<br />
Early referral is recommended for the following:<br />
• Two or more traumatic dislocations<br />
• Recurrent posterior/other instabilities<br />
• Where the diagnosis is in doubt.<br />
A number <strong>of</strong> specialist groups are competent to<br />
evaluate shoulder problems. <strong>The</strong> decision about to<br />
40 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Significant weakness not due to pain<br />
Suspected malignancy<br />
Significant unexplained sensory/motor deficit<br />
Pulmonary or vascular compromise<br />
Other significant structural damage<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Displaced or unstable fracture<br />
Failed attempt (x2) reduction <strong>of</strong> dislocated shoulder<br />
Massive tear <strong>of</strong> the rotator cuff (>5 cm)<br />
Isolated rupture <strong>of</strong> subscapularis or pectoralis major<br />
Severe dislocation GH, AC or SC joints<br />
Undiagnosed severe shoulder pain
whom to refer a patient will vary depending on<br />
the nature <strong>of</strong> the shoulder injury, the availability<br />
<strong>of</strong> specialist groups and the preferences <strong>of</strong> the<br />
patient and referring health pr<strong>of</strong>essional.<br />
Discussion<br />
While there is an abundance <strong>of</strong> diagnostic tests<br />
in clinical practice, this guideline indicates that<br />
no one test or combination <strong>of</strong> tests has been<br />
shown to accurately and reliability discriminate<br />
s<strong>of</strong>t t<strong>issue</strong> shoulder disorders. However diagnostic<br />
ultrasound is a modality available to primary<br />
care practitioners and this has been found to be<br />
useful in confirming a diagnosis <strong>of</strong> a full thickness<br />
rotator cuff tear, but less useful for partial<br />
thickness rotator cuff tears.<br />
Since the publication <strong>of</strong> the guideline two systematic<br />
reviews relevant to the diagnosis <strong>of</strong> key<br />
shoulder pathologies have been published. <strong>The</strong><br />
first investigated the diagnosis <strong>of</strong> instability and<br />
labral tears, 3 and the second the diagnosis <strong>of</strong> superior<br />
glenoid labral lesions only (SLAP lesions). 4<br />
<strong>The</strong> first review evaluated tests to distinguish<br />
between shoulder instability classified on the<br />
basis <strong>of</strong> degree (subluxation or dislocation) and<br />
direction (anterior, posterior, inferior or multidirectional)<br />
and labral lesions classified on the basis<br />
<strong>of</strong> location and type <strong>of</strong> tear. 3 This review evaluated<br />
four provocation and three laxity tests for<br />
instability <strong>of</strong> the shoulder, and 14 tests for labral<br />
tears. <strong>The</strong> evidence suggests that the relocation<br />
and anterior release tests are best for establishing<br />
the diagnosis <strong>of</strong> instability while the biceps load<br />
I and II test, the pain provocation test <strong>of</strong> Mimori<br />
and the internal rotation resistance strength<br />
tests are best for the diagnosis <strong>of</strong> a SLAP lesion.<br />
It should be noted that these studies were all<br />
located in specialised care centres and may have<br />
limited applicability to primary care. Limitations<br />
regarding methodology <strong>of</strong> individual studies were<br />
also noted.<br />
<strong>The</strong> second review evaluated nine tests for superior<br />
glenoid labral lesions (SLAP lesions) from<br />
11 studies. 4 <strong>The</strong> authors concluded that physical<br />
examination cannot provide a definitive diagnosis<br />
for SLAP lesions at this stage. Limited reliability<br />
due to the inherent difficulties in performing<br />
these tests and the heterogeneity <strong>of</strong> the patient<br />
populations studied contributed to the lack <strong>of</strong><br />
evidence for any one test or combination <strong>of</strong> tests<br />
to accurately diagnose SLAP lesions.<br />
Even with this additional evidence, the evidence<br />
base to diagnosis <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> injuries to the<br />
shoulder is limited. Assessment relies on thorough<br />
history-taking and physician examination,<br />
with appropriate referral where there is evidence<br />
<strong>of</strong> serious damage or the diagnosis remains<br />
unclear.<br />
References<br />
ORIGINAL SCIENTIFIC PAPERS<br />
1. Accident Compensation Corporation. Injury Statistics. ACC<br />
Injury Statistics 2006. Wellington: ACC; 2006.<br />
2. <strong>New</strong> <strong>Zealand</strong> Guideline Group. Diagnosis and management <strong>of</strong><br />
s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and related disorders: Best practice<br />
evidence-based guideline. Wellington: NZGG; 2004. p.86.<br />
3. Luime JJ, Verhagen AP, Miedema HS, Kuiper JI, Burdorf A,<br />
Verhaar JAN, et al. Does this patient have an instability <strong>of</strong> the<br />
shoulder or a labrum lesion? JAMA 2004;292(16):1989–99.<br />
4. Jones GL, Galluch DB. Clinical assessment <strong>of</strong> superior glenoid<br />
labral lesions: a systematic review. Clin Orthop Relat Res<br />
2007;455:45–51.<br />
5. Dinnes J, Loveman E, McIntyre LF, Waugh N. <strong>The</strong> effectiveness<br />
<strong>of</strong> diagnostic tests for the assessment <strong>of</strong> shoulder pain<br />
due to s<strong>of</strong>t t<strong>issue</strong> disorders: a systematic review. Health<br />
Technol Assess 2003;7(29).<br />
SYSTEMATIC REVIEW<br />
ACKNOWLEDGEMENTS<br />
Funded by the Accident<br />
Compensation Corporation<br />
<strong>New</strong> <strong>Zealand</strong><br />
COMPETING INTERESTS<br />
None declared<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 41
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
1 Section <strong>of</strong> Epidemiology<br />
& Biostatistics, School <strong>of</strong><br />
Population Health, Faculty <strong>of</strong><br />
Medical and Health Science,<br />
<strong>The</strong> University <strong>of</strong> Auckland,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
2 Department <strong>of</strong> <strong>General</strong><br />
Practice and Primary Health<br />
Care, School <strong>of</strong> Population<br />
Health, Faculty <strong>of</strong> Medical<br />
and Health Science, <strong>The</strong><br />
University <strong>of</strong> Auckland,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
3 School <strong>of</strong> Rehabilitation and<br />
Occupation Studies, AUT<br />
University, Auckland<br />
J PRIMARY HEALTH CARE<br />
2009;1(1):42–49.<br />
CORRESPONDENCE TO:<br />
Gillian Robb<br />
Section <strong>of</strong> Epidemiology<br />
& Biostatistics, School<br />
<strong>of</strong> Population Health,<br />
University <strong>of</strong> Auckland<br />
Private Bag 92019,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
g.robb@auckland.ac.nz<br />
Summary <strong>of</strong> an evidence-based guideline<br />
on s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and related<br />
disorders—Part 2: Management<br />
Gillian Robb MPH (Hons), Dip Physiotherapy, Dip Ergonomics; 1 Bruce Arroll MBChB, PhD, FRNZCGP; 2 Duncan<br />
Reid MHSc (Hons), PGD (Manip Physiotherapy), MNZCP; 3 Felicity Goodyear-Smith MBChB, MGP, FRNZCGP 2<br />
ABSTRACT<br />
AIM: To provide a succinct summary <strong>of</strong> the management <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> injuries to the shoulder for primary<br />
health care practitioners based on the <strong>New</strong> <strong>Zealand</strong> guideline.<br />
METHODS: A multidisciplinary team developed the guideline by critically appraising and grading retrieved<br />
literature using the Graphic Appraisal Tool for Epidemiology (GATE); and the Scottish Intercollegiate<br />
Guideline Network. Recommendations were derived from resulting evidence tables.<br />
RESULTS: For the management <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder disorders there is little evidence to support or<br />
refute the efficacy <strong>of</strong> common interventions for shoulder disorders in general and rotator cuff disorders in<br />
particular. For rotator cuff tendinosis and partial tears, use NSAIDs and subacromial corticosteroid injections<br />
with caution and provide a trial <strong>of</strong> supervised exercise. For frozen shoulders, intra-articular corticosteroid<br />
injection should be considered and refer for supervised exercise after acute pain has settled. For<br />
shoulder instability, good evidence supports the referral <strong>of</strong> physically active young adults for orthopaedic<br />
intervention following a first traumatic shoulder dislocation.<br />
CONCLUSION: While there is a dearth <strong>of</strong> good evidence, this guideline does provide a framework for<br />
the management <strong>of</strong> common s<strong>of</strong>t t<strong>issue</strong> injuries <strong>of</strong> the shoulder.<br />
KEyWORDS: Shoulder, s<strong>of</strong>t t<strong>issue</strong> injuries, primary health care<br />
Introduction<br />
Diagnosis and management <strong>of</strong> shoulder injuries is<br />
one <strong>of</strong> the most challenging areas <strong>of</strong> musculoskeletal<br />
medicine. Prevalence figures for shoulder<br />
disorders vary widely for point prevalence<br />
(7–26%), one month prevalence (19–31%), one<br />
year prevalence (5–47%) and lifetime prevalence<br />
(7–66%). 1 Shoulder disorders are therefore relatively<br />
common, but only 50% <strong>of</strong> new episodes <strong>of</strong><br />
shoulder complaints presented in primary care are<br />
completely recovered within six months, increasing<br />
to only 60% at one year. 2<br />
It is likely that suboptimal management contributes<br />
to unfavourable outcomes for patients. This<br />
paper is the second <strong>of</strong> a two-part series which<br />
summarises the evidence for assessment and management<br />
<strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder injuries based on<br />
the evidence-based guideline <strong>The</strong> diagnosis and<br />
management <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder injuries and<br />
related disorders developed in <strong>New</strong> <strong>Zealand</strong> (NZ),<br />
led by EPIQ, University <strong>of</strong> Auckland under the<br />
auspices <strong>of</strong> the <strong>New</strong> <strong>Zealand</strong> Guidelines Group<br />
(NZGG). 3 This guideline was commissioned by<br />
ACC in 2003 to reduce identified variation in<br />
both diagnosis and management and to improve<br />
outcomes for claimants.<br />
This guideline was endorsed by the <strong>Royal</strong> <strong>New</strong><br />
<strong>Zealand</strong> <strong>College</strong> <strong>of</strong> <strong>General</strong> Practitioners, the<br />
NZ Orthopaedic Association, the NZ Society <strong>of</strong><br />
Physiotherapists Inc., the NZ Association <strong>of</strong> Mus-<br />
42 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
culoskeletal Medicine, Sports Medicine NZ, and<br />
the <strong>Royal</strong> Australasian and <strong>New</strong> <strong>Zealand</strong> <strong>College</strong><br />
<strong>of</strong> Radiologists. <strong>The</strong> full document is available on<br />
the NZGG website (http://www.nzgg.org.nz).<br />
<strong>The</strong> aim <strong>of</strong> this paper is to provide a succinct<br />
summary <strong>of</strong> the management <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong><br />
injuries to the shoulder in a form that is readily<br />
accessible to primary health care practitioners.<br />
Methods<br />
Methods have been described in Part 1. Part 2<br />
<strong>of</strong> this summary addresses the management <strong>of</strong><br />
adults with the following shoulder injuries. Adolescents<br />
were included for shoulder instabilities<br />
given that dislocation and recurrent dislocation<br />
are more common in this age group.<br />
1. Rotator cuff and related disorders (including<br />
impingement, subacromial bursitis, tendinosis,<br />
painful arc syndrome, partial, full thickness<br />
and massive tears <strong>of</strong> the rotator cuff, long<br />
head <strong>of</strong> biceps rupture and calcific tendonitis)<br />
2. Frozen shoulder (also known as adhesive<br />
capsulitis)<br />
3. Glenohumeral instabilities (acute and<br />
recurrent dislocation, labral injuries and other<br />
instabilities)<br />
4. Acromioclavicular (AC) joint injuries<br />
(including stress osteolysis, osteoarthritis and<br />
dislocation)<br />
5. Sternoclavicular (SC) joint injuries (including<br />
sprains, dislocation and arthritis and related<br />
conditions).<br />
This guideline specifically excludes fractures, inflammatory<br />
conditions, degenerative conditions,<br />
endocrinological and neurological conditions.<br />
hemiplegic shoulder and chronic shoulder pain<br />
including occupational overuse disorders.<br />
For each <strong>of</strong> the included conditions evidence for<br />
management was sought based on searches relating<br />
to interventions commonly used in practice.<br />
For each condition a comprehensive literature<br />
search was undertaken in the major electronic<br />
databases (Medline, CINAHL, EMBASE, AMED,<br />
SPORTdiscus and Current Contents). Searching<br />
also included the Cochrane Database <strong>of</strong> Systematic<br />
Reviews, Cochrane Controlled Trials Register,<br />
WHAT GAP THIS FILLS<br />
What we already know: In general, the evidence for the management <strong>of</strong><br />
acute s<strong>of</strong>t t<strong>issue</strong> shoulder injuries is weak and limited.<br />
What this study adds: For rotator cuff tendinosis and partial tears, use<br />
NSAIDs and subacromial corticosteroid injections with caution and provide<br />
a trial <strong>of</strong> supervised exercise. For frozen shoulders, intra-articular corticosteroid<br />
injection should be considered and refer for supervised exercise after<br />
acute pain has settled. For shoulder instability, good evidence supports the<br />
referral <strong>of</strong> physically active young adults for orthopaedic intervention following<br />
a first traumatic shoulder dislocation.<br />
the Database <strong>of</strong> Reviews <strong>of</strong> Effectiveness (DARE)<br />
and relevant Internet sites including PEDro, NHS<br />
clinical trials, Health Technology Assessments for<br />
NHS, Bandolier and National Guideline Clearing<br />
House. Reference lists <strong>of</strong> included studies were<br />
checked for additional studies.<br />
Only published randomised controlled trials,<br />
meta-analyses and systematic reviews in the<br />
English language were considered for inclusion.<br />
Quality was assessed using the Generic Appraisal<br />
Tool for Epidemiology (GATE) available at: http://<br />
www.epiq.co.nz (modified since this guideline<br />
developed).<br />
Evidence from the relevant studies was summarised<br />
into evidence tables. Recommendations<br />
were developed using the SIGN ‘Considered<br />
Judgment’ process. (SIGN Guideline development<br />
process: http://www.sign.ac.uk/guidelines/fulltext/50/compjudgement.html)<br />
Grading is based on the strength <strong>of</strong> the evidence<br />
and does not indicate the relative importance <strong>of</strong><br />
the recommendations.<br />
Results<br />
Results are presented for each condition according<br />
to the grade <strong>of</strong> recommendation as follows:<br />
• A Recommendation:<br />
Supported by good evidence<br />
• B Recommendation:<br />
Supported by fair evidence<br />
• Good practice point:<br />
Consensus <strong>of</strong> the guideline team.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 43
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
In general, due to lack <strong>of</strong> agreement in defining<br />
shoulder disorders, poor quality <strong>of</strong> studies,<br />
and heterogeneity <strong>of</strong> studies with respect<br />
to participants, interventions, and outcomes,<br />
there is little evidence to support or refute the<br />
efficacy <strong>of</strong> common interventions for shoulder<br />
disorders in general 4,5 and rotator cuff disorders<br />
in particular. 6<br />
1. Rotator cuff and related disorders<br />
Rotator cuff disorders are the most common<br />
sources <strong>of</strong> shoulder problems. <strong>The</strong>y range from<br />
mild strain causing impingement-type symptoms<br />
to massive tears and total absence <strong>of</strong> the cuff<br />
with severe loss <strong>of</strong> function. 7<br />
Tendinosis causing impingement-type symptoms<br />
(painful arc) is due to collagen fatigue resulting<br />
from repetitive overhead activities. 8 In contrast,<br />
rotator cuff tears typically result from trauma<br />
and are more common in people over the age <strong>of</strong><br />
35 years.<br />
Partial thickness tears can occur on the bursal<br />
or articular side <strong>of</strong> the rotator cuff and do not<br />
extend through the full thickness <strong>of</strong> the tendon.<br />
<strong>The</strong>se are more common than full thickness tears<br />
which extend through the full thickness <strong>of</strong> the<br />
tendon and are <strong>of</strong>ten more symptomatic. 9 Full<br />
thickness tears increase with advancing age, frequently<br />
occurring as a result <strong>of</strong> minimal trauma.<br />
<strong>The</strong>se tears are <strong>of</strong>ten asymptomatic and compatible<br />
with normal painless functional activity. 10<br />
Massive tears have been defined as tears >5cm or<br />
tears involving two or more tendons (more <strong>of</strong>ten<br />
supraspinatus and infraspinatus, but also supraspinatus<br />
with subscapularis). 11<br />
Weakness is the primary sign <strong>of</strong> loss <strong>of</strong> integrity<br />
<strong>of</strong> the rotator cuff, but should be distinguished<br />
from weakness due to pain inhibition. 10<br />
B recommendations<br />
• Prescribe NSAIDS with caution. <strong>The</strong>y<br />
provide short-term symptomatic pain relief<br />
but can have serious consequences. 12<br />
• Use subacromial corticosteroid injection<br />
with caution. It provides short-term<br />
symptomatic relief for people with tendinosis<br />
and partial thickness tears. 13,14<br />
<strong>The</strong>re is insufficient evidence to determine<br />
the benefits or harms <strong>of</strong> subacromial steroid<br />
injection for full thickness rotator cuff tears. 6<br />
Provide a trial <strong>of</strong> supervised exercise<br />
by a recognised treatment provider for<br />
people with rotator cuff disorders. 4<br />
Avoid the use <strong>of</strong> therapeutic ultrasound<br />
(no additional benefit over<br />
and above exercise alone). 4<br />
For calcific tendonitis, there is limited<br />
evidence for the use <strong>of</strong> ultrasound for pain<br />
relief, 15 and weak evidence for the use <strong>of</strong> Extracorporeal<br />
Shock Wave <strong>The</strong>rapy (ESWT). 16-19<br />
44 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE<br />
•<br />
•<br />
•<br />
•<br />
Good practice points for<br />
rotator cuff and related disorders<br />
• Simple analgesics provide pain relief with<br />
potential for less serious side effects.<br />
• Subacromial corticosteroid injections may<br />
be appropriate for full thickness tears as<br />
part <strong>of</strong> long-term management where surgery<br />
is not considered as a treatment option.<br />
• If there is no significant improvement<br />
in patients with a full thickness<br />
tear <strong>of</strong> the rotator cuff after four to six<br />
weeks <strong>of</strong> non-operative management,<br />
refer to an orthopaedic specialist.<br />
• Early surgical management for a rotator<br />
cuff tears has the most to <strong>of</strong>fer people<br />
with otherwise healthy t<strong>issue</strong> and who<br />
are physiologically young and active.<br />
<strong>The</strong>re are a number <strong>of</strong> disorders closely related to<br />
rotator cuff tears which should be considered as<br />
part <strong>of</strong> the differential diagnosis.<br />
• Biceps tendinosis is part <strong>of</strong> the spectrum <strong>of</strong><br />
pathological processes <strong>of</strong> rotator cuff disorders<br />
and should be managed in the same<br />
way as rotator cuff tendinosis. Rupture <strong>of</strong><br />
the biceps tendon is more common with<br />
increasing age. 20 Management is symptomatic<br />
with almost no indication for operative<br />
repair. Where instability (subluxation<br />
or dislocation <strong>of</strong> the biceps tendon) is suspected,<br />
refer to an orthopaedic surgeon.<br />
• Calcific tendonitis usually occurs spontaneously<br />
and is self-limiting. 16 People with
severe pain and dysfunction may require<br />
urgent referral to an orthopaedic specialist.<br />
• Isolated muscle tears,<br />
while rare, occur<br />
most commonly in the subscapularis 21<br />
and pectoralis major. 22 Both require urgent<br />
referral for orthopaedic evaluation.<br />
2. Frozen shoulder<br />
<strong>The</strong> true frozen shoulder is characterised by an<br />
unknown aetiology, spontaneous and gradual<br />
onset <strong>of</strong> pain and global restriction <strong>of</strong> movement.<br />
23,24 <strong>The</strong> clinical presentation is described as<br />
involving three phases. An initial painful phase<br />
lasting two to three months in which pain is<br />
severe and movement severely restricted is<br />
followed by a second phase also lasting two to<br />
three months where pain diminishes and the<br />
predominant feature is stiffness. Resolution<br />
typically occurs over the next six to 12 months in<br />
which there is a gradual gain in range <strong>of</strong> movement<br />
with less discomfort. In contrast with rotator<br />
cuff impingement or tear, a key diagnostic feature<br />
<strong>of</strong> frozen shoulder is stiffness (limitation <strong>of</strong> both<br />
passive and active range), lack <strong>of</strong> discomfort with<br />
resisted movement and no weakness. <strong>The</strong>re is<br />
frequently substantial functional limitation with<br />
respect to activities <strong>of</strong> daily living. 25<br />
B recommendations<br />
• In the painful phase actively consider intraarticular<br />
corticosteroid injection performed by<br />
an experienced clinician. 14,26<br />
• After the acute pain has settled <strong>of</strong>fer supervised<br />
exercise by a recognised treatment provider to<br />
improve range <strong>of</strong> movement. 26 Mobilisation<br />
does not <strong>of</strong>fer any additional benefit. 14<br />
• Laser therapy and acupuncture may be beneficial<br />
in the treatment <strong>of</strong> frozen shoulder. 4,27<br />
• Hydrodilation has not been found to be<br />
effective. 5<br />
Good practice points for<br />
frozen shoulder<br />
• Avoid vigorous stretching in the early<br />
phase as this will exacerbate pain.<br />
• It is important that people with a frozen<br />
shoulder understand the time it<br />
takes for this condition to resolve.<br />
3. Glenohumeral instabilities<br />
Instabilities are symptomatic manifestation<br />
<strong>of</strong> pathological movement <strong>of</strong> one joint surface<br />
in relation to another and should be contrasted<br />
with laxity which is the non-pathological<br />
linear displacement <strong>of</strong> one articular surface<br />
in relation to the other. 28 Instabilities include<br />
acute glenohumeral dislocations (anterior, posterior<br />
and inferior), multidirectional instability<br />
(global laxity <strong>of</strong> the shoulder) and tears <strong>of</strong> the<br />
glenoid labrum.<br />
Anterior dislocations are the most common<br />
acute traumatic dislocation. In younger people<br />
these are <strong>of</strong>ten associated with detachment <strong>of</strong><br />
the labrum from the rim (Bankart lesions) with<br />
a 90% chance <strong>of</strong> recurrence in people under 20<br />
years. 29 Dislocations are also common in the<br />
sixth decade <strong>of</strong> life 30 but are more likely to be<br />
associated with capsular tear and concomitant<br />
rotator cuff tears. 31<br />
Labral injuries (including detachment <strong>of</strong> the<br />
superior labrum either anteriorly, superiorly<br />
or both) are common in overhead athletes as<br />
progressive failure <strong>of</strong> the labrum or may occur<br />
as a traumatic event in association with anterior<br />
dislocation. 32 <strong>The</strong>se are <strong>of</strong>ten associated with<br />
vague symptoms <strong>of</strong> impingement associated with<br />
activity, clicking, locking and in some a ‘dead<br />
arm’ which is the sudden sharp paralysing pain<br />
or sense <strong>of</strong> subluxation associated with weakness,<br />
tingling and numbness. 33<br />
A recommendations<br />
• Young adults engaged in demanding<br />
physical activities with a first traumatic<br />
shoulder dislocation should be<br />
referred for orthopaedic evaluation. 34<br />
Good practice points for<br />
glenohumeral instabilities<br />
• Investigations for acute dislocations:<br />
– Pre-reduction x-ray is recommended<br />
for people >40 years <strong>of</strong> age.<br />
– Post-reduction x-ray is recommended<br />
for all people with a first time<br />
dislocation to confirm the reduction<br />
and assess for bony injury.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 45
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
– X-ray is required for all people with<br />
a failed attempt at reduction.<br />
– X-ray is recommended for those with<br />
recurrent dislocation where surgical stabilisation<br />
may be a management option.<br />
• Acute management <strong>of</strong> dislocations:<br />
– Only clinicians with expertise should<br />
reduce anterior or posterior dislocations.<br />
– Relaxation is critical for successful reduction.<br />
Ensure adequate analgesia is given<br />
as required before attempting reduction.<br />
– Attempt slow steady traction for at least<br />
30 seconds, avoiding excessive force while<br />
attempting to reduce a dislocated shoulder.<br />
– Urgent referral to an orthopaedic specialist<br />
is required when reduction is<br />
unsuccessful after two attempts.<br />
• Post-reduction management <strong>of</strong> dislocations:<br />
– In people with a primary dislocation<br />
for whom non-operative management<br />
is appropriate apply a sling,<br />
provide analgesia and refer for a supervised<br />
exercise programme.<br />
– Following dislocation, people should<br />
not return to sport for at least six<br />
weeks, or when they have achieved<br />
near normal muscle strength.<br />
• Recurrent dislocation:<br />
– People with recurrent dislocation<br />
(>2) should be referred to an orthopaedic<br />
specialist to evaluate the<br />
need for surgical stabilisation.<br />
• Multidirectional instability:<br />
– A comprehensive rehabilitation programme<br />
focusing on strengthening<br />
the scapular stabilisers and rotator<br />
cuff muscle may improve function.<br />
– Where treatment fails to improve<br />
function by six months, surgical intervention<br />
may be considered.<br />
• Labral tears:<br />
– Labral injuries should be referred to an<br />
orthopaedic surgeon for evaluation.<br />
4. Acromioclavicular joint injuries<br />
Acromioclavicular (AC) joint injuries are common<br />
in men between the second and fourth decade <strong>of</strong><br />
life, frequently occurring during sport from a fall<br />
on the point <strong>of</strong> the shoulder. 35 AC joint injuries<br />
are classified as Grade I (intact joint), Grade II (up<br />
to 50% vertical subluxation <strong>of</strong> the clavicle with<br />
rupture <strong>of</strong> the AC ligament) and Grade III (more<br />
than 50% vertical subluxation <strong>of</strong> the clavicle and<br />
complete rupture <strong>of</strong> both the AC and coracoclavicular<br />
ligaments). 35,36<br />
Good practice points for<br />
acromioclavicular joint injuries<br />
• People with Grade I and II sprains can be<br />
provided with a sling and analgesics for<br />
five to seven days until comfortable.<br />
• <strong>The</strong>re is a lack <strong>of</strong> evidence to support<br />
any particular method <strong>of</strong> taping.<br />
• Advise gradual return to activity as<br />
symptoms settle, avoiding heavy lifting<br />
and contact sports for eight to 12 weeks.<br />
• People with Grade III AC joint sprains<br />
can be managed non-operatively, but<br />
if this is not successful after three<br />
months, consider referral to a specialist<br />
for further evaluation.<br />
• More serious AC joint dislocations require<br />
referral for orthopaedic evaluation.<br />
5. Sternoclavicular joint injuries<br />
<strong>The</strong> most common sternoclavicular (SC) disorders<br />
are strains sustained from motor vehicle and<br />
sporting injuries. 37,38 In mild strains, the ligaments<br />
are intact and the joint stable. In moderate<br />
strains, the ligaments may be partially disrupted<br />
and the joint is subluxed. Severe strains (dislocations)<br />
are rare, the most common being anterior<br />
dislocations. Posterior dislocations, however,<br />
while uncommon, may compromise major vessels,<br />
the trachea and oesophagus which are in close<br />
proximity. 39,40<br />
Local tenderness and swelling characterise milder<br />
strains, whereas a palpable gap may be present in<br />
more serious injuries. CT may be the best radiological<br />
technique for SC joints.<br />
46 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Good practice points for<br />
sternoclavicular joint injuries<br />
• Although rare, clinicians should watch<br />
for pulmonary or vascular compromise<br />
due to a posterior dislocation <strong>of</strong> the SC<br />
joint usually resulting from severe compression<br />
trauma. Immediate referral to<br />
an appropriate specialist is required.<br />
• Most injures <strong>of</strong> the SC joint are mild<br />
and can be managed with a sling, analgesics<br />
and return to activity as tolerated.<br />
Discussion<br />
In general, the evidence for the management <strong>of</strong><br />
acute s<strong>of</strong>t t<strong>issue</strong> shoulder injuries is weak and<br />
limited. Little has been added in the years since<br />
publication <strong>of</strong> the guideline.<br />
A brief search for guidelines, systematic reviews<br />
or meta-analyses published since the development<br />
<strong>of</strong> the NZ guideline 3 revealed an additional three<br />
Cochrane reviews 41-43 and a number <strong>of</strong> reviews<br />
published in other journals. 44,45,46-53<br />
<strong>The</strong> first <strong>of</strong> the three Cochrane reviews found<br />
little evidence to support or refute the use <strong>of</strong><br />
acupuncture for shoulder pain in general, but<br />
suggested there may be short-term benefit with<br />
respect to pain and function. 41<br />
<strong>The</strong> second Cochrane review was suggestive that<br />
oral steroids confer a worthwhile short-term<br />
(six weeks) benefit for pain, range <strong>of</strong> movement<br />
and function in people with adhesive capsulitis.<br />
42 <strong>The</strong> stage at which this was most effective<br />
was not specified, but the median duration <strong>of</strong><br />
symptoms <strong>of</strong> participants in the included studies<br />
was six months. While adverse effects reported<br />
were minor, the potential risk <strong>of</strong> oral steroids<br />
should be considered when making treatment<br />
decisions. 42<br />
<strong>The</strong> third Cochrane review reported a lack <strong>of</strong><br />
evidence to inform choices for conservative<br />
management following closed reduction <strong>of</strong> traumatic<br />
anterior dislocation <strong>of</strong> the shoulder. 43<br />
This review was based on one small, preliminary,<br />
poor quality study which was also included in<br />
the shoulder guideline. 54 While the review reported<br />
no significant differences between groups<br />
for any outcome, the study did claim that<br />
fixation in external rotation was effective in<br />
reducing redislocation at 15-months’ follow-up<br />
(p=0.008). Given that this was a small, poor quality<br />
study, the conclusions <strong>of</strong> the review<br />
are relevant.<br />
Of the additional reviews located, seven related<br />
to disorders <strong>of</strong> the rotator cuff, 44, 45,46-49,53 one<br />
related to adhesive capsulitis, 50 one focused on<br />
instability, 51 and one reviewed the management<br />
<strong>of</strong> Grade III acromioclavicular injuries. 52 For<br />
disorders <strong>of</strong> the rotator cuff, the findings <strong>of</strong><br />
these reviews are consistent with the guideline<br />
and no new evidence was reported for treatment<br />
options. One review, however, investigated factors<br />
influencing the decisions to surgically repair<br />
symptomatic full thickness rotator cuff tears,<br />
including demographic variables (age and gender),<br />
duration <strong>of</strong> symptoms, non-operative treatment,<br />
timing <strong>of</strong> surgery, physical examination findings,<br />
In general, the evidence for the management<br />
<strong>of</strong> acute s<strong>of</strong>t t<strong>issue</strong> shoulder injuries is weak<br />
and limited<br />
ORIGINAL SCIENTIFIC PAPERS<br />
size <strong>of</strong> the tear and pending workers compensation<br />
claims. While there was no randomised trial<br />
evidence for any one factor, they suggested that<br />
older chronological age should not be considered<br />
a barrier to operative repair as studies have reported<br />
good outcomes for older patients and that<br />
pending workers’ compensation claims did not<br />
appear to influence treatment results. 53<br />
A systematic review <strong>of</strong> randomised trials using<br />
multiple corticosteroid injections for adhesive<br />
capsulitis evaluated nine trials, <strong>of</strong> which four<br />
were considered to be <strong>of</strong> high methodological<br />
quality. This review found a benefit for up<br />
to three corticosteroid injections and limited<br />
evidence that six injections were beneficial. <strong>The</strong>re<br />
was no evidence that more than six injections<br />
were <strong>of</strong> benefit. It should be noted that while five<br />
different corticosteroids were used, all were given<br />
SYSTEMATIC REVIEW<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 47
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
intra-articularly. Also, only two <strong>of</strong> these studies<br />
were based in general practice. 50<br />
A review <strong>of</strong> the effectiveness <strong>of</strong> rehabilitation for<br />
non-operative management <strong>of</strong> shoulder instability<br />
found only weak evidence to support immobilisation<br />
for three to four weeks followed by a<br />
structured rehabilitation programme for people<br />
with a primary dislocation. 51 Instability in this<br />
review was defined as symptomatic hypermobility<br />
(single plane or multidirectional) resulting<br />
from traumatic and atraumatic subluxation or<br />
dislocation.<br />
For Grade III acromioclavicular injuries, nonoperative<br />
treatment is the preferred option based<br />
on three randomised trials included in a review<br />
which concluded that while surgical results were<br />
‘no better’ they were associated with more complications,<br />
increased convalescence and time away<br />
from work. 52<br />
Conclusion<br />
As with diagnosis <strong>of</strong> shoulder injuries, the<br />
evidence for management <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder<br />
injuries is limited and largely determined by the<br />
collective experience and expertise <strong>of</strong> practitioners<br />
in the field.<br />
References<br />
1. Luime JJ, Koes BW, Hendrikson LJM, Burdorf A, Verhagen<br />
AP, Miedema HS, et al. Prevalence and incidence <strong>of</strong> shoulder<br />
pain in the general population: A systematic review. Scand J<br />
Rheumatol 2004;33:73–81.<br />
2. Kuijpers T, Van der Windt DA, Van der Heijden GJ, Bouter LM.<br />
Systematic review <strong>of</strong> prognostic cohort studies on shoulder<br />
disorders. Pain 2004;109:420–431.<br />
3. Accident Compensation Corporation, <strong>New</strong> <strong>Zealand</strong> Guidelines<br />
Group. <strong>The</strong> diagnosis and management <strong>of</strong> s<strong>of</strong>t t<strong>issue</strong> shoulder<br />
injuries and related disorders. Wellington: ACC; 2004.<br />
4. Green A. Physiotherapy interventions for shoulder pain.<br />
Cochrane Database Syst Rev 2003(3).<br />
5. Green S, Buchbinder R, Glazier R, Forbes A. Interventions for<br />
shoulder pain (Cochrane Review). Cochrane Database Syst<br />
Rev 2003(2).<br />
6. Ejnisman B, Carrera EF, Fallopa F, Peccin MS, Cohen M.<br />
Interventions for tears <strong>of</strong> the rotator cuff in adults. Cochrane<br />
Library 2004(Issue 1).<br />
7. Sher JS. Anatomy, biomechanics and pathophysiology <strong>of</strong> rotator<br />
cuff disease. Philadelphia: Lippincott Williams & Wilkins;<br />
1999.<br />
8. Khan KM, Cook JL, Taunton JE, Bonar F. Overuse tendinsosis:<br />
not tendinitis. Part 1: A new paragidm for a difficult clinical<br />
problem. Physician Sports Med 2000;28(5):31–46.<br />
9. Fukuda H. <strong>The</strong> management <strong>of</strong> partial-thickness tears <strong>of</strong> the<br />
rotator cuff. J Bone Joint Surg—Series B 2003;85(1):3–11.<br />
10. Matsen FA, Arntz CT, Lippitt S. Rotator Cuff. 2nd ed. WB<br />
Saunders Co.; 1998.<br />
11. Gerber C. Massive rotator cuff tears. Philadelphia: Lippincott<br />
Williams and Wilkins; 1999.<br />
12. Van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder<br />
disorders in general practice: incidence, patient characteristics<br />
and management. Ann Rheum Dis 1995;54:959–964.<br />
13. Arroll B, Goodyear-Smith F. Corticosteroid injections for<br />
painful shoulder:a meta-analysis. Br J Gen Pract 2005;<br />
55:224–228.<br />
14. Buchbinder R, Green S, Youd JM. Corticosteroid injections<br />
for shoulder pain. Cochrane Database Syst Rev<br />
2003(1):CD004016.<br />
15. Ebenbichler GR, Erdogmus CB, Resch KL, Funovics MA,<br />
Kainberger F, Barisani G, et al. Ultrasound therapy for<br />
calcific tendinitis <strong>of</strong> the shoulder.[comment]. N Engl J Med<br />
1999;340(20):1533–8.<br />
16. Gerdesmeyer L, Wagenpfeil S, Haake M, Maier M, Loew M,<br />
Wortler K, et al. Extracorporeal shock wave therapy for the<br />
treatment <strong>of</strong> chronic calcifying tendonitis <strong>of</strong> the rotator cuff: A<br />
randomised controlled trial. JAMA 2003;290(19):2573–2580.<br />
17. Pan P, Chou CL, Chiou HJ, Ma HL, Lee HC, Chan RC. Extracorporeal<br />
shock wave therapy for chronic calcific tendinitis <strong>of</strong> the<br />
shoulders: a functional and sonographic study. Arch Phys Med<br />
Rehabil 2003;84:988–993.<br />
18. Cosentino R, De Stefano R, Selvi E, Frati E, manca S, Frediani<br />
B, et al. Extracorporeal shock wave therapy for chronic calcific<br />
tedninitis <strong>of</strong> the shoulder: single blind study. Ann Rheum Dis<br />
2003;62(3):248–250.<br />
19. Loew M, Daecke W, Kusnierczak D, Rahmanzadeh M,<br />
Ewerbeck V. Shock-wave therapy is effective for chronic<br />
calcifying tendinitis <strong>of</strong> the shoulder. J Bone Joint Surg—Br<br />
1999;81(5):863–7.<br />
20. Yamaguchi K, Bindra R. Disorders <strong>of</strong> the biceps tendon. Philadelphia:<br />
Lippincott Williams and Wilkins; 1999.<br />
21. Warner JJ, Answorth AA. Diagnosis and management <strong>of</strong><br />
subscpularis tendon tears. Tech Orthop 1994;9:116–125.<br />
22. Dodds SD, Wolfe SW. Injuries to the pectoralis major. Sports<br />
Medicine 2002;32(14):945–52.<br />
23. Harryman DT, Lazarus JM, Rozencwaig R. <strong>The</strong> stiff shoulder.<br />
Second Edition ed: WB Saunders Co.; 1998.<br />
24. Rizk TE, Christopher RP, Pinals RS, et al. Adhesive capsulitis<br />
(frozen shoulder): A new approach to its management. Arch<br />
Phys Med Rehabil 1983;64(1):29–33.<br />
25. Neviaser RJ. Radiologic assessment <strong>of</strong> the shoulder. Plain and<br />
arthrographic. Orthop Clin <strong>of</strong> North Am 1987;18(3):343–349.<br />
26. Carette S, M<strong>of</strong>fet H, Tardif J, Bessette L, Morin F, Fremont P, et<br />
al. Intraarticular corticosteroids, supervised physiotherapy, or<br />
a combination <strong>of</strong> the two in the treatment <strong>of</strong> adhesive capsulitis<br />
<strong>of</strong> the shoulder: A placebo-controlled trial. 01 MAR 2003<br />
Arthritis Rheum 2003;48(3):829–838.<br />
27. Sun KO, Chan KC, Lo SL, Fong DY. Acupuncture for frozen<br />
shoulder. Hong Kong Med J 2001;7(4):381–91.<br />
28. Cole BJ, Warner JJ. Anatomy, Biomechanics, and pathophysiology<br />
<strong>of</strong> glenohumeral instabiltiy. Philadelphia: Lippincott<br />
Williams & Wilkins; 1999.<br />
29. Matsen FA, Thomas SC, Rockwood CA, Wirth CJ. Glenohumeral<br />
instability. WB Saunders Co.; 1998.<br />
30. Hayes K, Callanan M, Walton J, Paxinos A, Murrell GAC.<br />
Shoulder instability: Management and rehabilitation. J Orthop<br />
Sports Phys <strong>The</strong>r 2002;32(10):497–509.<br />
31. Liu SH, Mark H. Anterior shoulder instability: Current Review.<br />
Clinical Orthopaedics & Related Research 1996;323:327–337.<br />
32. Parentis MA, Mohr KJ, ElAttrache NS. Disorders <strong>of</strong> the<br />
superior labrum: review and treatment guidelines. Clin Orthop<br />
Relat Res 2002(400):77–87.<br />
33. Rowe CR. Recurrent transient anterior subluxation <strong>of</strong> the<br />
shoulder. Clin Orthop Relat Res 1987;223:11–19.<br />
48 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
34. Handoll HHG, Almaiyah MA, Rangan A. Surgical versus<br />
non-surgical treatment for acute anterior shoulder dislocation.<br />
Cochrane Database Syst Rev 2004(Issue 1).<br />
35. Rockwood CA, Williams GR, Young DC. Disorders <strong>of</strong> the<br />
acromioclavicular joint. WB Saunders Co.; 1998.<br />
36. Bossart PJ, Jouce SM, Manaster BJ, Packer SM. Lack <strong>of</strong> efficacy<br />
<strong>of</strong> ‘weighted’ radiographs in diagnosing acute acromioclavicular<br />
separation. Ann Emerg Med 1988;17(1):20–24.<br />
37. Wirth MA, Rockwood CA. Disorders <strong>of</strong> the sternoclavicular<br />
joint:Pathophysiology, diagnosis and management. Philadelphia:<br />
Lippincott Williams and Wilkins; 1999.<br />
38. Yeh GL, Williams GR, Jr. Conservative management <strong>of</strong> sternoclavicular<br />
injuries. Orthop Clin North Am 2000;31(2):189–203.<br />
39. Rockwood CA, WIrth MA. Disorders <strong>of</strong> the sternoclavicular<br />
joint. 2nd ed. WB Saunders Co.; 1999.<br />
40. Szalay EA, Rockwood CA, Jr. Injuries <strong>of</strong> the shoulder and arm.<br />
Emerg Med Clinics North Am 1984;2(2):279–94.<br />
41. Green S, Buchbinder R, Hetrick S. Acupuncture for shoulder<br />
pain. Cochrane Database <strong>of</strong> Syst Rev 2005; Issue 2.<br />
42. Buchbinder R, Green S, Youd JM, Johnstone RV. Oral steroids<br />
for adhesive capsulitis Cochrane Database Syst Rev 2006;<br />
Issue 4.<br />
43. Handoll HHG, Hanchard NCA, Goodchild L, Feary J. Conservative<br />
management following closed reduction <strong>of</strong> traumatic<br />
dislocation <strong>of</strong> the shoulder Cochrane Database Syst Rev 2006;<br />
Issue 1.<br />
44. Michener LA, Walsworth MK, Burnet EN. Effectiveness <strong>of</strong><br />
rehabilitation for patients with subacromial impingement syndrome.<br />
A systematic review. J Hand <strong>The</strong>r 2004;17:152–164.<br />
45. Faber KJ, Kuiper JI, Burdorf A, Miedema HS, Verhaar J. Treatment<br />
<strong>of</strong> impingement syndrome: a systematic review on the<br />
effects on functional limitations and return to work. J Occup<br />
Rehab 2006;16:7–25.<br />
46. Grant HJ, Arthur A, Pichora DR. Evaluation <strong>of</strong> interventions<br />
for rotator cuff pathology. A systematic review. J Hand <strong>The</strong>r<br />
2004;17:274–299.<br />
47. Koester MC, Dunn WR, Kuhn JE, Spindler KP. <strong>The</strong> efficacy <strong>of</strong><br />
subacromial corticosteroid injection in the treatment <strong>of</strong> rotator<br />
cuff disease. A systematic review. J Am Acad Orthop Surg<br />
2007;15:3–11.<br />
48. Ainsworth R, Lewis JS. Exercise therapy <strong>of</strong> the conservative<br />
management <strong>of</strong> full thickness tears <strong>of</strong> the rotator cuff. A<br />
systematic review. Br J Sports Med 2007;41:200–210.<br />
49. Harniman E, Carette S, Kennedy C, Beaton DE. Extracorporeal<br />
shock wave therapy for calcific and noncalcific tendonitis<br />
<strong>of</strong> the rotator cuff. A systematic review. J Hand <strong>The</strong>r<br />
2004;17:132–151.<br />
50. Shah N, Lewis M. Shoulder adhesive capsulitis: systematic<br />
review <strong>of</strong> randomised trials using multiple corticosteroid<br />
injections. British Journal <strong>of</strong> <strong>General</strong> Practice 2007(August):662–667.<br />
51. Gibson K, Growse A, Korda L, Wray E, MacDermid JC. <strong>The</strong><br />
effectiveness <strong>of</strong> rehabilitation for nonoperative management<br />
<strong>of</strong> shoulder instability. J Hand <strong>The</strong>r 2004;17:229–242.<br />
52. Spencer EE. Treatment <strong>of</strong> Grade III acromiclavicular<br />
joint injuries. Clinical Orthopaedics & Related Research<br />
2006;455:38–44.<br />
53. Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for<br />
rotator cuff repair. Clin Orthop Relat Res 2006;455:52–63.<br />
54. Itoi E, Hatakeyama Y, Kido T. A new method <strong>of</strong> immobilization<br />
after traumatic anterior dislocation <strong>of</strong> the shoulder: a preliminary<br />
study. J Shoulder Elbow Surg 2003;12(5):413–415.<br />
ORIGINAL SCIENTIFIC PAPERS<br />
SYSTEMATIC REVIEW<br />
ACKNOWLEDGEMENTS<br />
Funded by the Accident<br />
Compensation Corporation<br />
<strong>New</strong> <strong>Zealand</strong><br />
COMPETING INTERESTS<br />
None declared.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 49
iMPROViNg PERfORMANCE<br />
1 Harbour Health Primary<br />
Health Organisation,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
2 HealthWEST Primary Health<br />
Organisation, Auckland,<br />
<strong>New</strong> <strong>Zealand</strong><br />
CORRESPONDENCE TO:<br />
Angela Verhoeven<br />
PO Box 104 098,<br />
Lincoln North, Auckland<br />
0654, <strong>New</strong> <strong>Zealand</strong><br />
Angela@healthwest.co.nz<br />
A patient-centred referral pathway for mild<br />
to moderate lifestyle and mental health<br />
problems: Does this model work in practice?<br />
Jill Calveley MBChB; 1 Angela Verhoeven PGDipHSc; 2 David Hopcr<strong>of</strong>t MBChB, FRNZCGP, PhD 1<br />
Harbour Health and HealthWEST Primary Health Organisations in collaboration with the University <strong>of</strong> Auckland<br />
ABSTRACT<br />
BACkgROUND AND CONTExT: <strong>The</strong> Primary Lifestyle Options Programme was an innovative eightmonth,<br />
patient-centred, early primary care–based pilot aimed at identifying and promptly enabling<br />
people with mild to moderate mental health and lifestyle problems to access a range <strong>of</strong> free interventions<br />
as soon as possible.<br />
PROBLEMS: Mild to moderate mental health and lifestyle <strong>issue</strong>s are easily overlooked in primary care. Patients<br />
with these problems, once identified, <strong>of</strong>ten need support to choose and access treatment providers.<br />
STRATEgiES fOR iMPROVEMENT: During a GP visit a patient requests help by completing a CHAT<br />
(Case-finding and Help Assessment Tool) which assesses depression, anxiety, abuse, anger, exercise<br />
level, insomnia, and addictions (gambling, tobacco, alcohol and other substances). Patients subsequently<br />
have a 30-minute GP consultation where a range <strong>of</strong> services to address identified problem(s) is <strong>of</strong>fered;<br />
this choice is assisted by a comprehensive resource manual. A programme coordinator facilitates access<br />
to services by making appointments and liaising between patients and providers. A follow-up GP consult<br />
is available.<br />
RESULTS: 456 patients (6% Maori) aged from 15 to 84 years requested help via the CHAT for one to<br />
seven <strong>issue</strong>s per patient, over an eight-month period. Anxiety, depression and insomnia were the commonest<br />
reasons for requesting help. A feedback questionnaire focussed on the usefulness and practicality<br />
<strong>of</strong> the pathway, showing widespread approval from patients, GPs and other treatment providers.<br />
CONCLUSiONS: This programme enables a patient to identify and request help for mental health and<br />
lifestyle problems at a mild–moderate stage, and to be supported through an intervention pathway that<br />
otherwise is unlikely to be available in a busy primary care environment.<br />
kEywORDS: Primary care, patient-centred, mental health<br />
Background<br />
Mild to moderate mental health and lifestyle<br />
problems are ubiquitous and pervasive 1 and can be<br />
overlooked not only by patients and their families<br />
but also by their primary caregivers. While GPs<br />
are well placed to identify such problems,<br />
historically they have been thwarted in doing so<br />
by time constraints 2 and referral uncertainties.<br />
Furthermore, mild or sub-threshold mental<br />
disorders can be diagnostically challenging,<br />
especially in the absence <strong>of</strong> concomitant disability.<br />
3 Mental health screening in primary care has<br />
been widely advocated to address these concerns.<br />
However, reliable means <strong>of</strong> doing so have been<br />
less forthcoming and concerns have been raised<br />
about the efficacy <strong>of</strong> routine screening and the<br />
degree to which a single screening tool can be a<br />
diagnostic ‘gold standard’. 4 In this regard the<br />
50 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
CHAT (Case-finding and Health Assessment<br />
Tool), a short, self-administered screening<br />
questionnaire, has been developed and trialled in<br />
<strong>New</strong> <strong>Zealand</strong> to expedite screening <strong>of</strong> adults for<br />
lifestyle and mental health problems in the GP<br />
setting. 5 <strong>The</strong> largest trial was in Auckland,<br />
demonstrating high sensitivity and specificity for<br />
depression, anxiety and stress, abuse, anger<br />
problems, and tobacco, alcohol and other drug<br />
misuse, but had lower levels for exercise and<br />
eating disorders. <strong>The</strong> tool also assesses whether<br />
patients want help with these <strong>issue</strong>s, which<br />
reduces the chance <strong>of</strong> false positives. 6<br />
Having detected a lifestyle/mental health <strong>issue</strong>,<br />
what does the GP then do? Case-finding is one<br />
thing; prompt and appropriate intervention can be<br />
quite another. Traditional referral pathways are to<br />
hospital outpatient clinics (depression, anxiety,<br />
eating disorders), community clinics (for example<br />
community alcohol and drugs clinic or CADs),<br />
and private specialists (psychiatrists, psychologists).<br />
Often however, and especially in public<br />
mental health services, only those patients with<br />
significant acute illness will be seen. Private<br />
clinics are expensive, especially for multiple visits.<br />
Thus, people with mild to moderate lifestyle and/<br />
or mental health disorders are <strong>of</strong>ten left untreated,<br />
adversely affecting their well-being. 7<br />
<strong>The</strong> Primary Lifestyle Options programme was<br />
initiated to enable people with mild to moderate<br />
mental health and lifestyle problems to be<br />
reliably identified and then to have access to<br />
appropriate services as soon as possible. A sense<br />
<strong>of</strong> engagement in a programme increases patients’<br />
likelihood that they will attend. 8 Telephone<br />
prompting can also improve attendance rates. 9<br />
<strong>The</strong> pathway described in this paper is patientcentric—the<br />
patient identifies a problem and<br />
participates in the selection <strong>of</strong> interventions appropriate<br />
to the treatment <strong>of</strong> that problem. This<br />
evaluation focused on the utility <strong>of</strong> the model<br />
in primary care—is it practicable, does it fit in<br />
with general practice workflow, and does it meet<br />
patient requirements for choice and timeframes?<br />
Is it a viable model for people providing the<br />
interventions (those who the GP refers the patient<br />
on to)? Essentially, is the Primary Lifestyle<br />
Options programme a feasible, sensible workable<br />
model <strong>of</strong> care?<br />
wHAT gAP THiS fiLLS<br />
What is already known: <strong>The</strong> current public mental health system focuses<br />
more on patients with significant illness. Those with mild–moderate mental<br />
health and lifestyle <strong>issue</strong>s are <strong>of</strong>ten overlooked in primary care, and have<br />
a limited choice <strong>of</strong> interventions and/or support. <strong>The</strong> CHAT (Case-finding<br />
and Health Assessment Tool) has been validated as a reliable screening tool<br />
for many <strong>of</strong> these <strong>issue</strong>s. A sense <strong>of</strong> engagement in a programme increases<br />
patients’ likelihood that they will attend, and telephone prompting can also<br />
improve attendance rates.<br />
What this study adds: <strong>The</strong> Primary Lifestyle Options programme provides<br />
a patient-centric prompt intervention pathway—the patient identifies<br />
and requests help for a problem and participates in the selection <strong>of</strong> treatment<br />
options. Feedback from patients, GPs and other treatment providers indicate<br />
that this is a practicable, timely, and useful model in primary care.<br />
Purpose<br />
To identify those people with mild to moderate<br />
mental health and lifestyle problems attending<br />
their GP and to follow this with prompt access to<br />
appropriate services, within available resources.<br />
Model<br />
iMPROViNg PERfORMANCE<br />
Patients who were school leavers and older<br />
were asked by their GPs to complete a CHAT<br />
Lifestyle Assessment Tool. This was slightly<br />
modified from the original CHAT by replacing<br />
Eating Disorders with Insomnia, a known<br />
risk factor for, and consequence <strong>of</strong>, depression.<br />
10 Selection <strong>of</strong> these patients was at the<br />
discretion <strong>of</strong> the GP. <strong>The</strong> patient discussed the<br />
completed CHAT with the GP. Those patients<br />
who answered ‘Yes’ to the question ‘Do you<br />
want help with this?’ were asked whether they<br />
would like to make a 30-minute appointment to<br />
see the GP, to discuss intervention options for<br />
the mental health/lifestyle problem revealed by<br />
the CHAT assessment. GPs were assisted in this<br />
by a comprehensive Resource Manual. Intervention,<br />
either internal or external (see below) was<br />
started within one month <strong>of</strong> referral and completed<br />
within three months. A programme coordinator<br />
based at Harbour Health PHO assisted<br />
at various stages in this process by (1) providing<br />
information and support to patients, GPs,<br />
practices and service providers; (2) facilitating<br />
patient access to services, and (3) following up<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 51
iMPROViNg PERfORMANCE<br />
Figure 1. Primary Lifestyle Options referral pathways<br />
PN = Practice nurse; FU = Follow-up; DNA = Did not attend<br />
Table 1. External treatment provider examples<br />
Provider examples only<br />
(full list given to GPs in Resource Manual)<br />
Exercise Green Prescription Waitakere or North Shore;<br />
10 weeks’ local gym<br />
Smoking Smokefree Harbour Health; Quitline; Asian Smokefree<br />
Alcohol/<br />
illicit drugs<br />
Individual sessions with psychologist/psychotherapist/counsellor;<br />
Community, Alcohol and Drugs Service (CADS); Alcoholics<br />
Anonymous (AA); <strong>The</strong> Alcohol and Drug Helpline etc.<br />
gambling Individual sessions with psychologist/psychotherapist/counsellor;<br />
Problem Gambling Foundation hotline or Internet<br />
Depression/<br />
anxiety<br />
Violence, abuse,<br />
anger<br />
Individual sessions with psychologist/psychotherapist/counsellor;<br />
Essentially Men Weekend Course; Youthlink Family Programme;<br />
Life Line; Youth Line; Phobic Trust and many other family and<br />
community service organisations<br />
Individual sessions with psychologist/psychotherapist/counsellor;<br />
Victim Support; Man Alive; North Harbour Living Without<br />
Violence; North Shore Women’s Centre<br />
insomnia Refer for CBT—four sessions, or five if extra GP consult used<br />
those patients who did not attend these services.<br />
Those patients requiring or already receiving<br />
secondary care–level mental health interventions<br />
were not eligible. <strong>The</strong> overall pathway is summarised<br />
in Figure 1.<br />
Intervention referral options<br />
(1) Internal<br />
Patients with lifestyle/mental health conditions<br />
could be seen by a GP for up to four consults (in<br />
addition to the first 30-minute and 15-minute<br />
follow-up consults) for problem-solving or behavioural<br />
change management.<br />
(2) External (Table 1)<br />
Approximately 150 different providers were<br />
available for selection, including individual,<br />
group, community and support services specifically<br />
for Maori, Pacific Island, and Asian patients.<br />
This new model therefore introduced four processes<br />
to primary care:<br />
1. Patient identification <strong>of</strong> problem area(s)<br />
and request for ‘help’ using the CHAT<br />
questionnaire.<br />
2. A 30-minute extended GP consultation.<br />
3. A PHO-based Programme Coordinator.<br />
4. A 15-minute GP follow-up appointment after<br />
the intervention stage.<br />
All services were free for patients. <strong>The</strong> pilot,<br />
a joint initiative between Harbour Health and<br />
HealthWEST Primary Health Organisations<br />
(PHOs), was funded by the Waitemata District<br />
Health Board (DHB) and was approved by their<br />
Ethics Committee.<br />
Results<br />
Utilisation<br />
Sixty-nine GPs participated in the pilot, each<br />
enrolling from one to 35 patients. Between 15<br />
October 2007 and 30 June 2008 a total <strong>of</strong> 456 patients<br />
were referred for one <strong>of</strong> the interventions.<br />
Of these:<br />
52 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
• 357 patients (78%) were referred<br />
to external providers.<br />
• 99 patients (22%) were referred internally<br />
(i.e. GP or practice nurse); 20 <strong>of</strong> these<br />
were for smoking cessation and eight for<br />
Green Prescription/exercise counselling.<br />
• 91 (20%) completed the full course <strong>of</strong> interventions<br />
and the ‘exit consult’ with<br />
their GP. Approximately 40 had not attended<br />
their final ‘exit’ consult with their<br />
GP despite completing their interventions,<br />
by the time this report was prepared.<br />
• 60 (13%) patients had not attended<br />
any intervention session by the<br />
time this report was prepared.<br />
People requested help in all 10 problem areas on<br />
CHAT (only one for gambling, but there have<br />
been several more requests for help with this<br />
since 30 June 2008). <strong>The</strong> commonest amongst<br />
the 839 listed reasons for referral were depression<br />
(37%) and anxiety (26%). Sixty-seven percent <strong>of</strong><br />
referred patients had depression as at least one <strong>of</strong><br />
their referral reasons, and 35% had anxiety as at<br />
least one <strong>of</strong> their reasons (Figure 2). Fifty-seven<br />
percent <strong>of</strong> patients had two or more reasons for<br />
referral; the commonest (35%) coexisting conditions<br />
were anxiety–depression.<br />
Table 2. Enrolled patient demographics<br />
N %<br />
Gender female 292 64<br />
Male 164 46<br />
Ethnicity Asian 8 1.8<br />
Maori 26 5.7<br />
NZ European 379 83.1<br />
Pacific 5 1.1<br />
Other 38 8.3<br />
Age in years 15–24 72 15.8<br />
25–34 117 25.7<br />
35–44 116 25.4<br />
45–54 74 16.2<br />
55–64 52 11.4<br />
65–74 14 3.1<br />
75–84 11 2.4<br />
Figure 2. Reasons for referral; N=839<br />
Figure 3. Patient rating <strong>of</strong> CHAT Lifestyle Assessment Form; N=48*<br />
* Two people could not recall; two did not answer.<br />
Where people indicated a range e.g. ‘7–8’, the lower <strong>of</strong> the two was recorded<br />
Patient feedback<br />
iMPROViNg PERfORMANCE<br />
Fifty-two <strong>of</strong> the 91 patients who had completed<br />
the PLO programme gave feedback via a confidential<br />
written questionnaire.<br />
• Most patients rated the CHAT assessment form<br />
as being ‘helpful or very helpful’ (Figure 3).<br />
• 89% felt that the initial 30-minute consult<br />
with their GP was enough time to discuss<br />
options for getting help.<br />
• 87% rated the assistance to get appointments<br />
with external providers as being ‘helpful or<br />
very helpful’.<br />
• Most patients (82%) referred to external<br />
providers were seen within two weeks, and<br />
91% felt that the waiting time to be seen was<br />
acceptable.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 53
iMPROViNg PERfORMANCE<br />
Patient comments about use <strong>of</strong> the CHAT tool<br />
mainly related to it being simple to use and helpful<br />
in identifying problems:<br />
‘Helped me to positively identify the areas where<br />
I was not coping and required focus.’<br />
‘Simple questions—all part <strong>of</strong> the realisation<br />
process that there was something wrong. It was<br />
good to not have too long with the form to think<br />
too deeply, better to just answer straight away.’<br />
‘<strong>General</strong> questions were asked, nothing too over<br />
the top. It was helpful because it was on paper,<br />
sometimes it’s easier to write things down.’<br />
‘Helpful in the way that it asked you a short, to<br />
the point relevant question for you to respond<br />
with a simple YES/NO answer.’<br />
‘It covered a broad range <strong>of</strong> questions. It was<br />
quick and easy to fill out.’<br />
‘Helped to specify problems, to identify stressors—made<br />
me think about it.’<br />
Some patients remarked that the CHAT form<br />
should be made more available:<br />
‘I felt a little under pressure at the doctor’s because<br />
<strong>of</strong> how I was feeling; maybe if I had taken<br />
the form home to consider it would have been<br />
more comfortable.’<br />
‘Having forms in the waiting room would have<br />
been good.’<br />
‘An idea might be [to put] these forms on display<br />
to increase awareness.’<br />
Patient comments regarding the programme<br />
coordinator’s role were all favourable and related<br />
to proximity and timing <strong>of</strong> referrals:<br />
‘Being new to Auckland, every assistance<br />
was given in finding an appointment close to<br />
where I lived.’<br />
‘<strong>The</strong> whole process was very quick and easy—<br />
superb that help could come close to home. All<br />
organised well.’<br />
‘I didn’t have to do anything. If it was left up to<br />
me I wouldn’t organise anything.’<br />
‘<strong>The</strong> extra time spent and care shown made me<br />
feel that somebody cared about me when I was<br />
very depressed.’<br />
Many patients made very favourable, <strong>of</strong>ten quite<br />
heartfelt remarks about their involvement in this<br />
programme.<br />
‘I hope the programme keeps running—I don’t<br />
know what I would have done if something like<br />
this wasn’t available.’<br />
‘This programme made a huge difference to me<br />
and my family. I felt throughout that I was being<br />
looked after (from my doctor onwards) and the<br />
results were awesome…Huge thumbs up for the<br />
programme from me!’<br />
‘I am very grateful that it exists and that it was<br />
available to me. It made me feel that financial<br />
hardship was dealt with in a sensitive way that<br />
recognised the need for treatment despite this<br />
barrier.’<br />
GP feedback<br />
Thirty-seven <strong>of</strong> the 69 GPs who enrolled their<br />
patients in the PLO programme gave feedback via<br />
a confidential online questionnaire.<br />
• 90% felt that the steps in the programme<br />
were clearly described, and 81%<br />
felt they were easy to implement.<br />
• 76% felt that the programme’s Resource Manual<br />
was ‘useful’ or ‘very useful’ and a further<br />
21% indicated that ‘some parts were useful’.<br />
• 71% introduced the CHAT form to their<br />
patients during the course <strong>of</strong> a consult; the<br />
remainder indicated that their practice nurse<br />
introduced this to a proportion <strong>of</strong> the patients.<br />
Practice receptionists were not involved.<br />
• 70% (<strong>of</strong> the foregoing 71%) gave the CHAT<br />
to those patients they thought would<br />
benefit, i.e. opportunistically. However,<br />
a further 22% selected patients specifically<br />
and invited their participation. No GP<br />
gave the form to every waiting patient.<br />
• 57% felt that the initial 30-minute PLO<br />
54 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
consult was ‘easily’ long enough, and a further<br />
41% felt that it was ‘just’ long enough.<br />
80% felt that the referral process to outside<br />
providers ‘went smoothly’.<br />
36% felt that the final 15-minute follow-up<br />
consult was ‘plenty’ and 55%<br />
felt it was ‘just’ long enough.<br />
Most felt that the role <strong>of</strong> the programme<br />
coordinator was helpful, with<br />
39% regarding this as ‘essential’.<br />
<strong>The</strong> invoicing/payment system relating to<br />
the PLO programme was generally regarded<br />
satisfactorily by GPs, with 79% rating this as<br />
3 or more out <strong>of</strong> 5 (where 5 was ‘very easy’).<br />
94% <strong>of</strong> GPs felt that this programme<br />
enabled their patients to access appropriate<br />
interventions, and 85% felt that<br />
this was within suitable timeframes.<br />
95% indicated that they would continue<br />
their involvement with this programme,<br />
and 74% would increase their<br />
involvement if funding permitted.<br />
GP criticisms related to too much paperwork/<br />
too many forms/needs to be electronic (x3), slow<br />
feedback from external providers (x2), and the<br />
funding period not being long enough (x2).<br />
Provider feedback<br />
Forty-four <strong>of</strong> the 49 external providers who had<br />
patients referred to them through the PLO programme<br />
gave feedback via a confidential online<br />
questionnaire.<br />
• All respondents indicated that the referrals<br />
made by GPs were ‘<strong>entire</strong>ly’ (84%)<br />
or ‘mostly’ (16%) appropriate to the particular<br />
service they provided, and most<br />
felt that the referring information was<br />
always (34%) or mostly (58%) adequate.<br />
• Respondents felt that the timeframe between<br />
the patient seeing the GP and<br />
then being seen by the provider was<br />
‘very timely’ (36%) or ‘timely (61%).<br />
• 78% felt that the role <strong>of</strong> the programme<br />
coordinator was ‘very useful’ in assisting<br />
them, with 68% indicating that the coordinator<br />
was ‘very useful’ in following up<br />
patients who did not attend appointments.<br />
• Overall, 55% <strong>of</strong> providers felt that<br />
the PLO programme was ‘very useful’<br />
as a model <strong>of</strong> care, and a further<br />
29% that it was ‘quite useful’.<br />
‘I believe the programme only touches the surface<br />
<strong>of</strong> the true need. It is evident to me most <strong>of</strong> the<br />
people that came for counselling would not have<br />
accessed help if they did not have this programme.<br />
<strong>The</strong> outcomes for the clients appeared in the main<br />
to have made a significant difference to their lives.’<br />
Lessons and messages<br />
iMPROViNg PERfORMANCE<br />
This pilot programme did not seek to demonstrate<br />
efficacy (upskilling, manage problems,<br />
reduce escalation). Rather, it focused on the<br />
utility <strong>of</strong> the model in primary care—is it practicable;<br />
does it work as a referral pathway within<br />
primary care? It introduced a number <strong>of</strong> new<br />
processes for both GPs and patients. Firstly, it<br />
utilised a now well-validated screening tool, the<br />
CHAT, 7 and, secondly, it gave the GP 30 minutes<br />
<strong>of</strong> dedicated time to discuss this and work<br />
with the patient to select a treatment provider.<br />
Thirdly, a coordinator facilitated the patient’s<br />
entrée to a wide choice <strong>of</strong> treatment providers external<br />
to their GP, and was available to deal with<br />
any follow-up <strong>issue</strong>s with the provider. Fourthly,<br />
the pathway was able to be ‘wrapped up’ by the<br />
patient seeing their GP for a dedicated follow-up<br />
consult to review progress. <strong>The</strong> whole process<br />
was funded, thereby enabling people who otherwise<br />
could not access this amount <strong>of</strong> treatment<br />
time to do so, at an earlier stage in their mental<br />
health/lifestyle problem than would otherwise<br />
be possible under existing referral pathways. It is<br />
a novel approach to an old problem. Does it work<br />
in practice?<br />
Feedback from all parties concerned has clearly<br />
shown widespread approval. Patients regarded<br />
the programme favourably, and some poignant<br />
comments were given in their feedback. It was<br />
important that the processes were practicable<br />
from the GP perspective, and generally the<br />
participating GPs rated the process well; 95%<br />
indicated they would continue their involvement<br />
with the programme. Likewise, external<br />
treatment providers—counsellors, psychologists,<br />
etc.—were generally approving <strong>of</strong> the programme,<br />
with 84% rating it as ‘very’ or ‘quite’ useful and<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 55
iMPROViNg PERfORMANCE<br />
ACkNOwLEDgEMENTS<br />
<strong>The</strong> authors warmly<br />
thank Maureen Langwell,<br />
Programme Coordinator,<br />
Primary Lifestyle Options<br />
at Harbour Health PHO,<br />
for her enthusiastic work<br />
on this project. <strong>The</strong><br />
support <strong>of</strong> participating<br />
Harbour Health and<br />
HealthWEST PHO GPs is<br />
gratefully acknowledged.<br />
This study was funded<br />
by the Waitemata<br />
District Health Board.<br />
COMPETiNg iNTERESTS<br />
None declared.<br />
100% felt they were referred appropriate patients<br />
for the services they provided.<br />
As such, the basic model does not require major<br />
changes as all processes were acceptable and<br />
practicable for the majority <strong>of</strong> patients, providers<br />
and GPs. However, there are some caveats to address<br />
if this programme is to move forward. Some<br />
patients felt under pressure at the time <strong>of</strong> consultation,<br />
preferring to take the CHAT home to answer;<br />
in future they need to be given this option.<br />
Completion <strong>of</strong> the programme by attending the<br />
follow-up GP consult was variable, and has continued<br />
to be so post–30 June. This appears to be<br />
redundant for those who were referred internally,<br />
i.e. consulted their GP for interventions or when<br />
they have had their needs adequately met by an<br />
external provider who has written a report to the<br />
GP. In future, this will be an optional component<br />
<strong>of</strong> the model. Moving to an online version was<br />
suggested by a number <strong>of</strong> GPs, so this too will be<br />
available in the next iteration.<br />
In conclusion, the Primary Lifestyle Options pilot<br />
appears to be well regarded by participants—<br />
patients, GPs and other treatment providers—and<br />
is realistic and practicable. It could be easily taken<br />
up by other PHOs, requiring only local adaptation<br />
<strong>of</strong> material in the Resource Manual. This<br />
programme enables identification in the primary<br />
care setting <strong>of</strong> mild to moderate mental health or<br />
lifestyle problems and initiation <strong>of</strong> a treatment<br />
pathway that, in many cases at least, would not<br />
otherwise occur.<br />
References<br />
1. MaGPIe Research Group. <strong>The</strong> nature and prevalence <strong>of</strong><br />
psychological problems in <strong>New</strong> <strong>Zealand</strong> primary healthcare:<br />
a report on Mental Health and <strong>General</strong> Practice<br />
Investigation (MaGPIe). NZ Med J 2003;116:U379<br />
2. Hutton C, Gunn J. Do longer consultations improve the<br />
management <strong>of</strong> psychological problems in general practice?<br />
A systematic literature review. BMC Health Serv Res<br />
2007:7:71.<br />
3. Collings S, MaGPIe Research Group. Disability and the<br />
detection <strong>of</strong> mental disorder in primary care. Soc Psych<br />
Psychiatr Epidemiol 2005;40:994–1002.<br />
4. <strong>The</strong> MaGPIe Research Group. <strong>The</strong> effectiveness <strong>of</strong> casefinding<br />
for mental health problems in primary care. Br J<br />
Gen Pract 2005;55:665–9.<br />
5. Goodyear-Smith F, Coupe N, Arroll B, Elley C, Sullivan<br />
S, McGill A. Case-finding <strong>of</strong> lifestyle and mental health<br />
problems in primary care: validation <strong>of</strong> the ‘CHAT’. Br J<br />
Gen Pract 2008;58:26–31.<br />
6. Arroll B, Goodyear-Smith F, Kerse N, Fishman T, Gunn J.<br />
Effect <strong>of</strong> the addition <strong>of</strong> a ‘help’ question to two screening<br />
questions on specificity for diagnosis <strong>of</strong> depression in<br />
general practice: diagnostic validity study. BMJ 2005;<br />
331(7521):884.<br />
7. Lyness JM, Heo M, Datto CJ. Outcomes <strong>of</strong> minor and subsyndromal<br />
depression among elderly patients in primary<br />
care settings. Ann Intern Med 2006;144(7):496–504.<br />
8. Hawker D. Increasing initial attendance at mental health<br />
out-patient clinics: opt-in systems and other interventions.<br />
Psych Bull 2007;31:179–82.<br />
9. MacDonald J, Brown N, Ellis P. Using telephone prompts<br />
to improve initial attendance at a community mental health<br />
center. Psychiatr Serv 2000;51:812–4.<br />
10. Ohayon MM, Roth T. Place <strong>of</strong> chronic insomnia in the<br />
course <strong>of</strong> depressive and anxiety disorders. J Psychiatric<br />
Res 2003;37:9–15.<br />
We were shocked to hear <strong>of</strong> Jill Calveley’s tragic, unexpected death on 30 December. As well as her role as the Clinical Director<br />
<strong>of</strong> Harbour Health PHO, Jill has made significant contributions in numerous parts <strong>of</strong> the health sector as a rural GP, within primary<br />
and secondary care organisations, the Accident Compensation Corporation and NGOs. As well as general practice, Jill had<br />
qualifications in epidemiology, public health and philosophy and was able to engage with the health sector from a wide range <strong>of</strong><br />
perspectives. She passionately believed that the sole purpose <strong>of</strong> the health service is to improve the health <strong>of</strong> people. She brought<br />
her compassion and her critical appraisal skills to all her many roles. Her legacy is huge and she is sadly missed—Editor.<br />
56 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
gPs should prescribe more<br />
benzodiazepines for the elderly<br />
yES<br />
We should stop moralizing and start prescribing<br />
benzodiazepines when required (for the<br />
elderly and others).<br />
I am currently cautious about prescribing<br />
benzodiazepines as I am concerned that, if I am<br />
too liberal, my colleagues may think I am a low<br />
quality physician. I am sure this is the prevailing<br />
mood amongst GPs, although I sense that<br />
psychiatrists are less cautious than we are. Many<br />
years ago I was involved in a practice where we<br />
(the new GPs) thought too many <strong>of</strong> the patients<br />
were on benzodiazepines and proceeded to wean<br />
them <strong>of</strong>f. This was a difficult task that required<br />
a lot <strong>of</strong> confrontation and conflict with the<br />
patients and, in many cases, we were unsuccessful<br />
in ‘assisting’ them to stop. <strong>The</strong> patients were<br />
functioning well and the problem seemed to be<br />
ours not theirs. <strong>The</strong>ir only concern was getting<br />
their repeat prescriptions as they realised they<br />
would have uncomfortable nights <strong>of</strong> sleep if<br />
they stopped them suddenly. Thus the ‘harm’<br />
for these patients was my/our high moral stance<br />
<strong>of</strong> thinking they should stop. Over the years I<br />
have seen many patients on long-term benzodiazepines,<br />
rarely prescribed by myself, and have<br />
had to suppress the mild irritation I feel if my<br />
colleagues start patients on these medications.<br />
In recent times I have had a rethink. I recently<br />
wrote a chapter on anxiety for a British medical<br />
textbook (in press) and was aware that benzodiazepines<br />
are effective for anxiety but there is<br />
concern about habituation and ‘addiction’. <strong>The</strong><br />
<strong>issue</strong> came to light recently when I was confronted<br />
by a 71-year-old patient who was having<br />
nightmares so severe they were affecting her the<br />
next day. She was not clinically depressed, nor<br />
did she have anxiety on gold standard questionnaires.<br />
I discussed with her the options. She<br />
could try a low dose tricyclic, a benzodiazepine<br />
or even quetiapine. I said the benzodiazepine<br />
would probably eliminate her nightmares but she<br />
would probably be on it forever and that when<br />
she was in her 80s she may be more prone to fall<br />
and break her hip (the numbers needed to harm,<br />
i.e break a hip in this situation is 91). 1 She was<br />
not concerned by the falling and I felt I had fully<br />
informed her <strong>of</strong> her options. Even more recently<br />
I spoke to an 87-year-old man who is on 0.5mg <strong>of</strong><br />
lorazepam prescribed by his GP. He is sleeping<br />
well now, but previously complained endlessly<br />
about his poor sleep. He has also had a number<br />
<strong>of</strong> falls since starting this medication. I asked<br />
him what would he prefer: having a good night’s<br />
sleep and having falls, or not sleeping and having<br />
While evidence can help inform best practice, it needs to be placed in context.<br />
<strong>The</strong>re may be no evidence available or applicable for a specific patient with<br />
his or her own set <strong>of</strong> conditions, capabilities, beliefs, expectations and social<br />
circumstances. <strong>The</strong>re are areas <strong>of</strong> uncertainty, ethics and aspects <strong>of</strong> care for which<br />
there is no one right answer. <strong>General</strong> practice is an art as well as a science. Quality<br />
<strong>of</strong> care also lies with the nature <strong>of</strong> the clinical relationship, with communication and<br />
with truly informed decision-making. <strong>The</strong> BACk to BACk section stimulates<br />
debate, with two pr<strong>of</strong>essionals presenting their opposing views regarding a clinical,<br />
ethical or political <strong>issue</strong>.<br />
Bruce Arroll<br />
BACk TO BACk<br />
Bruce Arroll<br />
MBChB, PhD, FRNZCGP<br />
Pr<strong>of</strong>essor <strong>of</strong> <strong>General</strong><br />
Practice and Primary<br />
Health Care,<br />
University <strong>of</strong> Auckland,<br />
Private Bag 92019,<br />
Auckland;<br />
b.arroll@<br />
auckland.ac.nz<br />
Ngaire Kerse<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 57<br />
BACk to BACk this <strong>issue</strong>:
BACk TO BACk<br />
fewer/no falls? He chose the former. He now goes<br />
to the toilet at night with his walking stick to ensure<br />
that he does not fall. I have asked a number<br />
<strong>of</strong> elderly patients about their benzodiazepines<br />
and they all prefer the good night’s sleep. Sleeping<br />
poorly is a considerable bother to those that<br />
suffer from it and the promise <strong>of</strong> sleeping well<br />
is immediate and welcomed. I would contend<br />
most would choose the short-term option against<br />
the hazard <strong>of</strong> a (small chance <strong>of</strong>) fractured hip at<br />
some distant point in the future.<br />
Insomnia and anxiety are <strong>of</strong>ten chronic conditions.<br />
It is interesting to consider that we consider<br />
diabetes a chronic condition and are happy to<br />
give long-term metformin, aspirin and statins to<br />
all, in spite <strong>of</strong> the (small) harms that accompany<br />
Insomnia is only a trivial condition<br />
for those who don’t have it<br />
these medications. Anxiety is a long-term condition,<br />
yet when standard treatments fail, we are<br />
reluctant to consider long-term benzodiazepine.<br />
Is this moralizing on our part or perhaps can<br />
we be a bit more rational? We know that the<br />
numbers needed to treat for cognitive behavioural<br />
therapy are about five for anxiety 2 and that for<br />
SSRIs they are also about five. 3 For some patients<br />
no other treatment works, so in those situations<br />
we should consider <strong>of</strong>fering benzodiazepines.<br />
We need to fully inform the patients. We need<br />
to say: this will help you sleep, but you may not<br />
be able to stop taking it (hence you will be on it<br />
indefinitely) and you may be more likely to fall<br />
when you are older. <strong>The</strong> risk <strong>of</strong> breaking your<br />
hip when not taking these medications (antidepressants<br />
and anxiolytics) is 10.1% and with these<br />
medications 11.2%. 1 What would you like to do?<br />
I would imagine most insomniac elderly patients<br />
would go for the benzodiazepines and take the<br />
risk. Insomnia is only a trivial condition for those<br />
who don’t have it. Philosophically I am not sure<br />
I want the whole nation on benezodiazepines as<br />
in Aldous Huxley’s Brave <strong>New</strong> World where the<br />
citizens were on their soma, but anxiety and insomnia<br />
are two conditions that are very prevalent<br />
in primary care (4.9% <strong>of</strong> men over 65 and 7.8%<br />
<strong>of</strong> women over 65 have anxiety 4 ) and 44% report<br />
insomnia from our unpublished data (2008).<br />
How should we do it? <strong>The</strong>re is evidence that falls<br />
are more likely in the first five days <strong>of</strong> starting<br />
benzodiazepines (odds ratio 3.43), but after 30<br />
days this risk becomes non-significant. 5 What I<br />
would take from this is that we should start with<br />
a low dose (e.g. 0.25mg lorazepam) and slowly<br />
increase as necessary. We should also monitor the<br />
risk <strong>of</strong> falling and encourage the use <strong>of</strong> walkers<br />
and walking sticks.<br />
Summary<br />
For the elderly (and for any age) I think it is<br />
worth trying other treatments for insomnia and<br />
anxiety. Where those treatments do not work, I<br />
think we should abandon our moral superiority<br />
and fully inform patients about a legal and therapeutically-effective<br />
medication that has some<br />
adverse effects (like any medication). We need to<br />
be more patient-focused and less concerned about<br />
what our colleagues think <strong>of</strong> us. We should stop<br />
moralizing and start prescribing benzodiazepines<br />
when required (for the elderly and others).<br />
References<br />
1. Robbins J, Aragaki AK, Kooperberg C, Watts N, Wactawski-Wende<br />
J, Jackson RD, LeB<strong>of</strong>f MS, Lewis CE, Chen Z,<br />
Stefanick ML, Cauley J. Factors associated with 5-year<br />
risk <strong>of</strong> hip fracture in postmenopausal women. JAMA<br />
2007;298(20):2389–98.<br />
2. http://clinicalevidence.bmj.com.ezproxy.auckland.ac.nz/<br />
ceweb/conditions/meh/1002/1002_I1.jsp; accessed 27<br />
June 2008.<br />
3. Kapczinski F, Lima MS, Souza JS, Cunha A, Schmitt<br />
R. Antidepressants for generalized anxiety disorder.<br />
Cochrane Database <strong>of</strong> Sys Rev 2003, Issue 2. Art. No.:<br />
CD003592. DOI: 10.1002/14651858.CD003592.<br />
4. MaGPIe Research Group. <strong>The</strong> nature and prevalence<br />
<strong>of</strong> psychological problems in <strong>New</strong> <strong>Zealand</strong> primary<br />
healthcare: a report on mental health and general practice<br />
investigation (MAGPIE). NZ Med J 2003;116:1171–1185.<br />
5. H<strong>of</strong>fmann, F. Glaeske, G. <strong>New</strong> use <strong>of</strong> benzodiazepines and<br />
the risk <strong>of</strong> hip fracture: A case-crossover study. Z Gerontol<br />
Geriatr 2006;39(2):143–8.<br />
58 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
gPs should prescribe more<br />
benzodiazepines for the elderly<br />
NO<br />
<strong>The</strong> answer is undoubtedly ‘no’, we are using too<br />
many <strong>of</strong> these dangerous, unnecessary medications<br />
and should be prescribing fewer. Resist<br />
the urge to take the easy way out—undoubtedly<br />
proposed by Pr<strong>of</strong>essor Arroll—and to use these<br />
drugs for inappropriate indications where the<br />
risks clearly outweigh the benefits. <strong>The</strong> risk for<br />
older people from using benzodiazepines is high.<br />
How much are we using them?<br />
Taking residential care as a key setting: 46% <strong>of</strong><br />
residents in 1999 took psychotropic medication. 1<br />
In 2005, 25% were taking short-acting sedatives, 2<br />
with benzodiazepines being one <strong>of</strong> the most commonly<br />
used. In the community it is more difficult<br />
to gauge accurate estimates <strong>of</strong> benzodiazepine use.<br />
<strong>The</strong> age standardised prevalence rate <strong>of</strong> benzodiazepine<br />
use in Auckland general practice was 3.4%<br />
for patients over 20 years <strong>of</strong> age in 1992; however<br />
use was predominantly in the elderly (70% were<br />
over 60 years <strong>of</strong> age) and female (62.5%).<br />
In the 2004–2005 Australian National Health<br />
Survey, anxiolytics, hypnotics and sedative<br />
prescriptions make up approximately 4–5% <strong>of</strong> the<br />
total prescriptions written by Australian general<br />
practitioners and 10% <strong>of</strong> patients used medication<br />
for anxiety or nerves. 3<br />
How much should we be using them?<br />
Anxiety disorder may be one <strong>of</strong> the only appropriate<br />
indications, where the benefits outweigh<br />
the risks <strong>of</strong> prescribing benzodiazepines.<br />
<strong>The</strong> prevalence <strong>of</strong> anxiety in the community is<br />
14.8% over one year and only 9.8 for the previous<br />
month. 4 <strong>The</strong> MaGPIe study primary care mental<br />
health survey in <strong>New</strong> <strong>Zealand</strong> shows that 15% <strong>of</strong><br />
all people get treated with psychotropic medication;<br />
5 however 12-month prevalence <strong>of</strong> anxiety<br />
disorder in general practice attenders aged 65+<br />
was only 4.9% for men and 7.8% for women in<br />
2003. <strong>The</strong>re is a clear mismatch between diagnosis<br />
and prescribing and it is likely that much <strong>of</strong><br />
the benzodiazepines use observed in community<br />
dwelling older people is related to treatment <strong>of</strong><br />
sleep disorder.<br />
what’s wrong with using<br />
them in late life?<br />
<strong>The</strong>re is little right with using benzodiazepines<br />
in late life. Reactions to benzodiazepines are<br />
<strong>of</strong>ten paradoxical and long-term management is<br />
notoriously problematic. 6 Apart from the risk <strong>of</strong><br />
confusion and development <strong>of</strong> tolerance, falls are<br />
the most problematic result <strong>of</strong> benzodiazepine<br />
use. <strong>The</strong> effects <strong>of</strong> hypnotics on balance, gait and<br />
equilibrium are the consequence <strong>of</strong> differential<br />
negative impacts on vigilance and cognitive functions,<br />
and are highly dose- and time-dependent.<br />
It is not surprising that almost no guideline<br />
recommends use <strong>of</strong> benzodiazepines for older<br />
people, i.e. Beers criteria for appropriate use <strong>of</strong><br />
medications. 7<br />
More importantly, the risk <strong>of</strong> fracture is increased<br />
by over 30%. <strong>The</strong> RR <strong>of</strong> fracture associated<br />
with use <strong>of</strong> benzodiazepines was 1.34 (95%<br />
CI 1.24, 1.45) in one systematic review <strong>of</strong> 23<br />
studies. 8 While any benzodiazepines carried the<br />
risk, it was higher for those taking the short-acting<br />
high-potency benzodiazepine (IRR, 1.27; 95%<br />
CI, 1.01–1.59), during the first two weeks after<br />
starting a benzodiazepine (IRR, 2.05; 95% CI,<br />
1.28–3.28), during the second two weeks after<br />
starting a benzodiazepine (IRR, 1.88; 95% CI,<br />
1.15–3.07), and for continued use (IRR, 1.18; 95%<br />
CI, 1.03–1.35), so short half-life benzodiazepines<br />
BACk TO BACk<br />
Ngaire kerse<br />
MBChB, PhD, FRNZCGP<br />
Associate Pr<strong>of</strong>essor <strong>of</strong><br />
<strong>General</strong> Practice and<br />
Primary Health Care,<br />
University <strong>of</strong> Auckland,<br />
Private Bag 92019,<br />
Auckland;<br />
n.kerse@auckland.ac.nz<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 59
BACk TO BACk<br />
are not safer than long half-life benzodiazepines.<br />
Hip fracture risk is highest during the first two<br />
weeks after starting a benzodiazepine. Those older<br />
people that just want something in the shortterm<br />
as a result <strong>of</strong> a recent stress are at highest<br />
risk <strong>of</strong> hip fracture from your prescriptions. Even<br />
with a reasonably high NNT, hip fracture is a<br />
devastating event. Less than 50% <strong>of</strong> those with<br />
hip fracture regain pre-fracture function and 20%<br />
die within 12 months after hip fracture.<br />
In a large group <strong>of</strong> cognitively normal Canadians,<br />
the frequency <strong>of</strong> falls was 60% greater in benzodiazepine<br />
users compared to non-users. Our own<br />
Pr<strong>of</strong>essor John Campbell successfully reduced the<br />
risk <strong>of</strong> falls to 18% (an NNT to cause a fall <strong>of</strong> 2),<br />
in an RCT <strong>of</strong> older people on benzodiazepines,<br />
by reducing the dose <strong>of</strong> benzodiazepine gradually<br />
over six months and continuing a placebo tablet.<br />
Unfortunately after unblinding, half <strong>of</strong> the<br />
older people in the intervention group returned<br />
to the GP to get their prescription successfully<br />
renewed! Systematic reviews also identified that<br />
chronic consumers <strong>of</strong> benzodiazepines are more<br />
susceptible to the appearance and progression <strong>of</strong><br />
many acute and chronic diseases (infectious and<br />
malignant diseases).<br />
<strong>The</strong> risk <strong>of</strong> using this medication usually far outweighs<br />
the benefits and use should be restricted to<br />
those with moderate to severe anxiety disorders.<br />
Are they needed for insomnia?<br />
Benzodiazepines do improve sleep; however more<br />
patients receiving benzodiazepines reported adverse<br />
effects, especially daytime drowsiness and<br />
dizziness or light-headedness (common odds ratio<br />
1.8, 95% CI 1.4 to 2.4) compared with other sleep<br />
treatments. Cognitive function decline including<br />
memory impairment was reported in several <strong>of</strong><br />
the studies and Zopiclone was not found to be superior<br />
to benzodiazepines on any <strong>of</strong> the outcome<br />
measures examined.<br />
A large systematic review compared sleep<br />
pharmacotreatments. Benzodiazepines were no<br />
better than non-benzodiazepines in reducing time<br />
to sleep. All drug groups had a statistically significant<br />
higher risk <strong>of</strong> harm compared to placebo, but<br />
benzodiazepines had the highest risk difference.<br />
Non-pharmacological treatment for insomnia is<br />
very effective. When identified accurately, primary<br />
insomnia responds best to sleep restriction<br />
techniques and medications are seldom needed for<br />
those in late life. If it is not primary insomnia<br />
then an underlying disorder, such as pain,<br />
depression or restless leg syndrome should be<br />
sought and appropriate treatment started.<br />
Can we stop them?<br />
It is relatively easy to encourage stopping benzodiazepines.<br />
A simple letter to patients using<br />
these drugs may be effective in reducing useage.<br />
Recognised tapering protocols are available and<br />
reasonably successful. Older people sleep less and<br />
relaxation and sleep hygiene along with sleep<br />
restriction can be very successful in improving<br />
satisfaction with sleep. Take it slow and make<br />
sure the older person wants to stop.<br />
So don’t be persuaded by the Pr<strong>of</strong>essor. We are<br />
currently using too many benzodiazepines in<br />
older people and exposing them to unacceptable<br />
risk associated with their use.<br />
We are definitely NOT under-prescribing<br />
benzodiazepines for older people.<br />
References<br />
1. Kerse N. Medication use in residential care. NZ Fam Phys<br />
2005;32:251–5.<br />
2. Peri K, Kerse N, Kiata L, Wilkinson T, Robinson E, Parsons<br />
J, et al. Promoting independence in residential care:<br />
Successful recruitment for a randomised controlled trial.<br />
JAMDA. 2007:doi10.1016/j.jamda.2007.11.008.<br />
3. Australian Institute <strong>of</strong> Health and Welfare. <strong>General</strong> practice<br />
activity in Australia 2004-05. Canberra: AIHW; 2005.<br />
4. Browne MO, Wells J, Scott K. Te Rau Hinengaro: <strong>The</strong> <strong>New</strong><br />
<strong>Zealand</strong> Mental Health Survey. Wellington: Ministry <strong>of</strong><br />
Health; 2006.<br />
5. Bushnell J, McLeod D, Dowell A, Salmond C, Ramage S,<br />
Collings S, et al. <strong>The</strong> treatment <strong>of</strong> common mental health<br />
problems in general practice. Fam Pract 2006;23(1):53–9.<br />
6. Mathew VM, Dursun SM, Reveley MA. Increased aggressive,<br />
violent, and impulsive behaviour in patients during<br />
chronic-prolonged benzodiazepine use. Can J Psychiatr -<br />
Revue Canadienne de Psychiatrie 2000 Feb;45(1):89–90.<br />
7. Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR,<br />
Beers MH. Updating the Beers criteria for potentially inappropriate<br />
medication use in older adults: results <strong>of</strong> a US consensus<br />
panel <strong>of</strong> experts. Arch Int Med 2003;163:2716–24.<br />
8. Takkouche B, Montes-Martinez A, Gill SS, Etminan M.<br />
Psychotropic medications and the risk <strong>of</strong> fracture: a metaanalysis.<br />
Drug Safety 2007;30(2):171–84.<br />
(Further references available from: n.kerse@auckland.ac.nz)<br />
60 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Patient Oriented Evidence that Matters<br />
Psychological interventions reduce onset<br />
<strong>of</strong> depression<br />
CLiNiCAL qUEsTiON: Do behavioural interventions reduce<br />
the risk <strong>of</strong> new onset depression?<br />
BOTTOM LiNE: Behavioural interventions to prevent depression<br />
reduce the incidence <strong>of</strong> newly diagnosed depression. Most<br />
<strong>of</strong> the studies included in this report were <strong>of</strong> cognitive behavioural<br />
therapy interventions in group format for individuals at<br />
increased risk for major depression. (LOE=1a-)<br />
REfERENCE: Cuijpers P, van Straten A, Smit F, Mihalopoulos<br />
C. Beekman A. Preventing the onset <strong>of</strong> depressive distorders:<br />
A meta-analytic review <strong>of</strong> psychological interventions. Am J<br />
Psychiatry 2008;165(10):1272–1280.<br />
sTUdy dEsigN: Meta-analysis (randomised controlled trials)<br />
fUNdiNg: Unknown/not stated<br />
ALLOCATiON: Concealed<br />
sETTiNg: Various (meta-analysis)<br />
syNOPsis: This is a meta-analysis <strong>of</strong> randomised trials to<br />
prevent depression using behavioural interventions. <strong>The</strong><br />
primary outcome was incident cases <strong>of</strong> depression. Because the<br />
length <strong>of</strong> the studies varied, the incidence rates were calculated<br />
by the authors in person-years. A total <strong>of</strong> 19 studies with 5806<br />
participants met inclusion criteria, one <strong>of</strong> which tested three<br />
different preventive interventions, for a total <strong>of</strong> 21 comparisons.<br />
Seven studies were about preventing postpartum depression,<br />
and the rest included various other targets, such as school and<br />
primary care settings. <strong>The</strong>re were three types <strong>of</strong> prevention;<br />
universal (two), selective programmes aimed at high-risk groups<br />
(11), and prevention aimed at individuals with depressive<br />
symptoms who do not meet the criteria for a diagnosis <strong>of</strong> major<br />
depression (eight). <strong>The</strong> majority <strong>of</strong> interventions were cognitive<br />
behavioural therapy (15). Group format was used in 18<br />
comparisons. <strong>The</strong> incidence ratio <strong>of</strong> new depression per<br />
person-year was 0.78 (95% CI, 0.65–0.93), indicating a reduction<br />
<strong>of</strong> the incidence <strong>of</strong> depressive disorders by 22% in the intervention<br />
groups compared with control groups. <strong>The</strong> authors<br />
calculated the number needed to treat as 22.<br />
© 1995–2009 John Wiley & Sons Inc. All Rights Reserved. www.infopoems.com<br />
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
CBT is effective for self-harm<br />
CLiNiCAL qUEsTiON: Is cognitive behavioural therapy an<br />
effective treatment for self-harm?<br />
BOTTOM LiNE: A brief series <strong>of</strong> cognitive behavioural therapy<br />
(CBT) sessions reduces the risk <strong>of</strong> self-harm and improves a<br />
number <strong>of</strong> other important psychological outcomes. (LOE=1b-)<br />
REfERENCE: Slee N, Garnefski N, van der Leeden R,<br />
Arensman E, Spinhoven P. Cognitive-behavioural intervention<br />
for self-harm: randomised controlled trial. Br J Psych<br />
2008;192:202–211.<br />
sTUdy dEsigN: Randomised controlled trial (nonblinded)<br />
fUNdiNg: Government<br />
sETTiNg: Outpatient (specialty)<br />
ALLOCATiON: Concealed<br />
POEMs<br />
syNOPsis: Self-harm is a poorly studied but psychologically<br />
devastating condition. In this study, 90 patients in the Netherlands<br />
with a recent history <strong>of</strong> self-harm were randomised to<br />
either CBT or treatment as usual. Of the 48 patients assigned<br />
to CBT, only 40 began the therapy but all 40 attended all 12<br />
sessions (the first 10 were weekly). Eight <strong>of</strong> 42 patients in the<br />
treatment-as-usual group were lost to follow-up because <strong>of</strong> suicide,<br />
severe psychological problems, or other reasons. Analysis<br />
was by modified intention to treat; the patients who did not<br />
begin the CBT were excluded. Patients were between the ages<br />
<strong>of</strong> 15 years and 35 years, and more than 90% were women. At<br />
nine months, the number <strong>of</strong> self-harm episodes in the previous<br />
three months declined more in the CBT group, from 14.4<br />
to 1.2, compared with a decline from 11.6 to 4.6 in the usual<br />
treatment group (P < .05). Secondary outcomes (depression,<br />
anxiety, self-esteem, helplessness, problem-solving, unlovability,<br />
and poor distress tolerance) all improved significantly more<br />
in the CBT group.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 61
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
PEARLs COCHRANE CORNER<br />
String <strong>of</strong> PEARLS<br />
Practical Evidence About Real Life Situations<br />
PEARLS are succinct summaries <strong>of</strong> Cochrane systematic Reviews<br />
for primary care practitioners—developed by the Cochrane Primary<br />
Care Field, <strong>New</strong> <strong>Zealand</strong> Branch <strong>of</strong> the Australasian Cochrane Centre<br />
at the Department <strong>of</strong> <strong>General</strong> Practice and Primary Health Care,<br />
University <strong>of</strong> Auckland, funded by the <strong>New</strong> <strong>Zealand</strong> Guidelines Group<br />
and published in NZ Doctor.<br />
Psychological therapy based on CBT is effective<br />
short-term treatment for generalised anxiety disorder<br />
Musical therapy for depression may improve mood<br />
Psychosocial & psychological interventions are<br />
effective for postpartum depression<br />
Antidepressants are effective for neuropathic pain<br />
No evidence supports use <strong>of</strong> antidepressants for<br />
nonspecific low-back pain<br />
CBT for tinnitus improves quality <strong>of</strong> life<br />
CBT is possible treatment for children with recurrent<br />
abdominal pain<br />
disCLAiMER: PEARLs are for educational use only and are not meant<br />
to guide clinical activity, nor are they a clinical guideline.<br />
Benzodiazepines may hasten<br />
improvement in major<br />
depression for up to six weeks<br />
Bruce Arroll MBChB, PhD, FRNZCGP, Pr<strong>of</strong>essor <strong>of</strong> <strong>General</strong> Practice<br />
and Primary Health Care, University <strong>of</strong> Auckland, Private Bag 92019,<br />
Auckland; Email: b.arroll@auckland.ac.nz<br />
THE PROBLEM: Depression <strong>of</strong>ten presents with anxiety. <strong>The</strong><br />
rate <strong>of</strong> anxiety comorbidity among patients with depression<br />
varies from 33% to 85%. Reviews <strong>of</strong> randomised controlled<br />
trials show, however, that anxiolytic benzodiazepines, with<br />
the possible exception <strong>of</strong> some triazolo-benzodiazepines for<br />
mild to moderate depression, are less effective than standard<br />
antidepressants in treating major depression. <strong>The</strong> advantages <strong>of</strong><br />
adding benzodiazepines to antidepressants are unclear. <strong>The</strong>re<br />
are suggestions that benzodiazepines may lose their efficacy<br />
with long-term administration and that their chronic use carries<br />
risks <strong>of</strong> dependence.<br />
CLiNiCAL BOTTOM LiNE: Benzodiazepines are effective<br />
in improving depression symptoms for the first six weeks,<br />
but after that appear to have no benefit. <strong>The</strong>y seem to work<br />
in addition to tricylic antidepressants such as imipramine in<br />
moderate to high doses (100 to 145mg) with triazolam 0.5mg<br />
and fluoxetine 20 to 40mg with clonazepam 0.5 to 1mg. <strong>The</strong>re<br />
are concerns about the risk <strong>of</strong> hip fracture in the elderly but<br />
the NNH=90 for those on antidepressants/anxiolytics. 1<br />
Table 1. Major depression<br />
Benzodiazepines<br />
in addition to<br />
antidepressants<br />
Success Evidence Harms<br />
At six weeks<br />
NNT=8<br />
(range 5 to 29)<br />
in terms <strong>of</strong><br />
improved<br />
symptoms<br />
NNT = numbers needed to treat<br />
NNH = numbers needed to harm<br />
References<br />
Cochrane<br />
review 2<br />
No additional<br />
benefit after six<br />
weeks plus risk <strong>of</strong><br />
addiction.<br />
NNH =90 for hip<br />
fracture in elderly<br />
1. Robbins J. Aragaki AK. Kooperberg C. Watts N. Wactawski-Wende J. Jackson<br />
RD. LeB<strong>of</strong>f Ms. Lewis CE. Chen Z. stefanick ML. Cauley J. Factors associated<br />
with 5-year risk <strong>of</strong> hip fracture in postmenopausal women. JAMA 2007;<br />
298(20):2389–98.<br />
2. Furukawa TA, streiner DL, Young LT, Kinoshita Y. Antidepressants plus benzodiazepines<br />
for major depression. Cochrane Database <strong>of</strong> syst Rev 2001; Issue 3.<br />
Art. No.: CD001026. DOI: 10.1002/14651858.CD001026. All people residing<br />
in <strong>New</strong> <strong>Zealand</strong> have access to the Cochrane Library via the Ministry website<br />
www.moh.govt.nz/cochranelibrary<br />
62 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Bridging two worlds in the interview process<br />
—the psychiatric assessment and Maori in primary care<br />
Pamela Ara Bennett MBChB, FRANZCP<br />
Mental health is an area <strong>of</strong><br />
particular concern for Maori.<br />
Pr<strong>of</strong>essor Mason Durie has<br />
stated that mental health is the greatest<br />
health problem facing Maori in the first<br />
two decades <strong>of</strong> this century. 1<br />
<strong>The</strong> assessment <strong>of</strong> mental health <strong>issue</strong>s<br />
across cultures is recognised as being<br />
fraught with difficulty. Psychiatry is<br />
unlike other medical disciplines in that<br />
the diagnosis <strong>of</strong> functional psychiatric<br />
disorders is based <strong>entire</strong>ly on the clinical<br />
interaction. <strong>The</strong> DSM-IV acknowledges<br />
difficulties may be encountered when<br />
applying DSM-IV diagnostic criteria<br />
across cultures, and has produced an<br />
outline for cultural formulations in<br />
psychiatric assessment. 2<br />
This paper aims to assist the primary<br />
care clinician to (i) develop empathic<br />
therapeutic relationships with their<br />
Maori patients and whanau through<br />
acknowledging difference and building<br />
CORREsPONdENCE TO:<br />
Pamela Ara Bennett<br />
Psychiatrist and senior<br />
Lecturer, Te Kupenga Hauora<br />
Maori, school <strong>of</strong> Population<br />
Health, <strong>The</strong> University<br />
<strong>of</strong> Auckland, PB 92019,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
pam.bennett@auckland.ac.nz<br />
Pounamu<br />
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
the notion <strong>of</strong> cultural difference into the<br />
clinical assessment process, and (ii) make<br />
diagnostic and management decisions<br />
based on their clinical knowledge, enhanced<br />
by such therapeutic relationships.<br />
To achieve these aims I use a fictional case<br />
history, based on my own clinical experience,<br />
and a modified version <strong>of</strong> the DSM-<br />
IV outline for cultural formulation. 3<br />
Case history<br />
Matiu, a tall handsome 17-year-old,<br />
comes into your <strong>of</strong>fice with his Aunt<br />
Estelle and older brother Manu. Matiu<br />
sits down in the chair the furthest away<br />
and looks at the ground. He obviously<br />
is not happy and says nothing. Auntie<br />
introduces herself and her two nephews.<br />
She is a retired social worker who<br />
worked in a large city hospital. She asks<br />
if the other whanau members outside<br />
may come in so the meeting can begin<br />
with karakia. An older man stands and<br />
prays in Maori. Whanau members then<br />
introduce themselves. You introduce<br />
yourself from a pr<strong>of</strong>essional perspective—‘I<br />
am Dr McDonald. I have been<br />
working as a general practitioner in this<br />
practice for six years. I spent three years<br />
working down south in Hokitika.’<br />
Auntie begins Matiu’s story. Matiu lives<br />
with his mother and older brother in<br />
MAoRi PRiMARy HEALtH cARE tREASuRES<br />
Pounamu (greenstone) is the most precious <strong>of</strong> stone to Maori.<br />
POUNAMU<br />
a large city. His parents divorced years<br />
ago. Mother never remarried. Two elder<br />
sisters are married and live elsewhere.<br />
Matiu is in his last year <strong>of</strong> secondary<br />
school, excels in rugby, dreams <strong>of</strong> being<br />
an All Black. He has many friends and<br />
was ‘going steady’ with Ara. Brother<br />
Manu is doing well at university after<br />
a year overseas, on a scholarship. Manu<br />
explains Matiu began to withdraw into<br />
himself about nine months ago (stayed<br />
in his bedroom, stopped football, broke<br />
with Ara, refused to speak to anyone).<br />
He was suspicious <strong>of</strong> everyone (mother,<br />
sisters, football coach, friends). He believed<br />
‘everyone was against him’. Matiu<br />
told Manu that he was hearing voices<br />
talking about him, arguing about him<br />
and telling him he was no good. <strong>The</strong><br />
voices were telling him that he might<br />
as well kill himself. Sometimes Matiu<br />
thought it was the neighbours outside<br />
his window, but he was never able to<br />
catch them, and the same voices were<br />
giving him the same messages through<br />
music so he had stopped listening. He<br />
was very distressed. Mother said Matiu<br />
had stopped eating and had been pacing<br />
the floor most nights, mumbling to himself.<br />
She says he is a very good boy and<br />
had never acted like this before.<br />
Until this stage in the proceedings you<br />
have been encouraging the family to tell<br />
their story and listening.<br />
‘Ahakoa he iti, he pounamu’<br />
(Although it is small, it is valuable)<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 63
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
POUNAMU<br />
On direct questioning Matiu just looks<br />
away. At one stage he mutters something<br />
unintelligible, looking sharply<br />
upwards and the older man who is his<br />
grandfather, puts an arm on his shoulder<br />
soothing him.<br />
You enquire if anyone else in the family<br />
has had difficulty like this. A distant<br />
cousin was in a psychiatric hospital years<br />
ago, no one knows why. She has passed<br />
away now.<br />
Matiu’s family are certain there is no<br />
drug involvement. He has been at home<br />
with no visitors. Manu has been to<br />
check with their mutual friends.<br />
<strong>The</strong> diagnosis is clearly <strong>of</strong> a psychosis.<br />
However there are many unanswered<br />
questions:<br />
• Is the psychosis functional (e.g.<br />
schizophreniform), organic (e.g.<br />
drug induced) or affective (e.g.<br />
depression, with mood congruent<br />
hallucinations and delusions)?<br />
• What role do cultural beliefs<br />
play in this presentation?<br />
• If hospitalisation and medication<br />
are required, as seems likely,<br />
how should this be managed?<br />
• What are the long-term needs <strong>of</strong><br />
this patient and his whanau likely<br />
to include and how should they<br />
be planned for and managed?<br />
Key factors in the assessment<br />
and management <strong>of</strong> mental<br />
health problems amongst Maori<br />
<strong>The</strong> following are key factors in the<br />
assessment and management <strong>of</strong> mental<br />
health problems amongst Maori necessary<br />
for the development <strong>of</strong> a management<br />
plan which is safe, useful and<br />
acceptable to the patient, clinician and<br />
whanau:<br />
(a) Ascertain the self-defined cultural<br />
identity <strong>of</strong> your patient from the<br />
outset. Cultural identity cannot<br />
be determined from appearance.<br />
Matiu looks Maori, but how does<br />
he identify? Matiu is almost silent<br />
during the consultation; however he<br />
should be asked how he identifies,<br />
culturally, as should his whanau.<br />
(b) Patient and whanau views <strong>of</strong> the<br />
illness. Maori views <strong>of</strong> well-being<br />
and illness may differ from those <strong>of</strong><br />
Western medicine. Listening to the<br />
views <strong>of</strong> patient and whanau about<br />
the illness will both assist you in<br />
the assessment process and enhance<br />
the therapeutic relationship. Keep in<br />
mind and bring up as appropriate:<br />
• What do they think is wrong?<br />
• Is there a name for it?<br />
• What may have caused it?<br />
• What, in their view,<br />
should be done now?<br />
• What do they think will<br />
be the outcome?<br />
It is important to know if the whanau<br />
believes the illness to be a Maori<br />
illness (mate Maori). If this the case,<br />
a Tohunga probably will have already<br />
been consulted. Sensitivity is required<br />
when speaking <strong>of</strong> such <strong>issue</strong>s.<br />
However, once you have established<br />
the whanau view, you can clearly<br />
explain your view as a Western clinician.<br />
Mate Maori and a functional<br />
psychosis may co-exist. Importantly<br />
they can be treated together safely<br />
and successfully.<br />
(c) support and safety—Matiu<br />
has<br />
support from his whanau. When<br />
Maori present to the consultation<br />
alone they should be asked if they<br />
would like to have another Maori<br />
present at the interview. Whanau<br />
and cultural consultants not only<br />
support the patient, but also can<br />
help the clinician and the patient<br />
understand each other. In Matiu’s<br />
case, the presence <strong>of</strong> kaumatua<br />
and kuia who performed karakia at<br />
the beginning and the end <strong>of</strong> the<br />
interview ensured that everyone<br />
involved was kept spiritually safe in a<br />
culturally sanctioned manner. Safety<br />
is <strong>of</strong> paramount importance. If the<br />
whanau feel the patient is not safe<br />
then mutually agreed steps have to<br />
be taken to ensure their safety. This<br />
may involve invoking the Mental<br />
Health Act. Matiu is experiencing<br />
command hallucinations telling<br />
him to kill himself. No one in such<br />
circumstances can be assumed to<br />
be safe with respect to themselves<br />
or others. <strong>The</strong> clinician may have<br />
to explain this to the patient and<br />
whanau.<br />
(d) <strong>The</strong> impact <strong>of</strong> culture (<strong>of</strong> patient and<br />
clinician) on the encounter between<br />
the physician and the patient: In<br />
order to establish a relationship with<br />
another person, Maori need to ‘get to<br />
know’ the other person and be known<br />
by that person. It is important to<br />
know who the person is, where they<br />
come from and who their family is.<br />
Thus time needs to be set aside for<br />
the clinician, the patient and whanau/<br />
support person to get to know each<br />
other. This can be difficult, with<br />
increasing time pressure on all<br />
clinicians. However it can be the<br />
difference between a positive outcome<br />
and treatment failure. Clinicians<br />
should feel comfortable about what<br />
they reveal about themselves. <strong>The</strong>re is<br />
no need to tell your life story. A ‘chat’<br />
before getting onto the presenting<br />
problem is helpful. It is important<br />
that the patient is given time to tell<br />
his story in his own way and time.<br />
(e) Language:<br />
Do not take it for granted<br />
that words and expressions in English<br />
mean the same thing for you and<br />
your patient. Ways to avoid such<br />
misunderstanding include:<br />
• Cultural consultant/interpreter<br />
at meetings;<br />
• Develop a therapeutic relationship<br />
in which the patient feels comfort-<br />
64 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
•<br />
•<br />
•<br />
able asking what you mean, e.g.<br />
‘what does anxious mean?’<br />
Be a good listener;<br />
Always be respectful;<br />
Explain your understanding <strong>of</strong><br />
the problem and your management<br />
plan until sure patient<br />
and whanau understand.<br />
in summary<br />
‘Te whare e kitea, te kokonga ngakau e<br />
kore e kitea’ is a Maori proverb, which<br />
literally translated means that we can<br />
see the corners <strong>of</strong> a house, but the<br />
corners <strong>of</strong> the heart are not visible. Its<br />
metaphorical meaning is that things<br />
are not always as they seem at first<br />
glance. I hope this paper goes some<br />
way to illustrating the relevance <strong>of</strong> the<br />
active acknowledgement <strong>of</strong> culture and<br />
difference in the practice <strong>of</strong> psychiatry<br />
amongst Maori; <strong>of</strong> ways to avoid<br />
misunderstanding and misinterpretation<br />
and to achieve a positive outcome<br />
for the patient, the family and the<br />
clinician.<br />
References<br />
1. Durie M. ‘Mauri Ora’. Auckland: Oxford University<br />
Press; 2001.<br />
2. American Psychiatric Association. ‘Diagnostic<br />
and statistical Manual <strong>of</strong> Mental Disorders:<br />
Fourth Edition Text Revision.’ Washington DC:<br />
American Psychiatric Association; 2000.<br />
3. McKendrick J and Bennett P Te Ara (2006).<br />
Indigenous <strong>issue</strong>s in GP psychiatry. In: Blashki,<br />
Judd, Piterman, editors. <strong>General</strong> practice psychiatry.<br />
sydney: McGraw Hill Medical. p 72-85.<br />
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
st John’s wort<br />
(Hypericum perforatum)<br />
Dr Joanne Barnes, Associate Pr<strong>of</strong>essor in Herbal Medicine, school <strong>of</strong> Pharmacy,<br />
University <strong>of</strong> Auckland<br />
PREPARATiONs: Extract <strong>of</strong> St John’s<br />
wort flowers or leaves is available in<br />
many forms, including capsules, tablets<br />
and tinctures, as well as topical preparations.<br />
Chopped or powdered forms <strong>of</strong><br />
the dried herb are also available.<br />
ACTiVE CONsTiTUENTs: Probably<br />
hypericin, hyperforin and/or flavonoid<br />
constituents.<br />
MAiN UsEs: Symptomatic relief in<br />
mild to moderately severe depression.<br />
EVidENCE fOR EffiCACy: Systematic<br />
review and meta-analysis <strong>of</strong> 30<br />
RCTs show that certain St John’s wort<br />
extracts are more effective than placebo<br />
(NNT=42) and as effective as certain<br />
conventional antidepressants (including<br />
selective serotonin reuptake inhibitors<br />
(SSRIs).<br />
AdVERsE EffECTs: Adverse effects<br />
reported in clinical studies are typically<br />
mild and most commonly gastrointestinal<br />
symptoms.<br />
dRUg iNTERACTiONs: Extracts <strong>of</strong><br />
St John’s wort interacts with certain<br />
prescription medicines through inducing<br />
several cytochrome P450 drug metabolising<br />
enzymes, resulting in reduced<br />
plasma concentrations <strong>of</strong> medicines<br />
metabolised by these enzymes, including<br />
certain anticonvulsants, ciclosporin,<br />
summary Message<br />
st John’s wort is about as effective as<br />
some conventional antidepressants<br />
(NNT=42) including certain ssRIs for<br />
treating mild to moderate depression<br />
and has a favourable adverse effect<br />
pr<strong>of</strong>ile, at least with short-term use.<br />
However, it interacts with several other<br />
medicines, including digoxin, theophylline,<br />
warfarin and oral contraceptives.<br />
As with all herbal medicines, different<br />
st John’s wort products differ in their<br />
pharmaceutical quality, and the implications<br />
<strong>of</strong> this for efficacy and safety<br />
should be considered.<br />
warfarin, digoxin, theophylline and oral<br />
contraceptives. <strong>The</strong>re is also a risk <strong>of</strong><br />
increased serotonergic effects where St<br />
John’s wort is taken concomitantly with<br />
triptans or SSRIs.<br />
Key references<br />
CHARMs & HARMs<br />
Barnes J, Anderson LA, Phillipson JD. Herbal medicines.<br />
3rd ed. London: Pharmaceutical<br />
Press; 2007.<br />
Linde K, Mulrow C, Berner M, et al. st John’s wort for<br />
depression. Cochrane Database <strong>of</strong> systematic<br />
Reviews, <strong>issue</strong> 2. Art. no. CD000448. Wiley<br />
Interscience; 2005.<br />
Izzo AA & Ernst E. Interactions between herbal medicines<br />
and prescribed drugs: a systematic review.<br />
Drugs 2001;15:2163–2175.<br />
Mills E, Montori VM, Wu P, et al. Interaction <strong>of</strong> st<br />
John’s wort with conventional drugs: systematic<br />
review <strong>of</strong> clinical trials. BMJ 2005;329:27–30.<br />
Herbal medicines are a popular health care choice, but few have been tested to<br />
contemporary standards. cHARMS & HARMS summarises the evidence for the<br />
potential benefits and possible harms <strong>of</strong> well-known herbal medicines.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 65
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
REsOURCE sUMMARY<br />
destination: Recovery<br />
Te Unga Ki Uta:Te Oranga<br />
future responses to mental distress and loss <strong>of</strong> well-being<br />
—a discussion paper from the Mental Health Advocacy Coalition<br />
Helen Rodenburg MBChB, FRNZCGP<br />
Ko te pae tawhiti whaia ki a tata—Seek your aspirations on the horizons<br />
This recent discussion paper is<br />
important for general practice and<br />
primary health care as it recognises<br />
the role we play in improving the<br />
mental health <strong>of</strong> our population:<br />
Easy access: Individuals and families know<br />
where to find independent information<br />
on the availability and quality <strong>of</strong> services.<br />
<strong>The</strong>re are many doors into services—a lot<br />
<strong>of</strong> them open into primary health settings<br />
which act as the hubs <strong>of</strong> service delivery<br />
and referral. People are not denied access<br />
to help on the basis that their distress<br />
or loss <strong>of</strong> well-being are insufficiently<br />
severe; they are either provided for or immediately<br />
referred elsewhere.<br />
<strong>The</strong> paper provides challenges for all<br />
health pr<strong>of</strong>essionals to change and improve<br />
the care we <strong>of</strong>fer and is part <strong>of</strong> an<br />
international movement in the provision<br />
<strong>of</strong> services. With the developments in<br />
<strong>New</strong> <strong>Zealand</strong> in primary mental health<br />
care it is important that we, as GPs, are<br />
aware <strong>of</strong> developments and able to take<br />
advantage <strong>of</strong> opportunities.<br />
‘When you’re trying to create things<br />
that are new, you have to be prepared to<br />
be on the edge <strong>of</strong> risk.’—Michael Eisner<br />
I have been the RNZCGP representative<br />
on the Coalition and appreciate the opportunity<br />
to contribute to improvement<br />
in mental health services, and for the<br />
support given to primary care. ‘Destination<br />
Recovery’ supports integrated<br />
collaborative approaches to service provision<br />
across both specialist clinical and<br />
support organisational boundaries, and<br />
the secondary-primary interface. Leadership<br />
is recognised as being important, as<br />
is support for change management.<br />
‘<strong>The</strong>re are risks and costs to a program<br />
<strong>of</strong> action. But they are far less than the<br />
long-range risks and costs <strong>of</strong> comfortable<br />
inaction.’—John F Kennedy<br />
Executive summary<br />
‘Vision is perhaps our greatest strength…<br />
it makes us peer into the future and lends<br />
shape to the unknown.’—Li Ka Shing<br />
<strong>The</strong> Mental Health Advocacy Coalition<br />
has a vision for society’s well-being.<br />
We believe everyone should experience<br />
not only good mental health, but the<br />
benefits <strong>of</strong> being able to cope with life<br />
stressors and enjoy a productive working<br />
life and fulfilling relationships. We believe<br />
mental health services have a major<br />
role to play in bringing about well-being<br />
for all; but only if these services are<br />
transformed.<br />
Forces for transformation<br />
<strong>The</strong> rise in human rights awareness,<br />
self-determination, the consumer soci-<br />
ety, multiculturalism and the Maori renaissance<br />
have all impacted on the mental<br />
health arena. Deinstitutionalisation,<br />
awareness <strong>of</strong> the social determinants <strong>of</strong><br />
distress, and the service-user movement<br />
are all drivers for mental health service<br />
transformation. Expectations are also<br />
changing—people with mental distress<br />
want the same from life as everyone<br />
else. <strong>The</strong>re is already change at mental<br />
health policy level in many countries,<br />
including <strong>New</strong> <strong>Zealand</strong>.<br />
in our vision:<br />
Values and people<br />
• Madness is a fully human experience.<br />
• <strong>The</strong> purpose <strong>of</strong> services is recovery.<br />
• Self-determination is the foundation<br />
<strong>of</strong> service delivery.<br />
Adopting these values changes the way<br />
people think. Everyone is encouraged to<br />
be informed, active and competent—this<br />
includes the workforce, people who use<br />
services, their families and the wider<br />
community.<br />
Services<br />
• Primary services are the most<br />
common point <strong>of</strong> access, and <strong>of</strong>fer<br />
service negotiation, navigation,<br />
drug and talking therapies<br />
and other forms <strong>of</strong> support.<br />
66 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
• Niche mental health services<br />
include acute, forensic, and early<br />
intervention services, and services<br />
for specific client groups.<br />
• Other sectors are structurally aligned<br />
and work closely with primary<br />
services and mental health services<br />
to promote well-being for all.<br />
• All agencies are accountable to<br />
powerful and well-resourced<br />
district leadership groups.<br />
Systems in our vision:<br />
• Policy is pr<strong>of</strong>oundly influenced by<br />
service users, families and those<br />
most affected by mental distress, and<br />
funding is planned and responsive.<br />
• Measures <strong>of</strong> effectiveness <strong>of</strong> services<br />
are simple and focus on outcomes<br />
that are important to service users.<br />
• Coordinated service development,<br />
workforce development<br />
and research lead to adaptive,<br />
responsive services for all.<br />
An independent national agency<br />
monitors services and provides<br />
information on quality and advocacy<br />
for service users and whanau.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 67<br />
•<br />
<strong>The</strong> discussion paper is available at:<br />
http://www.mentalhealth.org.nz/file/down<br />
loads/pdf/Destination%20Recovery_FINAL<br />
_low%20res.pdf<br />
Effective communication strategies to enhance<br />
patient self-care<br />
Fiona Moir MBChB; Renske van den Brink MBChB, FRNZCGP; Richard Fox MBChB, FRNZCGP; Susan Hawken MBChB, FRNZCGP<br />
introduction<br />
Can primary care practitioners influence<br />
and improve patient self-care, simply by<br />
the way they communicate with their<br />
patients? If so, can this be done within<br />
the consultation, even when practitioners<br />
already feel constrained by lack <strong>of</strong> time? 1<br />
Currently in <strong>New</strong> <strong>Zealand</strong> (NZ) there<br />
is significant morbidity and mortality<br />
associated with lifestyle-related disease,<br />
and constraints on health resources<br />
increasingly mean that patients need to<br />
be more responsible for their own health.<br />
After indicating the general context <strong>of</strong><br />
lifestyle-related illness, this paper will<br />
outline the different approaches available<br />
to primary care practitioners. <strong>The</strong> prin-<br />
CORREsPONdENCE TO:<br />
fiona Moir<br />
Department <strong>of</strong> <strong>General</strong><br />
Practice and Primary<br />
Health Care, Faculty<br />
<strong>of</strong> Medical and Health<br />
sciences, <strong>The</strong> University<br />
<strong>of</strong> Auckland, PB 92019,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong><br />
f.moir@auckland.ac.nz<br />
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
ciples <strong>of</strong> motivational interviewing, the<br />
stages <strong>of</strong> change model, the ‘catastrophe<br />
theory’ model, 2 and the essential elements<br />
<strong>of</strong> brief intervention in primary<br />
care settings will be outlined. This will<br />
be followed by practical examples on<br />
how to communicate with the patient<br />
in ways that will enhance behavioural<br />
change and self-care.<br />
Background<br />
<strong>The</strong>re are some concerning trends in the<br />
rates <strong>of</strong> lifestyle-related disease. <strong>The</strong><br />
prevalence <strong>of</strong> obesity has more than<br />
doubled from 1982 to 2003, 3 and the<br />
future impact <strong>of</strong> the obesity epidemic<br />
on the NZ population and health system<br />
will be significant. 4 Smoking rates are no<br />
longer dropping. 3 Although the overall<br />
ischaemic heart disease mortality rate for<br />
2011–15 is predicted to decline, there is<br />
an expected actual increase in the mortality<br />
rate for Maori. 5 Disparities across a<br />
range <strong>of</strong> risk factors and health outcomes<br />
for Maori and Pacific peoples, compared<br />
to the total population, persist and are <strong>of</strong><br />
grave concern. 6 With effective lifestyle<br />
REsOURCE sUMMARY<br />
PRACTICAL POINTERs<br />
intervention targeting obesity, smoking,<br />
exercise, and alcohol use, such lifestylerelated<br />
conditions could be reduced.<br />
A NZ study identified patients with lifestyle<br />
<strong>issue</strong>s by using a short screening<br />
tool consisting <strong>of</strong> lifestyle and mental<br />
health risk factors. It was found to be acceptable<br />
to patients and not burdensome<br />
to practitioners. 7 It is well known that<br />
<strong>of</strong>fering patients information only does<br />
not necessarily effect behaviour change,<br />
so other approaches are needed. An<br />
intervention that is currently being trialled<br />
and evaluated 8 involves a ‘lifestyle<br />
script’ administered by primary care<br />
nurses and followed up with telephone<br />
counselling. Utilising programmes that<br />
are culturally appropriate is important<br />
to success. 9 Other studies have shown<br />
that although there is acceptability<br />
and recognition <strong>of</strong> the value <strong>of</strong> chronic<br />
disease management programmes, there<br />
is still concern by practitioners about the<br />
amount <strong>of</strong> time involved. 10<br />
Promoting patient self-care ideally is<br />
the responsibility <strong>of</strong> all members <strong>of</strong> the
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
PRACTICAL POINTERs<br />
multi-disciplinary team. For example, a<br />
current initiative to improve medication<br />
adherence involves pharmacists undertaking<br />
a ‘Medicine Use Review’ (MUR),<br />
and discussing all <strong>of</strong> the patient’s<br />
medications with them. Central to the<br />
MUR consultation is the way in which<br />
the pharmacist communicates with the<br />
patient, exploring their health beliefs<br />
and their illness perspective. An exploration<br />
<strong>of</strong> the patient’s illness perspective<br />
involves finding out their ideas, concerns<br />
and expectations relating to their illness<br />
and medications. 11 Once this information<br />
has been gathered, the pharmacist and<br />
the patient use joint decision-making to<br />
agree on the next step. This is a good<br />
example <strong>of</strong> how communication can aid<br />
patient behaviour change.<br />
A variety <strong>of</strong> models have attempted to<br />
facilitate patient self-care in the context<br />
<strong>of</strong> the patient-centred interview, but one<br />
<strong>of</strong> their limitations in primary care is<br />
the amount <strong>of</strong> time they take to deliver.<br />
In this paper we briefly describe four <strong>of</strong><br />
these models, and then indicate stylistic<br />
elements within them, which may usefully<br />
be used within a time-constrained<br />
interview.<br />
Motivational interviewing<br />
Motivational interviewing is a directive<br />
client-centered style <strong>of</strong> counselling<br />
for eliciting behaviour change. It has<br />
its roots in the drug and alcohol field,<br />
and has been used for many years in<br />
addictions counselling, predominantly<br />
focusing on problem drinking. Although<br />
initially developed for longer consultations,<br />
elements <strong>of</strong> it have been adapted<br />
for use in shorter interactions in many<br />
other areas <strong>of</strong> health behaviour change. 12<br />
<strong>The</strong> underlying ethos or spirit <strong>of</strong> motivational<br />
interviewing is that the practitioner–patient<br />
relationship works best as a<br />
partnership, that the quality <strong>of</strong> that relationship<br />
is the key to behaviour change,<br />
and that the motivation and ideas about<br />
change come from the patient, not from<br />
the practitioner. For example, the patient<br />
can be asked to identify and explore any<br />
ambivalence they have to the particular<br />
behaviour, e.g. ‘what are the good<br />
things and the not so good things about<br />
smoking?’ In motivational interviewing,<br />
it is the practitioner’s job to direct the<br />
patient towards exploring and discussing<br />
ambivalence and to summarise this<br />
for them, and it is the patient’s job to<br />
examine the ambivalence and to decide<br />
on the next step.<br />
<strong>The</strong> main aspects <strong>of</strong> motivational interviewing<br />
13 are summarised in Table 1.<br />
<strong>The</strong> stages <strong>of</strong> change<br />
Another model, referred to as ‘the stages<br />
<strong>of</strong> change’, played a vital role in the<br />
development <strong>of</strong> both motivational interviewing<br />
and brief intervention. 15 Central<br />
to this model is the idea that behaviour<br />
change is incremental and involves specific<br />
tasks. <strong>The</strong> model describes a series<br />
<strong>of</strong> changes progressing from pre-contemplative<br />
(unaware, unable or unwilling to<br />
change), to contemplative (evaluating pros<br />
and cons <strong>of</strong> change), to preparation, then<br />
action and maintenance. <strong>The</strong> model recognises<br />
that relapse is common, and that<br />
many people will have several attempts<br />
before achieving a successful outcome.<br />
Table 1<br />
Motivational interviewing 14<br />
spirit Autonomy<br />
collaboration<br />
Evocation<br />
Principles Roll with resistance and<br />
Counselling<br />
skills required<br />
avoid arguments<br />
Express empathy<br />
Develop discrepancy<br />
Support Self-efficacy<br />
open questions<br />
Affirm<br />
Reflect<br />
Summarise<br />
Catastrophe theory model<br />
Critics <strong>of</strong> the stages <strong>of</strong> change model<br />
state that the boundaries between the<br />
stages are arbitrary, and furthermore that<br />
<strong>of</strong>ten behaviour change does not actually<br />
involve any planning or preparation. 16 In<br />
a recent study, almost half <strong>of</strong> smokers’<br />
attempts to stop involved no previous<br />
planning, and unplanned attempts to<br />
stop were more likely to be successful. 2<br />
A new model in 2006, based on ‘catastrophe<br />
theory’, hypothesizes that behaviour<br />
change is influenced by ‘motivational<br />
tension’ (the levels <strong>of</strong> which depend on<br />
beliefs, past experiences, and the current<br />
situation), and that in the presence <strong>of</strong><br />
this tension, even a small trigger can<br />
lead to a sudden change. 2<br />
Brief intervention<br />
<strong>The</strong> stages <strong>of</strong> change can be a helpful<br />
model to use alongside motivational<br />
interviewing, but where does brief<br />
intervention come into play? Brief<br />
interventions are those practices that<br />
aim to identify a problem and motivate<br />
an individual to do something about it,<br />
which can <strong>of</strong>ten be used in the course<br />
<strong>of</strong> routine practice without requiring<br />
significantly more time. 17 Multiple trials<br />
have shown the effectiveness <strong>of</strong> brief<br />
intervention. 18 Successful brief interventions<br />
have been found to contain six key<br />
elements in common. 19<br />
Brief intervention: FRAMES 20<br />
Feedback given about impairment/current<br />
risks, e.g. giving test results<br />
Responsibility is the patient’s<br />
Advice about change<br />
Menu <strong>of</strong> options—alternative strategies<br />
Empathy<br />
Self-efficacy and optimism for change<br />
A brief (five to 10 minute) smoking<br />
intervention has been developed based<br />
on motivational interviewing, assessing<br />
the patient’s confidence and their level<br />
68 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
<strong>of</strong> motivation. 12 A patient was ‘ready<br />
to change’ if they had a high level <strong>of</strong><br />
confidence and felt that the change was<br />
important to them.<br />
integrating the models<br />
in practice<br />
By calling on our experience, we have<br />
identified ways in which elements <strong>of</strong><br />
each <strong>of</strong> these models can be used in dayto-day<br />
practice.<br />
First, it is important to bring up the topic<br />
<strong>of</strong> possible health behaviour change<br />
carefully, especially if we are introducing<br />
the idea opportunistically. A good<br />
transition into this is to ask permission<br />
to discuss the topic: ‘Could we talk<br />
about smoking for a couple <strong>of</strong> minutes?’<br />
This approach avoids an abrupt change<br />
the rapport by using reflection, state<br />
our concern about the health behaviour<br />
and its implications, and leave the<br />
door open for future discussion <strong>of</strong> the<br />
behaviour should the patient wish to<br />
pursue this. Some argue that we can also<br />
<strong>of</strong>fer an intervention at this stage if it<br />
is appropriate. 16 However, enthusiastic<br />
suggestions by the doctor to think about<br />
behaviour change, or an <strong>of</strong>fer to try a<br />
new treatment, can sometimes come<br />
at the expense <strong>of</strong> connection with the<br />
patient. For this reason it is important<br />
to be very aware <strong>of</strong> the patient’s verbal<br />
and non-verbal reaction throughout the<br />
discussion and to respond to this appropriately<br />
for individual situations.<br />
If the patient is contemplative, we can<br />
encourage them to explore the pros and<br />
cons <strong>of</strong> the behaviour, whilst we reflect<br />
When styles and strategies from motivational<br />
interviewing are employed with skill, it begins to feel<br />
like a dance instead <strong>of</strong> a struggle<br />
into a potentially sensitive area for the<br />
patient. As emphasised in the FRAMES<br />
model, the timing <strong>of</strong> this can be important.<br />
For instance, giving a patient their<br />
abnormal liver function test results may<br />
provide an opportunity to introduce the<br />
topic <strong>of</strong> alcohol consumption.<br />
Next we can assess the patient’s ‘readiness<br />
to change’. This is best done with<br />
an open question: ‘What are your<br />
thoughts about smoking?’ In this way,<br />
we avoid making assumptions about<br />
what the patient thinks or ‘should’ be<br />
thinking.<br />
<strong>The</strong> next step can be dictated by where<br />
the patient is in the stages <strong>of</strong> change.<br />
Using a motivational interviewing style<br />
in our discussion for all <strong>of</strong> the stages <strong>of</strong><br />
change can be beneficial. If the patient<br />
is precontemplative, we can maintain<br />
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
their ambivalence or discrepancy about<br />
their current behaviour and their goals.<br />
We want the patient to take responsibility,<br />
and to come up with the motivation<br />
and ideas about change, whilst we listen<br />
and summarise. <strong>The</strong> practitioner and the<br />
patient can also work together in the<br />
preparation, action and maintenance<br />
stages. <strong>The</strong> practitioner can enable the<br />
patient to work out a personal action<br />
plan, anticipate barriers and triggers, and<br />
to identify supports and enablers. A<br />
vital part <strong>of</strong> the practitioner’s role is to<br />
increase self-efficacy and reinforce any<br />
accomplishments. In relapse, we must<br />
empathise and normalise the reality <strong>of</strong><br />
relapse, whilst not assuming the<br />
patient’s next step.<br />
Brief intervention can be useful with<br />
someone who is in the action or preparation<br />
stage, as we will be exploring a list<br />
PRACTICAL POINTERs<br />
<strong>of</strong> possible options <strong>of</strong> behaviour change<br />
they could pursue—some <strong>of</strong> which have<br />
been suggested by the doctor, and some<br />
by the patient. <strong>The</strong> recent model based<br />
on ‘catastrophe’ theory 2 illustrates that<br />
many patients’ attempts to stop will not<br />
involve planning, and that immediate<br />
availability <strong>of</strong> treatment is important to<br />
support those attempts.<br />
When time is short, the main idea is to<br />
use the underlying spirit <strong>of</strong> motivational<br />
interviewing, 11 and to remember that<br />
the practitioner–patient relationship and<br />
interaction is the vital component <strong>of</strong> the<br />
success <strong>of</strong> health behaviour change.<br />
Practitioner–patient<br />
relationship<br />
Judgement, lecturing and advice giving<br />
has been shown to be less effective in<br />
health behaviour change than genuine<br />
empathic use <strong>of</strong> motivational interviewing<br />
styles and strategies. Empathy is a<br />
powerful relational skill which helps<br />
patients to feel connected with their<br />
practitioner even when there is mutual<br />
disagreement over <strong>issue</strong>s such as smoking<br />
or medication compliance. 21<br />
<strong>The</strong> capacity to influence patients hinges<br />
upon the quality <strong>of</strong> rapport between<br />
practitioner and patient, and rapport is<br />
perceived by the patient as the ability <strong>of</strong><br />
the practitioner to relate to the patient’s<br />
world. 22<br />
Empathy is fairly easy to master when<br />
we agree with the patient and we can<br />
relate to their culture, their social status<br />
and their world view. However, when we<br />
disagree or disapprove <strong>of</strong> our patients,<br />
empathy is much more difficult. How<br />
can we be empathic when we know that<br />
the patient’s smoking is making their<br />
chest disease worse, and all we want to<br />
do is to tell them to stop? Firstly we can<br />
remind ourselves that the way in which<br />
we communicate can have an impact on<br />
the likelihood <strong>of</strong> the patient changing<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 69
CONTiNUiNg PROfEssiONAL dEVELOPMENT<br />
PRACTICAL POINTERs<br />
their behaviour. A useful technique to<br />
use when we notice ourselves feeling<br />
disapproving or annoyed by our patients<br />
is to try to ‘park’ that feeling and to first<br />
<strong>of</strong>fer the patient an empathic reflection.<br />
Contrast the difference in these two responses<br />
to a patient bothered by lithium<br />
side effects:<br />
Practitioner A: How about trying to split<br />
the dose, as well as having it with food?<br />
That should help cut down the nausea.<br />
Practitioner B: It sounds like the nausea<br />
is really awful for you and taking the<br />
lithium regularly is the last thing you<br />
feel like doing.<br />
Practitioner A has got their own agenda<br />
in the foreground, and the patient is likely<br />
to feel isolated and perhaps even irritated.<br />
Practitioner B however is putting<br />
the patient’s concern at centre stage. This<br />
is not the same as approving <strong>of</strong> their<br />
behaviour. It just demonstrates to the<br />
patient that Practitioner B understands<br />
them in a non-judgemental way. After<br />
that, once the rapport is more strongly<br />
established, Practitioner B can go on to<br />
let them know their medical concerns.<br />
When styles and strategies from motivational<br />
interviewing are employed<br />
with skill, it begins to feel like a dance<br />
instead <strong>of</strong> a struggle. Rather than trying<br />
to convince the patient to change, the<br />
practitioner uses a Socratic questioning<br />
style to evoke the patient’s own problemsolving<br />
skills and to galvanise them into<br />
action. <strong>The</strong> patient is doing all the work,<br />
and the practitioner’s genuine non-judgemental<br />
reflective style steadily builds<br />
rapport. If it feels more like a struggle<br />
then usually this is because the practitioner<br />
is working very hard to convince<br />
the patient to change, resulting in either<br />
a confrontation or the patient ceasing to<br />
play an active part in the process.<br />
Compare the following interventions for<br />
someone who needs more exercise:<br />
Practitioner A: How about trying to get<br />
<strong>of</strong>f the bus two stops early so that you<br />
can get in a bit <strong>of</strong> exercise that way?<br />
Practitioner B: If you were to find a way<br />
to increase your exercise even a little bit,<br />
what would you choose to try?<br />
Working in a motivational interviewing<br />
style challenges the practitioner to initially<br />
hold back their own opinions and<br />
advice, giving priority to the patient’s<br />
ideas and reflection <strong>of</strong> the patient’s illness<br />
experience, in order to strengthen<br />
the therapeutic relationship. Once this<br />
is established, the strong therapeutic<br />
relationship can then withstand the<br />
challenge <strong>of</strong> the practitioner’s medical<br />
opinion, even when this is in direct<br />
conflict with the patient’s view.<br />
Conclusion<br />
Lifestyle-related disease is <strong>of</strong> significant<br />
concern in NZ, and there is a need to raise<br />
awareness <strong>of</strong> opportunities for intervention.<br />
Brief intervention, motivational<br />
interviewing, stages <strong>of</strong> change, and the<br />
‘catastrophe model’ are all useful frameworks<br />
for promoting behavioural change,<br />
and elements from all four may be<br />
adapted for use in primary care settings.<br />
In a short consultation the most important<br />
factor is the skilful use <strong>of</strong> empathy to<br />
strengthen rapport in the practitioner–patient<br />
relationship. Good rapport creates a<br />
platform from which the practitioner can<br />
enhance their capacity to influence health<br />
behaviour and optimise patient self-care.<br />
References<br />
1. Goodyear-smith F, Wearn A, Everts H, Huggard P,<br />
Halliwell J. Communication in practice: Auckland<br />
general practitioners reflect on communication<br />
events and identify training needs. N Z Fam Physician<br />
2006;33(1):30–38.<br />
2. West R, sohal T. ‘Catastrophic’ pathways to smoking<br />
cessation: findings from national survey. BMJ<br />
2006;332(7539):458–60.<br />
3. Metcalf P, scragg RK, schaaf D, Dyall L, Black<br />
P, Jackson R. Trends in major cardiovascular<br />
risk factors in Auckland, <strong>New</strong> <strong>Zealand</strong>: 1982 to<br />
2002–2003. N Z Med J 2006;119(1245):U2308.<br />
4. Turley M, Tobias M, Paul s. Non-fatal disease<br />
burden associated with excess body mass index<br />
and waist circumference in <strong>New</strong> <strong>Zealand</strong> adults.<br />
Aust N Z J Public Health 2006;30(3):231–7.<br />
5. Tobias M, sexton K, Mann s, sharpe N. How<br />
low can it go? Projecting ischaemic heart disease<br />
mortality in <strong>New</strong> <strong>Zealand</strong> to 2015. N Z Med J<br />
2006;119(1232):U1932.<br />
6. Ministry <strong>of</strong> Health. A portrait <strong>of</strong> health: Key results<br />
<strong>of</strong> the 2006/7 <strong>New</strong> <strong>Zealand</strong> Health survey. In:<br />
Wellington: Ministry <strong>of</strong> Health; 2008.<br />
7. Goodyear-smith F, Arroll B, sullivan s, Elley R,<br />
Docherty B, Janes R. Lifestyle screening: development<br />
<strong>of</strong> an acceptable multi-item general practice<br />
tool. N Z Med J 2004;117(1205):U1146.<br />
8. Rose sB, Lawton BA, Elley CR, Dowell AC,<br />
Fenton AJ. <strong>The</strong> ‘Women’s Lifestyle study’, 2-year<br />
randomized controlled trial <strong>of</strong> physical activity<br />
counselling in primary health care: rationale and<br />
study design. BMC Public Health 2007;7(147):166.<br />
9. McAuley KA, Murphy E, McLay RT, Chisholm A,<br />
story G, Mann JI, et al. Implementation <strong>of</strong> a successful<br />
lifestyle intervention programme for <strong>New</strong><br />
<strong>Zealand</strong> Maori to reduce the risk <strong>of</strong> type 2 diabetes<br />
and cardiovascular disease. Asia Pac J Clin Nutr<br />
2003;12(4):423–6.<br />
10. Tracey J, Bramley D. <strong>The</strong> acceptability <strong>of</strong> chronic<br />
disease management programmes to patients,<br />
general practitioners and practice nurses. N Z Med<br />
J 2003;116(1169):U331.<br />
11. stewart M, Brown JB, Weston WW, McWhinney<br />
IR, McWilliam CL, Freeman TR. Patient-centered<br />
medicine. Transforming the clinical method. Thousand<br />
Oaks: sage Publications; 1995.<br />
12. Emmons KM, Rollnick s. Motivational interviewing<br />
in health care settings. Opportunities and limitations.<br />
Am J Prev Med 2001;20(1):68–74.<br />
13. Miller WR, Rollnick s. Motivational interviewing:<br />
Preparing people for change. 2nd ed. <strong>New</strong> York:<br />
Guilford Press; 2002.<br />
14. Miller W, Rollnick s. Motivational interviewing:<br />
preparing people to change addictive behaviour.<br />
<strong>New</strong> York: Guilford; 1991.<br />
15. DiClemente CC, Velasquez MM. Motivational<br />
interviewing and the stages <strong>of</strong> change. In: Miller<br />
WR, Rollnick s, editors. Motivational interviewing:<br />
Preparing people for change. <strong>New</strong> York: Guilford<br />
Press; 2002.<br />
16. West R. Time for a change: putting the Transtheoretical<br />
(stages <strong>of</strong> Change) Model to rest. Addiction<br />
2005;100(8):1036–9.<br />
17. Babor TF, Higgins-Biddle JC. Brief intervention.<br />
For hazardous and harmful drinking. A manual<br />
for use in Primary care. In: 2nd ed: Department <strong>of</strong><br />
Mental Health and substance Dependence, World<br />
Health Organization; 2001.<br />
18. Bien TH, Miller WR, Tonigan Js. Brief interventions<br />
for alcohol problems: a review. Addiction<br />
1993;88(3):315–35.<br />
19. Miller WR, sanchez VC. Motivating young adults for<br />
treatment and lifestyle change. In: Howard G, editor.<br />
Issues in alcohol use and misuse by young adults.<br />
Notre Dame: University <strong>of</strong> Notre Dame Press; 1993.<br />
20. Miller W, sanchez V. Motivating young adults for<br />
treatment and lifestyle change. In: Howard G, editor.<br />
Issues in alcohol use and misuse by young adults.<br />
Notre Dame: University <strong>of</strong> Notre Dame Press; 1993.<br />
21. Halpern J. Empathy and patient-physician conflicts.<br />
J Gen Intern Med 2007;22(5):696–700.<br />
22. Yapko MD. Breaking the patterns <strong>of</strong> depression.<br />
<strong>New</strong> York: Doubleday; 1997.<br />
70 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Uncertainty, fear and whistling<br />
happy tunes<br />
Katherine Wallis MBChB, MBHL, FRNZCGP<br />
ABstRACt<br />
Uncertainty in medical practice is<br />
ineradicable, despite great scientific<br />
advances over the last century. Uncertainty<br />
provokes fear, not just in patients<br />
but also in doctors. Patients cope with<br />
their fear by seeking the advice and reassurance<br />
<strong>of</strong> doctors; doctors, on the other<br />
hand, cope by denial and self-deception.<br />
But today, in this scientific, truth-seeking<br />
age doctors are encouraged to share<br />
their uncertainty with patients in order<br />
to ‘empower’ patients and improve doctor–patient<br />
relations. While in theory<br />
doctors might agree with this approach,<br />
in practice they continue to deny it and<br />
instead whistle happy tunes—deceiving<br />
both themselves and their patients.<br />
A disclosure <strong>of</strong> uncertainty requires an<br />
acknowledgement <strong>of</strong> uncertainty and,<br />
in practice, the ability <strong>of</strong> doctors to acknowledge<br />
and to tolerate uncertainty<br />
is limited.<br />
Whenever I feel afraid, I hold my head<br />
erect<br />
And whistle a happy tune, So no one<br />
will suspect<br />
I’m afraid.<br />
While shivering in my shoes, I strike a<br />
careless pose<br />
And whistle a happy tune, And no one<br />
ever knows<br />
I’m afraid.<br />
<strong>The</strong> result <strong>of</strong> this deception, Is very<br />
strange to tell<br />
For when I fool the people I fear, I fool<br />
myself as well! 1<br />
If one thing in this life is certain, it<br />
is that the practice <strong>of</strong> medicine is a<br />
practice in uncertainty. Renée Fox, 2 in<br />
her landmark studies <strong>of</strong> uncertainty in<br />
medical practice in the 1950s, characterised<br />
three types <strong>of</strong> uncertainty: the<br />
uncertainty <strong>of</strong> medical knowledge, the<br />
uncertainty <strong>of</strong> the practitioner, and the<br />
uncertainty in discerning between these<br />
two types <strong>of</strong> uncertainty (is the answer<br />
out there somewhere and I just haven’t<br />
come across it, or has the answer not<br />
been discovered yet?). In clinical practice<br />
we face uncertainty about the diagnosis,<br />
compounded by the inherent variability<br />
in how patients perceive and describe<br />
their problems; uncertainty about the<br />
treatment, as we know patients respond<br />
differently to treatments and that applying<br />
general knowledge to individuals<br />
is flawed; and uncertainty about the<br />
role that we are expected to play today:<br />
are we to be rational scientist, shaman,<br />
social worker or counsellor?<br />
Over the last century great advances<br />
in medical knowledge have been made,<br />
leading some enthusiasts to believe<br />
that uncertainty in medicine could<br />
be eradicated. It was hoped that,<br />
with enough research, all questions<br />
would be answered and that illness<br />
and suffering could be dealt with by<br />
EtHiCs<br />
a rational scientific approach, making<br />
intuition and spiritualism redundant.<br />
Such hopes, however, look increasingly<br />
unlikely ever to be fulfilled, in part<br />
because medicine, if it is a science at<br />
all, is a science <strong>of</strong> individuals. <strong>The</strong>re<br />
are no great generalisable truths to be<br />
discovered and applied; the expression<br />
and the experience <strong>of</strong> illness will<br />
always remain unique. Randomised<br />
controlled trials will never be able<br />
to tell us how a particular individual<br />
will respond to a particular treatment.<br />
As Kant once remarked, ‘Out <strong>of</strong> the<br />
crooked timber <strong>of</strong> humanity no straight<br />
thing was ever made’. 3<br />
Uncertainty exists in all facets <strong>of</strong> life,<br />
but in the health care context in particular,<br />
uncertainty breeds anxiety and fear.<br />
<strong>The</strong>re is a Chinese proverb claiming that<br />
‘more people die <strong>of</strong> fear <strong>of</strong> their illness<br />
than die <strong>of</strong> the illness itself’. As <strong>of</strong>ten<br />
as not it is fear, born <strong>of</strong> uncertainty, that<br />
prompts a patient to seek the opinion <strong>of</strong><br />
a doctor. Patients want to know whether<br />
their symptoms are significant, what<br />
can be done and, preferably, also to be<br />
reassured that all will be well. However,<br />
given that we must all die one day, there<br />
will come a day when all will not be<br />
well. It is the doctor’s role to sort out<br />
and communicate the known from the<br />
<strong>The</strong> ethics column explores <strong>issue</strong>s around practising ethically in primary health care<br />
and aims to encourage thoughtfulness about ethical dilemmas that we may face.<br />
tHis issUE: Our guest ethicist and GP Katherine Wallis discusses balancing the acknowledgment<br />
to patients that medical practice is uncertain with managing their fears<br />
and anxieties.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 71
EtHiCs<br />
unknown, and to manage the patient’s<br />
anxiety and fear.<br />
For the doctor’s part too, there is fear.<br />
From the confusing, inaccurate, or even<br />
contradictory information 4 presented<br />
we must sort the relevant from the<br />
irrelevant and establish a management<br />
plan. We can never be certain and yet<br />
still we must act, even if only to advise<br />
a ‘wait and see’ approach. And with<br />
action, <strong>of</strong> course, comes responsibility.<br />
We can be guided by probabilities,<br />
but individual differences reduce our<br />
ability to predict from generalities and<br />
there is the constant risk <strong>of</strong> error. Error<br />
is unavoidable, not only because <strong>of</strong> the<br />
limitations <strong>of</strong> medical knowledge and<br />
the limits <strong>of</strong> the human intellect, but<br />
also because <strong>of</strong> the ‘necessary fallibility<br />
<strong>of</strong> a knowledge <strong>of</strong> particulars’. 5 <strong>The</strong> fact<br />
that we must act before certainty can<br />
be established (if it ever can be) makes<br />
clinical medicine, not a rational science<br />
nor an art, but a ‘practice’. 6<br />
Elstein, who spent much <strong>of</strong> his life<br />
studying diagnostic decision-making, estimated<br />
that the rate <strong>of</strong> diagnostic error<br />
in medical practice was approximately<br />
15%. 7 This figure has subsequently been<br />
corroborated. 8 <strong>The</strong>se diagnostic errors,<br />
however, are only errors in hindsight:<br />
At the time the diagnosis was made it<br />
seemed the most likely, most reasonable<br />
and therefore the most correct diagnosis<br />
to make. As a doctor in Paget’s study<br />
remarked ‘…the errors are errors now,<br />
but they weren’t errors then’. 9<br />
Experienced practitioners use heuristics<br />
(rapid pattern recognition processes) 3 to<br />
reach a diagnosis. This intuitive decision-making<br />
process saves time and gives<br />
the correct diagnosis most <strong>of</strong> the time; 10<br />
however there is a price to pay for this<br />
efficiency: Predictable error. Sometimes<br />
the most likely diagnosis, rather than<br />
the correct diagnosis, is made. As James<br />
Reason says: ‘Our propensity for certain<br />
types <strong>of</strong> error is the price we pay for the<br />
brain’s remarkable ability to think and<br />
act intuitively.’ 11<br />
In hindsight the correct diagnosis is<br />
obvious, but in the complex, chaotic, and<br />
uncertain world <strong>of</strong> clinical practice the<br />
most likely diagnosis at the time seems<br />
the most reasonable one to make. Thus<br />
there is a trade <strong>of</strong>f between efficiency<br />
and accuracy.<br />
In such a mire <strong>of</strong> uncertainty and error,<br />
how can either doctor or patient make<br />
a rational decision about treatment,<br />
let alone continue to practise? To cope<br />
with the fear, doctors employ various<br />
strategies designed to reduce either the<br />
responsibility or the uncertainty. 12 Responsibility<br />
can be reduced by referral,<br />
healing to take place, a pr<strong>of</strong>ession <strong>of</strong><br />
certainty is required.<br />
Today, while doctors might accept<br />
(in theory) that medical knowledge is<br />
uncertain, in practice they continue<br />
to pr<strong>of</strong>ess certainty. In practice the art<br />
<strong>of</strong> self-deception is alive and well. In<br />
front <strong>of</strong> patients, doctors instinctively<br />
suppress and deny their knowledge <strong>of</strong><br />
uncertainty 6,14 in favour <strong>of</strong> providing<br />
reassurance and hope. And, given the<br />
patient’s desire for reassurance, and the<br />
essential uncertainty <strong>of</strong> clinical practice,<br />
whistling such a happy tune might just<br />
be the pragmatic approach to take.<br />
Katz considers that the denial <strong>of</strong> uncertainty<br />
in medicine has something<br />
In hindsight the correct diagnosis is obvious, but in the<br />
complex, chaotic, and uncertain world <strong>of</strong> clinical<br />
practice the most likely diagnosis at the time seems the<br />
most reasonable one to make. Thus there is a trade <strong>of</strong>f<br />
between efficiency and accuracy<br />
by deferring to guidelines and protocols,<br />
or by abandoning the patient in a misconstruing<br />
<strong>of</strong> patient-centred medicine.<br />
Uncertainty, on the other hand, can be<br />
reduced by specialisation (developing<br />
‘special interests’), or by an appeal to ‘in<br />
my clinical experience’ arguments; in<br />
other words, the long-favoured technique<br />
<strong>of</strong> denial and self-deception.<br />
Self-deception is not, <strong>of</strong> course, unique<br />
to doctors. Most drivers consider themselves<br />
‘better than average’ drivers and<br />
94% <strong>of</strong> college pr<strong>of</strong>essors rate themselves<br />
in the top half <strong>of</strong> their pr<strong>of</strong>ession. 13<br />
Nevertheless, in medicine there is a<br />
particularly long and entrenched tradition<br />
<strong>of</strong> self (and patient) deception. <strong>The</strong><br />
justification has been that, in order for<br />
to do with making sense in a complex<br />
and confusing world so that action<br />
is possible. <strong>The</strong>re are limits to living<br />
with uncertainty; the resultant fear can<br />
paralyse. In practice, given that we must<br />
act in uncertainty, 14 self-deception might<br />
just be essential.<br />
Today, however, doctors are encouraged<br />
to take a different approach. <strong>The</strong>y are<br />
encouraged to share their uncertainty<br />
with patients as a means to improving<br />
doctor–patient relations. 15 Disclosure <strong>of</strong><br />
uncertainty, or truth-telling, is about<br />
empowerment, about setting patients<br />
free to decide and to act rationally according<br />
to their true nature. But does<br />
knowledge <strong>of</strong> uncertainty, the truth,<br />
really set patients free?<br />
72 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
<strong>The</strong> view <strong>of</strong> the classical Greek philosophers,<br />
shared by much, though perhaps<br />
not all, Christian theology, is that it<br />
does. ‘And ye shall know the truth, and<br />
the truth shall make you free.’ (Gospel<br />
according to St John, chapter 8, verse 32).<br />
Ancient Stoics and most modern rationalists<br />
are at one with Christian teaching on<br />
this <strong>issue</strong>. 3<br />
Telling the truth is ‘good’. Doctors<br />
believe this (in theory) and medical<br />
regulators promote it.<br />
And yet, for some reason, arguments<br />
against truth-telling in medical practice<br />
have persisted for centuries. In 1672,<br />
French physician, priest and philosopher<br />
Samuel de Sorbiere cautioned young doctors<br />
looking to establish themselves in<br />
practice ‘what not to say’:<br />
…in order to safeguard your interests,<br />
I must tell you that medicine is a very<br />
imperfect science, that it is quite full <strong>of</strong><br />
guesswork, that it scarcely understands its<br />
subject matter, nor is it familiar with the<br />
things employed to maintain it; that the<br />
more enlightened only feel their way in<br />
it groping amidst a thick gloom; and that<br />
after having considered seriously all the<br />
matters which may be useful, collected all<br />
one’s thoughts, examined all one’s experiences,<br />
it will indeed be a wise physician<br />
who can promise relief to a poor patient. 16<br />
Of course medical knowledge has<br />
progressed dramatically since 1672;<br />
nevertheless, the net amount <strong>of</strong> disease<br />
and suffering does not appear to have<br />
been reduced. 17 Much remains unknown<br />
about how best to ‘promise relief to a<br />
[particular] poor patient’. Thus critics <strong>of</strong><br />
the uncertainty-sharing doctrine persist,<br />
arguing that patients want to deceive<br />
themselves, and to be deceived about the<br />
deficiencies <strong>of</strong> medicine, and that, rather<br />
than improving doctor–patient relations,<br />
such disclosure actually damages the relationship<br />
reducing trust, confidence and<br />
patient satisfaction. 18 Questions remain,<br />
however, as to whether the noted deleterious<br />
effect <strong>of</strong> the disclosure <strong>of</strong> uncertainty<br />
is due to the way the uncertainty<br />
was disclosed or the uncertainty itself.<br />
Despite the scientific commitment to<br />
truth and the increased access to information<br />
today, healing is not a rational<br />
science. In practice, we can eliminate<br />
neither the uncertainty nor the fear;<br />
there will always be room for clinical<br />
judgment, for appeals to ‘in my experience…’<br />
arguments. It is possible that<br />
the knowledge <strong>of</strong> uncertainty might<br />
set patients free to choose, but it won’t<br />
set them free from fear. Nor will such<br />
knowledge set doctors free from fear and<br />
enable them to act. Perhaps the disclosure<br />
<strong>of</strong> uncertainty does interfere with<br />
our effectiveness as healers? Perhaps<br />
patients do still need to be set free from<br />
anxiety so that they can heal?<br />
<strong>The</strong> problem with the disclosure <strong>of</strong><br />
uncertainty is that, not only might it<br />
kill <strong>of</strong>f our patients and our practice, but<br />
that it might also kill <strong>of</strong>f us. Doctors<br />
have some <strong>of</strong> the worst statistics when it<br />
comes to suicide, divorce and substance<br />
abuse. Perhaps we should be bolstering,<br />
rather than tearing down, the strategies<br />
developed over millennia to aid survival<br />
in practice? As that well-known physician<br />
Dr Hibbert, who chuckles rather<br />
than whistles, says: ‘Before I learned to<br />
chuckle mindlessly, I was headed to an<br />
early grave myself.’<br />
Hibbert: Lisa, I’m afraid your tummy<br />
ache may be caused by stress.<br />
Homer: Well, that’s a relief.<br />
Hibbert: Heh, yeah. Anyway, when it<br />
comes to stress, I believe laughter is the<br />
best medicine. You know, before I learned<br />
to chuckle mindlessly, I was headed for<br />
an early grave myself. (chuckles)<br />
Homer: Give it a try, honey. (Lisa tries<br />
to chuckle). 19<br />
References<br />
EtHiCs<br />
1. Rodgers R, Hammerstein O. Whistle a happy tune.<br />
Lyrics from <strong>The</strong> King And I Musical; 1951.<br />
2. Fox R. Experiment Perilous: physicians and patients<br />
facing the unknown. Glencoe, Ill: Free Press;<br />
1959.<br />
3. Berlin I. Two concepts <strong>of</strong> liberty. In: Hardy H,<br />
editor. Liberty: Isaiah Berlin. <strong>New</strong> York: Oxford<br />
University Press; 2002. p 166–217.<br />
4. Graber M, Gordon R, Franklin N. Reducing diagnostic<br />
errors in medicine: what’s the goal? Acad<br />
Med 2002; 77(10):981–92.<br />
5. Gorovitz S, MacIntyre A. Toward a theory <strong>of</strong> medical<br />
fallibility. Hastings Cent Rep 1975; 5(6):13–23.<br />
6. Montgomery K. How doctors think: Clinical<br />
judgment and the practice <strong>of</strong> medicine. <strong>New</strong> York:<br />
Oxford University Press; 2006.<br />
7. Elstein AS. Clinical reasoning in medicine. In:<br />
Higgs J, Jones MA, editors. Clinical Reasoning<br />
in the Health Pr<strong>of</strong>essions. Woburn, Mass:<br />
Butterworth-Heinemann; 1995. p 49–59.<br />
8. Berner ES, Graber ML. Overconfidence as a cause<br />
<strong>of</strong> diagnostic error in medicine. Am J Med 2008;<br />
121(5 Suppl):S2–23.<br />
9. Paget M. <strong>The</strong> Unity <strong>of</strong> Mistakes: a phenomenological<br />
interpretation <strong>of</strong> medical work. Philadelphia:<br />
Temple University Press; 1988.<br />
10. Elstein AS. Heuristics and biases: selected errors<br />
in clinical reasoning. Acad Med 1999;74(7):791–4.<br />
11. Reason J. Human Error: Cambridge University<br />
Press; 1990.<br />
12. Dowrick C, Frith L, editors. <strong>General</strong> practice and<br />
ethics: Uncertainty and responsibility. London:<br />
Routledge; 1999.<br />
13. Mele AR. Real self-deception. Behav Brain Sci<br />
1997; 20(1):91–102; discussion 3–36.<br />
14. Katz J. Why doctors don’t disclose uncertainty.<br />
Hastings Cent Rep 1984;14(1):35–44.<br />
15. Henry MS. Uncertainty, responsibility, and the<br />
evolution <strong>of</strong> the physician/patient relationship. J<br />
Med Ethics 2006;32(6):321–3.<br />
16. Katz J. <strong>The</strong> silent world <strong>of</strong> doctor and patient. <strong>New</strong><br />
York: <strong>The</strong> Free Press; 1984.<br />
17. Lantos J. Do we still need doctors? <strong>New</strong> York:<br />
Routledge; 1997.<br />
18. Johnson CG, Levenkron JC, Suchman AL,<br />
Manchester R. Does physician uncertainty affect<br />
patient satisfaction? J Gen Intern Med 1988;<br />
3(2):144–9.<br />
19. Scully B. Make room for Lisa: <strong>The</strong> Simpsons.<br />
Episode 219; 1999.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 73
EssAYs<br />
sub-threshold mental health syndromes:<br />
Finding an alternative to the medication <strong>of</strong> unhappiness<br />
Fiona Mathieson MA(Applied), DipTchg; sunny collings MBChB, MRCPsych, FRANZCP, DPH, PhD; Anthony Dowell MBChB, FRNZCGP<br />
ABstRACt<br />
Sub-threshold anxiety and depression<br />
are common presentations in primary<br />
care. <strong>The</strong>y carry a significant disability<br />
burden along with the risk <strong>of</strong> developing<br />
a frank disorder. Intervention<br />
options are limited, although there is<br />
some evidence that ultra brief interventions<br />
may be effective with this<br />
patient group. We argue that there is<br />
a need for a systematic but ultra brief,<br />
minimal contact intervention, that can<br />
be delivered by GPs or practice nurses.<br />
Such an intervention would be a form <strong>of</strong><br />
facilitated self-management, a step up<br />
from self-help, from which people could<br />
be referred on to more intensive treatment<br />
or medication if required.<br />
MesH keywords: Primary health<br />
care, mental health, psychotherapy,<br />
mental disorders<br />
CORREsPONDENCE tO:<br />
sunny Collings<br />
Director Social Psychiatry<br />
& Population Mental<br />
Health Research Unit,<br />
Otago University<br />
Wellington, <strong>New</strong> <strong>Zealand</strong><br />
sunny.collings@<br />
otago.ac.nz<br />
introduction<br />
Just over one quarter (26.5%) <strong>of</strong> primary<br />
care patients in NZ and overseas 1,2 are<br />
considered by GPs to have sub-threshold<br />
mental health syndromes. <strong>The</strong>se are<br />
combinations <strong>of</strong> signs and symptoms<br />
that do not meet the threshold for<br />
disorder in standard diagnostic systems<br />
such as DSM-IV. 3 Unlike secondary<br />
mental health service populations, the<br />
primary care mental health population<br />
includes people with a broad spectrum<br />
<strong>of</strong> undifferentiated syndromes ranging<br />
from few, mild or transient symptoms to<br />
symptom combinations and severity that<br />
meet diagnostic criteria. Often these<br />
arise in the context <strong>of</strong> social problems<br />
such as family or economic stress. In<br />
a NZ primary care sample, functional<br />
impairment was found not to differ<br />
significantly between diagnosed disorder<br />
and sub-threshold syndromes. 7 Furthermore,<br />
a subset <strong>of</strong> those with sub-threshold<br />
syndromes are at increased risk for<br />
development <strong>of</strong> clinical depression 4 or<br />
eventual suicide. 5 Sub-threshold mental<br />
health syndromes therefore represent<br />
an important morbidity and disability<br />
burden to the community, 6 in terms <strong>of</strong><br />
work and role impairment as well as<br />
distress. 7,8 It has been suggested that<br />
intervention may be warranted for up to<br />
80% <strong>of</strong> those affected. 9,10<br />
Despite the extent <strong>of</strong> morbidity burden,<br />
in <strong>New</strong> <strong>Zealand</strong> only 22% <strong>of</strong> these people<br />
receive an intervention <strong>of</strong> any kind,<br />
most commonly supportive discussion<br />
and non-specific counselling. 10 Access to<br />
interventions for sub-threshold syndromes<br />
is likely to be even less equitably<br />
distributed than access to treatment<br />
for diagnosed disorders. <strong>The</strong> evaluation<br />
<strong>of</strong> Ministry <strong>of</strong> Health–funded NZ<br />
demonstration projects for primary care<br />
services for common mental disorders<br />
and sub-threshold syndromes shows a<br />
high degree <strong>of</strong> perceived unmet need<br />
for treatment and substantial variability<br />
in what is <strong>of</strong>fered for sub-threshold<br />
syndromes. 11<br />
Given this information, the key questions<br />
are, firstly, should people with<br />
such syndromes receive an intervention<br />
and, secondly, if so, what should the<br />
intervention be? <strong>The</strong>se questions can be<br />
answered by considering the nature <strong>of</strong><br />
contemporary primary care practice, the<br />
availability <strong>of</strong> interventions, the existing<br />
evidence about interventions, the policy<br />
context, and primary care sector workforce<br />
development.<br />
Nature <strong>of</strong> primary care practice<br />
GPs face a number <strong>of</strong> challenges in the<br />
management <strong>of</strong> sub-threshold syndromes:<br />
<strong>The</strong> primary care environment<br />
is complex and chaotic, with dynamic<br />
treatment plans that change to meet the<br />
changing need <strong>of</strong> the patient, competing<br />
illness priorities and difficult socioeconomic<br />
problems. <strong>The</strong> current classification<br />
<strong>of</strong> psychiatric illness does not apply<br />
well to undifferentiated psychosocial<br />
problems in primary care. Sub-threshold<br />
syndromes do not always conform to the<br />
boundaries <strong>of</strong> less severe forms <strong>of</strong> DSM-<br />
IV defined entities. 7,12–15 In practice, GPs<br />
tend to make pragmatic management<br />
decisions based as much on functioning<br />
74 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
as on whether or not syndromes exceed a<br />
diagnostic threshold. 16,17 In this context,<br />
management <strong>of</strong> sub-threshold syndromes<br />
is inevitable, as GPs are balancing a<br />
focused and pragmatic response to competing<br />
presenting problems. 18 Common<br />
non-specific GP management strategies<br />
include giving advice and/or reassurance,<br />
sometimes in extended consultations. 19<br />
Availability <strong>of</strong> interventions<br />
Other options for sub-threshold mental<br />
health syndromes are limited. Secondary<br />
care services are not appropriate for<br />
this group, even if they were available<br />
and patients wished to use them. GPs<br />
can refer patients for generic counselling<br />
or specific psychotherapies but,<br />
despite recent policy initiatives, 20 cost<br />
may still be an important barrier. <strong>The</strong><br />
need for referral out <strong>of</strong> the practice is a<br />
barrier for both patients (due to waiting<br />
and uncertainty about eligibility for<br />
treatment) and some practitioners (due<br />
to administration and supply <strong>of</strong> trusted<br />
providers to refer to). 11,17,20 Furthermore,<br />
the notion <strong>of</strong> on-referral to a ‘specialist’<br />
or ‘expert’ is a secondary care model<br />
which may not be appropriate for the<br />
majority <strong>of</strong> these problems. <strong>The</strong> Internet<br />
<strong>of</strong>fers the possibility <strong>of</strong> direct patient<br />
access to self-management information.<br />
<strong>The</strong> HRC has funded a clinical trial <strong>of</strong><br />
Internet treatment for clinical depression<br />
(RID, i PI Dr S Nada-Raja, University <strong>of</strong><br />
Otago), which is also available to those<br />
with sub-threshold syndromes.<br />
Evidence for interventions<br />
Treatments used in primary care RCTs<br />
are commonly described generically<br />
using terms such as ‘counselling’, 21 and<br />
they are being conducted with varied<br />
clinical groups (e.g. sub-threshold<br />
depression, 22 major depression, or sub-<br />
i http://www.otago.ac.nz/rid/<br />
threshold syndromes, 23 meaning trials<br />
cannot be readily compared or replicated.<br />
<strong>The</strong>re is some limited evidence supporting<br />
the use <strong>of</strong> ultra brief interventions<br />
for sub-threshold depression in primary<br />
care, using cognitive behavioural and<br />
interpersonal–dynamic principles 24 and<br />
interpersonal psychotherapy. 25 A smaller<br />
evidence base is developing in relation to<br />
self-help for sub-threshold syndromes. 8<br />
<strong>The</strong> evidence to date indicates that the<br />
treatments best supported by evidence<br />
include exercise and relaxation training,<br />
bibliotherapy based on CBT 26,27 and webbased<br />
psycho-education. 26<br />
Many brief treatments, including selfhelp,<br />
appear to be condensed versions <strong>of</strong><br />
interventions developed to treat discrete<br />
disorders over many months. 28 Some <strong>of</strong><br />
these interventions may be too densely<br />
packed with therapeutic elements to<br />
actually be feasible over a short period.<br />
<strong>The</strong> Primary Care Initiatives Evaluation<br />
therapist survey revealed that counsellors<br />
and therapists generally considered<br />
that six sessions were too few. 20<br />
While severity <strong>of</strong> the conditions being<br />
treated may explain some <strong>of</strong> this, several<br />
therapists also described difficulties in<br />
choosing the ‘right’ approach in such<br />
a short space <strong>of</strong> time. <strong>The</strong> underlying<br />
assumption that the nature <strong>of</strong> the<br />
psychopathology is the same as for full<br />
(especially severe) disorders may be<br />
flawed, 29,30 and this may partly explain<br />
the smaller effect sizes commonly seen<br />
for more established treatments such as<br />
CBT in primary care settings, although<br />
lower distress at baseline and the effectiveness<br />
<strong>of</strong> ‘usual GP care’ may also<br />
contribute. 21 In their seminal review<br />
<strong>of</strong> psychotherapy research, leading UK<br />
psychotherapists Roth and Fonagy called<br />
for further development work on the<br />
management <strong>of</strong> sub-threshold syndromes<br />
in primary care. 28<br />
Policy context<br />
EssAYs<br />
<strong>The</strong> Primary Health Care Strategy 31<br />
prompted a new direction for NZ<br />
primary health care, within an overarching<br />
public health framework. <strong>The</strong><br />
vehicle for achieving the changes was<br />
Primary Health Organisations (PHOs),<br />
which have evolved from a range <strong>of</strong><br />
other provider entities, resulting in<br />
diversity in philosophical approaches,<br />
capacities and rates <strong>of</strong> development, and<br />
different expectations with respect to<br />
infrastructure and workforce. 20 <strong>The</strong>se<br />
structures and the revision <strong>of</strong> funding<br />
mechanisms made it possible for mental<br />
health services to be developed as an<br />
integral part <strong>of</strong> PHOs and these are<br />
now embedded as a core part <strong>of</strong> funded<br />
primary care activity. <strong>The</strong> expectation<br />
is that primary care will manage<br />
mental disorders <strong>of</strong> ‘mild’ to ‘moderate’<br />
severity and also be proactive in mental<br />
health promotion (with a possible hope<br />
that this will reduce incident cases <strong>of</strong><br />
frank disorder). Clearly in this policy<br />
context there is an intention to address<br />
sub-threshold syndromes given their<br />
position in this spectrum.<br />
Primary care sector<br />
workforce development<br />
<strong>The</strong> evaluation <strong>of</strong> the Primary Mental<br />
Health Initiatives showed that there<br />
was great diversity among clinicians<br />
providing psychological interventions,<br />
in terms <strong>of</strong> pr<strong>of</strong>essional and theoretical<br />
backgrounds. <strong>The</strong>re will need to be<br />
considerable primary mental health<br />
workforce expansion and skill enhancement<br />
in order to meet the extent <strong>of</strong><br />
unmet need. Existing staff working in<br />
this area have particularly emphasised<br />
the need for skill development in brief<br />
interventions. 20 Substantial work will<br />
be required in relation to this, as most<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 75
EssAYs<br />
training for psychological treatments is<br />
time-consuming, whether it is delivered<br />
intensively or intermittently.<br />
should people with subthreshold<br />
mental health<br />
syndromes receive<br />
intervention and, if so, what?<br />
We suggest that the evidence supports<br />
intervention on the grounds <strong>of</strong> relief<br />
<strong>of</strong> suffering and the restoration <strong>of</strong><br />
functioning. However, the over-riding<br />
argument is that the nature <strong>of</strong> primary<br />
care practice means that people with<br />
these syndromes are already receiving<br />
interventions <strong>of</strong> various kinds. On the<br />
whole these are likely to be pragmatic<br />
approaches to common and complex<br />
presentations, <strong>of</strong> the kind that GPs<br />
have been delivering for many decades,<br />
variably infused with evidence as it<br />
comes to hand. In light <strong>of</strong> this, and the<br />
need to be thoughtful about the use <strong>of</strong><br />
scarce health resources, the focus needs<br />
to be on the most effective way <strong>of</strong><br />
delivering this care.<br />
A useful framework for considering<br />
the problem <strong>of</strong> provision <strong>of</strong> treatment<br />
for mental health problems in the face<br />
<strong>of</strong> scarce resources is that proposed by<br />
Jorm. 26 <strong>The</strong> model suggests that a range<br />
<strong>of</strong> responses is available for subpopulations<br />
with varying levels <strong>of</strong> symptoms<br />
and impairment. As symptoms and<br />
impairment increase from a low base<br />
due to stresses in everyday life, 32,33 so<br />
the interventions called into play move<br />
from the first ‘wave’ <strong>of</strong> self-help using<br />
everyday strategies such as exercise<br />
and talking to family or friends,<br />
through a second ‘wave’ <strong>of</strong> facilitated<br />
self-help. <strong>The</strong> next ‘wave’ is pr<strong>of</strong>essional<br />
help-seeking, with, finally,<br />
provision <strong>of</strong> specific treatments once<br />
severity is at the disorder threshold.<br />
This approach is consistent with the<br />
‘stepped care’ model now commonly<br />
accepted as a structure for funding<br />
mental health services.<br />
In this framework, presentation or<br />
detection in primary care represents<br />
part <strong>of</strong> the first wave <strong>of</strong> pr<strong>of</strong>essional<br />
help-seeking. Primary care practitioners<br />
need a range <strong>of</strong> management options<br />
to call on at this level, and there have<br />
been calls for investment in research to<br />
establish whether the use <strong>of</strong> ‘minimal’<br />
interventions are an efficient method <strong>of</strong><br />
delivering psychological treatments. 34<br />
We have been fortunate to receive<br />
Health Research Council funding to<br />
develop an ultra-brief intervention that<br />
can be delivered by a trained but nonmental<br />
health–specialist primary care<br />
practitioner (e.g. practice nurse or GP).<br />
This will involve a pragmatic two–three<br />
contact intervention to reduce the disability<br />
associated with sub-threshold<br />
mental health syndromes, as a step up<br />
from self help in the ‘wave’ framework.<br />
<strong>The</strong> intervention will require minimal<br />
additional training; and we hope it will<br />
reduce the need for referral on, thus<br />
maintaining patient links with the<br />
primary care team; and will reinforce<br />
the patient’s existing self-help strategies,<br />
consistent with the strengths-based<br />
approaches now being emphasised in NZ<br />
mental health practice. Following development<br />
we hope to take the intervention<br />
to pragmatic clinical trial in the NZ<br />
primary care setting.<br />
Novel intervention research such as this<br />
is central to meeting demand in primary<br />
care mental health in NZ and it will<br />
contribute to the national and international<br />
evidence base for the management<br />
<strong>of</strong> this common and burdensome<br />
problem. We acknowledge that secondary<br />
care mental health clinicians may be<br />
doubtful about the idea <strong>of</strong> an ultra brief<br />
intervention that can be used by people<br />
with a minimum <strong>of</strong> training: ‘Where are<br />
the formulations? <strong>The</strong> risk assessments?<br />
<strong>The</strong> highly trained mental health clinicians?’<br />
However, current mental health<br />
funding policy in <strong>New</strong> <strong>Zealand</strong> provides<br />
access to sophisticated, expensive treatment,<br />
which is in relatively short supply,<br />
and is aimed at diagnosable disorders.<br />
Most primary care patients cannot<br />
jump this high threshold for access to<br />
services, and this is probably appropriate.<br />
However, below this threshold there a<br />
large group <strong>of</strong> people with, at best, (and<br />
only recently) partly-met need. We aim<br />
to help meet this need.<br />
References<br />
1. <strong>The</strong> MaGPIe research group. <strong>The</strong> nature and<br />
prevalence <strong>of</strong> psychological problems in <strong>New</strong><br />
<strong>Zealand</strong> primary health care: a report on Mental<br />
Health and <strong>General</strong> Practice Investigation. NZMJ<br />
2003;116(1171):1–15.<br />
2. Ustun T, Sartorius N. Mental illness in general<br />
health care. England: Wiley, 1995.<br />
3. American Psychiatric Association A. DSM IV.<br />
Washington DC: American Psychiatric Association;<br />
1995.<br />
4. Kessler R, Zhao S, Blazer D, Swartz M. Prevalence,<br />
correlates, and course <strong>of</strong> minor depression in<br />
the national comorbidity survey. J Affect Disord<br />
1997;45(1–2):19–30.<br />
5. Sadek N, Bona J. Subsyndromal symptomatic<br />
depression: a new concept. Depress Anxiety<br />
2000;12:30–39.<br />
6. Judd L, Schettler P, Akiskal H. <strong>The</strong> prevalence,<br />
clinical relevance and public health significance<br />
<strong>of</strong> subthreshold depressions. Psychiatr Clin North<br />
Am 2002;25:685–698.<br />
7. Hickie I. Primary care psychiatry is not specialist<br />
psychiatry in general practice. Med J Aust<br />
1999;170:171–173.<br />
8. Jorm AF, Griffiths KM. Population promotion <strong>of</strong><br />
informal self help strategies for early intervention<br />
against depression and anxiety. Psychol Med<br />
2006;36(3–6).<br />
9. Wagner H, Burns B, Broadhead W, Yarnall K,<br />
Sigmon A, Gaynes B. Minor depresssion in family<br />
practice: functional morbidity, co-morbidity,<br />
service utilisation and outcomes. Psychol Med<br />
2000;30:1377–1390.<br />
10. <strong>The</strong> MaGPIe Research Group. <strong>The</strong> treatment <strong>of</strong><br />
common mental health problems in general practice.<br />
Fam Pract 2006;23:53–59.<br />
11. Dowell A, Garrett S, Collings S, McBain L, McKinlay<br />
E, Stanley J. Primary Mental Health Initiatives:<br />
Interim Report. Wellington: School <strong>of</strong> Medicine &<br />
Health Sciences, University <strong>of</strong> Otago, Wellington,<br />
2007;242.<br />
12. <strong>The</strong> MaGPIe Research Group. <strong>General</strong><br />
practitioner recognition <strong>of</strong> mental ilness in the<br />
absence <strong>of</strong> a ‘gold standard’. Aust NZ J Psychiatry<br />
2004;38:789–794.<br />
13. Goldberg D. Plato versus Aristotle: categorical and<br />
dimensional models for common mental disorders.<br />
Compr Psychiatry 2000;41:8–13.<br />
14. Backenstrass M, Frank A, Joest K, Hingman S,<br />
Mundt C, Kronmuller K. A comparative study<br />
<strong>of</strong> nonspecific depressive symptoms and minor<br />
depression regarding functional impairment and<br />
associated characteristics in primary care. Compr<br />
Psychiatry 2006;47:35–41.<br />
76 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
15. Collings S. Clinical practice is as important as<br />
diagnosis. BMJ 2001;322(13 Jan):80–81.<br />
16. Collings S, MaGPie Research Group. Disability and<br />
the detection <strong>of</strong> mental disorder in primary care. Soc<br />
Psychiatry Psychiatr Epidemiol 2005;40:994–1002.<br />
17. Dew K, Dowell A, McLeod D, Collings S, Bushnell<br />
J. ‘This glorious twilight zone <strong>of</strong> uncertainty’: mental<br />
health consultations in general practice in <strong>New</strong><br />
<strong>Zealand</strong>. Soc Sci Med 2005;61(6):1189–1200.<br />
18. Klinkman MS. Competing demands in psychosocial<br />
care: A model for the identification and<br />
treatment <strong>of</strong> depressive disorders in primary care.<br />
Gen Hosp Psychiatry 1997;19:98–111.<br />
19. Hemmings A. A systematic review <strong>of</strong> the effectiveness<br />
<strong>of</strong> brief psychological therapies in primary<br />
health care. Fam Syst Health 2000;18(3):279–313.<br />
20. Dowell A, Garrett S, Collings S, McBain L, McKinlay<br />
E, Stanley J. Evaluation <strong>of</strong> the Primary Mental<br />
Health Initiatives: summary report 2008. Wellington:<br />
Otago University Wellington and Ministry<br />
<strong>of</strong> Health; 2008.<br />
21. Bower P. <strong>The</strong> clinical effectiveness <strong>of</strong> couselling in<br />
primary care: a systematic review and meta-analysis.<br />
Psychol Med 2003;33:203–215.<br />
22. Willemse G, Smit F, Cuijpers P, Tiemens B. Minimal<br />
contact psychotherapy for sub-threshold depression<br />
in primary care: a randomised controlled trial.<br />
Br J Psychiatry 2004;185:416–421.<br />
23. Mead N, MacDonald W, Bower P, Lovell K, Richards<br />
D, Roberts C, et al. <strong>The</strong> clinical effectiveness <strong>of</strong> guided<br />
self-help versus waiting-list control in the management<br />
<strong>of</strong> anxiety and depression: a randomised<br />
controlled trial. Psychol Med 2005;35:1633–1643.<br />
24. Barkham M, Shapiro DA, Hardy GE, Rees A. Psychotherapy<br />
in two-plus-one sessions: Outcomes <strong>of</strong><br />
a randomized controlled trial <strong>of</strong> cognitive-behavioral<br />
and psychodynamic-interpersonal therapy for<br />
subsyndromal depression. J Consult Clin Psychol<br />
1999;67(2):201–211.<br />
25. Klerman GL, Budman S, Berwick D, Weissman<br />
MM, Damico-White J, Demby A, et al. Efficacy <strong>of</strong><br />
a brief psychosocial intervention for symptoms <strong>of</strong><br />
stress and distress among patients in primary care.<br />
Med Care 1987;25(11):1078–88.<br />
26. Jorm A, Griffiths K, Christensen H, Parslow R.<br />
Actions taken to cope with depression at different<br />
levels <strong>of</strong> severity: a community survey. Psychol<br />
Med 2004;34:293–299.<br />
27. den Boer P, Wiersma D, van den Bosch R. Why is<br />
self-help neglected in the treatment <strong>of</strong> emotional<br />
disorders? Psychol Med 2004;34:959–971.<br />
28. Roth A, Fonagy P. What works for whom? A critical<br />
review <strong>of</strong> psychotherapy research. 2nd ed. <strong>New</strong><br />
York: Guilford Press; 2005.<br />
29. Parker G. Evaluating treatments for the mood<br />
disorders: time for the evidence to get real. Aust<br />
NZ J Psychiatry 2004;38(6):408–414.<br />
30. Parker G, Parker I, Brotchie H, Stuart S. Interpersonal<br />
psychotherapy for depression? <strong>The</strong> need<br />
to define its ecological niche. J Affect Disord<br />
2006;95(1–3):1–11.<br />
31. Ministry <strong>of</strong> Health. <strong>The</strong> Primary Health Care<br />
Strategy. Wellington: Ministry <strong>of</strong> Health; 2001.<br />
32. Mulder R. An epidemic <strong>of</strong> depression or the medicalisation<br />
<strong>of</strong> unhappiness? NZ Family Physician<br />
2005;32(3):161–163.<br />
33. Mulder R. Psychiatric illness in primary care:<br />
whom should we treat? NZMJ 2003;116(1171).<br />
34. Bower P, Gilbody S. Stepped care in psychological<br />
therapies: access, effectiveness and efficiency:<br />
Narrative literature review. Br J Psychiatry<br />
20 05;186(1):11–17.<br />
Mind over matter—implications for general practice<br />
Andrew corin MBChB, FRNZCGP<br />
For centuries, it has been recognised<br />
that the mind has power over the<br />
body, and experience <strong>of</strong> external<br />
stimuli is subjective and variable. This<br />
paper will explore some <strong>of</strong> the evidence<br />
for this, and seek to apply the phenomenon<br />
to a health care setting.<br />
In the <strong>New</strong> <strong>Zealand</strong> (NZ) primary care<br />
environment where patients are increasingly<br />
critical <strong>of</strong> the service they receive,<br />
where retention <strong>of</strong> capitation base is<br />
important, and recruitment <strong>of</strong> appropriate<br />
new patients is desirable and, most importantly,<br />
where efficient delivery <strong>of</strong> quality<br />
health care is paramount, a good under-<br />
CORREsPONDENCE tO:<br />
Andrew P Corin<br />
CentralMed, 434 Devonport Rd,<br />
Tauranga, <strong>New</strong> <strong>Zealand</strong><br />
andrewc@centralmed.co.nz<br />
standing <strong>of</strong> the relationship between<br />
expectations and experience is vital. 1<br />
Patients in primary care are increasingly<br />
mobile, and many will seek provision <strong>of</strong><br />
their health care from various sources,<br />
depending on the specific problem. This<br />
may be due to a desire for confidentiality,<br />
an opportunity to seek specialised<br />
care, or merely a geographical or temporal<br />
convenience. <strong>The</strong> fourth reason for<br />
patient movement is dissatisfaction with<br />
care provision, from phone to reception<br />
to nursing and doctor involvement. <strong>The</strong><br />
advent <strong>of</strong> fully capitated general practice<br />
funding in NZ is encouraging patients<br />
to seek all their primary care needs from<br />
the one provider, as subsidy is enrolment-specific<br />
to one practice.<br />
If general practitioners and primary care<br />
business owners are able to understand<br />
and cooperate with patient expectations,<br />
EssAYs<br />
they will have better opportunity to manage<br />
patient movement and financial risk, as<br />
well as provide improved health outcomes.<br />
Many studies have been undertaken to<br />
demonstrate the psychological relationship<br />
between the brain’s expectation <strong>of</strong><br />
a sensory input, and the actual report<br />
<strong>of</strong> that experience. 2–7 Most famous are<br />
the experiments involving wine tasting<br />
and pain stimulation. In these various<br />
blinded experiments, different subjects<br />
reported variable experiences despite<br />
identical sensory challenges. Being told<br />
that you are drinking an expensive<br />
wine, or about to receive a reduced pain<br />
impulse, results in tasting a fine wine<br />
or feeling less pain, despite the wine<br />
being poor or pain level unchanged,<br />
respectively. <strong>The</strong> conclusions are that the<br />
pre-frontal cortex modulates the actual<br />
sensory assessment to fit with a pre-determined<br />
expectation. Indeed, Magnetic<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 77
EssAYs<br />
Resonance Imaging (MRI) analysis<br />
demonstrates complex cerebral processes<br />
involved in the association <strong>of</strong> expectation<br />
and subjective pain experience. 6 In<br />
this study subjects with a positive (more<br />
optimistic) expectation <strong>of</strong> the pain experience<br />
reported reduced pain levels. MRI<br />
has also been used to demonstrate that<br />
altering a subject’s expectation <strong>of</strong> a specific<br />
taste will modify brain activity in<br />
that related region <strong>of</strong> the cortex, and so<br />
subjectively alter the taste experience. 7<br />
<strong>The</strong> relevance to primary care is that if<br />
GPs able to understand the expectations<br />
<strong>of</strong> their patients and over time create an<br />
expectation set that is one <strong>of</strong> satisfaction<br />
and wellness, the level <strong>of</strong> health,<br />
compliance with treatment and patient<br />
retention will be maximised. 8<br />
More specifically, the following example<br />
may help:<br />
Ms D is a 46-year-old woman. She is<br />
eight weeks post-laparoscopic cholecystectomy,<br />
and suffering severe right subscapula<br />
pain, with nausea, weight loss<br />
and insomnia. She has been thoroughly<br />
assessed in recent weeks by her surgeon<br />
as an outpatient and then an inpatient<br />
for six days, with no cause for her pain<br />
found. She was treated with strong analgesia,<br />
without improvement.<br />
Her sister, who is a patient <strong>of</strong> mine,<br />
suggested that a second opinion from me<br />
would help her. Examination <strong>of</strong> Ms D<br />
was normal, apart from her anxious and<br />
exhausted appearance.<br />
My suspicion was that there was a complex<br />
neuralgia process here, heightened<br />
by her anxiety, and I recommended cessation<br />
<strong>of</strong> her tramadol, and started a low<br />
dose <strong>of</strong> gabapentin. Reassurance was an<br />
important part <strong>of</strong> the consultation.<br />
At review one week later Ms D reported<br />
almost full resolution <strong>of</strong> her pain,<br />
insomnia and nausea after taking one<br />
gabapentin dose! At that consult she also<br />
confessed to having significant preoperative<br />
anxiety regarding the outcome<br />
<strong>of</strong> the surgery.<br />
I believe that the dramatic resolution <strong>of</strong><br />
her pain syndrome was largely mediated<br />
by her state <strong>of</strong> mind, and the expectation<br />
created at the consultation <strong>of</strong><br />
improvement. In addition, I suspect that<br />
her atypical pain behaviour following<br />
surgery may well have been due to her<br />
anxious expectation <strong>of</strong> a poor outcome<br />
from the operation.<br />
<strong>The</strong>re are two <strong>issue</strong>s which should be<br />
considered and addressed by a GP concerned<br />
about the realities <strong>of</strong> maintaining<br />
a successful medical practice. Firstly,<br />
and waiting environment, being given<br />
opportunity to talk and be listened to by<br />
the doctor, having clear communication<br />
and a management plan from the doctor,<br />
a focus on preventative medicine, and<br />
having confidence in the pr<strong>of</strong>essionalism<br />
and skill <strong>of</strong> the doctor. 9 Patients gave<br />
higher priority than GPs to availability<br />
and accessibility <strong>of</strong> the practice and seeing<br />
the same GP. 10<br />
A review <strong>of</strong> the literature on patient priorities<br />
found that the most common priorities<br />
were informative-ness, ‘humane-ness’,<br />
and competence/accuracy. 11 Other aspects<br />
included involving patients in decisions,<br />
time for care, availability/accessibility,<br />
exploring patients’ needs, good communication<br />
and availability <strong>of</strong> special services.<br />
Part <strong>of</strong> an effective clinical and consultation relationship<br />
involves assessing expectations and agendas, and<br />
educating the patient where those expectations and<br />
agendas are inappropriate<br />
they should seek to have an understanding<br />
<strong>of</strong> the expectations <strong>of</strong> their patients.<br />
This will <strong>of</strong>ten not be immediately obvious<br />
or volunteered, and a relationship<br />
<strong>of</strong> trust may be necessary before honest<br />
expectations are volunteered. Secondly,<br />
they should aim to create a set <strong>of</strong> expectations<br />
that are associated with patient<br />
satisfaction, and thus achieve business<br />
growth, patient health and staff gratification.<br />
<strong>The</strong> expectation <strong>of</strong> the patient<br />
can reasonably be influenced by their<br />
understanding <strong>of</strong> the dynamics <strong>of</strong> the<br />
medical practice they attend. If the staff<br />
consistently provides prompt, informative<br />
and pr<strong>of</strong>essional health care, this<br />
will become the expectation and, indeed,<br />
the experience, even when occasionally<br />
the quality <strong>of</strong> care is substandard.<br />
Issues to consider here are acceptable<br />
access and cost, acceptable waiting times<br />
Webb and Lloyd identified two strong<br />
factors which influenced the management<br />
behaviour <strong>of</strong> GPs in two North<br />
London practices. 12 <strong>The</strong> first was the<br />
patient’s level <strong>of</strong> anxiety. If a given<br />
patient presented with a problem about<br />
which they were particularly anxious,<br />
they were more likely to receive either<br />
a prescription or hospital referral. <strong>The</strong><br />
second was patient expectation. This<br />
suggests that the patient also communicated<br />
the expectation <strong>of</strong> either prescription<br />
or referral.<br />
A medical practitioner needs to balance<br />
patient expectations with the realities<br />
<strong>of</strong> clinically appropriate and responsible<br />
practice. It is obviously not appropriate<br />
to prescribe antibiotics at every patient<br />
request, nor order every test a patient demands,<br />
nor refer without restraint. Part <strong>of</strong><br />
an effective clinical and consultation re-<br />
78 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
lationship involves assessing expectations<br />
and agendas, and educating the patient<br />
where those expectations and agendas<br />
are inappropriate. <strong>The</strong> GP and their team<br />
are well placed and generally respected<br />
opinion-holders, such that in the space <strong>of</strong><br />
a consultation unreasonable expectations<br />
can be identified and modified.<br />
<strong>New</strong>somel and Wright present an excellent<br />
summary with exhaustive references<br />
relating to the theories <strong>of</strong> satisfaction. 13<br />
In particular, the ‘zone <strong>of</strong> tolerance’<br />
seems to fit the medical model. Here<br />
patients have a zone <strong>of</strong> expectation from<br />
the health care contact. If the actual<br />
service delivery falls within this zone,<br />
or above it, then satisfaction is experienced.<br />
<strong>The</strong> more important the health<br />
experience, the more narrow the zone <strong>of</strong><br />
tolerance. If the expectation levels are<br />
too high, the patient is more likely to<br />
be dissatisfied more <strong>of</strong>ten. However, the<br />
theory propounded to under promise to<br />
achieve higher levels <strong>of</strong> satisfaction is<br />
not well supported.<br />
Clearly, it is important to understand<br />
what the zone <strong>of</strong> expectation is for a patient,<br />
reinforce this when it is appropriate,<br />
and seek to adjust it when inappropriate.<br />
GPs, by virtue <strong>of</strong> their training<br />
and experience, are generally adept at<br />
adapting style and structure in the consultation<br />
to suit the needs <strong>of</strong> the patient<br />
and doctor. Thus, it should present no<br />
significant challenge to suggest that<br />
the GP assesses the expectations <strong>of</strong> the<br />
patient on a regular basis, and adjusts<br />
the interaction accordingly. Two patients<br />
who receive identical care may evaluate<br />
the consultation differently, according to<br />
their expectations. 14,15<br />
A recent US survey <strong>of</strong> physician attitudes<br />
to prescribing ‘placebos’ revealed a<br />
reasonably widespread acceptance <strong>of</strong> the<br />
role <strong>of</strong> exploiting the patient’s expectation<br />
<strong>of</strong> a treatment by using a pharmacologically<br />
neutral substance to achieve a<br />
therapeutic outcome. 16<br />
<strong>The</strong> opening gambit <strong>of</strong> a consultation<br />
such as ‘What can I do for you?’ or ‘how<br />
can I help today?’ provides opportunity<br />
for the patient to verbalise and GP to<br />
assess the agenda and expectation set for<br />
the interaction. In addition, during and<br />
at the end <strong>of</strong> the consultation there can<br />
be opportunity to reinforce the management<br />
message. This can take the form <strong>of</strong><br />
simple repetition, or may include positive<br />
suggestion such as ‘I am sure you will<br />
improve with this medication’. Whilst<br />
this is not medico-legally binding promise-making,<br />
it can be a very powerful tool<br />
to turn the pre-frontal cortex activity<br />
into one that supports the optimal health<br />
goals <strong>of</strong> the doctor and patient.<br />
In summary then, understanding<br />
patients and their expectations from the<br />
health care experience is important in<br />
targeting intervention and management.<br />
Such an understanding will provide opportunity<br />
for maximising the success <strong>of</strong><br />
health care, from building location and<br />
design, to staffing and training, to education<br />
strategies and models <strong>of</strong> chronic<br />
care delivery, as well as to the nuances<br />
<strong>of</strong> the individual consultation.<br />
References<br />
1. Gabbott M, Hogg G. Competing for Patients:<br />
Understanding Consumer Evaluation <strong>of</strong> Primary<br />
Care. J Manag Med 1994;8(1):12–18.<br />
2. Koyama T, McHaffie J, Laurienti P, Coghill<br />
RC. <strong>The</strong> subjective experience <strong>of</strong> pain: where<br />
expectation becomes reality. Proc Natl Acad Sci<br />
2005;102(36):12950–12955.<br />
3. d’Hauteville F, Fornerino M, Perrouty J. Disconfirmation<br />
<strong>of</strong> taste as a measure <strong>of</strong> region <strong>of</strong> origin<br />
equity: An experimental study on five French wine<br />
regions. Intl J Wine Bus Res 2007;19(1):33–48.<br />
4. Coggins A, Beardsmore A. Blind Faith. <strong>The</strong> Strad<br />
(<strong>New</strong>squest Specialist Media Limited). Feb 2007.<br />
5. Taber G, Mondavi R. Judgement <strong>of</strong> Paris: California<br />
vs. France and the Historic 1976 Paris Tasting<br />
That Revolutionized Wine. Simon and Schuster<br />
Adult Publishing Group; Nov 2006.352.<br />
6. Berk L. Beta-endorphins and HGH increase are associated<br />
with both the anticipation and experience<br />
<strong>of</strong> mirthful laughter. Paper presented at: American<br />
Physiological Society session at Experimental Biology;<br />
2006 March 31; SanFrancisco, CA.<br />
7. Sarinopoulos I, Dixon GE, Short SJ, Davidson RJ,<br />
Nitschke JB.Brain mechanisms <strong>of</strong> expectation<br />
associated with insula and amygdala response<br />
EssAYs<br />
to aversive taste: Implications for placebo. Brain<br />
Behav and Immun 2006;20:120–132.<br />
8. Kumar R, Kirking D, Hass S, et al. <strong>The</strong> association<br />
<strong>of</strong> consumer expectation, experiences and satisfaction<br />
with newly prescribed medicines. Qual Life<br />
Res 2007;16(7):1127–1136.<br />
9. Rahman MM, Rahman S, Begum N, Asaduzzaman<br />
AM, Shahjahan M, Firoz A, Metul MS. Client<br />
expectation from doctors: Expectation—reality<br />
gap. KUMJ 2007;5 (4):566–573.<br />
10. Vedsted P, Mainz J, Lauritzen T, Olesen F. Patient<br />
and GP agreement on aspects <strong>of</strong> general practice<br />
care. Fam Pract 2002;19:339–343.<br />
11. Wensing M, Jung H, Mainz J, Olesen F, Grol R.<br />
A systematic review <strong>of</strong> the literature on patient<br />
priorities for general practice care. Soc Sci Med<br />
1998;47(10):1573–1588.<br />
12. Webb S, Lloyd M. Prescribing and referral<br />
in general practice: a study <strong>of</strong> patients’<br />
expectations and doctors’ actions. Br J Gen<br />
Pract.1994;44(381):165–169.<br />
13. <strong>New</strong>somel P, Wright G. A review <strong>of</strong> patient<br />
satisfaction: 1. Concepts <strong>of</strong> satisfaction. Br Den J<br />
1999;186(4):161–165.<br />
14. Lilford RJ, Brown CA. Using outcomes to monitor<br />
the quality <strong>of</strong> clinical practice—handle with care.<br />
BMJ 2007;335:648–650.<br />
15. Conway T, Willcocks S. <strong>The</strong> role <strong>of</strong> expectations in<br />
the perception <strong>of</strong> health care quality: developing<br />
a conceptual model. Intl J Health Care Qual Assur<br />
Inc Leadersh Health Serv 1997;10(2-3):131–40.<br />
16. Tilburt J, Emanuel E, Kaptchuk T, Curlin F, Miller<br />
FG. Prescribing ‘placebo treatments’: results <strong>of</strong><br />
national survey <strong>of</strong> US internists and rheumatologists.<br />
BMJ 2008;337:a1938.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 79
LETTERS TO THE EDITOR<br />
Vignette from the ‘olden days’<br />
Many years ago, when I was a Southland country GP, I<br />
was called to visit an elderly lady living alone. <strong>The</strong> front<br />
‘fence’ was an indication <strong>of</strong> what was to come. <strong>The</strong> neglected<br />
bushes had grown to tall trees, shading the house. <strong>The</strong> decaying<br />
farmhouse had not seen paint or maintenance in many<br />
years.<br />
Entering through the billiard room <strong>of</strong> this erstwhile mansion,<br />
I noticed the large arched skylight leaking at the corners,<br />
with green mould growing down the walls. In the dim and<br />
dusty bedroom I found an emaciated 80-year-old lady thin as a<br />
Belsen concentration camp victim. <strong>The</strong> low point <strong>of</strong> the clinical<br />
examination was finding wriggling maggots under each<br />
shrunken breast.<br />
Transferred to hospital, she died in a few days. <strong>The</strong> frail old<br />
soul would have had little resistance to the basal pneumonia<br />
that ended her days. On enquiry, it transpired that she had<br />
lived alone for many years, the last <strong>of</strong> the family, after caring<br />
for her father until he died <strong>of</strong> old age.<br />
She had been living without heating (in Southland winters!)<br />
and severely restricting her diet, all to save money to<br />
bequeath to Scottish cousins she had never met. How strange<br />
are the ways <strong>of</strong> the human race! I trust the inheritors <strong>of</strong> such<br />
hardly come by money were duly appreciative.<br />
Lance Austin<br />
Concern about the name change<br />
read ePulse 16 September with much interest noting the sug-<br />
I gestion that the journal invites nurses and community pharmacists<br />
to be a part <strong>of</strong> the journal and that there be a move to<br />
focus on primary health care with a name change to that <strong>of</strong><br />
the Journal <strong>of</strong> Primary Health Care. Nurses and pharmacists<br />
already have their journals.<br />
<strong>The</strong> journal as I understand its role is to focus on medical<br />
<strong>issue</strong>s and the family physician. <strong>The</strong> cornerstone <strong>of</strong> primary<br />
care is about the credentials <strong>of</strong> the practising family physician.<br />
What I hope your role as the new editor is, firstly, to<br />
attract more enthusiasm from colleagues to submit articles for<br />
publication. Letters to the Editor might occupy one section <strong>of</strong><br />
the journal.<br />
If ever a change in name is contemplated then might I suggest<br />
that the college become, <strong>The</strong> <strong>Royal</strong> <strong>New</strong> <strong>Zealand</strong> <strong>College</strong><br />
<strong>of</strong> Family Physicians, then we achieve equity with our Physician<br />
colleagues in other branches <strong>of</strong> medicine. <strong>The</strong> medical<br />
specialty <strong>of</strong> primary care therefore is a focus on the interaction<br />
between the patient as a family member and the attending<br />
family physician.<br />
It is an unwise move to dilute this role <strong>of</strong> the GP for which<br />
the primary care strategy appears to be achieving.<br />
Henare Broughton<br />
Homeopathy and acupuncture reviews are not CME<br />
am concerned to find the Journal Review Service continuing<br />
I to publish reviews <strong>of</strong> homeopathy and acupuncture under the<br />
guise <strong>of</strong> ‘continuing medical education’. 1 I am, however, heartened<br />
by Dr Tony Hanne’s trenchant criticism <strong>of</strong> homeopathy.<br />
This absurd belief system has no place in any medical journal.<br />
Acupuncture can be similarly criticised. Many <strong>of</strong> the<br />
reviews are unintentionally funny. Could there be anything<br />
more absurd than the statement2 ‘One could also argue that a<br />
major acuppoint, e.g. LR-3, from the Liver meridian for detoxification<br />
should have been included in the prescription used.’?<br />
Such foolishness reminded me <strong>of</strong> a spo<strong>of</strong> <strong>of</strong> a British Medical<br />
Journal article entitled ‘Delayed ketoalkalotic effects <strong>of</strong><br />
aldosterone-producing adenoma in a man with a pig’s head’.<br />
Although I still have a copy <strong>of</strong> this I am unsure as its provenance.<br />
<strong>The</strong> new Editor has promised to improve the journal even<br />
further. Please let us drop the alternative medical nonsense<br />
and have more useful material from people like Pr<strong>of</strong>essor<br />
Bruce Arroll and others.<br />
Dr John Welch MBChB FRNZCGP DipAvMed<br />
Competing Interests: I am a reformed acupuncturist, member <strong>of</strong> the<br />
<strong>New</strong> <strong>Zealand</strong> Skeptic’s Society for whom I write a column (Hokum Locum)<br />
on alternative medicine.<br />
References<br />
1. NZFP 2008; 35:74–75.<br />
2. NZFP 2008; 35:137.<br />
Letters may respond to published papers, briefly report original research or case reports, or raise matters <strong>of</strong> interest relevant to<br />
primary health care. <strong>The</strong> best letters are succinct and stimulating. Letters <strong>of</strong> no more than 400 words may be emailed to:<br />
editor@rnzcgp.org.nz. All letters are subject to editing and may be shortened.<br />
80 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
Intravenous Vitamin C<br />
Enjoyed seeing the Vitamin C article in the recent NZMJ<br />
[sic]. Was interesting and informative. I enjoy incorporating<br />
some nutritional work into my own general practice. Would<br />
enjoy seeing more nutritional medicine type articles over time.<br />
Dr Helen Smith, GP<br />
How disappointing that the NZFP saw fit to publish a<br />
summary <strong>of</strong> personal opinion and anecdote as an ‘original<br />
scientific paper’ (Vitamin C: Evidence, application and commentary.<br />
Melissa Ge et al. NZFP 2008;35:312–318).<br />
After a careful read <strong>of</strong> the claims that megadoses <strong>of</strong> vitamin<br />
C can cure a wide range <strong>of</strong> terminal illnesses as well as<br />
infectious diseases I was quite intrigued and sceptical. When<br />
looking further however, I noticed the references used to<br />
authenticate this paper do not provide the evidence to support<br />
the claims.<br />
Here is a single example: ‘Over the past 10-year period I have<br />
treated over 9550 patients with large doses <strong>of</strong> vitamin C’. 1 <strong>The</strong><br />
author <strong>of</strong> this paper, Cathcart, does not discuss these patients—<br />
he only refers to single episodes and individual results. He also<br />
mentions that when treating bacterial infections ‘Ascorbic Acid<br />
should be used with the appropriate antibiotic.’ He reports that<br />
this broadens the spectrum for the antibiotic but the evidence is<br />
lacking any specific information—it is just noted in passing.<br />
<strong>The</strong> authors <strong>of</strong> this paper claim that Cathcart ‘was giving<br />
megadoses <strong>of</strong> vitamin C to patients with polio, diphtheria,<br />
herpes, chicken pox, influenza, measles, mumps, pneumonia,<br />
viral encephalitis and Shiga toxin poisoning.’ This scientific<br />
paper was written before the availability <strong>of</strong> the polio vaccine<br />
in the 1940s. <strong>The</strong> patients treated with the IV Vitamin C were<br />
‘considered infected’ during an epidemic, which is different<br />
than a confirmed case <strong>of</strong> polio. 1 Surely the authors <strong>of</strong> this<br />
paper aren’t suggesting that vitamin C is a treatment for polio<br />
based on one article.<br />
<strong>The</strong> authors advocated ‘Several case studies, small clinical<br />
trials and in vitro experiments have been published suggesting<br />
that vitamin C at the correct dosage has anti-cancer effects.’<br />
This might lead one to believe that vitamin C can hinder<br />
cancer cells from metastasising when really the authors are<br />
<strong>of</strong>fering ‘palliative’ care for terminal patients.<br />
<strong>The</strong>re is no disclosure <strong>of</strong> the possible adverse effects. Extreme<br />
doses <strong>of</strong> ascorbic acid are not as harmless as suggested in<br />
this paper—when ingested in large amounts ‘may cause renal<br />
failure’. 2 Vitamin C deficiency may cause scurvy but the effects<br />
<strong>of</strong> an overdose <strong>of</strong> vitamin C are not necessarily innocuous.<br />
‘<strong>The</strong> role <strong>of</strong> vitamin C in disease intervention at doses<br />
higher than previously considered relevant should be thor-<br />
LETTERS TO THE EDITOR<br />
oughly investigated in a clinical setting.’ I totally agree with<br />
this statement as many <strong>of</strong> the referenced articles lacked the<br />
evidence to support the claims made, specifically using vitamin<br />
C to treat infectious diseases.<br />
Erin Hanlon-Wake, Registered midwife<br />
References<br />
1. Cathcart RF. Vitamin C, titrating to bowel tolerance, anascorbemia, and<br />
acute induced scurvy. Med Hypothesis 1981;7:1359–1376.<br />
2. Material Safety Data Sheet: Ascorbic Acid MSDS. ScienceLab. http://<br />
www.sciencelab.com/xMSDS-Ascorbic_acid-9922972. Published 9<br />
October 2005. Accessed 5 May 2008.<br />
was appalled to see the opinion piece in NZFP masquerad-<br />
I ing as an original scientific paper ‘Vitamin C: Evidence,<br />
application and commentary’ but will resist the temptation to<br />
perform an autopsy and critique on the authors’ interpretation<br />
<strong>of</strong> the literature.<br />
It appears that all <strong>of</strong> the authors have a vested interest in<br />
plying desperate patients with intravenous vitamin C, presumably<br />
at a reasonable pr<strong>of</strong>it, and to be fair this is declared.<br />
However, it is deceitful to misrepresent the literature and<br />
evidence. A quick glance at the list <strong>of</strong> references is enough to<br />
raise immediate scepticism as they generally consist <strong>of</strong> hypotheses,<br />
laboratory studies or case studies; some are 30 and even<br />
60 years old. This is about as low level as evidence gets and is<br />
certainly not sufficient to inform practice.<br />
One part that is so dubious that it is actually funny is the<br />
table that shows Vitamin C synthesis in the rat, dog and goat<br />
and then extrapolates this to humans. Humans are not rats,<br />
dogs or goats and I think we have had enough lessons from<br />
animal models to know this. If humans behaved like their distant<br />
rodent cousins according to laboratory studies we would<br />
have cures for a lot more diseases than we do now. This is not<br />
something that belongs under the name science as it does not<br />
employ any.<br />
Helen Petousis-Harris, Senior Lecturer, <strong>General</strong> Practice and<br />
Primary Health Care<br />
REpLy: JPHC will publish the nature and quality <strong>of</strong> evidence<br />
around efficacy and safety <strong>of</strong> herbal medicines in our column<br />
Charms and Harms. We also welcome systematic reviews and<br />
meta-analyses on complementary and alternative medicines<br />
(CAM) and nutritional supplements that critique the available<br />
evidence on efficacy and harm, produce evidence tables and<br />
<strong>of</strong>fer recommendations based on the graded evidence in the<br />
accepted scientific fashion (see http://www.rnzcgp.org.nz/<br />
journal-<strong>of</strong>-primary-health-care/systematic reviews). – Editor<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 81
BOOK REVIEWS<br />
<strong>The</strong> Baby Business:<br />
What’s happened to maternity care in <strong>New</strong> <strong>Zealand</strong><br />
By Lynda Exton<br />
Review by William Fergusson, GP<br />
<strong>The</strong> Baby Business is a modern history<br />
book that had to be written.<br />
Its author, Christchurch <strong>General</strong><br />
Practitioner Lynda Exton, needed a<br />
more than usual amount <strong>of</strong> courage and<br />
determination to surmount this task.<br />
All participants in the tortuous saga <strong>of</strong><br />
<strong>New</strong> <strong>Zealand</strong>’s maternity services over<br />
the last 18 years should be interested,<br />
if not required, to read this detailed<br />
and extensively referenced account <strong>of</strong><br />
events. <strong>The</strong> book manages piece by<br />
piece to explain how it is that a medical<br />
sub-speciality, that <strong>of</strong> the general<br />
practitioner obstetrician, that was both<br />
revered by its practitioners and in ceaseless<br />
demand from its patients, could be<br />
simply erased.<br />
What ideologically driven unholy alliance<br />
<strong>of</strong> ministry bureaucrats, politicians and<br />
midwifery interests expended so much<br />
effort over so long to ensure the absolute<br />
demise <strong>of</strong> GP Obstetrics? <strong>The</strong> cast <strong>of</strong> characters<br />
is fairly well detailed in the book. It<br />
stops short however <strong>of</strong> attempting to properly<br />
explain the rationale <strong>of</strong> this shadowy<br />
force. What were they really thinking?<br />
Perhaps more time needs to elapse for clarity<br />
around this to emerge. <strong>General</strong>ly, the<br />
perpetrators have continued to imagine<br />
themselves sunned by some reflected<br />
glory in achieving choice for women, or<br />
the de-medicalisation <strong>of</strong> childbirth, or<br />
some such thing. <strong>The</strong> evidence the book<br />
presents suggests they are doing so somewhere<br />
in a parallel universe that does not<br />
relate to mothers and babies in NZ.<br />
<strong>The</strong> beginning chapters are dedicated<br />
to some <strong>of</strong> the landmarks in the history<br />
<strong>of</strong> our maternity service, and reference<br />
several brave and dedicated early NZ<br />
doctors. <strong>The</strong> author documents many <strong>of</strong><br />
the national controversies <strong>of</strong> the time,<br />
such as the use <strong>of</strong> ‘twilight sleep’, infant<br />
feedings and the culture change towards<br />
the hospitalisation <strong>of</strong> childbirth. <strong>The</strong>re<br />
are vividly conjured images <strong>of</strong> some <strong>of</strong><br />
the hair-raising and skilful exploits <strong>of</strong><br />
our early GPOs and midwives. This sets<br />
the stage for the inexplicable, calculated<br />
and ruthless path that was pursued, it<br />
seems, from the anti medical politics<br />
<strong>of</strong> the late 1980s, to eliminate choice<br />
<strong>of</strong> maternity care provider and create<br />
a midwifery-only service in NZ. <strong>The</strong><br />
author has painstakingly gathered the<br />
meagre existing scraps <strong>of</strong> data by which<br />
this momentous juggling <strong>of</strong> vulnerable<br />
lives was ‘monitored’ or evaluated, and<br />
there emerges the sketchy outline <strong>of</strong> a<br />
deteriorating maternity service relative<br />
to our past performance, and the services<br />
within comparable countries.<br />
Perhaps it is only now these policies have<br />
fully achieved their goals that the wider<br />
public will be able to read this book and<br />
gasp in horror at what has been taken<br />
from them. I am reminded <strong>of</strong> a quote<br />
from Doris Gordon’s autobiography Back<br />
Blocks Baby Doctor in which she recounts<br />
the formation <strong>of</strong> the NZ Obstetric and<br />
Gynaecological Society, in February<br />
1927. <strong>The</strong> O & G Society, as it came to<br />
be known, was formed in response to a<br />
drive from the Ministry <strong>of</strong> Health <strong>of</strong> the<br />
time to remove doctors from maternity<br />
care. <strong>New</strong>spaper headlines <strong>of</strong> the day<br />
exclaimed ‘women advised not to have<br />
doctors at confinements’. <strong>The</strong> society<br />
went on to be a bastion <strong>of</strong> CME provision<br />
throughout the country for GPOs,<br />
specialists and midwives for many<br />
decades, until it was severely holed by<br />
the infamous July 1996 Section 88 Maternity<br />
Notice, and sank without trace<br />
soon afterwards as GPs pulled out <strong>of</strong><br />
maternity care. Doris Gordon recounts:<br />
‘fed up with ever increasing “shalts”<br />
and “shalt nots” 180 doctors signed as<br />
foundation members. A few doctors<br />
who had no prospects <strong>of</strong> begetting or<br />
delivering babies gave us the backing <strong>of</strong><br />
their membership, saying, “you do well<br />
to found your society, for what threatens<br />
maternity care today will threaten all<br />
branches <strong>of</strong> medicine tomorrow”.’<br />
Review by Joan Carll, midwife<br />
<strong>The</strong> Baby Business records the<br />
changes to the NZ maternity service<br />
over the past 20 years and, in<br />
particular, the changes for general practitioners<br />
which led to their move away from<br />
active involvement in maternity care.<br />
<strong>The</strong> book outlines the journey <strong>of</strong> change<br />
beginning with a history <strong>of</strong> birthing<br />
from the 1880s. <strong>The</strong> history gives<br />
insight into the players who determined<br />
the early formation <strong>of</strong> the service and an<br />
explanation for the difficulties to change<br />
a service that became deeply entrenched.<br />
<strong>The</strong> ensuing changes to NZ’s maternity<br />
service (well passed its use-by-date in<br />
1988) lacked the necessary processes to<br />
prevent the political and collegial fallout<br />
exposed in this recount.<br />
Dr Exton details the changing NZ maternity<br />
service from 1988. However, go<br />
back 10 years to the end <strong>of</strong> the training<br />
<strong>of</strong> midwives at the St Helens Hospitals<br />
82 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
and the talk <strong>of</strong> change at the Midwives<br />
section. A time when women suffered<br />
the indignity <strong>of</strong> enemas, pubic shaves,<br />
episiotomies and limited choice for place<br />
to deliver. Women were even required to<br />
write a letter to have their husband present<br />
in the delivery room! A service that<br />
would encourage any newly graduated<br />
midwife to walk away and say—if that is<br />
midwifery and if that is what having a<br />
baby is about then why would you want<br />
a bar <strong>of</strong> either? Change was inevitable,<br />
supported by pr<strong>of</strong>essionals within the<br />
service, and women and families for<br />
whom the service is all about.<br />
As a midwife I have found the record<br />
<strong>of</strong> events interesting reading and a<br />
forum for reflection and insight into the<br />
turnaround <strong>of</strong> what was certainly a very<br />
<strong>The</strong> <strong>New</strong> <strong>Zealand</strong> pregnancy Book:<br />
A guide to pregnancy, birth and a baby’s first three months<br />
3RD EDITION<br />
By Sue Pullon and Cheryl Benn<br />
Review by Jon Wilcox, GP<br />
At first glance the latest edition<br />
<strong>of</strong> this venerable 20-year-old<br />
matter-<strong>of</strong>-fact guide for new<br />
parents looks very different from<br />
earlier versions. It immediately seems<br />
more user friendly and the layout is<br />
now more upmarket—there is an<br />
abundance <strong>of</strong> colour photography and<br />
excellent illustrations. Wellington GP<br />
Sue Pullon has changed the approach<br />
a little to perhaps steer away from the<br />
perceptually ‘medicalised’ editions we<br />
might have been more familiar with<br />
during the infamous years <strong>of</strong> what<br />
some might call the de-commissioning<br />
<strong>of</strong> general practice obstetrics. <strong>The</strong><br />
market is now unashamedly—and<br />
probably in order <strong>of</strong> preference—midwives<br />
and mothers.<br />
unfriendly maternity service to one with<br />
new achievements and challenges.<br />
<strong>The</strong> author captures the feeling <strong>of</strong> grief<br />
felt by GP obstetricians who are no<br />
longer part <strong>of</strong> the maternity service;<br />
however she misses the opportunity to<br />
provide positive steps forward. Hands up<br />
those who have been to their GP needing<br />
attention only to be left in the waiting<br />
room while they dash <strong>of</strong>f to deliver a<br />
baby? Perhaps there was also a need for<br />
general practice to change, and find new<br />
ways to rebuild the relationships with<br />
their patients in a different manner, to<br />
maintain that holistic approach to family<br />
medicine and create the important links<br />
with the new maternity service. I believe<br />
Dr Exton has inadvertently exposed a<br />
missed opportunity for primary care.<br />
Overall the new edition is excellent and<br />
I feel it is good value for new parents.<br />
<strong>The</strong>re is accurate information on a huge<br />
range <strong>of</strong> important <strong>issue</strong>s relating to<br />
preparing for pregnancy and childbirth,<br />
including parental leave, benefits, new<br />
maternal serum screening initiatives and<br />
so forth. <strong>General</strong>ly the information is <strong>of</strong><br />
high quality and, even though the book<br />
now could give the impression <strong>of</strong> being<br />
just another ‘touchy feely’ publication<br />
to peruse during the last four weeks <strong>of</strong><br />
pregnancy, it still has the excellent practical<br />
content relating to real life <strong>issue</strong>s<br />
such as common problems in pregnancy,<br />
labour and childbirth. Having been<br />
written from the standpoint <strong>of</strong> a clinician<br />
with a lot <strong>of</strong> experience in obstetrics<br />
and neonatal paediatric care, the<br />
advice is generally extremely sensible<br />
and very comprehensive.<br />
BOOK REVIEWS<br />
A good read for health pr<strong>of</strong>essionals who<br />
would like to recall the events <strong>of</strong> NZ’s<br />
changing maternity services. A rather<br />
negative read for consumers who are the<br />
beneficiaries <strong>of</strong> the change and remain unable<br />
to assess the current system through<br />
lack <strong>of</strong> data. A reminder to midwives the<br />
challenges have been and continue to be<br />
extreme. And to GPs, who are critically<br />
placed to ensure primary care is seamless,<br />
efficient and continuous, this book<br />
provides reason to look at new ways.<br />
Publisher: Craig Potton Publishing<br />
Publication Date: Oct 2008<br />
No. <strong>of</strong> pages: 260<br />
RRP: $29.99<br />
<strong>The</strong> Baby Business can be ordered<br />
through www.craigpotton.co.nz<br />
Furthermore, Pullon does not give the<br />
reader the misleading impression that<br />
almost all pregnancies and labour are normal<br />
(which can tend to give many mothers<br />
feelings <strong>of</strong> inadequacy or failure) and, as<br />
many <strong>of</strong> us who are still actively involved<br />
in intra-partum care know, each and every<br />
labour has its own idiosyncrasies.<br />
Pullon has joined with midwife Cheryl<br />
Benn to produce the new format and by<br />
and large it has been an excellent team<br />
effort. I have for 20 years recommended<br />
this book to all my own maternity<br />
patients, and for those with limited<br />
resources we have even had a cache <strong>of</strong><br />
secondhand editions to loan for the<br />
duration <strong>of</strong> pregnancy. I would certainly<br />
continue to endorse the latest edition as<br />
first choice for NZ GPs to recommend to<br />
their expecting client couples.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 83
BOOK REVIEWS<br />
Review by Ms Helen Ride, midwife<br />
This is the third edition <strong>of</strong> Pullon<br />
and Benn’s <strong>New</strong> <strong>Zealand</strong> Pregnancy<br />
Book. Since it was first<br />
published in 1991 there have been<br />
many changes within the delivery <strong>of</strong><br />
maternity care in <strong>New</strong> <strong>Zealand</strong> with<br />
the introduction <strong>of</strong> the Lead Maternity<br />
Care system. This third edition has been<br />
written for <strong>New</strong> <strong>Zealand</strong> parents and<br />
parents-to-be and includes information<br />
specific to the <strong>New</strong> <strong>Zealand</strong> maternity<br />
system, and all <strong>New</strong> <strong>Zealand</strong>ers. <strong>The</strong><br />
aim <strong>of</strong> the authors is to present a book<br />
which prepares the reader, her partner<br />
and family for the pregnancy, birth and<br />
the first three months <strong>of</strong> the baby’s life.<br />
This book is written chronologically<br />
from planning for a pregnancy through<br />
to the first three months with your<br />
baby, and provides vast amounts <strong>of</strong> information<br />
which appears to cover everything<br />
the reader would wish to know.<br />
It includes the physical and emotional<br />
changes occurring within the pregnant<br />
woman, common health problems,<br />
potential problems and the birth. <strong>The</strong><br />
format <strong>of</strong> the book is very appealing to<br />
the reader. <strong>The</strong> photographs are beautiful,<br />
the diagrams are excellent and the<br />
personal stories complete the experience.<br />
<strong>The</strong> reader can dip in and out <strong>of</strong> the<br />
book choosing specific topics or stages<br />
within the pregnancy to read, and crossreferencing<br />
is made throughout the book<br />
for further information.<br />
This is a very informative book. However,<br />
there is very little reference to homeopathy<br />
throughout the text but there<br />
is a reference within the appendix to the<br />
homeopathy website. I am aware that<br />
quite a few midwives use homeopathy<br />
and many women are interested in this<br />
during their pregnancies yet there was<br />
very little information within the book.<br />
As a former Bereavement Support<br />
Midwife I have a particular interest in<br />
the care and support <strong>of</strong> bereaved parents.<br />
One error that I found within this book<br />
is the information that a baby born dead<br />
Ideological Debates in Family Medicine<br />
By Stephen Buetow and Tim Kenealy<br />
Review by Pr<strong>of</strong>essor Marjan Kljakovic,<br />
School <strong>of</strong> <strong>General</strong> Practice, Rural, &<br />
Indigenous Health, Australian National<br />
University Medical School, Canberra,<br />
Australia<br />
This is a book written for the academic<br />
who likes to ponder ideological<br />
debates that occur within the<br />
field <strong>of</strong> family medicine. <strong>The</strong> book would<br />
also appeal to people who want a comprehensive<br />
way <strong>of</strong> looking at the world <strong>of</strong><br />
general practice and primary health care.<br />
<strong>The</strong> book presents a collection <strong>of</strong> ideas<br />
about family medicine around 13<br />
debates, each <strong>of</strong> which was written in<br />
two chapters posing the affirmative<br />
and negative position on a theme. Each<br />
theme began with the words ‘Family<br />
Medicine should…’ and then continued<br />
with the following words: ‘Refine its<br />
essential attributes; Rediscover a focus<br />
<strong>of</strong> family care; Emphasise population on<br />
health care; Focus on the sick; Encourage<br />
its clinicians to sub-specialise; Tolerate<br />
uncertainty to manage clinical risk; Use<br />
more Evidence Based Medicine than at<br />
present; Shift attention from rationality<br />
to emotions; Encourage the development<br />
<strong>of</strong> Luxury Practices; Promote the<br />
delivery <strong>of</strong> care through group practice;<br />
Emphasise the Provision <strong>of</strong> Health Care<br />
as a social good; Promote the optimal au-<br />
before 28 weeks gestation does not need<br />
a funeral. However the Births, Deaths<br />
and Marriages Registrations Act 1995<br />
redefined what constituted a still birth<br />
and changed it to a foetus born after 20<br />
weeks gestation or weighing over 400<br />
grams. Babies in this category are legally<br />
required to have a funeral.<br />
I found this book to be informative and<br />
great to read. Many first-time parents<br />
will enjoy reading it from cover to cover.<br />
<strong>The</strong> beautiful photographs add to the<br />
pleasurable experience.<br />
Publisher: Bridget Williams Books<br />
Publication date: Nov 2008<br />
No. <strong>of</strong> pages: 432<br />
Bridget Williams Books<br />
Phone: 04 473 8128<br />
Email: info@bwb.co.nz<br />
Web: www.bwb.co.nz<br />
<strong>The</strong> <strong>New</strong> <strong>Zealand</strong> Pregnancy Book is<br />
available to health pr<strong>of</strong>essionals at 20%<br />
discount <strong>of</strong>f the recommended retail price<br />
($44 rather than $54.99).<br />
tonomy <strong>of</strong> patients in decision making;<br />
And finally, Self-regulate to best protect<br />
patient and pr<strong>of</strong>essional autonomy’.<br />
<strong>The</strong> aim <strong>of</strong> giving ideological perspectives<br />
is to <strong>of</strong>fer change in the field <strong>of</strong><br />
family medicine through a normative<br />
thought process. An ideology is a system<br />
<strong>of</strong> abstract thought applied to public<br />
matters, and thus makes this concept<br />
central to family medicine. <strong>The</strong> book<br />
has 36 authors who came from different<br />
parts <strong>of</strong> the Western world and therefore<br />
gave very different perspectives<br />
on particular ideological themes. For<br />
example the debate on ‘Family Medicine<br />
should encourage its specialists to<br />
84 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
sub-specialise’ had Leese arguing for<br />
the affirmative having come from the<br />
UK where the concept <strong>of</strong> the generalist<br />
is most developed, and the GP acts<br />
as gatekeepers for specialist services.<br />
Starfield argued for the negative having<br />
come from the USA where the concept<br />
<strong>of</strong> the generalist is least developed and<br />
there is a huge negative impact <strong>of</strong> subspecialisation<br />
in primary care.<br />
Some <strong>of</strong> the debates reminded me about<br />
themes I had been taking for granted. For<br />
example, Svab and van Weels’ negative position<br />
on ‘Family Medicine should refine<br />
its essential attributes’ reminded me that<br />
family medicine is an emancipated field <strong>of</strong><br />
medicine and no longer needed to debate<br />
this position (been there, done that).<br />
Furthermore, family medicine should get<br />
on with improving its image and be rid <strong>of</strong><br />
‘the harmful benefits <strong>of</strong> extreme complexity,<br />
uniqueness, exclusivity, and threat’.<br />
Other debates taught me a lot. For<br />
example, Bohan and Donohoe argued for<br />
and against the theme: ‘Family Medicine<br />
should encourage the development <strong>of</strong><br />
Luxury Practices’. <strong>The</strong>ir debate revealed<br />
how much luxury Practices have flourished<br />
in the USA in the last few years<br />
and how malignant such a growth was<br />
for patient care and provider greed.<br />
A few <strong>of</strong> the debates annoyed me. For<br />
example Upshur and Tracey’s negative<br />
position that ‘Family Medicine should<br />
use more Evidence Based Medicine<br />
than at present’. <strong>The</strong>y argued that EBM<br />
cannot meet its own standards, is no<br />
Integrating mental health into primary care:<br />
A global perspective<br />
This report on integrating mental<br />
health into primary care, developed<br />
jointly by the World Health<br />
Organization (WHO) and the World Organization<br />
<strong>of</strong> Family Doctors (Wonca),<br />
presents the justification and advantages<br />
<strong>of</strong> providing mental health services in<br />
primary care. It provides advice on how<br />
to implement and scale-up primary care<br />
for mental health, and describes how a<br />
range <strong>of</strong> health systems have successfully<br />
undertaken this transformation.<br />
Key messages<br />
1. Mental disorders affect hundreds<br />
<strong>of</strong> millions <strong>of</strong> people and, if left<br />
untreated, create an enormous toll <strong>of</strong><br />
suffering, disability and economic loss.<br />
2. Despite the potential to successfully<br />
treat mental disorders, only a small<br />
minority <strong>of</strong> those in need receive<br />
even the most basic treatment.<br />
3. Integrating mental health services<br />
into primary care is the most viable<br />
4.<br />
5.<br />
6.<br />
7.<br />
way <strong>of</strong> closing the treatment gap and<br />
ensuring that people get the mental<br />
health care they need.<br />
Primary care for mental health is<br />
affordable, and investments can bring<br />
important benefits.<br />
Certain skills and competencies<br />
are required to effectively assess,<br />
diagnose, treat, support and refer<br />
people with mental disorders; it is<br />
essential that primary care workers are<br />
adequately prepared and supported in<br />
their mental health work.<br />
<strong>The</strong>re is no single best practice model<br />
that can be followed by all countries.<br />
Rather, successes have been achieved<br />
through sensible local application <strong>of</strong><br />
broad principles.<br />
Integration is most successful<br />
when mental health is incorporated<br />
into health policy and legislative<br />
frameworks and supported by senior<br />
leadership, adequate resources, and<br />
ongoing governance.<br />
BOOK REVIEWS<br />
superior to other modes <strong>of</strong> obtaining<br />
evidence, and lacks legitimacy. <strong>The</strong>ir<br />
solution was for family medicine ‘to be<br />
descriptive, careful in observation, and<br />
explicitly recognise and integrate the<br />
interpretive grammar <strong>of</strong> medicine’. A<br />
solution I find is easily accepted by an<br />
arcane social scientist <strong>of</strong> family medicine,<br />
rather than a pragmatic GP whose<br />
patient wants evidence from outside the<br />
consultation to answer a health question.<br />
<strong>The</strong> virtue <strong>of</strong> this book is that it does<br />
generate feelings such as annoyance,<br />
disagreement, and surprise. It stimulates<br />
the reader and for that reason alone I<br />
recommend buying this book.<br />
Publisher: Nova Science<br />
Date <strong>of</strong> Publication: Dec 2007<br />
No. <strong>of</strong> pages: 302<br />
8. To be fully effective and efficient,<br />
primary care for mental health must<br />
be coordinated with a network <strong>of</strong><br />
services at different levels <strong>of</strong> care<br />
and complemented by broader health<br />
system development.<br />
9. Numerous low- and middle-income<br />
countries have successfully made the<br />
transition to integrated primary care<br />
for mental health.<br />
10. Mental health is central to the values<br />
and principles <strong>of</strong> the Alma Ata<br />
Declaration; holistic care will never<br />
be achieved until mental health is<br />
integrated into primary care.<br />
<strong>The</strong> full report can be accessed at http://<br />
www.globalfamilydoctor.com/index.<br />
asp?PageID=9063<br />
Publisher: World Health Organization and<br />
World Organization <strong>of</strong> Family Doctors<br />
(Wonca)<br />
Date <strong>of</strong> publication: 2008<br />
No. <strong>of</strong> pages: 206<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 85
RESEARCH GEMS<br />
GemS Of NeW ZeAlAND<br />
primary Health Care Research<br />
Access to CME an <strong>issue</strong> for<br />
overseas-trained rural Gps<br />
Difficulty in accessing CME has been<br />
identified as a negative aspect <strong>of</strong> rural<br />
practice in a study investigating retention<br />
<strong>of</strong> overseas-trained doctors in<br />
rural NZ. <strong>The</strong> study included thematic<br />
analysis <strong>of</strong> nine in-depth interviews<br />
<strong>of</strong> overseas-trained doctors working<br />
in rural settings. Other factors noted<br />
by interviewees as detracting from the<br />
rural practice environment were reduced<br />
options for employment <strong>of</strong> their spouse<br />
and for secondary schooling, and limited<br />
cultural and entertainment activities.<br />
On the positive side, doctors valued<br />
the scope <strong>of</strong> the practice work and the<br />
sense <strong>of</strong> community loyalty. <strong>The</strong> rural<br />
lifestyle <strong>of</strong>fered also featured as a key<br />
attraction.<br />
Kearns RA, Myers JM, Adair V, Coster H, Coster<br />
G. What makes ‘place’ attractive to overseas-<br />
trained doctors in rural <strong>New</strong> <strong>Zealand</strong>? Health &<br />
Social Care in the Community 2006;14:532-40.<br />
Corresponding author: R. Kearns. Email:<br />
r.kearns@auckland.ac.nz<br />
Antibiotics not first-line treatment<br />
for acute purulent rhinitis<br />
A meta-analysis <strong>of</strong> data from seven<br />
RCTs <strong>of</strong> antibiotics versus placebo<br />
for acute purulent rhinitis concludes<br />
that antibiotics are probably effective.<br />
However, as no serious adverse events<br />
occurred in the placebo group, antibiotics<br />
are not indicated as first line treat-<br />
ment. This conclusion is in keeping<br />
with most guidelines which recommend<br />
against using antibiotics on the basis<br />
<strong>of</strong> one earlier study. Harms attributed<br />
to antibiotics in the RCTs were mainly<br />
vomiting, diarrhoea, and abdominal pain<br />
but also included rashes and hyperactivity<br />
(in children). A treatment approach<br />
<strong>of</strong> ‘watchful waiting’ is suggested, with<br />
antibiotics used only when symptoms<br />
have persisted for long enough to concern<br />
parents or patients.<br />
Arroll B, Kenealy T. Are antibiotics effective for<br />
acute purulent rhinitis? Systematic review and<br />
meta-analysis <strong>of</strong> placebo controlled randomised<br />
trials. BMJ 2006;333:279. Corresponding au-<br />
thor: B. Arroll. Email: b.arroll@auckland.ac.nz<br />
problem gamblers <strong>of</strong>ten<br />
have other problems<br />
Primary care screening for problem<br />
gambling highlights common lifestyle<br />
and mental health co-morbidities. <strong>The</strong><br />
cross-sectional study conducted in 51<br />
urban and rural primary care practices<br />
in NZ found that people identified with<br />
concerns about their gambling behaviour<br />
were significantly more likely to have<br />
concerns about alcohol use, recreational<br />
drug use, and smoking. Problems with<br />
depression, anxiety and anger control<br />
were also more likely to be reported by<br />
these individuals. Problem gambling<br />
was readily identified using a brief<br />
multi-item screening tool containing a<br />
validated gambling question: ‘Sometimes<br />
I’ve felt depressed or anxious after a session<br />
<strong>of</strong> gambling—yes or no’. <strong>The</strong> study<br />
signals the potential <strong>of</strong> screening for<br />
problem gambling in the primary care<br />
setting.<br />
Goodyear-Smith F, Arroll B, Kerse N, et al.<br />
Primary care patients reporting concerns about<br />
their gambling frequently have other co-occur-<br />
ring lifestyle and mental health <strong>issue</strong>s. BMC<br />
Fam Pract 2006;7:25. Corresponding author:<br />
Felicity Goodyear-Smith Email:f.goodyear-<br />
smith@auckland.ac.nz<br />
No geographic disparity for NZ<br />
women with breast cancer<br />
Studies in Australia, Canada and the<br />
USA have shown that people living in<br />
regional and remote areas have higher<br />
mortality rates from cancer than people<br />
living in urban and suburban areas. A<br />
recent study <strong>of</strong> NZ with breast cancer<br />
showed no such geographic disparity,<br />
however. <strong>The</strong> study drew on the NZ<br />
Cancer Registry Data from a four-year<br />
period, involving 11 340 women. Just<br />
under a third lived within 10km <strong>of</strong> a cancer<br />
centre, another third lived 11–50km<br />
away, and the remaining third lived more<br />
than 50km away. Reasons put forward<br />
to explain the equity seen in stage at<br />
diagnosis include BreastScreen Aotearoa<br />
which has mobile/outreach services, high<br />
community awareness, and the natural<br />
history <strong>of</strong> the disease. Regional coordination<br />
<strong>of</strong> cancer services was seen as<br />
contributing to equity <strong>of</strong> survival, with<br />
GEMS are short précis <strong>of</strong> original papers published by NZ researchers. FOR A COpy <strong>of</strong> a full paper please<br />
email the corresponding author. Researchers, TO HAVE yOUR WORK INCLUDED please send your<br />
references and pdfs <strong>of</strong> your papers to: editor@rnzcgp.org.nz<br />
86 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE
service configuration attempting to balance<br />
centralisation and local access.<br />
Bennett H, Marshall R, Campbell I, Lawrenson<br />
R. <strong>The</strong> effect <strong>of</strong> urban versus rural residence<br />
on stage at diagnosis and survival for women<br />
with breast cancer in Aotearoa-<strong>New</strong> <strong>Zealand</strong>.<br />
NZ Med J 2007;120(1266). Corresponding<br />
author: H. Bennett. Email: hayleyandcam@<br />
clear.net.nz<br />
Dairy calves are a potential<br />
source for Giardia infection<br />
A recent Otago study characterising<br />
Giardia genotypes present in calves and<br />
humans has found a substantial overlap<br />
<strong>of</strong> identical genotypes for assemblages<br />
A and B, the only assemblages capable<br />
<strong>of</strong> causing human infection, in the two<br />
hosts. <strong>The</strong> finding implies zoonotic<br />
transmission may have occurred and<br />
demonstrates the possibility <strong>of</strong> the dairy<br />
herd as a reservoir for human infection.<br />
It is <strong>of</strong> particular note given recent intensification<br />
<strong>of</strong> dairying in NZ and the<br />
potential for transmission via waterways<br />
contaminated by run<strong>of</strong>f.<br />
Winkworth CL, Learmonth JL, Matthaei CD,<br />
Townsend CR. Molecular characterization <strong>of</strong><br />
Giardia isolates from calves and humans in a<br />
region in which dairy farming has recently inten-<br />
sified. Appl Environ Microbiol 2008;74:5100-<br />
5105. Corresponding author: C. Winkworth.<br />
Email: Cynthia.winkworth@zoology.otago.ac.nz<br />
Fast acting agents essential<br />
to breakthrough pain<br />
management in cancer<br />
Most breakthrough analgesia for cancer<br />
pain fails to be effective in the time<br />
required. No useful analgesia is therefore<br />
provided but drug adverse effects<br />
increase. This paper addresses this problem,<br />
outlining a systematic, evidencebased<br />
approach to breakthrough pain<br />
management, whether due to end-<strong>of</strong>dose<br />
failure, incident or idiopathic pain.<br />
<strong>The</strong> paper details non-pharmacological<br />
as well as pharmacological approaches,<br />
while highlighting the value <strong>of</strong> fast<br />
acting fentanyl formulations (such as the<br />
oral transmucosal fentanyl citrate lozenge<br />
and the fentanyl buccal tablet), and<br />
analogues (such as intranasal alfentanil),<br />
specifically developed for breakthrough<br />
pain treatment.<br />
William L, MacLeod R. Management <strong>of</strong> break-<br />
through pain in patients with cancer. Drugs<br />
2008;68:913–924. Corresponding author:<br />
L. William. Email: leeroy.william@waitemat-<br />
adhb.govt.nz<br />
Thiazide diuretics ‘justifiable’<br />
for hypertension in patients<br />
with pre-diabetes<br />
This article, part <strong>of</strong> a series exploring<br />
uncertainties in clinical practice, considers<br />
whether diuretics are appropriate<br />
antihypertensive agents for patients<br />
with pre-diabetes. <strong>The</strong> ALLHAT 2002<br />
trial provides the basis for this clinical<br />
uncertainty, having reported an increase<br />
in cardiac risk factors, including<br />
development <strong>of</strong> diabetes, as a result <strong>of</strong><br />
treatment with the thiazide-like diuretic<br />
chlortalidone. A Japanese clinical trial<br />
(diuretics in the management <strong>of</strong> essential<br />
hypertension study; http://clinicaltrials.gov/show/NCT00131846)<br />
currently<br />
underway should provide the definitive<br />
answer when it concludes in a few<br />
years. In the interim, existing evidence<br />
suggests that use <strong>of</strong> thiazide diuretics<br />
as first-line agents for hypertension in<br />
pre-diabetic patients is ‘justifiable’, especially<br />
in resource-poor settings.<br />
Arroll B, Kenealy T, CR Elley. Should we pre-<br />
scribe diuretics for patients with prediabetes<br />
and hypertension? BMJ 2008;337:a679. Cor-<br />
responding author: B. Arroll. Email: b.arroll@<br />
auckland.ac.nz<br />
Mobile phone cameras have potential<br />
for triage in rural practice<br />
A study designed to assess population<br />
access and clinical usefulness <strong>of</strong> mobile<br />
phone cameras has shown the potential<br />
<strong>of</strong> such technology for triaging afterhours<br />
care. <strong>The</strong> study was conducted<br />
among 480 patients in two rural primary<br />
care practices in NZ. Mobile phone cameras<br />
were found to be widely available,<br />
with most patients open to the idea <strong>of</strong><br />
their use for medical triaging. Clinical<br />
utility was tested by quizzing 30 health<br />
pr<strong>of</strong>essionals using photographs <strong>of</strong> 10<br />
primary care cases. <strong>The</strong> photographs<br />
used were taken on a standard mobile<br />
phone (Motorola v 360 with an integrated<br />
camera and 4 x zoom). Picture resolution<br />
was 176 x 220 pixels. Images were<br />
found to increase diagnostic confidence<br />
for all but one case.<br />
Jayaraman C, Kennedy P, Dutu G, Lawrenson<br />
R. Use <strong>of</strong> mobile phone cameras for after-hours<br />
triage in primary care. J Telemed Telecare<br />
2008;14:271–274. Corresponding author:<br />
R. Lawrenson. Email: LawrensR@waikatodhb.<br />
VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE 87<br />
govt.nz<br />
RESEARCH GEMS<br />
Tenosynovitis due to text messaging<br />
This brief case report draws reader attention<br />
to a new overuse condition, ‘texting<br />
tenosynovitis’. <strong>The</strong> case in question presented<br />
with tenderness over the tendons<br />
<strong>of</strong> extensor pollicis brevis and abductor<br />
pollicis longus at the wrist and distally,<br />
consistent with de Quervain’s tenosynovitis.<br />
This had developed over a 3-month<br />
period during which the right-handed<br />
student had sent about 2500 texts every<br />
month, each <strong>of</strong> about 150 characters.<br />
Two international case reports <strong>of</strong> this<br />
condition are cited by the authors and<br />
the question is raised as to whether more<br />
cases are likely, given growing ownership<br />
and use <strong>of</strong> mobile phones.<br />
Storr EF, de Vere Beavis FO, Stringer MD.<br />
Texting tenosynovitis. NZ Med J 2007;1267.<br />
Corresponding author: M. Stringer Email:<br />
mark.stringer@anatomy.otago.ac.nz
JOURNAL OF pRIMARy HEALTH CARE<br />
<strong>The</strong> Journal <strong>of</strong> Primary Health Care (JPHC) is a peer-reviewed journal<br />
which has replaced the <strong>New</strong> <strong>Zealand</strong> Family Physician. It is a multidisciplinary<br />
publication aimed at moving research into primary health<br />
care practice and practice into research. This includes the fields <strong>of</strong><br />
family practice, primary health care nursing and community pharmacy<br />
as well as areas such as health care delivery, health promotion, epidemiology,<br />
public health and medical sociology <strong>of</strong> interest to a primary<br />
health care provider audience.<br />
<strong>The</strong> journal publishes peer-reviewed quantitative and qualitative original<br />
research, systematic reviews, papers on improving performance<br />
and short reports that are relevant to its primary health care practitioners.<br />
For the aim, scope, instructions to authors and templates for<br />
publications see www.rnzcgp.org.nz/journal-<strong>of</strong>-primary-health-care/.<br />
JPHC acts as a knowledge refinery to provide busy practitioners with<br />
up-to-date knowledge about the latest evidence and best practice.<br />
Continuing pr<strong>of</strong>essional development includes pithy summaries <strong>of</strong> the<br />
latest evidence such as Cochrane Corner, POEMS (Patient Oriented<br />
Evidence that Matters), brief synopses <strong>of</strong> guidelines and bulletins, a<br />
String <strong>of</strong> PEARLS (Practical Evidence About Real Life Situations) and<br />
Charms and Harms (evidence <strong>of</strong> effectiveness and safety <strong>of</strong> complementary<br />
and alternative medicines). JPHC includes Poumanu (treasures<br />
<strong>of</strong> Maori wisdom) and Gems <strong>of</strong> NZ Primary Health Care Research<br />
published at home and internationally.<br />
Evidence can help inform best practice. However sometimes there is no<br />
evidence available or applicable for a specific patient with his or her own<br />
set <strong>of</strong> conditions, capabilities, beliefs, expectations and social circumstances.<br />
Evidence needs to be placed in context. <strong>General</strong> practice is an<br />
art as well as a science. Quality <strong>of</strong> care lies also with the nature <strong>of</strong> the<br />
clinical relationship, with communication and with truly informed decision-making.<br />
JPHC publishes viewpoints, commentaries and reflections<br />
that explore areas <strong>of</strong> uncertainty on aspects <strong>of</strong> care for which there is<br />
no one right answer. Debate is stimulated by the Back to Back section<br />
where two pr<strong>of</strong>essionals present their opposing views on a topic. <strong>The</strong>re<br />
is a regular Ethics column. Letters to the Editor are welcomed.<br />
While published in <strong>New</strong> <strong>Zealand</strong> by the <strong>Royal</strong> <strong>New</strong> <strong>Zealand</strong> <strong>College</strong> <strong>of</strong><br />
<strong>General</strong> Practitioners, much <strong>of</strong> this research has generic implications.<br />
Our Editorial Board comprises renowned and active primary care clinicians,<br />
clinical and scientific academics and health policy experts with<br />
both <strong>New</strong> <strong>Zealand</strong> and international representation.<br />
Editor<br />
Dr Felicity Goodyear-Smith, Associate Pr<strong>of</strong>essor, Department <strong>of</strong><br />
<strong>General</strong> Practice & Primary Health Care, University <strong>of</strong> Auckland,<br />
Auckland, <strong>New</strong> <strong>Zealand</strong>; editor@rnzcgp.org.nz<br />
Editorial Board<br />
Pr<strong>of</strong> Bruce Arroll: Pr<strong>of</strong>essor and Head <strong>of</strong> the Department <strong>of</strong> <strong>General</strong><br />
Practice & Primary Health Care, University <strong>of</strong> Auckland, NZ<br />
Dr Jo Barnes: Associate Pr<strong>of</strong>essor <strong>of</strong> Pharmacy, School <strong>of</strong> Pharmacy,<br />
University <strong>of</strong> Auckland, NZ<br />
Pr<strong>of</strong> Peter Crampton: Dean and Head <strong>of</strong> Campus, Wellington School<br />
<strong>of</strong> Medicine & Health Sciences, University <strong>of</strong> Otago, NZ<br />
Pr<strong>of</strong> Tony Dowell: Pr<strong>of</strong>essor and Head <strong>of</strong> the Department <strong>of</strong> Primary<br />
Health Care & <strong>General</strong> Practice, Wellington School <strong>of</strong> Medicine,<br />
University <strong>of</strong> Otago, NZ<br />
Dr Pat Farry: Director <strong>of</strong> Te Waipounamu Rural Health Unit, University<br />
<strong>of</strong> Otago, NZ<br />
Dr Ron Janes: Associate Pr<strong>of</strong>essor <strong>of</strong> Rural Health, Department <strong>of</strong><br />
<strong>General</strong> Practice and Primary Health Care, University <strong>of</strong> Auckland, NZ<br />
Dr Derelie Mangin: Associate Pr<strong>of</strong>essor, Department <strong>of</strong> Public Health<br />
& <strong>General</strong> Practice, University <strong>of</strong> Otago, Christchurch, NZ<br />
Dr Barry Parsonson: Psychologist for NZ Ministry <strong>of</strong> Education and<br />
International Consultant, UNICEF (Georgia) Training Project for Institutional<br />
Staff working with disabled children<br />
Dr Shane Reti: Assistant Pr<strong>of</strong>essor, International Program Director<br />
Clinical Informatics and CEO <strong>of</strong> Clinical Informatics Industrial<br />
Research, Harvard Medical School, USA<br />
Pr<strong>of</strong> Kurt Stange: Pr<strong>of</strong>essor <strong>of</strong> Family Medicine, Case Western Reserve<br />
University, Cleveland, OH, USA and Editor, Annals <strong>of</strong> Family Medicine<br />
Dr Colin Tukuitonga: Associate Pr<strong>of</strong>essor and CEO <strong>of</strong> the Ministry <strong>of</strong><br />
Pacific Island Affairs, Wellington, NZ<br />
Editorial assistant<br />
Please send all submissions to the Editor: editor@rnzcgp.org.nz or to<br />
the Editorial Assistant Pam Berry: editorialassistant@rnzcgp.org.nz<br />
accompanied by a covering letter as outlined at http://www.rnzcgp.<br />
org.nz/journal-<strong>of</strong>-primary-health-care/#cover<br />
Subscription or advertising queries<br />
Cherylyn Borlase, Publications Coordinator<br />
RNZCGP, PO Box 10440, Wellington 6143<br />
jphcnz@rnzcgp.org.nz<br />
<strong>The</strong> Journal <strong>of</strong> Primary Health Care is the <strong>of</strong>ficial journal <strong>of</strong> the RNZCGP. However, views expressed are not necessarily those <strong>of</strong> the <strong>College</strong>, the Edi-<br />
tor, or the Editorial Board. ©<strong>The</strong> <strong>Royal</strong> <strong>New</strong> <strong>Zealand</strong> <strong>College</strong> <strong>of</strong> <strong>General</strong> Practitioners 2009. All Rights Reserved.<br />
88 VOLUME 1 • NUMBER 1 • MARCH 2009 J OURNAL OF PRIMARY HEALTH CARE