Neonatal Unconjugated Hyperbilirubinemia
Neonatal Unconjugated Hyperbilirubinemia
Neonatal Unconjugated Hyperbilirubinemia
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
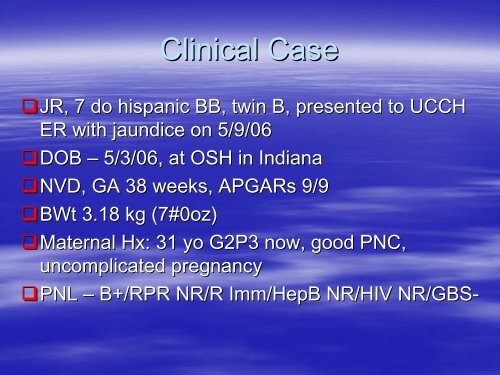
Clinical Case<br />
JR, JR, 7 do hispanic BB, twin B, presented to UCCH<br />
ER with jaundice on 5/9/06<br />
DOB DOB – 5/3/06, at OSH in Indiana<br />
NVD, NVD, GA 38 weeks, APGARs 9/9<br />
BWt BWt 3.18 kg (7#0oz)<br />
Maternal Maternal Hx: Hx:<br />
31 yo G2P3 now, good PNC,<br />
uncomplicated pregnancy<br />
PNL PNL – B+/RPR NR/R Imm/HepB NR/HIV NR/GBS-<br />
NR/GBS
Perinatal course<br />
Initial Initial PE unremarkable; + some facial bruising<br />
noted<br />
Wt Wt 2.9 kg<br />
Feeding Feeding BM/E20 – well per GCN records<br />
Voiding Voiding and stooling well<br />
Discharged Discharged at 48 hrs<br />
D/C D/C Wt – 2.03 kg<br />
Mom Mom told that baby had “borderline borderline” jaundice<br />
To call Pediatrician if she sees baby gets yellow
Baby Baby was OK at home, eating well – 10-15 10 15<br />
min each breast<br />
Stooling Stooling well – per mother<br />
On On DOL 5 mother thought babies look<br />
yellow and called the PMD<br />
She She was told to go to the hospital next day<br />
for Bili check
Baby Baby B+/Coombs-<br />
B+/Coombs<br />
Mom Mom B+<br />
Labs
Work Up<br />
CBC CBC – WBC 13.6, H/H 18.9/54, Plt 301<br />
Diff Diff N26, Bn4<br />
Retic Retic count 0.7%
Bilirubin<br />
5/5/06 5/5/06 - @48 hrs (OSH) – 13.0/0.4<br />
5/9/06 5/9/06 – DOL 7 – (OSH) – 30.9/0.6<br />
5/9/04 5/9/04 – UCCH – 31.5/0.8<br />
Sibling Sibling’s s Bili was 21 – admitted to Peds<br />
Floor for phothotherapy
ER course<br />
VSS, VSS, baby was jaundiced and “sleepy sleepy”<br />
Placed Placed under phothotherapy<br />
Given Given IVF<br />
Admitted Admitted to PICU for exchange transfusion
Here comes the NICU<br />
0230 0230 – NICU fellow received a call from<br />
upstairs to help with the exchange transfusion<br />
By By 0530 baby was in the PICU<br />
Blood Blood ordered<br />
UVC UVC placed<br />
Double Double volume exchange transfusion was<br />
done<br />
Rpt Rpt Bili – 23.8/0.7 half way through the<br />
exchange
<strong>Neonatal</strong> <strong>Hyperbilirubinemia</strong>
WHAT IS HYPERBILIRUBINEMIA AND WHY<br />
DO WE WORRY ABOUT IT?
Jaundice<br />
A A visible manifestation in the skin and sclera<br />
of elevated bilirubin concentrations<br />
Adults Adults are usually jaundiced when bilirubin<br />
levels exceed 2 mg/dL<br />
Neonates Neonates appear jaundiced when serum total<br />
bilirubin (STB) levels reach 5-7 5 7 mg/dL
Some Some degree of jaundice develops in 60-70% 60 70% of<br />
all neonates born on the United States<br />
More than 2.7 million neonates born each year in the<br />
United States will develop jaundice<br />
Chemical Chemical hyperbilirubinemia, a STB > 2.0 mg/dL,<br />
is virtually universal<br />
Although Although most jaundice is benign, there is a<br />
potential for neurological devastation and death<br />
and consequently all newborns must be assessed
WHY DO INFANTS DEVELOP<br />
HYPERBILIRUBINEMIA?
Increased Increased Bilirubin Production<br />
Decreased Decreased Binding and Transport Capacity<br />
Limited Limited Conjugation and Excretion Capacity<br />
Increased Increased Enterohepatic Circulation of<br />
Bilirubin
Bilirubin Bilirubin is the breakdown product of<br />
hemoglobin<br />
Lysis Lysis of red cells releases heme from<br />
hemoglobin<br />
Heme Heme is then converted to bilirubin and<br />
excreted
Bilirubin Synthesis<br />
There There is increased production of bilirubin in the<br />
newborn because of:<br />
Increased rate of degradation<br />
A shortened circulating erythrocyte life span (70-90 (70 90 days<br />
versus 120 days) of an increased mass<br />
A very large pool of hematopoietic tissue that ceases to<br />
function shortly after birth resulting in heme degradation<br />
An increased turnover of cytochromes (nonhemoglobin<br />
heme proteins)<br />
An increase in enterohepatic circulation
Binding and Transport<br />
<strong>Unconjugated</strong> <strong>Unconjugated</strong> bilirubin is quickly bound to<br />
albumin in the serum<br />
Newborns Newborns have reduced albumin<br />
concentrations and consequently a lower<br />
plasma binding capacity for bilirubin<br />
There There is consequently more free bilirubin in<br />
the serum<br />
It It is the free bilirubin that is believed to<br />
cause neurological damage in newborns
Conjugation and Excretion<br />
During During fetal life, removal of bilirubin is<br />
accomplished by the placenta<br />
In In the newborn, bilirubin excretion requires<br />
conversion of the nonpolar unconjugated<br />
bilirubin into a more polar water-soluble<br />
water soluble<br />
substance, conjugated bilirubin
Blood Blood flow through the hepatic artery develops<br />
during the first week of life<br />
The The ductus venosus allows blood to bypass the<br />
liver completely<br />
Conjugation Conjugation depends on the maturity of the liver<br />
cell
UDPGT<br />
UDPGT UDPGT in the newborn liver must be<br />
induced<br />
UDPGT UDPGT activity is extremely low in infants<br />
born at less than 30 weeks, 0.1% of adult<br />
levels<br />
This This activity increases to only 1% at term<br />
The The activity reaches adult levels by 6-12 6 12<br />
weeks of age
Conjugation<br />
Bilirubin Bilirubin dissociates from circulating albumin<br />
before its entry into the liver cell<br />
Bilirubin Bilirubin enters the liver by a process of carrier-<br />
mediated diffusion<br />
It It is carried by hepatic ligandin (Y protein) and Z<br />
protein<br />
Bilirubin Bilirubin is presumed to be transported from the<br />
liver cell membrane to the endoplasmic reticulum,<br />
the site of the conjugating enzyme uridine<br />
diphosphate glucuronyl transferase (UDPGT)<br />
After After conjugation, bilirubin is then excreted into<br />
bile in the intestine
Increased Enterohepatic Circulation<br />
Conjugated Conjugated bilirubin is unstable and can be<br />
easily hydrolyzed back to unconjugated bilirubin<br />
and reabsorbed through the intestinal mucosa<br />
High High mucosal beta-glucuronidase beta glucuronidase activity leads<br />
to increased hydrolysis<br />
An An alkaline environment also facilitates<br />
hydrolysis<br />
In In the newborn, the relative lack of intestinal<br />
bacterial flora to reduce bilirubin to urobilinogen<br />
further increases the bilirubin pool
<strong>Neonatal</strong> <strong>Hyperbilirubinemia</strong><br />
Physiologic Physiologic Jaundice<br />
A A progressive rise in unconjugated bilirubin to a<br />
peak of 5-6 5 6 mg/dL between 60 and 72 hours of<br />
life in white and African-American African American babies and<br />
10-14 10 14 mg/dL between 72-120 72 120 hours of life in<br />
Asian babies<br />
A A rapid decline in TSBs occurs by the 5 th or 7- 7<br />
10 th day respectively
Pathologic <strong>Unconjugated</strong><br />
<strong>Hyperbilirubinemia</strong><br />
Pathologic hyperbilirubinemia is defined as a<br />
prolonged or exaggerated<br />
hyperbilirubinemia<br />
Occurs because of disorders of:<br />
Production Production<br />
Hepatic Hepatic Uptake<br />
Conjugation<br />
Conjugation<br />
Enterohepatic Enterohepatic Circulation
Disorders of Production<br />
Isoimmunization<br />
Isoimmunization<br />
Erythrocyte Erythrocyte Enzymatic Defects<br />
Erythrocyte Erythrocyte Structural Defects<br />
Infection Infection<br />
Sequestration<br />
Sequestration<br />
Polycythemia<br />
Polycythemia
Isoimmunization<br />
Rh Rh Incompatibility<br />
ABO ABO Incompatibility<br />
Other Other Blood Group Incompatibilities
Rh Incompatibility<br />
This is a blood group incompatibility between the mother<br />
and newborn that can cause severe hemolytic anemia in<br />
the fetus and newborn<br />
The Rh antibody is produced by a Rh negative mother after<br />
being exposed to a Rh antigen from fetal blood<br />
The initial response is to make IgM antibodies<br />
Later IgG are produced which cross the placenta and bind<br />
to fetal red blood cells which are consequently destroyed<br />
Infants do not appear jaundiced at birth, but severe anemia<br />
can lead to hydrops and death<br />
After birth, infants may develop hyperbilirubinemia rapidly
The The D antigen may produce sensitization<br />
with a fetomaternal hemorrhage as small as<br />
0.1 mL<br />
At At one time this was the most common<br />
cause of kernicterus; but with the use of<br />
RhoGAM (anti-D (anti D immunoglobulin G) and<br />
careful fetal monitoring, the incidence and<br />
severity have decreased
ABO Incompatibility<br />
This This is a hemolytic disease caused by a<br />
reaction of maternal anti-A anti A or anti-B anti B<br />
antibodies with fetal A or B antigens<br />
Usually Usually milder than Rh<br />
Almost Almost exclusively in type O mothers<br />
Jaundice Jaundice appears at 24-72 24 72 hours<br />
Half Half of infants with a positive Coombs show<br />
hemolysis and some with a negative Coombs<br />
have hemolysis
Minor Blood Groups<br />
Kell, Kell, Kidd, Duffy, Lutheran<br />
< < 2 % of hemolysis from isoimmunization
Erythrocyte Enzymatic Defects<br />
Glucose Glucose-6-Phosphate Phosphate Dehydrogenase<br />
Deficiency<br />
Pyruvate Pyruvate Kinase Deficiency<br />
These These defects may have profound effects on<br />
erythrocyte function and life span
Glucose-6-Phosphate<br />
Glucose Phosphate<br />
Dehydrogenase Deficiency<br />
Glucose Glucose-6-phosphate phosphate dehydrogenase deficiency<br />
(G6PD) is a common disease, especially in people<br />
of Mediterranean; African; and Asian decent<br />
G6PD G6PD deficiency occurs in 11-13% 11 13% of African<br />
Americans<br />
Estimated Estimated 200-400 200 400 million people carry the gene<br />
X-linked linked<br />
Presentation Presentation is heterogeneous<br />
Hemolysis Hemolysis occurs, but can be absent<br />
<strong>Hyperbilirubinemia</strong> <strong>Hyperbilirubinemia</strong> occurs between 24 and 72<br />
hours of life
RBCs RBCs are unable to activate the pentose<br />
phosphate metabolic pathway<br />
And And consequently cannot defend against<br />
oxidative stress<br />
Sepsis and Vitamin K analogues<br />
Severity Severity of disease depends on type and<br />
amount of stress
Pyruvate Kinase Deficiency<br />
This This is the second most common cause of<br />
enzymatic-related enzymatic related hemolytic anemia<br />
Autosomal Autosomal recessive<br />
It It is common in people of Northern<br />
European decent<br />
It It is an enzyme required for production of<br />
ATP in RBCs
Its Its deficiency leads to decreased RBC life<br />
span and hemolysis
Erythrocyte Structural Defects<br />
Hereditary Hereditary Spherocytosis<br />
Hereditary Hereditary Elliptocytosis<br />
These These defects alter RBC structure and cause<br />
sequestration
Hereditary Elliptocytosis<br />
Incidence Incidence of 1:4000<br />
Autosomal Autosomal dominant<br />
Abnormality Abnormality in spectrin or glycophorin C<br />
Hemolysis Hemolysis and hyperbilirubinemia are<br />
unusual in the newborn period
Hereditary Spherocytosis<br />
Incidence Incidence of 1:5000<br />
Autosomal Autosomal dominant<br />
Heterogeneous presentation<br />
Fifty Fifty percent present with hemolytic anemia,<br />
hyperbilirubinemia, reticulocytosis, and<br />
increased erythrocyte osmotic fragility
Infection<br />
<strong>Hyperbilirubinemia</strong> <strong>Hyperbilirubinemia</strong> is believed to be<br />
secondary to hemolysis<br />
Sepsis Sepsis may impair conjugation also leading<br />
to increased bilirubin levels
Sequestration<br />
Sequestration Sequestration of blood in body cavities may<br />
lead to hyperbilirubinemia as the body<br />
metabolizes hemoglobin<br />
Cephalohematomas, Cephalohematomas, subdural hematomas,<br />
subgaleal hematomas<br />
Excessive Excessive bruising
Polycythemia<br />
The The increase in red blood cell mass has the<br />
potential to overload the newborn<br />
hemoglobin metabolism capacities
Disorders of Hepatic Uptake<br />
Gilberts Gilberts Syndrome<br />
This This is a benign disorder producing persistent<br />
unconjugated hyperbilirubinemia<br />
There is defective hepatic uptake and decreased<br />
UDPGT activity<br />
It usually occurs in the second decade of life, but can<br />
present in neonates
Disorders of Conjugation<br />
Crigler Crigler-Najjar Najjar Syndrome<br />
Transient Transient Familial <strong>Neonatal</strong><br />
<strong>Hyperbilirubinemia</strong> (Lucey-Driscoll (Lucey Driscoll Syndrome)<br />
Pyloric Pyloric Stenosis<br />
Hypothyroidism<br />
Hypothyroidism
Type Type I<br />
Crigler-Najjar Crigler Najjar Syndrome<br />
There is absence of UDPGT activity<br />
Autosomal recessive<br />
1:1,000,000<br />
Severe unconjugated hyperbilirubinemia develops and<br />
persists beyond the first week of life<br />
No hemolysis<br />
Lifelong risk of kernicterus<br />
Lifelong phototherapy is needed
Type Type II<br />
There There is various degree of decrease of UDPGT<br />
activity<br />
Typically Typically benign<br />
There There is unconjugated hyperbilirubinemia in the<br />
first few days of life that does not exceed 20<br />
mg/dL<br />
<strong>Hyperbilirubinemia</strong> <strong>Hyperbilirubinemia</strong> persists into adulthood<br />
The The treatment is phenobarbital
Transient Familial <strong>Neonatal</strong><br />
<strong>Hyperbilirubinemia</strong><br />
Neonates Neonates develop severe nonhemolytic<br />
hyperbilirubinemia<br />
Their Their serum contains high concentrations of<br />
glucuronyl transferase inhibitors<br />
This This inhibitor decreases by about 14 days of<br />
life and consequently hyperbilirubinemia<br />
resolves
Pyloric Stenosis<br />
10 10-25% 25% of babies with pyloric stenosis have<br />
hyperbilirubinemia at the time of<br />
presentation<br />
Hepatic Hepatic glucuronyl tranferase activity is<br />
reduced<br />
Surgical Surgical correction improves bilirubin levels
Hypothyroidism<br />
UDPGT UDPGT activity is deficient and remains low<br />
for weeks with hypothyroidism
Disorders of Enterohepatic<br />
Circulation<br />
Breast Breast Feeding Jaundice<br />
Breast Breast Milk Jaundice
Breast Feeding Jaundice<br />
<strong>Unconjugated</strong> <strong>Unconjugated</strong> hyperbilirubinemia is secondary to a<br />
suboptimal establishment of breastfeeding<br />
Newborns Newborns are under-hydrated under hydrated and in a state of<br />
starvation.<br />
They They also have delayed passage of meconium<br />
Enterohepatic Enterohepatic reuptake of bilirubin is consequently<br />
increased, leading to hyperbilirubinemia<br />
Treatment Treatment and prevention include frequent<br />
feedings (8-12/day) (8 12/day)
Breast Milk Jaundice<br />
Occurs Occurs after 3-5 3 5 days of life, typically at 2-3 2 3<br />
weeks of life<br />
The The etiology is unknown, but believed to be<br />
a factor in breast milk or an altered<br />
chemistry in breast milk that enhances<br />
intestinal reabsorption of bilirubin<br />
No No need to stop breastfeeding unless<br />
bilirubin levels are dangerously high
WHY DO WE WORRY ABOUT<br />
HYPERBILIRUBINEMIA?
Sequelae<br />
Bilirubin Bilirubin may penetrate the brain cell and<br />
cause neuronal dysfunction or death if not<br />
carefully managed<br />
Bilirubin Bilirubin causes staining and necrosis of<br />
neurons in the basal ganglia, hippocampal<br />
cortex, subthalamic nuclei, and cerebellum<br />
which is followed by gliosis<br />
50%of 50%of patients with kernicterus die
Acute Bilirubin Encephalopathy<br />
Phase Phase 1 - poor suck, hypotonia, and<br />
depressed sensorium<br />
Phase Phase 2 - fever and hypertonia or<br />
opisthotonos<br />
Phase Phase 3 - less hypertonia, high pitched cry,<br />
hearing and visual abnormalities, poor<br />
feeding, athetosis
Long Long term sequelae:<br />
Kernicterus<br />
Chorioathetoid Chorioathetoid cerebral palsy<br />
Sensorineural Sensorineural hearing loss<br />
Upward Upward gaze palsy<br />
Dental Dental-enamel enamel dysplasia<br />
Mental Mental retardation
SO, WHAT CAN WE DO?
Diagnosis and Management<br />
There There has been evidence that neonatal<br />
jaundice can be treated less aggressively,<br />
but there is not a consensus yet and until<br />
then it should be managed conservatively
Diagnosis<br />
All All neonates are entitled to a thorough<br />
physical examination and evaluation to<br />
determine which neonates are at an<br />
increased risk for becoming abnormally<br />
jaundiced and developing sequelae
Risk Assessment<br />
Every Every newborn should be assessed,<br />
especially if discharged before 72 hours of<br />
life<br />
2 2 options:<br />
TSB or TcB before discharge and plot results on the<br />
nomogram
Nomogram for designation of risk in 2840 well newborns at 36 or more weeks'<br />
gestational age with birth weight of 2000 g or more or 35 or more weeks' gestational<br />
age and birth weight of 2500 g or more based on the hour-specific serum bilirubin<br />
values<br />
Subcommittee on <strong>Hyperbilirubinemia</strong>, Pediatrics 2004;114:297-316<br />
Copyright ©2004 American Academy of Pediatrics
Assessment of risk<br />
– Major<br />
Predischarge TSB or TcB in the high-risk high risk zone<br />
Jaundice in the first 24h<br />
Hemolytic disease<br />
Gestational age 35-36 35 36 weeks<br />
Sibling received phototherapy<br />
Cephalohematoma or bruising<br />
Poor breastfeeding<br />
East Asian descent
Carbon Monoxide<br />
End End Tidal Carbon Monoxide detection<br />
allows rapid noninvasive detection of infants<br />
at risk for hemolytic disease and<br />
consequently at high risk for neurological<br />
sequelae
Carbon Monoxide<br />
The The breakdown of hemoglobin by heme<br />
oxygenase produces free iron and carbon<br />
monoxide in equimolar amounts<br />
The The carbon monoxide formed by heme<br />
degradation is excreted unchanged by the lungs.<br />
Although Although there are other endogenous and<br />
exogenous sources of CO, quantitative estimation<br />
of its excretion or synthesis offers a reasonably<br />
accurate assessment of bilirubin synthesis
Physical Examination<br />
Detection Detection of clinical jaundice requires digital<br />
pressure and the proper lighting, preferably<br />
daylight<br />
If If clinical jaundice is detected, a total and<br />
direct serum bilirubin or transcutaneous<br />
bilirubin (TcB) should be measured and<br />
plotted on the nomogram
If: If:<br />
When should I do more?<br />
Cord Cord bilirubin is greater than 4 mg/dL<br />
A A rate of rise greater than or equal to 0.5<br />
mg/dL/hour over a 4-8 4 8 hour period<br />
An An increase of 5 mg/dL per day<br />
13 13-15 15 mg/dL in a term infant<br />
10 10 mg/dL in a preterm infant<br />
If If jaundice persist greater than 10 days
Then what?<br />
Determination Determination of maternal blood group and Rh<br />
type<br />
Screen Screen for antibodies directed against minor<br />
erythrocyte antigens<br />
Determination Determination of newborns blood type and Rh<br />
type<br />
Direct Direct Coombs test<br />
Hemoglobin Hemoglobin and Hematocrit<br />
Peripheral Peripheral blood smear<br />
Reticulocyte Reticulocyte count<br />
G6PD G6PD level
Algorithm for the management of jaundice in the newborn nursery<br />
Subcommittee on <strong>Hyperbilirubinemia</strong>, Pediatrics 2004;114:297-316<br />
Copyright ©2004 American Academy of Pediatrics
Guidelines for phototherapy in hospitalized infants of 35 or more weeks' gestation<br />
Subcommittee on <strong>Hyperbilirubinemia</strong>, Pediatrics 2004;114:297-316<br />
opyright ©2004 American Academy of Pediatrics
Helpful resources<br />
Bili-Aid Bili Aid
Phototherapy<br />
The The main mechanism of action<br />
Geometric Geometric photoisomerization of unconjugated<br />
bilirubin that can then be excreted without<br />
conjugation
Wavelength<br />
Wavelength<br />
Technique<br />
Bilirubin Bilirubin absorbs light maximally in the blue<br />
range (420-500 (420 500 nm), with a peak at 460 nm for<br />
albumin-bound albumin bound bilirubin and 440 nm for free<br />
bilirubin<br />
Special blue lamps have a spectrum between 420- 420<br />
480
Irradiance Irradiance<br />
The The energy output measured in microwatts per<br />
square centimeter per nanometer<br />
Optimal Optimal level is 11 microwatts per square<br />
centimeter per nanometer<br />
Intensive Intensive phototherapy is 30 microwatts per<br />
square centimeter per nanometer
Positioning Positioning<br />
Within Within 10 cm of the patient for fluorescent tubes<br />
Surface Surface area<br />
The The greater the surface area exposed, the more<br />
effective the phototherapy
Hydration<br />
There There is no evidence that excessive fluid<br />
administration affects the serum bilirubin<br />
concentration<br />
If If admitted with dehydration, babies will<br />
need to be rehydrated and then fed<br />
Feeding Feeding inhibits enterohepatic circulation of<br />
bilirubin<br />
Important Important to watch fluid status for excretion<br />
of bilirubin
The The TSB level for discontinuing<br />
phototherapy depends on the age at which<br />
phototherapy was started and the etiology<br />
For For infants readmitted after birth admission, you<br />
can discontinue usually at 13-14 13 14 mg/dL with a<br />
follow up visit 24 hours after discharge<br />
There There is no need for a rebound bilirubin, unless<br />
there is hemolytic disease
Pharmacological Therapy<br />
Phenobarbital<br />
Phenobarbital<br />
Albumin Albumin<br />
Tin Tin-mesoporphyrin<br />
mesoporphyrin<br />
Inhibits Inhibits heme oxygenase<br />
Intravenous Intravenous gamma-globulin<br />
gamma globulin<br />
Shown Shown to reduce the need for exchange<br />
transfusions in isoimmune hemolytic disease
Guidelines for exchange transfusion in infants 35 or more weeks' gestation<br />
Subcommittee on <strong>Hyperbilirubinemia</strong>, Pediatrics 2004;114:297-316<br />
Copyright ©2004 American Academy of Pediatrics
Exchange Exchange transfusions are recommended if<br />
TSB is greater than or equal to 25 mg/dL in<br />
a healthy full term infant<br />
If If rate of rise is greater than or equal to 0.5<br />
mg/dL/hour<br />
If If there is active hemolysis or other risk<br />
factors, then an exchange transfusion may<br />
be warranted at a lower bilirubin level
Exchange Transfusion<br />
With With a exchange transfusion, approximately<br />
85% of erythrocytes will be replaced<br />
Serum Serum bilirubin levels should decrease by<br />
50%
American Academy of Pediatrics<br />
In In 1994 the AAP established practice<br />
parameters for the management of<br />
hyperbilirubinemia<br />
Revised Revised in 2004
Management Management of <strong>Hyperbilirubinemia</strong> in the<br />
Newborn Infant 35 or More Weeks of<br />
Gestation<br />
Goals: Goals:<br />
Promote and support successful breastfeeding<br />
Establish nursery protocols for the identification and<br />
evaluation of hyperbilirubinemia<br />
Measure the total serum bilirubin or transcutaneous<br />
bilirubin levels on infants jaundiced in the first24<br />
hours
Recognize that visual estimation of the degree of<br />
jaundice can lead to errors, particularly in darkly<br />
pigmented infants<br />
Interpret all bilirubin levels according to the infant’s infant s<br />
age in hours<br />
Recognize that infants less than 38 weeks’ weeks gestation,<br />
particularly those who are breast fed, are at higher risk<br />
of developing hyperbilirubinemai and require closer<br />
surveillance and monitoring<br />
Perform a systematic assessment on all infants before<br />
discharge for the risk of severe hyperbilirubinemia
Provide parents with written and verbal information<br />
about newborn jaundice<br />
Provide appropriate follow-up follow up based on the time of<br />
discharge and the risk assessment<br />
Treat infants, when indicated, with phototherapy or<br />
exchange transfusion
Infant Infant Discharged<br />
< 24 hours<br />
24 to 47.9 hours<br />
48 to 72 hours<br />
Follow Up<br />
Should Be Seen By Age<br />
72 hours<br />
96 hours<br />
120 hours
Fanaroff, Fanaroff, Martin. <strong>Neonatal</strong>-Perinatal<br />
<strong>Neonatal</strong> Perinatal<br />
Medicine, 7 th Edition.<br />
Management Management of <strong>Hyperbilirubinemia</strong> in the<br />
Newborn Infant 35 or More Weeks of<br />
Gestation, Pediatrics 2004;114;297-316<br />
2004;114;297 316<br />
Taeusch, Taeusch, Ballard, Gleason. Avery’s Avery s<br />
Diseases of the Newborn, 8 th Edition