Isolation of Legionella pneumophila from clinical & environmental ...
Isolation of Legionella pneumophila from clinical & environmental ...
Isolation of Legionella pneumophila from clinical & environmental ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
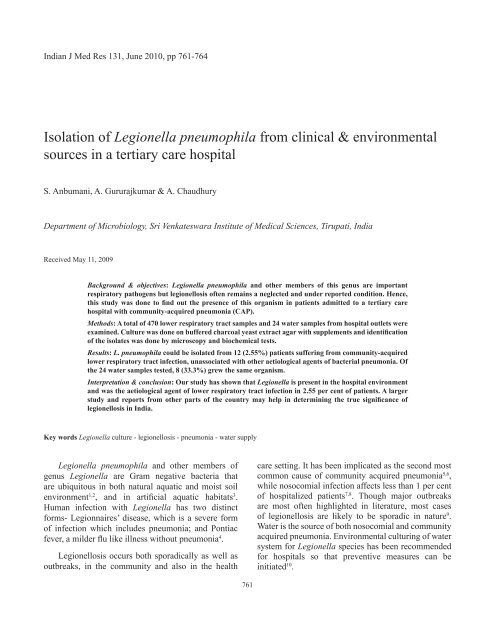
Indian J Med Res 131, June 2010, pp 761-764<br />
<strong>Isolation</strong> <strong>of</strong> <strong>Legionella</strong> <strong>pneumophila</strong> <strong>from</strong> <strong>clinical</strong> & <strong>environmental</strong><br />
sources in a tertiary care hospital<br />
S. Anbumani, A. Gururajkumar & A. Chaudhury<br />
Department <strong>of</strong> Microbiology, Sri Venkateswara Institute <strong>of</strong> Medical Sciences, Tirupati, India<br />
Received May 11, 2009<br />
Background & objectives: <strong>Legionella</strong> <strong>pneumophila</strong> and other members <strong>of</strong> this genus are important<br />
respiratory pathogens but legionellosis <strong>of</strong>ten remains a neglected and under reported condition. Hence,<br />
this study was done to find out the presence <strong>of</strong> this organism in patients admitted to a tertiary care<br />
hospital with community-acquired pneumonia (CAP).<br />
Methods: A total <strong>of</strong> 470 lower respiratory tract samples and 24 water samples <strong>from</strong> hospital outlets were<br />
examined. Culture was done on buffered charcoal yeast extract agar with supplements and identification<br />
<strong>of</strong> the isolates was done by microscopy and biochemical tests.<br />
Results: L. <strong>pneumophila</strong> could be isolated <strong>from</strong> 12 (2.55%) patients suffering <strong>from</strong> community-acquired<br />
lower respiratory tract infection, unassociated with other aetiological agents <strong>of</strong> bacterial pneumonia. Of<br />
the 24 water samples tested, 8 (33.3%) grew the same organism.<br />
Interpretation & conclusion: Our study has shown that <strong>Legionella</strong> is present in the hospital environment<br />
and was the aetiological agent <strong>of</strong> lower respiratory tract infection in 2.55 per cent <strong>of</strong> patients. A larger<br />
study and reports <strong>from</strong> other parts <strong>of</strong> the country may help in determining the true significance <strong>of</strong><br />
legionellosis in India.<br />
Key words <strong>Legionella</strong> culture - legionellosis - pneumonia - water supply<br />
<strong>Legionella</strong> <strong>pneumophila</strong> and other members <strong>of</strong><br />
genus <strong>Legionella</strong> are Gram negative bacteria that<br />
are ubiquitous in both natural aquatic and moist soil<br />
environment 1,2 , and in artificial aquatic habitats 3 .<br />
Human infection with <strong>Legionella</strong> has two distinct<br />
forms- Legionnaires’ disease, which is a severe form<br />
<strong>of</strong> infection which includes pneumonia; and Pontiac<br />
fever, a milder flu like illness without pneumonia 4 .<br />
Legionellosis occurs both sporadically as well as<br />
outbreaks, in the community and also in the health<br />
761<br />
care setting. It has been implicated as the second most<br />
common cause <strong>of</strong> community acquired pneumonia 5,6 ,<br />
while nosocomial infection affects less than 1 per cent<br />
<strong>of</strong> hospitalized patients 7,8 . Though major outbreaks<br />
are most <strong>of</strong>ten highlighted in literature, most cases<br />
<strong>of</strong> legionellosis are likely to be sporadic in nature 9 .<br />
Water is the source <strong>of</strong> both nosocomial and community<br />
acquired pneumonia. Environmental culturing <strong>of</strong> water<br />
system for <strong>Legionella</strong> species has been recommended<br />
for hospitals so that preventive measures can be<br />
initiated 10 .
762 INDIAN J MED RES, JUNE 2010<br />
Legionnaires’ disease remains a grossly under<br />
reported condition as it is difficult to distinguish the<br />
condition <strong>from</strong> other forms <strong>of</strong> pneumonia, unless<br />
the organism is specifically looked for. In spite <strong>of</strong><br />
the under-reporting, many studies are available <strong>from</strong><br />
Europe and North America, but studies regarding<br />
the isolation <strong>of</strong> <strong>Legionella</strong> either <strong>from</strong> <strong>clinical</strong> or<br />
<strong>environmental</strong> samples are rare <strong>from</strong> India 11,12 . We<br />
studied the presence <strong>of</strong> <strong>Legionella</strong> infection on the<br />
basis <strong>of</strong> culture in patients admitted to the hospital with<br />
signs and symptoms <strong>of</strong> lower respiratory tract infection<br />
acquired in the community. Sampling <strong>of</strong> the hospital<br />
water was also carried out to detect any <strong>Legionella</strong><br />
contamination in the hospital water supply system so<br />
as to alert the hospital infection control committee<br />
about its consequences.<br />
Material & Methods<br />
Patient samples: This study was carried out at Sri<br />
Venkateswara Institute <strong>of</strong> Medical Sciences, Tirupati,<br />
a post graduate teaching hospital in south India.<br />
Clinical samples <strong>from</strong> respiratory tract received in<br />
the Department <strong>of</strong> Microbiology <strong>from</strong> July 2007 to<br />
December 2008 were included in this study. The samples<br />
were obtained <strong>from</strong> patients who were hospitalized with<br />
signs and symptoms <strong>of</strong> lower respiratory tract infection<br />
(LRTI). Apart <strong>from</strong> sputum, the specimens included<br />
bronchoalveolar lavage (BAL), endotracheal aspirate<br />
and pleural fluid. After careful selection, 470 samples<br />
which did not yield any bacterial respiratory pathogen<br />
on routine culture and which were smear negative for<br />
acid fast bacilli were processed for <strong>Legionella</strong>.<br />
The samples were decontaminated by acid treatment<br />
(0.2 KCl-HCl) followed by plating on buffered charcoal<br />
yeast extract agar (BCYE) (Oxoid, UK) and BCYE<br />
supplemented with polymyxin(80 u/ml), anisomycin<br />
(40 µg/ml) and cefamandole (4 µg/ml) to make BCYE<br />
selective for respiratory samples 13 . Plates were incubated<br />
at 37 0 C and observed daily for 7 days.<br />
Water samples: A total <strong>of</strong> 24 water samples were<br />
collected <strong>from</strong> the taps <strong>of</strong> various wards and ICUs. Six<br />
samples were obtained at 2 months’ interval <strong>from</strong> July<br />
2007 to April 2008. The areas included the Medicine<br />
ward, General ward-Male, General ward-Female,<br />
Medicine ICU, Respiratory ICU, and the Emergency<br />
Room. Samples were obtained by introducing a sterile<br />
cotton swab into the opening <strong>of</strong> the taps and rotating it<br />
along the inner sides <strong>of</strong> the nozzles. The swab was then<br />
lightly streaked directly onto BCYE and then immersed<br />
in 2.5 ml acid buffer, shaken vigorously and neutralized<br />
with KOH. 0.1ml <strong>of</strong> the samples was spread with another<br />
swab onto duplicate plates <strong>of</strong> the same medium 14 .<br />
Identification: Iridescent, frosted glass colonies, 3-4<br />
mm size, typical <strong>of</strong> <strong>Legionella</strong> spp. appearing in 3-4<br />
days time were used for identification. Gram stain<br />
was done to show the thin, faintly stained filamentous<br />
Gram-negative morphology. Catalase positive and<br />
oxidase negative colonies showing the typical<br />
morphology were subcultured on plain BCYE and on<br />
blood agar (BA) to determine if L-cysteine is essential<br />
for growth 13 . Colonies growing only on BCYE and not<br />
on BA were presumptively identified as <strong>Legionella</strong><br />
spp. The reference strain L. <strong>pneumophila</strong> Serogroup<br />
1 Paris strain (CIP 107629T) obtained <strong>from</strong> French<br />
National <strong>Legionella</strong> Reference Centre, Lyon, France,<br />
was cultured in parallel with the <strong>clinical</strong> isolates and<br />
the morphology and biochemical characteristics <strong>of</strong> the<br />
<strong>clinical</strong> isolates were compared with this reference<br />
strain before definitive identification. Hippurate<br />
hydrolysis test was done by standard method 15 to<br />
identify L. <strong>pneumophila</strong> species. Briefly, 0.4 ml <strong>of</strong><br />
1 per cent sodium hippurate (Hi-Media, Mumbai) was<br />
inoculated with a loopful <strong>of</strong> organism and incubated<br />
overnight at 37 0 C. Next day, 0.2 ml <strong>of</strong> 3.5 per cent<br />
ninhydrin (Hi Media, Mumbai) solution in 1:1<br />
acetone:butanol was added to the organism in hippurate<br />
solution, mixed well, and incubated at 37 0 C for 10<br />
min. Blue purple colour developing within 20 min<br />
was considered positive. L. <strong>pneumophila</strong> CIP 107629T<br />
strain was used as a positive control and Enterobacter<br />
cloacae as the negative control.<br />
Results<br />
A total <strong>of</strong> 470 respiratory specimens <strong>from</strong> <strong>clinical</strong>ly<br />
suspected cases <strong>of</strong> LRTI did not yield any respiratory<br />
pathogenic bacterial isolate and were included in this<br />
study. Among the patient population studied, 12 out<br />
<strong>of</strong> the 470 (2.55%) were found to be culture positive<br />
for L. <strong>pneumophila</strong> as identified by positive hippurate<br />
hydrolysis test. The pr<strong>of</strong>ile <strong>of</strong> these 12 patients,<br />
along with the risk factors and <strong>clinical</strong> presentation<br />
is shown in the Table. Majority were males, and were<br />
>50 yr <strong>of</strong> age. Among the risk factors alcohol and /<br />
or smoking habit was found in five patients and one<br />
third <strong>of</strong> the patients had diabetes mellitus. Three<br />
patients did not have any underlying risk factor. Fever<br />
(100%), dyspnoea (91.7%) and cough (66.7%) were<br />
the most common presenting features. Three quarters<br />
<strong>of</strong> the patients had some radiological abnormality.<br />
Maximum isolation was <strong>from</strong> sputum samples<br />
(11/12) and one was <strong>from</strong> endotracheal aspirate.
Table. Characteristics <strong>of</strong> patients with legionellosis (n=12)<br />
Characteristics No. (%)<br />
Age (yr)<br />
Range<br />
Age groups (yr)<br />
20-30<br />
31-40<br />
41-50<br />
>50<br />
Males<br />
Females<br />
RISK FACTORS<br />
Smoking status<br />
Current<br />
Ex Smoker<br />
Never<br />
Alcohol consumption<br />
Alcoholic<br />
Non alcoholic<br />
Co-morbid illnesses<br />
None<br />
Diabetes mellitus<br />
Ischaemic heart disease<br />
Asthma<br />
End stage renal disease<br />
Clinical presentation<br />
Fever<br />
Cough<br />
Absent<br />
Productive<br />
Dry<br />
Dyspnoea<br />
Haemoptysis<br />
Chest pain<br />
Vomiting<br />
Diarrhoea<br />
X- ray finding (Consolidation)<br />
ANBUMANI et al: LEGIONELLA ISOLATION FROM PATIENTS & ENVIRONMENT 763<br />
Among 24 samples <strong>of</strong> water tested, 8 (33%) were<br />
positive for L. <strong>pneumophila</strong> by culture. Among these<br />
samples, maximum isolations were in the months <strong>of</strong><br />
July and October (three each), and one each in January<br />
and April. The colony count was in the range <strong>of</strong> 180-<br />
356/ plate (swab).<br />
Discussion<br />
24-76<br />
3 (25)<br />
1 (8.3)<br />
0<br />
8 (66.7)<br />
10 (83.3)<br />
2 (16.7)<br />
1 (8.3)<br />
2 (16.7)<br />
9 (75)<br />
2 (16.7)<br />
10 (83.3)<br />
3 (25)<br />
4 (33.3)<br />
3 (25)<br />
3 (25)<br />
1 (8.3)<br />
12 (100)<br />
4 (33.3)<br />
6 (50)<br />
2 (16.7)<br />
11 (91.7)<br />
2 (16.7)<br />
1 (8.3)<br />
4 (33.3)<br />
1 (8.3)<br />
9 (75)<br />
Epidemics were the original presenting scenario<br />
for Legionnaires’ disease in the 1980s, but most cases<br />
are now known to be sporadic. Numerous observational<br />
studies <strong>of</strong> patients with community-acquired pneumonia<br />
(CAP) requiring hospitalization have documented that<br />
the incidence <strong>of</strong> Legionnaires’ disease ranges <strong>from</strong> 2 to<br />
9 per cent 6,16 . A recent Australian study has found that<br />
3.4 per cent <strong>of</strong> CAP was caused by <strong>Legionella</strong> 17 , while<br />
another study <strong>from</strong> UK reported the corresponding<br />
figure to be 3 per cent 18 . Our study showed Legionelle<br />
infection in 2.55 per cent patients. Male population<br />
and age >50 yr are established predisposing factors<br />
which have been found in the present study also. In<br />
these patients, fever was the most common finding<br />
(mean temperature at admission 39 0 C) followed<br />
by respiratory symptom like cough and dyspnoea.<br />
Studies 6,19 have found that a significant population <strong>of</strong><br />
patients have mild to moderate disease and do not have<br />
expected co-morbidities like diabetes mellitus which<br />
are also the finding in our study. Apart <strong>from</strong> systemic<br />
and respiratory symptoms, gastrointestinal symptoms<br />
like nausea, vomiting, and diarrhoea are known to be<br />
common 4 as seen in our patients also. In our study,<br />
majority (75%) had some radiological abnormality,<br />
which is a common feature <strong>of</strong> <strong>Legionella</strong> pneumonia<br />
and hence Legionnaires’ disease cannot be distinguished<br />
<strong>from</strong> other causes <strong>of</strong> CAP on radiological grounds<br />
alone 4 . For these reasons confining laboratory testing<br />
for this organism specifically to high risk patients will<br />
overlook a notable number <strong>of</strong> cases and our study also<br />
supports the practice <strong>of</strong> placing more emphasis on<br />
ascertaining the aetiology <strong>of</strong> pneumonia 19 .<br />
Centres for Disease Control and Prevention<br />
(CDC) does not support routine <strong>environmental</strong> culture<br />
for <strong>Legionella</strong> because <strong>of</strong> the supposedly ill defined<br />
relationship between the presence <strong>of</strong> the organism in<br />
water system and risk <strong>of</strong> acquiring the infection 20 . In our<br />
study, <strong>Legionella</strong> could be isolated <strong>from</strong> the hospital<br />
water supply over a nine months period. There is an<br />
increased yield <strong>of</strong> <strong>Legionella</strong> <strong>from</strong> the swab compared<br />
to the filtration concentration technique 21 . This can be<br />
explained by the fact that swab technique results in<br />
direct sampling <strong>of</strong> the organisms present in the bi<strong>of</strong>ilm<br />
consortium, which gives a greater yield than sampling<br />
<strong>of</strong> water. It has been recommended that swab samples<br />
be collected as part <strong>of</strong> any <strong>environmental</strong> <strong>Legionella</strong><br />
sampling protocol 21 . Our study has not included<br />
hospital acquired pneumonia patients and the potential<br />
sources <strong>of</strong> the infections were located outside this<br />
hospital. So no immediate conclusion can be drawn<br />
whether it is causing hospital acquired infections.<br />
However, it has been advocated that if the water<br />
supply is colonized by <strong>Legionella</strong>, then Legionnaires’<br />
disease should be included in the differential diagnosis<br />
<strong>of</strong> hospital acquired pneumonia 22 . In a study <strong>from</strong><br />
various hospitals, positive <strong>environmental</strong> sampling<br />
raised the suspicion, and once culture for <strong>Legionella</strong> <strong>of</strong><br />
hospitalized patients started, cases were discovered 23 .
764 INDIAN J MED RES, JUNE 2010<br />
Three important factors need to be mentioned.<br />
Firstly, we have focused on a particular pathogen, but<br />
in literature, concurrent infection particularly with<br />
Streptococcus pneumoniae is well documented 24,25 .<br />
Secondly, the fact that although culture is the most<br />
sensitive method, but still it cannot detect all cases<br />
since its sensitivity is 80 per cent 13 . And lastly, we have<br />
not used other tests like urinary antigen testing or direct<br />
fluorescent antibody stain which might have enhanced<br />
the overall sensitivity <strong>of</strong> the microbiological diagnostic<br />
workup. Our study highlights the importance <strong>of</strong><br />
<strong>environmental</strong> sampling <strong>of</strong> water and also the need for<br />
introduction <strong>of</strong> routine laboratory testing for this not<br />
so uncommon organism. Thus, a greater focus should<br />
be placed on diagnosis <strong>of</strong> aetiology for early therapy<br />
with appropriate antimicrobial substances. There is an<br />
urgent need to find out the incidence <strong>of</strong> infection in<br />
other parts <strong>of</strong> India to establish diagnostic setup for this<br />
organism in referral hospitals.<br />
Acknowledgment<br />
Authors thank the physicians in the department <strong>of</strong> medicine and<br />
the Emergency department for their co-operation, and acknowledge<br />
Dr Sophie Jarraud <strong>of</strong> the French National <strong>Legionella</strong> Reference<br />
Centre, Lyon, France, for providing the reference strain.<br />
References<br />
1. Costa J, Tiago I, da Costa MS, Verissimo A. Presence and<br />
persistence <strong>of</strong> <strong>Legionella</strong> spp. in groundwater. Appl Environ<br />
Microbiol 2005; 71 : 663-71.<br />
2. Wallis L, Robinson P. Soil as a source <strong>of</strong> <strong>Legionella</strong> <strong>pneumophila</strong><br />
serogroup 1(Lp1). Aust NZ J Public Health 2005; 29 : 518-20.<br />
3. Declerck P, Behets J, van Hoef V, Ollevier F. Detection <strong>of</strong><br />
<strong>Legionella</strong> spp. and some <strong>of</strong> their amoeba hosts in floating<br />
bi<strong>of</strong>ilms <strong>from</strong> anthropogenic and natural aquatic environments.<br />
Water Res 2007; 41 : 3159-67.<br />
4. Darby J, Buising K. Could it be <strong>Legionella</strong>? Aus Fam Physician<br />
2008; 37 : 812-5.<br />
5. Vergis EN, Akbas E, Yu VL. <strong>Legionella</strong> as a cause <strong>of</strong> severe<br />
pneumonia. Semin Respir Crit Care Med 2000; 21 : 295-304.<br />
6. von Baum H, Ewig S, Marre R, Suttorp N, Gonschior S,<br />
Welte T, et al. Competence Network for Community Acquired<br />
Pneumonia Study Group. Community-acquired <strong>Legionella</strong><br />
pneumonia: new insights <strong>from</strong> the German competence network<br />
for community acquired pneumonia. Clin Infect Dis 2008; 46 :<br />
1356-64.<br />
7. Haley CE, Cohen ML, Halter J, Meyer RD. Nosocomial<br />
Legionnaires’ disease: continuing common-source epidemic at<br />
Wadsworth Medical Center. Ann Intern Med 1979; 90 : 583-6.<br />
8. Broome CV, Fraser DW. Epidemiologic aspects <strong>of</strong> legionellosis.<br />
Epidemiol Rev 1979; 1 : 1-16.<br />
9. Ng V, Tang P, Jamieson F, Guyard C, Low DE, Fisman DN.<br />
Laboratory-based evaluation <strong>of</strong> legionellosis epidemiology in<br />
Ontario, Canada, 1978 to 2006. BMC Infect Dis 2009; 9 : 68.<br />
10. Sabria M, Modol JM, Garcia-Nunez M, Reynaga E, Pedro-Botet<br />
ML, Sopena N, et al. Environmental cultures and hospitalacquired<br />
Legionnaires’ disease: 5 year prospective study in 20<br />
hospitals in Catalonia, Spain. Infect Control Hosp Epidemiol<br />
2004; 25 : 1072-6.<br />
11. Chaudhry R, Dhawan B, Dey AB. The incidence <strong>of</strong> <strong>Legionella</strong><br />
<strong>pneumophila</strong>: A prospective study in a tertiary care hospital in<br />
India. Trop Doct 2000; 30 : 197-200.<br />
12. Agrawal L, Dhunjibhoy KR, Nair KG. <strong>Isolation</strong> <strong>of</strong> <strong>Legionella</strong><br />
<strong>pneumophila</strong> <strong>from</strong> patients <strong>of</strong> respiratory tract disease and<br />
<strong>environmental</strong> samples. Indian J Med Res 1991; 93 : 364-5.<br />
13. Stout JE, Rihs JD, Yu VL. <strong>Legionella</strong>. In: Murray PR, Baron<br />
EJ, Jorgensen JH, Pfaller MA, Yelken RH, editors. Manual<br />
<strong>of</strong> <strong>clinical</strong> microbiology, vol. 2, 8th ed. Washington DC: ASM<br />
Press; 2003. p. 809-23.<br />
14. Vickers RM, Stout JE, Yu VL, Rihs JD. Manual <strong>of</strong> culture<br />
methodology for <strong>Legionella</strong>. Semin Respir Infect 1987; 2 :<br />
274-9.<br />
15. Hebert GA. Hippurate hydrolysis by <strong>Legionella</strong> <strong>pneumophila</strong>.<br />
J Clin Microbiol 1981; 13 : 240-2.<br />
16. Yu VL, Stout JE. Community-acquired legionnaires’ disease:<br />
implications for under diagnosis and laboratory testing. Clin<br />
Infect Dis 2008; 46 : 1365-7.<br />
17. Charles PG, Whitby M, Fuller AJ, Stirling R, Wright AA,<br />
Korman TM, et al. The etiology <strong>of</strong> community-acquired<br />
pneumonia in Australia: why penicillin plus doxycycline or a<br />
macrolide is the most appropriate therapy. Clin Infect Dis 2008;<br />
46 : 1513-21.<br />
18. Lim WS, Macfarlane JT, Boswell TC, Harrison TG, Rose D,<br />
Leinonen M, et al. Study <strong>of</strong> community acquired pneumonia<br />
aetiology (SCAPA) in adults admitted to hospital: implications<br />
for management guidelines. Thorax 2001; 56 : 296-301.<br />
19. Yu VL, Greenberg RN, Zadekis N, Stout JE, Khashab MM,<br />
Olson WH, et al. Lev<strong>of</strong>loxacin efficacy in the treatment <strong>of</strong><br />
community-acquired legionellosis. Chest 2004; 125 : 135-9.<br />
20. Sehulster L, Chinn RYW. Guidelines for <strong>environmental</strong><br />
infections control in health care facilities. Recommendations <strong>of</strong><br />
CDC and the Health Care Infections Control Practices Advisory<br />
Committee (HICPAC). MMWR Morb Mortal Wkly Rep 2003;<br />
52 : 1-42.<br />
21. Ta AC, Stout JE, Yu VL, Wagener MM. Comparison <strong>of</strong> culture<br />
methods for monitoring <strong>Legionella</strong> species in hospital potable<br />
water systems and recommendations for standardization <strong>of</strong><br />
such methods. J Clin Microbiol 1995; 33 : 2118-23.<br />
22. Goetz A, Yu VL. Nosocomical legionella infection. In: Mayhail<br />
CG, editor. Hospital epidemiology and infection control.<br />
Baltimore: Williams & Wilkins; 1996. p. 388-99.<br />
23. Goetz AM, Stout JE, Jacobs SL, Fisher MA, Ponzer RE,<br />
Drenning S, et al. Nosocomial legionnaires’ disease discovered<br />
in community hospitals following cultures <strong>of</strong> the water system:<br />
Seek and ye shall find. Am J Infect Control 1998; 26 : 8-11.<br />
24. Brown RB, Sands M, Ryczak M. Community-acquired<br />
pneumonia caused by mixed aerobic bacteria. Chest 1986; 90<br />
: 810-4.<br />
25. Wattanathum A, Chaoprasong C, Nunthapisud P, Chantaratchada<br />
S, Limpairojn N, Jatakanon A, et al. Community-acquired<br />
pneumonia in Southeast Asia: the microbial differences<br />
between ambulatory and hospitalized patients. Chest 2003; 123<br />
: 1512-9.<br />
Reprint requests: Dr Abhijit Chaudhury, Additional Pr<strong>of</strong>essor, Department <strong>of</strong> Microbiology, Sri Venkateswara Institute <strong>of</strong> Medical<br />
Sciences, Tirupati 517 507, Andhra Pradesh, India<br />
e-mail: ach1964@rediffmail.com