Orthopedic Coder's Pink Sheet - DecisionHealth Store
Orthopedic Coder's Pink Sheet - DecisionHealth Store
Orthopedic Coder's Pink Sheet - DecisionHealth Store
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
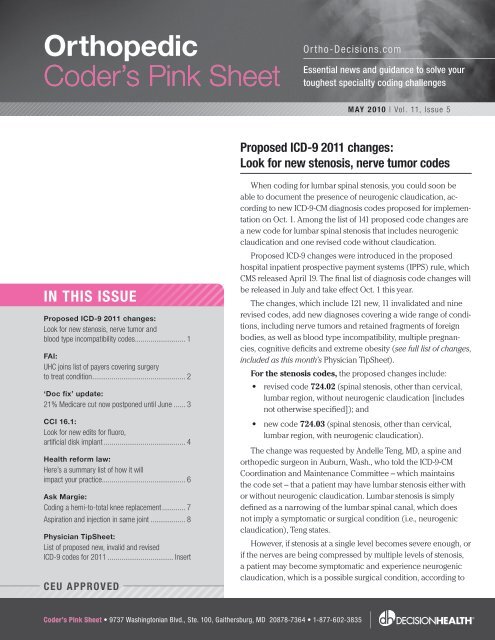
<strong>Orthopedic</strong><br />
Coder’s <strong>Pink</strong> <strong>Sheet</strong><br />
In ThIs Issue<br />
Proposed ICD-9 2011 changes:<br />
Look for new stenosis, nerve tumor and<br />
blood type incompatibility codes .......................... 1<br />
FAI:<br />
UHC joins list of payers covering surgery<br />
to treat condition ................................................ 2<br />
‘Doc fix’ update:<br />
21% Medicare cut now postponed until June ...... 3<br />
CCI 16.1:<br />
Look for new edits for fluoro,<br />
artificial disk implant .......................................... 4<br />
Health reform law:<br />
Here’s a summary list of how it will<br />
impact your practice ........................................... 6<br />
Ask Margie:<br />
Coding a hemi-to-total knee replacement ............ 7<br />
Aspiration and injection in same joint .................. 8<br />
Physician Tip<strong>Sheet</strong>:<br />
List of proposed new, invalid and revised<br />
ICD-9 codes for 2011 .................................. Insert<br />
Ceu APProved<br />
Ortho-Decisions.com<br />
Coder’s <strong>Pink</strong> sheet • 9737 Washingtonian Blvd., Ste. 100, Gaithersburg, MD 20878-7364 • 1-877-602-3835<br />
Essential news and guidance to solve your<br />
toughest speciality coding challenges<br />
MAY 2010 | Vol. 11, Issue 5<br />
Proposed ICd-9 2011 changes:<br />
Look for new stenosis, nerve tumor codes<br />
When coding for lumbar spinal stenosis, you could soon be<br />
able to document the presence of neurogenic claudication, according<br />
to new ICD-9-CM diagnosis codes proposed for implementation<br />
on Oct. 1. Among the list of 141 proposed code changes are<br />
a new code for lumbar spinal stenosis that includes neurogenic<br />
claudication and one revised code without claudication.<br />
Proposed ICD-9 changes were introduced in the proposed<br />
hospital inpatient prospective payment systems (IPPS) rule, which<br />
CMS released April 19. The final list of diagnosis code changes will<br />
be released in July and take effect Oct. 1 this year.<br />
The changes, which include 121 new, 11 invalidated and nine<br />
revised codes, add new diagnoses covering a wide range of conditions,<br />
including nerve tumors and retained fragments of foreign<br />
bodies, as well as blood type incompatibility, multiple pregnancies,<br />
cognitive deficits and extreme obesity (see full list of changes,<br />
included as this month’s Physician Tip<strong>Sheet</strong>).<br />
For the stenosis codes, the proposed changes include:<br />
• revised code 724.02 (spinal stenosis, other than cervical,<br />
lumbar region, without neurogenic claudication [includes<br />
not otherwise specified]); and<br />
• new code 724.03 (spinal stenosis, other than cervical,<br />
lumbar region, with neurogenic claudication).<br />
The change was requested by Andelle Teng, MD, a spine and<br />
orthopedic surgeon in Auburn, Wash., who told the ICD-9-CM<br />
Coordination and Maintenance Committee – which maintains<br />
the code set – that a patient may have lumbar stenosis either with<br />
or without neurogenic claudication. Lumbar stenosis is simply<br />
defined as a narrowing of the lumbar spinal canal, which does<br />
not imply a symptomatic or surgical condition (i.e., neurogenic<br />
claudication), Teng states.<br />
However, if stenosis at a single level becomes severe enough, or<br />
if the nerves are being compressed by multiple levels of stenosis,<br />
a patient may become symptomatic and experience neurogenic<br />
claudication, which is a possible surgical condition, according to
May 2010 <strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong><br />
Teng’s code request. Symptoms of neurogenic claudication<br />
include buttock and lower extremity cramping, pain and<br />
fatigue, exacerbated by standing erect.<br />
Nerve tumors: You’ll have two new codes in the series<br />
for neurofibromatosis (237.7), a genetic disorder that<br />
causes tumors to grow along various types of nerves and,<br />
in some cases, other tissue such as bone and muscle. In the<br />
past, there have been two classified types of neurofibromatosis,<br />
and ICD-9 codes already exist for these:<br />
• Neurofibromatosis, type 1 (von Recklinghausen’s<br />
disease) – 237.71 – is distinguished by spots and/or<br />
nodules just beneath the skin, which can also lead<br />
to enlargement and deformity of bone and scoliosis;<br />
and<br />
• Neurofibromatosis, type 2 (acoustic neurofibromatosis)<br />
– 237.72 – can lead to multiple tumors on the<br />
brain and/or cranial nerves, and often affects the<br />
auditory nerve, causing hearing loss.<br />
Now, a rare third type of neurofibromatosis has<br />
emerged, called Schwannomatosis, and the ICD-9 Committee<br />
has a proposed new code for it (273.73). The<br />
additional code was requested by the American Academy<br />
of Neurology. Patients with this disorder may have multiple<br />
tumors on cranial, spinal and peripheral nerves, but they<br />
don’t develop vestibular tumors or go deaf, as in Type 2 NF.<br />
The ICD-9 Committee also proposed a new code<br />
(273.78) for “other neurofibromatosis.”<br />
Retained foreign body fragments: A series of proposed<br />
new V-codes allow you to document when a patient<br />
has retained fragments or splinters of substances that may<br />
have become embedded in the body. The codes were<br />
requested by the Department of Defense to identify materials<br />
from bombs retained by injured soldiers; however, they<br />
may be applicable to any injury resulting in embedded fragments.<br />
They are to be used as secondary status codes to<br />
primary injury codes, according to the ICD-9 Coordination<br />
and Maintenance Committee. However, you should not use<br />
these codes to describe implanted medical devices, such<br />
as an artificial joint or pacemaker.<br />
The list of proposed new codes for retained fragments<br />
includes: depleted uranium (V90.01); other radioactive<br />
fragments (V90.09); metal, unspecified (V90.10); magnetic<br />
metal (V90.11); nonmagnetic metal (V90.12); plastic<br />
(V90.2); animal quills or spines (V90.31); retained tooth<br />
(V90.32); wood (V90.33); glass (V90.81); and stone or<br />
crystalline fragments (V90.83), among others.<br />
2<br />
Any embedded object has the potential to cause infection,<br />
the ICD-9 Committee notes. In addition, an embedded<br />
magnetic object would be a relative contraindication for an<br />
MRI exam. Other types of metal, such as lead or tungsten,<br />
can also pose long-term toxicological risks.<br />
In this update, the ICD-9 Committee proposes an additional<br />
code (V15.53), for “personal history of retained<br />
foreign body fully removed.”<br />
Other proposed new diagnosis codes include:<br />
• new V-codes for “personal history of (corrected)<br />
congenital malformations” of various body systems,<br />
including V13.68 (personal history of [corrected]<br />
congenital malformations of integument, limbs and<br />
musculoskeletal system);<br />
• V49.86 (do not resuscitate status);<br />
• three new code series that describe different<br />
blood-type incompatibilities, including ABO incompatibility<br />
(999.60-999.69), Rh incompatibility<br />
(999.70-999.74) and non-ABO incompatibilities<br />
(999.75-999.79);<br />
• new V-codes for multiple pregnancies, including<br />
twins to quads and “other specified multiple gestation,”<br />
that allow you to code for the number of<br />
placenta and amniotic sacs (V91.00-V91.99);<br />
• V-codes that allow you to code body mass index<br />
(BMI) for extremely overweight adults, from a BMI<br />
of 40 to “70 and over” (V85.41-V85.45); and<br />
• new cognitive deficit codes ( 799.50-799.59).<br />
Official rEsOurcEs:<br />
Hospital IPPS proposed rule:<br />
www.federalregister.gov/OFRUpload/OFRData/2010-09163_PI.pdf<br />
© 2010 <strong>DecisionHealth</strong> ® • www.ortho-decisions.com • 1-877-602-3835<br />
`<br />
`<br />
ICD-9-CM Coordination & Maintenance Committee:<br />
www.cdc.gov/nchs/icd/icd9cm_maintenance.htm<br />
uhC is latest payer covering FAI surgery<br />
An increasing number of private payers are electing to<br />
cover either open or arthroscopic surgery to treat femoroacetabular<br />
impingement (FAI), a painful hip condition<br />
faced by some young, active patients.<br />
Most significantly, UnitedHealthCare this spring announced<br />
it will pay for both open and arthroscopic treatment<br />
of FAI.
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> May 2010<br />
“We are all dancing around at this office,” reports Kristi<br />
Stumpf, MCS-P, CPC, COSC, ACS-OR, coding and compliance<br />
supervisor, Proliance <strong>Orthopedic</strong>s and Sports Medicine,<br />
Bellevue, Wash.<br />
“We do 10 to 12 of these cases weekly, sometimes more,”<br />
she adds. That has led to a tremendous number of appeals<br />
and an “unbelievable workload surrounding this procedure.<br />
Finally, the tides are turning for us after years and<br />
years of a complete and total nightmare!”<br />
But while orthopedic coders celebrate the new UHC<br />
policy, the battle is not over, Stumpf says. For example,<br />
even if a big insurance company says it will cover FAI, the<br />
patient’s individual plan (e.g., an employer-paid insurance<br />
plan) may decide not to pay for it, Stumpf explains. “We’ve<br />
had that happen in a couple of cases. You really have to dig<br />
all the way down,” sometimes filing two separate pre-authorization<br />
requests to nail down payment, she says.<br />
That can also work to your benefit, however. For example,<br />
even though Aetna formally has a non-coverage policy<br />
for FAI, some of its private, employer-paid plans have opted<br />
to cover it, she says.<br />
The new UHC policy does not list specific indications<br />
or conditions when FAI surgery would be covered. It states<br />
only that “the best surgical outcomes are achieved in patients<br />
who have ALL of the following:<br />
• pain unresponsive to medical management<br />
(e.g., restricted activity, nonsteroidal anti-inflammatory<br />
drugs).<br />
• moderate-to-severe persistent hip or groin pain that<br />
limits activity and is worsened by flexion activities<br />
(e.g., squatting or prolonged sitting).<br />
• positive impingement sign (i.e., sudden pain on<br />
90-degree hip flexion with adduction and internal<br />
rotation or extension and external rotation).<br />
• radiographic confirmation of FAI (e.g., pistol-grip<br />
deformity, alpha angle greater than 50 degrees, coax<br />
profunda and/or acetabular retroversion).<br />
• do not have advanced osteoarthritis (i.e., Tönnis<br />
grade 2 or 3) and/or severe cartilage damage (i.e.,<br />
Outerbridge grade III or IV).”<br />
Stumpf says the UHC FAI policy is similar to other<br />
payers’ published policies for the procedure; they are all<br />
vague. She states the condition itself may present differently<br />
in different patients – the problem doesn’t always show up<br />
on X-rays or MRIs, for example.<br />
However most FAI patients fit a distinct pattern of not<br />
being able to sit without pain because of bones abutting<br />
against soft tissue, she says. From her experience, “what<br />
payers really do want to see is that the patient did not<br />
just walk in the door and you took them right to the OR,”<br />
Stumpf explains. “They expect you to have attempted palliative<br />
care at a bare minimum.”<br />
UHC joins a growing list of commercial payers now<br />
covering surgical intervention for FAI. CIGNA, Blue Cross<br />
Blue Shield of North Carolina and Empire Blue Cross Blue<br />
Shield (New York) have recently joined the list of payers<br />
that say they will cover the procedure. Regence Blue Cross/<br />
Blue Shield (Idaho, Oregon, Utah and some counties in<br />
Washington) and First Choice of Washington were among<br />
the first payers to cover FAI surgery (see OCPS, 9/09).<br />
Medicare has no national coverage policy for FAI and<br />
lists no local coverage policies for it. FAI is generally prevalent<br />
among young, active patients, who don’t tend to be<br />
Medicare beneficiaries.<br />
Until CPT ® issues new codes for FAI surgeries (expected<br />
as early as next year), most payers are directing you to<br />
use 27299 for open treatment or 29999 for arthroscopic<br />
FAI. There is no specific diagnosis code, so you’re likely left<br />
with 718.85 (other joint derangement, NEC).<br />
Official rEsOurcEs:<br />
` Carrier FAI policies<br />
` UHC: http://tinyurl.com/UHC-FAI-Policy<br />
` CIGNA: http://tinyurl.com/CIGNA-FAI-Policy<br />
` Empire BCBS: http://tinyurl.com/EmpireBCBS-FAI-Policy<br />
` BCBS of North Carolina: http://tinyurl.com/BCBSofNC-FAI-Policy<br />
` Regence BCBS: http://tinyurl.com/RegenceBCBS-FAI-Policy<br />
President signs ‘doc Fix’ bill;<br />
21% cut averted until June<br />
President Obama signed, late on April 15, an unemployment<br />
benefits extension bill (H.R. 4851), which contained a<br />
measure postponing the sustainable growth rate (SGR) cut<br />
to Medicare reimbursements until May 31. Lawmakers in<br />
Washington must enact another pay-fix bill before June 1 to<br />
again prevent the 21% cut to physician Medicare payments.<br />
Claims with dates of service on or after April 1 had been<br />
frozen by CMS to prevent practices from being paid at the<br />
lower rate. However, that claims hold expired at midnight<br />
on April 14. Medicare contractors had just begun process-<br />
© 2010 <strong>DecisionHealth</strong> ® • www.ortho-decisions.com • 1-877-602-3835 3
May 2010 <strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong><br />
ing these claims at the lower rate when the president<br />
signed the extension bill, so the 21% cut was in effect for<br />
less than 24 hours before Congressional action reversed it.<br />
It is unclear how many claims were processed at the lower<br />
rate, but CMS previously said these claims would be reprocessed<br />
automatically in the event of a pay fix, without any<br />
need for provider action.<br />
The pay-fix bill previously would have extended the<br />
fee fix until April 30, but this date was pushed back to May<br />
31 in an amendment by Sen. Max Baucus, D-Mont. The<br />
amendment delayed passage of the bill, which had to be<br />
sent back to the House for a second vote. Fortunately, the<br />
House moved quickly to give its approval.<br />
CCI 16.1 tightens your coding<br />
of fluoro, artificial disk implant<br />
You’ll notice quite a few new code pairs bundling<br />
fluoroscopy into injections in version 16.1 of the National<br />
Correct Coding Initiative (CCI), which took effect April 1. In<br />
addition, you’ll see that the artificial disk codes are bundled<br />
into a number of other spinal fusion procedures, as is<br />
Category III code 0195T (presacral arthrodesis).<br />
On the nervous system side, look for new CCI code pairs<br />
involving the codes for injection or destruction of the plantar<br />
common digital nerve, e.g., Morton’s neuroma (64455<br />
and 64632), among other edits.<br />
Note also a new set of edits that will prevent you<br />
from getting paid for newborn care per-day E/M codes<br />
99460-99462 on the same day as a subsequent hospital<br />
care service.<br />
How CCI works: CCI is a form of claims processing<br />
software used by your Medicare carrier – and some private<br />
payers – to keep you from billing certain codes together<br />
(e.g., components of a surgical procedure in addition to the<br />
comprehensive procedure, or two codes that realistically<br />
wouldn’t be performed together).<br />
Correct Code Solutions LLC, Carmel, Ind., a CMS contractor,<br />
maintains the CCI edits and updates them quarterly.<br />
You can also review CCI’s policy manual (updated annually)<br />
for many of the rules behind the edits. The full list of<br />
CCI edits and the policy manual are available on the CMS<br />
website (www.cms.gov).<br />
CCI code pairs, or “edits,” affect codes you report for<br />
the same patient, performed by the same provider on<br />
4<br />
the same day. Within a code pair, Medicare will pay the<br />
“Column 1” (left-most) code. The code in “Column 2” gets<br />
bundled, or denied.<br />
A code pair with a modifier indicator of “1” means you<br />
can use an appropriate modifier (e.g., 50, RT/LT, 78, 58,<br />
59, 57 or 25) to override the edit. Modifier indicator “0”<br />
means you can’t. Many of these edits may be overridden,<br />
but be careful not to routinely override without documentation<br />
of medical necessity. Keep in mind CCI edits represent<br />
Medicare coding policy.<br />
Unless otherwise noted, the CCI edits described<br />
below all have a “1” modifier indicator, meaning the<br />
appropriate modifier may be used to override the edits<br />
when warranted.<br />
Musculoskeletal<br />
` Multiplane external fixation codes 20696 and<br />
20697 have the following imaging codes as Column 2<br />
components:<br />
• 76942 (echo guidance for biopsy).<br />
• 77002 (needle localization by X-ray).<br />
• 77012 (CT scan for needle biopsy).<br />
• 77021 (MR guidance for needle placement).<br />
• 77031 (stereotactic guidance for breast biopsy).<br />
` A number of new edits bundle cervical artificial disc<br />
arthroplasty procedures as column 2 components of spinal<br />
fusion to treat deformity and kyphectomy:<br />
• Posterior fusion of 7-12 segments ( 22802) includes<br />
cervical artificial disc arthroplasty (22856) and<br />
removal (22864).<br />
• Posterior fusion of 13 or more segments ( 22804)<br />
includes 22856, 22861 (artificial disc revision)<br />
and 22864.<br />
• Anterior fusion, 2-3 segments ( 22808)<br />
includes 22856.<br />
• Anterior fusion, 4-7 segments ( 22810) includes<br />
22856 and 22864.<br />
• Anterior fusion, 8 or more segments ( 22812)<br />
includes 22856, 22861 and 22864.<br />
• Kyphectomy codes 22818 and 22819 include artificial<br />
disc codes 22856, 22861 and 22864.<br />
` Artificial disc codes also received their own new<br />
Column 2 components:<br />
© 2010 <strong>DecisionHealth</strong> ® • www.ortho-decisions.com • 1-877-602-3835
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> May 2010<br />
•<br />
•<br />
•<br />
Cervical artificial disc arthroplasty (22856) includes<br />
components 22505 (manipulation of spine), 62291<br />
(spinal diskography), 22220 (spinal osteotomy) and<br />
22600 (cervical arthrodesis, single level).<br />
Revision of cervical artificial disc (22861) includes<br />
components 22220, 22505, 62291, cervical fusion<br />
(22554 and 22600) and spinal fusion (22800, 22802,<br />
22808 and 22810), as well as 22856.<br />
Removal of cervical artificial disc (22864) includes<br />
components 22220, 22505, 22554, 22600, 22800,<br />
22808, 22845, instrumentation (22851), 22856, 62291,<br />
and diskectomy (63075).<br />
• Lumbar artificial disc arthroplasty ( 22857), revision<br />
(22862) and removal (22865) all have 0195T (presacral<br />
arthrodesis) as a Column 2 component.<br />
` Injection for elbow arthrography (24220) includes<br />
fluoroscopy codes 76000, 76001 as Column 2 components.<br />
` Buttock fasciotomy (27027) includes hip/thigh fasciotomy<br />
(27025) as a Column 2 component.<br />
` Don’t forget: It is never appropriate for a surgeon to<br />
report an anesthesia code for the surgery he is also performing.<br />
Look for new edits bundling 01400 (anesthesia for<br />
knee surgery) as a Column 2 component of all open knee<br />
procedures, from incision and drainage (27301) to amputation<br />
(27596). Similarly, anesthesia code 01404 is bundled<br />
as a component of lower leg amputation (27598). Also,<br />
anesthesia codes 01250, 01320 and 01400 are all Column<br />
2 components of knee arthroscopy codes 29866-29889.<br />
Note that these edits have a “0” modifier indicator.<br />
` Category III pre-sacral arthrodesis code 0195T is a Column<br />
2 component of lumbar spinal fusion (22630). In turn,<br />
0195T has the following new Column 2 components:<br />
• 22505 (manipulation of spine).<br />
• 22830 (exploration of spinal fusion).<br />
• 49000-49010 (abdominal endoscopy).<br />
• 62290 (injection for spine disk X-ray).<br />
Nervous system<br />
` Percutaneous aspiration of intervertebral nucleus pulposus<br />
(62267) has the following Column 2 components:<br />
• 10021 (fine needle aspiration w/o image).<br />
• 20220,<br />
20240, 20245, 20250 and 20251<br />
(bone biopsy).<br />
• 77002 (fluoroscopic needle guidance).<br />
` Fluoroscopic needle guidance code 77002 is a<br />
Column 2 component of 62268 (aspiration of spinal cord<br />
cyst) and 62269 (spinal cord needle biopsy).<br />
` Percutaneous disk decompression (62287) includes<br />
Category III code 0195T (presacral arthrodesis) as a<br />
Column 2 component.<br />
` Removal of implanted spinal infusion pump<br />
(62365) is a Column 2 component of 62360 (reservoir<br />
implant) and 62361-62362 (pump implant), all with a “0”<br />
modifier indicator.<br />
` Stereotactic spinal cord stimulation (63610)<br />
includes fluoroscopy codes 77002 and 77003 as<br />
Column 2 components.<br />
` Fluoroscopy code 77003 is a Column 2 component of<br />
nerve block codes 64510, 64520 and 64530.<br />
` Fluoro codes 76000, 76001 and 77002 are Column<br />
2 components of neurostimulator electrodes (64555) and<br />
nerve destruction codes 64600, 64605, 64610 and 64620.<br />
` Stimulator implant (64561) includes 76000, 76001,<br />
77002 and 77003 as Column 2 components.<br />
` Plantar common digit nerve destruction (64632)<br />
is a Column 2 component of 64640 (destruction, other<br />
peripheral nerve).<br />
<strong>Orthopedic</strong> Conferences<br />
Train your staff and keep your continuing education credits<br />
up-to-date with these live conferences and webinars.<br />
Bundling Intelligence: Achieving Maximum<br />
reimbursement for orthopedic surgeries<br />
speaker: Margie Scalley Vaught, CPC, CPC-H, PCE, CCS-P, MCS-P,<br />
ACS-EM, ACS-OR<br />
Wed., May 19, 1-2 p.m. ET<br />
www.decisionhealth.com/conferences/A1967<br />
2011 ICd-9 Codes: Learn how Key Changes Will Impact Your<br />
documentation, Coding and Billing – and Your Bottom Line<br />
speaker: Margie Scalley Vaught, CPC, CPC-H, PCE, CCS-P, MCS-P,<br />
ACS-EM, ACS-OR<br />
Thurs., May 20, 1-2:30 p.m. ET<br />
www.decisionhealth.com/conferences/A1957<br />
Advanced orthopedic Coding & reimbursement symposium<br />
Loews Philadephia Hotel, Philadelphia<br />
Sept. 12-15, 2010<br />
www.decisionhealth.com/orthopedic_coding_reimbursement<br />
For more information about all events, visit the websites<br />
listed above or call 1-866-620-5939.<br />
© 2010 <strong>DecisionHealth</strong> ® • www.ortho-decisions.com • 1-877-602-3835 5
May 2010 <strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong><br />
` Injection into plantar common digital nerve, e.g.,<br />
Morton’s neuroma (64455) includes the following Column<br />
2 components:<br />
• 29515 and 29590 (splint application).<br />
6<br />
• 29540 and 29550 (strapping).<br />
• 29580 (application of paste boot).<br />
• J2001 (injection, lidocaine hcl for intravenous<br />
infusion, 10 mg).<br />
Code 64455 is itself a Column 2 component of:<br />
• 64640 (injection treatment of nerve).<br />
• 64774, 64776, 64782, 64788 (nerve excision).<br />
• 64795 (biopsy of nerve).<br />
• 64820, 64831, 64834 (nerve repair).<br />
• 64890, 64891, 64896, 64895 (nerve graft).<br />
• 64905, 64907 (nerve pedicle transfer).<br />
• 64910 (nerve repair w/allograft).<br />
• 64911 (neurorraphy w/vein autograft).<br />
Evaluation and management<br />
` Subsequent hospital care codes 99231-99233 bundle<br />
newborn care per-day E/M codes 99460-99462 as Column<br />
2 components with a “0” modifier indicator.<br />
` Newborn E/M code 99460 includes 99462 as a<br />
Column 2 component. Also, code 99461 includes 99460<br />
and 99462 as Column 2 components. All edits have a “0”<br />
modifier indicator.<br />
health reform law extends therapy<br />
exemptions, shortens claims filing deadline<br />
CMS is moving to implement provisions in the Patient<br />
Protection and Affordable Care Act (PPACA), the official<br />
name of the new health care reform law. Here is a brief<br />
summary of actions the agency has taken so far, as well as<br />
some of the other changes practices can expect.<br />
Agency officials estimate that changes affecting physician<br />
fees may take as long as 60 days to implement (even<br />
if they retroactively take effect Jan. 1, 2010), because of<br />
recalculations that will have to take place across all fee<br />
schedules (e.g., hospital outpatient), according to officials<br />
speaking on an April 13 conference call with providers.<br />
Therapy cap exceptions process extended (Sec.<br />
3103): Outpatient therapy service providers may continue<br />
to submit claims with the KX modifier, when an exception<br />
is appropriate, for services furnished on or after Jan.<br />
1, 2010, through Dec. 31, 2010. For physical therapy and<br />
speech language pathology services combined, and occupational<br />
therapy services the limit on incurred expenses<br />
is $1,860. Deductible and coinsurance amounts applied to<br />
therapy services count toward the amount accrued before<br />
a cap is reached.<br />
New timely filing deadline for claims (Sec. 6404):<br />
Providers no longer have 15 to 24 months to file Medicare<br />
claims. PPACA now requires practices to submit claims<br />
within 12 months of the date of service. That means a<br />
claim for any service provided to a Medicare patient in<br />
2010 will need to be submitted one calendar year later.<br />
CMS says it will phase the new law in with the following<br />
interim deadlines:<br />
• Claims for services between Oct. 1, 2009, and Dec.<br />
31, 2009, need to be submitted by Dec. 31, 2010.<br />
• Claims for services rendered before Oct. 1, 2009, will<br />
follow the previous rules for timely Medicare claims.<br />
The change is considered a fraud, waste and abuse<br />
provision, not just a change to make a provider’s life more<br />
difficult. Also, the new timely claims rules are not set in<br />
stone. HHS has the power to alter the timely claims provision<br />
in future rulemaking.<br />
Overpayments must be repaid sooner (Sec. 6402):<br />
Effective immediately, providers have just 60 days to report<br />
and return any overpayments they discover. Practices<br />
could face civil money penalties if the government can<br />
prove they should have known they needed to return<br />
money to their carrier.<br />
The work geographic index floor extended and the<br />
practice expense geographic adjustment revised under<br />
the Medicare physician fee schedule (Sec. 3102):<br />
PPACA extends a floor of 1.00 on geographic price cost<br />
index (GPCI) adjustments to the work portion of the fee<br />
schedule through the end of 2010, with the effect of increasing<br />
practitioner fees in rural areas. The law also provides<br />
immediate relief to areas negatively impacted by the geographic<br />
adjustment for practice expenses and requires the<br />
HHS secretary to improve the methodology for calculating<br />
practice expense adjustments beginning in 2012. Physicians<br />
in more than 50 geographic localities will likely see a small<br />
boost in their fees as a result of the GPCI adjustments.<br />
CMS will continue to review misvalued codes<br />
under the physician fee schedule (Sec. 3134): PPACA<br />
© 2010 <strong>DecisionHealth</strong> ® • www.ortho-decisions.com • 1-877-602-3835
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> May 2010<br />
directs the HHS secretary to regularly review Medicare<br />
physician fee schedule rates, including services that have<br />
experienced high growth rates. The law also strengthens<br />
the secretary’s authority to adjust fees found to be misvalued<br />
or inaccurate.<br />
Payment for bone density tests (Sec. 3111): PPACA<br />
restores payment for dual-energy x-ray absorptiometry<br />
(DXA) services furnished during 2010 and 2011 to 70% of<br />
the Medicare rate paid in 2006. The American College of<br />
Radiology estimates this will increase the fee to about $98.<br />
Presumed utilization rate increases for high-cost<br />
imaging equipment (Sec. 3135): The presumed utilization<br />
rate (PUR) helps Medicare set the technical payment<br />
for imaging services in a non-hospital setting (e.g., physician’s<br />
office). In effect, a higher UAR tends to drive down<br />
the technical fee practices receive. PPACA will phase in a<br />
gradually higher PUR for imaging services, starting at a rate<br />
of 50% to 65% for 2010 through 2012, 70% in 2013 and 75%<br />
thereafter. The law excludes low-tech imaging such as ultrasounds,<br />
x-rays and EKGs from this adjustment. This provision<br />
supercedes the CMS rule requiring the rate to increase<br />
to 90% in 2013.<br />
PQRI changes (Secs. 3002, 3003 and 3007): PPACA<br />
extends the PQRI program through 2014 and allocates $75<br />
million for quality measure development. You’ll continue<br />
to receive bonus payments for quality reporting for another<br />
four years, but bonuses will decrease over time from<br />
current incentives of 2% of your overall Medicare charges<br />
to 0.5% of charges in 2012, 2013 and 2014. Providers who<br />
don’t participate in PQRI will see payments drop by 1.5%<br />
in 2015 and 2% in 2016, according to the bill.<br />
The bill also requires upgrades to PQRI feedback<br />
forms by 2012 and public reporting of participation in the<br />
PQRI program.<br />
In 2015, CMS will start to phase-in a “value-based<br />
payment modifier” to the physician fee schedule. The<br />
modifier will adjust your payments based on the quality<br />
and cost of care physicians deliver. You’ll start to see the<br />
program develop in 2012 and physician fee schedule rulemaking<br />
in 2013.<br />
Limitation on Medicare exception to the prohibition<br />
on certain physician referrals for hospitals (Sec.<br />
6001): PPACA prohibits physician-owned hospitals that do<br />
not have a provider agreement prior to Aug. 1, 2010, from<br />
participation with Medicare. Such hospitals that have a<br />
provider agreement prior to Aug. 1, 2010, could continue<br />
to participate in Medicare under certain requirements addressing<br />
conflict of interest, bona fide investments, patient<br />
safety issues and expansion limitations.<br />
A new independent payment advisory board<br />
(Sec. 3403): The 15-member board will be formed to act<br />
when Medicare costs are projected to be unsustainable,<br />
but it may not ration patient care, raise taxes or change<br />
premiums, eligibility or benefits. The board will look at<br />
trends and can recommend that Congress implement new<br />
payment models, such as pay-for-performance. Reports<br />
from the board will no longer be non-binding, as MedPAC<br />
reports are now. Congress must accept the board’s recommendations<br />
or modify recommendations in a way that<br />
doesn’t reduce their impact. The first of these reports is due<br />
in 2014.<br />
Contiguous body part discount rate to increase<br />
(Sec. 3135): The discount CMS applies to imaging services,<br />
such as X-rays, performed on contiguous body parts will<br />
increase in 2011 to 50% from the current 25%.<br />
Self-referral disclosure (Sec. 6003): PPACA adds an<br />
additional requirement to the Medicare in-office ancillary<br />
exception that requires the referring physician to inform<br />
the patient in writing that the individual may obtain the<br />
specified service from a person other than the referring<br />
physician, a physician who is a member of the same group<br />
practice as the referring physician or an individual who is<br />
directly supervised by the physician or by another physician<br />
in the group practice.<br />
Official rEsOurcEs:<br />
`<br />
PPACA section-by-section summary:<br />
http://dpc.senate.gov/healthreformbill/healthbill53.pdf<br />
` Health reform law timeline: www.kff.org/healthreform/8060.cfm<br />
Coding a hemi-to-total knee revision<br />
Question: Patient underwent a medial unicompartmental<br />
arthroplasty 19 years ago. He now presents with mechanical<br />
symptoms and pain. X-rays demonstrate poly liner<br />
completely dislodged and worn down to be bone on bone.<br />
Surgery is performed to revise the medial unicompartmental<br />
hemiarthroplasty to a total knee arthroplasty. As there is<br />
not a “conversion of previous knee surgery to a total arthroplasty”<br />
as there is for hips (27132), do we bill for removal of<br />
© 2010 <strong>DecisionHealth</strong> ® • www.ortho-decisions.com • 1-877-602-3835 7
May 2010 <strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong><br />
the previous prosthesis (27488) AND the total knee arthroplasty<br />
(27447)? What is the most appropriate way to code<br />
the procedures performed?<br />
Answer: This question was posed recently to the AMA,<br />
which checked with the American Academy of Orthopaedic<br />
Surgeons, then responded that 27482-52 (revision of<br />
total knee arthroplasty, with or without allograft, femoral<br />
and entire tibial component) would be the most appropriate<br />
code. You should append the 52 modifier (reduced<br />
services) since the code describes revision of a total knee,<br />
but you are revising only a unicompartmental arthroplasty.<br />
It would not be appropriate to use 27488 (removal<br />
of prosthesis, including total knee prosthesis, methylmethacrylate<br />
with or without insertion of spacer, knee)<br />
if you are putting another prosthesis in, according to<br />
the AMA.<br />
Aspiration and injection in same joint<br />
Question: Can I report 20610 twice in the same joint –<br />
once for aspiration and once for injection?<br />
Answer: No, you can’t. I am starting to see this error<br />
coming up in audits more and more for some reason. The<br />
CPT descriptor for 20610 reads: “Arthrocentesis, aspiration<br />
and/or injection; major joint or bursa (e.g., shoulder,<br />
hip, knee joint, subacromial bursa).” The term “and/or”<br />
in the description tells you the code “includes the performance<br />
of one or all of the procedures described in the same<br />
major joint or bursa,” CPT explains. “Therefore, code 20610<br />
should only be reported one time when both aspiration and<br />
injection are performed in the same major joint or bursa”<br />
(CPT Assistant, March 2001).<br />
Similarly, for knee or hip injections, at least, you also<br />
may not report multiple units of 20610 for multiple injections<br />
into the same joint.<br />
A few years ago, I asked members of the American<br />
Academy of Orthopaedic Surgeons’ (AAOS) Coding<br />
Committee about separate reporting of injection codes<br />
to the shoulder during the same treatment session (e.g.,<br />
20610 to the glenohumeral joint and 20605 to the acromioclavicular<br />
joint). In general, they agreed that separate<br />
billing could be warranted if separate needles were<br />
used. In the shoulder, the AC and GH joints are separated<br />
by the joint capsule. By contrast, in the knee, once the<br />
solution is injected it will cover the medial, lateral and<br />
patellofemoral compartments.<br />
8<br />
www.ortho-decisions.com<br />
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong><br />
` SubSCriber ServiCeS<br />
editor: Laura Evans: 1-301-287-2376 or fax 1-301-287-2916;<br />
email: levans@decisionhealth.com<br />
Contributing editor: Steve Brust, 1-301-287-2438 or fax 1-301-287-2749;<br />
email: sbrust@decisionhealth.com<br />
Technical Advisor: Margie Scalley Vaught, CPC, CCS-P, MSC-P, ACS-EM, ACS-OR<br />
vice President of Publishing: Tonya Nevin, 1-301-287-2454<br />
or fax 1-301-287-2151; email: tnevin@decisionhealth.com<br />
subscriptions: Direct questions about newsletter delivery and<br />
account status, toll free, to 1-877-602-3835 or email to:<br />
orthocustomer@decisionhealth.com.<br />
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> Online – As a subscriber, you can read and<br />
download your newsletter electronically at www.ortho-decisions.com.<br />
extra Benefits: Search back issues by code or keyword, look up CPT ® codes and<br />
Medicare billing rules for CPT ® , HCPCS and ICD-9 diagnosis codes, and create<br />
printable pdfs of key billing and payment information. how to register: Visit<br />
www.ortho-decisions.com/register and fill out the online form. After that, just<br />
visit www.ortho-decisions.com as often as you like. If you have any problems or<br />
questions about registering, please call 1-877-602-3835.<br />
Free Internet Forum: To join Ortho-L, our free Internet forum for orthopedic<br />
practice coders, billers, managers and administrators, set your Internet browser to<br />
www.decisionhealth.com/ortho-l-enroll and fill out the form.<br />
Conferences: <strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> holds seminars<br />
to help you meet coding and billing challenges. For program schedules,<br />
call 1-301-287-2684; email: conference@decisionhealth.com; or go to<br />
www.decisionhealth.com.<br />
Ceus: Each <strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> has prior approval, through June<br />
2010, of the American Academy of Professional Coders (AAPC) for 0.5 CEUs.<br />
Granting of this approval in no way constitutes endorsement by the Academy of the<br />
program, content or the program sponsor. You can earn your CEUs by passing a<br />
five-question quiz delivered through your <strong>Orthopedic</strong> Decisions website<br />
(www.ortho-decisions.com). Once you have logged in, go to the “Library” page, find<br />
the issue and click the adjacent hyperlink marked “Quiz.” Log in to the Online Quiz<br />
System using your <strong>Orthopedic</strong> Decisions site userID/password.<br />
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> is also approved for CEUs from the Board of<br />
Medical specialty Coding (BMsC) for up to 6 CEUs each toward the ACS-OR<br />
credential and 3 CEUs toward other ACS credentials. Contact BMSC directly for<br />
information at 1-800-897-4509; www.medicalspecialtycoding.com.<br />
reprints: To request permission to make photocopy or electronic reprints, call<br />
toll-free 1-866-265-0148 or email gbelski@decisionhealth.com and ask about our<br />
copyright waiver, multiple copy and site license programs.<br />
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> is published monthly by <strong>DecisionHealth</strong>, LLC,<br />
Two Washingtonian Center, 9737 Washingtonian Blvd., Ste. 100, Gaithersburg, MD<br />
20878-7364. The price is: $450 per year. Copyright © 2010 <strong>DecisionHealth</strong>.<br />
CoPYrIGhT WArnInG: Copyright viola tions will be prosecuted. OCPS shares<br />
10% of the net proceeds of settlements or jury awards with individuals who<br />
provide essential evidence of illegal photocopying or electronic redistribution. To<br />
confidentially report suspected copyright violations, call our copyright attorney<br />
Steve McVearry at 1-301-287-2266 or email him at smcvearry@ucg.com.<br />
CPT ® is a trademark of the American Medical Association.<br />
CPT© 2009 American Medical Association. All rights reserved.
<strong>Orthopedic</strong> Coder’s <strong>Pink</strong> <strong>Sheet</strong> May 2010<br />
Copyright notice<br />
It is illegal to forward this electronic version of <strong>Orthopedic</strong> <strong>Coder's</strong> <strong>Pink</strong> <strong>Sheet</strong> to anyone else. It is a free<br />
benefit only for the individual listed by name as the subscriber. It’s illegal to distribute electronically <strong>Orthopedic</strong><br />
<strong>Coder's</strong> <strong>Pink</strong> <strong>Sheet</strong> to others in your office or other sites affiliated with your organization. If this email has<br />
been forwarded to you and you’re not the named subscriber, that is a violation of federal copyright law.<br />
However, only the party that forwards a copyrighted email is at risk, not you.<br />
To confidentially report suspected copyright violations, call our copyright attorney Steve McVearry at<br />
1-301-287-2266 or email him at smcvearry@ucg.com. Copyright violations will be prosecuted. And<br />
<strong>Orthopedic</strong> <strong>Coder's</strong> <strong>Pink</strong> <strong>Sheet</strong> shares 10% of the net proceeds of settlements or jury awards with<br />
individuals who provide essential evidence of illegal electronic forwarding of <strong>Orthopedic</strong> <strong>Coder's</strong> <strong>Pink</strong> <strong>Sheet</strong><br />
or photocopying of our newsletter.<br />
© 2010 <strong>DecisionHealth</strong> ® • www.ortho-decisions.com • 1-877-602-3835 9