With a prenatal - Children's Hospital & Research Center Oakland
With a prenatal - Children's Hospital & Research Center Oakland
With a prenatal - Children's Hospital & Research Center Oakland
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>With</strong> a <strong>prenatal</strong><br />
diagnosis, Children’s<br />
cleft lip team helps<br />
a family prepare.<br />
ALSO INSIDE:<br />
Barbara Staggers, MD, is a<br />
Force of<br />
[Adolescent] Nature<br />
Thanks to Dr. Staggers, Children’s<br />
has a national-model, urban-based<br />
Adolescent Medicine department.<br />
WINTER 2007<br />
From Fat to Fit<br />
Children’s HEAL team<br />
helps families learn healthy<br />
living habits and how to<br />
beat childhood obesity.
2<br />
CHILDREN’S HANDPRINTS<br />
Latest technology<br />
at Children’s<br />
7 Children’s <strong>Hospital</strong> is the<br />
first pediatric medical center<br />
on the West Coast to get its<br />
own portable CT scanner.<br />
From Fat to Fit<br />
9 Children’s HEAL<br />
team helps families<br />
learn healthy living<br />
habits and helps kids<br />
beat childhood obesity.<br />
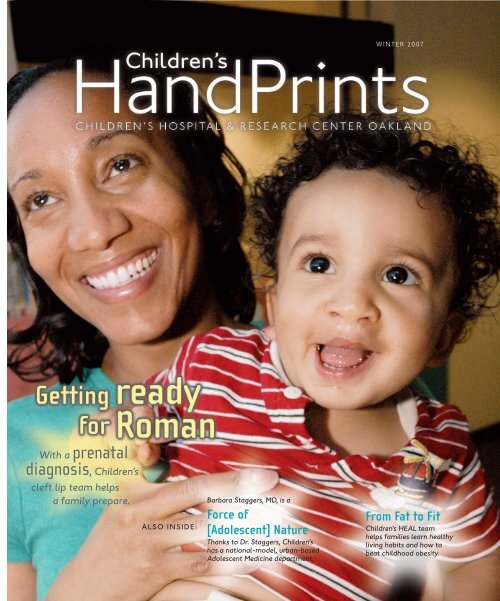
On the cover<br />
Roman Leigh and his mom, Robin, have<br />
big smiles now that the surgeries to<br />
repair Roman’s cleft lip and palate are<br />
behind them. See Getting ready for<br />
Roman on page 6. Photo by Gary<br />
Turchin.<br />
table of contents<br />
Force of<br />
(adolescent) nature<br />
19<br />
When people think of Children’s <strong>Hospital</strong>, they think of babies and<br />
small children. But thanks to Barbara Staggers, MD, Children’s also<br />
has a national-model, urban-based Adolescent Medicine department.<br />
3 DEAR READER<br />
Letter from the president.<br />
4 THIS AND THAT<br />
NICU nurses take flight, increasing their REACH <strong>With</strong> Children’s<br />
NICU nurses on board, REACH helicopters can now transport smaller preemies.<br />
More Children’s services available at East Bay satellite offices<br />
New Modesto office opens in March; Walnut Creek office growing, too.<br />
Rep. Barbara Lee at Children’s Rep. Barbara Lee’s (D-<strong>Oakland</strong>) press conference<br />
at Children’s rallied support for SCHIP, which helps bring health insurance<br />
to uninsured, low-income children.<br />
Getting ready for Roman <strong>With</strong> a <strong>prenatal</strong> diagnosis of cleft lip and palate,<br />
Children’s Craniofacial department helps a family prepare.<br />
13 FEATURE: HEMATOLOGY/ONCOLOGY<br />
Toughing out leukemia Adrianna’s fighting spirit sees her through a<br />
battle against acute myelogenous leukemia (AML).<br />
16 FEATURE: PEDIATRIC REHABILITATION<br />
Food fight Feeding specialists offer tips, and help children with feeding disorders<br />
expand their diet.<br />
24 FEATURE: CHILDREN’S NEW HOSPITAL<br />
Children’s will build in <strong>Oakland</strong> Why we’re building at our existing site;<br />
plus more about how we’ll do it and and how you can help.<br />
28 CHILDREN’S HOSPITAL’S FOUNDATION<br />
A 95-year history of visionary philanthropy at Children’s How<br />
Children’s foundation will continue its commitment to help Children’s grow.<br />
Gala to Help Raise Healthy Children January event will benefit<br />
Children’s Healthy Eating Active Living (HEAL) program.<br />
Good karma builds happy faces Yoga students donate to help a craniofacial<br />
patient and his family pay for care and travel expenses.<br />
Children’s most generous benefactors honored at international<br />
event An annual gala celebrates major donors to children’s hospitals.<br />
Make a gift to Children’s before you ring in the New Year<br />
Make a year-end gift to Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong><br />
and you could save money on your taxes.
Dear Reader:<br />
As Northern California moves from fall to winter, raindrops fall and<br />
temperatures cool. But at Children’s <strong>Hospital</strong>, our efforts to build a new<br />
hospital are just warming up.<br />
You may already know that in September we announced our decision<br />
to build a new hospital on land adjacent to our existing campus. You can<br />
read more about this on page 24.<br />
It was on this site in 1912 that nurse Bertha Wright and a group of East<br />
Bay women decided to found what eventually became today’s Children’s<br />
<strong>Hospital</strong>. But it wasn’t until 1914 that they opened; they had to raise<br />
money and convert existing buildings before their dream became a reality.<br />
For us too it will take time: two years of planning before we break<br />
ground in 2010, and then three years of construction.<br />
To make our dream a reality we need to listen—to neighbors, friends<br />
and supporters—and work with all of them. Children’s <strong>Hospital</strong> wants to<br />
be a good neighbor, as well as Northern California’s premier pediatric<br />
healthcare provider.<br />
One important supporter, Rep. Barbara Lee (D-<strong>Oakland</strong>), asked us to<br />
host her October press conference urging reauthorization of the State<br />
Children’s Health Insurance Program. Read about this and other advocacy<br />
efforts on page 5.<br />
In this issue we also profile Barbara Staggers, MD, our renowned chief<br />
of Adolescent Medicine. Dr. Staggers offers hard-earned advice to parents<br />
of teenagers.<br />
Other articles in this issue contain tips about preventing childhood<br />
obesity and addressing feeding disorders, news about our new portable<br />
CT scanner and inspiration from leukemia survivor Adrianna Tucker.<br />
To all those supporting Children’s <strong>Hospital</strong>—especially our generous<br />
donors—thank you.<br />
Frank Tiedemann<br />
President and Chief Executive Officer<br />
Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong><br />
WINTER 2007 3<br />
Children’s HandPrints is a publication of Children’s<br />
<strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong>, 747 52nd Street,<br />
<strong>Oakland</strong>, CA 94609; 510-428-3000.<br />
Written, designed and produced by:<br />
Communications Dept.<br />
Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong><br />
665 53rd Street, <strong>Oakland</strong>, CA 94609<br />
Phone: 510-428-3367<br />
Fax: 510-601-3907<br />
Frank Tiedemann<br />
President and Chief Executive Officer<br />
Mary L. Dean<br />
Senior Vice President, Chief Strategic Development Officer<br />
Tina Amey<br />
Receptionist<br />
Debbie Dare<br />
Senior Graphic Designer<br />
Susan Foxall<br />
Project Manager<br />
Tom Levy<br />
Senior Writer<br />
Venita Robinson<br />
Director, Media and Community Relations<br />
Erika Sandstrom<br />
Graphic Designer<br />
Gary Turchin<br />
Director, Public Relations, and Senior Writer<br />
Diana Yee<br />
Media Relations Specialist<br />
Board of Directors<br />
Harold Davis, Chairman<br />
Jeffrey Cheung, Vice Chair<br />
Arthur D’Harlingue, MD<br />
Arnold Grisham<br />
James Keefe, Treasurer<br />
Watson M. Laetsch, PhD<br />
Michael LeNoir, MD<br />
Barbara May, Secretary<br />
Melba Muscarolas<br />
Karen Stout<br />
Lloyd Takao, MD<br />
Frank Tiedemann<br />
Gene Upshaw<br />
Harold (Tim) C. Warner, PhD<br />
Story requests, comments or suggestions for Children’s<br />
HandPrints may be emailed to comm@mail.cho.org or<br />
sent to 747 52nd St., <strong>Oakland</strong>, CA 94609.
4<br />
CHILDREN’S HANDPRINTS<br />
this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat<br />
ON LOCATION: (Left) At right, Tess Estocapia, RN, Children’s transport coordinator, helps move an incubator out of a REACH<br />
helicopter during a practice run of the new joint service. (Right) REACH’s Debbie Biederwolf, RN, and (l) Children’s Helen<br />
Nguyen, RN, prepare to transfer a baby to the transport incubator as part of the practice run.<br />
NEW SERVICES<br />
NICU nurses<br />
take flight,<br />
increasing their<br />
REACH<br />
Children’s nurses assure faster<br />
care for more preemies.<br />
REACH helicopters have been providing<br />
medical air transport to Bay Area children<br />
since 1987. Thanks to a new partnership<br />
with Children’s <strong>Hospital</strong>’s Neonatal<br />
Intensive Care Nursery (NICU), the<br />
familiar red choppers can now serve preemies<br />
as young as 24 weeks, gestation.<br />
Under a new agreement with Santa<br />
Rosa–based REACH Air Medical Services,<br />
a Children’s neonatal nurse specialist will<br />
www.childrenshospitaloakland.org<br />
this<br />
ANDthat<br />
now accompany REACH helicopters on<br />
neonatal transports. The collaboration<br />
took flight in July after 16 Children’s<br />
NICU nurses received helicopter transport<br />
training. Children’s NICU nurses are now<br />
available to fly when needed.<br />
“This gives (REACH) greater acuity in<br />
handling newborns,” said Kathy Logee,<br />
RN, a REACH flight nurse.<br />
REACH handles all types of patients,<br />
said Logee, but has only two flight nurses<br />
specializing in neonatal care. This limited<br />
REACH’s services, as well as the size of<br />
the preemies they could transport.<br />
Bringing Children’s 16 NICU nurses<br />
aboard, trained and experienced in handling<br />
and moving very small preemies,<br />
expands REACH’s capabilities. REACH<br />
may now transport by air, tiny preemies<br />
that previously had to be transferred more<br />
slowly, by road.<br />
this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat<br />
<strong>With</strong> Children’s NICU nurses at the<br />
ready, REACH can now provide life-saving<br />
transportation to these tiny babies faster. ★<br />
EXPANDING<br />
SERVICES<br />
More Children’s<br />
services available<br />
at East Bay<br />
satellite offices<br />
In early 2008, Children’s <strong>Hospital</strong><br />
plans to open its fifth physicians’ offices<br />
site, at 4016 Dale Road in Modesto.<br />
Children’s clinicians from Cardiology and<br />
Neurosurgery are already serving<br />
Children’s patient families in the northern<br />
Central Valley area out of a Modesto location.<br />
More services will be added soon. To<br />
t<br />
AN
this<br />
ANDthat<br />
this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat<br />
Walnut Creek 2 (New)<br />
108 La Casa Via, Suite 104<br />
925-952-3849<br />
Specialties: Endocrinology,<br />
Surgery, Neurology and<br />
Behavioral Pediatrics<br />
this<br />
ANDthat<br />
WALNUT CREEK EXPANSION: Children’s satellite physicians’<br />
offices in Walnut Creek added space for additional services in a<br />
building adjacent to its current site.<br />
all our referring physicians and patient<br />
families in the Stockton/Tracy/ Modesto<br />
area: please stay tuned.<br />
The Walnut Creek physicians’ offices<br />
have been outgrowing their space at 106<br />
La Casa Via. They will expand, adding<br />
space next door at 108 La Casa Via, for<br />
use by clinicians from Endocrinology,<br />
Surgery, Neurology and Behavioral<br />
Pediatrics. See map above for addresses<br />
and phone numbers. ★<br />
ADVOCACY<br />
Rep. Barbara Lee<br />
at Children’s<br />
Collaborating to support<br />
children’s healthcare.<br />
When the people we care for can’t<br />
speak up, we must speak for them. That’s<br />
advocacy, an important part of the mis-<br />
Walnut Creek 1<br />
106 La Casa Via, Suite 220<br />
Cardiology/Orthopedics:<br />
925-939-8687<br />
Other specialties:<br />
925-979-4000<br />
sion of Children’s <strong>Hospital</strong> & <strong>Research</strong><br />
<strong>Center</strong> <strong>Oakland</strong>.<br />
Back in January, Children’s <strong>Hospital</strong><br />
was one of 36 sites hosting a National<br />
Town Hall Meeting on Children’s Health<br />
Coverage. More than 150 people gathered<br />
here to talk about children’s healthcare,<br />
including the State Children’s<br />
Health Insurance Program (SCHIP).<br />
Recently, SCHIP was back in the<br />
news. Congress twice reauthorized it,<br />
expanding coverage nationally from 6.6<br />
million to 10 million children.<br />
Unfortunately, President Bush vetoed<br />
Congress’ efforts.<br />
In October, Rep. Barbara Lee (D-<br />
<strong>Oakland</strong>) asked Children’s <strong>Hospital</strong> to<br />
host her press conference to rally support<br />
for SCHIP expansion. “If our children<br />
are not healthy, we don’t really have a<br />
future,” said Rep. Lee.<br />
WINTER 2007 5<br />
this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat<br />
ADVOCACY AT CHILDREN’S: Rep. Barbara Lee called for healthcare<br />
for all kids during a press conference she held at Children’s<br />
<strong>Hospital</strong>. Children’s President and CEO Frank Tiedemann looks on.<br />
Children’s <strong>Hospital</strong> is proud to<br />
collaborate with Rep. Lee and others,<br />
whether it’s to support children’s health<br />
insurance, graduate medical education<br />
funding—which helps train the next<br />
generation of pediatricians—or obesity<br />
research and funding.<br />
Children’s <strong>Hospital</strong>’s advocacy program—the<br />
Child Advocacy Network<br />
(CAN)—will speak up for those who<br />
can’t speak up for themselves.<br />
To receive updates and advocacy<br />
alerts, go to Children’s <strong>Hospital</strong>’s Web<br />
site, www.childrenshospitaloakland.org,<br />
and click on the “Join Us” tab. From<br />
there, click on “Advocate for children,”<br />
and sign up for Children’s CAN. ★
6<br />
CHILDREN’S HANDPRINTS<br />
this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat<br />
ROMAN BEFORE AND AFTER: (Left) Little Roman on his blankie at home before his surgeries. (Right) Roman visits<br />
Children’s, with a smiling mom and dad, after his surgeries.<br />
CLEFT LIP SERVICES<br />
Getting ready<br />
for Roman<br />
<strong>With</strong> a <strong>prenatal</strong> diagnosis,<br />
Children’s team helps a<br />
family prepare.<br />
Robin and Rodrigo Leigh went for a<br />
routine ultrasound during the twentieth<br />
week of Robin’s pregnancy. The technician<br />
reading the images pointed out two feet,<br />
two hands, two eyes. “Then she got really<br />
quiet,” Robin recalled, “when she got<br />
around to the mouth.” The baby, they were<br />
informed, had a cleft lip and possibly a<br />
cleft palate.<br />
The Leighs were immediately referred<br />
to the Craniofacial department at<br />
Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong><br />
<strong>Oakland</strong>. Nurse practitioner Peg Langham,<br />
RN, MS, PNP, took Robin’s call and<br />
assured her that everything would be OK.<br />
www.childrenshospitaloakland.org<br />
this<br />
ANDthat<br />
Peg became the Leighs’ guide through the<br />
coming months.<br />
When a 3-D sonogram more accurately<br />
portrayed the baby’s condition, the Leighs<br />
shared the images with Peg and with<br />
Bryant Toth, MD, a Children’s plastic surgeon,<br />
who would repair the lip and palate.<br />
“Dr. Toth showed us his past work,”<br />
Robin said. “He spent a lot of time making<br />
us feel comfortable.”<br />
Not that there weren’t anxious<br />
moments ahead.<br />
“Don’t get me wrong, I did panic,”<br />
Robin acknowledged.<br />
Roman Leigh was born on Sept. 10,<br />
2006, “an adorable 8-pound, 21-inch<br />
happy little boy,” Robin remembered.<br />
Roman’s first stop, before even going<br />
home, was Children’s <strong>Hospital</strong>. There he<br />
smiled for nurse Peg.<br />
Peg assured them that Roman looked<br />
fine. She scheduled the first surgery before<br />
the holidays, so Robin could start back to<br />
this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat this<br />
ANDthat<br />
work afterwards.<br />
A few weeks later, the Leighs met oneon-one<br />
with Children’s interdisciplinary<br />
baby panel, including a speech pathologist,<br />
an otolaryngologist (ENT specialist), Dr.<br />
Toth and Elio Gizzi, MD, medical director,<br />
Craniofacial department.<br />
“I told them what I tell all parents,”<br />
Dr. Gizzi explained, “that our goal, if we<br />
do our job correctly, is to make sure parents<br />
get to be parents, and not medical<br />
coordinators.”<br />
On Dec. 5, in a three-hour operation,<br />
Dr. Toth repaired Roman’s lip. Seven<br />
months later, he repaired Roman’s palate.<br />
His picture is worth a thousand words.<br />
“I don’t think we could have asked for<br />
anything more from Children’s,” Rod said.<br />
“They were so well organized, we didn’t<br />
have to worry about the process. Peg, being<br />
our main contact, was always there for any<br />
question. She was there from beginning to<br />
end. She’s still there.” ★
Patients at Children’s <strong>Hospital</strong> &<br />
<strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong> no<br />
longer have to be moved out of<br />
the intensive care unit or operating<br />
room to get a CT scan. Children’s is<br />
now the first and only pediatric medical<br />
center on the West Coast to have and<br />
use the portable CereTom CT scanner.<br />
The CereTom minimizes risk and<br />
saves time by eliminating the need to<br />
transport critical patients from a hospital<br />
bed or operating room to the Diagnostic<br />
Imaging department.<br />
Mounted on wheels, and able to pass<br />
through any standard doorway, the unit<br />
can easily be moved to where it’s needed,<br />
mostly intensive care units and operating<br />
rooms.<br />
Diagnostic Imaging technologists<br />
will primarily use the new scanner to<br />
examine children having a variety of<br />
head or neck conditions. Each year,<br />
Children’s treats nearly 300 children<br />
with serious head injuries and performs<br />
more than 350 neurosurgical procedures<br />
that could require an immediate CT<br />
scan.<br />
“Children’s is committed to the latest<br />
technology that benefits clinical<br />
care,” said Peter Sun, MD, Children’s<br />
<strong>Hospital</strong>’s Neurosurgery medical director.<br />
“The portable CereTom scanner<br />
brings the CT scanner to the patient in<br />
the OR during surgery, where we can<br />
get a clear and immediate image of surgical<br />
results. It also brings the scanner to<br />
the ICU, eliminating the need to transport<br />
some critically ill patients to the<br />
CT scanner in Diagnostic Imaging.”<br />
This state-of-the-art technology,<br />
WINTER 2007 7<br />
Diagnostic Imaging: Children’s <strong>Hospital</strong> is first pediatric<br />
medical center on West Coast to get<br />
portable<br />
CT scanner<br />
ROLL ‘EM: Hauwie Nguyen, RT(R), CRT, at left, and David Westwater, RT(R), CRT,<br />
roll Children’s <strong>Hospital</strong>’s portable CT scanner out of the OR.<br />
Written and photographed<br />
by Tom Levy.<br />
developed by Massachusetts-based<br />
NeuroLogica Corporation, also integrates<br />
with Children’s Picture Archiving<br />
and Communications System (PACS).<br />
PACS allows physicians at Children’s to<br />
view all diagnostic imaging exams,<br />
including CereTom images, on any<br />
PACS-capable computer in the hospital.<br />
The CereTom is a wireless-capable,<br />
multi-slice system that’s able to generate<br />
up to eight slices per revolution.<br />
During operation, images are sent<br />
wirelessly to a portable workstation for<br />
viewing. The workstation resembles a<br />
large laptop computer with an accessory<br />
keyboard and mouse.<br />
Pediatric radiologists at Children’s<br />
<strong>Hospital</strong> have a long-standing interest in<br />
radiation safety, and will use their<br />
expertise to develop appropriate pediatric<br />
techniques for the CereTom, previously<br />
used mostly with adults.<br />
Although the machine was developed<br />
specifically for CT scanning of the<br />
head, in selected cases it may also be<br />
used to examine extremities or to do<br />
full-body scans of small infants in emergency<br />
situations.<br />
MRI upgrades speed<br />
imaging, add features<br />
Upgrading MRI capabilities at<br />
Children’s <strong>Hospital</strong>, a project begun in
8<br />
CHILDREN’S HANDPRINTS<br />
July, is enabling faster image reconstruction<br />
times, up to 33 percent faster, as<br />
well as new capabilities for cardiac,<br />
orthopedic and neurological imaging.<br />
Some of the newer techniques offer<br />
more than evolution; the newest capabilities<br />
in MRI are a diagnostic imaging<br />
revolution. What once gave only a static<br />
roadmap—anatomy—can now practically<br />
give a bird’s eye view of moving traffic—physiology.<br />
“It used to be that we depicted<br />
anatomy,” said Kenneth Martin, MD, a<br />
radiologist in Children’s Diagnostic<br />
Imaging department. “You do a CT<br />
scan—you see the bone, it’s white; you<br />
see the air in the lung, it’s black; you see<br />
the blood vessels and the soft tissues of<br />
the chest, they’re gray. There’s the anatomy.<br />
“Now, with some specialized MRI<br />
techniques, we’re looking at physiology.<br />
For example, when we look at the brain,<br />
in addition to simple vascular permeability<br />
or contrast enhancement, we can<br />
now image and quantify blood flow and<br />
water diffusion, and determine relative<br />
amounts of the chemical constituents of<br />
normal and abnormal metabolism.<br />
“What are these tissues doing? Are<br />
they producing neurons? If they are, we<br />
would see N-acetyl-aspartate (NAA indicates<br />
neuronal activity) elevated. If they<br />
are producing tumor cells, you would see<br />
choline elevated (associated with rapid<br />
cell growth).<br />
“Does the tissue display normal energy<br />
metabolism? If it were abnormal,<br />
you’d see lactic acid.<br />
“And we can detect all of those<br />
things. So we are looking not only at the<br />
size and shape of things these days; we’re<br />
also looking at physiology.”<br />
The combination of hardware and<br />
www.childrenshospitaloakland.org<br />
software upgrades gives<br />
Children’s <strong>Hospital</strong><br />
access to all MRI procedures<br />
shown to be useful,<br />
said Dr. Martin, one<br />
of seven Children’s radiologists—physicians<br />
specializing in diagnostic<br />
imaging.<br />
The upgrades allow<br />
for future expansion and<br />
upgradeability, as well as<br />
faster scans now.<br />
For example, the<br />
patient most frequently<br />
needing an MRI scan is<br />
a child suffering from<br />
seizures, said Dr. Martin.<br />
A thorough scan, including a minimum<br />
of eight sequences, which once took 42<br />
minutes, now only requires about 28<br />
minutes—a third less time.<br />
“These are kids who can’t lie there<br />
without moving the whole time; they<br />
have to be under general anesthesia,”<br />
said Dr. Martin. So shorter scan times<br />
also means a significantly shorter time<br />
under general anesthesia for these young<br />
patients.<br />
The hardware upgrade includes a<br />
new computer and digital amplifiers<br />
replacing analog amplifiers, allowing<br />
greater resolution and more future capabilities.<br />
Adding software upgrades gives<br />
Children’s Diagnostic Imaging department<br />
the ability to do perfusion scanning,<br />
tractography, functional imaging<br />
and spectroscopy.<br />
Perfusion scanning allows physicians<br />
to examine the quantity and quality<br />
of blood flow to particular tissues.<br />
This adds valuable insight to tumor and<br />
stroke imaging.<br />
PORTABLE CT SCANNER: The laptop at left shows<br />
an image from a pre-surgery scan of the patient<br />
at right, visible through the scanner’s circular<br />
opening.<br />
Tractography allows examination<br />
of how particular cortical and subcortical<br />
regions in the brain interconnect with<br />
each other by tracking individual axons.<br />
The color maps of interconnected axons<br />
that are generated depict pathways in the<br />
brain.<br />
Functional imaging uses the<br />
MRI’s ability to detect blood flow<br />
increases to regions of the brain during<br />
specific activities, such as speech and<br />
motor tasks. This can be useful for localizing<br />
certain functions in the brain<br />
before surgery.<br />
Spectroscopy allows Diagnostic<br />
Imaging experts to actually measure relative<br />
amounts of chemical constituents<br />
within the brain, providing valuable<br />
clues to metabolic diseases, stroke, infection<br />
and tumor imaging.<br />
For example, looking at relative<br />
choline levels may give an additional<br />
clue to a brain tumor’s borders because<br />
high levels of choline are associated with<br />
abnormally rapid cell growth, a cancer<br />
clue.
Zach<br />
A team of Children’s<br />
clinicians helps children<br />
and their families learn<br />
healthy living habits.<br />
Written and photographed<br />
by Tom Levy.<br />
Jesus<br />
Every day there’s more bad news<br />
about childhood obesity. People<br />
across the world, and their children,<br />
are getting fatter, and the number<br />
of children with obesity-related health<br />
problems grows. Healthcare providers fear<br />
they’ll one day drown under a tidal wave<br />
of people suffering from diseases associated<br />
with being overweight.<br />
But housed in the Gastroenterology<br />
department, one Children’s <strong>Hospital</strong> &<br />
<strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong> program is<br />
doing its best to shrink the wave, one<br />
child and one family at a time. The<br />
Healthy Eating Active Living (HEAL)<br />
program’s tight-knit cadre of clinicians<br />
helps lead kids and their families back to<br />
healthier ways of living.<br />
Zachary Fernandez, a bright and precociously<br />
articulate 8-year-old, calls him-<br />
WINTER 2007 9<br />
self an art geek and exercise-phobe. “He<br />
was struggling with his weight,” said<br />
Karin Schiffman, MD, his pediatrician.<br />
“He’d begun to realize it and was concerned<br />
about potential health problems.”<br />
Since Dr. Schiffman referred him to<br />
HEAL in June, Zachary is swimming<br />
after school twice a week and has given<br />
up soda, chips and Gatorade. He’s also<br />
added trampoline jumping and jumproping<br />
to his exercise regime.<br />
Jesus Rico, a HEAL teen, is active<br />
enough to have become a 15-year-old<br />
karate black belt. The thoughtful softspoken<br />
teen also enjoys playing basketball<br />
and soccer; he plays right midfielder with<br />
the Mustangs at St. Elizabeth High<br />
School in <strong>Oakland</strong>. But about a year ago,<br />
while his height wasn’t changing, he was<br />
steadily gaining weight.
10 CHILDREN’S HANDPRINTS<br />
Zachary calls<br />
himself an art geek<br />
and exercise-phobe.<br />
Since Dr. Schiffman referred him<br />
to HEAL in June, Zachary is<br />
swimming after school<br />
twice a week and has given<br />
up soda, chips and Gatorade.<br />
HEADFIRST: Zachary Fernandez takes swimming lessons twice a week after school at the King<br />
Swim <strong>Center</strong> in Berkeley. This and other activities, like jump-roping and trampoline jumping, at<br />
right, are helping him control his weight, and keeping him healthy and energetic.<br />
His pediatrician recommended quarterly<br />
weigh-ins. After a year of continued<br />
weight gain, his pediatrician referred him<br />
and his family to HEAL.<br />
Now, after completing the six-visit<br />
HEAL program and participating in two<br />
months of support group meetings, Jesus<br />
has sworn off calorie-packed Gatorade<br />
before soccer practice, gotten used to eating<br />
dinners that are steamed instead of<br />
fried and added inches to his height.<br />
HEAL’s ability to tailor its program to<br />
fit each kid is a plus for referring clinicians.<br />
“It’s well thought out and founded<br />
on the idea of developing a very individualized<br />
program geared to each specific<br />
patient,” said Mary Ann Franks, MD, of<br />
Alta Bates Summit Medical <strong>Center</strong> in<br />
Berkeley. “HEAL is intensive and patient<br />
oriented.”<br />
While most public health officials<br />
and researchers favor public policy fixes,<br />
www.childrenshospitaloakland.org<br />
some, like Joanne P. Ikeda, MA, RD, also<br />
see value in intervention programs like<br />
HEAL.<br />
“Providing treatment is important—<br />
there are too many 100-pound 5-yearolds<br />
and 200-pound 10-year-olds out<br />
there to ignore,” said Ikeda, nutritionist<br />
emeritus at the University of California,<br />
Berkeley’s School of Public Health.<br />
“Programs such as the one Children’s<br />
<strong>Hospital</strong> provides are important interventions—they<br />
can prevent the 100-pound<br />
5-year-old from becoming the 200pound<br />
10-year-old, and they can help the<br />
200-pound 10-year-old gradually achieve<br />
a healthier weight, rather than becoming<br />
a candidate for bariatric surgery.”<br />
For the HEAL team, led by Lydia<br />
Tinajero-Deck, MD, helping overweight<br />
kids is less about changing their weight<br />
and more about changing how they, and<br />
their families, eat and exercise. “It’s<br />
Zach<br />
important to teach parents how to be<br />
lifelong role models,” said Dr. Tinajero-<br />
Deck.<br />
The HEALers recognize that children<br />
don’t exist apart from their families; the<br />
family is a unit. An overweight child is<br />
also a symptom of a family needing help<br />
with food and activity choices.<br />
Red flags to obesity risk:<br />
• Rapid weight gain, more than 1 pound<br />
a month<br />
Tip for parents: Ask your pediatrician<br />
how your child is growing.<br />
• Drinking lots of sugary beverages, such<br />
as soda and juice<br />
• Little to no physical activity<br />
• Eating junk food or fast food every day<br />
• Eating little to no fruits and vegetables<br />
(lack of a balanced diet)
HEALing your home: Daily eating tips<br />
5—4—3—2—1—0—lift off<br />
5: Eat 5 servings of fruits and vegetables a day.<br />
4: Drink a minimum of 4 glasses of water, instead of sugary beverages,<br />
every day.<br />
3: Eat an average of 3 servings of dairy-based foods every day.<br />
2: Limit daily screen time to 2 hours or less.<br />
1: Get 1 hour or more of physical activity or exercise daily.<br />
0: Avoid eating fast food and junk food every day<br />
“Before the program, I had the habit<br />
of cooking a lot of pork and a lot of<br />
fried foods,” said Jesus’ mother, Alma,<br />
through a Spanish interpreter. “Now I’ve<br />
learned to steam a lot of foods, including<br />
pasta and vegetables, and only serve<br />
pork maybe once a month, if at all.”<br />
It can be hard for parents to accept<br />
the power they have over their child’s<br />
health. But as Spiderman’s uncle famously<br />
told him in the web-slinger’s first<br />
movie, “<strong>With</strong> great power comes great<br />
responsibility.” Jesus’ mother gets it.<br />
“I came to terms with the fact that<br />
this was all in my hands,” said Alma.<br />
“I’m the mom, and they’re going to eat<br />
what I cook. And I’m the only one who<br />
decides what they’re going to eat.”<br />
Now, instead of cases of Gatorade<br />
on the dining room floor of their San<br />
Leandro home, there are cases of water<br />
and Propel, a fruit-flavored water-based<br />
drink. Propel boasts 25 calories per 20ounce<br />
bottle, far less than Gatorade’s<br />
125.<br />
A recent Sunday lunch featured halibut,<br />
cooked in small amounts of butter,<br />
served with steamed pasta mixed with<br />
shredded carrots. There were also raw<br />
baby carrots and broccoli on the side.<br />
Alma and her husband, Francisco, meat<br />
cutters at an <strong>Oakland</strong> grocery store,<br />
shared cooking duties.<br />
Even Spiderman would stay healthy<br />
on food like that.<br />
* * * * *<br />
At the Fernandez family’s home in<br />
Berkeley, Zachary’s father, Rick, handles<br />
most grocery buying and cooking. He<br />
learned to cook from his father, a restaurant<br />
chef. Rick ticks off some of the<br />
many changes in the family’s eating<br />
habits. “I stopped buying potato chips,”<br />
said Rick. “No more chips, we have<br />
crackers instead.”<br />
“Crackers and cheese!” adds<br />
Zachary.<br />
Rick also got a salad spinner, the<br />
better to prepare the many salads the<br />
family is now eating. He lists more<br />
changes: reading food labels, no more<br />
fried chicken, burgers made with turkey<br />
instead of beef, no more juice boxes,<br />
and using soy and nonfat milk instead<br />
of whole milk.<br />
“We also stopped going to fast food<br />
places,” said Rick. “We haven’t been to<br />
McDonald’s in three months.”<br />
Rick’s mother, who loves to cook,<br />
also supports his family’s health efforts.<br />
“(Rick’s mom) has been telling us for<br />
the longest time to quit the soda, to quit<br />
this, to quit that,” said his wife,<br />
Camille.<br />
* * * * *<br />
But it’s not always easy to shift culinary<br />
gears. Alma and Francisco, childhood<br />
sweethearts, were born and raised<br />
in Mexico City. They, Jesus and their<br />
two daughters were used to traditional<br />
WINTER 2007 11<br />
Mexican-style foods.<br />
There were complaints when Alma<br />
took the HEAL sessions to heart. “It was<br />
hard, because we just changed (food<br />
habits) from one day to another,” said<br />
Jesus.<br />
His mother agrees. “Believe me, in<br />
the beginning there were a lot of struggles,<br />
a lot of verbal arguments, a lot of<br />
resistance,” said Alma. “But I’ve learned<br />
how to overcome the resistance, perhaps<br />
to ignore it to a certain extent.”<br />
She not only stopped frying, she<br />
even cut way back on some Mexican<br />
favorites. “From one day to the next I<br />
stopped buying Mexican sweetbread,<br />
which is a huge staple,” said Alma, “and<br />
that was hard.”<br />
She also reduced how often she<br />
serves atole de maiz to the children<br />
before school. Atole (ah-tollay), a hot,<br />
creamy corn beverage, can be sweetened<br />
with high-calorie extras like sugar, honey<br />
or chocolate. Adding sweeteners, a common<br />
practice in many cultures, quickly<br />
turns a wholesome beverage or food<br />
from nutritious to unhealthy.<br />
The Fernandez family had its<br />
favorites, too. “Ice cream was our downfall,”<br />
said Zachary’s mother, Camille.<br />
They’ve now switched to frozen yogurt.<br />
* * * * *<br />
The families’ progress showcases<br />
HEAL’s emphasis on education and<br />
motivation. Zachary still remembers<br />
HEAL nutritionist Afroz Subedar showing<br />
them how much sugar is in a bottle<br />
of soda. Afroz stresses the importance of<br />
reading and comparing food labels.<br />
“We offer families ideas about how<br />
to make healthy food choices,” said<br />
Afroz, “then let them decide what they<br />
want to work on.”<br />
Family members are now reading
12<br />
CHILDREN’S HANDPRINTS<br />
www.childrenshospitaloakland.org<br />
“I came to terms with the fact<br />
that this was all in my hands,”<br />
said Jesus’ mother, Alma. “I’m the mom,<br />
and they’re going to eat what I cook. And I’m the<br />
only one who decides what they’re going to eat.”<br />
HEALTHY FAMILY LUNCH: At Sunday lunch, Jesus’ mom, Alma, and her husband, Francisco, serve a healthy lunch of halibut,<br />
pasta, and raw broccoli and carrots. Jesus joins his parents and his 6-year-old sister, Karla, at the family’s dining room table.<br />
HEAL program:<br />
Six visits<br />
Jesus<br />
1) Meet with physician or nurse practitioner:<br />
Help the patient to know their strengths.<br />
Identify barriers to doing the right thing.<br />
2) Dietitian: Keep a food diary.<br />
3) Exercise specialist: Do aerobic activity four<br />
days a week for 30 minutes and you’ll have a<br />
healthy heart, stronger body, more energy<br />
and improved self-esteem.<br />
4) Health counselor: Get motivated. See your<br />
strengths, challenge your barriers, develop<br />
self-confidence and deal with teasing.<br />
5) Nutrition: Eat fruits and vegetables regularly.<br />
6) Make a plan: How to make HEALing an ongoing<br />
priority in your life, with help from your<br />
pediatrician.<br />
food labels and avoiding high-calorie foods and high-calorie preparation<br />
techniques like frying.<br />
Both families also encourage healthy choices: in food—more<br />
fruits and vegetables, and more salads—and in activity—less TV<br />
and more walking. “Yesterday we had to go to the mall and<br />
(Zachary) skipped the escalator, taking the stairs, without being<br />
asked,” said Camille.<br />
The customized HEAL experience is about the child and their<br />
family. As Zachary goes, so goes the Fernandez family.<br />
“The HEAL program seemed like a great way to get the whole<br />
(Fernandez) family involved,” said Dr. Schiffman. “When<br />
(Zachary) comes into the office, he’s so proud of what he can do<br />
physically. He’s looking for new ways to make his body his own.”<br />
For more information about the HEAL<br />
program at Children’s <strong>Hospital</strong>, call the<br />
HEAL Line at 510-428-3762 or visit their Web page<br />
at www.childrenshospitaloakland.org.
Written and photographed by Gary Turchin.<br />
Adrianna has a fighting<br />
spirit. She needed every<br />
ounce of it to kick leukemia.<br />
Now she’s back to kicking<br />
what 11-year-olds are supposed<br />
to kick: soccer balls.<br />
A drianna Tucker is tough. The 11-year-old Castro<br />
Valley youth has a first-degree black belt in karate<br />
and can hold her own against most boys her age. She<br />
runs the fastest mile of any girl in her class, has a killer<br />
soccer kick and regularly enjoys off-road dirt biking<br />
with her “G-Pa Ray,” a retired 29-year veteran of the
14<br />
CHILDREN’S HANDPRINTS<br />
Alameda County Sheriff’s<br />
department. Her mom,<br />
Lauren, also works in the<br />
department, as a detective in<br />
the sex crimes unit. It’s a<br />
tough family.<br />
But back in October 2005,<br />
Adrianna wasn’t feeling tough. She lasted<br />
only five minutes in a soccer game<br />
before she raised her hand to be subbed<br />
out.<br />
“I was tired,” she recalled. “That<br />
was real unusual for me. I don’t get tired<br />
easily.”<br />
Later that weekend, while dirt biking<br />
with Grandpa Ray, Adrianna couldn’t<br />
keep up. “I was going real slow, normally<br />
I bump into his tires…. I was<br />
lethargic.”<br />
Lethargic?<br />
“Yeah, I know almost all the words<br />
from the hospital now.”<br />
In days to come she felt even worse.<br />
Lauren took Adrianna to their pediatrician<br />
and insisted on a blood test. The<br />
next day, the pediatrician called Lauren<br />
and reported that Adrianna was severely<br />
anemic and needed to go to Children’s<br />
<strong>Hospital</strong> <strong>Oakland</strong> right away.<br />
“Grandpa picked me up and took<br />
me, and mom met us there,” Adrianna<br />
recalled.<br />
At Children’s, Adrianna was given<br />
another blood test and was admitted.<br />
Children’s doctors also ordered a bone<br />
marrow test.<br />
The bone marrow test revealed the<br />
diagnosis: acute myelogenous leukemia<br />
(AML), a very aggressive kind of<br />
leukemia. Only about 15 percent of the<br />
2,000 pediatric leukemia cases seen in<br />
www.childrenshospitaloakland.org<br />
ALL SMILES: (Previous page) It’s high fives for<br />
Adrianna and her teammates after a soccer<br />
match in Hayward. She played almost the entire<br />
game, and still had plenty of energy when it was<br />
over. (Above) Adrianna on the couch at home,<br />
showing off for Grandpa Ray. (<strong>Center</strong>) In her<br />
backyard, hugging her pooch. (Far right) Back on<br />
the soccer field, running down the ball. (Right)<br />
Lauren and Adrianna are all hugs after the game.<br />
the United States every year are AML.<br />
The AML had moved through<br />
Adrianna’s system so fast that 85 percent<br />
of her bone marrow cells were leukemic.<br />
<strong>With</strong>out treatment, she was only weeks<br />
from death.<br />
“On that day (Nov. 3, 2005) I got a<br />
room, and that’s how everything started,”<br />
Adrianna remembered.<br />
Her room was in Children’s 5 South<br />
Immunocompromised unit; and she was<br />
put on chemotherapy immediately by<br />
Elliott Vichinsky, MD, division chief of<br />
Hematology/Oncology.<br />
“AML is very aggressive and requires<br />
extremely intensive therapy,” Dr.<br />
Vichinsky explained.<br />
For the next five months, she stayed<br />
on repeating cycles of chemotherapy:<br />
blast away at the AML cells, wait for her<br />
blood counts to recover, blast away<br />
again. Recover. Blast.<br />
It was very intense.<br />
How did she cope?<br />
“I honestly think, that when I was in<br />
there, that this is a life and death situation.<br />
There’s no changing it, you have it<br />
and you can’t refuse it.<br />
“I have a saying: God won’t give me<br />
anything that I can’t handle…. I was so<br />
physically and mentally strong that I<br />
coped with it better than some, and I<br />
think my body took in the chemo<br />
well…. I personally think if I did not<br />
have my attitude, I would have died.”<br />
Over the ensuing months, she and
her family watched her leukemia count<br />
dwindle to 15 percent, then 2 percent,<br />
then less than 1 percent. But the treatments<br />
took their toll.<br />
“I handled it well, but the last seven<br />
weeks, I could hardly walk, my bones<br />
were in pain, I was so sick, I could barely<br />
hold my legs up.” She also broke out<br />
in rashes, had burns in her esophagus,<br />
nonstop fevers and painful swollen<br />
lymph nodes.<br />
“I had to say in my head, ‘I’ve got to<br />
make it through this. I will not die from<br />
this. I will not surrender. I’m not going<br />
to give up.’<br />
“It doesn’t take mercy on anyone. I<br />
was looking at pictures in the hospital,<br />
of my friends who were there, too, and<br />
this disease really is ruthless; it doesn’t<br />
“I had to say in my head,<br />
‘I’ve got to make it<br />
through this. I will<br />
not die from this. I will not<br />
surrender. I’m not<br />
going to give up.’”<br />
show mercy to anyone. It will kill you.”<br />
Protocol for her treatment was six to<br />
nine months of chemotherapy. But<br />
because she recovered so well between<br />
treatments, and didn’t have to wait too<br />
long for her next cycle, she was able to<br />
complete the course in five months.<br />
Finally in remission, with her<br />
immune system restored, she went<br />
home. Two weeks later she went to summer<br />
camp and climbed a rope course<br />
through the trees. A couple of months<br />
after that, at her first soccer game since<br />
coming home, she scored four goals.<br />
Then she finished her black belt test,<br />
after a grueling 10-hour day. And she<br />
recently ran a 7:26 mile, the fastest for<br />
any girl in her PE class.<br />
“Never surrender,” she says of her<br />
WINTER 2007 15<br />
ordeal. “How do you know you can get<br />
through it if you don’t try? If you have<br />
courage and you have heart and you<br />
have the right attitude, anything you<br />
put your mind to, you can do.”<br />
If you’d like to contact<br />
Dr. Vichinsky,<br />
or learn more<br />
about Children’s<br />
Hematology/Oncology<br />
department, please call<br />
510-428-3372.
16<br />
CHILDREN’S HANDPRINTS<br />
www.childrenshospitaloakland.org<br />
Written and photographed by Tom Levy.
For a parent, there’s nothing more<br />
important than feeding their<br />
child. Parents often feel they’re<br />
failures when their baby has trouble<br />
making the transition from liquid to<br />
solid food.<br />
But telling the difference between a<br />
picky eater and a child with a feeding<br />
problem is a combination of art and science.<br />
For mother Lisa Turner, whose last<br />
name has been changed at her request to<br />
protect her privacy, the fear came when<br />
her daughter, Carly, was 10 months old.<br />
Carly wouldn’t transition from breastfeeding<br />
to a bottle or sippy cup; she<br />
gagged on purees or solid foods.<br />
Since Carly took nothing but breast<br />
milk from mom and wouldn’t accept it<br />
from a bottle, Lisa couldn’t leave her<br />
daughter’s side for more than a few hours<br />
or even let another caregiver feed her. “I<br />
was depressed,” said Lisa. “I just could<br />
not ever get a break from her, knowing<br />
she was constantly dependent on me. I<br />
didn’t know when it was ever going to<br />
end.”<br />
Her pediatrician’s staff tried to help,<br />
and Lisa tried all their suggestions. None<br />
were effective. “My intuition was saying,<br />
this is not it,” said Lisa. “When I had a<br />
cup out there with baby food, Carly<br />
would start crying. We were trying anything,<br />
even cookies; Carly would look at<br />
it, touch it and feel it, but put nothing<br />
in her mouth.”<br />
Pediatrician refers to Children’s<br />
By the time Carly had her 9-month<br />
well-baby visit, Lara Lembach, MD,<br />
Carly’s pediatrician, also knew something<br />
was wrong. “I knew there was a problem,<br />
because most babies by this age are also<br />
taking other foods, including table<br />
food.” She referred Carly to<br />
Occupational Therapy in the Pediatric<br />
Rehabilitation department at Children’s<br />
<strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong>.<br />
Dr. Lembach, who has practiced in<br />
the Bay Area since 1998, had referred<br />
patients to Children’s many times, but it<br />
was the first time for a feeding problem.<br />
“Children’s is a good partner to the pediatricians<br />
in our area,” said Dr. Lembach.<br />
“Children’s is very well known and well<br />
respected.”<br />
OT’s evaluation is first step<br />
In October 2006, Amelia Foos, MS,<br />
OTR/L, a Children’s occupational therapist<br />
specializing in feeding disorders,<br />
began working with Carly and Lisa.<br />
Amelia always begins with a thorough<br />
evaluation of the child, the parents<br />
and their interaction. In this case, she<br />
WINTER 2007 17<br />
determined that Carly had oral hypersensitivity<br />
and more rudimentary oral motor<br />
skills than expected for her age. She<br />
noticed the youngster wasn’t exploring<br />
the world with her mouth, the way most<br />
kids her age do.<br />
Amelia, like other Children’s OTs,<br />
takes a holistic approach. She doesn’t<br />
analyze a problem in isolation. She gathers<br />
a detailed history, observing the<br />
child’s mechanical abilities and skills, and<br />
their social interactions with caregivers<br />
and family members.<br />
She emphasizes how charged feeding<br />
issues can be: “Many parents feel that ‘If I<br />
can feed my child, I’m a good caregiver.’”<br />
Amelia started off with three recommendations<br />
for Lisa:<br />
Increase nonfood oral stimulation<br />
to reduce oral hypersensitivity<br />
MODELING HEALTHY EATING BEHAVIOR: (Previous page) Occupational therapist Amelia<br />
Foos, at right, models feeding behavior while working with Carly and her mom, Lisa. Playful<br />
food items like red licorice can be used to help children with feeding disorders.<br />
(Below) During a session, Amelia tries to make eating new foods more fun for Carly by<br />
showing how much she likes trying new foods herself.
18<br />
CHILDREN’S HANDPRINTS<br />
Structure mealtime so Carly would<br />
anticipate the routine<br />
Develop oral-motor exercises.<br />
Lisa introduced oral stimulation into<br />
play with Carly, including gum massage,<br />
with a finger and a toothbrush. She also<br />
developed a detailed plan for mealtime<br />
structure, including food positioning;<br />
when to offer food, especially new foods;<br />
and eliminating distractions, to increase<br />
family mealtime socializing.<br />
It was all designed to help desensitize<br />
Carly to oral stimulation, minimize her<br />
discomfort around new foods and textures,<br />
and improve her oral motor skills<br />
and sensorimotor capabilities.<br />
For example, Lisa might place a snack<br />
in Carly’s mouth back by her molars,<br />
instead of in the front, encouraging<br />
Carly’s developing chewing skills. Or she<br />
might place food in the side of Carly’s<br />
mouth, so she’d have to use her tongue to<br />
retrieve it.<br />
Sensitivity to sensory stimulation<br />
affects feeding behavior<br />
While no medical “cause” was identified<br />
for Carly’s feeding disorder, Amelia<br />
stresses that children’s tolerance for sensory<br />
stimulation and sensorimotor abilities<br />
varies across a spectrum, just like those of<br />
adults.<br />
In some children with high sensitivity<br />
to sensory stimuli like textures and flavors,<br />
or who have less developed oral<br />
motor skills, feeding behavior can be disturbed<br />
when transitioning to solids.<br />
The key to helping a child and caregiver(s)<br />
is identifying a problem quickly,<br />
analyzing it carefully and developing a<br />
detailed plan for child and caregiver to<br />
follow, whether or not there are also medical<br />
complications.<br />
Six months and 14 clinic visits later,<br />
Carly had graduated to taking liquids<br />
from a cup; was tolerating oral stimula-<br />
www.childrenshospitaloakland.org<br />
tion, including toothbrushing; and was<br />
eating a good variety of age-appropriate<br />
solid foods.<br />
She’d also put on weight, going from<br />
the 20th to the 45th percentile for her<br />
age. At her 15-month well-baby visit, Dr.<br />
Lembach saw that Carly had “vastly<br />
improved.”<br />
By then, Lisa had also achieved a personal<br />
goal, taking a shopping trip to a<br />
nearby mall. It was proof that Carly’s<br />
feeding ability had improved and that<br />
mom could get needed breaks.<br />
“It was an easy process,” said Lisa.<br />
“Amelia is just fantastic. She told me<br />
exactly what to do and I would just do it<br />
at home. I highly recommend (the<br />
Children’s program). Once Amelia gave<br />
us information, about the oral defensiveness<br />
and sensory issues, it made everything<br />
more understandable.”<br />
Fortunately, in Carly’s case, there were<br />
no medical complications. When there<br />
are complications, such as aspiration<br />
problems or a gastrostomy tube, the<br />
Pediatric Rehabilitation Medicine team<br />
works with other Children’s specialists<br />
from across the entire hospital.<br />
Lisa was part of the rehab team too.<br />
Over the course of Carly’s treatment she’d<br />
collected an inches-thick binder of her<br />
own notes. “This is also why Carly did so<br />
well,” said Amelia, indicating the binder.<br />
“Mom was motivated and showed excellent<br />
use of our techniques at home.”<br />
To make a referral to<br />
the Occupational<br />
Therapy team at<br />
Children’s Pediatric<br />
Rehabilitation Medicine<br />
department, or to get more<br />
information about feeding<br />
disorders, call 510-428-3885, ext.<br />
2821. Ask for Sue Edelmann, OTR/L, the<br />
Occupational Therapy coordinator.<br />
Amelia Foos, an occupational therapist on<br />
the Rehabilitation Medicine team at<br />
Children’s <strong>Hospital</strong>, offers simple rules of<br />
thumb for pediatricians and parents to<br />
keep in mind, courtesy of veteran feeding<br />
disorders expert Kay A. Toomey, PhD.<br />
Red flags for feeding<br />
disorders<br />
When to ask for help:<br />
• Ongoing poor weight gain or weight<br />
loss<br />
• Ongoing choking, gagging or coughing<br />
during meals<br />
• Ongoing problems with vomiting<br />
• More than one incident of nasal reflux<br />
• History of a traumatic choking incident<br />
• History of eating and breathing<br />
coordination problems, with ongoing<br />
respiratory issues<br />
• Inability to transition to baby food<br />
purees by 10 months of age<br />
• Inability to accept any table food<br />
solids by 12 months of age<br />
• Inability to transition from breast/<br />
bottle to a cup by 16 months of age<br />
• Has not weaned off baby foods by 16<br />
months of age<br />
• Aversion or avoidance of all foods in<br />
specific texture or food group<br />
• Food range of less than 20 foods,<br />
especially if foods are being dropped<br />
over time with no new foods replacing<br />
those lost<br />
• An infant who cries and/or arches her<br />
back at most meals<br />
• Family is fighting about food and<br />
feeding (i.e., meals are battles)<br />
• Parent repeatedly reports that the<br />
child is difficult for everyone to feed<br />
• Parental history of an eating disorder,<br />
with a child not meeting weight goals<br />
Reprinted with permission of the author.<br />
© 2002 by Kay A. Toomey, PhD
Children’s chief of<br />
Adolescent Medicine,<br />
and advocate-in-chief<br />
for adolescents everywhere,<br />
talks about her<br />
life and the motivation<br />
for her work.<br />
Written and<br />
photographed by Gary Turchin.<br />
Barbara Staggers, MD<br />
As a teenager, Barbara Staggers, MD, chief of the division of<br />
Adolescent Medicine, Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong><br />
<strong>Oakland</strong>, had the usual girlhood dreams: to be a ballerina (she<br />
was a professional at age 10) or maybe a veterinarian (she loves<br />
all sorts of critters). But the summer of her 18th year changed<br />
everything.<br />
Working at a summer sports program for inner-city youths at what was then Cal<br />
State Hayward, the young Barbara Staggers—a naval officer’s daughter, a scholar, a<br />
somewhat protected child—watched as “a pimp” pulled up to claim a 14-year-old<br />
girl who was in her class. When phoned, the girl’s mother instructed the program<br />
director to let her daughter go because they “needed the money.”<br />
The future Dr. Staggers was “appalled,” as much by the mother as the man.<br />
Something deep inside of her—a social conscience, a righteous indignation, a passion<br />
for making a difference—was awakened.<br />
“I was 18,” she said, “I’m 53 now, and I can still close my eyes and see that<br />
young lady’s face. I don’t know what happened to her; maybe she got killed that<br />
night, maybe she was too embarrassed to come back. She just disappeared off the<br />
face of the Earth, but I’ll never forget her.”
20<br />
CHILDREN’S HANDPRINTS<br />
Later that summer her dad’s oldest<br />
brother went into an emergency room in<br />
Southern California with chest pains.<br />
While the receptionist dilly-dallied—<br />
she was more focused on whether the<br />
hospital would be paid than on admitting<br />
him—her uncle died. A hospital<br />
administrator called her father to apologize.<br />
“He told my father, ‘If we’d have<br />
known (his brother) was a doctor, we’d<br />
have treated him differently.’”<br />
Whatever woke her up earlier that<br />
summer now roared out of its gate. The<br />
overachieving, well-rounded young<br />
lady—ballet dancer, pom-pom girl,<br />
debutante, with the world at her finger-<br />
www.childrenshospitaloakland.org<br />
tips—was ready to do battle to help the<br />
most underrepresented, least-served population<br />
of all.<br />
“Those two incidents made me say,<br />
hmm, who gets screwed, who gets<br />
screwed the most?” Dr. Staggers<br />
explained. “Who has problems assessing<br />
healthcare? People of color. Who has the<br />
most trouble? Teens. After that it was<br />
clear to me, I wanted to do adolescent<br />
healthcare, and deal with youth.”<br />
She found her mission, and she hasn’t<br />
strayed an inch from it since.<br />
Medicine in her blood<br />
It should have been little surprise<br />
that Dr. Staggers chose medicine for her<br />
COUNSELOR, DOCTOR: Dr. Staggers chats with a patient. Part of adolescent medicine<br />
for Dr. Staggers is talking to her patients, finding out what’s going on in their<br />
homes, heads and hearts.<br />
Dr. Staggers<br />
speaks on<br />
adolescence<br />
In a wide-ranging interview,<br />
Dr. Staggers talked about her life<br />
and vision. She also shared her<br />
perspective on dealing with<br />
adolescents. In the following<br />
excerpts, she tells it like it is, and<br />
then some.<br />
What I do know about adolescent<br />
healthcare is two<br />
things:<br />
1) All teens need to be parented;<br />
but they’re not necessarily<br />
going to thank you for parenting<br />
them, that’s normal. And<br />
parents have to be a teen’s parent<br />
and not their friend; and<br />
2) There has to be somewhere<br />
in a teen’s life unconditional<br />
love; one person that<br />
they can think about, look at<br />
and know is going love them<br />
unconditionally.<br />
Those two things are critical.<br />
It may not be a parent who<br />
loves them unconditionally. But<br />
there has to be that one person<br />
in their life that they know,<br />
come hell or high water, is<br />
going to be there for them.
I get asked: Is it OK for my son or<br />
daughter to be on the Internet 18<br />
hours a day?<br />
I tell them: Why would you as a parent<br />
think that that’s appropriate?<br />
Or is it OK to have a party with thirty<br />
17- to 18-year-olds in a room<br />
without an adult?<br />
Why would you think that’s OK?<br />
Part of good parenting, and you<br />
don’t have to be the perfect parent<br />
yourself, but you better find someone<br />
who can be the parent for your kid and<br />
can be there when you can’t be there.<br />
If you know you have a deficiency<br />
somewhere, or you know something is<br />
difficult for you to deal with, then be<br />
proactive instead of reactive. Go to<br />
another adult you trust, that you have a<br />
relationship with, and say, “This is my<br />
weakness, can you help me parent my<br />
child in this area?”<br />
That’s good parenting, not just<br />
ignoring it and hoping it goes away.<br />
Be strategic, have someone in place<br />
to be there when you can’t be. Have an<br />
extended family.<br />
Teens don’t expect parents to<br />
be perfect, but when you make a<br />
mistake, they expect you to admit that<br />
you’ve made the mistake. And that’s the<br />
piece that’s important. To them, it’s not<br />
that you are perfect, not that you are<br />
always 100 percent, not that you know<br />
everything; it’s that if you don’t know<br />
something, you’re willing to admit<br />
it and maybe you can go find it out<br />
together.<br />
They don’t expect you to have all the<br />
answers, but they expect you to help<br />
them get the answers.<br />
Here’s the beauty of it: When teens<br />
do well, the community is doing<br />
well. Because if we’re doing the right<br />
thing in the community, and it makes<br />
sense and it’s consistent, and they aren’t<br />
getting one message at home, one mes-<br />
sage on TV, one message in the church<br />
or mosque or synagogue, then the teen<br />
does well, they’re healthy, they don’t kill<br />
each other, don’t kill themselves, don’t<br />
kill anybody else.<br />
The other piece I love about<br />
adolescent healthcare is flipping<br />
the paradigm. There is nobody more<br />
energetic or more resilient than adolescents,<br />
and we don’t market that. We’re<br />
so busy putting them down, being afraid<br />
of them, we have this negative image of<br />
them, but we don’t invest in them in<br />
ways that help them develop what they<br />
need to have as adults: resiliency, flexibility,<br />
the ability to make decisions….<br />
We don’t celebrate these skills that we<br />
can develop in them, but boy, when you<br />
develop those skills, give them the<br />
opportunity, they’re off and running and<br />
they do phenomenal things.<br />
We’re good at punishing teens, we<br />
can lock them up if they go bad, but<br />
how do we reward them? What do<br />
they get when they get a good grade?<br />
What do they get when they don’t get in<br />
trouble? Where’s the pat on the back?<br />
WINTER 2007 21<br />
MENTOR, DOCTOR: In Adolescent Medicine’s compact office, Dr. Staggers consults<br />
with a resident about her patients.<br />
Where’s the reward?<br />
We don’t think about that. Where do<br />
they go if they don’t want to drink?<br />
Where do they go to have fun with their<br />
peers where it’s safe?<br />
We have lots of activities for little<br />
kids, play structures and parks, but we<br />
don’t think about party places for teens.<br />
What else besides sports is there for<br />
them? If they can’t play sports, how<br />
does the community embrace that other<br />
part of life? I like challenging communities<br />
to think about that…. What are you<br />
doing for teens? We don’t have that<br />
structured into society.<br />
You can’t be inconsistent with what<br />
you do with teens. You have to be<br />
honest, you have to be truthful. You<br />
can’t lie. That’s the kiss of death in<br />
adolescent healthcare; you’d be retired<br />
forever, out the door and never coming<br />
back. Teens keep you honest, that’s why<br />
people either love them or hate them. If<br />
you have something to hide, don’t be<br />
around a 14-year-old. That’s a bad<br />
thing, they go straight for the jugular.
22<br />
CHILDREN’S HANDPRINTS<br />
life’s work. It was in her blood.<br />
Her father, Frank Staggers, MD, was<br />
the first African-American surgical subspecialist<br />
the United States Navy ever<br />
trained. He was only the second<br />
African-American to be president of the<br />
California Medical Association. Dr.<br />
Staggers was one of nine surviving children<br />
of South Carolina sharecroppers—<br />
all of whom earned advanced degrees.<br />
To give it perspective: This was in the<br />
pre–civil rights movement segregated<br />
South.<br />
Her mom, Carolyn, a highly intelligent<br />
woman (she started college at 16)<br />
was born to an affluent West Virginia<br />
family—affluent because the Irish slaveholder<br />
who spawned the clan left his<br />
money to his only family, his slave<br />
family.<br />
Carolyn and Frank provided a structured<br />
and loving environment where the<br />
benchmark was “doing well, being the<br />
MANAGER, DOCTOR: (Above) At a working lunch in their conference room, Dr. Staggers meets with her Adolescent Medicine<br />
team, going over department business. (Next page) William, the oldest of Dr. Staggers’ three children, drops in to the office to visit<br />
with mom.<br />
www.childrenshospitaloakland.org<br />
best at whatever we wanted to do,” Dr.<br />
Staggers said.<br />
“When I look back on my life, the<br />
reason I was able to do the things I did<br />
and take the challenges I took, was<br />
because my parents always told us we<br />
were respected, we were valued, we were<br />
loved as human beings. I always had<br />
that safety net. I always knew I was<br />
loved. That gave me the freedom to do<br />
what I wanted to do.”<br />
Getting credentials<br />
What she wanted to do, was driven<br />
like a force of nature to do, was adolescent<br />
medicine. That required credentials,<br />
and she set out to get them with the<br />
same passion with which she would one<br />
day attack adolescent health issues.<br />
At the University of California,<br />
Berkeley, she was mentored by Reginald<br />
L. Jones, PhD, pioneer of the discipline<br />
of Black Psychology. Jones and his work<br />
had a huge impact on her—“it affirmed<br />
my identity,” she said—and she almost<br />
followed in his footsteps by applying to<br />
a doctoral psychology program. But<br />
Jones intervened.<br />
“He asked me: ‘Who writes the<br />
medication order—a psychologist or<br />
psychiatrist?’ I said the psychiatrist. ‘So<br />
who has control of the client?’<br />
“He knew getting an MD would<br />
give me more authority.”<br />
She earned her MD at the University<br />
of California, San Francisco (UCSF),<br />
(“Berkeley didn’t have a med school so I<br />
chose the closest one.”) in three years,<br />
and got a Masters of Public Health<br />
degree at Berkeley in her fourth year.<br />
“They told me nobody had ever<br />
done an MPH and an MD in four years<br />
before. Well, I said, that’s not my problem.<br />
“By the time I came to Children’s<br />
<strong>Hospital</strong> for a residency (in pediatrics), I
had an MPH. I had done community<br />
forums, I had had an opportunity to<br />
expand and grow.”<br />
After her residency, she returned to<br />
UCSF for her Adolescent Medicine fellowship.<br />
Then she came back to<br />
Children’s to practice what she<br />
preached—a holistic view of adolescent<br />
medicine that includes prevention, intervention,<br />
mentoring, youth development,<br />
community involvement, schools, social<br />
service agencies, grandparents, neighbors,<br />
pets and even some good old-fashioned<br />
doctoring.<br />
Adolescent Medicine as public<br />
health issue<br />
“Adolescent healthcare, to me, is<br />
about things that kill teenagers, and these<br />
are public health, not traditional medicine,<br />
issues,” Dr. Staggers explained.<br />
“You have to look at motor vehicle<br />
injuries, homicides, suicides. There’s not a<br />
pill or medicine or an antibiotic for those<br />
three things (which account for 65 percent<br />
of adolescent deaths nationally). I<br />
have to look at what’s going on with a<br />
teen, how they interface with the community,<br />
how the community interfaces with<br />
them.<br />
“My adolescent medicine paradigm is:<br />
Youth development. If you do youth<br />
development right, you do community<br />
development.”<br />
She continues:<br />
“My philosophy of adolescent healthcare<br />
is: Teens are wonderful mirrors of the<br />
society, where we’re either doing really<br />
well or really badly. Right now we’re not<br />
doing things really well. The things that<br />
are killing them are preventable. We have<br />
to ask ourselves, as a community … what<br />
exists out there in the world that puts<br />
them at risk, and how do we as adults<br />
take responsibility for these things?...<br />
That forces a real frank conversation in<br />
the community.”<br />
That’s a conversation Dr. Staggers relishes,<br />
whether it’s in community forums<br />
in Castro Valley, her longtime hometown,<br />
or at speakers forums around the country,<br />
or in physicians’ offices, where she is<br />
often consulted on adolescent health matters,<br />
or in school districts across the state,<br />
or in Sacramento, where she is called<br />
upon to inform policy.<br />
Reaching the community<br />
Today, Dr. Staggers manages a division<br />
that, thanks to her vision, reaches<br />
out into the community to serve underserved<br />
youth, her original goal.<br />
Under her guidance, Children’s has<br />
established two national-model high<br />
school–based health clinics in <strong>Oakland</strong>,<br />
the Chappelle Hayes Health Clinic at<br />
McClymond’s High School, and Youth<br />
Uprising, next to Castlemont High<br />
School. These are full-fledged medical<br />
and mental health clinics adjacent to two<br />
inner-city high schools, offering at-risk<br />
youth services on their own turf.<br />
Practicing at Children’s<br />
Dr. Staggers gives Children’s a lot of<br />
the credit for the success of her practice.<br />
“The beauty of Children’s is I can do<br />
everything from primary care to quaternary<br />
care—cutting-edge research and cutting-edge<br />
medical care working together—and<br />
cover any part of that spectrum I<br />
need to be involved in. If I feel I need to<br />
WINTER 2007 23<br />
“My philosophy of adolescent healthcare is:<br />
Teens are wonderful mirrors<br />
of the society, where we’re either<br />
doing really well or really badly. Right now<br />
we’re not doing things really well.”<br />
go to the research institute to ask Dr.<br />
Deborah Dean a question about chlamydia<br />
in the lab, I can talk to her about<br />
that. I can get the cutting-edge research.<br />
But I can also talk to a teenager in my<br />
office about doing mentoring and peer<br />
advocacy work to help them all stop getting<br />
chlamydia in the first place. What a<br />
fabulous place to work. I’m really thankful<br />
that I didn’t have to leave my community<br />
to find what I felt was needed in<br />
healthcare.”<br />
President of Medical Staff<br />
Next April, Dr. Staggers will serve<br />
Children’s in a new capacity: as president<br />
of the Medical Staff, an honor for which<br />
she was chosen by her peers.<br />
In April she will also receive the<br />
Regional Healthcare Champions award<br />
from the University of California,<br />
Berkeley, School of Public Health. She’ll<br />
add this to a host of other awards and<br />
honors, including the 2004 Peter E. Haas<br />
Public Service Award from UC Berkeley.<br />
The awards are nice, she acknowledges,<br />
but at the end of the day, it’s the<br />
work itself that moves her.<br />
“I get asked, ‘How come you have<br />
such passion for what you do?’ And I say,<br />
‘Because I love my work. I really do. I<br />
don’t like the stories I hear, but I can’t<br />
really think of anything else I’d rather do.’<br />
“I’m real clear that the only reason I<br />
exist is to do the work I’m doing.”<br />
Call to action:<br />
To contact Dr. Staggers<br />
and Children’s Teen Clinic,<br />
please call 510-428-3387.
24<br />
CHILDREN’S HANDPRINTS<br />
Children’s to stay in <strong>Oakland</strong>:<br />
Will rebuild next to current site<br />
PRESS CONFERENCE: Harold Davis, the chair of Children’s <strong>Hospital</strong> <strong>Oakland</strong>’s board of directors, made the official announcement of<br />
Children’s rebuilding plans at a Sept. 5 press conference, while <strong>Oakland</strong> Mayor Ron Dellums and City Council President Ignacio De La<br />
Fuente listened.<br />
Children’s <strong>Hospital</strong>’s board of<br />
directors approved a plan to<br />
keep Children’s <strong>Hospital</strong> &<br />
<strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong> in <strong>Oakland</strong>.<br />
The plan calls for rebuilding the hospital<br />
on land adjacent to its current site.<br />
Harold Davis, the board’s chair, made<br />
the announcement Sept. 5 at a press conference<br />
attended by Ron Dellums,<br />
<strong>Oakland</strong>’s mayor; Ignacio De La Fuente,<br />
<strong>Oakland</strong> City Council president; and<br />
Jane Brunner, the council member representing<br />
Children’s <strong>Hospital</strong>’s district.<br />
“Children’s <strong>Hospital</strong> & <strong>Research</strong><br />
www.childrenshospitaloakland.org<br />
<strong>Center</strong> <strong>Oakland</strong> will remain in<br />
<strong>Oakland</strong>,” said Harold, “and it will<br />
expand in its current location.”<br />
Mayor Dellums also signaled his<br />
approval. “It’s with extraordinary pleasure<br />
that I witness this announcement that<br />
Children’s <strong>Hospital</strong> will stay here in<br />
<strong>Oakland</strong>,” said the mayor.<br />
“First, (because) Children’s <strong>Hospital</strong><br />
is an icon in the city of <strong>Oakland</strong> and in<br />
this region, for its extraordinary service<br />
to children, the most precious resource in<br />
our community. It has demonstrated<br />
tremendous excellence in the treatment<br />
of children. And secondly, (because) this<br />
is a world-class research center as well.”<br />
Rebuilding location and plan<br />
The new hospital will be constructed<br />
on land between 52nd and 53rd streets,<br />
extending west from the curve of<br />
Highway 24 to the east sides of the parking<br />
garage and Outpatient <strong>Center</strong>. (See<br />
aerial view on page 26.)<br />
Once completed, the new hospital<br />
will increase Children’s capacity from<br />
171 on-site beds to 250 private patient<br />
rooms.
The identified site is about oneand-a-half<br />
acres, which may require<br />
building a 12-story building to accommodate<br />
the hospital’s needs.<br />
Children’s will continue to operate<br />
in its current facility during construction,<br />
expected to begin in 2010. The<br />
project must be completed by 2013 to<br />
meet the state’s deadline for seismic<br />
upgrades.<br />
Paying for rebuilding<br />
Children’s<br />
The project, estimated to cost<br />
about $700 million, will be financed<br />
through three primary sources, Harold<br />
said. First, Children’s has $100 million<br />
in the bank, $73 million of it from<br />
state Proposition 61 funds. A second<br />
statewide children’s hospitals proposition<br />
scheduled for the November 2008<br />
ballot, if successful, will provide<br />
Children’s another $100 million.<br />
Second, the Children’s <strong>Hospital</strong> &<br />
<strong>Research</strong> <strong>Center</strong> Foundation will raise<br />
$150 million through private donations<br />
(see page 28).<br />
Finally, Alameda County voters are<br />
being asked to approve a modest $2 a<br />
month parcel tax on the Feb. 5 presidential<br />
primary ballot. Called Measure<br />
A, the “Special Tax to Support<br />
Children’s <strong>Hospital</strong> Construction<br />
Program,” it will provide another $300<br />
million (see details in Q&A sidebar).<br />
Campaign to rebuild<br />
Children’s gathered enough signatures<br />
to get its property tax initiative<br />
on the Alameda County ballot. But<br />
A letter from Bertha Wright,<br />
Children’s <strong>Hospital</strong>’s founder, sent to<br />
Reverend Edward L. Parsons (later<br />
Bishop Parsons), was uncovered last<br />
month in the archives of the Episcopal<br />
Diocese of California. Suzanne<br />
Thompson, the diocese’s archivist, found<br />
the two-page handwritten letter, dated<br />
July 30, 1912. This was before the “Baby<br />
<strong>Hospital</strong>” opened.<br />
Suzanne notified Children’s<br />
Communications department and forwarded<br />
a copy.<br />
The letter, written on “Charity<br />
Organization Society of America”<br />
stationery, is a chatty note to “Mr.<br />
Parsons,” describing, among other<br />
things, the state of the hospital’s development,<br />
concerns about where it will be<br />
located and who will be in charge.<br />
The following is an excerpt from the<br />
letter:<br />
“Dear Mr. Parsons,<br />
Your card was received this afternoon<br />
and I want to thank you for it. I do so<br />
hope you are being able to rest and not<br />
having to preach the sermons for every<br />
minister for miles about. Ministers and<br />
doctors always seem in demand wherever<br />
they are. Miss Weed (Mabel Weed,<br />
WINTER 2007 25<br />
Letter from Children’s founder uncovered:<br />
“We have the best doctors of Berkeley and<br />
<strong>Oakland</strong> interested in the project....”<br />
Children’s cofounder) is still away on her<br />
vacation so nothing very thrilling happens<br />
at the office….<br />
The Baby <strong>Hospital</strong> is getting along<br />
very nicely. We have eight splendid doctors<br />
from Berkeley and will have nine from<br />
<strong>Oakland</strong>. I have interested <strong>Oakland</strong> and<br />
Berkeley churches so we have all our<br />
beds. The location still has to be decided<br />
but I think it will be somewhere on the<br />
border between here (Berkeley) and<br />
<strong>Oakland</strong>….<br />
Dr. McCleave (president of the Charity<br />
Organization’s board) is very anxious to be<br />
“chief in charge” but Miss Weed and I had<br />
a private talk with Mrs. Seabury (one of<br />
the hospital’s founding committee members)<br />
so I guess it will come out all right.<br />
We have the best doctors of Berkeley and<br />
<strong>Oakland</strong> interested in the project so I<br />
don’t see why it can’t be put right through<br />
now.”<br />
Rev. Parsons spoke at the Baby<br />
<strong>Hospital</strong>’s dedication on Sept 16, 1914.<br />
Dr. T. C. McCleave was on the medical<br />
staff, but was not its chairman.<br />
Children’s still has the best doctors<br />
in Berkeley and <strong>Oakland</strong>; everything did<br />
come out all right.<br />
A BIT OF HISTORY: A section of the letter (highlighted) stating, “The Baby <strong>Hospital</strong> is getting<br />
along very nicely. We have eight splendid doctors from Berkeley and will have nine from<br />
<strong>Oakland</strong>.”
26 CHILDREN’S HANDPRINTS<br />
the county board of supervisors asked<br />
Children’s to make some changes in the<br />
measure’s wording.<br />
Children’s agreed; the board<br />
approved the new version and then<br />
placed both versions on the ballot.<br />
While the first version is still on the<br />
ballot, Children’s <strong>Hospital</strong> is throwing<br />
its full support behind the new version—Measure<br />
A—and asks you to vote<br />
for it.<br />
www.childrenshospitaloakland.org<br />
To win, Measure A requires twothirds<br />
of the electorate to vote yes. If<br />
both measures pass, only the one with<br />
the most votes will become law.<br />
Please vote yes on Measure A, the<br />
“Special Tax to Support Children’s<br />
<strong>Hospital</strong> Construction Program.”<br />
Listening to neighbors<br />
<strong>With</strong> any large development project,<br />
communication and collaboration with<br />
the neighborhood are essential.<br />
Why does Children’s <strong>Hospital</strong><br />
<strong>Oakland</strong> need to be rebuilt?<br />
California law requires inpatient areas of<br />
hospitals to be built to withstand strong<br />
earthquakes by 2013. This triggered<br />
Children’s <strong>Hospital</strong> <strong>Oakland</strong>’s decision<br />
to rebuild. Rebuilding hospitals periodically<br />
also assures advances in medical<br />
technology are incorporated into the<br />
new or retrofitted buildings. It’s also<br />
important for Children’s, an East Bay<br />
icon since 1912, to be able to meet the<br />
future needs of Northern California’s<br />
growing population of children.<br />
Why does Children’s need to<br />
expand the number of patient<br />
beds?<br />
As Northern California’s population<br />
grows, the number of hospital beds at<br />
Children’s must also grow. For example,<br />
it’s estimated that our core service<br />
area population will grow by about<br />
10 percent by 2014.<br />
When will the new hospital open?<br />
Construction of the new medical center<br />
is expected to begin in 2010 and must<br />
be completed by 2013 to meet the<br />
state’s deadline for seismic upgrades.<br />
How much will a new hospital<br />
cost? How will it be paid for?<br />
Construction is currently estimated to<br />
cost approximately $700 million. The<br />
hospital plans to finance the new<br />
medical center through three primary<br />
sources:<br />
• $200 million in past and future state<br />
bonds, and money in the bank<br />
• $150 million raised through private<br />
donations<br />
• $300 million from a parcel tax<br />
measure on Alameda County’s<br />
February 2008 ballot.<br />
How will the tax measure work?<br />
Measure A, if approved, will raise $300<br />
million over 35 years through a modest<br />
$2 per month ($24 a year) parcel tax on<br />
residential properties in Alameda<br />
County, a $100 per year assessment on<br />
small non-residential properties and<br />
$250 per year for large nonresidential
properties. Homeowners over age 65<br />
and very low-income residents are<br />
exempt from paying the assessment.<br />
The money raised will pay off bonds<br />
used to finance a portion of hospital<br />
construction.<br />
Language in the measure assures that<br />
the funds will be used in Alameda<br />
County and that the county will be<br />
compensated for all expenses in administering<br />
the measure.<br />
What are some of the distinctive<br />
features of the new hospital?<br />
While the plans for the new hospital are<br />
still being developed, the new hospital<br />
will be designed so that all 250 patient<br />
rooms will be private, giving children<br />
and their families more privacy to heal,<br />
and helping control and reduce infection<br />
transmission. Emergency services<br />
will also be improved—with the helipad<br />
on the roof, patients can be taken down<br />
a special elevator directly to the<br />
Emergency Department.<br />
Will the new hospital be a green<br />
building?<br />
The new hospital will incorporate<br />
current best practices in sustainable<br />
design and energy management.<br />
Children’s selected the architectural<br />
firm partly because of their expertise in<br />
delivering sustainable design solutions.<br />
Will there be any disruption to<br />
services while the new hospital<br />
is being built?<br />
Children’s will continue to operate in<br />
its current facility during construction.<br />
There shouldn’t be any disruption or<br />
displacement of services.<br />
What will become of the current<br />
hospital facility?<br />
The current hospital will continue to<br />
be used for services and offices.<br />
Children’s has many clinics and off-site<br />
programs. The hospital anticipates<br />
bringing these back on campus into<br />
the current hospital.<br />
Children’s has already begun holding<br />
community meetings to present the<br />
building project to the hospital’s neighbors,<br />
and to listen to their concerns.<br />
“We realize this building project<br />
will impact our neighbors, and it is our<br />
commitment to preserve their quality<br />
of life as much as possible,” said Mary<br />
Dean, Children’s <strong>Hospital</strong>’s senior vice<br />
president, external affairs. “To succeed,<br />
this project must be a partnership with<br />
the neighborhood, city and county.”<br />
The hospital board is “committed<br />
to respecting and partnering with our<br />
neighbors as part of the planning<br />
process,” said Frank Tiedemann,<br />
Children’s president and chief executive<br />
officer.<br />
“This is a historic time for our<br />
hospital and the community that<br />
WINTER 2007 27<br />
OUR SUPPORTERS (Left) Ron Dellums,<br />
<strong>Oakland</strong>’s mayor, praises Children’s for staying<br />
in <strong>Oakland</strong>. (Below) Jane Brunner and<br />
Ignacio De La Fuente, who have worked<br />
together on the city council for 11 years,<br />
came to the press conference to support<br />
Children’s <strong>Hospital</strong>.<br />
(Previous page) An aerial view of the hospital<br />
site: The area in orange represents the new<br />
building site.<br />
depends on our services,” said Frank.<br />
“The construction of our new medical<br />
center provides a long-awaited opportunity<br />
to match the excellence of our<br />
medical staff with a superb facility.<br />
We’re treating an increasing number of<br />
children with some of the most complex<br />
and serious illnesses. We need a<br />
new building to give them the best<br />
possible healthcare experience.”<br />
To support<br />
healthcare for kids,<br />
please vote yes on<br />
Alameda County’s<br />
Measure A.
28 CHILDREN’S HANDPRINTS<br />
A 95-year history of visionary philanthropy a<br />
By Lynn Sagramoso<br />
In 1912, Bertha Wright, an Alameda<br />
County nurse, witnessed the rapid<br />
growth of the East Bay following<br />
the San Francisco earthquake.<br />
Recognizing a need for better healthcare<br />
for the region’s new children, she and<br />
other visionary women founded The<br />
Baby <strong>Hospital</strong>. It was the first hospital<br />
on the West Coast where equipment<br />
and management would be exclusively<br />
for the care of children, no matter what<br />
their family circumstances.<br />
<strong>With</strong> the philanthropic support of<br />
the community, churches and neighbors,<br />
the women raised $12,500 to buy<br />
the old McElrath estate at the current<br />
site of the hospital. Because the need<br />
was so pressing, they began seeing<br />
patients in what was once the stable,<br />
while the main building was being renovated.<br />
The practice of medicine and the<br />
delivery of healthcare have undergone<br />
vast changes since then, but the mission<br />
at Children’s <strong>Hospital</strong> & <strong>Research</strong><br />
<strong>Center</strong> <strong>Oakland</strong> remains essentially the<br />
same: to ensure delivery of the highestquality<br />
pediatric care to all children.<br />
The mission of philanthropy at<br />
Children’s also remains the same: to<br />
support the medical center so it can<br />
continue serving all children in the<br />
region.<br />
That’s why the Children’s <strong>Hospital</strong><br />
& <strong>Research</strong> <strong>Center</strong> Foundation will<br />
play a central role in funding construction<br />
of a new hospital by 2013. (For<br />
more about the new hospital, see page<br />
24.)<br />
Children’s has grown and expanded<br />
over the years to meet the needs of the<br />
community it serves, and at every step<br />
of the way, the philanthropic leadership<br />
www.chofoundation.org<br />
ORIGINAL BUILDING—1913<br />
The McElrath mansion housed the first Children’s <strong>Hospital</strong>,<br />
and its first 30 beds, when it opened in September 1914.<br />
and generosity of the community made<br />
its growth possible.<br />
In 1928, Children’s built a new 50patient<br />
hospital of brick; much of this<br />
building still exists on our campus<br />
today.<br />
Later years saw more population<br />
growth, and Children’s responded by<br />
adding a new patient wing with more<br />
beds and a surgical facility.<br />
Meanwhile, new discoveries and<br />
therapies were revolutionizing medicine,<br />
and in 1959, private support helped<br />
build the Bruce Lyon Memorial<br />
<strong>Research</strong> Laboratory at Children’s. It<br />
began Children’s involvement in<br />
research to advance new pediatric<br />
knowledge, care and cures.<br />
Private philanthropy was also the<br />
cornerstone of many initiatives in succeeding<br />
decades.<br />
In 1994, the airy Outpatient <strong>Center</strong><br />
with its whimsically decorated atrium<br />
opened. It heralded a new, child-friendly<br />
focus to care for thousands of outpatient<br />
visits.<br />
CHILDREN’S HOSPITAL—PRES<br />
Today, Children’s <strong>Hospital</strong> has 181<br />
visits every year. Children’s philan<br />
In 1999, the research institute<br />
moved to the renovated University<br />
High School building, seven blocks<br />
north of the main campus. It’s now one<br />
of the nation’s top pediatric research<br />
centers in terms of National Institutes<br />
of Health grant funding.<br />
This expansion enables a special collaboration<br />
called translational research,<br />
which brings our scientists and treating<br />
physicians together to find new treatments<br />
and ways to prevent life-threatening<br />
pediatric illnesses.<br />
Work to expand the Emergency<br />
Department was completed in 2003,<br />
allowing Children’s to become a designated<br />
level 1 pediatric trauma center,<br />
and to offer care to over 50,000 seriously<br />
injured and ill patients every year.<br />
To serve other East Bay communities<br />
more effectively, Children’s brought<br />
its pediatric expertise to outlying areas<br />
through satellite physicians’ offices in<br />
Pleasanton, Walnut Creek, Larkspur<br />
and Brentwood. A new satellite is slated<br />
to open in Modesto in March 2008.
at Children’s<br />
RESENT DAY<br />
s 181 beds and receives more than 200,000 patient<br />
ilanthropy will be essential to rebuilding plans.<br />
Children’s is proud to be one of only 45<br />
freestanding children’s hospitals in the nation,<br />
with healthcare designed especially for kids and<br />
their families.<br />
Children’s has the largest pediatric intensive<br />
care unit in Northern California, 166 hospitalbased<br />
physicians in 31 subspecialties, and more<br />
than 200,000 patient visits a year; trains about<br />
78 pediatric residents during each three-year<br />
residency program; and has an intensive care<br />
nursery designated the regional referral center<br />
for high-risk newborns.<br />
The leadership of visionary philanthropic<br />
partners and community support created and<br />
has sustained Children’s for nearly a century.<br />
Together, we have built one of the most comprehensive<br />
pediatric medical centers in the<br />
country.<br />
Inspired by Bertha Wright’s vision 95 years<br />
ago, we will build a state-of-the-art hospital by<br />
2013 for the children of today as well as for<br />
the generations to come.<br />
To learn more about how you can support<br />
this vision, please call the Children’s <strong>Hospital</strong><br />
foundation at 510-428-3814, or visit<br />
www.chofoundation.org.<br />
Honorary Chairs<br />
Former President Bill Clinton<br />
Gov. Arnold Schwarzenegger<br />
Honorary Committee<br />
Rep. Nancy Pelosi, Speaker of the<br />
House<br />
Sen. Dianne Feinstein<br />
Sen. Barbara Boxer<br />
Gavin Newsom, mayor of San<br />
Francisco<br />
Ron Dellums, mayor of <strong>Oakland</strong><br />
Yoriko Kishimoto, mayor of Palo<br />
Alto<br />
Elizabeth Edwards<br />
Chairperson<br />
Deborah Strobin<br />
Honorary Co-Chairs<br />
David Alexander, MD<br />
Larry and Pam Baer<br />
Wilkes Bashford<br />
Dr. Ernest A. Bates<br />
Frances F. Bowes<br />
Mark and Susie Buell<br />
Harvey J. Cohen, MD, PhD<br />
Reverend and Mrs. Warren<br />
Debenham<br />
Ray and Dagmar Dolby<br />
Stanlee Gatti<br />
Larry Goldfarb<br />
Richard Goldman<br />
Rich and Judy Guggenhime<br />
WINTER 2007 29<br />
Gala to Help Raise Healthy Children<br />
Benefiting Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong><br />
Help Raise Healthy Children is a<br />
project dedicated to transforming children’s<br />
lives by advocating for healthy<br />
eating, active living and positive life<br />
choices for children. The project raises<br />
money for Children’s<br />
<strong>Hospital</strong> & <strong>Research</strong><br />
<strong>Center</strong> <strong>Oakland</strong>, and<br />
other regional medical<br />
centers, to help expand<br />
medical services to children<br />
and families with<br />
weight management<br />
issues, research childhood<br />
obesity and bring<br />
public attention to this<br />
growing problem.<br />
Help Raise Healthy Children is hosting<br />
a black-tie gala on Monday, Jan. 14, 2008<br />
in San Francisco. The star-studded event<br />
begins at San Francisco City Hall with a<br />
dinner created by Alice Waters of Chez<br />
Panisse, followed by a gala show at the War<br />
Memorial Opera House featuring worldclass<br />
entertainment, including Academy<br />
Award winner Jennifer Hudson. Ms.<br />
Hudson first gained notice as one of the<br />
finalists on the third season of the FOX television<br />
series American Idol. She went on to<br />
star in the 2006 musical film, Dreamgirls,<br />
BENEFICIARIES<br />
Children’s <strong>Hospital</strong> & <strong>Research</strong><br />
<strong>Center</strong> <strong>Oakland</strong><br />
Healthy Eating Active Living<br />
Program<br />
Lucile Packard Children’s<br />
<strong>Hospital</strong><br />
<strong>Center</strong> for Healthy Weight<br />
San Francisco General <strong>Hospital</strong><br />
Healthy Lifestyle Clinic<br />
The Chez Panisse Foundation<br />
for which she won an Oscar and a<br />
Golden Globe.<br />
Proceeds from the gala will<br />
help support Children’s Healthy<br />
Eating Active Living (HEAL) clinic.<br />
Established in July 2004, the<br />
HEAL clinic is an obesity prevention<br />
and treatment program that<br />
empowers patients and their families<br />
with culturally appropriate<br />
information and tools. HEAL<br />
support enables them to make life-saving<br />
behavior changes, reducing overweightrelated<br />
diagnoses such as type 2 diabetes<br />
and hypertension.<br />
“We are thrilled to be among the beneficiaries<br />
of this first annual gala benefit,” said<br />
Lydia Tinajero-Deck, MD, director of<br />
Children’s <strong>Hospital</strong>’s HEAL clinic. “We<br />
have an innovative program that combines<br />
obesity treatment, prevention, research and<br />
community outreach to give children the<br />
help they need to maintain a healthy weight<br />
and lifestyle.”<br />
For more information about the gala and to purchase tickets,<br />
call 415-409-4299 or visit www.helpraisehealthychildren.org.<br />
Denise Hale<br />
Michael and Kelly Halper<br />
Susan Halpern<br />
Frank and Wendy Jordan<br />
Dr. David Kessler<br />
Steve and Michele Kirsch<br />
Lois Lehrman<br />
Madeline Levine, PhD<br />
Bertram H. Lubin, MD<br />
Bill and Leigh Matthes<br />
Susan Packard Orr<br />
Sean Penn and Robin Wright<br />
Penn<br />
George and Charlotte Shultz<br />
Frank Tiedemann<br />
Ilie Wacs<br />
Dr. Charles B. Wilson and Frances<br />
Petrocelli
30 CHILDREN’S HANDPRINTS<br />
Ingrid and Dan Sanderman and their son, Tomas, are all smiles after<br />
his surgery. They’re grateful for the good karma and money provided<br />
by generous yoga students in Northern California and Nevada.<br />
Every Wednesday is “karma class”<br />
at Tanya Paul’s three Bikram Yoga<br />
studios: one in the Northern<br />
California mountain town of Truckee,<br />
and two more in Nevada. Believing in<br />
the positive karma of philanthropy, yoga<br />
instructor Ingrid Sanderman joins her<br />
students in donating to a chosen cause<br />
each week during one of her classes.<br />
Little did Ingrid or her husband, Dan,<br />
know that these philanthropic karma<br />
classes would one day help their infant<br />
son, Tomas, receive crucial surgery at<br />
Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong><br />
<strong>Oakland</strong>.<br />
“Ingrid noticed right away that something<br />
was wrong with the shape of<br />
Tomas’ head,” said Dan, “so we went to<br />
see our pediatrician in Truckee.” Their<br />
doctor suspected that Tomas had unilateral<br />
coronal craniosynostosis, a serious<br />
condition in which two or more bones<br />
comprising a baby’s skull prematurely<br />
fuse.<br />
“Our pediatrician used to be a surgeon<br />
at Children’s<br />
<strong>Hospital</strong> <strong>Oakland</strong>, and<br />
he recommended that<br />
we go there for Tomas’<br />
treatment,” said Dan.<br />
“We did some research<br />
and found that the<br />
Northern California<br />
www.chofoundation.org<br />
Are you a grateful parent?<br />
Join the Grateful Families<br />
program to help support<br />
Children’s <strong>Hospital</strong>. Call<br />
Katia Merriman at 510-428-<br />
3885, ext. 5025, or visit<br />
www.gratefulfamilies.org.<br />
Good karma<br />
builds happy faces<br />
Craniofacial <strong>Center</strong> at<br />
Children’s is one of the<br />
leading centers in the<br />
nation, and we wanted<br />
the best for our son.”<br />
So the family made<br />
the trip to <strong>Oakland</strong>,<br />
and met with Elio<br />
Gizzi, MD, the center’s<br />
medical director. He<br />
confirmed their pediatrician’s<br />
diagnosis and<br />
discussed Tomas’ condition.<br />
“Every baby’s skull is made up of<br />
bones separated by sutures, small gaps<br />
that allow for growth,” explained Dr.<br />
Gizzi. “In a child with craniosynostosis,<br />
one or more of these ‘growth lines’ fuse<br />
prematurely, forcing the skull to expand<br />
in the direction of the remaining open<br />
sutures.”<br />
This can cause a noticeably abnormal<br />
head shape. In Tomas’ case, his left<br />
eye socket had been pushed significantly<br />
lower than the right.<br />
Since a child’s brain grows rapidly—<br />
reaching 70 percent of its adult size in<br />
the first year—surgical release of the<br />
closed suture is necessary to prevent the<br />
psychosocial impacts of facial deformity<br />
and potential tissue damage caused by<br />
constriction of the brain.<br />
Children’s craniofacial center treats<br />
more than 35 cases of craniosynostosis<br />
annually. The center’s team approach to<br />
craniofacial care brings together a panel<br />
of specialists; they customize treatment<br />
plans for each child they<br />
see.<br />
“We met with each of<br />
the specialists to discuss<br />
Tomas’ needs,” Dan<br />
recalled. “There was a neurosurgeon<br />
to make sure<br />
Tomas’ cognitive abilities<br />
By Lynn Sagramoso<br />
wouldn’t suffer, a dentist and ophthalmologist<br />
to evaluate how this might<br />
affect his teeth and vision, and a plastic<br />
surgeon to make sure the outside looks<br />
great. It was scary to think of the<br />
impending surgery, but we were confident<br />
in our team, and knew what to<br />
expect.”<br />
The hardest thing for Ingrid and Dan<br />
was handing 6-month-old Tomas to the<br />
anesthesiologist on the day of the surgery.<br />
“We knew the procedure would<br />
take four hours, and we knew that the<br />
incision in his scalp would zigzag from<br />
one ear to the other so that the doctors<br />
could release the suture and reshape<br />
some of his skull,” Dan said. “We were<br />
very nervous, but the nurses were fantastic,<br />
calling periodically to keep us at<br />
ease.”<br />
Since the family lives in Truckee,<br />
about 175 miles from <strong>Oakland</strong>, it was a<br />
considerable financial burden to come to<br />
Children’s—with travel, lodging and lost<br />
work time of several days for Tomas’ preand<br />
postoperative care. When the yoga<br />
studio members heard about Tomas’<br />
treatment needs, they decided to donate<br />
a month’s worth of karma class funds<br />
from Tanya Paul’s three studios to help<br />
offset some of the family’s costs. “It<br />
meant so much to us to have the karma<br />
class donations—it helped our family<br />
emotionally and financially,” Ingrid said.<br />
About half of the karma class donations<br />
went towards Tomas’ medical<br />
expenses, but the couple wanted to pass<br />
on the class’ good will, so they donated<br />
the remainder to Children’s. “We are so<br />
grateful that Tomas’ condition has been<br />
corrected and that he won’t require further<br />
operations,” said Dan. “He’s a year<br />
old now, fully recovered, and we can<br />
hardly keep up with him—he’s captain of<br />
the world!”
Children’s<br />
most generous benefactors<br />
honored at<br />
international event<br />
Leading children’s hospital benefactors from the United States<br />
and Canada meet once a year to celebrate their support of pediatric<br />
healthcare; they are members of the Children’s Circle of Care (CCC), an<br />
international honor society founded in 1995.<br />
On May 3, Children’s <strong>Hospital</strong> Boston hosted 2006 CCC members, honoring<br />
them with a series of exclusive events. Many Children’s <strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong><br />
<strong>Oakland</strong> donors and members from hospital senior leadership were there.<br />
The 2007 North American Leadership Conference & Gala Dinner included presentations<br />
by renowned physicians from pediatric hospitals nationwide at Boston’s<br />
beautiful restored Opera House. The festivities also included a live performance by<br />
the Boston Pops, led by conductor Keith Lockhart, and a black-tie gala featuring a<br />
private concert by Sir Elton John.<br />
Children’s <strong>Hospital</strong> Denver will host this prestigious annual event—in June 2008<br />
—for those who are members in 2007.<br />
If you are interested in becoming a CCC member or would like more information<br />
about membership, please call Carolyn Otis Catanzaro at 510-428-3885, ext. 7306,<br />
or email her at ccatanzaro@mail.cho.org.<br />
Help ring in the New Year at Children’s!<br />
In the true spirit of the season, all of us at Children’s<br />
<strong>Hospital</strong> & <strong>Research</strong> <strong>Center</strong> <strong>Oakland</strong> give thanks to<br />
those who have given so generously of their time and<br />
money to support our crucial mission. We couldn’t do it<br />
without you!<br />
Remember, charitable donations to Children’s, postmarked<br />
no later than Dec. 31, 2007, may give you a considerable<br />
benefit at tax time by saving you money on<br />
your income taxes. The IRS encourages those giving to<br />
nonprofit organizations, like Children’s, by offering significant<br />
tax advantages to donors.<br />
More importantly, your gift will help Children’s provide<br />
a standard of healthcare that exceeds the expectations<br />
of every family within our diverse and vibrant community.<br />
Your investment in pediatric health also allows<br />
our research scientists and clinical physicians to advance<br />
breakthrough treatments of cancer, blood diseases and<br />
WINTER 2007 31<br />
Children’s Circle of Care is<br />
grateful to the following<br />
sponsors for their support of<br />
the 2007 North American<br />
Leadership Conference:<br />
Founding Sponsors<br />
Costco Wholesale<br />
The Oki Foundation<br />
Signature Sponsors<br />
Cushman & Wakefield of<br />
Massachusetts, Inc.<br />
Fidelity Investments<br />
Harrah’s Entertainment, Inc.<br />
Tudor Investment Corporation<br />
Silver Sponsors<br />
AJ Gallagher<br />
Bank of America<br />
Bentz Whaley Flessner<br />
The H. N. and Frances C. Berger<br />
Foundation<br />
Goldman Sachs<br />
Kintera Inc.<br />
Opus Search Partners<br />
Nixon Peabody<br />
Tsoi/Kobus & Associates<br />
The Westin Boston Waterfront<br />
other life-threatening<br />
illnesses, benefiting<br />
countless children<br />
worldwide.<br />
For more information<br />
about donating to<br />
Children’s, please<br />
call Ken McKinney at<br />
510-428-3885, ext. 2846,<br />
or email him at<br />
Let our patients know you care; send<br />
kmckinney@mail.cho.org. this card with your donation today!<br />
You may also give online at<br />
www.chofoundation.org/donate.<br />
Your gift truly makes a difference. And if you give<br />
before Dec. 31, we will present a special Get Well Soon<br />
holiday card (pictured) in your name, to a hospitalized<br />
child during this holiday season.
Pediatric neurosurgeon Peter Sun, MD,<br />
and the portable CereTom CT scanner.<br />
Only at Children’s <strong>Hospital</strong> <strong>Oakland</strong>.<br />
747 52nd Street<br />
<strong>Oakland</strong>, CA 94609-1809<br />
SM<br />
Undivided attention. Unsurpassed care.<br />
In October, Children’s<br />
<strong>Hospital</strong> <strong>Oakland</strong> became<br />
the first and only pediatric<br />
medical center on the West<br />
Coast to own and use a<br />
portable CT scanner.<br />
Now, when the need is<br />
critical, Dr. Sun can bring<br />
the scanner to the child,<br />
minimizing risk and<br />
saving time.<br />
Read more about<br />
Children’s cutting-edge<br />
technology on page 7.<br />
Non-Profit Org.<br />
U.S. Postage<br />
PAID<br />
<strong>Oakland</strong>, CA<br />
Permit No. 3