Joint major incident plan .pdf - NHS Dorset
Joint major incident plan .pdf - NHS Dorset
Joint major incident plan .pdf - NHS Dorset
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Major Incident Plan<br />
<strong>Joint</strong> Plan for <strong>NHS</strong> Bournemouth & Poole and <strong>NHS</strong> <strong>Dorset</strong><br />
April 2012
DOCUMENT DETAILS<br />
Document Title<br />
Version<br />
Status Final version<br />
Date Version Published 1 st April 2012<br />
<strong>NHS</strong> <strong>Dorset</strong> and <strong>NHS</strong> Bournemouth & Poole Major Incident<br />
Plan<br />
v. Final Available from:<br />
X:\PUBLIC HEALTH\PHFS\EMERGENCY PLANNING\EMERGENCY PLANNING\1.<br />
WITHIN DORSET\2. <strong>NHS</strong> DORSET\05 - EMERGENCY RESPONSE & RECOVERY<br />
PLAN - MAJOR INCIDENT PLAN\2012 MIP\2012 MARCH 29TH JOINT MIP<br />
VFINAL.DOCX<br />
Author(s) Emergency Planning Managers, Public Health Directorate<br />
Distribution<br />
Purpose:<br />
Intranet:- Yes<br />
Extranet:- No<br />
PCT Website:- No<br />
Policy Application Organisation wide<br />
Approving Committee PCT Trust Board<br />
Date of Review<br />
Date of Next Review April 2013<br />
Responsibility for<br />
Implementation<br />
Policy Statement<br />
Under the Civil Contingencies Act 2004, the Primary care<br />
Trust is a Category One Responder with specific statutory<br />
duties including Emergency Planning and Business<br />
Continuity.<br />
This <strong>plan</strong> sets out generic arrangements for <strong>NHS</strong><br />
Bournemouth & Poole and <strong>NHS</strong> <strong>Dorset</strong> for the response to<br />
and management of <strong>incident</strong>s and emergencies.<br />
Chief Executive Officer and all organisational Directors<br />
It is the responsibility of staff at all levels to ensure that they<br />
are working to the most up to date and relevant policies and<br />
procedures. By so doing, the quality of services offered will<br />
be maintained and the chances of staff making erroneous<br />
decisions, which may affect patient, staff or visitor safety,<br />
will be reduced.
IMMEDIATE ACTION<br />
If you have received notification that a<br />
Major Incident has been declared,<br />
find your relevant action card and<br />
follow the instructions
This page is intentionally blank
CONTENTS<br />
Page(s):<br />
PART ONE - INTRODUCTION 11<br />
Introduction 13<br />
Definitions 16<br />
Declaration of a <strong>major</strong> <strong>incident</strong> 17<br />
Types of <strong>major</strong> <strong>incident</strong> 18<br />
PART TWO - CONCEPT OF OPERATIONS 23<br />
Trigger and Alerting Arrangements 25<br />
Command and Control Arrangements/PCT command and control 27<br />
Local PCT Alerting Procedures 36<br />
Rest Centre 43<br />
Briefings 43<br />
Post Incident Actions and Debriefing 45<br />
Major Incident Documentation 49<br />
Communications 49<br />
PART THREE - ACTION CARDS 51<br />
PCT INCIDENT ROOM ROLES:<br />
Incident Commander (Gold PCT) 55<br />
Major Incident Room Manager (Silver PCT) 57<br />
Major Incident Room Coordinator 59<br />
Administration (and Telecommunications) Support 1 61<br />
Administration (and Telecommunications) Support 2 63<br />
Loggist 64<br />
Communications and Media Co-ordinator 65<br />
IT Support 67<br />
Resourcing 68<br />
SPRIG Lead 70<br />
Director of Public Health 71<br />
PART FOUR - TEMPLATES 74
Background to forms and reporting templates 76<br />
CHALET Report – Major Incident notification report 78<br />
DH Situation Report (SITREP- Response Phase) 82<br />
Common Recognised Information Picture (CRIP) 87<br />
Major Incident Task Form 99<br />
Incident Log Sheet 100<br />
PART FIVE - MAJOR INCIDENT ROOM SET-UP 101<br />
Canford House 105<br />
Vespasian House 118<br />
PART SIX- APPENDICES 124<br />
Training Pathway 125<br />
Sainsbury’s assistance policy 126<br />
Satellite phone user instructions 129<br />
Example of an <strong>incident</strong> site 130
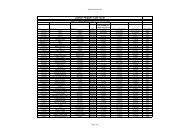
VERSION CONTROL AND REVISIONS<br />
Version<br />
Version<br />
Changed<br />
to<br />
CONSULTATION RECORD<br />
Description of<br />
Change(s)<br />
Reason for<br />
Change<br />
Author/s Date<br />
Name Organisation Date consulted<br />
David Philips <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Suzanne Rastrick <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Paul Vater <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Tim Goodson <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Caroline Dawe <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Contrad Lakeman <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Michaela Dyer <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Jacqueline Cotgrove <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Cindy Shaw-Fletcher <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Sally Sandcraft <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Jane Pike <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Charles Summers <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Frances Stevens <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
John Morton <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Nikki Osborne <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Fiona Richardson <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Sarah Walker <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 8 th March 2012<br />
Emily Youngman <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 7 th March 2012<br />
Stuart Brown <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole 7 th March 2012<br />
Kate Mears <strong>NHS</strong> South West 8 th March 2012<br />
Libby Beesley DHUFT 8 th March 2012
DORSET, BOURNEMOUTH AND POOLE CLUSTER MAJOR INCIDENT PLAN<br />
Authorisation and Declaration<br />
I, Suzanne Rastrick, Acting Chief Executive of the <strong>Dorset</strong>, Bournemouth and Poole Cluster<br />
(incorporating <strong>Dorset</strong>, Bournemouth and Poole Primary Care Trusts), endorse the contents<br />
of this Major Incident Plan and commend it to all staff.<br />
The original signed document is held on file.<br />
Signed Date: 11 th April 2012
Chief Executive Endorsement<br />
The <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth and Poole Cluster consisting of <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth<br />
and Poole Primary Care Trusts (PCTs) has a duty to protect and promote the health of the<br />
community, this including during a Major Incident or an Emergency. We have a central role<br />
in <strong>plan</strong>ning for and responding to any <strong>incident</strong> which has <strong>major</strong> consequences for health or<br />
health services; in partnership with other parts of the <strong>NHS</strong>: the strategic health authority,<br />
our provider organisations, the emergency services and local authorities. The Cluster works<br />
closely with <strong>NHS</strong> South Emergency Planning and with other Trusts within this area, in<br />
<strong>plan</strong>ning for and managing all types of Major Incident or Emergency.<br />
Although PCTs are currently in a period of transition, and Clinical Commissioning Groups<br />
are being established, the PCTs within the Cluster remain ‘legal entities’ with the<br />
responsibility for drafting, maintaining and exercising a Major Incident Plan (MIP).<br />
Additionally, in view of the separation of the Commissioning and Providing functions it is<br />
vital that all members of staff understand the MIP, their role and the resources that can be<br />
provided from within the Cluster and those that must be sought from elsewhere.<br />
It is therefore worth emphasising that every member of staff of the Cluster plays a vital role<br />
in ensuring a professional <strong>NHS</strong> response to crises. As such, it is essential that we are all<br />
familiar with the Cluster operating procedures during such an event, what role each of us<br />
may play and what other organisations that we may be working with will be able to provide.<br />
It is important that we consider the wide range of events which we may be called upon to<br />
deal with including; transport <strong>incident</strong>s, terrorism, outbreaks of disease and internal<br />
<strong>incident</strong>s; such as a hospital evacuation, serious health scare or service continuity failure.<br />
A Major Incident or Emergency, by its nature is a stressful and uncertain situation. As such<br />
it is vital that you feel supported with effective emergency management. The response<br />
teams will work with staff to co-ordinate a Trust response. There may be a need for staff to<br />
work in unfamiliar environments and for extended periods, and we rely on your co-operation<br />
and support in order to manage a crisis effectively.<br />
This <strong>plan</strong> sets out the framework for our response. It has been developed in association<br />
with <strong>NHS</strong> South, the providers, the Health Protection Agency (HPA), and the local<br />
authorities. It is reviewed annually and we will be updating and training on its contents<br />
throughout the year in order to support our response to any emergency and to ensure that<br />
we are prepared for the Olympic event period.<br />
A Major Incident or Emergency can occur at any time of the day or night. It is vital that we<br />
are prepared and can respond at short notice, providing a coordinated range of emergency,<br />
midterm and long term services. As such, emergency <strong>plan</strong>ning is considered a priority<br />
within the trust and I commend this <strong>plan</strong> to you.<br />
Suzanne Rastrick<br />
Acting Chief Executive<br />
<strong>NHS</strong> <strong>Dorset</strong>, Bournemouth and Poole Cluster
This page is intentionally blank
PART ONE<br />
Introduction<br />
This section provides a<br />
background to the Major Incident<br />
Plan, the generic response and<br />
details of underpinning <strong>plan</strong>s and<br />
processes.
This page is intentionally blank
1. INTRODUCTION<br />
Background<br />
1.1 This Major Incident Plan details the arrangements for the <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth<br />
and Poole cluster to respond to, and manage, <strong>incident</strong>s and emergencies.<br />
Aim<br />
1.2 This <strong>plan</strong> has been developed to provide the following guidance:<br />
• Cascade and alerting arrangements;<br />
• Detail the arrangements for activating the Major Incident Room;<br />
• Set out specific roles and responsibilities of staff in Action Cards;<br />
• Set out the primary functions of the Major Incident Room;<br />
• Outline the command and control arrangements for managing <strong>incident</strong>s;<br />
• Set out a basis for <strong>major</strong> <strong>incident</strong> training.<br />
Supporting Plans and Processes<br />
1.3 This <strong>plan</strong> is underpinned by the arrangements outlined within the Bournemouth,<br />
<strong>Dorset</strong> and Poole Local Resilience Forum’s Initial Responders Major Incident<br />
Manual, and other specific response <strong>plan</strong>s.<br />
1.4 For the purposes of this document the On-Call Duty Manager is the On-call PCT<br />
Manager, who will act as the <strong>NHS</strong> Gold Officer during an <strong>incident</strong>, until relieved by<br />
an appropriate Director. The PCT Silver Incident Manager is a manager who will be a<br />
non-rostered manager from the On-Call Duty Manager roster (activated, if available<br />
via SMS alerting or a telephone call) – this is a best endeavours response. The <strong>NHS</strong><br />
Gold Officer and PCT Silver Incident Manager roles may need to be merged during<br />
the initial stages of the <strong>incident</strong>.<br />
1.5 The <strong>NHS</strong> and Social Care Act 2008 (Regulated Activities) Regulations 2010 is<br />
regulated by the Care Quality Commission and lists actions that are relevant to<br />
emergency <strong>plan</strong>ning and are therefore taken into account by the PCT cluster.<br />
1.6 The Civil Contingencies Act 2004 (CCA) defines an Emergency (known with the <strong>NHS</strong><br />
as a Major Incident) as an event or situation (within the United Kingdom), which<br />
INTRODUCTION Page 13
threatens serious damage to human welfare, which threatens serious damage to the<br />
environment, or war or terrorism which threatens serious damage to security.<br />
1.7 The Act places a number of legal requirements on healthcare organisations with<br />
effect from 15th November 2005. Additionally the DH published the <strong>NHS</strong> Emergency<br />
Planning Guidance in 2005.<br />
1.8 Each of the above place obligations and requirements on PCTs; these are<br />
summarised as follows. Under Schedule 1 of the Act PCTs were designated as a<br />
Category One Responders and are thus required to:<br />
• Have developed generic emergency <strong>plan</strong>s (Emergency Preparedness – chapter<br />
5 (Emergency Planning) & DH guidelines (sec 4.6))<br />
• Have developed resilient business contingency <strong>plan</strong> (Emergency Preparedness -<br />
chapter 6 (Business Continuity Management) & DH Guidelines (sec 4.7)<br />
• Contribute to the community risk register (Emergency Preparedness – chapter 4<br />
– Local Responder – Risk Assessment Duty & DH Guidelines (section 4.5))<br />
• Information Sharing (Emergency Preparedness – chapter 3 - Information Sharing<br />
& Chapter 7 – Communicating with the Public (Warning & Informing) & DH<br />
Guidelines Section 4.4))<br />
• Co-ordinate a local response to a <strong>major</strong> <strong>incident</strong> (DH Guidelines, underpinning<br />
materials; PCTs)<br />
• Demonstrate high level of preparedness of Primary Care and Community<br />
services and ensure that they can respond at any time. (underpinning materials:<br />
PCTs)<br />
• Ensure that the PCTs own staff, GPs, Primary care and Community Care staff<br />
are appropriately trained and competent to <strong>plan</strong> for and to respond to a Major<br />
Incident.<br />
1.9 The Bournemouth, <strong>Dorset</strong> and Poole Local Resilience Forum (LRF) Community Risk<br />
Register (CRR) provides an agreed position of the risks affecting the local area. The<br />
LRF is responsible for maintaining the CRR, and Category One organisations are<br />
required under the CCA to participate in its preparation and maintenance. The CRR<br />
provides essential information as to the risks within a local area, the organisations<br />
best able to manage these risks and help Category One organisations to identify the<br />
<strong>plan</strong>s that it needs to develop.<br />
1.10 The Major Incident Plan, emergency <strong>plan</strong>s and on call protocol cards are validated<br />
through training, tests and exercises, and should include:<br />
• Familiarisation of staff with this <strong>plan</strong> – particularly new staff, Directors and Senior<br />
Managers who have responsibility for the PCTs response<br />
• Participation in a live exercise every 3 years. (DH guidelines (sec5.10) Learning<br />
from exercises and <strong>incident</strong>s should also be incorporated.<br />
• Testing communications every 6 months (DH guidelines (sec 5.10))<br />
• Undertaking desk top testing of <strong>plan</strong>s annually (DH Guidelines (sec 5.10)<br />
• No notice exercises known as “Exercise Alacrity” that will be conducted every 3<br />
months<br />
INTRODUCTION Page 14
1.11 The PCT Cluster Training Pathway can be found in the appendices, and lists the<br />
recommended training for all staff involved in the response to an <strong>incident</strong>. The Trust<br />
is committed to annual refresher training for all key response staff and the annual<br />
training schedule for staff. We are committed to involving other organisations in<br />
these exercises at a local and corporate level.<br />
1.12 The Trust Management Team will act in a governance role agreeing the release of<br />
controlled updates to the <strong>plan</strong> as needed except in the case of amendments to the<br />
contact information, which will be regularly maintained to ensure accuracy.<br />
Emergency Planning will be a standing agenda item at the Trust Management Team<br />
meeting once a quarter, during which the Director of Public Health will provide<br />
updates to Directors and the Chief Executive as needed, for onward transmission to<br />
the Board as needed.<br />
INTRODUCTION Page 15
2. DEFINITION OF MAJOR INCIDENT<br />
2.1 A <strong>major</strong> <strong>incident</strong> is defined by the <strong>NHS</strong> Emergency Planning Guidance 2005 as:<br />
“A Major Incident is any event whose impact cannot be handled within routine<br />
service arrangements. It requires the implementation of special procedures by<br />
one or more of the emergency services, the <strong>NHS</strong>, or a Local Authority to<br />
respond to it”.<br />
2.2 Under The Civil Contingencies Act 2004, <strong>NHS</strong> <strong>Dorset</strong> is defined as a Category 1<br />
Responder.<br />
2.3 A Category 1 responder is required to respond:<br />
• Where the organisation would consider it necessary or desirable to act to<br />
prevent, reduce, control or mitigate the emergency’s effects, or otherwise take<br />
action, and would be unable to act without changing the deployment of its<br />
resources or acquiring additional resources;<br />
• Where the emergency would be likely to seriously obstruct the organisation’s<br />
ability to perform its functions.<br />
INTRODUCTION Page 16
3. DECLARATION OF A MAJOR INCIDENT<br />
3.1 All Category 1 Responder Organisations have the power to declare a Major Incident.<br />
3.2 All <strong>NHS</strong> <strong>Dorset</strong> Bournemouth & Poole On-Call Duty Managers On-Call are able to<br />
declare a <strong>major</strong> <strong>incident</strong> if the ‘Major Incident’ <strong>NHS</strong> definition is met.<br />
3.3 Declaration should be considered where the effect on any part of the system is<br />
likely to be disproportionately large. It may be necessary when, for instance,<br />
additional special resources such as intensive care beds, operating theatre<br />
resources, or burns facilities will be required, even though the total number of<br />
casualties is limited.<br />
3.4 The <strong>NHS</strong> has standard messages to be used in connection with the declaration of a<br />
<strong>major</strong> <strong>incident</strong>. These are as follows:<br />
<strong>NHS</strong> Standard Messages Application<br />
Major Incident Standby This alerts organisations that a <strong>major</strong><br />
<strong>incident</strong> may need to be declared.<br />
Organisations must consider what<br />
preparatory arrangements they may<br />
need to make appropriate to the<br />
<strong>incident</strong>.<br />
Major Incident Declared Organisations to activate Major Incident<br />
(Activate Plan)<br />
Plans.<br />
Major Incident Cancelled This message cancels either of the<br />
above messages at any time.<br />
Major Incident -<br />
Casualty Evacuation<br />
Complete.<br />
This message is mostly applicable to<br />
receiving hospitals, and is used when all<br />
the casualties have been cleared from<br />
the <strong>incident</strong> site and none are still en<br />
route to hospitals.<br />
Major Incident Stand Down This message ends the <strong>incident</strong>.<br />
However, it is the responsibility of each<br />
organisation to assess when it is<br />
appropriate for them to stand down.<br />
Information to Provide when Declaring a Major Incident<br />
INTRODUCTION Page 17
3.5 The organisation which declares a Major Incident should provide, as appropriate, the<br />
following information:<br />
• Type of <strong>incident</strong>;<br />
• Location of <strong>incident</strong>;<br />
• Time of <strong>incident</strong>;<br />
• Estimated number of casualties;<br />
• Predominant nature of injuries if known; and<br />
• Which hospitals if any have been alerted.<br />
4. TYPES OF MAJOR INCIDENT<br />
4.1 Assess what type of <strong>incident</strong> you are dealing with. Incidents vary but tend to fall into<br />
the following general level of casualties and categories:<br />
<strong>NHS</strong> Level<br />
Nos of<br />
Casualties<br />
Description Local Response <strong>NHS</strong> South<br />
DH Response<br />
Major = 10s Individual Trusts<br />
handle <strong>incident</strong><br />
within<br />
established MIP<br />
Mass =<br />
100s<br />
Catastrophic<br />
= 1000s<br />
Large scale<br />
Possible closure<br />
/evacuation.<br />
Major health<br />
facility or<br />
persistent<br />
disruption over<br />
time<br />
Collective mutual<br />
aid from<br />
neighbours<br />
Incident of such<br />
proportions that it<br />
severely disrupts<br />
health & social<br />
care and other<br />
support functions<br />
Local <strong>NHS</strong> activate<br />
local Command and<br />
Control (C2) -<br />
participate in local<br />
multi-agency<br />
arrangements<br />
Local <strong>NHS</strong> activate<br />
local C2 – participate<br />
in local multi-agency<br />
arrangements<br />
All Trusts link to <strong>NHS</strong><br />
Command<br />
arrangements – <strong>NHS</strong><br />
South coordinates<br />
mutual aid SHA<br />
Local <strong>plan</strong>s activated –<br />
<strong>NHS</strong> South advised<br />
and Trusts link to <strong>NHS</strong><br />
Command<br />
arrangements<br />
SHA coordination and<br />
<strong>NHS</strong> South and DH<br />
(Emergency<br />
Preparedness<br />
Department) informed<br />
<strong>NHS</strong> South activates<br />
C2 to coordinate health<br />
care across region<br />
Consider<br />
implementation of<br />
revised clinical<br />
protocols<br />
DH(EPD) notified and<br />
available to support<br />
<strong>NHS</strong> South<br />
Potential for more than<br />
one SHA region to be<br />
affected and each<br />
activates own Strategic<br />
Command<br />
arrangements<br />
INTRODUCTION Page 18
4.2 Big bang<br />
– Response<br />
exceeds<br />
collective local<br />
capacities<br />
mutual aid<br />
DH explains the definition of a “Big Bang” <strong>incident</strong> as follows:<br />
DH (EPD ) National MI<br />
Coordination Centre<br />
activated – national coord<br />
strategic response<br />
and mobilisation of<br />
mutual aid<br />
‘A health service <strong>major</strong> <strong>incident</strong> is classically triggered by a sudden <strong>major</strong><br />
transport or industrial accident. The ambulance service and receiving hospitals<br />
will be the first health responders. What may not be so obvious at first, however,<br />
are the wider health implications. A <strong>major</strong> <strong>incident</strong> may also build slowly from a<br />
series of smaller <strong>incident</strong>s such as might occur on a fogbound motorway’.<br />
Big Bang Incidents will in most cases cause significant numbers of casualties or<br />
fatalities, and may require evacuations.<br />
In nearly all cases these types of <strong>incident</strong>s will require a multi-agency response.<br />
4.3 Rising Tide Incidents<br />
DH explains a “Rising Tide” <strong>incident</strong> in the following way:<br />
‘The problem creeps up gradually, such as occurs in a developing infectious<br />
disease, epidemic or a winter bed availability crisis. There is no clear starting<br />
point for the <strong>major</strong> <strong>incident</strong> and the point at which an outbreak becomes ‘<strong>major</strong>’<br />
may only be clear in retrospect’.<br />
A clear assessment of the situation is required. It may require a bold judgement to<br />
declare a <strong>major</strong> <strong>incident</strong>, but it is better to trigger a formal response and later have to<br />
stand it down than to delay and be behind the curve.<br />
4.4 Cloud on the Horizon Incidents<br />
DH explains a “Cloud on the Horizon” <strong>incident</strong> in the following way:<br />
‘An <strong>incident</strong> in one place may affect others following the <strong>incident</strong>. Preparatory<br />
action is needed in response to an evolving threat elsewhere, even perhaps<br />
overseas, such as a <strong>major</strong> chemical or nuclear release, a dangerous epidemic or<br />
an armed conflict involving British troops. A chemical or radiation <strong>incident</strong> may<br />
INTRODUCTION Page 19
literally cause a cloud on the horizon. In a similar way, but on a longer time scale<br />
the progress of a ’flu epidemic can be observed and predicted’.<br />
4.5 Headline News<br />
Headline News <strong>incident</strong>s may be highly local, and remain so, or have the potential to<br />
develop into regional or national interest stories.<br />
Alternately they may start as national or regional stories but develop to have a local<br />
impact.<br />
In any event it is essential that the Communications Director or Team are given an<br />
immediate briefing to enable them to make a judgement regarding the best course of<br />
action.<br />
4.6 Internal Incidents<br />
Internal <strong>incident</strong>s can often be resolved through Business Continuity arrangements,<br />
however, establishing a control room can often assist in achieving a coordinated<br />
response. Managers should not hesitate to establish a Major Incident Room if<br />
appropriate.<br />
4.7 Deliberate or Terrorist Incidents<br />
Terrorist-related <strong>incident</strong>s require a specialist response from trained and properly<br />
equipped staff.<br />
Assessing the health and safety of staff is respect of all proposed actions is<br />
essential.<br />
All Chemical, Biological, Radiological and Nuclear (CBRN) <strong>incident</strong>s, whether<br />
terrorist-related or not, require a specialist response from staff who are<br />
appropriately trained and equipped.<br />
4.8 Mass Casualties<br />
A Mass Casualty <strong>incident</strong> is one that involves numbers of casualties that exceed the<br />
capacity afforded by normal <strong>major</strong> <strong>incident</strong> arrangements. Normally this will require a<br />
regional level response.<br />
The numbers that trigger a regional level response are deliberately not defined and<br />
will depend on a range of factors, including the nature and severity of the injuries<br />
sustained and current local hospital bed capacity, so a flexible approach needs to be<br />
taken.<br />
INTRODUCTION Page 20
4.9 Mass Fatalities<br />
A Mass Fatality <strong>incident</strong> is one that involves numbers of deaths that exceed the<br />
capacity afforded by normal <strong>major</strong> <strong>incident</strong> arrangements. This will invariably need a<br />
multi–agency response and require the triggering of the Local Resilience Forum<br />
Mass Fatality Plan.<br />
Each <strong>incident</strong> will be judged on the circumstances at the time.<br />
Considerations which determine whether to declare a Mass Fatalities emergency<br />
include:<br />
• The number of deceased<br />
• Fragmentation of bodies<br />
• Is the <strong>incident</strong> which resulted in the deaths a terrorist or other criminal act<br />
• Current mortuary capacity<br />
• Are there other similar <strong>incident</strong>s elsewhere in the Region or United Kingdom<br />
• Are the deceased contaminated in any way<br />
• Is there a requirement for a forensic post-mortem<br />
The decision to declare a Mass Fatalities emergency will be made by the appropriate<br />
HM Coroner in conjunction with the Chair of the Strategic Coordinating Group (SCG)<br />
for the LRF.<br />
Once declared the Mass Fatalities Coordination group will form and sit as a sub<br />
group of the SCG.<br />
INTRODUCTION Page 21
This page is intentionally blank<br />
INTRODUCTION Page 22
PART TWO<br />
Major Incident<br />
Concept of Operations<br />
This section provides an<br />
overview on the concept of<br />
operations for responding to a<br />
<strong>major</strong> <strong>incident</strong> in the<br />
Bournemouth, <strong>Dorset</strong> and Poole<br />
Local Resilience Forum.<br />
CONCEPT OF OPERATIONS Page 23
This page is intentionally blank<br />
CONCEPT OF OPERATIONS Page 24
1. TRIGGER AND ALERTING ARRANGEMENTS<br />
Local Major Incident notification when declared by any of the “blue light”<br />
services<br />
1.1 South Western Ambulance Service (SWAST) is the primary route through which any<br />
of the <strong>Dorset</strong> emergency services declares a multi-agency <strong>major</strong> <strong>incident</strong> to Health<br />
organisations (See Figure One).<br />
1.2 As part of established <strong>major</strong> <strong>incident</strong> response arrangements for the <strong>NHS</strong>, South<br />
Western Ambulance Service (SWAST) will notify the immediate receiving hospitals,<br />
<strong>NHS</strong> <strong>Dorset</strong>, Bournemouth & Poole, and the Health Protection Agency of the<br />
<strong>incident</strong>. This may be a “Major Incident Standby” alert or the declaration of a <strong>major</strong><br />
<strong>incident</strong>.<br />
1.3 SWAST’s Incident Commander at the scene of the <strong>incident</strong> will submit a CHALET<br />
report to the SWAST Control Room. This report will then be cascaded to appropriate<br />
<strong>NHS</strong> organisations in <strong>Dorset</strong>.<br />
CONCEPT OF OPERATIONS Page 25
Figure One: Major Incident Thresholds and Cascades<br />
CONCEPT OF OPERATIONS Page 26
2. COMMAND AND CONTROL ARRANGEMENTS/PCT COMMAND AND CONTROL<br />
Initial Arrangements<br />
2.1 The initial stages of most <strong>incident</strong>s, the <strong>incident</strong> cascade will be implemented by<br />
SWAST, based upon their on-scene assessment. In accordance to this initial<br />
assessment, they will call relevant organisations and either declare a <strong>major</strong> <strong>incident</strong><br />
or a <strong>major</strong> <strong>incident</strong> standby as appropriate.<br />
Tactical Coordinating Group – TCG (Silver)<br />
2.2 If a multi-agency response is required, the initial cascade will be followed by details<br />
of where multi-agency Silver is to be established. This will usually be at Winfrith<br />
Police HQ, but may be elsewhere if the situation dictates.<br />
2.3 This Group will be required to make key decisions on the <strong>incident</strong> response. The<br />
Ambulance Service, working where appropriate with the PCT Silver Incident<br />
Manager will coordinate the health response. It may be more appropriate for the PCT<br />
Silver Incident Manager to coordinate the health response from the PCT Major<br />
Incident Room (MIR) at Vespasian House, Dorchester or Canford House,<br />
Bournemouth.<br />
2.4 Key tasks are command and coordination of resources and communications,<br />
Situation Reporting SITREPs and preparing briefings for Gold (if instigated).<br />
Strategic Coordinating Group (Gold)<br />
2.5 If required, a multi-agency Strategic Coordinating Group will be established, and<br />
receive reports from the Tactical Coordinating Group regarding <strong>incident</strong> response<br />
issues and support required. The Ambulance Service will provide reports on casualty<br />
numbers.<br />
2.6 The Strategic Coordinating Group is the strategic decision making body, and as such<br />
requires appropriate Director level attendance. SWAST have their own<br />
representative, but the PCT On-Call Duty Manager represents all other health<br />
resources in <strong>Dorset</strong>. It may also be necessary for the On-Call Duty Manager to<br />
consider instigating a PCT Gold Team to manage business continuity issues.<br />
2.7 For <strong>incident</strong>s with regional impact, representatives from the Strategic Health<br />
Authority, will send appropriate representatives to attend as liaison officers as<br />
necessary.<br />
2.8 An illustration of the command and control structure throughout the <strong>incident</strong> lifetime<br />
is detailed at Figure Two.<br />
CONCEPT OF OPERATIONS Page 27
Figure Two: Command and Control Structure Illustration<br />
CONCEPT OF OPERATIONS Page 28
2.9 Key role and responsibilities of the Gold Group include:<br />
Director / Chief Executive<br />
The Director / Chief Executive will set the strategic objectives and longer-term tasks<br />
for the Team and will provide a co-ordinating function for the Team and the PCT.<br />
Their roles include:<br />
• Regularly review the strategic objectives of the PCT cluster<br />
• Convening regular meetings to review progress. (The meetings must follow an<br />
agenda, be minuted (including persons present), actions and decisions noted<br />
and minutes circulated)<br />
• The provision of the co-ordinating function for the team and the PCT response<br />
• Instigation of the Business Continuity Team and subsequent arrangements<br />
• Agreeing additional financial commitment as needed by either the PCT cluster or<br />
the provider<br />
• Responsibility for the welfare of the team, resources and resilience in terms of<br />
continuing operations over extended periods<br />
• Be the public face of the PCT cluster when responding to media requests<br />
• To support the PCT Gold Officer as required<br />
Director of Public Health<br />
The PCT Director of Public Health will ensure:<br />
• Adequate health protection measures are implemented to protect the public<br />
• Immediate actions are taken to minimise risk to the community e.g. mass<br />
counter-measures<br />
• Health organisations are notified of appropriate action<br />
• Liaise with the HPA as needed<br />
• That liaison with the Local Authority takes places regarding to public health<br />
emergencies<br />
• That they (or deputy) can chair the Scientific and Technical Advice Cell (STAC)<br />
as needed<br />
Director of Finance<br />
The PCT Director of Finance will ensure:<br />
• That the Gold Officer is being given the appropriate guidance with regard to<br />
financial commitments and support during substantial or long term finance<br />
resource allocation<br />
Representation from the community provider<br />
If required and appropriate, the Gold Officer may request the attendance of the<br />
community provider service or GP lead or other provider who will support the PCT<br />
CONCEPT OF OPERATIONS Page 29
cluster management team with ensuring and agreeing that the appropriate and<br />
measured response to the <strong>incident</strong> is being managed. This may include the<br />
appropriate allocation and deployment of funds, staff or resources. They will readily<br />
provide updated allocated resource or other information or patient information in<br />
order for the PCT cluster to report to <strong>NHS</strong> South.<br />
Major Incident Response Teams - Gold Team arrangements<br />
2.10 The PCT Cluster Major Incident Gold Team will include the following staff or roles:<br />
• On-Call Duty Manager<br />
• Chief Executive (when needed)<br />
• Director of Public Health or deputy<br />
• Loggist(s)<br />
• Telecommunications and Administrative support Officer(s) (when needed)<br />
• Senior representation from our providers for co-ordination/liaison purposes<br />
should also be considered<br />
• Supported by the Emergency Planning Officer (when needed)<br />
• Supported by the Director of Finance (when needed)<br />
• Supported by the Communications and Media Co-ordinator (when needed)<br />
• Supported by the Estates Department representative (when needed)<br />
2.11 It is important that there is appropriate level membership for the authorisation of<br />
funds and resources and for determining the resources that are available and those<br />
that are likely to be needed. The following staff and resources can be provided<br />
directly from within the PCT cluster or may be requested from our community<br />
providers as part of a joint response to an <strong>incident</strong>, this will be agreed at strategic<br />
level between the organisations:<br />
PCT Cluster<br />
• General Practitioners<br />
• Out of hours GP service<br />
• Dentist<br />
• Optometry<br />
• Pharmacy<br />
• Communications<br />
• Human Resources (via DHUFT<br />
support service)<br />
• Voluntary Sector (via Local<br />
Authority)<br />
• Chairmanship of Scientific and<br />
Technical Advice Cell (STAC)usually<br />
the DPH<br />
Community Providers<br />
• District Nurses<br />
• Health Visitors<br />
• Specialist Nurses (Children’s Nursing<br />
Team)<br />
• Other community health staff may be<br />
redeployed to assist (e.g.: Podiatrists,<br />
Physiotherapists, Dental Nurses)<br />
• Managers (those with clinical<br />
backgrounds may be redeployed to<br />
assist)<br />
• Supplies and Equipment that may be<br />
relevant to the <strong>incident</strong><br />
• Buildings<br />
• Estates/Facilities<br />
• Vehicles, supplies and equipment<br />
CONCEPT OF OPERATIONS Page 30
elevant to the <strong>incident</strong><br />
• IT<br />
2.12 Any or all of the above resources are likely to be required at different response<br />
and/or recovery stages of an <strong>incident</strong>. There is a need to ensure a <strong>plan</strong>ned and<br />
systematic way of putting in to action the Emergency Plans, particularly with regard<br />
to contacting the providers both in and out of hours. This will require the PCT cluster<br />
to ensure that there are effective and reliable mechanisms in place to alert and<br />
mobilise its own key staff members, to assess the impact and manage the response<br />
to any <strong>incident</strong> and alert the community provider as early as practical if it is believed<br />
that provider resources may be required.<br />
2.13 The terms of reference of the PCT Gold Officer and/or Team are:<br />
• To make an initial assessment of the situation and determine an organisational<br />
intention/aim relevant objectives<br />
• To determine the key organisations with which to establish communications with<br />
• To instigate the mass casualty <strong>plan</strong>, by declaring and mobilising the additional<br />
resources as needed until such time this task can be handed to the Silver<br />
Incident Manager or the Major Incident Room<br />
• To continually assess the potential impact of the <strong>incident</strong> on acute services,<br />
public health, primary care, community care, mental health and <strong>NHS</strong> services<br />
• To activate appropriate specific <strong>plan</strong>s held by the PCT<br />
• To identify key PCT sites that are equipped to deliver an appropriate Primary<br />
Care response, if required<br />
• To make arrangements for access and safe staffing of responding service sites<br />
• To assess the internal resources required to deal with the <strong>incident</strong> and to ensure<br />
that arrangements are put in place to respond appropriately<br />
• Consider mutual aid requirements from adjoining PCT areas for support with<br />
community services or PCT infrastructure, Local Authorities/SWAST for additional<br />
support including that of the voluntary sector and SWAST for private<br />
ambulance/medical services<br />
• To assess the ability of local health services to deal with the <strong>incident</strong> and<br />
estimate the extra resources required where the assessment indicates<br />
inadequacies<br />
• To seek expert advice where the expertise does not exist within the PCT<br />
• To ensure there is an effective communications strategy that is consistent with<br />
any national message and can deliver information and advice to staff, partners,<br />
stakeholders and the wider media (through <strong>NHS</strong> South as appropriate)<br />
• To liaise with <strong>NHS</strong> South and implement their advice<br />
• To support other PCT and <strong>NHS</strong> organisations<br />
• To decide when the <strong>incident</strong> should be declared over and inform the appropriate<br />
organisations that this has been done<br />
• To <strong>plan</strong> for the recovery and return to normality as needed dependent on the<br />
level of internal disruption and consider the activation of use of business<br />
continuity <strong>plan</strong>s as needed<br />
PCT Gold Team Meetings Agenda<br />
CONCEPT OF OPERATIONS Page 31
- To confirm the strategic intention<br />
- Information/Intelligence:<br />
• Update from Strategic Coordination Centre<br />
• Update from <strong>incident</strong>(s) site(s) /situation report<br />
• Update from receiving hospitals and provider<br />
• Update from Major Incident Control Room<br />
• Review resource availability including mutual aid requirements<br />
- Major Incident requirement review<br />
- Operational Support:<br />
• Logistics<br />
• Feeding arrangements<br />
- Review Technical Communications/IT<br />
- Media<br />
- Review Strategic Intent<br />
- Strategic Direction<br />
- Recovery <strong>plan</strong>ning after <strong>incident</strong> and any Business continuity issues<br />
- AOB<br />
- Next Meeting<br />
Key Cluster PCT Arrangements<br />
2.14 <strong>NHS</strong> <strong>Dorset</strong>, Bournemouth and Poole Primary Care Trust cluster response to <strong>major</strong><br />
<strong>incident</strong>s is based on the following key arrangements:<br />
• On-Call staff: A 24/7 On-Call rota, staffed by nominated PCT managers<br />
providing a single point of contact for the Trust and Local Resilience Forum<br />
organisations. The PCT On-Call Duty Manager represents and is the guardian<br />
to all <strong>NHS</strong> assets.<br />
• Public Health Advice: The formation of a Scientific and Technical Advice<br />
Cell (STAC), in co-operation with Health Protection Units, to safeguard public<br />
health.<br />
CONCEPT OF OPERATIONS Page 32
• Major Incident Management Team (MIMT) and PCT Gold Team: It may be<br />
necessary to set up a Major Incident Room using the Major Incident<br />
Management Team. The staffing for this team is outlined in specific action<br />
cards for key roles, and below. The PCT Gold Team may be necessary to<br />
manage internal <strong>incident</strong>s.<br />
• Major Incident Room: The current default designated Major Incident Rooms<br />
for the cluster, if required to accommodate a Major Incident Management<br />
Team, will be:<br />
- <strong>NHS</strong> <strong>Dorset</strong> PCT located at Vespasian House, Bridport Road,<br />
Dorchester, <strong>Dorset</strong>, DT1 1TS on the 3 rd floor East in the Public Health<br />
Department or;<br />
- <strong>NHS</strong> Bournemouth and Poole PCT located at Canford House,<br />
Discovery Court, 551 – 553 Wallisdown Road, Poole, <strong>Dorset</strong>, BH12<br />
5AG in Meeting Room One.<br />
All relevant <strong>plan</strong>s and documentation are kept within each Major Incident<br />
Room store.<br />
• Emergency Contact Directory: In and Out of Hours contact telephone<br />
numbers for all key staff are held in the Emergency Contacts Directory.<br />
• Remote Access to the Major Incident email account: In the event of a<br />
Major Incident, the On-Call staff will be able to access the Major Incident<br />
email account remotely, if required.<br />
• Bournemouth and Poole PCT webmail multi-user control room email<br />
• Web address: https://webmail.dshc.nhs.uk<br />
• Email address: <strong>major</strong>.<strong>incident</strong>@bp-pct.nhs.uk<br />
• Username: <strong>major</strong>.<strong>incident</strong>.<br />
• Password: Pa55word<br />
• <strong>Dorset</strong> PCT webmail multi-user control room email<br />
• Web address: https://webmail.dshc.nhs.uk<br />
• Email address: nhsdorset.control@dorset-pct.nhs.uk<br />
• Username: nhsdorset.control<br />
• Password: Pa55word<br />
Major Incident Response Teams - MIMT arrangements<br />
2.15 The PCT cluster Major Incident Management Team working in the Major Incident<br />
Room will include the following staff or roles:<br />
• Major Incident Room Manager (PCT Silver Incident Manager); usually<br />
performed by the On-Call Duty Manager unless they are required at Police HQ,<br />
in a multi agency Silver room at which point the responsibility will be included in<br />
the Major Incident Room Co-ordinator list of tasks<br />
CONCEPT OF OPERATIONS Page 33
• Major Incident Room Co-ordinator<br />
• Resourcing/HR<br />
• Administrative and Telecommunications Support Officer(s)<br />
• Communications and Media Coordinator<br />
• IT support<br />
• Supported by representation from the community provider (when needed)<br />
• Supported by a SPRIG Lead (when needed, and if the <strong>incident</strong> is a public<br />
health emergency)<br />
• Supported by a Public Health lead representing the Director of Public Health<br />
(when needed)<br />
• Supported by the Primary Care Coordinator (when needed)<br />
• Supported by the on call pharmacist (when needed)<br />
2.16 Roles and Responsibilities of the MIMT<br />
Listed below is an overview of the key roles and responsibilities of the MIMT:<br />
Duty Manager On-Call<br />
After the initial on call actions the On-Call Duty Manager will then be responsible for<br />
either acting as the “Major Incident Room Manager” or responding to Police HQ as<br />
the <strong>NHS</strong> Silver Incident Manager as part of the Tactical Coordination Group (TCG).<br />
They will be responsible for the tactical management of the <strong>incident</strong>, management of<br />
the Major Incident Room, collation of all records relating to the <strong>incident</strong> and submit a<br />
post-<strong>incident</strong> report to the Director of Public Health at the conclusion of the Incident<br />
or such interim report(s) as may be required for onward submission to the Chief<br />
Executive, <strong>NHS</strong> South and the Health Protection Agency.<br />
Communications and Media Co-ordinator<br />
The post-holder will ensure there is an effective communications strategy that is<br />
consistent with any national and local LRF message and can deliver information and<br />
advice to staff, partners, stakeholders and the wider media (through <strong>NHS</strong> South as<br />
appropriate) and to establish effective media liaison in order to deliver a coherent<br />
message to the public – consistent with local events and in keeping with a national<br />
message. They will have responsibility to ensure that they have a <strong>plan</strong> in place to<br />
manage any incoming press and media calls so that no impact is made on the Major<br />
Incident Room.<br />
Resourcing<br />
The post-holder will actively resource the required staff or volunteers to respond to<br />
the <strong>incident</strong> over a mid to long term period ensuring appropriate resilience. This will<br />
include the PCT or primary PCT assets responding to the <strong>incident</strong> site (e.g. GPs,<br />
etc.), the MIMT staff and Gold Team staff. They will be responsible for making<br />
arrangements for temporary PCT staff accommodation as needed.<br />
CONCEPT OF OPERATIONS Page 34
Telecommunications and Administration Support Officer<br />
Generally two post-holders will support the work of the response teams by<br />
maintaining accurate record keeping procedures, including providing telephony and<br />
communication support in the Major Incident control room, ensuring that information<br />
is appropriate recorded, resources allocated to work and that tasks are actioned in a<br />
timely fashion using the task system. They will ensure that all actions are recorded<br />
and documented appropriately on the <strong>incident</strong> log forms and task allocation sheets.<br />
Loggist<br />
The post-holder will ensure there is an accurate log of the actions taken by the Gold<br />
and ensure that all actions are recorded and documented appropriately in the<br />
Emergency Log Book and Decision Log Book. Additionally they will provide<br />
administrative support to the PCT Gold. The Loggist positioned at the Major Incident<br />
Room will use the Decision Log Book to record decisions being made by the Silver<br />
Incident Manager.<br />
IT support<br />
They will support the response teams with the appropriate IT infrastructure as<br />
needed, dealing with problems with computers, printers and communications<br />
equipment as they present themselves. Liaise with IT department to ensure that<br />
problems as dealt with swiftly contact: From 17:30 to 08:30 and 17:00 Friday til 08:30<br />
Monday the number is 01305361499 or normal times is 01305361223.<br />
Emergency Planning Manager<br />
The Emergency Planning Manager will provide support and advice to the response<br />
teams as necessary by liaising with emergency <strong>plan</strong>ning officers in other agencies in<br />
order to ensure a multi-borough coordinated response to a <strong>major</strong> <strong>incident</strong>. They will<br />
act as, or deputise for the Silver Incident Manager as needed.<br />
CONCEPT OF OPERATIONS Page 35
3. LOCAL PCT ALERTING PROCEDURES<br />
3.1 STEP ONE: The single point of contact for notifying the Trust of a <strong>major</strong> <strong>incident</strong> will be<br />
the On-Call Duty Manager. This will apply for office hours and out-of-hours. From the<br />
time the alert is received, the On-Call Duty Manager will be in command of the Trust<br />
response until relieved of that responsibility.<br />
3.2 In most <strong>incident</strong>s, the alert will come from the Ambulance Trust control room as they<br />
are usually the first health responding organisation at the scene of the <strong>incident</strong>.<br />
3.3 STEP TWO: It is important to gather as much information as possible when alerted, in<br />
particular, all of the elements of the Major Incident Notification form (See Templates).<br />
‘CHALETS’ is an accepted mnemonic for initial situation reports about the <strong>incident</strong>.<br />
3.4 The following information should be recorded:<br />
• The time the alert call was received<br />
• Organisation the alert call was received from<br />
• Name of the caller<br />
• Telephone number of the caller<br />
• As much of the CHALETS report as possible, as follows:<br />
Mnemonic<br />
Casualties:<br />
Hazards:<br />
Access:<br />
Location:<br />
Emergency:<br />
Type:<br />
Start:<br />
Information Needed<br />
Numbers of fatalities and injured<br />
Actual or potential hazards at the scene, any concerns about<br />
contamination, toxic smoke. Any evacuation, if so, where to<br />
Rendezvous point and any restrictions on access to the scene<br />
As precise a location for the <strong>incident</strong> as possible<br />
Services, Which ones are present. Who is in command, contact number<br />
Nature of the <strong>incident</strong>, for example, <strong>major</strong> fire, building collapse,<br />
flooding<br />
A log of your decisions<br />
CONCEPT OF OPERATIONS Page 36
.<br />
3.5 STEP THREE: Depending on the type of <strong>incident</strong>, a response may be required in<br />
varying phases. In the initial stages of an <strong>incident</strong>, the call will be received by the On-<br />
Call Duty Manager of the PCT cluster. Assembly of the response teams will be<br />
determined at this point with the support of the Emergency Planning Manager and<br />
information on the appropriate action card. The On-Call Duty Manager or others may<br />
be advised of external <strong>incident</strong>s or lesser internal <strong>incident</strong>s; however, generally no<br />
team will be required in either of these scenarios. The On-Call Duty Manager is to<br />
determine the response of the PCT using the information at Figure 3 to assist in his or<br />
her decision:<br />
CONCEPT OF OPERATIONS Page 37
Figure Three: Local PCT Response Assessment<br />
NO ACTION<br />
REQUIRED<br />
Complete Emergency Call<br />
form and send it to the<br />
Emergency Planning Manager<br />
for their records. If you are not<br />
sure if you should have taken<br />
any action, review the Major<br />
Incident Plan or on call<br />
protocol cards for further<br />
advice or contact the initial<br />
caller for more information<br />
about the <strong>incident</strong>.<br />
COMPLETE MAJOR INCIDENT<br />
NOTIFICATION FORM<br />
(On-Call Duty Manager)<br />
Verify information if necessary<br />
Assess the PCT cluster Response:<br />
Is there a reception centre set up?<br />
Are there road closures effecting health assets?<br />
Are there any public health risks?<br />
Do you need to send information to GPs?<br />
Are any PCT staff affected?<br />
Are any healthcare facilities affected?<br />
Does the hospital need assistance?<br />
Are there any business continuity issues?<br />
Does the Local Authority need help?<br />
Is the media involved?<br />
Is the <strong>incident</strong> room operational?<br />
Do you need to declare a Major/Mass Incident?<br />
MINOR INCIDENT<br />
OR EMERGENCY<br />
(able to respond using<br />
normal resources)<br />
Check if there are any healthcare<br />
facilities or staff affected in the<br />
area of the <strong>incident</strong>. If there are<br />
public health implications, contact<br />
Public Health (or the Health<br />
Protection Unit). Check with the<br />
Local Authority if there has been<br />
an evacuation and also with the<br />
local Acute Trusts if you think they<br />
may have been affected.<br />
MAJOR<br />
INCIDENT<br />
Major <strong>incident</strong> declared.<br />
You are now the PCT Gold Officer.<br />
Refer to action cards.<br />
Do you need to form a Major<br />
Incident Management Team (MIMT)?<br />
– If yes SMS alert them!<br />
If a mass casualty <strong>incident</strong> check<br />
out that <strong>plan</strong> now<br />
CONCEPT OF OPERATIONS Page 38
3.6 The response team(s) are required to be assembled in the event of an <strong>incident</strong> that<br />
affects or results in the following: Business Continuity of the PCT cluster, declaration<br />
of a Major Incident, a significant external event that affects the health of the<br />
community and requires health coordination.<br />
3.7 STEP FOUR: MIMT activation:<br />
The PCT cluster On-Call Duty Manager (acting in the Gold Officer role) is reliant on<br />
the availability of PCT staff to respond. During working hours this may be referred to<br />
an appropriate Director/line manager who will instruct the required staff to attend as<br />
needed. Out of hours response if reliant on staff volunteering to respond to the<br />
<strong>incident</strong> – activation will generally be via SMS text or phone calls to staff that have<br />
already offered their time for emergency call outs - their details are held on the SMS<br />
activation system<br />
3.8 The On-Call Duty Manager will be required to decide at this point whether they<br />
attend the Major Incident Room in lieu of additional PCT staff; in order to set<br />
up the control room, manage the <strong>incident</strong> and call out staff or attend Police HQ<br />
in the Strategic Coordination Group (SCG).<br />
3.9 On receipt of a serious <strong>incident</strong> or a Major Incident, where pagers or SMS is used to<br />
activate or advise our members of staff with information, the following pagers<br />
protocol should be used as a best practice process. Pager messages should refer to<br />
the name or group of people that the message is meant for as some alerts go to<br />
multiple users. Each paged message will have one of three colour coded prefixes:<br />
GREEN: FOR ALL ROUTINE / INFORMATION ONLY MESSAGES<br />
AMBER: PREPARE A STATE OF READINESS/INCIDENT MESSAGES<br />
RED: ACTIVATION REQUIRED<br />
3.10 STEP FIVE: Common Recognised Information Picture (CRIP):<br />
3.11 In the event of a <strong>major</strong> <strong>incident</strong>, the Bournemouth, <strong>Dorset</strong> and Poole Local<br />
Resilience Forum will establish a Silver Command Centre and if required Gold<br />
Command at the SCG.<br />
3.12 Silver Command will establish a Common Recognised Information Picture (CRIP) –<br />
see Templates – which within a multi-agency setting, provides a shared statement of<br />
awareness of the <strong>major</strong> <strong>incident</strong>.<br />
3.13 All decisions that follow are based on a single and shared interpretation of what the<br />
problem is. It is therefore essential that the CRIP is established shortly after the alert<br />
is received and all data from within the Major Incident Notification form is<br />
acknowledged within the CRIP by the Incident Manager. The CRIP will also be the<br />
means of accurately briefing the Chief Executive and Trust Board on the <strong>incident</strong>.<br />
CONCEPT OF OPERATIONS Page 39
Major Incident Phases and Key PCT Actions<br />
3.14 There are distinct phases within a <strong>major</strong> <strong>incident</strong>. The key actions for each phase are<br />
as follows:<br />
Phase Description Action<br />
Pre – Major<br />
Incident<br />
Response<br />
Pre-<strong>plan</strong>ned activation of a<br />
<strong>plan</strong> in advance of the<br />
<strong>incident</strong>.<br />
Emergency response to<br />
the <strong>incident</strong>.<br />
Recovery Returning conditions to<br />
normality.<br />
Normality End of the <strong>incident</strong>,<br />
conditions returned to as<br />
near normal as possible.<br />
Activate the <strong>plan</strong> and implement the response<br />
required to mitigate the effects of the <strong>incident</strong>.<br />
• On-Call Duty Manager to determine scale of<br />
response, and activates Major Incident Plan if<br />
required.<br />
• Activate MIMT staff as needed.<br />
• Open Major Incident Room if required.<br />
• Ensure health represented at TCG Silver level<br />
if required.<br />
• Ensure health representation at SCG for <strong>NHS</strong><br />
Co-ordination and the Science and Technical<br />
Advice Cell if required.<br />
• Ensure communications links between Major<br />
Incident Room and SCG and SHA.<br />
• Provide co-ordinated primary care response to<br />
<strong>incident</strong>.<br />
• Mobilise community staff and resources.<br />
• Provide community nursing support to local<br />
Rest Centre if established.<br />
• Assess medium term impact and priorities for<br />
recovery.<br />
• Provide briefings and feedback at regular<br />
intervals.<br />
• Provide local health input into Local Resilience<br />
Forum Recovery Group if required.<br />
• Establish medium to long-term monitoring<br />
requirements.<br />
• Preserve all <strong>plan</strong>s and documentation used<br />
during the course of the emergency response.<br />
• Ensure learning from <strong>incident</strong> is captured<br />
• prepare for subsequent <strong>incident</strong> inquiries;<br />
public inquiries<br />
3.15 A health system alerting cascade chat is shown on the following pages, describing<br />
how and which organisations to contact during an <strong>incident</strong>.<br />
CONCEPT OF OPERATIONS Page 40
Health System Alerting Cascade – Page One of Two<br />
CONCEPT OF OPERATIONS Page 41
Health System Alerting Cascade – Page Two of Two<br />
CONCEPT OF OPERATIONS Page 42
4. Rest Centre/Reception Centre/Survival Centre/Safe Havens<br />
4.1 On receipt of a request from the Local Authority for a PCT Health response to<br />
support the Rest Centre/ Reception Centre/ Safe Haven, the On-Call Duty Manager<br />
will go through the following checklist before deciding the appointed PCT or Primary<br />
Care staff to represent the Health Dispatch Team. Clear co-ordination with DHUFT is<br />
vital to ensure that their staff are also despatched if required to augment the PCT<br />
Health Despatch Team.<br />
• Ascertain level of response required:<br />
• Has Major Incident been called?<br />
• Incident is present involving other organisations but requires health<br />
support.<br />
• Call is for information only at this time.<br />
• Initial information required:<br />
• Callers name and contact details.<br />
• Incident Co-ordinators name and contact details.<br />
• Where <strong>incident</strong> is taking place.<br />
• Address of rest centre, contact details, contact name.<br />
• Requirements of caller.<br />
• Are there medical emergencies/requirements.<br />
• Number of potential patients/evacuees involved.<br />
• Establish when to contact caller/co-ordinator i.e. regular time intervals, or<br />
with progression of tasks.<br />
• Time and date of call.<br />
• Consider the most appropriate, immediate links to a General Practice in the<br />
event of the need for urgent medical attention. During working hours, contact<br />
the Primary Care Commissioning Manager on 01202 541664 or for out of<br />
hours, contact the Urgent Care Centre (UCS) out-of hours service on 0845<br />
6001013 (Mon to Fri: 08.00am to 18.30pm. Sat to Sun: 24 hour service).<br />
• If there is a requirement to provide Pharmaceutical support to a Major<br />
Incident, the On-Call Staff will contact the PCT On-Call Duty Primary Care<br />
Pharmacist on Mobile number 07766 923915 requesting assistance.<br />
• If there is a requirement for DHUFT staff, the On-Call Duty Manager is to<br />
contact the DHUFT On-Call Director in the first instance on mobile 07789<br />
371954.<br />
CONCEPT OF OPERATIONS Page 43
5. Briefings<br />
5.1 Briefings enable those working on the PCT response to the <strong>major</strong> <strong>incident</strong> to be kept<br />
informed on the progress of the response to date; the most current objectives for the<br />
response and the opportunity to contribute to the bigger picture.<br />
5.2 Briefings are important at all levels of command within the <strong>incident</strong> and must be a<br />
priority for those leading the response at Gold and Silver levels. Potential audiences<br />
for briefings include:<br />
• Chief Executive: to enable briefing of the PCT Board;<br />
• Communications Lead: to enable media briefings to be prepared;<br />
• Staff supporting Gold and Silver Commanders: to ensure they can provide<br />
effective support through a sharing of objectives and information; and<br />
• Health staff operating at a Strategic Co-ordination Centre: to be updated on the<br />
Strategic Co-ordination Group meetings and what is happening at the Silver<br />
command level and within the STAC. This is to enable more effective <strong>NHS</strong><br />
co -ordination and return briefing for Silver.<br />
5.3 Briefings must be focused and provided at appropriate intervals at the discretion of<br />
the Director in Command of the response. Initially, briefings may only consist of the<br />
information gleaned from the CHALETS report. The content of the briefing should be<br />
formally recorded.<br />
5.4 Briefings can also be structure using the following format:<br />
I – Information = the background to the <strong>incident</strong><br />
I – Intention = the intention (what we are try to do) of the PCT and the <strong>NHS</strong><br />
M – Method = how we propose to manage the <strong>incident</strong>/command/resources<br />
A – Administration = any other items<br />
C – Communications = the communication structure in place<br />
R – Risk Assessment = the risks associated with the <strong>incident</strong><br />
(H) – Human Rights = any issues that may apply to the <strong>NHS</strong> setting<br />
CONCEPT OF OPERATIONS Page 44
6. Post Incident Actions and debriefing<br />
6.1 Once an <strong>incident</strong> has been declared, the PCT cluster have a responsibility to ensure<br />
that a number of important activities take place. These can be split into two groups.<br />
“Operational activities” include the procedural and administration needs of the<br />
service. “Post traumatic activities” include the psychological management of the staff<br />
involved in the <strong>incident</strong>.<br />
OPERATIONAL ACTIVITIES<br />
6.2 Post <strong>incident</strong>, the PCT cluster has a duty to ensure that operational procedures are<br />
carried out to restock our Major Incident Room and other equipment stocks.<br />
Debriefing is a very important process in order for the organisation to gain from<br />
lessons identified (positive or negative), make recommendations for change to our<br />
partners, and adapt service protocols if needed. It is therefore the Emergency<br />
Planning Manager who has the responsibility on behalf of the Gold Officer to<br />
organise, chair and administer <strong>major</strong> <strong>incident</strong> debriefs – monitoring the progress of<br />
actions as necessary.<br />
6.3 Post <strong>incident</strong> the PCT cluster has a responsibility to ensure that the following<br />
procedural and administrative activities are carried:<br />
a. A “hot debrief” immediately after the <strong>incident</strong> chaired by the Gold Officer or<br />
Silver Incident Manager and to include the circulation of welfare information<br />
b. The re-stock of PCT resources including the Major Incident Rooms<br />
c. “Stand down” time for all PCT staff involved<br />
d. Feeding of staff where necessary<br />
e. The collation of all paperwork and voice recordings to form a primary<br />
transcript record<br />
f. All members of staff receive a debrief proforma (found in the appendices)<br />
g. All MIMT staff to submit a report to the Emergency Planning Manager<br />
h. An internal Gold Team debrief<br />
i. An internal PCT <strong>major</strong> <strong>incident</strong> debrief<br />
j. Lessons identified and debrief actions to be allocated to individuals or the risk<br />
register guardian for progress <strong>plan</strong><br />
DEBRIEFING<br />
6.4 The purpose of a debrief is to:<br />
• Thank staff who have been involved for their efforts<br />
• Afford the opportunity to validate good practices and procedures<br />
• Highlight problem areas and flaws within procedures/equipment<br />
• Facilitate the flow of communication<br />
CONCEPT OF OPERATIONS Page 45
• Allow staff to input their perspective of the management of the <strong>incident</strong><br />
• Identify improvements in service delivery by feeding forward suggestions on<br />
training and policy<br />
• Provide support and encouragement for individual and team welfare<br />
• Identify the overall success or failure of the handling of the <strong>incident</strong><br />
6.5 The internal debriefing process should be followed at an early opportunity by a joint<br />
health services debrief involving representatives from all the medical organisations<br />
involved in the <strong>incident</strong> where there was a link with the PCT response. It would be<br />
usual for the lead PCT Incident Officer to chair the debrief.<br />
6.6 Information gathered from these debriefings can then be presented, where<br />
appropriate, to the <strong>Joint</strong> Services debriefing, usually organised by the Police Service.<br />
This will review the response overall, identify any lessons and any revision required<br />
to the existing <strong>plan</strong>s.<br />
6.7 It must be remembered that the notes taken at debriefs are subject to legal rules on<br />
disclosure and may form the basis of evidence before an inquiry.<br />
6.8 Areas to be considered at the debriefing should include:<br />
• Possible changes to policy and training if required.<br />
• Provision of an essential feedback loop in policy development and<br />
organizational wide contingency <strong>plan</strong>ning.<br />
• Comparison between <strong>incident</strong>s using a consistent approach.<br />
• Ensuring a spirit of co-ordination and co-operation with other services<br />
and agencies.<br />
• Provision of a valuable database for future reference, exercise and<br />
training.<br />
This process will be facilitated by examining the following specific issues during the<br />
debriefing:<br />
Systems<br />
Command and Control<br />
Community, patient & client<br />
management<br />
Media Management<br />
Personnel<br />
Mobilisation<br />
Numbers Involved<br />
Welfare<br />
Equipment<br />
Communications<br />
Forms and Stationery<br />
Protective Equipment<br />
Specialist Items<br />
CONCEPT OF OPERATIONS Page 46
6.9 A properly organised debrief will involve contributions from personnel from all<br />
departments involved in the <strong>incident</strong> or event e.g. IT, Communications,<br />
Commissioning, Provider services etc. as well as those staff directly involved in the<br />
<strong>incident</strong> response. These should be carefully recorded and follow up actions initiated<br />
to ensure that they are not forgotten.<br />
6.10 Lessons identified must have an associated action <strong>plan</strong> to convert them to lessons<br />
learnt.<br />
POST TRAUMATIC ACTIVITIES – STAFF AND VOLUNTEERS<br />
6.11 Post <strong>incident</strong> the PCT cluster have a moral and legal duty to consider staff’s<br />
psychological needs after exposure to a potentially traumatic or <strong>major</strong> <strong>incident</strong>.<br />
Additionally it makes economic sense to avoid loss of valuable personnel to the<br />
effect of psychological trauma. The following strategy aims to identify, with the use of<br />
appropriate psychological support workers, those who need support after an <strong>incident</strong><br />
and aims to refer them for early intervention. These actions must be carried out inconjunction<br />
with the Occupational Health Department within the sector and Trust.<br />
6.12 Post <strong>incident</strong> the PCT cluster have a responsibility to ensure the following actions<br />
are carried out:<br />
a. Provide staff with a welfare information pack available from Occupational<br />
Health department including information from the 24/7 Employee Assistance<br />
Programme available from Right Corecare who can be contacted on 0800<br />
1116 387<br />
b. Provide the line managers with names of all of their staff involved in the<br />
<strong>incident</strong><br />
c. Conduct a meeting with an Emergency Planning Manager, Silver Incident<br />
Manager and a senior support worker to determine whether a psychological<br />
risk assessment is required to take place for members of staff<br />
d. Where required, allocation of a support worker (s) to carry out a group or<br />
individual risk assessment to analyse the traumatic event or <strong>major</strong> <strong>incident</strong><br />
e. Where required, conduct an initial risk assessment interview within 3 days (but<br />
no more than one week) after the <strong>incident</strong><br />
f. Where required, conduct a further risk assessment interview after a month of<br />
the <strong>incident</strong> taking place<br />
g. Facilitation of a timely referral to an appropriate agency for treatment<br />
6.13 It is incumbent on managers to recognise that all staff and management colleagues<br />
exposed to a Major Incident may become vulnerable to post traumatic stress –<br />
concern for individual members of staff should be highlighted with the staff member<br />
and a support worker for risk assessment where necessary.<br />
CONCEPT OF OPERATIONS Page 47
6.14 Despite their training personnel may be affected psychologically after a Major<br />
Incident. The intensity and duration of the traumatic event can influence the<br />
development of a post traumatic illness. Examples of psychological and behavioral<br />
signs can include:<br />
• Clear signs of psychological distress that are not improving<br />
• Distressing feelings of having “changed”<br />
• Panic attacks<br />
• Vague signs of inexplicable physical illness that were not present prior to the<br />
traumatic event<br />
• Persistent sleeping difficulties, especially if sleep is disturbed by nightmares<br />
• Persistent verbal or physical aggression<br />
• Overwhelming emotions such as guilt, depression, anger or anxiety that are not<br />
improving with time<br />
• Problems in relationships that were positive or enjoyable prior to the traumatic<br />
event<br />
• A persistent desire to avoid work, anti-socialisation, and any activities that were<br />
previously enjoyable<br />
• Heavy drinking or abuse of other substances<br />
• Strong feelings that one cannot cope or go on<br />
POST TRAUMATIC ACTIVITIES – COMMUNITY AND PATIENTS<br />
6.15 It is very likely that several groups of people may be affected by a <strong>major</strong> <strong>incident</strong>.<br />
They may include:<br />
• Casualties (fatal, serious, slight)<br />
• Survivors (involved but not injured)<br />
• Evacuees (residents, passengers, employees, customers)<br />
• Local Community – not directly involved<br />
• Relatives & friends (home, work, hospitals, mortuaries)<br />
• Witnesses<br />
• Emergency services and other responding agencies (Statutory, Voluntary etc)<br />
• Individuals traumatised through 24/7 media viewing<br />
6.16 Similar to the process for support staff, the PCT should carry out the following actions<br />
in order to support local communities:<br />
a. Liaise with the Occupational Health Department of the sector/Trust and the Local<br />
Authority Social Services Department to seek advice on the course of action<br />
dependent on the <strong>incident</strong><br />
b. Where known patients or clients can be referred ensure that Occupational Health<br />
or local GPs practices follow up this information.<br />
c. Communications Department to publicise information and signposting on the Trust<br />
website<br />
CONCEPT OF OPERATIONS Page 48
d. Circulate this information and guidance to community providers including<br />
pharmacists and GP practices<br />
e. Circulate this information to borough partners for their staff and websites<br />
f. Consider community surgery sessions as needed<br />
7. Major Incident Documentation<br />
7.1 All decisions made by the Incident Manager must be recorded. Within the Major<br />
Incident Room, the Incident Log Books and Decision Log Books will be completed to<br />
provide a record of all tactical instructions received and actions taken. The Incident<br />
Log Books will be maintained by the Loggists.<br />
7.2 Incident logs and task allocation sheets must be completed for all general<br />
conversations and actions taken by the team.<br />
7.3 At the conclusion of the <strong>incident</strong>, all proformas, Log Books and any other<br />
documentation produced during the <strong>incident</strong> will be collated, filed and kept securely<br />
as determined by the PCT Business and Corporate (Non-Health) Records Retention<br />
Schedule.<br />
7.4 Following a <strong>major</strong> <strong>incident</strong>, the Trust may be required to provide evidence to an<br />
enforcement agency (such as the Health and Safety Executive), a judicial inquiry, a<br />
coroner’s inquest, the Police or a civil court hearing compensation claims. The Trust<br />
may be obliged or advised to give access to documents produced prior to, during<br />
and as a result of the <strong>incident</strong>.<br />
7.5 Under no circumstances must any document in any way relating, however<br />
slightly, to the <strong>incident</strong> be destroyed, amended, held back or mislaid.<br />
7.6 For these purposes ‘documents’ means not only pieces of paper but also<br />
photographs, audio and video tapes, and information held on word processors or<br />
other computers. It also includes electronic mail.<br />
7.7 The need to ‘preserve and protect’ all documentation must be understood in advance<br />
of a <strong>major</strong> <strong>incident</strong>, but also needs to be spread very quickly during an <strong>incident</strong> to<br />
reach those who might quite unknowingly hold significant documents. The Incident<br />
Manager will issue appropriate instructions and guidance on the procedures to be<br />
adopted in the immediate aftermath of a <strong>major</strong> <strong>incident</strong> to preserve all<br />
documentation.<br />
8. Communications<br />
8.1 Good arrangements for communications will be essential for the effective<br />
management of the <strong>major</strong> <strong>incident</strong> and will require dedicated management for<br />
CONCEPT OF OPERATIONS Page 49
success. On being alerted to the <strong>incident</strong>, the Duty Manager On-Call will be<br />
responsible for contacting the Trust Communications Lead, Chief Executive, Director<br />
of Public Health and other key staff, as appropriate. One of the Deputy Director of<br />
Communications should be nominated as the lead person during the <strong>incident</strong>.<br />
8.2 The Deputy Director of Communications is lead on delivering the PCT<br />
Communications Plan using pre-determined channels of communication to ‘Warn<br />
and Inform’ the Public, Local Health Community partners, Primary Care<br />
organisations leads, and link with the Local Resilience Forum (LRF) Warning and<br />
Informing Lead to communicate with other LRF Organisations. Communication has<br />
been further developed through the PCT Website which has a dedicated Emergency<br />
Planning webpage (http://www.bournemouthandpoole.nhs.uk/WS-Pan-<br />
<strong>Dorset</strong>/Pages/<strong>NHS</strong>-BP/aboutus/emergency-<strong>plan</strong>ning.htm). This is aimed at making<br />
the public aware of their own responsibilities in the event of a <strong>major</strong> emergency, the<br />
remit of the PCT, so that that everyone understands what their role is, and what they<br />
need to do. This will help us to:<br />
• Minimise the effects of an emergency as far as possible<br />
• Contain the immediate effects<br />
• Preserve essential services<br />
• Protect the population and the environment<br />
• Restore normally as quickly as possible<br />
• Preserve essential services<br />
8.3 The Deputy Director of Communications will liaise with the Strategic Health Authority<br />
Communications Lead and the LRF Warning and Informing Lead who will coordinate<br />
arrangements to deal with localised communications (including media<br />
liaison and information to the public) in discussion with the PCT. The Strategic<br />
Health Authority will be responsible for all media contacts at the Department of<br />
Health and Regional Emergency Departments (RED).<br />
8.4 All local <strong>NHS</strong> organisations and individual members of staff must channel upward<br />
communication, for example, to the Department of Health, through the Strategic<br />
Health Authority. The Strategic Health Authority will then ensure all health media<br />
releases are co-ordinated with the multi-agency media lead where a Strategic Coordination<br />
Centre is in place.<br />
8.5 Briefing the Chief Medical Officer, if necessary, will be the responsibility of the<br />
Strategic Health Authority Director of Public Health, who will also co-ordinate liaison<br />
with local public health staff and Health Protection Units.<br />
8.6 A comprehensive Local Contact Directory forms part of the Major Incident Plan.<br />
CONCEPT OF OPERATIONS Page 50
PART THREE<br />
Action Cards<br />
This section provides an<br />
overview of the roles of the<br />
On-Call Duty Manager and those<br />
members of the PCT Major<br />
Incident Management Team<br />
(MIMT)<br />
CONCEPT OF OPERATIONS Page 51
This page is intentionally blank<br />
ACTION CARDS Page 52
PCT MAJOR INCIDENT ROOM (INTERNAL) ROLES<br />
CARD<br />
NO<br />
RESPONSE ROLE<br />
1 Incident Commander (Gold PCT)<br />
2<br />
Major Incident Room Manager (Silver<br />
PCT)<br />
3 Major Incident Room Coordinator<br />
4/5<br />
Administration (and<br />
Telecommunications) Support 1& 2<br />
STAFF WHO MAY UNDERTAKE<br />
ROLE<br />
Senior manager from the On-Call Duty<br />
Manager roster, until relieved by an<br />
appropriate Director<br />
A Deputy Director or Senior Manager able<br />
to lead / co-ordinate the health system<br />
response. Usually the On-Call Duty<br />
Manager unless relieved<br />
A Senior Manager who has the team<br />
leading skills necessary to task manage,<br />
coordinate the staff and processes within<br />
the Major Incident Team.<br />
Admin and Clerical<br />
6 Loggist One of the PCT’s Loggist-trained staff<br />
7<br />
Communications and Media<br />
Coordinator<br />
8 IT support IT support officer<br />
9 Resourcing/HR<br />
A member of the Communications Team<br />
Any member of staff or a staff from the<br />
HR team<br />
10 SPRIG Lead PCT SPRIG Lead or Deputy<br />
11 Public Health Lead<br />
Director of Public Health or Public Health<br />
Consultant<br />
ACTION CARDS Page 53
Member of staff for the<br />
role is suggested<br />
below the role title.<br />
Primary role is in<br />
bold<br />
For specific actions write the<br />
time the action was started<br />
and completed in this<br />
column. Add your initials in<br />
case you pass the card to<br />
another person.<br />
Blue indicates<br />
on-call for the<br />
role.<br />
Colour Indicates<br />
Whether role is drawn<br />
from an On-Call rota<br />
Yellow indicates<br />
no on-call for the<br />
role.<br />
ACTION CARDS Page 54
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
INCIDENT COMMANDER (GOLD PCT)<br />
(On-Call Duty Manager<br />
then transferred to a Director – level 3 trained)<br />
1<br />
ACTION CARDS Page 55<br />
Name<br />
It is the responsibility of this role to set the strategic direction of the organisation during the <strong>incident</strong> and to support<br />
the provisions required by the PCT Silver Incident Manager or operational staff as needed. They are responsible for<br />
the overall commitment of staff, funding and resources to the <strong>incident</strong>. They have responsibility to ensure business<br />
continuity and resilience within the PCT’s daily activities.<br />
Directors attending the SCG on behalf of the Chief Executive will be representing the three <strong>Dorset</strong> Acute hospitals<br />
and <strong>Dorset</strong> HealthCare as well as local primary care resources. They will need to be able to make decisions<br />
regarding the deployment of these organisations’ resources and assets, including funding, without need to refer back<br />
for authority. In a significant <strong>incident</strong> where strategic decision making is required, a muti agency Gold meeting will be<br />
called. This calls together representatives from the responding organisations at Chief Executive level, and will<br />
usually take place no sooner than an hour after the <strong>incident</strong> occurred, and will in most cases take place at Winfrith<br />
Police Headquarters.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Receive <strong>incident</strong> call and log date and time of call and caller’s name<br />
Obtain a detailed understanding of the problem and its impact.<br />
• Who, if anyone, has requested the Major Incident Plan activation?<br />
• Type of <strong>incident</strong>?<br />
• Number of casualties?<br />
• Scope of Impact / Trusts affected?<br />
• Any specific or urgent action required?<br />
Any other relevant information<br />
2. Formally activate <strong>plan</strong>;<br />
• MAJOR INCIDENT STAND-BY or MAJOR INCIDENT DECLARED<br />
3. Liaise with Tactical Advisor (Emergency Planning Officer) as needed<br />
4. Allocate a Senior Manager or Emergency Planning Officer at Silver level to manage the <strong>incident</strong>,<br />
confirm whether they need to set up the Major Incident control room and act as the Major Incident<br />
Room Manager.<br />
5. Contact the Communications and Media on call officer or deputy for commencement of action card<br />
6. Contact the Director of Public Health or deputy for specialist advice and commencement of action<br />
card<br />
7. Consider advising the Chief Executive if you feel it is relevant<br />
8. Ensure appropriate evacuation of trust sites as required<br />
9. IF YOU ARE UNABLE TO ALLOCATE THE SILVER INCIDENT MANAGER ROLE REFER TO<br />
THEIR ACTION CARD AND USE IN TANDEM NOW<br />
10. Move to Police HQ, Winfrith if needed<br />
11. Activate a trained loggist if needed<br />
12. Support requests from local Acute Trusts for resources and in order to facilitate accelerated<br />
discharge through the SPRIG Lead where available<br />
13. Contact local acute providers and establish if an accelerated discharge to the PCT cluster areas is<br />
expected and consider requesting whether an accelerated discharge team can be put in place by the<br />
providers in order to support releasing of acute capacity.
14. Agree actions as appropriate, and offer most appropriate member of the PCT staff to attend local<br />
acute provider control room for link into the control suite (if required)<br />
15. Keep staff informed of developments to ensure those involved in the response know what they are<br />
working towards and have a good awareness of the situation.<br />
16. Consult with <strong>NHS</strong> South – initial call and schedule in further calls as needed<br />
17. Consider the need for normal service suspension<br />
18. Agree actions as appropriate and request most appropriate member of the provider staff to attend<br />
control suite for link into the PCT control team (if needed and required)<br />
19. Provide a response to all PCT staff and independent contractors using Major Incident control room<br />
e-mail account. Number each Major Incident Message for reference<br />
20. Consider mutual aid requirements from adjoining PCTs for the provision of additional community<br />
services and PCT infrastructure, Local Authorities for voluntary sector and social services and<br />
SWAST for private ambulance/medical services; allocate the cascade of information to the Silver<br />
Incident Manager.<br />
21. Ensure regular communication continues across the area and with the local borough at strategic<br />
level as needed<br />
22. Ensure the safety of the wider-team and provide regular update messages to all staff<br />
23. Ensure business recovery actions begin before the end of the <strong>incident</strong> to allow a smooth return to<br />
normal operations – make provision for normal service continuity / resumption<br />
24. Establish criteria for Major Incident stand down<br />
25. Declare Major Incident stand-down as appropriate<br />
26. Check through the Log Book with the loggist and correct mistakes accordingly, this is your legal<br />
back-up<br />
27. Attend any debriefing sessions as appropriate<br />
28. Provide post-<strong>incident</strong> report to <strong>NHS</strong> South<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
ACTION CARDS Page 56
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
MAJOR INCIDENT ROOM MANAGER<br />
(SILVER PCT)<br />
(Non-rostered manager from the On-Call Duty<br />
Manager roster – level 2 trained)<br />
2<br />
ACTION CARDS Page 57<br />
Name<br />
It is the responsibility of this role to either be responsible for acting as the “Major Incident Room Manager” or<br />
responding to the multi-agency Tactical Coordination Group (TCG) as the <strong>NHS</strong> “Silver” Incident Manager to liaise<br />
with the emergency services and other partners. They will be responsible for the tactical management of the <strong>incident</strong><br />
either at by forming a control team to manage the <strong>incident</strong>.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Receive <strong>incident</strong> call and log date and time of call and caller’s name<br />
Obtain a detailed understanding of the problem and its impact.<br />
• Who, if anyone, has requested the Major Incident Plan activation?<br />
• Type of <strong>incident</strong>?<br />
• Number of casualties?<br />
• Scope of Impact / Trusts affected?<br />
• Any specific or urgent action required?<br />
Any other relevant information<br />
2. Log actions in your Emergency Log Book<br />
3. Agree immediate action with On-Call Duty Manager or designated Director acting as Gold PCT –<br />
respond to the TCG (if requested and if it ) and deal with the actions as required at “Silver” level or<br />
respond to the control suite and ensure that the following is carried out<br />
4. Contact other members of the Major Incident Management Team (Major Incident control room)<br />
(MIMT) to commence actions in cards and request, if appropriate, Major Incident control room<br />
assembly (see next action)<br />
5. Call out staff using the SMS system, Click SMS. Select the appropriate groups for call out and<br />
monitor the responses in the inbox. This can be used at any work or home PC.<br />
6. Establish a communications method between control team members, with a contingency<br />
arrangement, until such time as the control room has been established<br />
7. On arrival at the control room, allocate a administration (and telecommunications) support officer to<br />
the first phone line<br />
8. Start recording any decisions in the room Decision Log Book<br />
9. Allocate a resource officer to assist with immediate, mid-long term staff requirements in the control<br />
room and site resources – ensure they use the SMS system to activate staff and record the<br />
attendees on the white board<br />
10. Allocate a Major Incident Control Room Coordinator to deal with tasks<br />
11. Allocate an Ambulance Liaison Officer to SWAST control if a mass casualty <strong>incident</strong> or as needed<br />
12. Allocate an administration (and telecommunications) support officer to the second phone line<br />
13. Liaise with Tactical Advisor (Emergency Planning Manager) as needed<br />
14. Contact the Communications and Media officer and confirm their attendance at the control room if
needed (and deal with press enquiries) or whether they will deal with them directly<br />
15. Contact the Director of Public Health and confirm their attendance at the control suite if the <strong>incident</strong><br />
is a public health issue or keep them updated via SMS<br />
16. Ensure that your team are logging all communications and dealing with the separate action tasks<br />
from the <strong>incident</strong> (i.e. difference between logged entries and tasks)<br />
17. Activate a loggist to the control room, then ensure they log actions in the Room Log Book<br />
18. Activate IT support to control room<br />
19. Assist with the appropriate alerting and co-ordination of evacuation of trust sites as required (e.g. if<br />
there is a risk to PCT, GP, pharmacies etc.)<br />
20. On the instruction of Gold, to consider allocating staff resources to create a discharge team, in order<br />
to facilitate accelerated discharge from an acute setting<br />
21. If not already carried out set up the control room and Major Incident e-mail account<br />
22. Prior to any service/staff mobilisation in response to a Major Incident, ensure via emergency<br />
services, that it is safe to commence a recovery phase<br />
23. Prepare and complete briefings as necessary:<br />
- To Strategic Co-ordination Group (if activated) - Common Recognised Information Picture (CRIP)<br />
- To Chief Executive – Chief Executives SITREP<br />
- To SHA – DH Health Regional SITREP<br />
24. Inform neighbouring <strong>NHS</strong> organisations / local authorities / social services<br />
25. Confirm with Gold PCT the criteria for Major Incident stand down<br />
26. Check through the Log Book and correct mistakes accordingly, this is your legal back-up<br />
27. Attend any debriefing sessions as appropriate<br />
28. Provide post-<strong>incident</strong> report to the Emergency Planning Manager<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
ACTION CARDS Page 58
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
MAJOR INCIDENT ROOM<br />
COORDINATOR<br />
(Non-rostered manager from the On-Call Duty<br />
Manager roster or Senior Manager – level 2 trained)<br />
3<br />
ACTION CARDS Page 59<br />
Name<br />
To provide operational task management support to Silver Incident Manager (if in post). The post holder will be<br />
responsible for managing the overall running of the Major Incident control room and dealing with tasks that come into<br />
the control room.<br />
The role will act as the focal point for tasks. They will channel any requests made by external partners to the Major<br />
Incident Management Team, ensuring the Silver Incident Manager is fully aware or involved as necessary.<br />
Similarly, they will channel any issues or barriers encountered by the Major Incident Management Team to for<br />
appropriate resolution e.g. Incident Director, IT Services, HR Lead etc.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Log actions on a log sheet and record decision in the Decision Log Book.<br />
2. Oversee the set-up of the Major Incident control room, and obtain a briefing from anyone else<br />
involved in its establishment to identify any outstanding actions to be completed. Ensure these are<br />
completed accordingly<br />
3. Establish Administration processes for the Major Incident Control Room operations, including:<br />
- Inputting information into the <strong>incident</strong> logs<br />
- Liaise with the Resourcing/HR role to ensure staff are being resourced as<br />
needed<br />
- A list of actions required for the <strong>incident</strong> response for the Admin Support to<br />
undertake<br />
- Define functions for the whiteboards: critical contact details, duty rota’s, location<br />
of Officers involved in multi-agency response etc<br />
- Define task management – i.e. all tasks to come via your position<br />
4. Liaise with the Silver Incident Officer and ensure that all MIMT staff positions have been allocated<br />
5. Admin Support on priority work tasks using the below list of administrative duties (if no administrative<br />
support available, ensure the tasks are undertaken yourself or by available officers as appropriate)<br />
6. Prioritise delivery of resources for <strong>major</strong> <strong>incident</strong> response and normal critical business functions.<br />
Identify those responsible for above<br />
7. On receipt of all in-coming messages (printed / telephone) from the MIMT staff, ensure appropriate<br />
action is taken, or escalated further to the Tactical Management Group if established. All decisions<br />
made must be captured by you in the Decision Log Book<br />
8. Ensure signage for Control Room is established in accordance to the floor <strong>plan</strong> in the Major Incident<br />
Plan<br />
9. Brief personnel on their arrival in the Control Room using CHALET or CRIPS reporting system, see<br />
Major Incident Plan<br />
10. Supervise effective management e.g. hold regular meetings with the MIMT and ensure staff are<br />
briefed<br />
11. Ensure all personnel are given a copy of the action card for the role they will be fulfilling, see Major<br />
Incident Plan. To include any staff coming in to a new shift
12. Ensure Health & Safety Regulations are adhered to by staff e.g. shift patterns, staff breaks and<br />
refreshments. Appoint HR Lead if deemed necessary<br />
13. Ensure all personnel are aware of the Fire Safety Instructions<br />
14. Take stock of actions taken and <strong>incident</strong> development. Consider what further actions/resources<br />
should be taken/deployed<br />
15. When resourcing of the Major Incident Control Room is complete, confirm extension numbers and<br />
distribute for internal use. Note: consider electronic distribution and whiteboards<br />
16. Ensure that everyone is supplied with stationery and aware of the telephone numbers / email<br />
address to be used<br />
17. At the end of your shift you should hand over to someone with similar skills. You should ensure that<br />
you hand over a progress report and management <strong>plan</strong> for the next shift<br />
18. Document Stand Down and inform all agencies/organisations that the Major Incident Control Room<br />
is being stood down.<br />
19. Stand-down Admin Support and thank them for their help<br />
20. Ensure all documentation relating to the <strong>incident</strong> is secured for future reference. Photograph white<br />
boards.<br />
21. Ensure Major Incident Control Room is returned to a state of normality.<br />
- Replace and restock used Incident Logs/books, template forms and stationery<br />
- Return furniture to original positions;<br />
- Clean all white boards;<br />
- If out of hours, ensure that the kitchen area is cleared up and re-stocked if<br />
appropriate<br />
- Arrange for the Major Incident Control Room to be cleaned (if necessary).<br />
22. Confirm with Silver Incident Manager the criteria for Major Incident stand down<br />
23. Check through the Log Book and correct mistakes accordingly, this is your legal back-up<br />
24. Attend any debriefing sessions as appropriate<br />
25. Provide post-<strong>incident</strong> report to the Emergency Planning Manager<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
ACTION CARDS Page 60
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
ADMINISTRATION (AND<br />
TELECOMMUNICATIONS) SUPPORT 1<br />
(Level 1 Control trained person)<br />
4<br />
ACTION CARDS Page 61<br />
Name<br />
It is the responsibility of this role to resource the required functions of the <strong>incident</strong> mid to long term to ensure that the<br />
response can be maintained with the required staffing seamlessly.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Start an authorised log book; or <strong>incident</strong> log form; to record your actions, decisions and<br />
conversations<br />
2. Deal with any requests that arise and record these requests<br />
3. Assist with the set up of the room – positioning the PCs, phones, printers and other equipment<br />
4. Log onto the PC system<br />
5. Liaise with your second administration support office to divide duties as needed<br />
6. Set up the printers and faxes – test them as needed<br />
7. Print off all incoming messages and pass to Major Incident Room Coordinator for action. Once<br />
action is determined.<br />
8. Liaise with IT department to ensure that problems as dealt with swiftly contact: From 17:30 to 08:30<br />
and 17:00 Friday til 08:30 Monday the number is 01305361499 or normal times is 01305361223<br />
9. Ensure that all tasks are separated, recorded and dealt with ensuring that each task is closed down<br />
as completed<br />
10. Monitor the <strong>major</strong>.<strong>incident</strong> email accounts for incoming emails as deal with as needed<br />
11. Direct any press enquiries to the Communications and Media officer<br />
12. Support the control suite manager or other officers in the control suite as needed<br />
13. Set up Click SMS to SMS or page additional staff as needed to request their attendance or keep<br />
them updated, monitor the receiver inbox on Click SMS for messages if there is no Administration<br />
(and Telecommunications) Support 2 staff member<br />
14. Assist with the <strong>NHS</strong> South reporting<br />
15. Keep external partners, GP’s, pharmacies, dentists and others in the health and non health economy<br />
updated as needed<br />
16. Check through the Log Book and correct mistakes accordingly, this is your legal back-up<br />
17. Attend any debriefing sessions as appropriate<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
ACTION CARDS Page 62
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
ADMINISTRATION (AND<br />
TELECOMMUNICATIONS) SUPPORT 2<br />
(Level 1 Control trained person)<br />
5<br />
ACTION CARDS Page 63<br />
Name<br />
It is the responsibility of this role to resource the required functions of the <strong>incident</strong> mid to long term to ensure that the<br />
response can be maintained with the required staffing seamlessly.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Start an authorised log book; or <strong>incident</strong> log form; to record your actions, decisions and<br />
conversations<br />
2. Deal with any requests that arise and record these requests<br />
3. Assist with the set up of the room – positioning the PCs, phones, printers and other equipment<br />
4. Log onto the PC system<br />
5. Liaise with your first administration support officer to divide duties as needed<br />
6. Set up the printers and faxes – test them as needed<br />
7. Liaise with IT department to ensure that problems as dealt with swiftly<br />
8. Ensure that all tasks are separated, recorded and dealt with ensuring that each task is closed down<br />
as completed<br />
9. Monitor the <strong>major</strong>.<strong>incident</strong> email accounts for incoming emails as deal with as needed<br />
10. Direct any press enquiries to the Communications and Media officer<br />
11. Support the Major Incident Room Co-ordinator or other managers in the control suite as needed<br />
12. Assist the Administration (and Telecommunications) Support 1 SMS or paging as needed and set up<br />
Click SMS to monitor the received messages box in order to pass information onto MIMT as needed<br />
13. Assist with the <strong>NHS</strong> South reporting<br />
14. Keep external partners, GP’s, pharmacies, dentists and others in the health and non health economy<br />
updated as needed<br />
15. Check through the Log Book and correct mistakes accordingly, this is your legal back-up<br />
16. Attend any debriefing sessions as appropriate<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
LOGGIST<br />
(HPA or LRF loggist trained person)<br />
6<br />
ACTION CARDS Page 64<br />
Name<br />
It is the responsibility of the loggist to maintain an accurate log of decisions and actions taken in the course of the<br />
<strong>incident</strong>. The loggist is NOT a minute taker/telephone operator/admin support. It is important that logs are<br />
comprehensive as they are a legal document that would be used in court during any subsequent public inquiry.<br />
There may be a loggist placed with Gold PCT at Police HQ, Winfrith and at Silver PCT at one of the PCT Major<br />
Incident Control rooms.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Obtain the Emergency Logbook from the responding manager if already started alternatively begin a<br />
new book.<br />
2. Complete log entries as trained.<br />
• Write in black ink, amendments in red.<br />
• Rule through mistakes with a single line and initial then add the correct word.<br />
• Do not tear pages from the Log Book.<br />
• Don’t leave blank spaces, rule through them.<br />
• Don’t overwrite<br />
• Make sure you put the correct information in the correct margin.<br />
• At the end of a series of entries Z through any empty space, sign, date and time.<br />
• Do not make assumptions.<br />
• Use reference numbers linked to records/actions as needed.<br />
Do not use correction fluid or similar.<br />
3. Position yourself close to or in contact with your <strong>incident</strong> manager.<br />
4. Maintain notes of all actions, events, decisions and rationale behind the decisions. Prompt the<br />
<strong>incident</strong> manager as required about outstanding issue and clarity of items to be included.<br />
5. Ensure all exhibits are marked on the reverse side, collected and inserted into exhibit log (if it fits)<br />
when the <strong>incident</strong> is stood down.<br />
6. Ensure photographs are taken of whiteboards, SITREPS and other visual sources and photos are<br />
put in exhibit log.<br />
7. Meet with the <strong>incident</strong> manager after the <strong>incident</strong> to go through the log and correct any mistakes<br />
accordingly<br />
8. Attend any debriefing sessions as appropriate<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
COMMS AND MEDIA CO-ORDINATOR<br />
(Head of Communications or deputy<br />
– level 2 trained)<br />
7<br />
ACTION CARDS Page 65<br />
Name<br />
It is the responsibility of this role to manage the relationship with the media and staff by ensuring consistent<br />
messages are disseminated to staff, health partners, services and the public, in line with national or local partner<br />
messages. The post holder will co-ordinate and monitor information from credible sources that is important for the<br />
running of the <strong>incident</strong> e.g. DH and <strong>NHS</strong> South, <strong>Dorset</strong> Police and BBC/Sky.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Start an authorised log book for your actions, decisions and communications<br />
2. Set up the press room, or another room designated for press monitoring<br />
3. Agree with the Incident Managers the strategy for dealing with the press<br />
4. Begin monitoring the situation and regularly update the Incident Managers at Silver and Gold<br />
5. Contact London Regional Communications to establish Regional / National situation, and local<br />
actions required and in order to confirm whether <strong>NHS</strong> South is managing the press response<br />
centrally for public messages<br />
6. Prepare all-staff e-mail for cascade by Gold and fax cascade to sites not accessible via e-mail e.g.<br />
Independent Contractors<br />
7. Liaise with the emergency services, <strong>NHS</strong> partners (in particular the community provider), private<br />
organisations involved in the <strong>incident</strong> to ensure that there is a consistent message<br />
8. Ensure the On Call Manager / Chief Executive delivers messages consistent with Department of<br />
Health and <strong>NHS</strong> South<br />
9. Continue monitoring the situation and ensure flow of consistent messages to staff and if necessary,<br />
the public, until informed to stand-down the <strong>major</strong> <strong>incident</strong> response<br />
10. If required, establish Press & Media Centre if there is a deluge of calls which the Control Suite cant<br />
manage<br />
11. Inform staff where to direct media enquiries<br />
12. If required, remain in the Press & Media room to respond to interests of the Media<br />
13. Contribute to the post-<strong>incident</strong> report being compiled by the nominated Senior Manager<br />
14. Pass all messages and notes of actions taken to the Administrator for chronological log<br />
15. Liaise with other communications teams members for further commitment as needed<br />
16. Identify post <strong>incident</strong> staff that could be used for soft news articles/follow up news<br />
17. Check through the Log Book with the loggist and correct mistakes accordingly, this is your legal<br />
back-up<br />
18. Attend any debriefing sessions as appropriate<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
ACTION CARDS Page 66
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
IT SUPPORT Name<br />
Provide support as necessary to the Major Incident Room. Calls for assistance should be made high priority.<br />
Ensure IT advice is available within the Major Incident room to assist with any queries or faults on equipment such as<br />
telephones, smartboard and laptops.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Set-up the emergency laptops and printer if necessary in the Major Incident Control Room in<br />
conjunction with the Standard Operating Procedures for the set-up of all technical and<br />
communication assets (as per the Major Incident Plan)<br />
2. Provide technology support to ensure that the Trust Satellite telephone is functional<br />
3. Ensure that procedures for setting up and using the computer equipment are available and<br />
accessible<br />
4. Ensure that the Major Incident room e-mail account if available and working on each laptop<br />
5. Ensure that the emergency laptops can access the internet and other relevant software as needed<br />
6. Provide support if required due to technical issues<br />
7. Determine what continued commitment is required by the PCT IT Team to maintain the continued<br />
longer term response<br />
8. Ensure all actions and response details are entered into the Incident Log.<br />
9. At the end of your shift you should hand over to someone with similar skills. You should ensure that<br />
you hand over a progress report and management <strong>plan</strong> for the next shift<br />
10. Attend any debriefing sessions as appropriate<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
8<br />
ACTION CARDS Page 67
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
RESOURCING<br />
(Any staff member or HR team )<br />
9<br />
ACTION CARDS Page 68<br />
Name<br />
It is the responsibility of this role to resource the required functions of the <strong>incident</strong> mid to long term to ensure that the<br />
response can be maintained with the required staffing seamlessly. Implement the Human Resources Framework.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Start an authorised log book or <strong>incident</strong> log form for your actions, decisions and communications<br />
2. Confirm the staff and volunteers that are currently being deployed and used on the <strong>incident</strong><br />
response, noting the area they are responding to (i.e. <strong>incident</strong> site, control suite, command officer<br />
roles, other support), the time they started and time they need to finish<br />
3. Confirm with the Silver and Gold managers the mid and long term requirements of the <strong>incident</strong> areas<br />
and the agreement on whether internal departments are ceasing certain activities to help the PCT<br />
response to the <strong>incident</strong><br />
4. Confirm with the Silver and Gold managers the mid and long term requirements of the <strong>incident</strong> areas<br />
in relation to other external resources that have a direct relationship with the PCT that may be<br />
required to assist with the <strong>incident</strong> (e.g. GP’s)<br />
5. Draw up or obtain a list of <strong>incident</strong> team members and the roles they are performing<br />
6. Use flip charts/whiteboards to identify any immediate gaps in the resource requirements<br />
7. Make contact with HR or department heads to obtain staff contact details and implement the Human<br />
Resources Framework<br />
8. Reschedule diaries of the MIMT members<br />
9. Alert Occupational Health to the <strong>incident</strong> and maintain lists of staff involvement for follow-up post<br />
<strong>incident</strong><br />
10. Consider setting up staff crèche facilities if the <strong>incident</strong> is likely to become protracted<br />
11. Confirm that band 1-7 will receive overtime payments for call out and band 8 and above will receive<br />
time in lieu. Ensure that staff working comply with the 48 hour working time directive.<br />
12. Contact staff via SMS/page/phone etc. to ask whether they would be available to respond to the<br />
<strong>incident</strong> request as needed<br />
13. Consider liaising with other borough areas for mutual aid support as needed<br />
14. Use flip charts/whiteboards to fill in the resource requirements for the mid to long term stages of the<br />
<strong>incident</strong> broken into manageable shifts as needed<br />
15. Ensure staff within the Major Incident Room take regular breaks<br />
16. Ensure that appropriate welfare is arranged for staff that need to stay overnight in local hotels or<br />
other requests as needed<br />
17. Consider your own resilience and handover to a new resource manager as needed<br />
18. Identify post <strong>incident</strong> staff that could be used for soft news articles/follow up news – pass these<br />
details to the Communications and Media Co-ordinator
19. Check through the Log Book and <strong>incident</strong> logs and correct mistakes accordingly, this is your legal<br />
back-up<br />
20. Attend any debriefing sessions as appropriate<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
ACTION CARDS Page 69
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
SPRIG LEAD<br />
10<br />
ACTION CARDS Page 70<br />
Name<br />
To ensure the escalation process is implemented as per the Seasonal Escalation Plan across the local health<br />
community.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Start an authorised log book or <strong>incident</strong> log form for your actions, decisions and communications<br />
2. Ensure all providers are updating Capacity Management System (CMS)<br />
3. Facilitate SPRIG teleconference as required (pre-<strong>major</strong> <strong>incident</strong> status)<br />
4. Communication to GP Practices and Care Homes to alert them of the situation<br />
5. Ensure all providers are fully escalated (in line with SPRIG action cards)<br />
6. Support de-escalation <strong>plan</strong>ning and implementation<br />
7. Ensure ambulance divert policy is implemented if appropriate<br />
8. Check through the Log Book and <strong>incident</strong> logs and correct mistakes accordingly, this is your legal<br />
back-up<br />
9. Attend any debriefing sessions as appropriate<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME
<strong>NHS</strong> DORSET, BOURNEMOUTH & POOLE<br />
MAJOR INCIDENT TEAM<br />
DIRECTOR OF PUBLIC HEALTH<br />
(Director of Public Health or deputy<br />
– level 3 trained)<br />
11<br />
ACTION CARDS Page 71<br />
Name<br />
It is the responsibility of this role to co-ordinate a public health <strong>incident</strong>. The have the responsibility to maintain<br />
communications with other Directors of Public Health, public health specialists, health protection unit and other senior<br />
clinicians as required. The Director of Public Health may have to chair the STAC.<br />
CORE ACTIONS TIME/<br />
INITIALS<br />
1. Start an authorised emergency log book or <strong>incident</strong> log forms for your actions, decisions and<br />
communications<br />
2. Take a lead in managing the public health and environmental consequences of the event, in liaison<br />
with the Health Protection Agency<br />
3. Discuss with HPU who will lead on the Public Health response and how you should stay informed<br />
about the <strong>incident</strong><br />
4. Update the Gold and Silver managers as appropriate<br />
5. Formulate Case Definitions, as appropriate, in liaison with the Health Protection Agency<br />
6. Undertake active case finding and site visits, as appropriate<br />
7. Investigate cases, including microbiology and toxicology testing, taking advice from the Health<br />
Protection Agency, as necessary<br />
8. Collect data on cases and set up and manage the database of cases<br />
9. Check that essential actions are undertaken by responders to address risks to public health and the<br />
environment<br />
10. Disseminate best available advice on clinical management to all health professionals, including<br />
environmental health colleagues<br />
11. Check and see if a ‘Stay In and Keep Your Doors and Windows Closed’ has already been issued via<br />
the Police or Fire Brigade. You may need to liaise with the ‘Fire Services' Team who may be<br />
carrying out environmental monitoring to determine whether people should stay in or be evacuated<br />
as required<br />
12. Work with <strong>Dorset</strong> Police to exchange information and discuss joint investigations, if necessary<br />
13. Work with <strong>Dorset</strong> Fire and Rescue - the HAZMAT (Hazardous Materials) Officer at the Scene will<br />
have additional information on any chemicals, please check with Health Protection Unit before<br />
contacting the Fire Service to avoid duplication if required<br />
14. Ensure adequate health protection measures are implemented<br />
15. Ensure immediate actions are taken to manage the risk, including decontamination<br />
16. Ensure that health service resources are notified and protected<br />
17. Ensure epidemiological follow up and health care provision for those affected, including responders<br />
and health care staff<br />
18. Coordinate activity to redress health and environmental issues, taking advice, where necessary,<br />
from the Health Protection Agency<br />
19. Assess the impact of the event on public health and the environment<br />
20. Link in with Occupational Health departments for affected responders and businesses and organise<br />
and provide sampling and the provision of countermeasures/medications, where indicated
21. Enact statutory legislation to effect actions (e.g. quarantine)<br />
22. Execute Proper Officer duties / ensure Proper Officer duties executed<br />
23. Liaise with the Communications and Media Co-ordinator to ensure consistent messages with the<br />
HPA<br />
24. Check through the Log Book with the loggist and correct mistakes accordingly, this is your legal<br />
back-up<br />
25. Attend any debriefing sessions as appropriate<br />
26. Provide post-<strong>incident</strong> report to <strong>NHS</strong> South<br />
COLLATION OF EVIDENCE ACTIONS – ALL PAPERWORK IS SUBJECT TO DISCLOSURE<br />
A. ONCE COMPLETE PERSONALLY HAND THIS FORM TO THE EMERGENCY PLANNING<br />
MANAGER<br />
B. COLLATE ANY AND ALL OTHER PAPERWORK USED (EVEN SCRAPS OF PAPER), INCLUDING<br />
THE LOG BOOK AND HAND TO THE EMERGENCY PLANNING MANAGER<br />
C. IF YOU HAVE USED A DICATPHONE BAG THIS UP AS EVIDENCE, LABEL IT AND HAND TO<br />
THE EMERGENCY PLANNING MANAGER<br />
D. COMPLETE AN INCIDENT REPORT WITHIN THREE DAYS OF THE INCIDENT<br />
E. ALL PAPERWORK MUST REMAIN IN SECURED <strong>NHS</strong> PREMISES AT ALL TIME<br />
ACTION CARDS Page 72
This page is intentionally blank<br />
ACTION CARDS Page 73
PART FOUR<br />
REPORTING<br />
TEMPLATES<br />
This section provides an<br />
overview of those reporting<br />
templates that may be used<br />
within <strong>major</strong> room in support of<br />
the Major Incident Management<br />
Team’s role and its reporting<br />
duties with multi –agency<br />
partners<br />
REPORTING TEMPLATES Page 74
This page is intentionally blank<br />
REPORTING TEMPLATES Page 75
Background<br />
REPORTING TEMPLATES<br />
The following are templates that the On-Call Incident Director may need to utilise on receiving<br />
notification of a Major Incident. They are as follows:<br />
• Major Incident Notification Form<br />
This is the generic template used by all <strong>NHS</strong> Trusts in capturing all information received on<br />
notification of a Major Incident. The first is an example of the detail that should be captured, and<br />
the second is a blank template.<br />
• Health Regional Situation Report<br />
his situation report will be completed supplementary to the Local Resilience Fora / Government<br />
Office situation report. The aim of this report is to present a concise summary of key information<br />
from each <strong>NHS</strong> Trust within the South West region at regular intervals. This report will be in<br />
addition to existing daily capacity reporting. This report is restricted to <strong>NHS</strong> service provision<br />
and it is operating on the assumption that social care issues will be communicated through the<br />
multi-agency situation reporting mechanisms.<br />
• Common Recognised Information Picture (CRIP)<br />
In the event of a <strong>major</strong> <strong>incident</strong>, the Bournemouth, <strong>Dorset</strong> and Poole Local Resilience Forum will<br />
convene a SCG. The SCG will establish a Common Recognised Information Picture (CRIP)<br />
which within a multi-agency setting provides a single, shared statement of awareness of the<br />
<strong>major</strong> <strong>incident</strong>.<br />
All decisions that follow are based on a singe and shared interpretation of what the problem is.<br />
It is therefore essential that the CRIP is established shortly after the alert is received and all data<br />
from within the Major Incident Notification form is acknowledged within the CRIP by the Incident<br />
Director. The CRIP will also be the means of accurately briefing the Chief Executive and Trust<br />
Board on all events by the Incident Director.<br />
• Major Incident Task Form<br />
All tasks that are requested via email, or telephone on generated in the Major Incident Control<br />
Room must be recorded on a Major Incident Task Form. The message sender records the task<br />
on the first section of the form (if the message comes from an external source e.g.<br />
email/telephone, any control room staff member records the message in this first section with<br />
the senders details); and then passes the task form to the Major Incident Room Coordinator who<br />
then deals with/or allocates to the task to a person to manage who then completes the message<br />
receiver section of the form. Once the task has been deal with the task form is then passed to<br />
the Major Incident Room Coordinator who records the time it was completed and then places it<br />
into the filing box.<br />
REPORTING TEMPLATES Page 76
• Incident Log Sheet<br />
Distinguishes between communications and decisions that are made during the <strong>incident</strong>.<br />
Therefore all general communications or conversations that take place or staffing<br />
entering/leaving the room should be recorded on an Incident Log Sheet. There would be log<br />
forms for each position. If a task is communicated and recorded on this form a Major Incident<br />
Task Form must be completed to ensure that it has been dealt with.<br />
• De-briefing Template<br />
This is the generic template used by all <strong>NHS</strong> Trusts in capturing all information following an<br />
Incident. This information will be used to capture all outcomes and actions, with further<br />
recommendations that can be used to enhance the Major Incident process, driven by a Action<br />
Plan to develop these.<br />
REPORTING TEMPLATES Page 77
COMPLETED EXAMPLE<br />
Major Incident Notification Form - Page 1<br />
Time/Date Received: 12.25pm/ 12 th Dec XX Actions:<br />
Callers Name: Alan Smith<br />
Callers Title / Dept: PC/ Bournemouth<br />
CallersAddress: Bournemouth Police Station<br />
Contact Number: 01202 123456<br />
CHALETS REPORT<br />
If there is any doubt about the authenticity of the call, the alert must be verified by calling a<br />
recognised number for the alerting body.<br />
C Casualties Number of fatalities; number injured<br />
H Hazards<br />
Actual or potential hazards at the scene, any concerns about<br />
contamination, toxic smoke. Any evacuation, if so, where to.<br />
A Access Rendezvous point and any restriction<br />
L Location Location of the emergency, as precise as possible.<br />
E Emergency Services<br />
Which emergency services are present and potential future<br />
needs? Who is in command?<br />
T Type Nature of the <strong>incident</strong>, for example, <strong>major</strong> fire, building collapse.<br />
S Start Log of Actions Begin to record your actions in the Log Book NOW!<br />
Name: Adam Abc Date: 12.25pm<br />
Position: On-Call Senior Manager Time: 12 th Dec XX<br />
Call Transferred to: (Duty Manager / Emergency Planning Lead)<br />
REPORTING TEMPLATES Page 78
Major Incident Notification Form - Page 1<br />
Time/Date Received: Actions:<br />
Callers Name:<br />
Callers Title / Dept:<br />
Callers Address:<br />
Contact Number:<br />
CHALETS REPORT<br />
If there is any doubt about the authenticity of the call, the alert must be verified by calling a<br />
recognised number for the alerting body.<br />
C Casualties<br />
H Hazards<br />
A Access<br />
L Location<br />
E Emergency Services<br />
T Type<br />
S Start Log of Actions<br />
REPORTING TEMPLATES Page 79
Name: Date:<br />
Position: Time:<br />
Call Transferred to: (Duty Manager / Emergency Planning Lead)<br />
ORGANISATION<br />
Primary Care Trusts<br />
Somerset<br />
Bournemouth and Poole<br />
<strong>Dorset</strong><br />
Bath and North East Somerset<br />
North Somerset<br />
Bristol<br />
South Gloucestershire<br />
Gloucestershire<br />
Swindon<br />
Wiltshire<br />
Devon<br />
Torbay<br />
Plymouth<br />
Cornwall<br />
Mental Health<br />
<strong>NHS</strong> Trusts and Primary Care Trusts<br />
<strong>Dorset</strong> HealthCare<br />
North <strong>Dorset</strong><br />
Somerset Partnership<br />
Cornwall Partnership<br />
Devon Partnership<br />
Avon and Wiltshire<br />
Gloucestershire Partnership<br />
Acute <strong>NHS</strong> Trusts<br />
Poole Hospital<br />
Taunton and Somerset<br />
Major Incident Notification Form - Page 2<br />
MESSAGE PASSED TO<br />
INFORMED TIME AND<br />
DATE<br />
YES NO<br />
PERSON INFORMED<br />
REPORTING TEMPLATES Page 80
The Royal Bournemouth and Christchurch<br />
Hospitals<br />
West <strong>Dorset</strong> General Hospitals<br />
Yeovil District Hospital<br />
Northern Devon<br />
Plymouth Hospitals<br />
Royal Cornwall<br />
Royal Devon and Exeter<br />
South Devon<br />
Gloucestershire Hospitals<br />
North Bristol<br />
Royal National Rheumatic<br />
Royal United Hospital Bath<br />
Salisbury Health Care<br />
Swindon and Marlborough<br />
United Bristol<br />
Weston Area Health<br />
Ambulance <strong>NHS</strong> Trusts<br />
Great Western Ambulance<br />
South Western Ambulance<br />
Department of Health<br />
Other<br />
Major Incident Notification Form - Page 3<br />
REPORTING TEMPLATES Page 81
Organisation(s):<br />
SHA, Trust, Hospital(s)<br />
Pre-Hospital<br />
Hospital<br />
Total<br />
P1<br />
CBRN (chemical, biological, radiological & nuclear)<br />
Substance(s) (description)<br />
Antidote(s) (description)<br />
Definitions<br />
P1: Casualties requiring immediate<br />
life-saving resuscitation and/or<br />
surgery<br />
Qu.<br />
Ans.<br />
Qu.<br />
SITREP<br />
DH SITUATION REPORT (RESPONSE Phase)<br />
Note: Please do not leave any blank<br />
boxes. If there is nothing to report, or the<br />
information request is not applicable,<br />
please insert nil or n/a<br />
Version: Incident + hr [version no.]<br />
Date:<br />
Time:<br />
Casualties<br />
P2 P3 Other<br />
Decontaminated<br />
Not Decontaminated<br />
Patients receiving antidotes<br />
Total<br />
Critical Information Requests<br />
P1<br />
Total<br />
P2 P3 Other Total<br />
REPORTING TEMPLATES Page 82
P2: Stabilised casualties needing<br />
early surgery but delay acceptable<br />
P3: Casualties requiring treatment<br />
but a longer delay is acceptable<br />
Other: Please Specify<br />
Ans.<br />
Qu.<br />
Ans.<br />
Qu.<br />
Ans.<br />
PRESSURES AND COPING STRATEGIES (inc. inter-organisation, inter-region and nationally agreed mutual aid arrangements)<br />
Pressure<br />
Coping Strategy<br />
Pressure<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
of which (optional if available)<br />
Coping Strategy<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
CLINICAL SERVICES AND CARE (primary, secondary & tertiary care including ambulance services)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
PRIMARY SERVICES AND CARE (including ambulance services)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
REPORTING TEMPLATES Page 83
Pressure<br />
Coping Strategy<br />
Pressure<br />
Coping Strategy<br />
Pressure<br />
Coping Strategy<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
SECONDARY SERVICES AND CARE (including ambulance services)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
TERTIARY SERVICES AND CARE<br />
Immediate Forward Look / Predictions<br />
SUPPORTING INFRASTRUCTURE (inc. bed capacity, communications, built environment etc.)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
REPORTING TEMPLATES Page 84
Pressure<br />
Coping Strategy<br />
Pressure<br />
Coping Strategy<br />
Pressure<br />
Coping Strategy<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
SUPPORTING SUPPLIES (primary, secondary & tertiary care)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
WORKFORCE<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
AUXILIARY SERVICES (inc. catering, laundry, business services etc.)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
REPORTING TEMPLATES Page 85
Pressure<br />
Coping Strategy<br />
Strategy & Key Messages<br />
Pressure<br />
Coping Strategy<br />
Major Incident Line (24hr): 0845 000<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
SUPPORTING UTILITIES (electricity, gas, water & sewage, petrochemicals and waste)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
COMMUNICATIONS & MEDIA STRATEGY (inc. public health messages)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
ONGOING INCIDENTS (impact on health response)<br />
Immediate Forward Look / Predictions<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Return to DH Major Incident Control Centre<br />
(MICC)<br />
Email:(Spoc-ccm@dh.gsi.gov.uk)<br />
Fax:0207 210 5899<br />
Major Incident Line (24hr):0845 000 555<br />
REPORTING TEMPLATES Page 86
UNCLASSIFIED<br />
CRIP<br />
CRIP #1<br />
Common Recognised Information Picture<br />
Situation Cell<br />
Date & Time<br />
REPORTING TEMPLATES Page 87
THIS BRIEFING WILL COVER<br />
CRIP # - Time and Date REPORTING TEMPLATES Page 2 88
SITUATION - Overview<br />
CRIP # - Time and Date Page 3<br />
REPORTING TEMPLATES Page 89
KEY NEW DEVELOPMENTS<br />
CRIP # - Time and Date<br />
Overview<br />
REPORTING TEMPLATES Page 90
What is the crisis?<br />
CRIP # - Time and Date Page 5<br />
REPORTING TEMPLATES Page 91
INCIDENT SUMMARY<br />
SITUATION- INCIDENT #<br />
CURRENT/OPERATIONAL RESPONSE<br />
CURRENT/OPERATIONAL RESPONSE<br />
RISK ASSESSMENT<br />
FORWARD LOOK<br />
CRIP # - Time and Date Page 6<br />
REPORTING TEMPLATES Page 92
RESPONSE – Other Issues<br />
CRIP # - Time and Date Page 7<br />
REPORTING TEMPLATES Page 93
RESPONSE – Recovery/Remedial Action<br />
• Details of agency(s) responsible<br />
CRIP # - Time and Date Page 8<br />
REPORTING TEMPLATES Page 94
OTHER ISSUES / IMPLICATIONS<br />
CRIP # - Time and Date Page 9<br />
REPORTING TEMPLATES Page 95
POLITICAL / POLICY IMPLICATIONS<br />
CRIP # - Time and Date Page 10<br />
REPORTING TEMPLATES Page 96
Media<br />
MEDIA HANDLING AND PRESENTATIONAL ISSUES<br />
Forthcoming Statements / Press Conferences<br />
REPORTING TEMPLATES Page 97
CRIP # - Time and Date<br />
DECISIONS TO BE TAKEN<br />
CRIP # - Time and Date REPORTING TEMPLATES Page Page 12 98
Major Incident Task Form<br />
REPORTING TEMPLATES Page 99
Incident Log Sheet<br />
REPORTING TEMPLATES Page 100
Debrief Template<br />
Section 1: Basic Information<br />
Your Name: Date:<br />
Area/Location:<br />
Emergency / Incident:<br />
Date of <strong>incident</strong>:<br />
When was your last <strong>major</strong> <strong>incident</strong> training: ___________________________________<br />
Section 2: Activation<br />
Q1: How did you find out about the emergency? (i.e. news report, called out by LA / emergency<br />
services?)<br />
Q1(a): What time did you find out about the emergency?<br />
Q2: How was your response activated? (i.e. who called you out? Was it through usual call-out<br />
process, proactive call by authorities?..)<br />
Section 3: Your response<br />
Q3: What did you do? (summary including your key decisions made)<br />
Q4: What resources did you use?<br />
Vehicles<br />
People<br />
Equipment<br />
Section 4: Evaluation of response<br />
Q5: What went well?<br />
Q6: What might you do differently another time?<br />
Q7: What specific lessons can we learn?<br />
REPORTING TEMPLATES Page 101
Practicalities: (Any lessons about buildings, equipment, internal and external communication<br />
channels, timing/sequencing?)<br />
Internal co-ordination: (lessons about our own management & co-ordination within the PCT/<strong>NHS</strong> eg<br />
between departments/ regional and local/ staff & GPs etc)<br />
Relationships with external organisations/ individuals: (who did we need to engage with? Were the<br />
relationships already sufficiently in place? Are there new relationships to develop as a result?<br />
Opportunities for better co-ordination?)<br />
Contact with general public: (email, phone calls & impact of media activity?)<br />
Staff and volunteer support needs: (practical, information / comms, developmental?)<br />
Implications for other business: (issues around backfilling pre-<strong>plan</strong>ned activity/ normal work?)<br />
Pre-<strong>plan</strong>ning: (did you have protocols or <strong>plan</strong>s in place for the operation you undertook? Did you<br />
follow them? Were there gaps that should be addressed in future <strong>plan</strong>s?)<br />
Q8: Do you have any immediate needs/concerns that need to be addressed?<br />
Q9: Any comments on external partner response?<br />
Section 5: Other comments<br />
Q10: Any other comments or observations not covered elsewhere?<br />
REPORTING TEMPLATES Page 102
PART FIVE<br />
MAJOR INCIDENT<br />
ROOM SET-UP<br />
This section provides an<br />
overview of the assets and<br />
equipment within the <strong>major</strong> room<br />
required in support of the Major<br />
Incident Management Team’s<br />
role, and those procedures to<br />
set-up this equipment<br />
MAJOR INCIDENT<br />
CONTROL ROOM SET UP<br />
Page 103
This page is intentionally blank<br />
MAJOR INCIDENT<br />
CONTROL ROOM SET UP<br />
Page 104
1. CANFORD HOUSE<br />
Background<br />
1.1 The decision by the On-Call Duty Manager to implement the Major Incident Plan may require the<br />
formation of a Major Incident Management Team (MIMT) and the opening of the Major Incident<br />
Room.<br />
1.2 The Major Incident Control Room is located at:<br />
Major Incident Room<br />
Meeting Room One, <strong>NHS</strong> Bournemouth and Poole, Canford House, Discovery Court, 551 – 553<br />
Wallisdown Road, Poole, <strong>Dorset</strong>, BH12 5AG<br />
1.3 The following Communications are used within this location in order to support the MIMT:<br />
1.4 TELEPHONE LINES – 6 live network points allocated to the room<br />
Major Incident 1 01202 541630<br />
Major Incident 2 01202 541631<br />
Major Incident 3 01202 541632<br />
Major Incident 4 01202 541633<br />
Major Incident 5 01202 541634<br />
Major Incident 6 01202 541635<br />
1.5 RED TELEPHONE PHONES – (Emergency Contingency Telephones)<br />
1.6 FAX LINES<br />
Major Incident 1 01202 524910 – Major Incident Room<br />
Major Incident 2 01202 533825 – Major Incident Room<br />
Major Incident 3 01202 532545 – Major Incident Room<br />
Major Incident 4 01202 529562 – Major Incident Room<br />
Major Incident 5 01202 516112 – Chief Executive’s Office<br />
Major Incident 6 01202 530429 – Training Room 1<br />
Incoming Fax: 01202 541636<br />
Outgoing Fax: 01202 541637<br />
1.7 SATELLITE TELEPHONE<br />
Sim: 898709907412316030<br />
Tel No: 00 870 772 215 615<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 105
1.8 EMAIL ADDRESS<br />
Major.<strong>incident</strong>@bp-pct.nhs.uk<br />
(Username – <strong>major</strong>.<strong>incident</strong>/ Password – Pa55word)<br />
2. CONFIGURATION OF COMMUNICATION ASSETS IN THE MAJOR INCIDENT ROOM<br />
Key Name Type Box Phone Number<br />
1 Red Phone 1 Red Phone 69-3 01202 533825<br />
Role<br />
IT Lead<br />
2 Red Phone 2 Red Phone 52-3 01202 529562 SPRIG Lead<br />
3 Red Phone 3 Red Phone 52-1 01202 532545<br />
Major Incident Room<br />
Manager<br />
4 Red Phone 4 Red Phone 52-2 01202 524910 Comms Lead<br />
5 Major Incident 5 Desk Phone 69-1 01202 541634 IT Lead<br />
6 Major Incident 2 Desk Phone 75-2 01202 541631 Admin Support<br />
7 Major Incident 1 Desk Phone 75-1 01202 541630 Comms Lead<br />
8 Major Incident 4 Desk Phone 75-4 01202 541633 SPRIG lead<br />
9 Major Incident 3 Desk Phone 75-3 01202 541632 Incident Room Manager<br />
10 Major Incident 6 Desk Phone 75-5 01202 541635 PH Lead<br />
11 Major Incident 7 Desk Phone 75- 6 01202 541655 HR Lead<br />
12 Major Incident 8 Desk Phone 52-5 01202 541658<br />
13 No Laptop Data Port Only 69-2 N/A IT Lead<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Major Incident Room Coordinator<br />
14 Laptop Data 82 N/A Admin Support<br />
15 Laptop Data 82 N/A Comms Lead<br />
16<br />
Laptop<br />
Data 82 N/A<br />
17 Laptop Data 82 N/A HR Lead<br />
Major Incident Room<br />
Manager<br />
18 Laptop Data 82 N/A SPRIG Lead<br />
19 Laptop Data 52-4 N/A Room Co-ordinator<br />
Page 106
Key Name Type Box Phone Number Role<br />
20 Laptop Data 62-6 N/A Smart Board<br />
21 Laptop Data 52-6 N/A Public Health Lead<br />
22 Fax In Analogue 62-1 01202 541636<br />
23 Fax Out Analogue 62-2 01202 541637<br />
24<br />
Meeting Room<br />
Phone Wall Phone 62-3 01202 541411<br />
25 Printer Data 62-4 WALLP1303<br />
26 TV-PC TV-PC 62-5 TV-PC<br />
27 RED PHONE RED PHONE 73-3 01202 530429 Based in Training Room 1<br />
2.1 The above communications assets are to be configured in relation to the below floor diagram, with<br />
identified assets numbered (in red) in relation to where they are to be placed within the room:<br />
2.2 Other Rooms to be utilised: The Major Incident Room can provide the focal point for all liaison,<br />
co-ordination and control matters. However, there are other rooms allocated in the event of a<br />
Major Incident Room for other functions. They are as follows:<br />
Function Room<br />
Major Incident Reception Canford House Reception<br />
Internal Communications and Media Room Meeting Room 4<br />
Rest Room Meeting Room 3<br />
HR Room Meeting Room 2<br />
3. ARRIVAL PROCEDURES - OUT OF HOURS<br />
3.1 On arrival at Discovery Court, you must carry out the following:<br />
• Enter the Discovery Court estate by entering the security code – 7586.<br />
• Enter the Canford House using the side or rear door using your allocated swipe card;<br />
• Make your way to the PCT Reception Room;<br />
• Start the set up of the Major Incident Room;<br />
• Contact relevant PCT staff to complete the MIMT, including a IT representative to assist in the<br />
assembling of the Major Incident Room;<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 107
• Contact Admin and IT personnel to assist with the set-up of the Major Incident Room;<br />
• Consider the need for additional personnel to support the MIMT Team;<br />
• Notify the Major Incident community that the MIMT Team has assembled and provide relevant<br />
phone and fax numbers and e-mail addresses.<br />
4. PROCEDURE FOR SETTING UP THE MAJOR INCIDENT ROOM (MEETING ROOM 1)<br />
GO TO RECEPTION<br />
• Make your way to the PCT Reception Room to acquire the keys to the Major Incident Room<br />
cupboards;<br />
• Enter the Reception Room by using the left hand door to the Reception. The door will be open<br />
with the key in the door;<br />
• Under the counter on the right hand side is the key press (small grey box). This is locked. The key<br />
is contained within the pedestal in the top drawer on the far right of the reception desk (below the<br />
key press);<br />
• Collect both cupboard keys on number 15 to the Major Incident Room cupboards;<br />
• Collect the Major Incident Room door key and cupboard keys from the reception key box (small<br />
grey box). Out of hours this key box will be locked; the key to the key box is kept in the top drawer<br />
on the far right of the reception desk (below the key box);<br />
GO TO THE MAJOR INCIDENT ROOM (MEETING ROOM 1)<br />
• Open the cupboards and locate the room <strong>plan</strong> attached to the inside of the doors (see below<br />
Major Incident Room Layout. The content of each cupboard is labelled to make things easier to<br />
find;<br />
• Move all chairs to the sides of the room and move tables by holding onto the black parts so they<br />
do not collapse;<br />
• Set up the laptops, phones, faxes and connect a laptop to the smart board. If the laptop<br />
connected to the Smart Board does not display on-screen, right click on the desktop, select<br />
‘Graphics Properties’, and lick ‘Intel Clone Dual Display’ and click ‘OK’ to confirm. IT can be<br />
contacted via the helpdesk if support is required. NB the cables for faxes and phones are colour<br />
coded – ensure the colours are matched when connecting them;<br />
• Set out the 2 x logbooks, trays, paper, pens etc from cupboard as appropriate;<br />
• Switch on the wide screen televisions on the wall to show BBC news and Sky News- turn the<br />
volume down and put on subtitles (remotes are located in the cupboard);<br />
• Display ‘please be quiet’ signs in corridor and on MI room door. Use other signs to illustrate<br />
seating <strong>plan</strong> as appropriate;<br />
• Display contact number laminates prominently on walls;<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 108
• Key for vending machine is located in the cupboard.<br />
MIMT REQUIREMENTS<br />
• Once the MIMT is assembled, establish all the known facts of the <strong>incident</strong>;<br />
• Open a Major Incident Log Book for Incident Director and Incident Team Manager – books are<br />
available in Major Incident Room cupboards. Loggists must maintain those Logs appointed to<br />
them for their respective role;<br />
• Identify whether there is a need for specialist input from personnel or organisations not present<br />
and alert them if required;<br />
• Establish separate rooms for the “Press Room”, HR and Rest Room, if required, and establish the<br />
necessary communications links.<br />
TELEPHONES<br />
Those telephones indicated on the following floor <strong>plan</strong> are to be arranged accordingly from those<br />
assets maintained within the MI Room cupboard.<br />
STATIONERY<br />
There are adequate supplies within the MI Room Cupboard. Trays, pens and notebooks should<br />
be given to each role listed on the following floor <strong>plan</strong>.<br />
TABLES AND CHAIRS<br />
The current set up in Meeting Room 1 is to be broken down and re-arranged to conform to the<br />
following floor <strong>plan</strong>:<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 109
5. MAJOR INCIDENT ROOM LAYOUT<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 110
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 111
6. STANDING OPERATING PROCEDURES FOR THE SET UP OF ALL TECHNICAL AND<br />
COMMUNICATION ASSETS<br />
6.1 The following Standing Operating Procedures are to be used in the setting up of the following key<br />
technical and communication assets:<br />
• Operating Procedures for Incident Room Laptops<br />
• Operating Procedures for Major Incident Television<br />
• Operating Procedures for the Major Incident TV PC<br />
• Operating Procedures for Major Incident Telephones<br />
• Operating Procedures for Major Incident Smart Board<br />
• Operating Procedures for Explorer 300 Satellite Phone<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 112
Operating Procedures for Incident Room Laptops<br />
This Operating Procedure outlines the key functions of the Major Incident Room Laptops. If you<br />
believe that this laptop is malfunctioning, contact the On Call IT on 01202 854445<br />
1. To Log on to Incident Room Laptops<br />
1. All MI Laptops are located in the left hand cupboard<br />
2. Turn the laptop on at the Power Button (on some Sony laptops this is located at the side of the<br />
hinge of the laptop)<br />
3. When the laptop has activated, you will need to enter a SAFEBOOT user name and password:<br />
Username: <strong>major</strong>.<strong>incident</strong> Password: Pa55word<br />
4. Press the enter button to confirm the password<br />
5. The laptop should automatically load onto Windows<br />
2. To Access the PCT Network & Internet<br />
1. Obtain a network cable from the cupboard nearest the door and connect the laptop to the live ports<br />
in the floor boxes as described in the MI Plan (Page 69)<br />
3. How to Access the PCT Network & Internet via 3G Connection<br />
1. Plug in Dongle to USB Port<br />
2. Wait for set up to complete if not already installed on laptop<br />
3. Once installed, double click on Vodafone icon on desktop<br />
4. Then click connect<br />
To access the Major Incident Account<br />
1. Connect a network cable from the laptop to the appropriate floor box (refer to MI <strong>plan</strong>)<br />
2. Click on Outlook Icon on the desktop.<br />
3. Dismiss any old Reminders<br />
4. How to Log off Major Incident Laptops<br />
1. Save and close down any applications<br />
2. Click on the Start button on the bottom left hand side of the screen<br />
3. Select the Shut Down option.<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 113
Operating Procedures for Major Incident Television<br />
This Operating outlines the key functions of the Television. If you believe that the TV is malfunctioning,<br />
contact the On Call IT 01202 854445.<br />
1. To Switch on the Television<br />
1. Press the power on button both remotes, the TV’s should switch on to the last channel that it was<br />
on.<br />
2. How to view a TV Channel<br />
1. Essential channels that may be needed during an <strong>incident</strong> are as follows:<br />
BBC 1 Channel 1<br />
BBC 2 Channel 2<br />
ITV Channel 3<br />
Channel 4 Channel 4<br />
BBC News 24 Channel 80<br />
Sky News Channel 82<br />
2. To select a channel, press the corresponding TV channel number and the channel will appear on<br />
the screen.<br />
3. To activate the TV subtitles<br />
1. The TV should remain on mute unless essential. To activate the subtitles, press the subtitles<br />
button. This will then allow those in the <strong>incident</strong> room to keep an eye on the media information<br />
and highlight anything essential to the <strong>incident</strong> manager.<br />
4. To listen to the radio<br />
1. The radio channels are as follows:<br />
BBC Radio 2 Channel 702<br />
BBC Radio 4 Channel 704<br />
BBC Radio 1 Channel 700<br />
2. To select the radio station that you need, press the TV channel number and the TV will switch to<br />
the radio station.<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 114
5. To tune the TV<br />
1. Press OK<br />
6. To turn off the TV<br />
**The TV pops up saying new DVB services found**<br />
1. Press the power button the remote and the TV will go into the standby mode.<br />
1. To connect the TV and the PC<br />
Operating Procedures for Major Incident TV-PC<br />
1. Retrieve the PC from the MI cupboard on the left (nearest to Door), the PC-TV keyboard and<br />
Mouse and TV remote.<br />
2. Plug Power cord for PC into floor box, use extension lead if needed and connect network cable<br />
from PC to floor box then plug the mouse into the back of the PC.<br />
3. Plug in the ‘Bizz Link’ to the PC which is located on the top of the PC when collecting items from<br />
the cupboard connect this with the white lead from the TV.<br />
4. Switch PC on and TV on, go to channel HDMI using the AV button on the TV remote.<br />
Operating Procedures for Major Incident Telephones<br />
This Operating Procedure outlines how to set up the Major Incident Room Telephones. If you believe<br />
that the telephones are malfunctioning, contact the On Call IT 01202 854445<br />
1. To Plug in and set up the Telephones<br />
1. Open the Major Incident Room Cupboard nearest the window to obtain both black and red<br />
phones (dedicated lines)<br />
2. Refer to the Major Incident Plan room set up (page 70) to locate which phones connect to which<br />
floor boxes.<br />
2. To make a call<br />
Internal telephone calls (black phones only)<br />
1. To make an internal telephone call, dial the extension (last 3 digits) of the person you wish to call.<br />
External telephone calls<br />
1. To make an external telephone call, dial 9 for an outside line and then the full contact number<br />
including the area code.<br />
2. If you know the name of a <strong>NHS</strong> person you wish to contact you can search for the number on the<br />
global system in outlook<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 115
Operating Procedures for Major Incident Smart Board<br />
This Operating Procedure outlines the key functions of the SMART Board. If you believe that the SMART<br />
board is malfunctioning, contact the IT On Call 01202 854445.<br />
1. How to turn on the SMART Board<br />
1. Turn on the power at the bottom left of the Smart Board, this will turn on the projector and Smart<br />
Board.<br />
2. Connecting Laptop to SMART Board<br />
1. Get the laptop labelled ‘Smart Board Laptop’ (asset number 1217) from the cupboard<br />
2. Get VGA cable out of cupboard and connect this to VGA port on laptop and smart board<br />
connector – located under the power button of smart board<br />
3. If the display does not come up on the screen: right click on desktop, click graphics properties,<br />
select dual display clone, and click OK<br />
4. Connect USB cable to the right hand side of the Smart Board to a free USB slot on laptop – Smart<br />
Board light on the left hand side should go green<br />
5. If Smart Board light does not go green, click on Smart Board icon in tool bar, click control panel,<br />
then smart board connection wizard – then follow wizard<br />
6. If you want Audio connect the 3.5mm Jack Cable from the laptop headphone port to the smart<br />
board. The speaker switch is in the left hand corner of the room (by the window) then switch the<br />
individual speakers on<br />
3. Tips<br />
1. Orientation of Smart Board<br />
If you touch the board as you are interacting with it and the cursor is more than an inch away from<br />
where you have pointed you will need to re orientate the board to do this you:<br />
- Right Click on the Smart Board Icon<br />
- Click Orient<br />
- Point at the markers (follow on screen Instructions<br />
2. Interact with the smart board by touching the screen to move the mouse and using the buttons on<br />
the front as you would on a mouse.<br />
3. Use the coloured pens to write or draw on the board, only using one at a time so that the board<br />
can pick up the sensors<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 116
4. Use the eraser to delete any writing or drawings made by the electronic pens, alternatively you<br />
can double tap the screen and this will clear all<br />
5. Use the control panel located on the left hand side of the screen to access all the icons.<br />
4. How to Log off the SMART board<br />
1. To close down the computer system, click start and then shut down as you would your PC.<br />
2. Unplug all leads<br />
3. Switch of the smart board at the power button, press again to turn off completely<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 117
Background<br />
Operating Procedures for Explorer 300 Satellite Phone<br />
This Operating Procedure outlines the key functions of the Satellite Phone. If you believe the Sat Phone<br />
is malfunctioning, contact the On Call IT 01202 854445<br />
1. To Switch on Satellite Phone<br />
1. To switch on the EXPLORER 300, push the Power button next to the display and hold it down<br />
until the green Power indicator lights up. It normally take a few seconds<br />
2. To Start using the Satellite Phone<br />
1. Enter the PIN and then point the antenna towards the satellite, take this outside at sit the phone<br />
on the wall by reception pointing towards the buildings ahead.<br />
2. Once the single strength is good , showing READY you can make a call:<br />
00 followed by # or off-hook key (# on analogue phones, offhook<br />
key on Bluetooth handsets).<br />
Please refer to the user manual kept in the MI Room Cupboard for more detailed information on<br />
the use of the Explorer 300 Satellite Phone.<br />
3. Our PCT Satellite Phone Number is 00870772215615<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 118
Establishing a Major Incident Control Room at VESPASIAN HOUSE<br />
ESTABLISH INCIDENT CONTROL ROOM<br />
This action card lists the actions to bring the Incident Control Room to operational readiness and is<br />
available in the control room.<br />
Vespasian House can provide an alternate location to Canford House for <strong>incident</strong> control and is<br />
located at:<br />
<strong>NHS</strong> <strong>Dorset</strong> PCT located at Vespasian House, Bridport Road, Dorchester, <strong>Dorset</strong>, DT1 1TS on the<br />
3 rd floor East in the Public Health Department.<br />
A as below:<br />
Telephone Number: 01305 36 8955<br />
Back up Number: 01305 XXXXX (back up analogue line)<br />
Mobile: XXXXXXX (back up mobile line)<br />
The On Call Manager will have 24 hour a day, 7 day a week swipe card access to all areas they can<br />
access in hours, through their <strong>NHS</strong> <strong>Dorset</strong> ID swipe card if they hold one. They will also have an<br />
alarm fob to disable to the alarm on each floor.<br />
Enter the Public Health Department using your ID card and disable to the alarm using your fob on<br />
the left hand side inside the door.<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 119
Step 1- Provision of Equipment<br />
No. Action: Done?<br />
Turn left and enter room 16, locate the control room on the left hand side, the desks<br />
and laptop computers and screens will already be set up for you as follows:<br />
Locate the equipment cupboards and open up the role boxes, where possible in<br />
order. These contain the action cards and associated equipment for each role to be<br />
carried out. Role boxes are checked monthly. Each box contains the following<br />
items:<br />
Role action card outlining the initials responsibilities and actions the person<br />
allocated to this role should carry out<br />
A high visibility vest in order to easily identify individuals directly involved in<br />
a response<br />
Log in information for IT, this information is also included in this <strong>plan</strong><br />
A log book or log sheets/task forms to record communications, actions and<br />
decisions of the post holder<br />
Black pens, only black pens should be used to record information during an<br />
<strong>incident</strong> as this will photocopy well should this be necessary at a later date<br />
A torch<br />
A mug<br />
Antibacterial hand gel<br />
Bottle of water<br />
Blackberry charger<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 120
Locate the spare equipment box to gain access to:<br />
Hard copy of this <strong>plan</strong><br />
Spare supplies including digital camera<br />
Spare log books<br />
Satellite phone<br />
Maps<br />
Pens<br />
First Aid Kit<br />
Chargers<br />
Battery Operated Lights<br />
Set up:<br />
- The Smart board should be set up to record important overview information for the<br />
Silver PCT<br />
- Printers switched on<br />
- Plotter switched on<br />
- Switch on the TV’s (Sky News and BBC News)<br />
Step 2 – Check the telephones<br />
No. Action: Done?<br />
Switch on and check the Major Incident telephones<br />
Numbers are:<br />
Incoming Telephone Number: 01305 36 8955<br />
Back up Number: 01305 XXXXX (back up analogue line)<br />
Mobile: XXXXXXX (back up mobile line)<br />
Fax: XXXXXXX<br />
Satellite phone (don’t waste time getting a signal inside, just switch it on an get it<br />
charged – user instructions in the appendix) :<br />
Voice: 00870 7722 15623<br />
Data: 00870 7822 14475<br />
Fax: 00870 7822 14476<br />
The telephones have the following numbers:<br />
• 3545<br />
• 3546<br />
• 3547<br />
• 3548<br />
• 3581<br />
• 3582<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 121
Dial 9 for an outside line as normal.<br />
Step 3 – Switch on the laptops<br />
No. Action: Done?<br />
Switch on the laptops and screens and log as follows<br />
Web based Incident email account:<br />
Web address: https://webmail.dshc.nhs.uk<br />
Domain/User name: nhsdorset.control<br />
Password: Pa55word<br />
In the event of a power failure you can take the laptops to the fallback control at<br />
Candford or <strong>Dorset</strong> County Council, at the Emergency Control Centre in<br />
Dorchester.<br />
Step 4 – Log on to <strong>NHS</strong> mail<br />
No. Action: Done?<br />
It may be necessary to cascade public health alerts or other important information<br />
to GP Practices. This can be done using the <strong>NHS</strong> Mail account. In the event that<br />
the PCT network is unavailable, you should use the <strong>NHS</strong> Mail back up email<br />
address.<br />
Log on to <strong>NHS</strong>mail at www.nhs.net<br />
Username Password<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 122
<strong>incident</strong>s.dorset Pa55word<br />
Email address is <strong>incident</strong>s.dorset@nhs.net<br />
The <strong>NHS</strong>mail account has email and fax numbers for all Practices in the <strong>Dorset</strong><br />
area in order to facilitate the quick dissemination of urgent information.<br />
If you need help with the account contact the <strong>NHS</strong>mail helpdesk on 0333 200 1133<br />
(this number is available 24 hours a day, every day of the year).<br />
Step 5 – Log into/onto info gathering<br />
No. Action: Done?<br />
The following should be logged onto:<br />
- ToxBase<br />
- Met Office Weather warning system<br />
- National Resilience Extranet (if in use)<br />
- CLIO <strong>Dorset</strong> Police <strong>incident</strong> reporting<br />
- Click SMS (see user card on desk or on call protocol cards)<br />
Emergency Response Sub Directory<br />
o The Emergency Response subdirectory is located on the Vespasian<br />
server at X:\Emergency Response Planning. Copies of <strong>plan</strong>s<br />
including templates are located here.<br />
o This subdirectory also has a Data subdirectory within it which can be<br />
used for saving documents created using the ‘nhsdorset.control’<br />
username. Please note that other usernames will not be able to save<br />
to this area of the Vespasian servers, so if you have logged in using<br />
your own username you will need to save files to your own area of<br />
the server.<br />
Step 6 – Running the <strong>incident</strong><br />
No. Action: Done?<br />
Open the role boxes and ensure that staff are wearing their jackets<br />
Ensure that you resource the control room as needed with staff – and allocate a<br />
person to resourcing and use the whiteboard to record availability from information<br />
gathered from SMS and telephone calls and take photographs of this board on a<br />
regular basis using the digital camera<br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 123
Start using the Major Incident Action Cards for each role as appropriate during the<br />
<strong>incident</strong><br />
MAJOR INCIDENT ROOM<br />
SET UP<br />
Page 124
PART SIX<br />
APPENDICES<br />
APPENDICES Page 125
APPENDICES Page 126
Sainsbury’s assistance policy<br />
APPENDICES Page 127
APPENDICES Page 128
APPENDICES Page 129
Usage<br />
SATELLITE PHONE USER INSTRUCTIONS<br />
o The following are examples of where use of this equipment may be appropriate:<br />
During a failure of conventional landline and mobile telephone networks;<br />
Where a remote control point needs to be established and where no other phone<br />
networks are available. For example, establishing a rest centre in a village hall with no<br />
land telephone and where mobile telephone networks cannot get a signal.<br />
o This telephone is stored in the Emergency Planning cabinet in Public Health, Level 3 East in<br />
Vespasian House.<br />
Setting up the Satellite Phone<br />
o The unit is regularly charged, but prior to use in a location without power it should be charged<br />
up by plugging it into the mains for a period. To recharge, connect the power supply to the<br />
dish, and plug into a normal mains electric socket. (Once recharged the unit can be operated<br />
without mains supply.)<br />
o Connect the handset to the dish. Sockets are located on the left hand side of the unit and<br />
marked.<br />
o Position the unit where it has a clear line of sight to the horizon in a south easterly<br />
direction, and angle it at approximately 25 degrees above the horizon. Buildings, trees, and<br />
window frames will block the signal.<br />
o Switch on the phone. The on switch is located on top of the unit.<br />
o After the start-up procedure is complete, the unit will start to bleep whilst it searches for a<br />
satellite signal. Once it has located the satellite it will register. The received signal strength is<br />
shown on the display on top of the unit. Move the unit slightly to left and right and change<br />
the angle up and down to receive the strongest signal.<br />
o Once a strong signal is achieved, use the handset much as a normal mobile phone.<br />
However, note that for all calls the international dialling code is required, (as the signal from<br />
the satellite is received back on earth in northern Italy.) and that each number dialled is<br />
completed with the # key. E.g.: Hillfort House is: 0044 1305 361300#<br />
o The phone can dial all landline and mobile numbers in the UK.<br />
o The satellite phone’s own numbers are as follows:<br />
Voice: 00870 7722 15623<br />
Data: 00870 7822 14475<br />
Fax: 00870 7822 14476<br />
APPENDICES Page 130
Example of an <strong>incident</strong> site<br />
APPENDICES Page 131