Diagnosis and management of early- and late-onset cerebellar ataxia
Diagnosis and management of early- and late-onset cerebellar ataxia
Diagnosis and management of early- and late-onset cerebellar ataxia
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
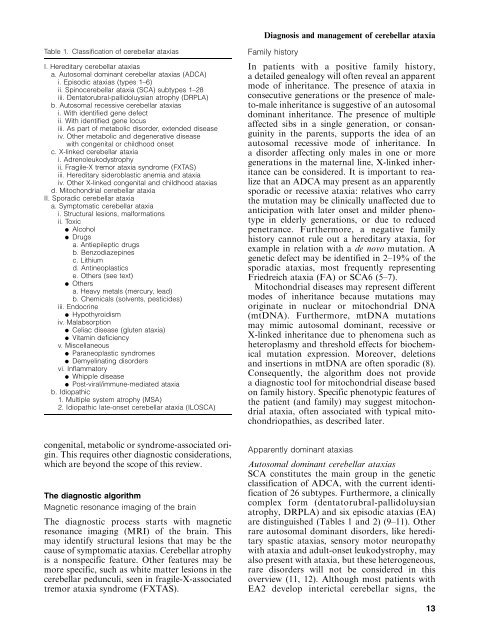
Table 1. Classification <strong>of</strong> <strong>cerebellar</strong> <strong>ataxia</strong>s<br />
I. Hereditary <strong>cerebellar</strong> <strong>ataxia</strong>s<br />
a. Autosomal dominant <strong>cerebellar</strong> <strong>ataxia</strong>s (ADCA)<br />
i. Episodic <strong>ataxia</strong>s (types 1–6)<br />
ii. Spino<strong>cerebellar</strong> <strong>ataxia</strong> (SCA) subtypes 1–28<br />
iii. Dentatorubral-pallidoluysian atrophy (DRPLA)<br />
b. Autosomal recessive <strong>cerebellar</strong> <strong>ataxia</strong>s<br />
i. With identified gene defect<br />
ii. With identified gene locus<br />
iii. As part <strong>of</strong> metabolic disorder, extended disease<br />
iv. Other metabolic <strong>and</strong> degenerative disease<br />
with congenital or childhood <strong>onset</strong><br />
c. X-linked <strong>cerebellar</strong> <strong>ataxia</strong><br />
i. Adrenoleukodystrophy<br />
ii. Fragile-X tremor <strong>ataxia</strong> syndrome (FXTAS)<br />
iii. Hereditary sideroblastic anemia <strong>and</strong> <strong>ataxia</strong><br />
iv. Other X-linked congenital <strong>and</strong> childhood <strong>ataxia</strong>s<br />
d. Mitochondrial <strong>cerebellar</strong> <strong>ataxia</strong><br />
II. Sporadic <strong>cerebellar</strong> <strong>ataxia</strong><br />
a. Symptomatic <strong>cerebellar</strong> <strong>ataxia</strong><br />
i. Structural lesions, malformations<br />
ii. Toxic<br />
d Alcohol<br />
d Drugs<br />
a. Antiepileptic drugs<br />
b. Benzodiazepines<br />
c. Lithium<br />
d. Antineoplastics<br />
e. Others (see text)<br />
d Others<br />
a. Heavy metals (mercury, lead)<br />
b. Chemicals (solvents, pesticides)<br />
iii. Endocrine<br />
d Hypothyroidism<br />
iv. Malabsorption<br />
d Celiac disease (gluten <strong>ataxia</strong>)<br />
d Vitamin deficiency<br />
v. Miscellaneous<br />
d Paraneoplastic syndromes<br />
d Demyelinating disorders<br />
vi. Inflammatory<br />
d Whipple disease<br />
d Post-viral/immune-mediated <strong>ataxia</strong><br />
b. Idiopathic<br />
1. Multiple system atrophy (MSA)<br />
2. Idiopathic <strong>late</strong>-<strong>onset</strong> <strong>cerebellar</strong> <strong>ataxia</strong> (ILOSCA)<br />
congenital, metabolic or syndrome-associated origin.<br />
This requires other diagnostic considerations,<br />
which are beyond the scope <strong>of</strong> this review.<br />
The diagnostic algorithm<br />
Magnetic resonance imaging <strong>of</strong> the brain<br />
The diagnostic process starts with magnetic<br />
resonance imaging (MRI) <strong>of</strong> the brain. This<br />
may identify structural lesions that may be the<br />
cause <strong>of</strong> symptomatic <strong>ataxia</strong>s. Cerebellar atrophy<br />
is a nonspecific feature. Other features may be<br />
more specific, such as white matter lesions in the<br />
<strong>cerebellar</strong> pedunculi, seen in fragile-X-associated<br />
tremor <strong>ataxia</strong> syndrome (FXTAS).<br />
<strong>Diagnosis</strong> <strong>and</strong> <strong>management</strong> <strong>of</strong> <strong>cerebellar</strong> <strong>ataxia</strong><br />
Family history<br />
In patients with a positive family history,<br />
a detailed genealogy will <strong>of</strong>ten reveal an apparent<br />
mode <strong>of</strong> inheritance. The presence <strong>of</strong> <strong>ataxia</strong> in<br />
consecutive generations or the presence <strong>of</strong> maleto-male<br />
inheritance is suggestive <strong>of</strong> an autosomal<br />
dominant inheritance. The presence <strong>of</strong> multiple<br />
affected sibs in a single generation, or consanguinity<br />
in the parents, supports the idea <strong>of</strong> an<br />
autosomal recessive mode <strong>of</strong> inheritance. In<br />
a disorder affecting only males in one or more<br />
generations in the maternal line, X-linked inheritance<br />
can be considered. It is important to realize<br />
that an ADCA may present as an apparently<br />
sporadic or recessive <strong>ataxia</strong>: relatives who carry<br />
the mutation may be clinically unaffected due to<br />
anticipation with <strong>late</strong>r <strong>onset</strong> <strong>and</strong> milder phenotype<br />
in elderly generations, or due to reduced<br />
penetrance. Furthermore, a negative family<br />
history cannot rule out a hereditary <strong>ataxia</strong>, for<br />
example in relation with a de novo mutation. A<br />
genetic defect may be identified in 2–19% <strong>of</strong> the<br />
sporadic <strong>ataxia</strong>s, most frequently representing<br />
Friedreich <strong>ataxia</strong> (FA) or SCA6 (5–7).<br />
Mitochondrial diseases may represent different<br />
modes <strong>of</strong> inheritance because mutations may<br />
originate in nuclear or mitochondrial DNA<br />
(mtDNA). Furthermore, mtDNA mutations<br />
may mimic autosomal dominant, recessive or<br />
X-linked inheritance due to phenomena such as<br />
heteroplasmy <strong>and</strong> threshold effects for biochemical<br />
mutation expression. Moreover, deletions<br />
<strong>and</strong> insertions in mtDNA are <strong>of</strong>ten sporadic (8).<br />
Consequently, the algorithm does not provide<br />
a diagnostic tool for mitochondrial disease based<br />
on family history. Specific phenotypic features <strong>of</strong><br />
the patient (<strong>and</strong> family) may suggest mitochondrial<br />
<strong>ataxia</strong>, <strong>of</strong>ten associated with typical mitochondriopathies,<br />
as described <strong>late</strong>r.<br />
Apparently dominant <strong>ataxia</strong>s<br />
Autosomal dominant <strong>cerebellar</strong> <strong>ataxia</strong>s<br />
SCA constitutes the main group in the genetic<br />
classification <strong>of</strong> ADCA, with the current identification<br />
<strong>of</strong> 26 subtypes. Furthermore, a clinically<br />
complex form (dentatorubral-pallidoluysian<br />
atrophy, DRPLA) <strong>and</strong> six episodic <strong>ataxia</strong>s (EA)<br />
are distinguished (Tables 1 <strong>and</strong> 2) (9–11). Other<br />
rare autosomal dominant disorders, like hereditary<br />
spastic <strong>ataxia</strong>s, sensory motor neuropathy<br />
with <strong>ataxia</strong> <strong>and</strong> adult-<strong>onset</strong> leukodystrophy, may<br />
also present with <strong>ataxia</strong>, but these heterogeneous,<br />
rare disorders will not be considered in this<br />
overview (11, 12). Although most patients with<br />
EA2 develop interictal <strong>cerebellar</strong> signs, the<br />
13