Angiotensin II Receptor Antagonists (ARBs), Renin Inhibitors, and ...
Angiotensin II Receptor Antagonists (ARBs), Renin Inhibitors, and ...
Angiotensin II Receptor Antagonists (ARBs), Renin Inhibitors, and ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Angiotensin</strong> <strong>II</strong> <strong>Receptor</strong> <strong>Antagonists</strong><br />
(<strong>ARBs</strong>),<br />
<strong>Renin</strong> <strong>Inhibitors</strong>, <strong>and</strong> Combinations<br />
Step Therapy Program Summary<br />
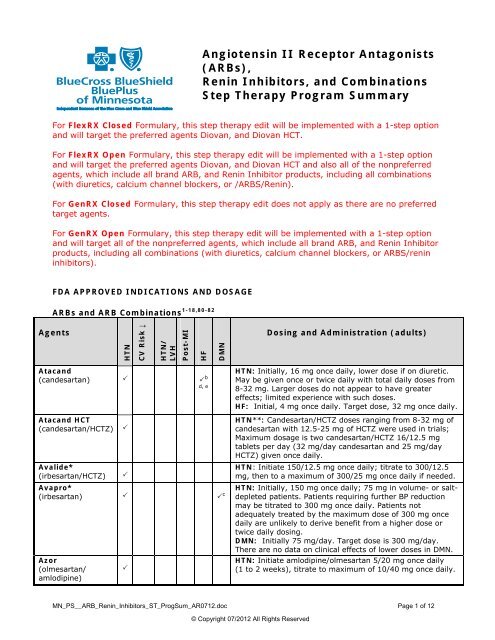
For FlexRX Closed Formulary, this step therapy edit will be implemented with a 1-step option<br />
<strong>and</strong> will target the preferred agents Diovan, <strong>and</strong> Diovan HCT.<br />
For FlexRX Open Formulary, this step therapy edit will be implemented with a 1-step option<br />
<strong>and</strong> will target the preferred agents Diovan, <strong>and</strong> Diovan HCT <strong>and</strong> also all of the nonpreferred<br />
agents, which include all br<strong>and</strong> ARB, <strong>and</strong> <strong>Renin</strong> Inhibitor products, including all combinations<br />
(with diuretics, calcium channel blockers, or /ARBS/<strong>Renin</strong>).<br />
For GenRX Closed Formulary, this step therapy edit does not apply as there are no preferred<br />
target agents.<br />
For GenRX Open Formulary, this step therapy edit will be implemented with a 1-step option<br />
<strong>and</strong> will target all of the nonpreferred agents, which include all br<strong>and</strong> ARB, <strong>and</strong> <strong>Renin</strong> Inhibitor<br />
products, including all combinations (with diuretics, calcium channel blockers, or ARBS/renin<br />
inhibitors).<br />
FDA APPROVED INDICATIONS AND DOSAGE<br />
<strong>ARBs</strong> <strong>and</strong> ARB Combinations 1-18,80-82<br />
Agents<br />
Atac<strong>and</strong><br />
(c<strong>and</strong>esartan)<br />
Atac<strong>and</strong> HCT<br />
(c<strong>and</strong>esartan/HCTZ)<br />
Avalide*<br />
(irbesartan/HCTZ)<br />
Avapro*<br />
(irbesartan)<br />
Azor<br />
(olmesartan/<br />
amlodipine)<br />
HTN<br />
<br />
<br />
<br />
<br />
<br />
CV Risk ↓<br />
HTN/<br />
LVH<br />
Post-MI<br />
HF<br />
b<br />
d, e<br />
DMN<br />
c<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 1 of 12<br />
© Copyright 07/2012 All Rights Reserved<br />
Dosing <strong>and</strong> Administration (adults)<br />
HTN: Initially, 16 mg once daily, lower dose if on diuretic.<br />
May be given once or twice daily with total daily doses from<br />
8-32 mg. Larger doses do not appear to have greater<br />
effects; limited experience with such doses.<br />
HF: Initial, 4 mg once daily. Target dose, 32 mg once daily.<br />
HTN**: C<strong>and</strong>esartan/HCTZ doses ranging from 8-32 mg of<br />
c<strong>and</strong>esartan with 12.5-25 mg of HCTZ were used in trials;<br />
Maximum dosage is two c<strong>and</strong>esartan/HCTZ 16/12.5 mg<br />
tablets per day (32 mg/day c<strong>and</strong>esartan <strong>and</strong> 25 mg/day<br />
HCTZ) given once daily.<br />
HTN: Initiate 150/12.5 mg once daily; titrate to 300/12.5<br />
mg, then to a maximum of 300/25 mg once daily if needed.<br />
HTN: Initially, 150 mg once daily; 75 mg in volume- or saltdepleted<br />
patients. Patients requiring further BP reduction<br />
may be titrated to 300 mg once daily. Patients not<br />
adequately treated by the maximum dose of 300 mg once<br />
daily are unlikely to derive benefit from a higher dose or<br />
twice daily dosing.<br />
DMN: Initially 75 mg/day. Target dose is 300 mg/day.<br />
There are no data on clinical effects of lower doses in DMN.<br />
HTN: Initiate amlodipine/olmesartan 5/20 mg once daily<br />
(1 to 2 weeks), titrate to maximum of 10/40 mg once daily.
Agents<br />
Benicar<br />
(olmesartan)<br />
Benicar HCT<br />
(olmesartan/HCTZ)<br />
Cozaar<br />
(losartan)*<br />
Diovan<br />
(valsartan)<br />
Diovan HCT<br />
(valsartan/HCTZ)<br />
Edarbi<br />
(azilsartan)<br />
Edarbyclor<br />
(azilsartan/<br />
chorthalidone<br />
Exforge<br />
(valsartan/<br />
amlodipine)<br />
Exforge HCT<br />
(valsartan/<br />
amlodipine/ HCTZ)<br />
Hyzaar<br />
(losartan/HCTZ)*<br />
Micardis<br />
(telmisartan)<br />
HTN<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
CV Risk ↓<br />
<br />
HTN/<br />
LVH<br />
a<br />
a<br />
Post-MI<br />
<br />
HF<br />
b<br />
d<br />
DMN<br />
c<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 2 of 12<br />
© Copyright 07/2012 All Rights Reserved<br />
Dosing <strong>and</strong> Administration (adults)<br />
HTN: Initially, 20 mg once daily; if volume-depleted, begin<br />
therapy with 5-10 mg once daily. Range 20-40 mg/day,<br />
given once daily. Doses >40 mg/day do not appear to have<br />
greater benefit; twice daily dosing has no advantage over<br />
the same dose given once daily.<br />
HTN**: Initial dose one tablet daily. Adjust based on<br />
clinical response. Olmesartan <strong>and</strong> HCTZ have been used<br />
together in clinical trials in doses from 10 to 40 mg of<br />
olmesartan with 12.5 to 25 mg of HCTZ. Maximum dosage is<br />
one tablet of olmesartan/HCTZ 40 mg/25 mg per day.<br />
HTN: Initial dose 50 mg once daily; 25 mg if volume<br />
depletion or hepatic impairment. May dose once or twice<br />
daily; total daily dose range is 25-100 mg.<br />
HTN/LVH: Usual initial dose is 50 mg once daily, may be<br />
increased to 100 mg once daily, followed by an increase in<br />
HCTZ to 25 mg once daily, based on BP response.<br />
DMN: Usual initial dose is 50 mg once daily. Dose should be<br />
increased to 100 mg once daily based on BP response.<br />
HTN: Initially, 80 or 160 mg once daily in patients not<br />
volume depleted. Patients requiring greater reduction can<br />
start at the higher dose. Range 80-320 mg once daily.<br />
Post-MI: Initiate 20 mg twice daily as early as 12 hours<br />
after MI, titrate over 7 days up to 40 mg twice daily. Titrate<br />
to maintenance dose of 160 mg twice daily, as tolerated.<br />
HF: Initially, 40 mg twice daily. Titrate to highest dose<br />
tolerated, range of 80-160 mg twice daily (maximum dose).<br />
HTN: Initiate with valsartan/HCTZ 160/12.5 mg once daily.<br />
Titrate to maximum of 320/25 mg once daily.<br />
HTN: The recommended dose is 80 mg once daily. Consider<br />
starting dose of 40 mg in patients on high dose diuretics.<br />
HTN: The recommended dose is 40/12.5 mg once daily.<br />
Maximum dose is 40/25 mg once daily.<br />
HTN: When used as initial therapy, start with amlodipine/<br />
valsartan 5/160 mg once daily; then titrate upwards as<br />
necessary to maximum of 10/320 mg once daily.<br />
HTN**: Individualize the dosage by titration of amlodipine,<br />
HCTZ, <strong>and</strong> valsartan. The dosage of one or all components<br />
may be increased after 2 weeks. Maximum daily dose is<br />
10 mg amlodipine, 25 mg HCTZ, <strong>and</strong> 320 mg valsartan.<br />
HTN**: Initial dose losartan/HCTZ 50/12.5 mg once daily.<br />
May increase to 2 tablets of 50/12.5 once daily or 1 tablet of<br />
100/25 once daily. Max daily dose is losartan/HCTZ 100/25.<br />
HTN/LVH: Initially, 50 mg losartan once daily. May add<br />
HCTZ 12.5 mg once daily, may increase losartan to 100 mg,<br />
or use losartan/HCTZ 100/12.5 once daily. Maximum daily<br />
dosage is losartan/HCTZ 100/25.<br />
HTN: Usual initial dose is 40 mg once daily; 20 mg once<br />
daily if volume-depleted; range 20-80 mg once daily.<br />
CV risk ↓: Recommended dose is 80 mg once daily;<br />
unknown whether doses
Agents<br />
Micardis HCT<br />
(telmisartan/HCTZ)<br />
Teveten<br />
(eprosartan)<br />
Teveten HCT<br />
(eprosartan/HCTZ)<br />
Tribenzor<br />
(olmesartan/<br />
amlodipine/HCTZ)<br />
Twynsta<br />
(telmisartan/<br />
amlodipine)<br />
HTN<br />
<br />
<br />
<br />
<br />
<br />
CV Risk ↓<br />
HTN/<br />
LVH<br />
Post-MI<br />
HF<br />
DMN<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 3 of 12<br />
© Copyright 07/2012 All Rights Reserved<br />
Dosing <strong>and</strong> Administration (adults)<br />
HTN**: Telmisartan/ HCTZ studied in clinical trials in doses<br />
20-160 mg of telmisartan with HCTZ 6.25-25 mg. Maximum<br />
dose is two telmisartan/ HCTZ 80/12.5 mg tablets per day<br />
(160 mg/day telmisartan <strong>and</strong> 25 mg/day HCTZ).<br />
HTN: Initially, 600 mg once daily in patients not volume<br />
depleted. Give once or twice daily, total daily doses range<br />
400-800 mg. Limited experience with doses >800 mg/day.<br />
HTN**: Initial dose is one tablet of eprosartan/ HCTZ<br />
600/12.5 mg once daily, which may be increased to one<br />
tablet of eprosartan/HCTZ 600/25 mg once daily. If needed,<br />
an additional 200-300 mg eprosartan may be given.<br />
Eprosartan <strong>and</strong> HCTZ have studied together in clinical trials<br />
in doses of 600-800 mg/day eprosartan (as single or divided<br />
doses) combined with 12.5-25 mg/day HCTZ. Maximum<br />
dosage- 900 mg/day eprosartan <strong>and</strong> 25 mg/day HCTZ.<br />
HTN: Dose once daily. Dosage may be increased after 2<br />
weeks. The maximum recommended doser is 40/10/25 mg.<br />
HTN: Initial: 1 tablet amlodipine/telmisartan 5/40 mg once<br />
daily. Initiate with amlodipine/ telmisartan 5/80 mg once<br />
daily in patients requiring larger BP reductions. Maximum<br />
dose: 10 mg/day amlodipine/80 mg/day telmisartan<br />
HTN= hypertension; LVH = left ventricular hypertrophy; MI = myocardial infarction; DMN = diabetic nephropathy;<br />
HCTZ = hydrochlorothiazide, HF=heart failure; CV risk ↓= cardiovascular risk reduction (MI, stroke, death) in high risk<br />
patients unable to take ACE inhibitors<br />
All ACEI <strong>and</strong> ARB single entity agents may be used as monotherapy or in combination for the treatment of hypertension.<br />
*agents available as generics<br />
** To minimize dose independent side effects, it is usual to begin combination therapy only after patients fail to achieve<br />
desired effects with monotherapy; combination products may be substituted for previously titrated components.<br />
a - Reduction in the risk of stroke in patients with hypertension <strong>and</strong> LVH<br />
b - Treatment of heart failure [New York Heart Association (NYHA) class <strong>II</strong>-IV] in patients unable to tolerate an ACEI<br />
c - Treatment of DMN with an elevated serum creatinine <strong>and</strong> in patients with type 2 diabetes <strong>and</strong> HTN<br />
d - In patients intolerant of ACEIs e - In combination with ACEI<br />
<strong>Renin</strong> <strong>Inhibitors</strong>, <strong>Renin</strong> Inhibitor Combinations 19-21,66,67<br />
Agents<br />
Amturnide<br />
(aliskiren/<br />
amlodipine/HCTZ)<br />
Tekamlo<br />
(aliskiren/<br />
amlodipine)<br />
Tekturna<br />
(aliskiren)<br />
Tekturna HCT<br />
(aliskiren/HCTZ)<br />
HTN<br />
<br />
<br />
<br />
<br />
CV Risk ↓<br />
HTN/LV<br />
H<br />
Post-MI<br />
HF<br />
DMN<br />
Dosing <strong>and</strong> Administration (adults)<br />
HTN: Initial dosing will depend on prior therapy. Dose<br />
once-daily. Maximum dose- 300 mg/10 mg/25 mg once<br />
daily.<br />
HTN: Initially, aliskiren/amlodipine 150 mg/5 mg once<br />
daily. Titrate as needed up to maximum dose of<br />
300 mg/10 mg daily.<br />
HTN: Initially, aliskiren 150 mg once daily. If BP<br />
remains uncontrolled, titrate up to 300 mg daily.<br />
Maximum dose- 300 mg/day.<br />
HTN: Usual recommended starting dose is<br />
aliskiren/HCTZ 150/12.5 mg once daily. If BP remains<br />
uncontrolled after 2-4 weeks of therapy, may be titrated<br />
to a maximum of 300 mg aliskiren, 25 mg HCTZ.
Valturna<br />
(aliskiren/valsartan)<br />
<br />
HTN: Initially, aliskiren/valsartan 150/160 mg once<br />
daily. Titrate up to a maximum of 300/320 mg if<br />
hypertension remains uncontrolled after 2-4 weeks.<br />
HTN= hypertension; LVH = left ventricular hypertrophy; MI = myocardial infarction; DMN = diabetic nephropathy;<br />
HCTZ = hydrochlorothiazide, HF=heart failure<br />
CLINICAL RATIONALE<br />
Hypertension<br />
All of the currently available ACEIs are indicated for the treatment of hypertension <strong>and</strong> there are<br />
minimal data to suggest that one ACEI is superior to another. 22.22, Multiple outcome trials with<br />
ACEIs in the treatment of hypertension have been conducted. Two outcome trials, ALLHAT 24 <strong>and</strong><br />
ANBP2, 25 are particularly important in establishing ACEIs as first or second line treatment<br />
options for hypertension.<br />
ACEIs are recommended as a first-line option for patients with hypertension, hypertension<br />
complicated by comorbidities, such as cerebrovascular disease, chronic kidney disease (of<br />
diabetic or nondiabetic origin), diabetes, HF, left ventricular dysfunction <strong>and</strong> MI by nine sets of<br />
clinical guidelines ( JNC 7 32 , European Society of Cardiology/European Society of Hypertension 70 ,<br />
American Heart Association / American College of Cardiology(AHA/ACC 49) , British Hypertension<br />
Society 71 National Kidney Foundation 72 American Diabetes Association 73 , Agency for Healthcare<br />
Research <strong>and</strong> Quality[AHRQ] 71 , AHA Council for High Blood Pressure Research <strong>and</strong> the Councils<br />
on Clinical Cardiology <strong>and</strong> Epidemiology, <strong>and</strong> Prevention 75 , <strong>and</strong> the Heart Failure Society of<br />
America 65 ) <strong>and</strong> all of these agencies do not establish a preference for one ACEI over another.<br />
<strong>ARBs</strong><br />
Large outcome trials 26-29 as well as nine sets of guidelines (National Institute for Health <strong>and</strong><br />
Human Excellence [NICE] 77 , Agency of Healthcare Research <strong>and</strong> Quality [AHRQ], 74 Heart Failure<br />
Society of America [HFSA], 65 American College of Cardiology Foundation/American Heart<br />
Association [ACCF/AHA Hypertension in the Elderly 50 , American Society of HTN [ASH] 79 ,<br />
International Society of Nephrology 100 , ACCF/AHA Guideline for the Diagnosis <strong>and</strong> Treatment of<br />
Hypertrophic Cardiomyopathy [HCM] 25 , The American Diabetes Association [ADA] 73 , <strong>and</strong> the<br />
Medical Letter 23 ) document that <strong>ARBs</strong> provide significant benefits <strong>and</strong> are recommended as first<br />
line agents in the treatment of HTN, HTN with left ventricular hypertrophy, diabetic<br />
nephropathy, chronic HF <strong>and</strong> HF following MI., <strong>ARBs</strong> are as effective as ACEIs , <strong>and</strong> appear<br />
equally reno <strong>and</strong> cardioprotective, with fewer adverse effects in some patients.<br />
In patients with essential hypertension, high cardiac risk factors, recent MI, HF, or nephropathy<br />
there are no data to suggest that one ARB is superior to another for safety or efficacy. 10,77,50,73<br />
Direct <strong>Renin</strong> <strong>Inhibitors</strong><br />
Aliskiren was evaluated by the FDA for treatment of hypertension in a large clinical development<br />
program including five primary r<strong>and</strong>omized, double-blind, placebo-controlled studies (these are<br />
all published); several other supportive studies (posters/abstracts <strong>and</strong>/or unpublished) were<br />
reviewed by the FDA as well. The five pivotal studies were r<strong>and</strong>omized, double-blind, placebocontrolled,<br />
8 week trials, with a primary endpoint of change from baseline in seated trough cuff<br />
diastolic blood pressure (DBP). Some trials evaluated active control arms, <strong>and</strong>/or combinations<br />
with another antihypertensive. The FDA felt that these studies provided evidence that aliskiren<br />
reduces blood pressure (BP). Blood pressure reduction was typically seen after two weeks of<br />
therapy, <strong>and</strong> effects were maximal by four weeks. Antihypertensive effects were sustained for at<br />
least 11 months in a r<strong>and</strong>omized, double-blind, placebo controlled withdrawal at the end of a<br />
long-term safety study. 20<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 4 of 12<br />
© Copyright 07/2012 All Rights Reserved
In December 2010 the FDA approved the triple combination product Amturnide (aliskerin/<br />
amlodipine/ HCTZ) for the treatment of hypertension. This fixed dose combination is not<br />
indicated for the initial treatment of hypertension. Amturnide is indicated for patients not<br />
adequately controlled with any tow ot the following: aliskerin, dihydropyridine calcium channel<br />
blockers, <strong>and</strong> thiazide diuretics. Amturnide was approved pursuant to section 505(b)(2) of the<br />
Federal Food, Drug <strong>and</strong> Cosmetic act 67 . A 505(b)(2) application is one for which one or more of<br />
the investigations relied upon by the applicant for approval "were not conducted by or for the<br />
applicant <strong>and</strong> for which the applicant has not obtained a right of reference or use from the<br />
person by or for whom the investigations were conducted" 68<br />
In 2010 the FDA also approved the combination product Tekamlo (aliskerin/amlodipine) for<br />
treatment of hypertension. 66 It is indicated as initial therapy in patients likely to need multiple<br />
drugs to achieve their blood pressure goals; in patients not adequately controlled with<br />
monotherapy; <strong>and</strong> as a substitute for Tekamlo’s titrated components. Similar to Amtunide,<br />
Tekamlo was FDA approved pursuant to section 505 (b)(2) of the Federal Food, Drug, <strong>and</strong><br />
Cosmetic act. 68<br />
In January 2012, Novartis Pharmaceuticals sent out a safety letter informing healthcare<br />
professionals of the results of the Aliskiren Trial in Type 2 Diabetics Using Cardio-Renal<br />
Endpoints (ALTITUDE) trial. 76 The ALTITUDE study was conducted in type 2 diabetic patients,<br />
known to be at risk of fatal <strong>and</strong> non-fatal cardiovascular <strong>and</strong> renal events. In this study,<br />
aliskiren 300 mg (or placebo) was given in addition to st<strong>and</strong>ard of care, including an angiotensin<br />
ACEI or an ARB. The independent Data Monitoring Committee overseeing the trial concluded<br />
that patients were unlikely to benefit from treatment added to st<strong>and</strong>ard antihypertensives. The<br />
committee also noted a higher adverse event rate in these high-risk patients receiving aliskiren<br />
combined with st<strong>and</strong>ard care. Specifically, the committee highlighted an increased incidence of<br />
nonfatal stroke, renal complications, hyperkalemia <strong>and</strong> hypotension among those who had<br />
received 18 to 24 months of treatment with aliskiren as well as st<strong>and</strong>ard therapy. Novartis<br />
advised healthcare professionals, pending further analyses, a contra-indication in patients with<br />
diabetes taking an ACEI or an ARB is now advised. The treatment of diabetic patients taking<br />
aliskiren-containing products should therefore be reviewed as early as possible, taking the<br />
following advice into consideration <strong>and</strong> stopped.<br />
Heart Failure, Including Post Myocardial Infarction<br />
ACEI <strong>and</strong> <strong>ARBs</strong>ACEIs are well established for the treatment of heart failure (HF), <strong>and</strong> are<br />
strongly recommended in treatment guidelines. 34,42 A retrospective cohort study comparing the<br />
effectiveness of different ACEIs in the treatment of patients with HF found no significant<br />
differences in the combined endpoint of hospital readmission for HF or mortality <strong>and</strong> suggests a<br />
class effect among the ACEIs for this indication. 46 There are outcomes data for three <strong>ARBs</strong><br />
(c<strong>and</strong>esartan, losartan, valsartan) in congestive heart failure (CHF). 32,34,42,44-48 One head-tohead<br />
trial found no difference in mortality between an ACEI <strong>and</strong> an ARB, but due to the study<br />
design, equivalence could not be concluded. 46 In another head-to-head trial valsartan was found<br />
to be as effective as captopril in patients who were at high risk for cardiovascular events after<br />
myocardial infarction (MI). 48 <strong>ARBs</strong> may be a reasonable alternative in HF patients unable to<br />
tolerate ACEIs.<br />
• The Heart Failure Society of America (HFSA) 2010 Comprehensive Heart Failure Practice<br />
Guideline states the following: 65 ACEIs are recommended for routine administration to<br />
symptomatic <strong>and</strong> asymptomatic patients with LVEF ≤ 40%. <strong>ARBs</strong> are recommended for<br />
routine administration to symptomatic <strong>and</strong> asymptomatic patients with LVEF≤ 40% who<br />
are intolerant to ACEIs for reasons other than hyperkalemia or renal insufficiency.<br />
Renal Disease Diabetic Nephropathy<br />
ACEIs<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 5 of 12<br />
© Copyright 07/2012 All Rights Reserved
While both ACEIs <strong>and</strong> <strong>ARBs</strong> given alone have been found to decrease the progression of<br />
microalbuminuria to overt proteinuria, ACEIs currently have the strongest evidence for delaying<br />
progression of chronic non-diabetic renal disease as well as nephropathy in type 1 diabetes. 23<br />
<strong>ARBs</strong><br />
Two <strong>ARBs</strong>, losartan <strong>and</strong> irbesartan, have been found to be of benefit in preventing worsening<br />
renal function in type 2 diabetes patients with proteinuria; 8,47 no ACEIs have been proven, in a<br />
single r<strong>and</strong>omized, controlled trial to offer this benefit in this population. However, captopril has<br />
been found to reduce risk of a combined endpoint of death, dialysis <strong>and</strong> transplantation in type<br />
1 diabetes patients with overt proteinuria, 52 <strong>and</strong> a meta-analysis of patients with or without<br />
diabetes <strong>and</strong> with overt proteinuria found that ACEIs reduced risk of a composite of doubling of<br />
serum creatinine or development of end stage renal disease (ESRD). 53 Furthermore, persons<br />
with type 2 diabetes <strong>and</strong> renal disease are at increased cardiovascular risk. There is evidence<br />
that indicates this risk may be reduced with the use of an ACEI. In the absence of long-term<br />
outcome trials comparing an ACEI to an ARB to determine if these agents provide similar<br />
benefits in patients with type 2 diabetes <strong>and</strong> microalbuminuria or nephropathy, major clinical<br />
guidelines either are neutral or recommend an ACEI as first line therapy. 33,54,55<br />
Guidelines from the American Diabetes Association (ADA, 2010) state: “Pharmacologic therapy<br />
for patients with diabetes <strong>and</strong> hypertension should be with a regimen that includes either an<br />
ACEI or an ARB. If one class is not tolerated, the other should be substituted.” 54<br />
Safety<br />
In a drug class review of ACEIs for its practitioner-managed prescription drug plan, the Oregon<br />
Evidence-based Practice Center identified 24 head-to-head trials comparing adverse event rates<br />
of different ACEIs in the treatment of hypertension, prevention of events after MI, <strong>and</strong> HF. 56<br />
There was little evidence of meaningful differences in tolerability profiles for the agents. 78 As a<br />
class, <strong>ARBs</strong> are well tolerated, with adverse events profiles for the agents generally similar to<br />
placebo, 56,67 though large placebo-controlled trials have found more discontinuations due to<br />
adverse events with <strong>ARBs</strong>. 44,58 Some trials comparing ACEIs <strong>and</strong> <strong>ARBs</strong> have found differences in<br />
rate of cough, <strong>and</strong> in discontinuations due to adverse events, favoring the <strong>ARBs</strong>, primarily due<br />
to differences in rate of cough. 45,46,59,60 Although the rate of angioedema appears to be lower<br />
with <strong>ARBs</strong> than ACEIs, the rates are low for each class. 60 It is unclear if there are important<br />
differences in effects on potassium between ACEIs <strong>and</strong> <strong>ARBs</strong>.<br />
For additional clinical information see the Prime Therapeutics Formulary Chapters 5.6A ACE<br />
<strong>Inhibitors</strong> & ACE/diuretic combinations; 5.6B <strong>Angiotensin</strong> <strong>II</strong> <strong>Receptor</strong> Blockers <strong>and</strong><br />
Combinations; 5.6H ACEI <strong>and</strong> ARB/Calcium Channel <strong>Antagonists</strong> Combinations.<br />
REFERENCES<br />
1. Atac<strong>and</strong> prescribing information. AstraZeneca. October 2009.<br />
2. Atac<strong>and</strong> HCT prescribing information. AstraZeneca. May 2008.<br />
3. Avapro prescribing information. Bristol-Myers Squibb, Sanofi-Aventis. April 2007.<br />
4. Avalide prescribing information. Bristol-Myers Squibb, Sanofi-Aventis. November 2008.<br />
5. Benicar prescribing information. Daiichi-Sankyo, Inc. 2009.<br />
6. Benicar HCT prescribing information. Daiichi-Sankyo, Inc. July 2007.<br />
7. Cozaar prescribing information. Merck & Co., Inc. December 2009.<br />
8. Hyzaar prescribing information. Merck & Co., Inc. December 2009.<br />
9. Diovan prescribing information. Novartis Pharmaceuticals Corporation. December 2008.<br />
10. Diovan HCT prescribing information. Novartis Pharmaceuticals Corporation. May 2009.<br />
11. Micardis prescribing information. Boehringer Ingelheim Pharmaceuticals, Inc. October<br />
2009.<br />
12. Micardis HCT prescribing information. Boehringer Ingelheim Pharmaceuticals, Inc.<br />
November 2009.<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 6 of 12<br />
© Copyright 07/2012 All Rights Reserved
13. Teveten prescribing information. Abbott Laboratories. August 2007.<br />
14. Teveten HCT prescribing information. Abbott Laboratories. October 2008.<br />
15. Azor prescribing information. Daiichi-Sankyo, Inc. May 2009.<br />
16. Exforge prescribing information. Novartis Pharmaceuticals Corporation. February 2009.<br />
17. Exforge HCT prescribing information. Novartis Pharmaceuticals Corporation. August<br />
2009.<br />
18. Twynsta prescribing information. Boehringer Ingelheim Pharmaceuticals Inc. October<br />
2009.<br />
19. Tekturna prescribing information. Novartis Pharmaceuticals Corporation. February 2010.<br />
20. Tekturna HCT prescribing information. Novartis Pharmaceuticals Corporation. February<br />
2010.<br />
21. Valturna prescribing information. Novartis Pharmaceuticals Corporation. February 2010.<br />
22. White CM. Pharmacologic, pharmacokinetic, <strong>and</strong> therapeutic differences among ACE<br />
inhibitors. Phamacotherapy 1998;18(3):588-599.<br />
23. Accessed May 18, 2007. The Medical Letter Treatment Guidelines. Drugs for HTN 2012.<br />
The Med Letter Treatment Guidelines 2012;10(113):1-10.<br />
24. The ALLHAT Officers <strong>and</strong> Co-ordinators for the ALLHAT Collaborative Research Group.<br />
Major cardiovascular events in hypertensive patients r<strong>and</strong>omly assigned to doxazosin vs<br />
chlorthalidone: the antihypertensive <strong>and</strong> lipid lowering treatment to prevent heart attack<br />
trial (ALLHAT). JAMA 2002;283:1967-1975.<br />
25. Wing LMH, Reid CM, Ryan P et al. A comparison of outcomes with angiotensinconverting-enzyme<br />
inhibitors <strong>and</strong> diuretics for hypertension in the elderly. N Engl J Med<br />
2003;348:583-92.<br />
26. Dalhöf B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity <strong>and</strong> mortality in the<br />
losartan intervention for endpoint reduction in hypertension study (LIFE): a r<strong>and</strong>omized<br />
trial against atenolol. Lancet 2002;359:995-1003.<br />
27. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotension<br />
receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N<br />
Engl J Med 2001;345:851-860.<br />
28. Brenner BM, Cooper ME, Zeeuw DD, et al. Effects of losartan on renal <strong>and</strong> cardiovascular<br />
outcomes in patients with type 2 diabetes <strong>and</strong> nephropathy. N Engl J Med 2001;345:861-<br />
869.<br />
29. Parving HH, Lehnert H, Mortensen Bröchner J et al. The effect of irbesartan on the<br />
development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med<br />
2001;345:870-8.<br />
30. Conlin PR. <strong>Angiotensin</strong> <strong>II</strong> antagonists in the treatment of hypertension: more similarities<br />
than differences. J Clin Hypertens 2(4):253-257, 2000.<br />
31. Agency for Healthcare Research <strong>and</strong> Quality (AHQR). Comparative effectiveness of<br />
angiotensin converting enzyme inhibitors (ACEIs) <strong>and</strong> angiotensin <strong>II</strong> receptor antagonists<br />
(<strong>ARBs</strong>) for treating hypertension (draft report). Jan 2007. Available at: www.ahrq.gov.<br />
Accessed May 2007.<br />
32. Chobanian AV, Bakris GL, Black HR, et al. Seventh Report of the Joint National<br />
Committee on Prevention, Detection, Evaluation, <strong>and</strong> Treatment of High Blood Pressure.<br />
Hypertension. 2003;42:1206-52.<br />
33. American Diabetes Association. St<strong>and</strong>ards of Medical Care in Diabetes – 2007. Diabetes<br />
Care. 2007;30(suppl 1): S4-S41.<br />
34. United Kingdom National Institute for Clinical Excellence. Chronic heart failure.<br />
Management of chronic heart failure in adults in primary <strong>and</strong> secondary care. Clinical<br />
Guideline 5, July 2003. http://www.nice.org.uk/pdf/CG5NICEguideline.pdf. Accessed May<br />
2007.<br />
35. Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines for<br />
hypertension management 2004 (BHS-IV): summary. BMJ. 2004;328:634-640.<br />
36. Practice Guidelines Writing Committee <strong>and</strong> ESH/ESC Hypertension Guidelines Committee.<br />
Practice Guidelines for Primary Care Physicians: 2003 ESH/ESC Hypertension Guidelines.<br />
J Hypertension 2003; 21:1779-1786.<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 7 of 12<br />
© Copyright 07/2012 All Rights Reserved
37. Kidney Disease Outcomes Quality Initiative (K/DOQI). K/DOQI clinical practice guidelines<br />
on hypertension <strong>and</strong> antihypertensive agents in chronic kidney disease. Am J Kidney Dis<br />
2004;43 (5 Supp1):S1-S290.<br />
38. Prime Therapeutics Formulary Chapter 5.6A: Antihypertensives: ACE <strong>Inhibitors</strong> &<br />
ACE/Diuretic Combinations. February 2009.<br />
39. Prime Therapeutics Formulary Chapter 5.6B: Antihypertensives: <strong>Angiotensin</strong> <strong>II</strong> <strong>Receptor</strong><br />
Blockers & Combinations. February 2009.<br />
40. Rosendorff C, Black HR, Cannon CP et al. Treatment of hypertension in the prevention<br />
<strong>and</strong> management of ischemic heart disease: a scientific statement from the American<br />
Heart Association Council for High Blood Pressure Research <strong>and</strong> the Councils on Clinical<br />
Cardiology <strong>and</strong> Epidemiology <strong>and</strong> Prevention. Circulation. 2007;115(21):2761-88.<br />
41. Barkis GL, Sowers JR, American Society of Hypertension Writing Group. ASH position<br />
paper: treatment of hypertension in patients with diabetes-an update. J Clin Hypertens<br />
2008;10:707-713.<br />
42. Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 guideline update for the diagnosis<br />
<strong>and</strong> management of chronic heart failure in the adult: summary article: a report of the<br />
American College of Cardiology/American Heart Association Task Force on Practice<br />
Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation <strong>and</strong><br />
Management of Heart Failure). Circulation 2005;112:154-235.<br />
43. Tu C, Mamdani M, Kopp A, Lee D. Comparison of angiotensin-converting enzyme<br />
inhibitors in the treatment of congestive heart failure. Am J Cardiol 2005;95(2):283-6.<br />
44. Cohn JN, Tognoni G for the Val-HeFT Investigators. A r<strong>and</strong>omized trial of the<br />
angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med<br />
2001;345:1667-1675.<br />
45. Pitt B, Segal R, Martinez FA, et al. R<strong>and</strong>omised trial of losartan versus captopril in<br />
patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE).<br />
Lancet 1997;349(9054):747-52.<br />
46. Pitt B, Poole-Wilson PA, Segal R, et al. Effect of losartan compared with captopril on<br />
mortality in patients with symptomatic heart failure: r<strong>and</strong>omised trial--the Losartan Heart<br />
Failure Survival Study ELITE <strong>II</strong>. Lancet 2000;355(9215):1582-7.<br />
47. Pfeffer MA, Swedberg K, Granger CB et al. Effects of c<strong>and</strong>esartan on mortality <strong>and</strong><br />
morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet<br />
2003;362:759-66.<br />
48. 70Dickstein K, Kjekshus J, <strong>and</strong> the OPTIMAAL Steering Committee. Effects of losartan<br />
<strong>and</strong> captopril on mortality <strong>and</strong> morbidity in high risk patients after acute myocardial<br />
infarction: the OPTIMAAL r<strong>and</strong>omized trial. Lancet 2002;360:752-60.<br />
49. Jessup M, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA guidelines for<br />
the diagnosis <strong>and</strong> management of heart failure in adults: a report of the American<br />
College of Cardiology Foundation/American Heart Association Task Force on Practice<br />
Guidelines developed in collaboration with the International Society for Heart <strong>and</strong> Lung<br />
Transplantation. J Am Coll Cardiol. 2009;53:1343-82.<br />
50. Aronow WS, Fleg JI, Pepine CJ, et al. ACCF/AHA 2011 Expert consensus document on<br />
hypertension in the elderly. J Am Coll Cardiol 2011;57:2037-2114.<br />
51. Fraker TD, Fihn SD, on behalf of the 2002 Chronic Stable Angina Writing Committee.<br />
2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the<br />
management of patients with chronic stable angina: a report of the American College of<br />
Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group<br />
to Develop the Focused Update of th 2002 Guidelines for the Management of Patients<br />
with Chronic Stable Angina. Circulation. 2007;116:2762-72.<br />
52. Lewis EJ, Hunsicker LG. The effect of angiotensin-converting-enzyme inhibition on<br />
diabetic nephropathy. N Engl J Med 1993;329:1456-62.<br />
53. Kshirsagar AV, Joy MS, Hogan SL et al. Effect of ACE inhibitors in diabetic <strong>and</strong><br />
nondiabetic chronic renal disease: a systematic review of r<strong>and</strong>omized placebo-controlled<br />
trials. Am J Kidney Dis 2000;35:695-707.<br />
54. American Diabetes Association. Executive Summary: St<strong>and</strong>ards of medical care in<br />
diabetes- 2010. Diabetes Care. 2010;33(suppl 1):s4-s10.<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 8 of 12<br />
© Copyright 07/2012 All Rights Reserved
55. McIntosh A, Hutchinson A, Marshall S et al (2002) Clinical Guidelines <strong>and</strong> Evidence<br />
Review for Type 2 Diabetes. Renal Disease: Prevention <strong>and</strong> Early Management. Sheffield:<br />
ScHAAR, University of Sheffield. http://www.shef.ac.uk/guidelines/guidelines/renal.pdf.<br />
Accessed May 2007.<br />
56. Oregon Evidence-Based Practice Center. Drug Class Review on <strong>Angiotensin</strong> Converting<br />
Enzyme <strong>Inhibitors</strong>. Final Report Update 2, June 2005. Available at:<br />
http://www.oregon.gov/DAS/OHPPR/HRC/docs/ACE_EPC.pdf . Accessed May 15, 2007.<br />
57. Oregon Health Services Commission Subcommittee Report <strong>ARBs</strong>, March 2006 Available<br />
at http://www.oregon.gov/DAS/OHPPR/HRC/docs/A<strong>II</strong>RA_HRC.pdf. Accessed May 15,<br />
2007.<br />
58. Granger CB, McMurray JJV, Yusuf S et al. Effects of c<strong>and</strong>esartan in patients with chronic<br />
heart failure <strong>and</strong> reduced left-ventricular systolic function intolerant to angiotensinconverting-enzyme<br />
inhibitors: the CHARM-Alternative trial. Lancet 2003;772-6.<br />
59. Pfeffer MA, McMurray JJV, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial<br />
infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med<br />
2003;349:1893-1906.<br />
60. Grossman E, Messerli FH, Neutel JM. <strong>Angiotensin</strong> <strong>II</strong> receptor blockers: equal or preferred<br />
substitutes for ACE inhibitors? Arch Intern Med 2000;160:1905-11.<br />
61. Miller AE, Cziracky M, Spinler SA. ACE inhibitors versus <strong>ARBs</strong>: comparison of practice<br />
guidelines <strong>and</strong> treatment selection considerations. Formulary 2006;41:274-284.<br />
62. Furberg CD, Pitt B. Are all angiotensin-converting enzyme inhibitors interchangeable? Am<br />
Coll Cardiol 2001 37: 1456-1460.<br />
63. Lee VC, Rhew DC, Dylan M, et al. Meta-analysis: angiotensin-receptor blockers in chronic<br />
heart failure <strong>and</strong> high-risk acute myocardial infarction. Ann Intern Med 2004;141:693-<br />
704.<br />
64. Gring CN, Francis GS. A hard look at angiotensin receptor blockers in heart failure. J Am<br />
Coll Cardiol 2004;44: 1841-1846.<br />
65. Albert NM, Boehmer JP, Collins SP, et al. Heart Failure Society of America (HFSA) 2010<br />
Comprehensive Heart Failure Practice Guidelines. J Cardiac Fail. 2010;16(6):475-539.<br />
66. Tekamlo prescribing information. Novartis Pharmaceuticals Corporation. August 2010.<br />
67. Amturnide prescribing information. Novartis Pharmaceuticals Corporation. December<br />
2010.<br />
68. FDA. Guidance for Industry : applications covered by section 505(b)(2). Available @<br />
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guida<br />
nces/ucm079345.pdf. Accessed January 2011.<br />
69. American Society of Hypertension. Combination therapy in hypertension. J Am Soc<br />
Hypertension. 2010;4(1):42-50.<br />
70. European Society of Cardiology. Expert consensus document on angiotensin converting<br />
enzyme inhibitors in cardiovascular disease. Eur Heart J 2005;25(16):1454-1470.<br />
71. British Hypertension Society. Guidelines <strong>and</strong> evaluation of hypertensive therapy. BMJ<br />
2009; 317:713-720.<br />
72. National Kidney Foundation. Clinical practice guidelines <strong>and</strong> clinical practice<br />
recommendations for diabetes <strong>and</strong> chronic kidney disease. Am J Kidney Dis<br />
2007;49(Supp1):S1-S180<br />
73. American Diabetes Association. St<strong>and</strong>ards of Care in Diabetes.Diabetes Care’ 2011<br />
Jan;34 Suppl 1:S11-61.<br />
74. S<strong>and</strong>ers GD, Coeytaux R, Dolor RJ, et al. <strong>Angiotensin</strong>-converting enzyme inhibitors<br />
(ACEIs), angiotensin <strong>II</strong> receptor antagonists (<strong>ARBs</strong>), <strong>and</strong> direct renin inhibitors for<br />
treating essential hypertension: an update . Comparative effectiveness review No.34<br />
AHQR Publication No 11-EHC063-EF. Agency for Healthcare Research <strong>and</strong> Quality<br />
(AHQR). June 2011. Accessed 1/17/2012 @<br />
www.effectivehealthcare.ahqr.gov/reports/final.cfm<br />
75. AHA. Treatment of hypertension in the prevention <strong>and</strong> management of ischemic heart<br />
disease: a scientific statement from the AHA Council for High Blood Pressure Research<br />
<strong>and</strong> the Councils on Clinical Cardiology <strong>and</strong> Epidemiology <strong>and</strong> Prevention. J Clinical HTN<br />
2007:9(8):649-651<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 9 of 12<br />
© Copyright 07/2012 All Rights Reserved
76. Novartis. Healthcare Professional Letter Regarding Aliskeri-containing Products. Jan 2012<br />
@ http://www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/prof/_2012/rasilez_hpc-cpseng.php<br />
77. National Health Service. NICE 2011 Guideline HTN #127. Accessed 2/6/2012 @<br />
www.nice.org<br />
78. 100International Society of Nephrology Clinical Update on Improving Global Outcomes<br />
2011;@ www.kidney-international.org<br />
79. American Society of Hypertension. Clinical Guidelines Hypertension. JClin Hpertens<br />
2008;10:707-713 33.<br />
80. Tribenzor prescribing information. Daiichi Sankyo, Inc. July 2010.<br />
81. Edarbi prescribing information. Takeda Pharmaceuticals Amerca, Inc. February 2011.<br />
82. Edarbyclor prescribing information. Takeda Pharmaceuticals America, Inc. December<br />
2011<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 10 of 12<br />
© Copyright 07/2012 All Rights Reserved
<strong>Angiotensin</strong> <strong>II</strong> <strong>Receptor</strong> <strong>Antagonists</strong> (<strong>ARBs</strong>), <strong>Renin</strong> <strong>Inhibitors</strong>, <strong>and</strong><br />
Combinations<br />
Step Therapy (1-Step)<br />
OBJECTIVE<br />
The intent of the <strong>Angiotensin</strong> <strong>II</strong> <strong>Receptor</strong> <strong>Antagonists</strong> (<strong>ARBs</strong>), <strong>Renin</strong> <strong>Inhibitors</strong> <strong>and</strong><br />
Combinations Step Therapy (ST) program is to encourage use of cost-effective generic<br />
products - ACEIs, ACEI combinations (ACEI/diuretics or ACEI/calcium channel blockers<br />
[CCBs]), <strong>ARBs</strong>, or ARB combinations - over the more expensive br<strong>and</strong> <strong>ARBs</strong>, br<strong>and</strong> ARB<br />
combinations, br<strong>and</strong> renin inhibitors <strong>and</strong> renin inhibitor combinations (renin inhibitor/diuretic,<br />
renin inhibitor/ARB, or renin inhibitor/CCB). This program will accommodate for use of br<strong>and</strong><br />
products when generic or preferred prerequisites cannot be used due to previous trial <strong>and</strong><br />
failure, documented intolerance, FDA labeled contraindication, or hypersensitivity. Requests for<br />
br<strong>and</strong> ARB or renin inhibitor products will be reviewed when patient-specific documentation is<br />
provided.<br />
TARGET DRUGS<br />
<strong>Angiotensin</strong> <strong>II</strong> <strong>Receptor</strong> <strong>Antagonists</strong> (<strong>ARBs</strong>),<br />
Combinations<br />
Br<strong>and</strong> Generic<br />
Atac<strong>and</strong> ® c<strong>and</strong>esartan c<br />
Atac<strong>and</strong> HCT ® c<strong>and</strong>esartan/HCTZ bc<br />
Avapro ® irbesartan a<br />
Avalide ® irbesartan/HCTZ ab<br />
Azor ® olmesartan/amlodipine<br />
Benicar ® olmesartan<br />
Benicar HCT ® olmesartan/HCTZ b<br />
Cozaar ® losartan a<br />
Edarbi ® azilsartan<br />
Edarbyclor ® azilsartan/chlorthalidone<br />
Exforge ® valsartan/amlodipine c<br />
Exforge HCT ® valsartan/amlodipine/HCTZ bc<br />
Hyzaar ® losartan/HCTZ ab<br />
Diovan ® valsartan c<br />
Diovan HCT ® valsartan/HCTZ bc<br />
Micardis ® telmisartan<br />
Micardis HCT ® telmisartan/HCTZ b<br />
Teveten ® eprosartan a<br />
Teveten HCT ® eprosartan/HCTZ b<br />
Tribenzor ® olmesartan/amlodipine/HCTZ<br />
Twynsta ® telmisartan/amlodipine<br />
<strong>Renin</strong> <strong>Inhibitors</strong>, Combinations<br />
Br<strong>and</strong> Generic<br />
Amturnide ® aliskiren/amlodipine/HCTZ b<br />
Tekamlo ® aliskiren/amlodipine<br />
Tekturna ® aliskiren<br />
Tekturna HCT ® aliskiren/HCTZ b<br />
Valturna ® aliskiren/valsartan<br />
a – generic available that is a prerequisite agent for step therapy program<br />
b - HCTZ = hydrochlorothiazide<br />
c – generic product anticipated in 2012; will be prerequisite for step therapy progam<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 11 of 12<br />
© Copyright 07/2012 All Rights Reserved
PRIOR AUTHORIZATION CRITERIA FOR APPROVAL<br />
Br<strong>and</strong> <strong>ARBs</strong>, ARB Combinations, <strong>Renin</strong> <strong>Inhibitors</strong>, or <strong>Renin</strong> Inhibitor combinations will<br />
be approved when ONE of the following is met:<br />
1. The patient’s medication history includes use of a generic ACEI, generic ACEI<br />
combination, generic ARB or a generic ARB combination OR<br />
2. There is documentation that the patient is currently using the requested br<strong>and</strong> ARB,<br />
ARB combination, renin inhibitor, or renin inhibitor combination, OR the requested<br />
br<strong>and</strong> ARB or renin inhibitor in another product (single ingredient or combination) OR<br />
3. The prescribing physician states the patient is using the requested br<strong>and</strong> ARB, ARB<br />
combination, renin inhibitor, or renin inhibitor combination or the requested br<strong>and</strong> ARB<br />
or renin inhibitor in another product (single ingredient or combination) AND is at risk if<br />
therapy is changed OR<br />
4. The patient has a documented intolerance, FDA labeled contraindication, or<br />
hypersensitivity to a generic ACEI, genric ACEI combination, generic ARB, or generic<br />
ARB combination product<br />
Length of Approval: 12 months<br />
NOTE: If Quantity Limit program also applies, please refer to Quantity Limit documents.<br />
MN_PS__ARB_<strong>Renin</strong>_<strong>Inhibitors</strong>_ST_ProgSum_AR0712.doc Page 12 of 12<br />
© Copyright 07/2012 All Rights Reserved