HURC Policy & Procedure Manual - Extranet - University of Rochester
HURC Policy & Procedure Manual - Extranet - University of Rochester
HURC Policy & Procedure Manual - Extranet - University of Rochester
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
To: All Principal Investigators<br />
<strong>University</strong> <strong>of</strong> <strong>Rochester</strong><br />
Human Use <strong>of</strong> Radiation Committee<br />
From: Human Use <strong>of</strong> Radiation Committee<br />
Subject: Application for the Use <strong>of</strong> Radioisotopes or Radiation-Generating Devices in<br />
Research involving Human Subjects<br />
The attached information has been prepared to assist you with completing an application to use<br />
ionizing radiation for human biomedical research. The committee is required to review certain<br />
activities and information prior to granting approval on an application. Please ensure that each<br />
application is supported by complete and accurate information so that the Committee can act on<br />
the application.<br />
Please submit a copy <strong>of</strong> CVs for all researchers participating in the proposed work. If CVs have<br />
been submitted previously, there is no need to submit a new CV.<br />
If assistance is needed to complete the application, please contact Radiation Safety, 275-3781.<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
1
Table <strong>of</strong> Contents<br />
A. Background………………………………………………………………………………………………..3<br />
B. General considerations for Application Submittal………………………………………………………..4<br />
C. Required involvement <strong>of</strong> an “authorized user”……………………………………………………….…..4<br />
D. Assessment <strong>of</strong> radiation risk……………………………………………………………………………...5<br />
E. Limitations on radiation dose…………………………………………………………………………….5<br />
F. Informed consent statements <strong>of</strong> radiation risk………………………………………………………….. 6<br />
G. Restrictions on human subject recruitment………………………………………………………………7<br />
H. Notification <strong>of</strong> auxiliary personnel………………………………………………………………………7<br />
I. Misadministrations and adverse reactions……………………………………………………………….7<br />
J. Modifications……………………………………………………………………….…………………...8<br />
K. Renewal/termination…………………………………………………………………………………….8<br />
L. Location for submission………………………………………………………………………………....8<br />
M. Meeting dates and deadlines………………………………………………………………………….…8<br />
N. Submission requirements………………………………………………………………………………..8<br />
O. Instructions for Completing <strong>HURC</strong> Form “Information Required in Support <strong>of</strong> the……………….…. .9<br />
Research Use <strong>of</strong> a Non-FDA Approved Radioactive Drug”<br />
P. Special Conditions for the Research Use <strong>of</strong> a Radioactive Drug That Is Not…………………………..13<br />
F.D.A. Approved (21 CFR Part 361.1)<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
2
A. Background<br />
THE HUMAN USE OF RADIATION COMMITTEE<br />
Exposure <strong>of</strong> human subjects to ionizing radiation in the course <strong>of</strong> a biomedical research<br />
study involves several considerations in addition to those applied to clinical research studies<br />
which do not incorporate such an intervention. The risks <strong>of</strong> involved radiation exposure<br />
must be appropriately addressed and delineated in a consent form. Also, the research study<br />
must be conducted in accordance with institutional policies and procedures and with state<br />
and/or federal regulations that govern the safe use and handling <strong>of</strong> radioactivity and<br />
radiation-generating devices. To ensure that these special considerations are properly<br />
addressed, biomedical research studies involving the exposure <strong>of</strong> human subjects to ionizing<br />
radiation must be reviewed and approved by the Human Use <strong>of</strong> Radiation (<strong>HURC</strong>).<br />
Approval <strong>of</strong> the <strong>HURC</strong> for such studies is in addition to the requirement for approval<br />
by the Research Subjects Review Board (RSRB).<br />
The <strong>HURC</strong> reviews, comments on and approves the following types <strong>of</strong> research studies:<br />
1. Tracer studies: Use <strong>of</strong> radioactive drugs or tracer compounds to obtain basic<br />
information about the metabolism <strong>of</strong> a radioactively labeled drug or regarding human<br />
physiology, pathophysiology or biochemistry, but not intended for immediate<br />
therapeutic or diagnostic purposes. The amount <strong>of</strong> drug or compound administered<br />
must not evoke a clinical response.<br />
2. Investigational new drug (IND) studies: Use <strong>of</strong> drugs at or above levels expected<br />
to evoke a clinical response. A formal FDA-approved IND application must<br />
accompany the <strong>HURC</strong> application.<br />
3. Research use <strong>of</strong> a non-FDA approved device (“non-significant risk”): Food and<br />
Drug administration policies permit the research use, in human subjects, <strong>of</strong> an<br />
ionizing radiation-emitting device that is not the subject <strong>of</strong> an approved<br />
Investigational Device Exemption (IDE) or 510K application provided that it is<br />
classified as a “non-significant risk device” based on review by the RSRB. To be<br />
considered a presenting a “non-significant risk,” use <strong>of</strong> the ionizing radiationemitting<br />
device must not be <strong>of</strong> substantial importance in diagnosing, curing,<br />
mitigating, or treating disease, or otherwise preventing impairment <strong>of</strong> human health.<br />
4. Research use <strong>of</strong> a non-FDA approved device: Failure to meet the criteria for “nonsignificant<br />
risk” requires that the sponsor <strong>of</strong> the device obtain FDA approval <strong>of</strong> an<br />
Investigational Device Exemption (IDE).<br />
5. Research use <strong>of</strong> a FDA-approved device: Use <strong>of</strong> a radiation-generating device for<br />
non-clinical research.<br />
6. “On label” research use <strong>of</strong> a FDA-approved radiopharmaceutical: Research<br />
using a radiopharmaceutical prepared and administered in accordance with the<br />
approved product labeling.<br />
7. “Off label” research use <strong>of</strong> a FDA-approved radiopharmaceutical: Research<br />
using a FDA-approved radiopharmaceutical prepared using a non-approved (i.e., not<br />
according to product labeling) method and/or administered by a non-approved (i.e.,<br />
not according to product labeling) route.<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
3
B. General Considerations for Application Submittal<br />
In planning a research study, investigators should first consider whether it is necessary to use<br />
ionizing radiation to obtain the desired information. Any investigation requiring the use <strong>of</strong><br />
ionizing radiation must produce the needed information at minimum radiation dose to the<br />
minimum number <strong>of</strong> human subjects and the research must be defensible in terms <strong>of</strong> clinical<br />
and scientific relevance.<br />
The application must clearly state:<br />
Hypothesis(es) to be tested and the specific aims <strong>of</strong> the research<br />
Why the use <strong>of</strong> radioactivity or a radiation-generating device is necessary to address<br />
the specific aims<br />
Scientific and statistical justification (where appropriate) for the number <strong>of</strong> subjects<br />
Justification for the estimated radiation dose<br />
C. Required involvement <strong>of</strong> an “authorized user”<br />
The use <strong>of</strong> radioactivity and radiation-generating devices in humans is strictly controlled by<br />
State and Federal regulations. Only a pr<strong>of</strong>essional practitioner (physician, dentist, podiatrist,<br />
osteopath or chiropractor) or certified nurse practitioner or physician assistant working<br />
within a practice agreement with a physician may order the use <strong>of</strong> x-rays.<br />
Radiopharmaceuticals may only be ordered by a physician who is approved by the <strong>University</strong><br />
<strong>of</strong> <strong>Rochester</strong> Radiation Safety Committee.<br />
An “authorized user” is an individual possessing the appropriate qualifications for the<br />
proposed human use <strong>of</strong> the radiation-emitting device or drug. Listed below are requirements:<br />
Tracer studies: individual approved by the Radiation Safety Committee who is<br />
qualified by training and experience to conduct the proposed research studies.<br />
Radioactive drugs administered under an IND or “on label” or “<strong>of</strong>f label”<br />
research use: physician authorized by the Radiation Safety Committee to prescribe<br />
radioactive materials<br />
Use <strong>of</strong> radiation-generating device: pr<strong>of</strong>essional practitioner (physician, dentist,<br />
podiatrist, osteopath or chiropractor) or certified nurse practitioner or physician<br />
assistant working within a practice agreement with a physician. NOTE: only a<br />
pr<strong>of</strong>essional practitioner or a licensed radiologic technologist or a properly<br />
supervised student technologist may position subjects, set techniques or apply<br />
radiation.<br />
The authorized user is responsible for<br />
Compliance with all statements and conditions approved by the <strong>HURC</strong><br />
Ensuring that each study is approved in writing by the appropriate individual, as<br />
described above, before administration<br />
Submission <strong>of</strong> routine reports (e.g., Research Study Progress Report, Modification<br />
Requests) and special (e.g., adverse event, misadministration) reports required by the<br />
<strong>HURC</strong><br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
4
D. Assessment <strong>of</strong> radiation risks<br />
A major responsibility <strong>of</strong> the <strong>HURC</strong> is the review <strong>of</strong> the radiation risks to human subjects<br />
participating in the proposed research project. The <strong>HURC</strong> pays special attention to the<br />
radiation risks associated with a single study (i.e., inclusive <strong>of</strong> all procedures performed on<br />
the subject during a single study session) and the cumulative risks (i.e., inclusive <strong>of</strong> all single<br />
studies performed on the subject) associated with total project participation. The <strong>HURC</strong> also<br />
reviews the methods or sources <strong>of</strong> information that were used to approximate these risks.<br />
Estimates <strong>of</strong> radiation exposure to human subjects must be made in advance and included as<br />
part <strong>of</strong> the research protocol submitted to the <strong>HURC</strong>. For radioactive materials, the dose to<br />
the whole body as well as specific organs known to be targeted by the drug/compound must<br />
be provided. Estimated doses to gonads, lens <strong>of</strong> the eye and red marrow must be provided as<br />
well, even though the drug or compound may not specifically target these organs. For<br />
studies involving radiation-generating devices, the skin entrance exposure or dose must also<br />
be provided. It is appropriate to assume 1 Roentgen = 1 rad = 1 rem for x-rays, gamma rays<br />
and beta particles. (Assistance is available from the Radiation Safety Unit, 275-3781.)<br />
The following radiation units must be included as appropriate:<br />
Whole body dose (effective dose equivalent) – mrem/rem<br />
Organ dose – mrad/rad<br />
Entrance skin dose – mrad/rad<br />
E. Limits on radiation dose<br />
The amount <strong>of</strong> the radioactive drug administered or exposure to radiation-generating devices<br />
shall be such that the subject receives the smallest radiation dose with which it is practical to<br />
perform the study without jeopardizing the benefits to be obtained from the study.<br />
Under no circumstances may the radiation dose to an adult research subject from a single<br />
study exceed 3 rem effective dose equivalent to the whole body, 3 rem to active bloodforming<br />
organs, lens <strong>of</strong> the eye or gonads; or 5 rem in a single study to any other organ. (A<br />
“single study” is defined as all procedures performed on a subject during a single study<br />
session). The total dose commitment from multiple studies (by all investigators) performed<br />
on the same subject within 1 year may not exceed 5 rem effective dose equivalent to the<br />
whole body, 5 rem to active blood-forming organs, lens <strong>of</strong> the eye, or gonads; or 15 rem to<br />
any other organ.<br />
• Radiation doses from x-ray or other procedures that are part <strong>of</strong> the research study<br />
(i.e., would not have occurred but for the research study) shall be included when<br />
determining the single study radiation absorbed doses and total dose commitments.<br />
• For research subject under 18 years <strong>of</strong> age at his/her last birthday, the radiation dose<br />
shall not exceed 10% <strong>of</strong> the limits described above.<br />
• Numerical definitions <strong>of</strong> the radiation dose shall be based on an absorbed fraction<br />
method <strong>of</strong> calculation such as the system set forth by the Medical Internal Radiation<br />
Dose Committee (MIRD) <strong>of</strong> the Society <strong>of</strong> Nuclear Medicine or the International<br />
Commission on Radiological Protection (ICRP).<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
5
F. Informed Consent statements <strong>of</strong> radiation risk<br />
The discussion <strong>of</strong> radiation risks in the informed consent document and patient dialogue<br />
should include comparisons with natural background (i.e., for low risk procedures) or<br />
occupational worker limits. Examples <strong>of</strong> statements that are reasonable include the<br />
following:<br />
(1) For whole body Effective Dose Equivalent (EDE) < 1000 mrem:<br />
“Participation in this research study involves exposure to radiation from (specify<br />
respective procedure(s) to be performed). The amount <strong>of</strong> radiation exposure that you<br />
will receive from this (these) procedure(s) is equivalent to a uniform whole body dose<br />
<strong>of</strong> mrem which is approximately (indicate multiplication factor, fraction,<br />
or percentage <strong>of</strong>) the average amount <strong>of</strong> natural environmental radiation exposure (360<br />
mrem dose) that each member <strong>of</strong> the general public receives per year. There is no<br />
known minimum level <strong>of</strong> radiation exposure that is recognized as being totally free <strong>of</strong><br />
the risk <strong>of</strong> causing genetic defects (cellular abnormalities) or cancer. However, the risk<br />
associated with the amount <strong>of</strong> radiation exposure that you will receive from this study is<br />
considered to be low when compared to other everyday risks.<br />
(2) For a whole body Effective Dose Equivalent (EDE) <strong>of</strong> 1000 mrem - 5000 mrem:<br />
“Participation in this research study involves exposure to radiation from (specify<br />
respective procedure(s) to be performed). The amount <strong>of</strong> radiation exposure that you<br />
will receive from this (these) procedure(s) is equivalent to a uniform whole body dose<br />
<strong>of</strong> rem which is approximately (indicate fraction or percentage <strong>of</strong>) the<br />
annual radiation exposure (5 rem) permitted to radiation workers by federal regulations.<br />
These is no known minimum level <strong>of</strong> radiation exposure that is recognized as being<br />
totally free <strong>of</strong> the risk <strong>of</strong> causing genetic defects (cellular abnormalities) or cancer.<br />
However, the risk associated with the amount <strong>of</strong> radiation exposure that you will<br />
receive from this study is considered to be low and comparable to other everyday risks.<br />
(3) For a whole body Effective Dose Equivalent (EDE) <strong>of</strong> > 5000 mrem.<br />
“Participation in this research study involves exposure to radiation from (specify<br />
respective procedure(s) to be performed). The amount <strong>of</strong> radiation exposure that you<br />
will receive from this (these) procedure(s) is equivalent to a uniform whole body dose<br />
<strong>of</strong> rem which is approximately (indicate multiplication factor) the annual<br />
radiation exposure (5 rem) permitted to radiation workers by federal regulations.<br />
Excess cancer risk associated with this level <strong>of</strong> radiation exposure is estimated to be<br />
(specify BEIR III, BEIR V, or ICRP 64 factor*) the standard risk.”<br />
*Contact the <strong>University</strong> Radiation Safety Unit 275-3781 for assistance in<br />
obtaining this data.<br />
(4) Note: Comparisons <strong>of</strong> radiation exposures or risks from radioactive drugs to those from<br />
X-ray procedures shall not be approved unless the risks are stated in comparable units<br />
(i.e., Effective Dose Equivalent).<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
6
G. Restrictions on human subject recruitment<br />
Definitions:<br />
• “Subjects” are defined as participants in research activities other than patients; these<br />
people include controls.<br />
• “Patients” are defined as participants in research activities for whom there is a<br />
pr<strong>of</strong>essional responsibility for diagnosis or treatment.<br />
• “Minors” are defined as subjects or patients < 18 years <strong>of</strong> age.<br />
If a research study involving exposure to ionizing radiation involves female subjects or<br />
patients, pregnancy must be ruled out on the basis <strong>of</strong> the research subject’s clinical history or<br />
by a highly sensitive test performed within a short time frame prior to exposure.<br />
Nursing females should not be included in any research study involving the administration <strong>of</strong><br />
a radioactive drug.<br />
H. Notification <strong>of</strong> auxiliary personnel<br />
All auxiliary personnel involved directly (e.g., radiologic or nuclear medicine technologists)<br />
or indirectly (e.g., nursing staff, laboratory technologists) in the conduct <strong>of</strong> the research<br />
study, in the care <strong>of</strong> human subjects or patients participating in the research, or in the<br />
handling <strong>of</strong> respective radioactive samples must be adequately informed <strong>of</strong> the nature <strong>of</strong> the<br />
research study and any radiation risks (including methods to reduce such risks) that may be<br />
associated with their involvement. Radiation safety training may be required for those<br />
personnel. Please contact Radiation Safety for information on Radiation Safety Training at<br />
275-3781.<br />
I. Misadministration and adverse reactions<br />
Any unintentional exposure to radiation (i.e., misadministration) or adverse reaction to a<br />
radioactive drug or radiation exposure occurring during the research study must be reported<br />
immediately to the Radiation Safety Officer at 275-3781.<br />
A misadministration is defined as administration <strong>of</strong><br />
A radioactive drug or radiation from a source other than the one ordered;<br />
A radioactive drug or radiation to the wrong person;<br />
A radioactive drug or radiation by a route or to a part <strong>of</strong> the body other than that<br />
intended by the authorized user;<br />
An activity <strong>of</strong> a radioactive drug for diagnostic purposes that differs from the activity<br />
ordered by more than 50%;<br />
An activity <strong>of</strong> a radioactive drug for therapeutic purposes that differs from the<br />
activity ordered by more than 10%;<br />
Therapeutic radiation dose from any source other than a radioactive drug differing<br />
from the final ordered dose by more than 10%;<br />
Therapeutic radiation dose in any fraction <strong>of</strong> a fractionated treatment such that the<br />
administered dose in the individual treatment or fraction differs from the dose ordered<br />
by more than 50%.<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
7
The Chair <strong>of</strong> the <strong>HURC</strong>/RDRC shall investigate and report the circumstances <strong>of</strong> the event to<br />
appropriate individuals, committees, and outside agencies as required:<br />
Medical Quality Assurance Committee<br />
Risk Management Committee<br />
Diagnostic Medical Imaging Quality Assurance Committee<br />
Research Subjects Review Committee<br />
Radiation Safety Committee<br />
New York State Department <strong>of</strong> Health<br />
U.S. Food and Drug Administration<br />
J. Submission requirements<br />
Submit eight (8) copies the following documents<br />
Application For The Research Use Of Ionizing Radiation (Appendix A); and<br />
Research protocol and informed consent document (RSRB format). This must include a<br />
statement <strong>of</strong> how the authorized user will ensure that approval is obtained in writing<br />
before administration <strong>of</strong> x-rays or radioactive drugs or compounds; and<br />
Curriculum vitae (C.V.) <strong>of</strong> the principal investigator and authorized user; and<br />
For research involving evaluation <strong>of</strong> a non-FDA-approved radiation generating device:<br />
device manufacturer’s clinical protocol and/or investigator’s brochure or the investigatorsponsored<br />
IDE application, if appropriate; or<br />
For research involving “<strong>of</strong>f label” use <strong>of</strong> a FDA-approved radiopharmaceutical:<br />
completed “Information Required in Support <strong>of</strong> the Research Use on a Non-Approved<br />
Radioactive Drug” (Appendix B); or<br />
For research involving use <strong>of</strong> a non-FDA approved radioactive drug or compound:<br />
“Information Required in Support <strong>of</strong> the Research Use <strong>of</strong> a Non-Approved Radioactive<br />
Drug” (Appendix B) and notification that the proposed research study has been approved<br />
by a scientific review committee representing the principal investigator’s primary<br />
academic or center affiliation; or<br />
For research evaluation <strong>of</strong> a radioactive drug which is the subject <strong>of</strong> a FDA-approved<br />
Investigational New Drug (IND) exemption: manufacturer’s clinical protocol and/or<br />
investigator’s brochure or the investigator-sponsored IND application.<br />
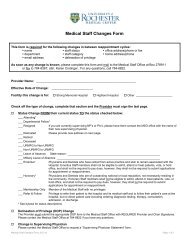
K. Modifications<br />
<strong>HURC</strong> must be notified <strong>of</strong> any changes in the research protocol that affect<br />
• Number <strong>of</strong> subjects<br />
• Age distribution if more minors will be included<br />
• Dose to subjects either from individual studies or from the total protocol<br />
The principal investigator will be required to submit additional documents supporting these<br />
changes and may be required to re-submit the initial forms described above.<br />
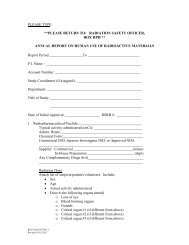
L. Renewal/Termination<br />
The <strong>HURC</strong> will monitor the status <strong>of</strong> approved research projects by requiring that the<br />
principal investigator and/or authorized user complete, on a periodic basis, a Research Study<br />
Progress Report.<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
8
M. Location for submissions<br />
Materials submitted for review and approval by the <strong>HURC</strong> should be delivered to Radiation<br />
Safety Unit, Box HPH, 275-3781.<br />
N. Meeting dates and deadlines<br />
The <strong>HURC</strong> is required by regulation to meet as a full committee to review research studies<br />
involving radioactive drugs. The <strong>HURC</strong> meets in each calendar quarter, (February, May,<br />
August and November). Other times can be arranged.<br />
The review <strong>of</strong> research studies involving (ionizing) radiation-emitting devices can be<br />
expedited by limited review process. Such research studies will be reviewed as received.<br />
O. Instructions for Completing <strong>HURC</strong> Form “Information Required in Support <strong>of</strong> the Research<br />
Use <strong>of</strong> a Non-FDA Approved Radioactive Drug”<br />
1. General Instructions<br />
a. Responses to the requests for information should be type written (i.e., handwritten<br />
responses will not be accepted.<br />
b. Use <strong>of</strong> supplementary pages or appendices is permitted if additional space is required.<br />
c. One completed <strong>HURC</strong> Form for given radioactive drug may serve as a “Master File”<br />
for multiple research projects involving the administration <strong>of</strong> that radioactive drug.<br />
Each new submission <strong>of</strong> a research protocol should specifically cite the current<br />
Master File for the applicable radioactive drug.<br />
2. Specific Instructions<br />
a. Identity <strong>of</strong> the Radioactive Drug<br />
• Identify the [radionuclide]-active ingredient/carrier (e.g., [C-14] glucose)<br />
• Identify the non-radioactive drug (e.g., glucose)<br />
b. Specify the maximum mass dose (i.e., ug or mg) <strong>of</strong> non-radioactive drug to be<br />
administered per subject, per single dose.<br />
c. Identify the non-radioactive ingredients that appear within the final dosage form (e.g.,<br />
10% V/V ethanol in 0.9% Sodium Chloride for Injection, U.S.P.)<br />
d. Identify radionuclide contaminants (e.g., Mo-99 when Tc-99m is administered).<br />
State the percent (%) <strong>of</strong> administered activity attributable to contaminants.<br />
3. Route <strong>of</strong> Administration<br />
a. Indicate the number <strong>of</strong> doses per subject and proposed route <strong>of</strong> administration.<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
9
3. Estimated Radiation Dose to Human Subjects<br />
a. Absorbed calculations:<br />
• Provide radiation absorbed dose estimates for the radioactive drug. At a<br />
minimum, radiation dose estimates must address the effective dose equivalent and<br />
absorbed doses to the total body, gonads, active blood-forming organs, critical<br />
organ, and lens <strong>of</strong> the eye. (The latter may be assumed to be equivalent to the<br />
total body dose unless specific eye uptake <strong>of</strong> the radioactive drug has been<br />
demonstrated or is expected.). Submit a complete list, to include absorbed doses<br />
to other organs, when respective data is available. These dose estimates must<br />
take into account the contribution <strong>of</strong> any significant radionuclide contaminant(s)<br />
present in the final project.<br />
• Specify the literature reference from which the biodistribution data for calculation<br />
<strong>of</strong> the radiation absorbed dose estimates were obtained; or, if not published,<br />
provide a summary <strong>of</strong> the biodistribution data and identify the laboratory and<br />
personnel involved in its collection.<br />
• Specify the individual or entity responsible for calculation <strong>of</strong> the radiation<br />
absorbed estimated and the methodology (e.g., MIRD or ICRP absorbed fraction)<br />
utilized; or, if taken from a published source, include a copy <strong>of</strong> the respective<br />
reference.<br />
b. Method <strong>of</strong> radioassay:<br />
• Specify the method by which the radioactive drug will be assayed prior to use so<br />
as to ensure that the administered radioactivity dosage and corresponding<br />
absorbed dose estimated are as stated in the research protocol.<br />
c. Assay instrumentation quality control:<br />
• Indicate the procedures that will be performed to ensure accurate operation <strong>of</strong> the<br />
instrumentation used to assay the radioactive drug.<br />
4. Pharmacological Dosage <strong>of</strong> Active Ingredient<br />
a. For an FDA-approved (i.e., NDA) radiopharmaceutical prepared using a nonapproved<br />
method and/or administered by a non-approved route: Provide supporting<br />
statements to address the requirement that deviation(s) from the approved product<br />
labeling will not significantly increase the risk to the research subject.<br />
b. For a radioactive drug prepared and administered under the authority <strong>of</strong> 21 CFR<br />
361.1; provide data, based on the published or other valid human studies,<br />
(1) In support <strong>of</strong> the requirement that the amount <strong>of</strong> active ingredient/carrier in the<br />
proposed dosage <strong>of</strong> the final radioactive drug will not cause any clinically<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
10
detectable pharmacological effects. (Append copies <strong>of</strong> key referenced<br />
publications or cited human studies.)<br />
(2) Maximum mass dose level at which no clinically detectable pharmacological<br />
effects are known to occur.<br />
5. Quality <strong>of</strong> the Radioactive Drug<br />
a. Method <strong>of</strong> preparation/dispensing:<br />
• Identify the individual(s) or entity that will be responsible for the preparation,<br />
repackaging, and/or dispensing <strong>of</strong> the radioactive drug.<br />
• Describe, in detail, the procedures that will be used in the preparation,<br />
repackaging, and/or dispensing <strong>of</strong> the radioactive drug. (May be appended in the<br />
form <strong>of</strong> a master formula card.)<br />
b. Minimum acceptance criteria:<br />
• Delineate minimum acceptance specifications for the final radioactive drug,<br />
addressing which <strong>of</strong> the criteria listed below:<br />
c. Preclinical validation studies:<br />
Visual appearance<br />
pH<br />
Radiochemical purity<br />
Chemical purity<br />
Specific activity<br />
Radionuclide purity or identification:<br />
Pyrogens or bacterial endotoxins (limited to parenteral<br />
administration)<br />
Sterility (limited to parenteral administration)<br />
• Summarize the outcome <strong>of</strong> any preclinical validation studies that have been<br />
performed to confirm that the final radioactive drug will meet the designated<br />
minimum acceptance criteria when prepared/repackaged according to the<br />
indicated procedures. Such validation studies may include procedures performed<br />
on site and/or obtained from the supplier <strong>of</strong> the radioactive drug.<br />
d. Routine quality control procedures:<br />
• Indicate the testing procedures that will be performed on each batch <strong>of</strong> the<br />
radioactive drug to ensure that it meets the designated minimum acceptance<br />
criteria.<br />
(Note that because <strong>of</strong> test complexity it may not be possible or practicable to<br />
address each <strong>of</strong> the designated minimum acceptance criteria on each batch <strong>of</strong> the<br />
radioactive drug. In such an event, compliance <strong>of</strong> the radioactive drug with the<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
11
applicable minimum acceptance criterion should be addressed in the preclinical<br />
validation studies. For certain criteria (e.g., sterility, pyrogens/ bacterial<br />
endotoxins), it may be a requirement (i.e., based on the physical half-life <strong>of</strong> the<br />
radionuclide) that testing be completed following release <strong>of</strong> the radioactive drug<br />
for human use.)<br />
• Indicate the individual(s) or entity that will be responsible for routine quality<br />
control testing <strong>of</strong> the radioactive drug.<br />
e. Expiration dating:<br />
6. Labeling<br />
• Specify an expiration period, post preparation or repackaging <strong>of</strong> the radioactive<br />
drug, wherein there is evidence that each <strong>of</strong> the designated minimum acceptance<br />
criteria will be retained. Summarize the studies that have been performed or<br />
provide a literature reference justifying this expiration period.<br />
a. For an FDA-approved (i.e., NDA) radiopharmaceutical prepared using a nonapproved<br />
method and/or administered by a non-approved route: Specify how the<br />
immediate container (e.g., vial syringe) shielding <strong>of</strong> the radiopharmaceutical will be<br />
labeled so as to address the identity <strong>of</strong> the responsible research area or investigator,<br />
the identity <strong>of</strong> the radiopharmaceutical, the total quantity <strong>of</strong> contained radioactivity at<br />
a designated assay time/date, the total contained volume or mass, the expiration<br />
time/date, and (if applicable) a lot or control number that will permit reference to the<br />
procedure/reagents involved in the non-approved method <strong>of</strong> preparation.<br />
• Note that if the radiopharmaceutical is to be distributed outside <strong>of</strong> the responsible<br />
research area, the information listed above must appear on the primary label<br />
attached to the immediate container or shielding. If the radiopharmaceutical is<br />
not distributed outside <strong>of</strong> the responsible research area, the information included<br />
on the primary label may be limited to the identity <strong>of</strong> the radiopharmaceutical and<br />
an identifier (e.g., lot number or batch number) that permits immediate access to<br />
the other information specified above.<br />
• Note that if the primary label is attached to the shielding, the immediate container<br />
<strong>of</strong> the radioactive drug must be labeled to include, at a minimum, the identity <strong>of</strong><br />
the radiopharmaceutical.<br />
b. For a radioactive drug used under the authority <strong>of</strong> 21 CFR 361.1: Specify how the<br />
immediate container (e.g., vial, syringe) or shielding f the radioactive drug will be<br />
labeled so as to comply with the requirements <strong>of</strong> 21 CFR 361.1 (available from the<br />
Radiation Safety Unit).<br />
• Note that if the radioactive drug is to be distributed outside <strong>of</strong> the responsible<br />
research area, each <strong>of</strong> the applicable information/statements listed in 21 CFR<br />
361.1 must appear on the primary label attached to the immediate container or<br />
shielding. If the radioactive drug is not distributed outside <strong>of</strong> the responsible<br />
research area, the information statements included on the primary label may be<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
12
limited to: 1) the statements, “Caution: Federal law prohibits dispensing without<br />
a prescription,” and “To be administered in compliance with the requirements <strong>of</strong><br />
Federal regulations regarding radioactive drugs for research use (21 CFR 361.1)”;<br />
2) the identity <strong>of</strong> the radioactive drug; and 3) an identifier (e.g., lot number, batch<br />
number) that permits immediate access to the other information listed in 21 CFR<br />
361.1.<br />
• Note that if the primary label is attached to the shielding, the immediate container<br />
<strong>of</strong> the radioactive drug must be labeled to include, at a minimum, the identity <strong>of</strong><br />
the radioactive drug and an identifier (e.g., lot number or batch number) that will<br />
permit correlation with the primary label.<br />
P. Special Conditions for the Research Use <strong>of</strong> a Radioactive Drug That Is Not F.D.A. Approved<br />
(21 CFR Part 361.1)<br />
1. Definition <strong>of</strong> “research use”<br />
Radioactive drugs or compounds are generally recognized as safe and effective when<br />
administered to human research subjects during the course <strong>of</strong> a research project intended to obtain<br />
basic information regarding the kinetics (including distribution and localization) and metabolism<br />
<strong>of</strong> the radioactive drug or regarding human physiology, pathophysiology, or biochemistry; but<br />
not when intended for immediate diagnostic, therapeutic, or similar purposes or to<br />
determine the safety and effectiveness <strong>of</strong> the drug in humans for such purpose (i.e., to carry<br />
out a clinical trial).<br />
2. Human research subjects:<br />
Research subjects shall be at least 18 years <strong>of</strong> age and legally competent. Exceptions are<br />
permitted only in those special situations when it can be demonstrated that the study presents a<br />
unique opportunity to gain information not currently available, and that the study requires the use<br />
<strong>of</strong> research subjects less than 18 years <strong>of</strong> age.<br />
The number <strong>of</strong> subjects included in the research study shall be sufficient but no greater than<br />
necessary to achieve the objective(s) <strong>of</strong> the study (i.e., to obtain basic research information).<br />
Inclusion <strong>of</strong> more than 30 subjects or subjects less than 18 years <strong>of</strong> age in the research study<br />
requires advanced notification <strong>of</strong> the F.D.A. and must be scientifically rationalized.<br />
3. Limit on radiation dose<br />
The amount <strong>of</strong> the radioactive drug administered shall be such that the subject receives the<br />
smallest radiation dose with which it is practical to perform the study without jeopardizing the<br />
benefits to be obtained from the study.<br />
Under no circumstances may the radiation dose to an adult research subject from a single study<br />
exceed 3 rems to the whole body, active blood-forming organs, lens <strong>of</strong> the eye, or gonads; or 5<br />
rems in a single study to any other organ. (A “single study” is defined as all procedures<br />
performed on a subject during a single study session). The total dose commitment from multiple<br />
studies (by all investigators) performed on the same subject within 1 year may not exceed 5 rems<br />
to the whole body, active blood-forming organs, lens <strong>of</strong> the eye, or gonads; or 15 rems to any<br />
other organ.<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
13
• Radiation doses from x-ray or other procedures that are part <strong>of</strong> the research study (i.e., would<br />
not have occurred but for the research study) shall be included when determining the single<br />
study radiation absorbed doses and total dose commitments.<br />
• For research subject under 18 years <strong>of</strong> age at his/her last birthday, the radiation dose shall not<br />
exceed 10% <strong>of</strong> the limits described above.<br />
• Numerical definitions <strong>of</strong> the radiation dose shall be based on an absorbed fraction method <strong>of</strong><br />
calculation such as the system set forth by the Medical Internal Radiation Dose Committee<br />
(MIRD) <strong>of</strong> the Society <strong>of</strong> Nuclear Medicine or the International Commission on Radiological<br />
Protection (ICRP).<br />
4. Limit on pharmacological dose<br />
The amount <strong>of</strong> active ingredient (or carrier) per administered dose <strong>of</strong> the radioactive drug shall be<br />
known, based on published or other valid studies, not to cause any clinically detectable<br />
pharmacological effect.<br />
5. Quality <strong>of</strong> the radioactive drug<br />
The radioactive drug must appropriate chemical, pharmaceutical, radiochemical, and radionclidic<br />
standards <strong>of</strong> identity, strength, quality and purity as needed such uniform and reproducible<br />
quality as to give significance to the research study conducted. Radioactive drugs for parenteral<br />
use must be prepared in sterile and pyrogen-free form.<br />
6. Labeling<br />
The final container the radioactive drug shall be labeled to include the following:<br />
• The statement “Caution: Federal law prohibits dispensing without a prescription.”<br />
• The statement “To be administered in compliance with the requirements <strong>of</strong> Federal<br />
regulations regarding radioactive drugs for research use (21 CFR 361.1).”<br />
• Identity <strong>of</strong> the radioactive drug to include the name and half-life <strong>of</strong> the radionuclide.<br />
• The identity and quantity <strong>of</strong> the active ingredient.<br />
• The total quantity <strong>of</strong> radioactivity within the immediate container at a designated reference<br />
time.<br />
• The amount <strong>of</strong> radioactivity per unit volume or unit mass at a designated reference time.<br />
• The net quantity <strong>of</strong> contents.<br />
• The route <strong>of</strong> administration if it is for other than oral use.<br />
• An identifying lot or control from which it is possible to determine the complete<br />
preparation/repackaging history <strong>of</strong> the batch <strong>of</strong> radioactive drug.<br />
• The name and address <strong>of</strong> the manufacturer, preparer, repackager, or distributor.<br />
• The expiration date<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
14
• If the drug is intended for patrenteral use, a statement as to whether the contents are sterile.<br />
• If the drug is for other than oral use, the identity <strong>of</strong> all inactive ingredients.<br />
<strong>HURC</strong> <strong>Manual</strong> Rev 3 – March 2008<br />
15