here - CD8 T cells - The Body
here - CD8 T cells - The Body
here - CD8 T cells - The Body
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
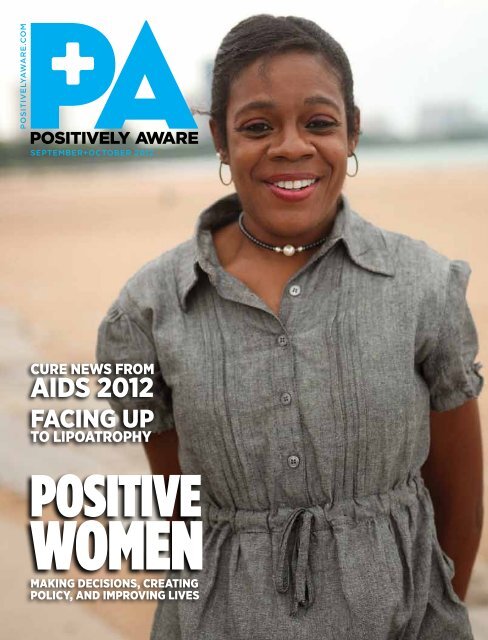
positivelyaware.com<br />
september+october 2012<br />
CURE NEWS FROM<br />
AIDS 2012<br />
FACINg Up<br />
tO lIpOAtROphy<br />
POSITIVE<br />
WOmEn<br />
MAkINg DECISIONS, CREAtINg<br />
pOlICy, AND IMpROvINg lIvES
ABOUT PREZISTA ®<br />
PREZISTA ® (darunavir) is a prescription medicine. It is one treatment option<br />
in the class of HIV (human immunodefi ciency virus) medicines known as<br />
protease inhibitors.<br />
PREZISTA ® is always taken with and at the same time as ritonavir (Norvir ® ),<br />
in combination with other HIV medicines for the treatment of HIV infection<br />
in adults. PREZISTA ® should also be taken with food.<br />
• <strong>The</strong> use of other medicines active against HIV in combination with<br />
PREZISTA ® /ritonavir (Norvir ® ) may increase your ability to fi ght HIV.<br />
Your healthcare professional will work with you to fi nd the right<br />
combination of HIV medicines<br />
• It is important that you remain under the care of your healthcare<br />
professional during treatment with PREZISTA ®<br />
PREZISTA ® does not cure HIV infection or AIDS and you may<br />
continue to experience illnesses associated with HIV-1 infection,<br />
including opportunistic infections. You should remain under the<br />
care of a doctor when using PREZISTA. ®<br />
Please read Important Safety Information below, and talk to your<br />
healthcare professional to learn if PREZISTA ® is right for you.<br />
IMPORTANT SAFETY INFORMATION<br />
What is the most important information I should know<br />
about PREZISTA ® ?<br />
• PREZISTA ® can interact with other medicines and cause<br />
serious side effects. See “Who should not take PREZISTA ® ?”<br />
• PREZISTA ® may cause liver problems. Some people taking<br />
PREZISTA, ® together with Norvir ® (ritonavir), have developed liver<br />
problems which may be life-threatening. Your healthcare professional<br />
should do blood tests before and during your combination treatment<br />
with PREZISTA. ® If you have chronic hepatitis B or C infection, your<br />
healthcare professional should check your blood tests more often<br />
because you have an increased chance of developing liver problems<br />
• Tell your healthcare professional if you have any of these signs and<br />
symptoms of liver problems: dark (tea-colored) urine, yellowing<br />
of your skin or whites of your eyes, pale-colored stools (bowel<br />
movements), nausea, vomiting, pain or tenderness on your right<br />
side below your ribs, or loss of appetite<br />
• PREZISTA ® may cause a severe or life-threatening skin<br />
reaction or rash. Sometimes these skin reactions and skin rashes<br />
can become severe and require treatment in a hospital. You should<br />
call your healthcare professional immediately if you develop a rash.<br />
However, stop taking PREZISTA ® and ritonavir combination treatment<br />
and call your healthcare professional immediately if you develop any<br />
skin changes with these symptoms: fever, tiredness, muscle or joint<br />
pain, blisters or skin lesions, mouth sores or ulcers, red or infl amed<br />
eyes, like “pink eye.” Rash occurred more often in patients taking<br />
PREZISTA ® and raltegravir together than with either drug separately,<br />
but was generally mild<br />
Who should not take PREZISTA ® ?<br />
• Do not take PREZISTA ® if you are taking the following<br />
medicines: alfuzosin (Uroxatral ® ), dihydroergotamine (D.H.E.45, ®<br />
Embolex, ® Migranal ® ), ergonovine, ergotamine (Cafergot, ® Ergomar ® ),<br />
methylergonovine, cisapride (Propulsid ® ), pimozide (Orap ® ), oral<br />
midazolam, triazolam (Halcion ® ), the herbal supplement St. John’s wort<br />
(Hypericum perforatum), lovastatin (Mevacor, ® Altoprev, ® Advicor ® ),<br />
simvastatin (Zocor, ® Simcor, ® Vytorin ® ), rifampin (Rifadin, ® Rifater, ®<br />
Rifamate, ® Rimactane ® ), sildenafi l (Revatio ® ) when used to treat<br />
pulmonary arterial hypertension, indinavir (Crixivan ® ), lopinavir/<br />
ritonavir (Kaletra ® ), saquinavir (Invirase ® ), boceprevir (Victrelis ),<br />
or telaprevir (Incivek )<br />
• Before taking PREZISTA, ® tell your healthcare professional if you are<br />
taking sildenafi l (Viagra, ® Revatio ® ), vardenafi l (Levitra, ® Staxyn ® ),<br />
tadalafi l (Cialis, ® Adcirca ® ), atorvastatin (Lipitor ® ), rosuvastatin<br />
(Crestor ® ), pravastatin (Pravachol ® ), or colchicine (Colcrys, ®<br />
Col-Probenecid ® ). Tell your healthcare professional if you are taking<br />
estrogen-based contraceptives (birth control). PREZISTA ® might reduce<br />
the effectiveness of estrogen-based contraceptives. You must take<br />
additional precautions for birth control, such as condoms<br />
This is not a complete list of medicines. Be sure to tell your<br />
healthcare professional about all the medicines you are taking or<br />
plan to take, including prescription and nonprescription medicines,<br />
vitamins, and herbal supplements.<br />
What should I tell my doctor before I take PREZISTA ® ?<br />
• Before taking PREZISTA, ® tell your healthcare professional if you have<br />
any medical conditions, including liver problems (including hepatitis B<br />
or C), allergy to sulfa medicines, diabetes, or hemophilia<br />
• Tell your healthcare professional if you are pregnant or planning<br />
to become pregnant, or are breastfeeding<br />
— <strong>The</strong> effects of PREZISTA ® on pregnant women or their unborn<br />
babies are not known. You and your healthcare professional will<br />
need to decide if taking PREZISTA ® is right for you<br />
— Do not breastfeed. It is not known if PREZISTA ® can be passed<br />
to your baby in your breast milk and whether it could harm your<br />
baby. Also, mothers with HIV should not breastfeed because HIV<br />
can be passed to your baby in the breast milk<br />
What are the possible side effects of PREZISTA ® ?<br />
• High blood sugar, diabetes or worsening of diabetes, and increased<br />
bleeding in people with hemophilia have been reported in patients<br />
taking protease inhibitor medicines, including PREZISTA ®<br />
• Changes in body fat have been seen in some patients taking HIV<br />
medicines, including PREZISTA. ® <strong>The</strong> cause and long-term health<br />
effects of these conditions are not known at this time<br />
• Changes in your immune system can happen when you start taking<br />
HIV medicines. Your immune system may get stronger and begin<br />
to fi ght infections that have been hidden<br />
• <strong>The</strong> most common side effects related to taking PREZISTA ® include<br />
diarrhea, nausea, rash, headache, stomach pain, and vomiting. This is<br />
not a complete list of all possible side effects. If you experience these<br />
or other side effects, talk to your healthcare professional. Do not stop<br />
taking PREZISTA ® or any other medicines without fi rst talking to your<br />
healthcare professional<br />
You are encouraged to report negative side effects of<br />
prescription drugs to the FDA. Visit www.fda.gov/medwatch,<br />
or call 1-800-FDA-1088.<br />
Please refer to the ritonavir (Norvir ® ) Product Information (PI and PPI)<br />
for additional information on precautionary measures.<br />
Please read accompanying Patient Information for PREZISTA ®<br />
and discuss any questions you have with your doctor.<br />
28PRZDTC0288R8
IS THE PREZISTA ®<br />
EXPERIENCE<br />
RIGHT FOR YOU?<br />
T<strong>here</strong> is no other person in the world who is exactly like you. And<br />
no HIV treatments are exactly alike, either. That’s why you should<br />
ask your healthcare professional about PREZISTA ® (darunavir).<br />
Once-Daily PREZISTA ® taken with ritonavir and in combination<br />
with other HIV medications can help lower your viral load<br />
and keep your HIV under control over the long term.<br />
In a clinical study* of almost 4 years (192 weeks), 7 out of 10<br />
adults who had never taken HIV medications before<br />
maintained undetectable † viral loads with PREZISTA ®<br />
plus ritonavir and Truvada. ®<br />
Find out if the PREZISTA ® EXPERIENCE is right for you.<br />
Ask your healthcare professional and learn more<br />
at DiscoverPREZISTA.com<br />
Please read the Important Safety Information and<br />
Patient Information on adjacent pages.<br />
Snap a quick pic of our logo to show your<br />
doctor and get the conversation started.<br />
*A randomized open label Phase 3 trial comparing PREZISTA ® /ritonavir 800/100 mg<br />
once daily (n=343) vs. Kaletra ® /ritonavir 800/200 mg/day (n=346).<br />
†Undetectable was defi ned as a viral load of less than 50 copies per mL.<br />
Registered trademarks are the property of their respective owners.<br />
Janssen <strong>The</strong>rapeutics,<br />
Division of Janssen Products, LP<br />
© Janssen <strong>The</strong>rapeutics, Division of Janssen Products, LP<br />
2012 06/12 28PRZ12036G
PREZISTA (pre-ZIS-ta)<br />
(darunavir)<br />
Oral Suspension<br />
PREZISTA (pre-ZIS-ta)<br />
(darunavir)<br />
Tablets<br />
Read this Patient Information before you start taking PREZISTA and<br />
each time you get a refill. T<strong>here</strong> may be new information. This<br />
information does not take the place of talking to your healthcare<br />
provider about your medical condition or your treatment.<br />
Also read the Patient Information leaflet for NORVIR ® (ritonavir).<br />
What is the most important information I should<br />
know about PREZISTA?<br />
• PREZISTA can interact with other medicines and cause serious<br />
side effects. It is important to know the medicines that should not be<br />
taken with PREZISTA. See the section “Who should not take<br />
PREZISTA?”<br />
• PREZISTA may cause liver problems. Some people taking PREZISTA<br />
in combination with NORVIR ® (ritonavir) have developed liver<br />
problems which may be life-threatening. Your healthcare provider<br />
should do blood tests before and during your combination treatment<br />
with PREZISTA. If you have chronic hepatitis B or C infection, your<br />
healthcare provider should check your blood tests more often<br />
because you have an increased chance of developing liver problems.<br />
• Tell your healthcare provider if you have any of the below signs and<br />
symptoms of liver problems.<br />
• Dark (tea colored) urine<br />
• yellowing of your skin or whites of your eyes<br />
• pale colored stools (bowel movements)<br />
• nausea<br />
• vomiting<br />
• pain or tenderness on your right side below your ribs<br />
• loss of appetite<br />
PREZISTA may cause severe or life-threatening skin reactions or rash.<br />
Sometimes these skin reactions and skin rashes can become severe<br />
and require treatment in a hospital. You should call your healthcare<br />
provider immediately if you develop a rash. However, stop taking<br />
PREZISTA and ritonavir combination treatment and call your healthcare<br />
provider immediately if you develop any skin changes with symptoms<br />
below:<br />
• fever<br />
• tiredness<br />
• muscle or joint pain<br />
• blisters or skin lesions<br />
• mouth sores or ulcers<br />
• red or inflamed eyes, like “pink eye” (conjunctivitis)<br />
Rash occurred more often in patients taking PREZISTA and raltegravir<br />
together than with either drug separately, but was generally mild.<br />
See “What are the possible side effects of PREZISTA?” for more<br />
information about side effects.<br />
What is PREZISTA?<br />
PREZISTA is a prescription anti-HIV medicine used with ritonavir and<br />
other anti-HIV medicines to treat adults with human immunodeficiency<br />
virus (HIV-1) infection. PREZISTA is a type of anti-HIV medicine called a<br />
protease inhibitor. HIV is the virus that causes AIDS (Acquired Immune<br />
Deficiency Syndrome).<br />
When used with other HIV medicines, PREZISTA may help to reduce<br />
the amount of HIV in your blood (called “viral load”). PREZISTA may<br />
also help to increase the number of white blood <strong>cells</strong> called CD4 (T) cell<br />
which help fight off other infections. Reducing the amount of HIV and<br />
increasing the CD4 (T) cell count may improve your immune system.<br />
This may reduce your risk of death or infections that can happen when<br />
your immune system is weak (opportunistic infections).<br />
PREZISTA does not cure HIV infection or AIDS and you may continue to<br />
experience illnesses associated with HIV-1 infection, including<br />
opportunistic infections. You should remain under the care of a doctor<br />
when using PREZISTA.<br />
Avoid doing things that can spread HIV-1 infection.<br />
• Do not share needles or other injection equipment.<br />
• Do not share personal items that can have blood or body fluids on<br />
them, like toothbrushes and razor blades.<br />
IMPORTANT PATIENT INFORMATION<br />
• Do not have any kind of sex without protection. Always practice<br />
safe sex by using a latex or polyurethane condom to lower the<br />
chance of sexual contact with semen, vaginal secretions, or blood.<br />
Ask your healthcare provider if you have any questions on how to<br />
prevent passing HIV to other people.<br />
Who should not take PREZISTA?<br />
Do not take PREZISTA with any of the following medicines:<br />
• alfuzosin (Uroxatral ® )<br />
• dihydroergotamine (D.H.E. 45 ® , Embolex ® , Migranal ® ), ergonovine,<br />
ergotamine (Cafergot ® , Ergomar ® ) methylergonovine<br />
• cisapride<br />
• pimozide (Orap ® )<br />
• oral midazolam, triazolam (Halcion ® )<br />
• the herbal supplement St. John’s Wort (Hypericum perforatum)<br />
• the cholesterol lowering medicines lovastatin (Mevacor ® , Altoprev ® ,<br />
Advicor ® ) or simvastatin (Zocor ® , Simcor ® , Vytorin ® )<br />
• rifampin (Rifadin ® , Rifater ® , Rifamate ® , Rimactane ® )<br />
• sildenafil (Revatio ® ) only when used for the treatment of pulmonary<br />
arterial hypertension.<br />
Serious problems can happen if you take any of these medicines with<br />
PREZISTA.<br />
What should I tell my doctor before I take PREZISTA?<br />
PREZISTA may not be right for you. Before taking PREZISTA, tell your<br />
healthcare provider if you:<br />
• have liver problems, including hepatitis B or hepatitis C<br />
• are allergic to sulfa medicines<br />
• have high blood sugar (diabetes)<br />
• have hemophilia<br />
• are pregnant or planning to become pregnant. It is not known if<br />
PREZISTA will harm your unborn baby.<br />
Pregnancy Registry: You and your healthcare provider will need to<br />
decide if taking PREZISTA is right for you. If you take PREZISTA<br />
while you are pregnant, talk to your healthcare provider about how<br />
you can be included in the Antiretroviral Pregnancy Registry. <strong>The</strong><br />
purpose of the registry is follow the health of you and your baby.<br />
• are breastfeeding or plan to breastfeed. Do not breastfeed. We do<br />
not know if PREZISTA can be passed to your baby in your breast<br />
milk and whether it could harm your baby. Also, mothers with HIV-1<br />
should not breastfeed because HIV-1 can be passed to the baby in<br />
the breast milk.<br />
Tell your healthcare provider about all the medicines you take including<br />
prescription and nonprescription medicines, vitamins, and herbal<br />
supplements. Using PREZISTA and certain other medicines may affect<br />
each other causing serious side effects. PREZISTA may affect the way<br />
other medicines work and other medicines may affect how PREZISTA<br />
works.<br />
Especially tell your healthcare provider if you take:<br />
• medicine to treat HIV<br />
• estrogen-based contraceptives (birth control). PREZISTA might<br />
reduce the effectiveness of estrogen-based contraceptives. You<br />
must take additional precautions for birth control such as a condom.<br />
• medicine for your heart such as bepridil, lidocaine (Xylocaine<br />
Viscous ® ), quinidine (Nuedexta ® ), amiodarone (Pacerone ® ,<br />
Cardarone ® ), digoxin (Lanoxin ® ), flecainide (Tambocor ® ),<br />
propafenone (Rythmol ® )<br />
• warfarin (Coumadin ® , Jantoven ® )<br />
• medicine for seizures such as carbamazepine (Carbatrol ® , Equetro ® ,<br />
Tegretol ® , Epitol ® ), phenobarbital, phenytoin (Dilantin ® , Phenytek ® )<br />
• medicine for depression such as trazadone and desipramine<br />
(Norpramin ® )<br />
• clarithromycin (Prevpac ® , Biaxin ® )<br />
• medicine for fungal infections such as ketoconazole (Nizoral ® ),<br />
itraconazole (Sporanox ® , Onmel ® ), voriconazole (VFend ® )<br />
• colchicine (Colcrys ® , Col-Probenecid ® )<br />
• rifabutin (Mycobutin ® )<br />
• medicine used to treat blood pressure, a heart attack, heart failure,<br />
or to lower pressure in the eye such as metoprolol (Lopressor ® ,<br />
Toprol-XL ® ), timolol (Cosopt ® , Betimol ® , Timoptic ® , Isatolol ® ,<br />
Combigan ® )<br />
• midazolam administered by injection<br />
• medicine for heart disease such as felodipine (Plendil ® ), nifedipine<br />
(Procardia ® , Adalat CC ® , Afeditab CR ® ), nicardipine (Cardene ® )
• steroids such as dexamethasone, fluticasone (Advair Diskus ® ,<br />
Veramyst ® , Flovent ® , Flonase ® )<br />
• bosentan (Tracleer ® )<br />
• medicine to treat chronic hepatitis C such as boceprevir<br />
(Victrelis TM ), telaprevir (Incivek TM )<br />
• medicine for cholesterol such as pravastatin (Pravachol ® ),<br />
atorvastatin (Lipitor ® ), rosuvastatin (Crestor ® )<br />
• medicine to prevent organ transplant failure such as cyclosporine<br />
(Gengraf ® , Sandimmune ® , Neoral ® ), tacrolimus (Prograf ® ), sirolimus<br />
(Rapamune ® )<br />
• salmeterol (Advair ® , Serevent ® )<br />
• medicine for narcotic withdrawal such as methadone (Methadose ® ,<br />
Dolophine Hydrochloride), buprenorphine (Butrans ® , Buprenex ® ,<br />
Subutex ® ), buprenorphine/naloxone (Suboxone ® )<br />
• medicine to treat schizophrenia such as risperidone (Risperdal ® ),<br />
thioridazine<br />
• medicine to treat erectile dysfunction or pulmonary hypertension<br />
such as sildenafil (Viagra ® , Revatio ® ), vardenafil (Levitra ® , Staxyn ® ),<br />
tadalafil (Cialis ® , Adcirca ® )<br />
• medicine to treat anxiety, depression or panic disorder such as<br />
sertraline (Zoloft ® ), paroxetine (Paxil ® )<br />
This is not a complete list of medicines that you should tell your<br />
healthcare provider that you are taking. Ask your healthcare provider<br />
or pharmacist if you are not sure if your medicine is one that is listed<br />
above. Know the medicines you take. Keep a list of them to show your<br />
doctor or pharmacist when you get a new medicine. Do not start any<br />
new medicines while you are taking PREZISTA without first talking with<br />
your healthcare provider.<br />
How should I take PREZISTA?<br />
• Take PREZISTA every day exactly as prescribed by your healthcare<br />
provider.<br />
• You must take ritonavir (NORVIR ® ) at the same time as PREZISTA.<br />
• Do not change your dose of PREZISTA or stop treatment without<br />
talking to your healthcare provider first.<br />
• Take PREZISTA and ritonavir (NORVIR ® ) with food.<br />
• Swallow PREZISTA tablets whole with a drink. If you have difficulty<br />
swallowing PREZISTA tablets, PREZISTA oral suspension is also<br />
available. Your health care provider will help determine whether<br />
PREZISTA tablets or oral suspension is right for you.<br />
• PREZISTA oral suspension should be given with the supplied oral<br />
dosing syringe. Shake the suspension well before each usage.<br />
• If you take too much PREZISTA, call your healthcare provider or go<br />
to the nearest hospital emergency room right away.<br />
What should I do if I miss a dose?<br />
People who take PREZISTA one time a day:<br />
• If you miss a dose of PREZISTA by less than 12 hours, take your<br />
missed dose of PREZISTA right away. <strong>The</strong>n take your next dose of<br />
PREZISTA at your regularly scheduled time.<br />
• If you miss a dose of PREZISTA by more than 12 hours, wait and then<br />
take the next dose of PREZISTA at your regularly scheduled time.<br />
People who take PREZISTA two times a day<br />
• If you miss a dose of PREZISTA by less than 6 hours, take your<br />
missed dose of PREZISTA right away. <strong>The</strong>n take your next dose of<br />
PREZISTA at your regularly scheduled time.<br />
• If you miss a dose of PREZISTA by more than 6 hours, wait and then<br />
take the next dose of PREZISTA at your regularly scheduled time.<br />
If a dose of PREZISTA is skipped, do not double the next dose. Do not<br />
take more or less than your prescribed dose of PREZISTA at any one<br />
time.<br />
What are the possible side effects of PREZISTA?<br />
PREZISTA can cause side effects including:<br />
• See “What is the most important information I should know about<br />
PREZISTA?”<br />
• Diabetes and high blood sugar (hyperglycemia). Some people who<br />
take protease inhibitors including PREZISTA can get high blood<br />
sugar, develop diabetes, or your diabetes can get worse. Tell your<br />
healthcare provider if you notice an increase in thirst or urinate<br />
often while taking PREZISTA.<br />
• Changes in body fat. <strong>The</strong>se changes can happen in people who take<br />
anti retroviral therapy. <strong>The</strong> changes may include an increased<br />
amount of fat in the upper back and neck (“buffalo hump”), breast,<br />
and around the back, chest, and stomach area. Loss of fat from the<br />
legs, arms, and face may also happen. <strong>The</strong> exact cause and longterm<br />
health effects of these conditions are not known.<br />
IMPORTANT PATIENT INFORMATION<br />
• Changes in your immune system (Immune Reconstitution Syndrome)<br />
can happen when you start taking HIV medicines. Your immune<br />
system may get stronger and begin to fight infections that have been<br />
hidden in your body for a long time. Call your healthcare provider<br />
right away if you start having new symptoms after starting your HIV<br />
medicine.<br />
• Increased bleeding for hemophiliacs. Some people with hemophilia<br />
have increased bleeding with protease inhibitors including<br />
PREZISTA.<br />
<strong>The</strong> most common side effects of PREZISTA include:<br />
• diarrhea • headache<br />
• nausea • abdominal pain<br />
• rash • vomiting<br />
Tell your healthcare provider if you have any side effect that bothers<br />
you or that does not go away.<br />
<strong>The</strong>se are not all of the possible side effects of PREZISTA. For more<br />
information, ask your health care provider.<br />
Call your doctor for medical advice about side effects. You may report<br />
side effects to the FDA at 1-800-FDA-1088.<br />
How should I store PREZISTA?<br />
• Store PREZISTA oral suspension and tablets at room temperature<br />
[77°F (25°C)].<br />
• Do not refrigerate or freeze PREZISTA oral suspension.<br />
• Keep PREZISTA away from high heat.<br />
• PREZISTA oral suspension should be stored in the original container.<br />
Keep PREZISTA and all medicines out of the reach of children.<br />
General information about PREZISTA<br />
Medicines are sometimes prescribed for purposes other than those<br />
listed in a Patient Information leaflet. Do not use PREZISTA for a<br />
condition for which it was not prescribed. Do not give PREZISTA to<br />
other people even if they have the same condition you have. It may<br />
harm them.<br />
This leaflet summarizes the most important information about<br />
PREZISTA. If you would like more information, talk to your healthcare<br />
provider. You can ask your healthcare provider or pharmacist for<br />
information about PREZISTA that is written for health professionals.<br />
For more information, call 1-800-526-7736.<br />
What are the ingredients in PREZISTA?<br />
Active ingredient: darunavir<br />
Inactive ingredients:<br />
PREZISTA Oral Suspension: hydroxypropyl cellulose, microcrystalline<br />
cellulose, sodium carboxymethylcellulose, methylparaben sodium, citric<br />
acid monohydrate, sucralose, masking flavor, strawberry cream flavor,<br />
hydrochloric acid (for pH adjustment), purified water.<br />
PREZISTA 75 mg and 150 mg Tablets: colloidal silicon dioxide,<br />
crospovidone, magnesium stearate, microcrystalline cellulose. <strong>The</strong> film<br />
coating contains: OPADRY ® White (polyethylene glycol 3350, polyvinyl<br />
alcohol-partially hydrolyzed, talc, titanium dioxide).<br />
PREZISTA 400 mg and 600 mg Tablets: colloidal silicon dioxide,<br />
crospovidone, magnesium stearate, microcrystalline cellulose. <strong>The</strong> film<br />
coating contains: OPADRY ® Orange (FD&C Yellow No. 6, polyethylene<br />
glycol 3350, polyvinyl alcohol-partially hydrolyzed, talc, titanium dioxide).<br />
This Patient Information has been approved by the U.S Food and Drug<br />
Administration.<br />
Manufactured by:<br />
PREZISTA Oral Suspension<br />
Janssen Pharmaceutica, N.V.<br />
Beerse, Belgium<br />
PREZISTA Tablets<br />
Janssen Ortho LLC, Gurabo, PR 00778<br />
Manufactured for:<br />
Janssen <strong>The</strong>rapeutics, Division of Janssen Products, LP, Titusville NJ<br />
08560<br />
NORVIR ® is a registered trademark of its respective owner.<br />
PREZISTA ® is a registered trademark of Janssen Pharmaceuticals<br />
© Janssen Pharmaceuticals, Inc. 2006<br />
Revised: June 2012 986588P
5537 N. broadway st.<br />
chicago, il 60640<br />
phone: (773) 989–9400<br />
fax: (773) 989–9494<br />
email: inbox@tpan.com<br />
www.positivelyaware.com<br />
editor-iN-chief Jeff Berry<br />
associate editor Enid vázquez<br />
copy editors Sue Saltmarsh,<br />
Jason lancaster<br />
web master Joshua thorne<br />
creative director Rick guasco<br />
coNtributiNg writers<br />
keith R. green, liz highleyman,<br />
Sal Iacopelli, laura Jones,<br />
Jim pickett, Matt Sharp<br />
photographers<br />
Chris knight, Joshua thorne<br />
medical advisors<br />
Daniel S. Berger, MD<br />
gary Bucher, MD<br />
Michael Cristofano, pA<br />
Joel gallant, MD<br />
Swarup Mehta, pharmD<br />
advertisiNg iNquiries<br />
lorraine hayes<br />
l.hayes@tpan.com<br />
distributioN maNager<br />
Bradley p Mazzie<br />
distribution@tpan.com<br />
POSITIVELY AWARE<br />
IS PUBLISHED BY<br />
eXclusively oN<br />
www.positivelyaware.com<br />
Surface vs. substance<br />
A website—and app—that encourages truth in Internet dating<br />
www.positivelyaware.com/2012/12_06/mister.shtml<br />
Additional conference coverage from AIDS 2012<br />
www.positivelyaware.com/2012/12_06/aids2012.shtml<br />
follow us<br />
on FacEBook anD on<br />
TwITTER (@PoSawaRE)<br />
we read you<br />
commEnT on oUR aRTIcLES<br />
aT positivelyaware.com<br />
© 2012. positively aware (ISSN: 1523-2883) is published bi-monthly by Test Positive Aware Network<br />
(TPAN), 5537 N. Broadway St, Chicago, IL 60640. TPAN is an Illinois not-for-profit corporation, providing<br />
information and support to anyone concerned with HIV and AIDS issues. PoSITIVeLy AwAre is a registered<br />
trademark of TPAN. All rights reserved. Circulation: 100,000. For reprint permission, contact Sue Saltmarsh. Six<br />
issues mailed bulk rate for $30 donation; mailed free to those living with HIV or those unable to contribute.<br />
we accept contribution of articles covering medical or personal aspects of HIV/AIDS. we reserve the right to edit or<br />
decline submitted articles. when published, the articles become the property of TPAN and its assigns. you may use<br />
your actual name or a pseudonym for publication, but please include your name and phone number.<br />
Although PoSITIVeLy AwAre takes great care to ensure the accuracy of all the information that it presents,<br />
PoSITIVeLy AwAre staff and volunteers, TPAN, or the institutions and personnel who provide us with information<br />
cannot be held responsible for any damages, direct or consequential, that arise from use of this material or due to<br />
errors contained <strong>here</strong>in. opinions expressed in PoSITIVeLy AwAre are not necessarily those of staff or TPAN, its<br />
supporters and sponsors, or distributing agencies. Information, resources, and advertising in PoSITIVeLy AwAre<br />
do not constitute endorsement or recommendation of any medical treatment or product. TPAN recommends that<br />
all medical treatments or products be discussed thoroughly and frankly with a licensed and fully HIV-informed<br />
medical practitioner, preferably a personal physician.<br />
A model, photographer, or author’s HIV status should not be assumed based on their appearance in PoSITIVeLy<br />
AwAre, association with TPAN, or contributions to this journal.<br />
Distribution of Positively AwAre is supported in part through an unrestricted grant from viiv Healthcare.<br />
4 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
SEP+OCT 2012<br />
VoLUmE 24 nUmBER 6<br />
departmeNts<br />
6 iN boX<br />
6 readers’ poll<br />
7 editor’s Note<br />
What is a woman?<br />
13 briefly<br />
FDA approves Truvada for HIV prevention. Rapid<br />
home HIV test approved. Initial study results find<br />
dolutegravir/Epzicom is superior to Atripla.<br />
34 coNfereNce update<br />
News from the XIX International AIDS Conference in<br />
Washington, D.C.<br />
44 ask the hiv specialist<br />
Safe sex is for seniors, too.<br />
45 wholistic picture<br />
Battle of the sexes?<br />
cover features<br />
22 Securing care for HIV-positive women<br />
Challenges and solutions for women living with HIV.<br />
26 Black women, society, and HIV<br />
An expert talks about the context of infection.<br />
28 ‘Everyone needs a support system’<br />
How one therapist helps HIV-positive women learn<br />
to take care of themselves.<br />
30 Nine months to birth day<br />
HIV and pregnancy—keeping yourself and your<br />
baby healthy.<br />
feature<br />
41 <strong>The</strong> mirror has two faces<br />
A personal account of using facial filler for lipoatrophy.<br />
oN the cover aNd this page:<br />
TamaRa wILSon, HIV-PoSITIVE SIncE 1999,<br />
PHoTogRaPHED BY cHRIS knIgHT<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 5
In BOx joIn THE conVERSaTIon: iNboX@tpaN.com anD @posaware<br />
HIV testing in prison?<br />
First let me say this is<br />
strictly my opinion in<br />
answer to your reader’s<br />
poll question concerning<br />
HIV testing in prison.<br />
I believe it should be<br />
required upon entering<br />
and leaving prison.<br />
Prior to my incarceration,<br />
I worked at Prevention<br />
Point Philadelphia (a needle<br />
exchange program), the Gay<br />
& Lesbian AIDS Education<br />
Initiative, and I spoke at various events<br />
about HIV/AIDS in the prison system. I’ve<br />
been positive for 18 years and for the last<br />
11 years I’ve been trying to get as many<br />
people tested as possible.<br />
At present, I have three and a half years<br />
left on my sentence. During my incarceration,<br />
I have been a Peer Educator teaching<br />
a class called Positive Voices behind the<br />
Walls (a little plug never hurts!) and an<br />
advocate for testing. I’m open about my<br />
HIV status, so HIV can have a “face” that<br />
defies the expectations of some of the<br />
men in <strong>here</strong>.<br />
After taking my class for 16 weeks, I<br />
have seen men’s attitudes change completely<br />
because they see me living healthy,<br />
happy, with a loving family, and looking<br />
forward to a long life.<br />
So, yes, testing should be mandatory,<br />
along with education and good information<br />
about prevention.<br />
—larry<br />
wHITE DEER, PEnnSYLVanIa<br />
you’re not the only one<br />
Finally, I’ve found relief! On May 21st, I<br />
read my first ever issue of PoSITIVELY<br />
awaRE—the March+April Drug Guide.<br />
I had no idea that anyone<br />
has the same problems as<br />
me. <strong>The</strong> issue touched me<br />
deeply.<br />
Simply knowing you’re<br />
t<strong>here</strong>, that I can reach out<br />
to someone for information<br />
seems to make everything a<br />
little bit better. I’m not sure<br />
how to receive future issues,<br />
but put me on your mailing<br />
list if at all possible!<br />
—Dwayne e.<br />
FLoRIDa<br />
good wishes<br />
Comment on July+August Editor’s Note:<br />
Thank you for the uplifting article, “Wish<br />
HIV Away.” Though easier said than done, I<br />
know that I’ll be able to pick my head up in<br />
the morning and continue on with a positive<br />
outlook on the day. I’m not at the stage<br />
yet w<strong>here</strong> people can know, only because<br />
I’m just two months into this disease, but I<br />
know I will get t<strong>here</strong> (fingers crossed).<br />
—steven<br />
VIa THEBoDY.com<br />
hidden no more<br />
I have to let you guys know how much<br />
I appreciated the article, “<strong>The</strong> Hidden<br />
People,” in your January+February 2012<br />
issue. I would love to have the Muslim<br />
brothers come to Memphis to speak in the<br />
very near future. My southern hat goes off<br />
to the writer Sue Saltmarsh for the article.<br />
And love to Karim Rush, Shadeed Jenkins,<br />
and Iman Boyd.<br />
Great job, PoSITIVELY awaRE! You<br />
guys rock!<br />
—Anthony Hardaway<br />
VIa THE InTERnET<br />
dO ThE WRITE ThInG. PoSITIVELY awaRE treats all communications (letters, e-mail,<br />
etc.) as letters to the editor unless otherwise instructed. We reserve the right to edit for<br />
length, style, or clarity. Unless you tell us not to, we will use your name and city.<br />
POSITIVELY AWARE<br />
5537 n. BRoaDwaY ST.<br />
cHIcago, IL 60640<br />
inbox@tpan.com<br />
WE REAd YOu.<br />
SHaRE YoUR commEnTS<br />
aBoUT oUR aRTIcLES aT<br />
positivelyaware.com<br />
REAdERS’ POLL<br />
In THE jULY+aUgUST ISSUE, wE aSkED<br />
Before you tested hIv-positive,<br />
did you think you were at risk?<br />
yes, but i<br />
practiced<br />
safer sex.<br />
24%<br />
i didn’t<br />
think<br />
about it.<br />
16%<br />
your commeNts:<br />
“I barebacked all the way after my first<br />
encounter—I have no one to blame but<br />
myself and my lack of self-esteem.”<br />
“After I found out, I wanted to kill myself—<br />
my partner never told me he had HIV.”<br />
“Before I tested positive, I always<br />
practiced safe sex. But I also remember<br />
feeling like no matter how much of a<br />
good boy I was, HIV was going to get me.”<br />
“I practiced safer sex until depression<br />
and drugs got in my way.”<br />
“I never thought about it. I suspect I<br />
was infected in 1986. At that time, t<strong>here</strong><br />
wasn’t much information available<br />
about infection and I had no idea what<br />
behavior was risky and what wasn’t.”<br />
“I thought those who caught HIV led<br />
reckless lives, taking drugs and having<br />
many anonymous partners and<br />
unprotected sex. I was naïve to believe<br />
I would be OK if I limited myself to one<br />
casual partner every few months.”<br />
this issue’s poll questioN:<br />
Who is more stigmatized<br />
because of hIv?<br />
cast your vote at<br />
POSITIVELYAWARE.COm<br />
6 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM<br />
No.<br />
8%<br />
yes, but i<br />
didn’t care.<br />
19%<br />
yes, but i<br />
thought i was<br />
at low risk.<br />
33%
PHOTO: CHRiS KnigHT<br />
EdITOR’S nOTE<br />
jEFF BERRY<br />
@PaEDIToR<br />
What is a woman?<br />
I’VE hAd mAnY TEAChERS In LIfE, InCLudInG WOmEn<br />
who have taught me particularly important lessons about<br />
courage, strength, resilience, caring, and compassion.<br />
Cindy, the oldest of my three sisters, realized at an<br />
early age that it was her job to help look after the other<br />
four kids in the Berry clan. My sister Barb became a<br />
veterinarian, the first doctor in our family. <strong>The</strong> one who<br />
was closest to me in age, Wendy, became my best friend<br />
growing up. My mother Norma went back to work when<br />
I started preschool in the early 1960’s, and continued<br />
working as a schoolteacher and elementary school principal<br />
until she retired. And my grandmother, Ruby, lived<br />
to be 101, and would often recount to us colorful stories<br />
from her life, such as the one about traveling all day in<br />
a covered wagon to see the Wright Brothers perform<br />
breathtaking feats in their amazing flying machines.<br />
All these women and others demonstrated to me<br />
wonderful qualities that I respected and admired, and<br />
sought to emulate and incorporate into my own sense<br />
of values and ideals. T<strong>here</strong> are countless examples in<br />
our culture of strong, courageous women and their<br />
many accomplishments and contributions to the world.<br />
So why is it that so many women who are in positions<br />
of power and leadership appear threatening to so many<br />
who live in our male-dominated society?<br />
A recurring theme at this year’s International AIDS<br />
Conference was the role of women in ending the<br />
epidemic. In her address at the conference opening<br />
plenary, Secretary of State Hillary Clinton talked about<br />
the essential role of communities, especially people living<br />
with HIV, in turning the tide on the epidemic. “And it<br />
will come as no surprise to you,” Clinton told the packed<br />
audience, “that I would like to highlight the particular<br />
role that women play.”<br />
Clinton pointed out that in Sub-Saharan Africa<br />
women account for 60% of people living with HIV.<br />
“Women want to protect themselves, and they want<br />
adequate health care, and we need to answer their call,”<br />
said Clinton. “Every woman should be able to decide<br />
when and whether to have children. This is true if she is<br />
HIV-positive or not. Women need and deserve a voice in<br />
the decisions that affect their lives.”<br />
In a lively morning plenary session by a panel made<br />
up of mostly women, HIV-positive<br />
educator and activist Linda Scruggs<br />
said it best by stating she wasn’t<br />
going to ask for anything, because<br />
women have been asking to be<br />
counted in for the last two decades. “Today I stand <strong>here</strong><br />
to give you some directions. We’ve decided to stop asking,<br />
and maybe you just need the recipe.”<br />
Scruggs called for meaningful involvement of women<br />
at every level, from the government to local communities<br />
and organizations, and also made it clear that women are<br />
not just asking for male-run organizations that “tolerate” a<br />
women’s program. “We need the support and resources…<br />
to give us the power to heal our sisters, to change our<br />
men. We are the mothers of the earth.”<br />
In her talk, Scruggs also shared part of what she says<br />
got her to the stage that day. She learned she was HIVpositive<br />
while visiting a perinatal clinic and was 13-weeks<br />
pregnant, and had to decide whether to terminate the<br />
pregnancy and live five years, or have the baby and possibly<br />
live three. She says she’s glad that day the doctor<br />
was wrong, and her son, Isaiah, was born free of HIV,<br />
and he just recently turned 21.<br />
“I could’ve made the decision to have an abortion.<br />
An abortion would not have been the first one I had had,<br />
but I had an experience with God. I had an experience<br />
that…made me really look and reflect about women.<br />
After all, what is a woman who thinks she’s ugly? What<br />
is a woman who feels she has no self-value? What is a<br />
woman who allows not one, but two men to rape her in<br />
silence? What is a woman who allows an uncle to molest<br />
her and others and still be silent?... What is a woman<br />
who feels that she’s been broken and voiceless? What is<br />
a woman who’s afraid of understanding herself? What<br />
is a woman who spent a lifetime trying to be someone<br />
other than herself?<br />
“I’ll tell you, that cold November day, that woman<br />
was me, but it was through the support of this community<br />
that I was able to find a voice and a place, that<br />
I could be just who I say I am. I am a woman.”<br />
Take care of yourself, and each other.<br />
t<strong>here</strong> are<br />
countless<br />
examples in<br />
our culture of<br />
strong, courageous<br />
women<br />
and their<br />
many accomplishments<br />
and contributions<br />
to the<br />
world. so why<br />
is it that so<br />
many women<br />
who are in<br />
positions<br />
of power<br />
and leadership<br />
appear<br />
threatening<br />
to so many<br />
who live in<br />
our maledominated<br />
society?<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 7
Please turn past this page; it has intentionally been left blank.➤<br />
POSITIVELY AWARE
Please turn past this page; it has intentionally been left blank.➤<br />
POSITIVELY AWARE
Please turn past this page; it has intentionally been left blank.➤<br />
POSITIVELY AWARE
Please turn past this page; it has intentionally been left blank.➤<br />
POSITIVELY AWARE
Please turn past this page; it has intentionally been left blank.➤<br />
POSITIVELY AWARE
PHOTO: JOSHuA THORnE<br />
BRIEFLY<br />
EnID VázqUEz<br />
FDA approves Truvada for PrEP<br />
<strong>The</strong> Food and Drug Administration (FDA)<br />
in July approved truvada as the first<br />
medication to help prevent Hiv infection.<br />
As expected, the approval came<br />
with restrictions.<br />
Truvada, a combination of tenofovir<br />
(Viread) and emtricitabine (Emtriva), is<br />
one of the most prescribed medications<br />
for HIV in this country. For HIV prevention,<br />
the use of Truvada is called “PrEP,”<br />
for “pre-exposure prophylaxis.”<br />
“[We] commend the FDA’s approval of<br />
[Truvada] for the use of [PrEP] to prevent<br />
HIV transmission. This approach can<br />
prevent many new infections and could<br />
dramatically impact HIV transmission<br />
worldwide,” said Kenneth H. Mayer, MD,<br />
Medical Research Director and Co-chair<br />
of <strong>The</strong> Fenway Institute at Fenway Health.<br />
“My colleagues and I are delighted to have<br />
helped to demonstrate the utility of this<br />
promising approach for HIV prevention.”<br />
David Ernesto Munar, President/CEO<br />
of the AIDS Foundation of Chicago, said,<br />
“Our challenge now is to implement PrEP<br />
as strategically as possible, and to ensure<br />
the people who need it most, those who<br />
are most at risk for HIV, have access.”<br />
“This is an enormous turning point, a<br />
real game changer, in the fight against<br />
HIV,” said Jim Pickett, AFC’s Director<br />
of Prevention Advocacy and Gay Men’s<br />
Health. “<strong>The</strong> toolbox we have now has<br />
Truvada as PrEP. We can look forward to<br />
more sex acts being protected, especially<br />
among individuals who have already<br />
chosen, for whatever reason, to not use<br />
condoms consistently.”<br />
According to a press release from the<br />
FDA, “Truvada is to be used for [PrEP] in<br />
combination with safer sex practices to<br />
prevent sexually-acquired HIV infection in<br />
adults at high risk.”<br />
<strong>The</strong> FDA said Truvada for PrEP should<br />
be used as part of a comprehensive<br />
HIV prevention plan that includes risk<br />
reduction counseling, consistent and<br />
correct condom use, regular HIV testing,<br />
and screening for and treatment of other<br />
sexually-transmitted infections, stating<br />
that “Truvada is not a substitute for safer<br />
sex practices.”<br />
Truvada now carries a Boxed Warning<br />
on its drug label alerting health care<br />
professionals and uninfected individuals<br />
that Truvada for PrEP must only be used<br />
by people confirmed to be HIV-negative<br />
before being prescribed the drug and<br />
tested at least every three months during<br />
use to reduce the risk of developing<br />
drug resistance. Both the antiviral and the<br />
PrEP dose is one pill taken once daily.<br />
Truvada maker Gilead Sciences worked<br />
with the FDA to create a Risk Evaluation<br />
and Mitigation Strategy (REMS) for<br />
Truvada PrEP. <strong>The</strong> REMS focuses on a prescriber<br />
training and education program<br />
in counseling and managing individuals<br />
who are taking or considering Truvada for<br />
PrEP. <strong>The</strong> REMS looks at the elements of<br />
a comprehensive HIV prevention strategy,<br />
the importance of adhering to the recommended<br />
daily dosing regimen, and the<br />
serious risks of taking Truvada for PrEP if<br />
already infected with HIV or of becoming<br />
infected while taking it.<br />
According to the press release,<br />
“Truvada’s safety and efficacy for PrEP<br />
were demonstrated in two large, randomized,<br />
double-blind, placebo-controlled<br />
clinical trials. <strong>The</strong> iPrEx trial evaluated<br />
Truvada in 2,499 HIV-negative men<br />
or transgender women who have sex<br />
with men and with evidence of high<br />
risk behavior for HIV infection... Results<br />
showed Truvada was effective in reducing<br />
the risk of HIV infection by 42% compared<br />
with placebo in this population.<br />
Efficacy was strongly correlated with<br />
drug ad<strong>here</strong>nce in this trial.”<br />
It was also shown in iPrEX that t<strong>here</strong><br />
was a 92% reduction of risk for HIV in<br />
participants who<br />
took Truvada in the<br />
prescribed oncedaily<br />
dose.<br />
“<strong>The</strong> Partners<br />
PrEP trial was conducted<br />
in 4,758 heterosexual couples,<br />
w<strong>here</strong> one partner was HIV-infected and<br />
the other was not (serodiscordant couples),”<br />
the press release continued. “<strong>The</strong><br />
trial evaluated the efficacy and safety of<br />
[both] Truvada and [Viread] tenofovir<br />
versus placebo in preventing HIV infection<br />
in the uninfected male or female partner.<br />
Results showed Truvada reduced the risk<br />
of becoming infected by 75% compared<br />
with placebo.<br />
“No new side effects were identified<br />
in the clinical trials evaluating Truvada<br />
for the PrEP indication. <strong>The</strong> most common<br />
side effects reported with Truvada<br />
include diarrhea, nausea, abdominal<br />
pain, headache, and weight loss. Serious<br />
adverse events in general, as well as<br />
those specifically related to kidney or<br />
bone toxicity, were uncommon.”<br />
As a condition of approval, Gilead<br />
Sciences is required to collect and<br />
analyze samples from individuals who<br />
become infected with HIV while taking<br />
Truvada to see if they’ve developed drug<br />
resistance. <strong>The</strong> company is also required<br />
to collect data on women who become<br />
pregnant while taking Truvada for PrEP<br />
and to conduct other research.<br />
“Today’s decision is the culmination<br />
of almost 20 years of research involving<br />
investigators, academic and medical<br />
institutions, funding agencies, and nearly<br />
20,000 trial participants around the<br />
world, and Gilead is proud to have been<br />
a partner in this effort,” said Norbert<br />
Bischofberger, PhD, Executive Vice<br />
President, Research and Development<br />
and Chief Scientific Officer, Gilead<br />
Sciences. >><br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 13
BRIEFLY<br />
EnID VázqUEz<br />
Moises Agosto<br />
>> the following is from a statement<br />
from Moises Agosto, Director of<br />
treatment education, Ad<strong>here</strong>nce, and<br />
Mobilization for the National Minority<br />
AiDs Council (NMAC):<br />
“While PrEP shows substantial promise as<br />
a supplement to current HIV prevention<br />
efforts, it is by no means a panacea and<br />
is only effective when used in conjunction<br />
with traditional prevention and risk reduction<br />
strategies, such as condom usage.<br />
“Anti-retroviral medications, like<br />
Truvada, are extremely powerful drugs<br />
with the potential for serious side<br />
effects. As such, PrEP should only be<br />
used by individuals who are highly vulnerable<br />
to HIV infection, including those<br />
in sero-discordant couples, sex workers,<br />
and gay men. Its efficacy is also directly<br />
related to an individual’s ad<strong>here</strong>nce to<br />
a regimen, and should only be used by<br />
those who can commit to taking it regularly.<br />
Finally, use of PrEP by individuals<br />
who may already be HIV-positive could<br />
increase the risk of drug resistance.<br />
“In recent years, t<strong>here</strong> have been a<br />
number of promising developments in<br />
biomedical interventions—from treatment<br />
as prevention and pre-exposure<br />
prophylaxis to microbicides and vaccine<br />
research. <strong>The</strong>se advances have resulted<br />
in the greatest expansion of HIV prevention<br />
tools than at any other time in the<br />
history of this epidemic. Coupled with the<br />
reforms included in the Patient Protection<br />
and Affordable Care Act, as well as the<br />
National HIV/AIDS Strategy, we are in a<br />
position for the first time in over three<br />
decades to finally end this epidemic.<br />
Today’s decision is another important<br />
step in realizing that goal.”<br />
Dolutegravir/Epzicom<br />
superior to Atripla?<br />
Shionogi-ViiV Healthcare LLC announced<br />
that initial results from its Phase 3 study<br />
SINGLE (ING114467) show superiority of<br />
its investigational HIV medication dolutegravir<br />
plus Epzicom over Atripla, one of<br />
the most widely prescribed antiviral medications<br />
in the country. At 48 weeks, 88%<br />
of study participants on the dolutegravir<br />
regimen achieved undetectable viral<br />
load (less than 50 copies/mL) vs. 81% of<br />
those on Atripla, a statistically significant<br />
difference. <strong>The</strong> company said the difference<br />
was primarily driven by a higher<br />
rate of discontinuation due to adverse<br />
events in the Atripla arm. All individuals<br />
in the study were taking antiviral therapy<br />
for the first time, a group that does the<br />
best in HIV treatment. T<strong>here</strong> were 414<br />
individuals put on dolutegravir and 419<br />
put on Atripla. Overall, 2% of those on the<br />
dolutegravir-based regimen discontinued<br />
due to adverse events vs. 10% of those<br />
receiving the Atripla regimen. <strong>The</strong> most<br />
common adverse events while on Atripla<br />
were neurological (reported by 41% of<br />
Atripla recipients vs. 15% of participants<br />
receiving the dolutegravir), while the<br />
most common drug-related adverse<br />
events with dolutegravir were in the gastrointestinal<br />
system (reported by 22% of<br />
people on dolutegravir vs. 22% of those<br />
given Atripla).<br />
Dolutegravir is an investigational<br />
integrase inhibitor (INSTI), the same class<br />
as Isentress, the only INSTI currently on<br />
the market.<br />
Rapid home<br />
HIV test approved<br />
In June, the Food and Drug<br />
Administration (FDA) approved the<br />
oraQuick in-Home Hiv test, an Hiv<br />
self-test kit that does not require sending<br />
a sample to a laboratory for analysis. <strong>The</strong><br />
kit, which tests a swab from your mouth,<br />
is approved for sale in stores and online<br />
to anyone age 17 and older. (Although<br />
HIV is not found in saliva, evidence of<br />
exposure to the virus—called HIV antibodies—is<br />
found in the mouth and indicates<br />
infection.) A positive result at home<br />
must then be followed up with a confirmatory<br />
blood test from a laboratory.<br />
<strong>The</strong> FDA said the test can be falsely<br />
negative for reasons that include the<br />
occurrence of HIV infection within three<br />
months before testing. People who<br />
engage in behaviors that put them at<br />
increased risk of getting HIV—including<br />
having unprotected sex with new partners,<br />
or injecting illegal drugs—should be<br />
re-tested on a regular basis. <strong>The</strong>y should<br />
not interpret a negative test to indicate<br />
that engaging in high risk behavior is<br />
safe.<br />
14 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
FRom THE wEEkLY E-nEwS<br />
Website offers<br />
access to HIV meds<br />
for uninsured<br />
HarborPath, a new non-profit organization,<br />
has been established to create a<br />
program that offers a single place w<strong>here</strong><br />
uninsured Hiv-positive people who<br />
otherwise qualify for manufacturersponsored<br />
patient assistance programs<br />
(PAPs) can apply for and receive their<br />
medications. <strong>The</strong> “one stop shop” portal<br />
will provide a streamlined, online process<br />
to qualify individuals and deliver the<br />
donated medications through a mailorder<br />
pharmacy. HarborPath will pilot the<br />
program in states with high need, including<br />
Alabama, Texas, and Virginia.<br />
To create the portal, HarborPath<br />
worked closely with the National Alliance<br />
of State and Territorial AIDS Directors<br />
(NASTAD) and the Clinton Health Access<br />
Initiative (CHAI), which provided the seed<br />
funding for the organization. On World<br />
AIDS Day 2011, President Bill Clinton noted<br />
the need to fight HIV/AIDS in the U.S.<br />
“I am proud that my foundation is<br />
partnering with NASTAD and other<br />
pharmaceutical manufacturers to make<br />
sure Americans living with HIV have<br />
access to the life-saving medications<br />
they need,” said President Clinton. “This<br />
E-NEWS |<br />
is an important step forward in our fight<br />
against the disease.”<br />
ViiV Healthcare is the first pharmaceutical<br />
company to support the program<br />
with HIV/AIDS medications and funding.<br />
<strong>The</strong> goal of HarborPath is to get all<br />
HIV/AIDS medications into the program<br />
and serve uninsured individuals with:<br />
n An easy-to-use website with a single<br />
portal to determine eligibility for the<br />
program and to fill prescriptions for<br />
participating companies’ HIV/AIDS<br />
medications.<br />
n Automatic notifications for both the<br />
individual and the case manager of<br />
qualification for the program.<br />
n A pharmacy that ships a 3-month supply<br />
of all participating medications in<br />
one package within two business days<br />
of final approval and confirms delivery<br />
of the medications.<br />
n Renewal reminders to individuals and<br />
case managers to improve medication<br />
ad<strong>here</strong>nce.<br />
n A fully automated portal that case<br />
managers can access at any time<br />
for up-to-the-minute status of an<br />
individual’s application or shipment. If<br />
needed, live support is also available<br />
through a toll-free call center.<br />
Murray Penner, Deputy Executive<br />
Director at NASTAD, said, “Under the current<br />
PAP process, an individual or their<br />
case manager has to apply<br />
separately to each company’s<br />
program for these<br />
medications, which can be<br />
complex and time-consuming.<br />
Missing doses or failing<br />
to fill prescriptions because<br />
of complications sometimes<br />
associated with these processes<br />
may result in serious<br />
health consequences, or<br />
even death, in addition to<br />
increased transmission of<br />
the virus. HarborPath is<br />
designed to address this<br />
urgent need in the U.S.”<br />
Sign up for the weekly email newSletter of<br />
poSitively aware. go to positivelyaware.com<br />
Studies find<br />
once-daily ‘Quad’<br />
is safe and effective<br />
<strong>The</strong> findings of two large international<br />
randomized studies published in <strong>The</strong><br />
Lancet medical journal indicate that the<br />
new once-daily pill combining three<br />
antiretrovirals and a booster molecule is<br />
a safe and effective alternative to two<br />
widely used drug regimens for newly<br />
diagnosed Hiv-positive adults who have<br />
had no previous treatment. <strong>The</strong> study<br />
results also indicate that the new “Quad”<br />
pill is faster acting, doesn’t have the neuropsychiatric<br />
side effects associated with<br />
other combinations, and could improve<br />
compliance with treatment.<br />
“Patient ad<strong>here</strong>nce to medication is<br />
vital, especially for patients with HIV,<br />
w<strong>here</strong> missed doses can quickly lead to<br />
the virus becoming resistant to medication.<br />
Older HIV treatment regimens<br />
involve taking several pills multiple times<br />
a day,” explains Paul Sax from Brigham<br />
and Women’s Hospital, Harvard Medical<br />
School, lead author of the first study.<br />
“Our results provide an additional highly<br />
potent, well-tolerated treatment option,<br />
and highlight the simplicity of treatment<br />
resulting from combining several antiretrovirals<br />
in a single pill. Studies have<br />
shown that single pill treatments improve<br />
both ad<strong>here</strong>nce and patient satisfaction,<br />
and help prevent prescription errors,<br />
t<strong>here</strong>by reducing the likelihood of treatment<br />
failure and drug resistance.”<br />
<strong>The</strong> first study randomly assigned<br />
700 patients from centers across North<br />
America to start treatment with two<br />
different single tablet regimens—either<br />
the Quad, combining the new integrase<br />
inhibitor elvitegravir (EVG) boosted with<br />
cobicistat (a new pharmacoenhancer;<br />
COBI) plus emtricitabine/tenofovir<br />
(Emtriva/Viread), or Atripla (efavirenz/<br />
emtricitabine/tenofovir), the current gold<br />
standard regimen approved by the FDA<br />
in 2006.<br />
After 48 weeks of treatment, 88% >><br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 15
BRIEFLY<br />
EnID VázqUEz<br />
of patients given the Quad had suppressed<br />
viral loads (less than 50 copies/<br />
mL), compared with 84% in the Atripla<br />
group.<br />
Adverse events that led to patients<br />
discontinuing treatment were infrequent<br />
and similar in both groups. Mild nausea<br />
was more common with the Quad, but<br />
patients were less likely to have dizziness,<br />
abnormal dreams, insomnia, and rash<br />
compared with the Atripla regimen.<br />
<strong>The</strong> second trial included 708<br />
treatment-naïve adults from 146 medical<br />
centers across Australia, Europe, North<br />
America, and Thailand. Patients were<br />
randomly assigned to receive a once-daily<br />
Quad or a popular and recommended<br />
twice-daily combination of Norvirboosted<br />
Reyataz (atazanavir/ritonavir)<br />
plus Truvada (emtricitabine/tenofovir).<br />
<strong>The</strong> primary endpoint, to achieve viral<br />
levels below 50 copies/mL by week 48,<br />
was reached by 90% of people in the<br />
Quad group compared with 87% in the<br />
atazanavir/ritonavir/emtricitabine/tenofovir<br />
group.<br />
<strong>The</strong> safety of the two regimens was<br />
also similar.<br />
PA’s editor debuts<br />
blog on HuffPo<br />
PoSITIVELY awaRE editor Jeff Berry has<br />
joined other AIDS activists and journalists<br />
such as <strong>The</strong> <strong>Body</strong>’s Kellee Turrell, the AIDS<br />
Foundation of Chicago’s David Ernesto<br />
Munar, and others in becoming a blogger<br />
published by the Huffington Post.<br />
In advance of the upcoming AIDS 2012<br />
World AIDS Conference, Berry wrote<br />
“Reflections from an Epidemic: Carrying<br />
the Torch to AIDS 2012.” In it, he talks<br />
about the significance of this being the<br />
Simplify your life.<br />
first conference to be held in the U.S.<br />
since President Obama lifted the travel<br />
ban on HIV-positive people, his anticipation<br />
of such events as displays of the<br />
AIDS Memorial Quilt, a planned march<br />
and demonstration, the performance<br />
of the Tony Award-winning play <strong>The</strong><br />
Normal Heart, as well as the many global<br />
leaders in AIDS policy, advocacy, and<br />
treatment advances that presented at the<br />
conference.<br />
Did he get infected?<br />
In the July+August issue of PoSITIVELY<br />
awaRE, a young man in Chicago, Chris,<br />
was anxiously awaiting the results of his<br />
HIV tests following a potential exposure<br />
through sex (“PrEPing,” July+August).<br />
Two months later, he remains<br />
HIV-negative.<br />
Turn your assorted prescription medicine bottles into single-dose packs.<br />
Easy to remember. Easy to take. Each pack contains all the pills of a single dose.<br />
Free FedEx shipping anyw<strong>here</strong> in the continental U.S.<br />
J Discount Pharmacy<br />
Call to plaCE yoUr FirSt ordEr:<br />
(773) 278-5337<br />
16 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
PHOTO: MATTHEw gARSTECK<br />
TPan, publisher of PoSITIVELY awaRE, is commemorating<br />
25 years of service to chicago’s HIV community.<br />
JoiN Jamar rogers, of Nbc’s “the voice,” for a special performaNce.<br />
OCTOBER 4, 2012<br />
5:30–8:30 Pm | cHIcago cULTURaL cEnTER<br />
TIckETS aVaILaBLE aT www.tpan.com<br />
EVEnT SPOnSORS<br />
$100,000 anD aBoVE<br />
alphawood Foundation<br />
Bristol-myers Squibb<br />
$25,000 anD aBoVE<br />
abbott Virology<br />
EmD Serono<br />
Lloyd a. Fry Foundation<br />
ViiV Healthcare<br />
walgreens<br />
AnnIVERSARY PARTnERS<br />
$50,000 anD aBoVE<br />
janssen <strong>The</strong>rapeutics<br />
$10,000 anD aBoVE<br />
aIDS Foundation of chicago<br />
Blue cross and Blue Shield<br />
of Illinois<br />
cheetah gyms<br />
gilead Sciences, Inc.<br />
macy’s<br />
millercoors<br />
Steamworks
INDICATION<br />
COMPLERA ® (emtricitabine 200 mg/rilpivirine 25 mg/tenofovir disoproxil fumarate<br />
300 mg) is a prescription HIV medicine that contains 3 medicines, EMTRIVA ®<br />
(emtricitabine), EDURANT (rilpivirine), and VIREAD ® (tenofovir disoproxil fumarate)<br />
combined in one pill. COMPLERA is used as a complete single-tablet regimen to treat<br />
HIV-1 infection in adults (age 18 and older) who have never taken HIV medicines before.<br />
COMPLERA does not cure HIV and has not been shown to prevent passing HIV<br />
to others. It is important to always practice safer sex, use latex or polyurethane<br />
condoms to lower the chance of sexual contact with any body fl uids, and to never<br />
re-use or share needles. Do not stop taking COMPLERA unless directed by your<br />
healthcare provider. See your healthcare provider regularly.<br />
IMPORTANT SAFETY INFORMATION<br />
Contact your healthcare provider right away if you get the following side effects<br />
or conditions while taking COMPLERA:<br />
• Nausea, vomiting, unusual muscle pain, and/or weakness. <strong>The</strong>se may be<br />
signs of a buildup of acid in the blood (lactic acidosis), which is a serious<br />
medical condition<br />
• Light-colored stools, dark-colored urine, and/or if your skin or the whites of your<br />
eyes turn yellow. <strong>The</strong>se may be signs of serious liver problems (hepatotoxicity),<br />
with liver enlargement (hepatomegaly), and fat in the liver (steatosis)<br />
• If you have HIV-1 and hepatitis B virus (HBV), your liver disease may suddenly<br />
get worse if you stop taking COMPLERA. Do not stop taking COMPLERA without<br />
fi rst talking to your healthcare provider. Your healthcare provider will monitor<br />
your condition<br />
COMPLERA may affect the way other medicines work, and other medicines may<br />
affect how COMPLERA works, and may cause serious side effects.<br />
COMPLERA (emtricitabine/rilpivirine/tenofovir disoproxil<br />
fumarate) is a prescription medicine used as a complete<br />
single-tablet regimen to treat HIV-1 in adults who have<br />
never taken HIV medicines before. COMPLERA does not<br />
cure HIV or AIDS or help prevent passing HIV to others.<br />
one<br />
<strong>The</strong> for me<br />
Patient model. Pill shown is not actual size.<br />
Do not take COMPLERA if you are taking the following medicines:<br />
• other HIV medicines (COMPLERA provides a complete treatment for HIV infection.)<br />
• the anti-seizure medicines carbamazepine (Carbatrol ® , Equetro ® , Tegretol ® ,<br />
Tegretol-XR ® , Teril ® , Epitol ® ), oxcarbazepine (Trileptal ® ), phenobarbital (Luminal ® ),<br />
phenytoin (Dilantin ® , Dilantin-125 ® , Phenytek ® )<br />
• the anti-tuberculosis medicines rifabutin (Mycobutin), rifampin (Rifater ® ,<br />
Rifamate ® , Rimactane ® , Rifadin ® ) and rifapentine (Priftin ® )<br />
• a proton pump inhibitor medicine for certain stomach or intestinal problems,<br />
including esomeprazole (Nexium ® , Vimovo ® ), lansoprazole (Prevacid ® ),<br />
omeprazole (Prilosec ® ), pantoprazole sodium (Protonix ® ), rabeprazole (Aciphex ® )<br />
• more than 1 dose of the steroid medicine dexamethasone or dexamethasone<br />
sodium phosphate<br />
• St. John’s wort (Hypericum perforatum)<br />
• other medicines that contain tenofovir (VIREAD ® , TRUVADA ® , ATRIPLA ® )<br />
• other medicines that contain emtricitabine or lamivudine (EMTRIVA ® , Combivir ® ,<br />
Epivir ® or Epivir-HBV ® , Epzicom ® , Trizivir ® )<br />
• rilpivirine (Edurant )<br />
• adefovir (HEPSERA ® )<br />
In addition, also tell your healthcare provider if you take:<br />
• an antacid medicine that contains aluminum, magnesium hydroxide, or calcium<br />
carbonate. Take antacids at least 2 hours before or at least 4 hours after you<br />
take COMPLERA<br />
• a histamine-2 blocker medicine, including famotidine (Pepcid ® ), cimetidine<br />
(Tagamet ® ), nizatidine (Axid ® ), or ranitidine hydrochloride (Zantac ® ). Take these<br />
medicines at least 12 hours before or at least 4 hours after you take COMPLERA<br />
• the antibiotic medicines clarithromycin (Biaxin ® ), erythromycin (E-Mycin ® , Eryc ® ,<br />
Ery-Tab ® , PCE ® , Pediazole ® , Ilosone ® ), and troleandomycin (TAO ® )<br />
• an antifungal medicine by mouth, including fl uconazole (Difl ucan ® ), itraconazole<br />
(Sporanox ® ), ketoconazole (Nizoral ® ), posaconazole (Noxafi l ® ), voriconazole (Vfend ® )<br />
• methadone (Dolophine ® )<br />
This list of medicines is not complete. Discuss with your healthcare provider all<br />
prescription and nonprescription medicines, vitamins, or herbal supplements you<br />
are taking or plan to take.
Save up to<br />
$200<br />
per month<br />
Before taking COMPLERA, tell your healthcare provider if you:<br />
• have liver problems, including hepatitis B or C virus infection<br />
• have kidney problems<br />
• have ever had a mental health problem<br />
• have bone problems<br />
• are pregnant or plan to become pregnant. It is not known if COMPLERA can harm<br />
your unborn child<br />
• are breastfeeding; women with HIV should not breast-feed because they can pass<br />
HIV through their milk to the baby<br />
Contact your healthcare provider right away if you experience any of the<br />
following serious or common side effects:<br />
Serious side effects associated with COMPLERA:<br />
• New or worse kidney problems can happen in some people who take COMPLERA.<br />
If you have had kidney problems in the past or take other medicines that can cause<br />
kidney problems, your healthcare provider may need to do blood tests to check your<br />
kidneys during your treatment with COMPLERA<br />
• Depression or mood changes can happen in some people who take COMPLERA.<br />
Tell your healthcare provider right away if you have any of the following symptoms:<br />
feeling sad or hopeless, feeling anxious or restless, or if you have thoughts of<br />
hurting yourself (suicide) or have tried to hurt yourself<br />
• Bone problems can happen in some people who take COMPLERA. Bone problems<br />
include bone pain, softening or thinning (which may lead to fractures). Your<br />
healthcare provider may need to do additional tests to check your bones<br />
• Changes in body fat can happen in people taking HIV medicine. <strong>The</strong>se changes<br />
may include increased amount of fat in the upper back and neck (“buffalo hump”),<br />
breast, and around the main part of your body (trunk). Loss of fat from the legs,<br />
arms and face may also happen. <strong>The</strong> cause and long-term health effect of these<br />
conditions are not known<br />
• Changes in your immune system (Immune Reconstitution Syndrome) can happen<br />
when you start taking HIV medicines. Your immune system may get stronger and<br />
begin to fi ght infections that have been hidden in your body for a long time. Tell<br />
your healthcare provider if you start having new symptoms after starting your<br />
HIV medicine<br />
You may be able to save on the co-pay for<br />
your COMPLERA prescription with a Gilead<br />
HIV Co-pay Assistance Card.<br />
Call 1-877-505-6986 for more information<br />
or visit www.COMPLERA.com.*<br />
COMPLERA. A complete HIV treatment in only 1 pill a day.<br />
Ask your healthcare provider if it’s the one for you.<br />
Common side effects associated with COMPLERA:<br />
• trouble sleeping (insomnia), abnormal dreams, headache, dizziness, diarrhea,<br />
nausea, rash, tiredness, and depression<br />
Other side effects associated with COMPLERA:<br />
• vomiting, stomach pain or discomfort, skin discoloration (small spots or freckles),<br />
and pain<br />
Tell your healthcare provider if you have any side effect that bothers you or that<br />
does not go away. <strong>The</strong>se are not all the possible side effects of COMPLERA. For more<br />
information, ask your healthcare provider or pharmacist. Call your healthcare provider<br />
for medical advice about side effects.<br />
You are encouraged to report negative side effects of prescription drugs to the<br />
FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.<br />
Take COMPLERA exactly as your healthcare provider tells you to take it<br />
• Always take COMPLERA with a meal. Taking COMPLERA with a meal is important to<br />
help get the right amount of medicine in your body. A protein drink does not replace<br />
a meal<br />
• Stay under the care of your healthcare provider during treatment with<br />
COMPLERA and see your healthcare provider regularly<br />
Please see Patient Information for COMPLERA on the following pages.<br />
* <strong>The</strong> co-pay program covers up to $200 per month for 1 year from card activation or until the<br />
card expires, up to $2400 in a calendar year. <strong>The</strong> program is subject to change or cancellation<br />
at any time.<br />
Learn more at www.COMPLERA.com
FDA-Approved Patient Labeling<br />
Patient Information<br />
COMPLERA ® (kom-PLEH-rah)<br />
(emtricitabine, rilpivirine and tenofovir disoproxil fumarate) Tablets<br />
Important: Ask your doctor or pharmacist about medicines that should not be<br />
taken with COMPLERA. For more information, see the section “What should I tell my<br />
healthcare provider before taking COMPLERA?”<br />
Read this Patient Information before you start taking COMPLERA and each time you<br />
get a refill. T<strong>here</strong> may be new information. This information does not take the place of<br />
talking to your healthcare provider about your medical condition or treatment.<br />
What is the most important information I should know about COMPLERA?<br />
COMPLERA can cause serious side effects, including:<br />
1. Build-up of an acid in your blood (lactic acidosis). Lactic acidosis can happen in<br />
some people who take COMPLERA or similar (nucleoside analogs) medicines. Lactic<br />
acidosis is a serious medical emergency that can lead to death.<br />
Lactic acidosis can be hard to identify early, because the symptoms could seem like<br />
symptoms of other health problems. Call your healthcare provider right away if you<br />
get any of the following symptoms which could be signs of lactic acidosis:<br />
• feeling very weak or tired<br />
• have unusual (not normal) muscle pain<br />
• have trouble breathing<br />
• have stomach pain with<br />
- nausea (feel sick to your stomach)<br />
- vomiting<br />
• feel cold, especially in your arms and legs<br />
• feel dizzy or lightheaded<br />
• have a fast or irregular heartbeat<br />
2. Severe liver problems. Severe liver problems can happen in people who take<br />
COMPLERA or similar medicines. In some cases these liver problems can lead to death.<br />
Your liver may become large (hepatomegaly) and you may develop fat in your liver<br />
(steatosis) when you take COMPLERA.<br />
Call your healthcare provider right away if you have any of the following symptoms<br />
of liver problems:<br />
• your skin or the white part of your eyes turns yellow (jaundice).<br />
• dark “tea-colored” urine<br />
• light-colored bowel movements (stools)<br />
• loss of appetite for several days or longer<br />
• nausea<br />
• stomach pain<br />
You may be more likely to get lactic acidosis or severe liver problems if you are<br />
female, very overweight (obese), or have been taking COMPLERA or a similar<br />
medicine containing nucleoside analogs for a long time.<br />
3. Worsening of Hepatitis B infection. If you also have hepatitis B virus (HBV) infection<br />
and you stop taking COMPLERA, your HBV infection may become worse (flare-up). A<br />
“flare-up” is when your HBV infection suddenly returns in a worse way than before.<br />
COMPLERA is not approved for the treatment of HBV, so you must discuss your HBV<br />
therapy with your healthcare provider.<br />
• Do not let your COMPLERA run out. Refill your prescription or talk to your healthcare<br />
provider before your COMPLERA is all gone.<br />
• Do not stop taking COMPLERA without first talking to your healthcare provider.<br />
• If you stop taking COMPLERA, your healthcare provider will need to check your health<br />
often and do regular blood tests to check your HBV infection. Tell your healthcare<br />
provider about any new or unusual symptoms you may have after you stop taking<br />
COMPLERA.<br />
What is COMPLERA?<br />
COMPLERA is a prescription HIV (Human Immunodeficiency Virus) medicine that:<br />
• is used to treat HIV-1 in adults who have never taken HIV medicines before. HIV is the<br />
virus that causes AIDS (Acquired Immunodeficiency Syndrome).<br />
• contains 3 medicines, (rilpivirine, emtricitabine, tenofovir disoproxil fumarate)<br />
combined in one tablet. EMTRIVA and VIREAD are HIV-1 (human immunodeficiency<br />
virus) nucleoside analog reverse transcriptase inhibitors (NRTIs) and EDURANT is an<br />
HIV-1 non-nucleoside analog reverse transcriptase inhibitor (NNRTI).<br />
It is not known if COMPLERA is safe and effective in children under the age of 18 years.<br />
COMPLERA may help:<br />
• Reduce the amount of HIV in your blood. This is called your “viral load”.<br />
• Increase the number of white blood <strong>cells</strong> called CD4+ (T) <strong>cells</strong> that help fight off<br />
other infections.<br />
Reducing the amount of HIV and increasing the CD4+ (T) cell count may improve your<br />
immune system. This may reduce your risk of death or infections that can happen when<br />
your immune system is weak (opportunistic infections).<br />
COMPLERA does not cure HIV infections or AIDS.<br />
• Always practice safer sex.<br />
• Use latex or polyurethane condoms to lower the chance of sexual contact with any<br />
body fluids such as semen, vaginal secretions, or blood.<br />
• Never re-use or share needles.<br />
Ask your healthcare provider if you have any questions about how to prevent passing<br />
HIV to other people.<br />
Who should not take COMPLERA?<br />
• Do not take COMPLERA if your HIV infection has been previously treated with<br />
HIV medicines.<br />
• Do not take COMPLERA if you are taking certain other medicines. For more<br />
information about medicines that must not be taken with COMPLERA, see “What<br />
should I tell my healthcare provider before taking COMPLERA?”<br />
What should I tell my healthcare provider before taking COMPLERA?<br />
Before you take COMPLERA, tell your healthcare provider if you:<br />
• have liver problems, including hepatitis B or C virus infection<br />
• have kidney problems<br />
• have ever had a mental health problem<br />
• have bone problems<br />
• are pregnant or plan to become pregnant. It is not known if COMPLERA can harm<br />
your unborn child<br />
Pregnancy Registry. T<strong>here</strong> is a pregnancy registry for women who take antiviral<br />
medicines during pregnancy. Its purpose is to collect information about the health<br />
of you and your baby. Talk to your healthcare provider about how you can take part<br />
in this registry.<br />
• are breast-feeding or plan to breast-feed. <strong>The</strong> Centers for Disease Control and<br />
Prevention recommends that mothers with HIV not breastfeed because they can pass<br />
the HIV through their milk to the baby. It is not known if COMPLERA can pass through<br />
your breast milk and harm your baby. Talk to your healthcare provider about the best<br />
way to feed your baby.<br />
Tell your healthcare provider about all the medicines you take, including prescription<br />
and nonprescription medicines, vitamins, and herbal supplements.<br />
COMPLERA may affect the way other medicines work, and other medicines may<br />
affect how COMPLERA works, and may cause serious side effects. If you take certain<br />
medicines with COMPLERA, the amount of COMPLERA in your body may be too low and<br />
it may not work to help control your HIV infection. <strong>The</strong> HIV virus in your body may become<br />
resistant to COMPLERA or other HIV medicines that are like it.<br />
Do not take COMPLERA if you also take these medicines:<br />
• COMPLERA provides a complete treatment for HIV infection. Do not take other HIV<br />
medicines with COMPLERA.<br />
• the anti-seizure medicines carbamazepine (CARBATROL ® , EQUETRO ® , TEGRETOL ® ,<br />
TEGRETOL-XR ® , TERIL ® , EPITOL ® ), oxcarbazepine (TRILEPTAL ® ), phenobarbital<br />
(LUMINAL ® ), phenytoin (DILANTIN ® , DILANTIN-125 ® , PHENYTEK ® )<br />
• the anti-tuberculosis medicines rifabutin (MYCOBUTIN ® ), rifampin (RIFATER ® ,<br />
RIFAMATE ® , RIMACTANE ® , RIFADIN ® ) and rifapentine (PRIFTIN ® )<br />
• a proton pump inhibitor medicine for certain stomach or intestinal problems,<br />
including esomeprazole (NEXIUM ® , VIMOVO ® ), lansoprazole (PREVACID ® ), omeprazole<br />
(PRILOSEC ® ), pantoprazole sodium (PROTONIX ® ), rabeprazole (ACIPHEX ® )<br />
• more than 1 dose of the steroid medicine dexamethasone or dexamethasone sodium<br />
phosphate<br />
• St. John’s wort (Hypericum perforatum)<br />
If you are taking COMPLERA, you should not take:<br />
• other medicines that contain tenofovir (VIREAD ® , TRUVADA ® , ATRIPLA ® )<br />
• other medicines that contain emtricitabine or lamivudine (EMTRIVA ® , COMBIVIR ® ,<br />
EPIVIR ® or EPIVIR-HBV ® , EPZICOM ® , TRIZIVIR ® )<br />
• rilpivirine (EDURANT )<br />
• adefovir (HEPSERA ® )
Also tell your healthcare provider if you take:<br />
• an antacid medicine that contains aluminum, magnesium hydroxide, or calcium<br />
carbonate. Take antacids at least 2 hours before or at least 4 hours after you take<br />
COMPLERA.<br />
• a histamine-2 blocker medicine, including famotidine (PEPCID ® ), cimetidine<br />
(TAGAMET ® ), nizatidine (AXID ® ), or ranitidine hydrochloride (ZANTAC ® ). Take these<br />
medicines at least 12 hours before or at least 4 hours after you take COMPLERA.<br />
• the antibiotic medicines clarithromycin (BIAXIN ® ), erythromycin (E-MYCIN ® , ERYC ® ,<br />
ERY-TAB ® , PCE ® , PEDIAZOLE ® , ILOSONE ® ), and troleandomycin (TAO ® )<br />
• an antifungal medicine by mouth, including fluconazole (DIFLUCAN ® ), itraconazole<br />
(SPORANOX ® ), ketoconazole (NIZORAL ® ), posaconazole (NOXAFIL ® ), voriconazole<br />
(VFEND ® )<br />
• methadone (DOLOPHINE ® )<br />
Ask your healthcare provider or pharmacist if you are not sure if your medicine is<br />
one that is listed above.<br />
Know the medicines you take. Keep a list of your medicines and show it to your<br />
healthcare provider and pharmacist when you get a new medicine. Your healthcare<br />
provider and your pharmacist can tell you if you can take these medicines with<br />
COMPLERA. Do not start any new medicines while you are taking COMPLERA without<br />
first talking with your healthcare provider or pharmacist. You can ask your healthcare<br />
provider or pharmacist for a list of medicines that can interact with COMPLERA.<br />
How should I take COMPLERA?<br />
• Stay under the care of your healthcare provider during treatment with COMPLERA.<br />
• Take COMPLERA exactly as your healthcare provider tells you to take it.<br />
• Always take COMPLERA with a meal. Taking COMPLERA with a meal is important<br />
to help get the right amount of medicine in your body. A protein drink does not<br />
replace a meal.<br />
• Do not change your dose or stop taking COMPLERA without first talking with your<br />
healthcare provider. See your healthcare provider regularly while taking COMPLERA.<br />
• If you miss a dose of COMPLERA within 12 hours of the time you usually take it, take<br />
your dose of COMPLERA with a meal as soon as possible. <strong>The</strong>n, take your next dose<br />
of COMPLERA at the regularly scheduled time. If you miss a dose of COMPLERA by<br />
more than 12 hours of the time you usually take it, wait and then take the next dose<br />
of COMPLERA at the regularly scheduled time.<br />
• Do not take more than your prescribed dose to make up for a missed dose.<br />
• When your COMPLERA supply starts to run low, get more from your healthcare provider<br />
or pharmacy. It is very important not to run out of COMPLERA. <strong>The</strong> amount of virus in<br />
your blood may increase if the medicine is stopped for even a short time.<br />
• If you take too much COMPLERA, contact your local poison control center or go to the<br />
nearest hospital emergency room right away.<br />
What are the possible side effects of COMPLERA?<br />
COMPLERA may cause the following serious side effects, including:<br />
• See “What is the most important information I should know about COMPLERA?”<br />
• New or worse kidney problems can happen in some people who take COMPLERA.<br />
If you have had kidney problems in the past or take other medicines that can cause<br />
kidney problems, your healthcare provider may need to do blood tests to check your<br />
kidneys during your treatment with COMPLERA.<br />
• Depression or mood changes. Tell your healthcare provider right away if you have<br />
any of the following symptoms:<br />
- feeling sad or hopeless<br />
- feeling anxious or restless<br />
- have thoughts of hurting yourself (suicide) or have tried to hurt yourself<br />
• Bone problems can happen in some people who take COMPLERA. Bone problems<br />
include bone pain, softening or thinning (which may lead to fractures). Your<br />
healthcare provider may need to do additional tests to check your bones.<br />
• Changes in body fat can happen in people taking HIV medicine. <strong>The</strong>se changes may<br />
include increased amount of fat in the upper back and neck (“buffalo hump”), breast,<br />
and around the main part of your body (trunk). Loss of fat from the legs, arms and<br />
face may also happen. <strong>The</strong> cause and long term health effect of these conditions are<br />
not known.<br />
• Changes in your immune system (Immune Reconstitution Syndrome) can happen<br />
when you start taking HIV medicines. Your immune system may get stronger<br />
and begin to fight infections that have been hidden in your body for a long time.<br />
Tell your healthcare provider if you start having new symptoms after starting your<br />
HIV medicine.<br />
<strong>The</strong> most common side effects of COMPLERA include:<br />
• trouble sleeping (insomnia)<br />
• abnormal dreams<br />
• headache<br />
• dizziness<br />
• diarrhea<br />
• nausea<br />
• rash<br />
• tiredness<br />
• depression<br />
Additional common side effects include:<br />
• vomiting<br />
• stomach pain or discomfort<br />
• skin discoloration (small spots or freckles)<br />
• pain<br />
Tell your healthcare provider if you have any side effect that bothers you or that does<br />
not go away.<br />
<strong>The</strong>se are not all the possible side effects of COMPLERA. For more information, ask your<br />
healthcare provider or pharmacist.<br />
Call your doctor for medical advice about side effects. You may report side effects to<br />
FDA at 1-800-FDA-1088 (1-800-332-1088).<br />
How do I store COMPLERA?<br />
• Store COMPLERA at room temperature 77 °F (25 °C).<br />
• Keep COMPLERA in its original container and keep the container tightly closed.<br />
• Do not use COMPLERA if the seal over the bottle opening is broken or missing.<br />
Keep COMPLERA and all other medicines out of reach of children.<br />
General information about COMPLERA:<br />
Medicines are sometimes prescribed for purposes other than those listed in a Patient<br />
Information leaflet. Do not use COMPLERA for a condition for which it was not prescribed.<br />
Do not give COMPLERA to other people, even if they have the same symptoms you have.<br />
It may harm them.<br />
This leaflet summarizes the most important information about COMPLERA. If you<br />
would like more information, talk with your healthcare provider. You can ask your<br />
healthcare provider or pharmacist for information about COMPLERA that is written<br />
for health professionals. For more information, call (1-800-445-3235) or go to<br />
www.COMPLERA.com.<br />
What are the ingredients of COMPLERA?<br />
Active ingredients: emtricitabine, rilpivirine hydrochloride, and tenofovir disoproxil<br />
fumarate<br />
Inactive ingredients: pregelatinized starch, lactose monohydrate, microcrystalline<br />
cellulose, croscarmellose sodium, magnesium stearate, povidone, polysorbate 20. <strong>The</strong><br />
tablet film coating contains polyethylene glycol, hypromellose, lactose monohydrate,<br />
triacetin, titanium dioxide, iron oxide red, FD&C Blue #2 aluminum lake, FD&C Yellow<br />
#6 aluminum lake.<br />
This Patient Information has been approved by the U.S. Food and Drug Administration<br />
Manufactured and distributed by:<br />
Gilead Sciences, Inc.<br />
Foster City, CA 94404<br />
Issued: August 2011<br />
COMPLERA, the COMPLERA Logo, EMTRIVA, HEPSERA, TRUVADA, VIREAD, GILEAD, and<br />
the GILEAD Logo are trademarks of Gilead Sciences, Inc. or its related companies.<br />
ATRIPLA is a trademark of Bristol-Myers Squibb & Gilead Sciences, LLC. All other<br />
trademarks referenced <strong>here</strong>in are the property of their respective owners.<br />
© 2012 Gilead Sciences, Inc. All rights reserved.<br />
202123-GS-000 02AUG2011 CON12383 3/12
Securing care<br />
for Women<br />
living With hiv<br />
Challenges and solutions for Hiv-positive women<br />
by NaiNa khaNNa<br />
FIVE YEaRS ago, womEn HaD THE DUBIoUS<br />
distinction of surpassing men as the majority of people<br />
in the world living with HIV. And in some countries,<br />
including Cambodia, Mozambique, and Rwanda, women<br />
now comprise nearly two-thirds of people living with the virus.<br />
In the U.S., the HIV epidemic looks<br />
very different. Women comprise over a<br />
quarter of the estimated 1.2 million people<br />
living with HIV in the U.S.—not including<br />
transgender women, for whom no accurate<br />
data are available. In 1984, women<br />
represented only 8% of HIV infections in<br />
the U.S. Thus, even at a national level, the<br />
trend is troubling. Data from 2012 show<br />
that in the District of Columbia, rates of<br />
new HIV diagnosis among black women<br />
have doubled. In Maryland, 35% of all AIDS<br />
diagnoses are among women, and in the<br />
U.S. Virgin Islands, 36.4% of people with<br />
an AIDS diagnosis were women in 2009.<br />
And when you drill down further, particularly<br />
in the U.S. South, in some counties,<br />
HIV infection rates among females may<br />
be even higher. Let’s be clear: this is not a<br />
numbers game anyone wants to win.<br />
Of even more concern, in the United<br />
States, HIV acquisition among women<br />
is correlated with race, poverty, experience<br />
of trauma, mental illness, substance<br />
use, and vulnerability to assorted social<br />
stigmas—the same factors that reduce<br />
likelihood of positive health outcomes in<br />
people living with HIV. That is, these socioeconomic<br />
factors increase vulnerability to<br />
poor health outcomes, with or without an<br />
HIV diagnosis. U.S. women living with HIV<br />
are disproportionately likely to be women<br />
of color (over 80%), especially black and<br />
Latina, and living in poverty, compared<br />
to men living with HIV. According to the<br />
HIV Cost Services and Utilization Study<br />
(HCSUS), 64% of HIV-positive women in<br />
ongoing medical care had annual incomes<br />
under $10,000, compared with 41% of<br />
HIV-positive men in care. More than twice<br />
as many HIV-positive women (76%) as<br />
HIV-positive men (34%) are living with and<br />
caring for at least one child under the age<br />
of 18. Thus, care systems for HIV-positive<br />
women must account for caretaking<br />
responsibilities, including provisions for<br />
minor children.<br />
Alarmingly, data show that ad<strong>here</strong>nce<br />
to anti-retroviral therapy tends to<br />
decrease among women living with HIV<br />
as the number of children under 18 living<br />
in the home increases. This is no real surprise.<br />
As women, we tend to prioritize caring<br />
for others over ourselves. Sometimes<br />
it’s a matter of practicality—we only have<br />
so many dollars to go around and hours<br />
in the day and bus vouchers. Sometimes<br />
it’s a matter of stigma—we don’t want<br />
others to see us taking our meds or going<br />
to medical appointments. And frequently<br />
it’s a reflection of how we value ourselves,<br />
especially as poor women, women of<br />
22 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM<br />
PHoTo: © IaS/STEVE SHaPIRo-commERcIaLImagE.nET<br />
ORGAnIzInG PRInCIPAL: Megaphone in hand,
Naina Khanna, Director of Policy and Community Organizing, WORLD, rallies demonstrators at the International AIDS Conference in July.<br />
color, women living with HIV. We have<br />
internalized that our health, our wellness,<br />
our wellbeing is too often not a priority for<br />
our society and political leaders—so why<br />
should we make it a priority for us?<br />
Transgender women are especially<br />
likely to live in extreme poverty, to face<br />
exceptional barriers to safe housing,<br />
employment, and access to quality health<br />
care, and, if HIV-positive, are less likely<br />
than other populations to receive antiretroviral<br />
therapy and more likely to experience<br />
negative interactions with health care<br />
providers. Transgender women are also<br />
disproportionately likely to face violence in<br />
their communities.<br />
Although researchers within the U.S.<br />
and internationally have known for years<br />
that women who have experienced violence<br />
and trauma are at elevated risk of<br />
acquiring HIV (even in non-conflict settings),<br />
new data released in 2012 show<br />
that women with HIV in the U.S. are<br />
twice as likely to have been victims of<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 23
Women’s bodies are not only about making babies.<br />
Fully upholding our human rights includes upholding our right<br />
to be sexual beings who experience joy and erotic pleasure.<br />
intimate partner violence and suffer posttraumatic<br />
stress disorder at a rate five<br />
times greater than HIV-negative women.<br />
Rates of violence faced by transgender<br />
women are likely to be even higher—data<br />
released in 2011 by the National Coalition<br />
of Anti-Violence Programs showed that<br />
transwomen comprised 44% of all LGBTQ<br />
murder victims. <strong>The</strong> same study found<br />
that over half of LGBTQ violence survivors<br />
did not even report attacks, with the highest<br />
rates of non-reporting being among<br />
transgender women of color. Not that<br />
surprising, given that transwomen also<br />
face disproportionate sexual, physical, and<br />
verbal harassment at the hands of police,<br />
according to Injustice at Every Turn—A<br />
Report of the National Transgender<br />
Discrimination Study. Research shows that<br />
women, including transwomen, who have<br />
experienced trauma are less likely to be<br />
ad<strong>here</strong>nt to medication and are more likely<br />
to face multiple barriers to care overall.<br />
Systemic violence against women also<br />
persists. Women living with HIV in the U.S.<br />
continue to report significant reproductive<br />
rights violations, despite medical progress<br />
and research and treatment advances that<br />
clearly demonstrate HIV-positive people<br />
can live a long and healthy life, avoid passing<br />
the virus to children with appropriate<br />
care and treatment, and even avoid passing<br />
the virus to their sexual partners, when<br />
viral load is suppressed and other factors<br />
that increase vulnerability (such as genital<br />
sores or ulcers) are not present.<br />
Importantly, for many women living<br />
with HIV, motherhood may be one of the<br />
only socially valued identities available to<br />
them. As described by Michelle Berger in<br />
Workable Sisterhood, many women living<br />
with HIV in the U.S. already exist at the<br />
intersection of race, class, and gender<br />
oppression, in addition to societal stigma<br />
about any behaviors they engage in, or life<br />
experiences they have had—even prior to<br />
HIV diagnosis. “When they became HIVpositive<br />
all the positions they occupied—<br />
drug user, sex worker, poor woman, were<br />
already concentrated, or saturated, with<br />
a set of representations and assumptions<br />
about those positions.” Thus, HIV becomes<br />
just another one of several stigmatizing<br />
social markers. Yet having a socially valued<br />
identity may impact HIV-positive women’s<br />
feelings about themselves and may inspire<br />
them to take better care of themselves. In<br />
one study, HIV-positive women reported<br />
that pregnancy and childrearing provided<br />
them a socially sanctified feeling of being<br />
important and valued. Motherhood<br />
became a highly valued identity that<br />
helped mitigate regret related to HIV<br />
acquisition and other life circumstances.<br />
One study, published in AIDS Patient<br />
Care and STDs in May 2010, demonstrated<br />
that of 181 predominantly African<br />
American HIV-positive women in care in<br />
two urban HIV medical clinics, only 31%<br />
reported a personalized discussion with<br />
their HIV provider about their own fertility<br />
desires and intentions. Of those 31%, 64%<br />
had initiated the conversation themselves<br />
with their providers. <strong>The</strong> same study<br />
found that age was a strong predictor of<br />
provider-patient communication about<br />
pregnancy, with women under the age of<br />
30 being six times more likely to have had<br />
a general conversation about pregnancy<br />
with their providers. Another study of 118<br />
HIV-positive women conducted at the<br />
University of Rochester found that 54%<br />
of participants in that study had been<br />
sterilized. <strong>The</strong> study found high rates of<br />
“tubal regret” among participants, and<br />
pointed to a need to counsel women living<br />
with HIV about reversible methods of<br />
contraception. And research conducted by<br />
the U.S. Positive Women’s Network found<br />
that women living with HIV self-reported<br />
high rates of coerced abortion, tubal ligation,<br />
and sterilization. When HIV-positive<br />
women do have conversations with providers<br />
about their fertility plans, some health<br />
care providers perceive the pregnancyrelated<br />
needs of women living with HIV<br />
to be limited exclusively to the prevention<br />
of vertical transmission. In addition, data<br />
collected by the U.S. Positive Women’s<br />
Network suggest that HIV criminalization<br />
laws, currently on the books in 36 states<br />
and U.S. territories, may deter women<br />
from HIV testing, from accessing care, and<br />
may intimidate them with regard to disclosing<br />
sexual behavior to providers.<br />
Despite the fact that t<strong>here</strong> are many<br />
other diseases and genetic disorders with<br />
higher risk of parent to child transmission,<br />
and that assisted reproduction is not only<br />
permitted but often encouraged in such<br />
cases, HIV status has been used as a special<br />
reason to deny HIV-positive women the<br />
right to conceive naturally or with assistance;<br />
the right to comprehensive family<br />
planning and counseling service; and the<br />
right to retain custody of their children.<br />
Given last year’s HPTN 052 data, which<br />
demonstrated a 96% reduction in HIV<br />
transmission among heterosexual serodiscordant<br />
partners when viral load was<br />
suppressed, people living with HIV and/<br />
or their partners who want to conceive<br />
should be counseled about a range of<br />
options, including natural conception and<br />
now pre-exposure prophylaxis (PrEP) for<br />
the negative partner. Prevention justice<br />
demands that a range of HIV prevention<br />
options be available, including options that<br />
are controlled by women. But women’s<br />
bodies are not only about making babies.<br />
Fully upholding our human rights includes<br />
upholding our right to be sexual beings<br />
who experience joy and erotic pleasure.<br />
And for some of us, that means not using<br />
condoms, with our partner’s knowledge<br />
and consent. This will require a conscious<br />
effort of providers counseling patients<br />
who have experienced stigma, sometimes<br />
multiple concurrent stigmas, to provide<br />
accurate information about risk.<br />
Despite the significant epidemic among<br />
U.S. women—it is estimated that 300,000<br />
women are living with HIV in the U.S., and<br />
25% is no minor proportion—the National<br />
HIV/AIDS Strategy, released in July 2010,<br />
failed to articulate a single goal specifically<br />
for women. It does not detail how to<br />
24 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
HIV care is more than just medical care. It must be coupled with<br />
services designed to uphold sexual and reproductive rights and<br />
to address the impact of violence and trauma in women’s lives.<br />
reduce new HIV infections among women,<br />
to increase access to care, or a strategy to<br />
improve women’s health outcomes. <strong>The</strong><br />
Strategy similarly failed to articulate the<br />
relationship between violence or trauma<br />
and HIV for women. And now<strong>here</strong> in the<br />
Strategy was the need to strengthen<br />
sexual health and reproductive choice for<br />
women living with HIV even mentioned.<br />
And just this year, although the<br />
President’s proposed domestic HIV budget<br />
for FY 2013 was relatively good, the Part D<br />
program was the only part of Ryan White<br />
for which a decrease was proposed. Part<br />
D is the only program within Ryan White<br />
specifically designed to meet the needs of<br />
women, youth, and families. This is indicative<br />
of an alarming trend away from women-centered<br />
care and supportive services<br />
when they are more critical than ever.<br />
Thus, not only are we faced with a<br />
well-documented social and political<br />
“war on women” from the far right, with<br />
all women’s rights and body sovereignty<br />
being utilized as a political football in the<br />
2012 election cycle—but women living with<br />
HIV are literally facing disproportionate<br />
wars: violence, and a battle for their lives,<br />
health, and dignity in their own communities,<br />
neighborhoods, and homes.<br />
And in the midst of all this, somew<strong>here</strong><br />
along the way we lost our will to address<br />
the gender nuances of the domestic HIV<br />
epidemic.<br />
2011’s HPTN 052 results demonstrated<br />
that achieving viral suppression in people<br />
living with HIV can effectively reduce<br />
onward transmission of HIV. Thus, ensuring<br />
high-quality care and access to voluntary<br />
treatment for people living with HIV should<br />
be one of our primary goals as an HIV community—to<br />
achieve the National HIV/AIDS<br />
Strategy’s prevention and care goals.<br />
In July, the International AIDS<br />
Conference (AIDS 2012) returned to the<br />
U.S. after a 22-year absence. <strong>The</strong> theme of<br />
AIDS 2012 was Turning the Tide Together—<br />
meaning that we have the science to end<br />
new HIV infections and to keep people<br />
living with HIV healthy. Now we have to<br />
muster the political will and resources to<br />
make this possibility a reality. Just last<br />
June, the Supreme Court of the United<br />
States upheld the Affordable Care Act<br />
(ACA)—a piece of legislation that holds<br />
great promise for all women, and especially<br />
for women living with HIV. But HIV<br />
care and treatment is more than just medication<br />
and more than just medical care,<br />
especially for women. It must be coupled<br />
with services designed to uphold sexual<br />
and reproductive rights and to address the<br />
impact of violence and trauma in women’s<br />
lives. Women living with HIV still face<br />
unique vulnerabilities in 2012 and turning<br />
the tide on the epidemic for women will<br />
require a gender-sensitive response.<br />
Because women’s access to health<br />
care and ability to ad<strong>here</strong> to medication<br />
is related in large part to other life factors,<br />
including our physical, psychological, and<br />
emotional safety, addressing logistical barriers<br />
to care and promoting safety for women<br />
is central to achieving the National HIV/AIDS<br />
Strategy’s goals and to achieving the promise<br />
of the Affordable Care Act for women.<br />
Through ACA implementation, we must<br />
also keep in place services that facilitate<br />
access to care for women living with HIV,<br />
including but not limited to psychosocial<br />
support, peer-based services, transportation,<br />
and childcare.<br />
Thankfully, President Obama’s March<br />
30 release of a memorandum establishing<br />
a federal interagency working group to<br />
address the intersection of HIV/AIDS, violence<br />
against women and girls, and gender-related<br />
health disparities presents a<br />
new opportunity to align the domestic HIV<br />
response with international standards and<br />
to rectify some of these serious oversights.<br />
<strong>The</strong> workgroup is charged with, among<br />
other things:<br />
n Integrating sexual and reproductive<br />
health services, gender-based violence<br />
services, and HIV/AIDS services, w<strong>here</strong><br />
research demonstrates that doing so<br />
will result in improved and sustained<br />
health outcomes.<br />
n Promoting research to better understand<br />
the intersection of the biological,<br />
behavioral, and social science bases<br />
for the relationship between increased<br />
HIV/AIDS risk, domestic violence, and<br />
gender-related health disparities.<br />
2012 marks a critical moment in the<br />
global HIV response. It’s time we truly<br />
commit to upholding women’s rights and<br />
the rights of all people living with and<br />
disproportionately impacted by HIV as an<br />
essential component to turning the tide of<br />
the epidemic. This must include:<br />
n Meaningful and visible leadership of<br />
women living with HIV in all aspects of<br />
decision-making.<br />
n Research on and funding for womencontrolled<br />
prevention options—tools<br />
which a woman can use without the<br />
consent or even the knowledge of her<br />
partner, and which uphold our full<br />
rights to sexual pleasure and sexual<br />
and reproductive health.<br />
n Bold action, including a plan and a<br />
timeline from the White House Office<br />
of National AIDS Policy to address<br />
the intersections of violence against<br />
women, HIV, sexual and reproductive<br />
rights, and women’s health.<br />
NaiNa khaNNa is the policy director at<br />
Women Organized to Respond to Lifethreatening<br />
Disease (WORLD) in Oakland,<br />
California and coordinates the U.S. Positive<br />
Women’s Network (PWN). She was<br />
appointed to President Obama’s Advisory<br />
Council on HIV/AIDS (PACHA) in 2010.<br />
She has presented and advised on women’s<br />
rights and achieving gender-sensitive,<br />
human rights-grounded policies informed<br />
by people living with HIV. Ms. Khanna was<br />
diagnosed with HIV in 2002.<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 25
lack WOmEn,<br />
SOcIETy,<br />
and HIV<br />
An expert talks about<br />
the context of infection<br />
takeN from aN iNterview with<br />
adaora a. adimora, md, mph<br />
editor’s Note: Adaora A. Adimora, MD, MPH, received her medical degree from<br />
Yale University School of Medicine and Master’s in Public Health in epidemiology<br />
(the study of how disease spreads among people) from the University of North<br />
Carolina at Chapel Hill (UNC). Dr. Adimora’s work as both a physician and an epidemiologist<br />
has focused on infectious disease, particularly HIV and its disproportionate<br />
effect on minority populations. Her groundbreaking research includes the<br />
publishing of the first national data on concurrent sexual partnerships in women<br />
and analysis of the contextual (social, economic, and environmental) factors that<br />
promote concurrent sexual partnerships among African Americans in the United<br />
States. She has testified before a Congressional committee on the HIV epidemic<br />
and, for World AIDS Day in 2010, was invited to the White House to speak in a<br />
panel discussion. <strong>The</strong> following is taken from an interview with Dr. Adimora.<br />
—EnID VázqUEz<br />
In THE mID-1900S, THERE waS<br />
the rise of so-called “risk factor<br />
epidemiology.” People became<br />
much more focused on individual<br />
determinants, the individual behaviors and<br />
characteristics of people that put them<br />
at risk for disease. And these things are<br />
important.<br />
But it turns out t<strong>here</strong>’s increasing<br />
evidence that in order to really make headway<br />
with the HIV epidemic in this country,<br />
and in the world, t<strong>here</strong>’s going to need<br />
to be more attention paid to some of the<br />
social factors that drive people’s behavior<br />
and also set them up to acquire infection.<br />
26 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
It appears, for example, that the connections<br />
between black people in the U.S.<br />
differ to some extent compared to the<br />
connections among white people in the<br />
sense that t<strong>here</strong> are more disassortative<br />
relationships, or relationships between<br />
people with different risk factors. T<strong>here</strong>’s<br />
more of a tendency for African Americans<br />
to have relationships with people who<br />
have much greater risk for HIV than they<br />
themselves do. T<strong>here</strong>’s also the issue of<br />
partnerships that overlap in time, or sexual<br />
concurrency. In addition, they tend to find<br />
partners within their communities, which<br />
are often segregated. Sexual concurrency<br />
TAmARA WILSOn, HIV-PoSITIVE SIncE 1999, VoLUnTEERS aT<br />
cHIcago womEn’S aIDS PRojEcT. SHE cREDITS HER moTHER<br />
wITH HELPIng HER To managE HER HIV, anD TPan FoR<br />
HELPIng To SaVE HER LIFE. PHoTogRaPH BY cHRIS knIgHT<br />
has been found to put people<br />
at greater risk for HIV than<br />
serial monogamy, even if<br />
people in both groups have<br />
had the same number of<br />
partners over the same<br />
period of time.<br />
THE THIng THaT<br />
is really, really<br />
important is the<br />
observation that<br />
it is the social context of<br />
life in the United States that<br />
really contributes to those<br />
partnership patterns. It’s<br />
pretty clear that black people<br />
as a whole tend to live under<br />
very different circumstances<br />
in the United States than<br />
white people do. And some<br />
of these characteristics that<br />
we have been studying, like<br />
incarceration for example,<br />
not only contribute to HIV,<br />
but they’re also emblematic<br />
of the oppression that<br />
minority populations are<br />
living under in the United<br />
States. A history of incarceration,<br />
for example, which is<br />
experienced by black men<br />
more than any other group,<br />
primarily as a result of the war on drugs,<br />
lowers the possibility of employment and<br />
increases the risk of poverty, while at the<br />
same time disrupting the stability of longterm<br />
partnerships. Incarceration and death<br />
due to violence and disease in black men<br />
lead more black women to enter into relationships<br />
with men who have greater risk<br />
factors for HIV than they do.<br />
This doesn’t mean that each and<br />
every minority, each and every African<br />
American, in the United States is poor and<br />
oppressed. But as a whole, it is these types<br />
of factors that contribute to the spread<br />
of HIV, STDs, and in fact different rates of<br />
other diseases, such as diabetes and heart<br />
disease. Black people are at greater risk<br />
of acquiring HIV infection independent of<br />
their own low-risk behavior compared to<br />
other groups.<br />
I<br />
woULD aLSo EmPHaSIzE THaT<br />
we do have personal responsibility for<br />
our behavior. However, I think some<br />
people tend to look at this work and<br />
say, “Oh, they’re just blaming the environment,<br />
blaming the majority population.”<br />
That’s really not exactly it. While we do<br />
have personal responsibility for our behavior,<br />
I think it’s very critically important to<br />
realize that black people have substantially<br />
increased risks than other populations,<br />
even with the same behavior. And this has<br />
been demonstrated. This is true for black<br />
gay men as well as for black heterosexual<br />
men and women.<br />
I would say to black women living with<br />
HIV, keep the faith. Teach your sons and<br />
daughters all the lessons you’ve learned.<br />
You have a wealth of experience, and certainly<br />
resiliency.<br />
We need to work in whatever ways we<br />
can to change the social and economic<br />
factors that are putting our people at risk,<br />
and putting our children at risk.<br />
It would help if everyone in the United<br />
States had health care. It’s astonishing to<br />
me that, apparently, health care is not a<br />
right. It remains an open question in the<br />
United States that people should have<br />
health coverage, even though it’s clearly<br />
most cost effective for the nation as a<br />
whole. This is a civil rights issue. That’s<br />
what I mean by working to change the<br />
economic factors that put people at risk.<br />
Health care availability, affordability for<br />
all, would make a huge difference in terms<br />
of transmission of HIV, and also in terms<br />
of the personal health of people who are<br />
living with HIV.<br />
go To positivelyaware.com To REaD<br />
PUBLISHED STUDIES anD aBSTRacTS.<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 27
‘everyone needS a Support<br />
How one therapist helps<br />
Hiv-positive women learn<br />
to take care of themselves<br />
by eNid vázquez<br />
FOR MORE THAN 10 YEARS,<br />
psychotherapist Kesha<br />
Burch, LCPC, has<br />
counseled HIV-positive<br />
women at the Chicago Women’s<br />
AIDS Project (CWAP). Whether<br />
positive or negative, the women<br />
she counsels face similar<br />
problems, she says, with health<br />
being an added and important<br />
concern for those living with<br />
HIV or any other chronic illness.<br />
“<strong>The</strong> HIV-positive women I work with<br />
have the same types of issues, but it’s even<br />
more important that they address emotional<br />
and life concerns because their health<br />
depends on it,” says Burch. While women<br />
often focus on interpersonal problems and<br />
family stress, improved health is always an<br />
underlying goal of Burch’s work at CWAP.<br />
“Stress that comes from emotional and<br />
psychological problems can be a threat to<br />
a woman with HIV,” she says, pointing out<br />
that stress and depression are known to<br />
increase mortality for positive women.<br />
Nevertheless, she finds that many<br />
women worry about their lovers and families<br />
more than they do about themselves,<br />
even in the face of HIV.<br />
“Women in our society are rewarded<br />
for taking care of other people,” Burch<br />
said. “We often don’t think about taking<br />
care of ourselves independent of someone<br />
helping us with that or coaching us<br />
through it. We may not be socialized to be<br />
assertive. And of course, all of that really<br />
comes through in thinking about how to<br />
28 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM<br />
PHOTO: PROEllEMEnTS PHOTOgRAPHy
SyStem’<br />
negotiate safe sex practices and so on and<br />
so forth.<br />
“You don’t want to get away from all<br />
the nurturing,” she notes, “but how do you<br />
take care of other people and take care of<br />
yourself as well? T<strong>here</strong> has to be some balance.<br />
Hopefully, counseling helps women<br />
achieve greater balance. It’s about feeling<br />
empowered enough to be themselves and<br />
to pursue things that they’re worthy of<br />
having in their lives,” says Burch.<br />
Instead, she finds that many women<br />
settle for less than they deserve, which can<br />
begin a cycle of more unhappiness in their<br />
lives. Others have problems establishing<br />
healthy relationships and may have negative<br />
coping skills, experiencing difficulty<br />
with attachment (including having many<br />
sexual partners) and figuring out who is<br />
worthy of being with them. <strong>The</strong>se women<br />
often feel that they have to accept bad<br />
behavior in order to be in a relationship or<br />
are confused about what they have to do<br />
to be in one.<br />
“T<strong>here</strong> are also issues around disclosure<br />
and that relates back to self-esteem and<br />
self-worth. It’s important for them to communicate<br />
with partners for their own health<br />
and also so that they can be truly known<br />
and accepted and loved,” she said. “This is<br />
similar to the things that other people are<br />
dealing with, being true to themselves.”<br />
Once a woman has a healthier relationship<br />
with herself, her other relationships<br />
are healthier too. Burch cites support<br />
groups and support buddies as being<br />
important for positive women, along with<br />
caring friends, family members, and supportive<br />
partners.<br />
“We were created to be in relationships<br />
with each other. It’s not just about<br />
romantic relationships, but about learning<br />
how to be a good parent and how<br />
to have a healthy friendship…all kinds of<br />
relationships that are essential to human<br />
existence,” she says. “Everyone needs a<br />
support system, and the healthier your<br />
support system, the better off you are.<br />
It’s about the people in your life who<br />
are for you and support you. That helps<br />
anybody’s mental health and physiological<br />
health as well. It helps anybody to become<br />
more resilient and do better.”<br />
What’s different for people living with a<br />
chronic illness like HIV, she says, is that the<br />
same skills they use for creating healthy<br />
relationships also work in managing their<br />
health care.<br />
“Sometimes negative issues can seep<br />
into their attitudes towards their health,<br />
their health care, and their provider.<br />
When I talk to them about using skills in a<br />
relationship, I recognize that those assertiveness<br />
skills can help them ask for what<br />
they need from their medical provider so<br />
they don’t just think that they go to their<br />
doctor and are told what to do, but report<br />
things that are of concern to them and<br />
ask, can we check into this?” Burch said.<br />
“Sometimes I rehearse with them. ‘What<br />
would you like to say when you go to the<br />
doctor?’ I had a client who felt that her<br />
doctor wasn’t listening to her. T<strong>here</strong> were<br />
some things that she thought needed to<br />
be addressed, but she was complaining<br />
about it to other people and not taking it<br />
back to the doctor to say ‘this really worries<br />
me’ or ‘I wish that at my last appointment<br />
we could have talked about this.’<br />
“So I helped her narrow down her complaints<br />
and her concerns to three things<br />
per visit, because t<strong>here</strong>’s some reality<br />
t<strong>here</strong> too. <strong>The</strong> doctor cannot spend 90<br />
minutes on a visit. <strong>The</strong> alternative was for<br />
her to feel consistently frustrated with her<br />
experience with the doctor,” Burch said.<br />
“She didn’t realize she could ask for what<br />
she wants. For the first item on her list, she<br />
was able to get a referral to a specialist.<br />
That also then reduced her anxiety and<br />
worry about what was going on with her.”<br />
She notes that not being able to communicate<br />
with a provider or understand<br />
what was being asked of them could lead<br />
some people to not take their medication<br />
correctly.<br />
Burch pointed to other practical things<br />
people can do to support their self-worth<br />
and value. “It could be as simple as putting<br />
on make-up. It could be signing up to take<br />
a class or to stop talking to someone who<br />
is not doing right by them—any behavioral<br />
steps that reinforce the message that<br />
they’re of value.”<br />
Going for counseling, she believes, is<br />
one big step towards self-care.<br />
“When you show up to therapy, that’s<br />
just in and of itself an affirmation that<br />
you’re worthy of a better life and this is<br />
part of what you are going to do about it,”<br />
Burch says. “T<strong>here</strong>’s always some kind of<br />
spark I see that pulls women in, something<br />
I can’t describe that gives them just a little<br />
bit of hope that things could be different.<br />
Especially for the women who are dealing<br />
with addiction, it’s that little piece of<br />
themselves that helps to pull them out,<br />
to show up on the doorstep of a detox or<br />
drug treatment program. T<strong>here</strong>’s a ton<br />
of internal strength and resiliency t<strong>here</strong>,<br />
and that’s something that I reflect back to<br />
them sometimes. ‘Look at all that you’ve<br />
been through to get to this point.’<br />
“When you see that spark, that’s the<br />
essence of who that person really is,” says<br />
Burch. “<strong>The</strong> trick is to get them to see it,<br />
despite their circumstances.”<br />
She sometimes suggests that people<br />
make positive affirmations, keep a journal,<br />
and read certain books or authors. While<br />
she can help weed out negative beliefs<br />
people have about themselves that they<br />
may not even be aware of, these activities<br />
can keep people focused on messages<br />
that are the opposite of the negative<br />
beliefs and feelings. “It’s about changing<br />
that message,” she said.<br />
She sometimes has clients take time<br />
to just relax and sit silently. Many people<br />
are often too busy running around doing<br />
everything they have to do to give themselves<br />
time for reflection and hearing<br />
what’s inside them, she said.<br />
Perhaps the most important part of<br />
her work, she believes, is treating people<br />
with kindness and respect. “That’s really<br />
at the core of the Chicago Women’s AIDS<br />
Project,” she notes. “<strong>The</strong> mission statement<br />
is about empowering women, seeing<br />
the value in each and every woman.”<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 29
nine monthS to Birt<br />
Hiv and pregnancy—keeping yourself and your baby healthy<br />
by JohN verNa, ms, pa-c<br />
WELL, aS YoU SUSPEcTED, YoUR PREgnancY<br />
test is positive. Congratulations! Pregnancy can<br />
be an exciting time, and a really wonderful experience.<br />
Of course, now that you’re expecting, you<br />
probably have lots of questions, some of which relate to how your<br />
HIV-positive status will impact your pregnancy and your baby.<br />
<strong>The</strong> goal in every pregnancy is to keep<br />
both mom and baby healthy—and I’m<br />
happy to say that this is a goal that’s well<br />
within your reach. Just because you have<br />
HIV does not mean you can’t have a happy,<br />
healthy pregnancy, and a happy, healthy<br />
baby. Basically, the same things that keep<br />
you healthy will keep your baby healthy.<br />
Risks of transmitting the virus to your baby<br />
decrease as your own viral load decreases.<br />
In fact, if you are on HIV medication<br />
and take the medications as prescribed,<br />
t<strong>here</strong>’s only a 1% chance of passing HIV<br />
to your baby. In my 11 years as an HIV<br />
specialist, and having seen over 150 pregnant<br />
patients with HIV, I have never had<br />
a patient pass HIV to her baby. However,<br />
if you’re not on HIV meds, or don’t take<br />
them like you’re supposed to, t<strong>here</strong>’s<br />
a 25% chance (basically a one in four<br />
chance) that you will pass HIV to the baby.<br />
Even medication at the last minute, at the<br />
time of labor, cuts the risk and some states<br />
have laws about testing mothers during<br />
labor if an HIV test result is not on file for<br />
the pregnancy.<br />
So let’s talk about what you need to<br />
do to keep both you and your little one<br />
healthy. Many women wonder how HIV<br />
can be transmitted to the baby. HIV can<br />
be transmitted during pregnancy, during<br />
labor and delivery, or by breastfeeding.<br />
We’ll talk about what you can do during<br />
pregnancy, during labor, and after your<br />
baby is born to decrease the chances of<br />
transmitting the virus.<br />
hOW TO REduCE ThE RISk Of<br />
TRAnSmITTInG hIV TO YOuR<br />
BABY duRInG PREGnAnCY<br />
KEEPIng YoUR VIRaL LoaD<br />
low is important during pregnancy<br />
to reduce the risk of<br />
transmission. Regardless of<br />
what is recommended based solely on<br />
your CD4+ and VL levels, you may want to<br />
start taking HIV meds as soon as you learn<br />
you are pregnant. Yes, t<strong>here</strong> are guidelines<br />
from the Department of Health and<br />
Human Services (DHHS) that recommend<br />
when to start treatment based on CD4+<br />
and VL, but t<strong>here</strong> are groups of people<br />
for which treatment is recommended no<br />
matter what. Pregnant women are one of<br />
those groups. We are trying to prevent<br />
your baby from becoming infected.<br />
Earlier initiation of therapy may<br />
be more effective in reducing in utero<br />
transmission. In fact, a 2010 study conducted<br />
in France found that “early and<br />
sustained control of HIV viral replication is<br />
associated with decreased residual risk of<br />
transmission and favors initiating HAART<br />
drugs as early in pregnancy as possible<br />
for all women.” In other words, starting<br />
HAART (highly active antiretroviral<br />
therapy) drugs early to control the viral<br />
load as much as possible decreased the<br />
chances that the virus would be transmitted<br />
to the baby. In fact, we know that having<br />
an undetectable viral load substantially<br />
lowers the risk of transmission of HIV to<br />
the fetus and lessens the need for consideration<br />
of cesarean delivery (C-section).<br />
That’s why I have always suggested that<br />
my patients start HAART immediately<br />
after learning about their pregnancy.<br />
So, if you are not currently taking HIV<br />
medications (whether you are treatmentnaïve<br />
or have taken them in the past), tell<br />
your HIV specialist about what medications<br />
you’ve taken in the past and provide<br />
all laboratory tests (genotypes, phenotypes,<br />
HLA B*5701) and be honest about<br />
any ad<strong>here</strong>nce issues that you’ve had in<br />
the past. Also talk about any tolerability<br />
issues and drug allergies you have had<br />
with any old regimen(s).<br />
As soon as you learn that you’re pregnant,<br />
you should contact your HIV specialist<br />
to discuss your options for medication<br />
and to review what you’re currently taking<br />
to make sure your medications are safe<br />
for the baby. If you are taking HIV medication,<br />
like HAART, your clinician will likely<br />
continue your treatment. However, if you<br />
are taking a regimen that contains efavirenz<br />
(Sustiva, which is also a component<br />
of Atripla), you’ll need to make a change.<br />
Efavirenz is a Pregnancy Category D medication,<br />
meaning it should not be taken<br />
30 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
h day<br />
while pregnant, especially during the<br />
first trimester of your pregnancy.<br />
It’s reassuring, however, to know<br />
that of 14 studies with 1,345<br />
pregnant women on efavirenz<br />
published in the journal AIDS<br />
two years ago, t<strong>here</strong> was only<br />
one infant born with a birth<br />
defect, a rate no different<br />
from the general population<br />
of pregnant women.<br />
Many women wonder<br />
if HIV medications are<br />
going to harm their<br />
babies or themselves.<br />
Several HIV medications<br />
have been found<br />
to be safe for pregnant<br />
women and babies. As<br />
a matter of fact, t<strong>here</strong> is<br />
an international registry<br />
(the Antiretroviral Pregnancy<br />
Registry) that monitors<br />
for potential<br />
birth defects<br />
in infants<br />
exposed to<br />
HIV medications<br />
in<br />
utero. <strong>The</strong><br />
Department<br />
of Health and<br />
Human Services<br />
(DHHS) currently<br />
recommends Kaletra<br />
and Combivir taken twice<br />
a day. Ask your HIV specialist<br />
what is going to be best for<br />
you and keep in mind that<br />
results of any past or current<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 31<br />
PHOTO © JAni BRySOn
You should have discussions with both your obstetrician and HIV specialist<br />
to help determine what is best for you and your baby. If you don’t have a<br />
specialist, now might be a good time to seek one out.<br />
genotype test will also be considered. If<br />
you have a viral load of more than 1,000<br />
copies, your provider will order a genotype<br />
before starting you on medications.<br />
Any drug resistance found by the test may<br />
limit your treatment options.<br />
So t<strong>here</strong> is a lot to consider <strong>here</strong>, and<br />
you should have discussions with both<br />
your obstetrician and HIV specialist to<br />
help determine what is best for you and<br />
your baby. Assuming that you have an<br />
HIV specialist, your specialist will refer<br />
you to an obstetrician who has experience<br />
with HIV-positive mothers. If you don’t<br />
have a specialist, now might be a good<br />
time to seek one out. You can visit the<br />
websites of the American Academy of HIV<br />
Medicine (www.aahivm.org) and the Gay<br />
and Lesbian Medical Association (http://<br />
glma.org), or call the National AIDS Hotline<br />
(open 24 hours a day every day of the<br />
year) at 1-800-CDC-INFO (232-4636).<br />
ThE RIGhT dOCTOR<br />
And ThE RIGhT TESTS<br />
IT can BE VERY HELPFUL To<br />
have an obstetrician with experience<br />
treating HIV-positive women, in part<br />
because the decisions regarding<br />
whether to use certain “invasive” genetic<br />
tests can be difficult. Many pregnant<br />
women undergo a variety of screening<br />
tests. During the first trimester these tests<br />
include a fetal ultrasound and a blood<br />
test for mom. This screening process can<br />
help determine the risk of the fetus having<br />
certain birth defects (Down syndrome, trisomy<br />
18, or trisomy 13). Second trimester<br />
prenatal screening may include additional<br />
blood testing (of mom) called Multiple<br />
Markers. <strong>The</strong>se include alpha-fetoprotein<br />
(AFP), hCG, estriol, and inhibin. <strong>The</strong>se<br />
markers provide information about a<br />
woman’s risk of having a baby with genetic<br />
conditions or birth defects. This screening<br />
is usually performed between the 15th and<br />
20th weeks of pregnancy.<br />
If the results of these tests are<br />
abnormal, genetic counseling is recommended.<br />
Additional testing may be<br />
needed for an accurate diagnosis. <strong>The</strong>se<br />
tests include chorionic villus sampling<br />
(CVS) and amniocentesis, both of which<br />
are considered “invasive.” During amniocentesis,<br />
a small amount of amniotic fluid<br />
is removed by inserting a long, thin needle<br />
through your belly and into the womb.<br />
In CVS, chorionic villi <strong>cells</strong> are removed<br />
from the placenta, either in the same way<br />
amniocentesis is performed or through the<br />
cervix using a catheter and gentle suction.<br />
Because these tests are invasive, they<br />
involve at least a theoretical increased<br />
risk of transmitting the virus to the baby.<br />
To date, t<strong>here</strong> have been 159 reported<br />
invasive procedures on HIV-positive moms<br />
with no transmission of HIV to the baby.<br />
In all cases, women were on HAART with<br />
undetectable viral loads and though no<br />
transmissions of HIV have occurred, a<br />
small increase in risk can’t be ruled out.<br />
T<strong>here</strong>fore, any HIV-positive woman undergoing<br />
any invasive procedure should be<br />
on HAART and have an undetectable viral<br />
load at the time of the procedure.<br />
Some experts consider CVS too risky<br />
to offer to their HIV-positive patients and<br />
recommend limiting invasive procedures<br />
to amniocentesis only, but existing data<br />
on transmission risk associated with<br />
these procedures are limited. Invasive<br />
testing procedures should be discussed<br />
thoroughly with your OB and between<br />
you and your partner. Your OB (or genetic<br />
counselor) will discuss the pros and cons<br />
of invasive testing with you. But ultimately,<br />
whether to test (or not to test) is a personal<br />
decision.<br />
LOWERInG ThE RISk<br />
duRInG LABOR And dELIVERY<br />
AgaIn, THE goaL IS To<br />
limit the baby’s exposure to<br />
the virus. So it’s probably not<br />
surprising that your options<br />
for labor and delivery depend upon your<br />
viral load (another important reason to<br />
take your HIV meds as prescribed). <strong>The</strong><br />
American College of Obstetricians and<br />
Gynecologists (ACOG) has recommended<br />
considering a scheduled C-section delivery<br />
for HIV-positive women since 1999. A<br />
scheduled C-section is recommended for<br />
women with a viral load that’s greater than<br />
1,000 copies/mL near the time of delivery<br />
(36 weeks’ gestation) and for any woman<br />
with an unknown viral load. It is also<br />
recommended for women who did not<br />
receive HIV medication during pregnancy.<br />
In these situations, ACOG recommends a<br />
scheduled C-section at 38 weeks’ gestation<br />
in order to decrease the likelihood of<br />
onset of labor or rupture of membranes<br />
before delivery.<br />
For women with a viral load that’s<br />
less than 1,000 copies/mL near time of<br />
delivery, a scheduled C-section is not<br />
routinely recommended. So, if your viral<br />
load is less than 1,000 copies/mL near the<br />
time of delivery, your choices for labor<br />
and delivery are essentially the same as<br />
a woman who doesn’t have the virus, and<br />
you can have a vaginal delivery. <strong>The</strong> risk<br />
of perinatal transmission of HIV in women<br />
with an undetectable viral load (at 36<br />
weeks gestation) is 1% or less, even with a<br />
vaginal delivery. No evidence is available<br />
to show that this risk can be lowered further<br />
by performing a scheduled C-section.<br />
Remember, a C-section is major surgery<br />
and has its own risk of complications, compared<br />
with vaginal delivery.<br />
Under new DHHS guidelines, only<br />
women with viral loads of more than 400<br />
copies/mL should be given IV zidovudine<br />
(AZT) continuously, even if your genotype<br />
shows resistance for this drug. <strong>The</strong><br />
use of AZT is recommended because of<br />
its unique characteristics and its proven<br />
record in reducing transmission.<br />
To help prevent transmission, your<br />
baby will be given liquid AZT immediately<br />
after birth and this will be continued (by<br />
you at home) twice a day for six weeks.<br />
32 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
ARE yOu AWAre? gET PosITIvely AWAre.<br />
❑ 1-year subscription: $30 donation.<br />
Six bi-monthly issues every year. Subscriptions are mailed free of<br />
charge within the U.S. to those who are HIV-positive.<br />
❑ Bulk copies (U.s. only):<br />
Available free of charge; however, a donation is requested to cover<br />
shipping. No international bulk orders. Minimum order 10 copies,<br />
shipped via UPS (No P.O. Box addresses): ______ copies<br />
❑ Back issues: $3 per copy. enclosed is my payment.<br />
______ copies: July+August 2012<br />
______ copies: May+June 2012<br />
______ copies: March+April 2012 (HIV Drug Guide)<br />
______ copies: January+February 2012<br />
❑ Sign me up for the E-News, PA’s weekly email newsletter:<br />
EmaIL aDDRESS<br />
Women in the U.S. with HIV should not breastfeed their babies<br />
due to increased risk of transmitting the virus. Baby formula<br />
is a safe and healthy alternative.<br />
Unfortunately, women in the U.S. with<br />
HIV should not breastfeed their babies<br />
due to increased risk of transmitting the<br />
virus. Baby formula is a safe and healthy<br />
alternative to breast milk and t<strong>here</strong> are<br />
many brands and options that are available<br />
to you. Also, while the risk is very<br />
low, HIV can also be transmitted to a baby<br />
through food that was pre-chewed by an<br />
HIV-positive mother (or caretaker). To be<br />
completely safe, babies should not be fed<br />
pre-chewed food.<br />
dOES ThE BABY hAVE hIV?<br />
THERE aRE Two TYPES oF<br />
tests that will be performed on<br />
your baby to find out if he or she<br />
has HIV. <strong>The</strong> first is the HIV antibody<br />
test. All babies born to a mom with<br />
HIV will test positive for the first several<br />
❑ Enclosed is my donation of<br />
❑ $25 ❑ $50 ❑ $100 ❑ $250 ❑ $500 ❑ $_______<br />
months of their lives. This does not mean<br />
that they have HIV. Rather, it means that<br />
the baby has simply been exposed to his/<br />
her mother’s HIV. <strong>The</strong> second test, PCR<br />
testing, looks for the virus and not just the<br />
antibodies to the virus. It is this test that<br />
can tell whether the baby has HIV or not.<br />
This test will be done during the first few<br />
days of his/her life.<br />
<strong>The</strong> PCR test will be repeated several<br />
times on your baby. To know for certain<br />
that your baby is not infected with HIV, the<br />
baby must not be breastfeeding and must<br />
have two negative PCR tests, the first at<br />
one month (or older) and the second at<br />
four months (or older). Many experts confirm<br />
the HIV-negative status of the baby<br />
with an HIV antibody test at age 12 to 18<br />
months. To be diagnosed with HIV, a baby<br />
must have two positive PCR tests.<br />
Bill to:<br />
CARd nuMBER ExPiRES<br />
nAME On CARd<br />
SignATuRE (REquiREd)<br />
charge my: ❑ Visa ❑ MasterCard ❑ American Express<br />
total amouNt: $___________<br />
Charges will appear on your credit card statement as TPA Network. test Positive<br />
Aware Network (tPAN) is a not-for-profit organization dedicated to providing<br />
support and information to all people affected by HIV.<br />
Ship to:<br />
Your contribution helps provide subscriptions to people who can’t<br />
afford them. All donations are tax-deductible to the full extent allowed<br />
by law.<br />
PHOnE<br />
mail to:<br />
E-MAil<br />
PosITIvely AWAre<br />
5537 n. BRoaDwaY ST.<br />
POSiTivElyAwARE.COM cHIcago, IL 60640 SEPTEMBER+OCTOBER 2012 33<br />
nAME<br />
AgEnCy (if APPliCABlE)<br />
AddRESS<br />
Again, just because you have HIV does<br />
not mean you can’t have a healthy pregnancy<br />
and baby. In fact, just this past year<br />
I had an HIV-positive patient who followed<br />
her regimen and had a healthy pregnancy,<br />
and an uncomplicated vaginal birth. She<br />
and her husband welcomed a healthy<br />
HIV-negative baby into the world. It can be<br />
done, and it is done by lots of women just<br />
like you every day. So, again, congratulations!<br />
JohN verNa has spent his entire professional<br />
career providing health care to individuals<br />
with HIV. For the past three years,<br />
he has worked at Access Community<br />
Health Network in Chicago. John knows<br />
just how special (and scary) pregnancy<br />
can be, as he and his wife recently welcomed<br />
their first child.<br />
CiTy STATE ZiP
COnfEREnCE uPdATE<br />
AIdS 2012<br />
washiNgtoN, d.c.<br />
CuRE CAuCuS: (above, from left) Sharon Lewin, MD, PhD; Rowena Johnston, vice president of research, amfAR; Steven Deeks, MD,<br />
University of California San Francisco; Françoise Barré-Sinoussi, new president of the International AIDS Society; Mark Harrington,<br />
Treatment Action Group; and UNAIDS executive director Michel Sidibé review developments in HIV cure research.<br />
After a 22-year absence, the International<br />
AIDS Conference returned to the U.S. following<br />
President Obama’s lifting of the federal immigration<br />
and travel ban against people from outside the<br />
U.S. with HIV/AIDS. An estimated 22,000 activists,<br />
advocates, clinicians, and others converged on<br />
Washington, D.C. in July. For conference webcasts<br />
and transcripts go to www.aids2012.org.<br />
IAS cure workshop highlights<br />
advances and challenges<br />
by Jeff berry<br />
At this year’s conference we<br />
heard about exciting advances<br />
in cure research, as well as<br />
the launch of the International<br />
AIDS Society’s (IAS) “Towards<br />
an HIV Cure” global scientific<br />
strategy. A two-day pre-conference<br />
workshop brought<br />
together researchers and<br />
community advocates to preview<br />
some of these advances<br />
and provide insight into work<br />
being done in the seven different<br />
areas of research that<br />
the agenda has identified as<br />
highest priority.<br />
<strong>The</strong> workshop, cochaired<br />
by Steven Deeks,<br />
MD, University of California,<br />
San Francisco, and IAS<br />
president and Nobel laureate<br />
Françoise Barré-Sinoussi,<br />
Pasteur Institute, Paris, was<br />
opened by Dr. Anthony S.<br />
Fauci, Director of the National<br />
Institute of Allergy and<br />
Infectious Diseases, NIH. In<br />
his opening remarks, Fauci<br />
stated that a cure that only<br />
benefits 0.01% of the population<br />
is not going to excite<br />
anyone—it has to be scalable.<br />
During the community<br />
literacy session Australian<br />
researcher Sharon Lewin, MD,<br />
PhD, gave an overview presentation<br />
addressing major<br />
barriers to a cure, including<br />
what actually defines a<br />
cure and potential targets<br />
and mechanisms, as well as<br />
underscoring the importance<br />
of assays for future research<br />
and the need for these tests<br />
to undergo rigorous standardization<br />
with labs before<br />
going into wider use.<br />
Activist and PoSITIVELY<br />
awaRE contributor Matt<br />
Sharp talked about his experiences<br />
as a cure research<br />
study participant, and the<br />
challenges that lie ahead,<br />
including ethical study<br />
design, Analytical Treatment<br />
Interruptions (ATI), and<br />
informed consent.<br />
Sharp noted that some<br />
cure research may be quite<br />
risky, with little chance for<br />
benefit. He asked what the<br />
“reasonable” risks are for HIVpositive<br />
individuals who will<br />
be participating in early and<br />
potentially dangerous cure<br />
studies, and how can we best<br />
protect them? Developing<br />
guidelines for determining<br />
when potentially risky<br />
treatment interruptions are<br />
appropriate is a critical next<br />
step, said Sharp, and community<br />
input and community<br />
advisory boards are essential<br />
in ensuring ethical, patientoriented<br />
studies.<br />
An elegant presentation<br />
given by Robert Siliciano, MD,<br />
PhD, Johns Hopkins University<br />
School of Medicine, was perhaps<br />
one of the clearest and<br />
most concise presentations<br />
I’ve ever seen on the basics<br />
of immunology, HIV infection,<br />
34 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM<br />
PHOTOS: ©iAS/STEvE SHAPiRO-COMMERCiAliMAgE.nET
and the multiple molecular<br />
mechanisms which maintain<br />
HIV latency. HIV is not completely<br />
eradicated from the<br />
body by standard antiretroviral<br />
therapy because some of it<br />
lies resting in memory CD4+T<strong>cells</strong>,<br />
which can proliferate for<br />
an average of 73.4 years in<br />
the human body. However, if<br />
you stop taking therapy, the<br />
virus typically comes roaring<br />
back within a matter of weeks.<br />
One eradication approach<br />
would be to remain on standard<br />
ARV therapy to keep<br />
the virus suppressed, while at<br />
the same time purging these<br />
latent reservoirs and blocking<br />
them from infecting new<br />
<strong>cells</strong>, so that they would have<br />
now<strong>here</strong> to go and eventually<br />
die off, ridding the body of<br />
HIV. But it’s complicated—the<br />
number of latently infected<br />
<strong>cells</strong> may be much higher<br />
than previously thought, by as<br />
much as 50-fold, according to<br />
Siliciano.<br />
Sarah Palmer, PhD, Swedish<br />
Institute for Communicable<br />
Disease Control and Karolinska<br />
Institute, gave a presentation<br />
on measuring persistent HIV<br />
infection, including an excellent<br />
slide outlining some of the<br />
advantages and disadvantages<br />
of the four currently available<br />
assays which measure persistence.<br />
In concluding her talk,<br />
Palmer emphasized that “looking<br />
ahead, to determine the<br />
effectiveness of curative strategies,<br />
our field will need to<br />
develop a more standardized<br />
assay system which is sensitive,<br />
efficient, less costly, and<br />
adaptable in local settings.”<br />
Other presentations<br />
covered recent advances in<br />
the development of accurate<br />
animal models for<br />
use in future cure<br />
research, vaccine<br />
and immune-based<br />
therapies and the role<br />
of immune activation<br />
and inflammation in<br />
viral persistence.<br />
<strong>The</strong> conference<br />
ended with a slightly<br />
unorthodox, yet<br />
immensely informative<br />
and entertaining<br />
presentation by Fred<br />
Verdult of Amsterdam<br />
on the psychosocial<br />
benefits of a cure for<br />
HIV. Verdult, after<br />
finding out he had HIV<br />
in 1998, started Volle<br />
Maan, an organization<br />
that conducts studies<br />
and communication projects<br />
on health and disease to<br />
encourage people to live full<br />
and worthwhile lives. Volle<br />
conducted a survey of 458<br />
individuals in the Netherlands<br />
asking how important to them<br />
a cure for HIV is, why a cure is<br />
important, and which type of<br />
cure is preferred.<br />
<strong>The</strong> majority of the survey<br />
respondents indicated they<br />
were in good health, with<br />
only 14% stating that their<br />
health was poor. Seventy-two<br />
percent said that it was very<br />
important to them to be cured<br />
of HIV, while another 22% said<br />
it was somewhat important.<br />
Yet when asked about how a<br />
cure might look, participants<br />
had varying responses. 95%<br />
thought that a total cure<br />
without any risk of future<br />
transmission or infection very<br />
desirable, while only 41% considered<br />
it desirable to have a<br />
cure that had no risk of future<br />
transmission but carried a risk<br />
ShARP TuRn: PA contributor Matt<br />
Sharp talks about his experiences as a<br />
cure research study participant.<br />
of future infection. <strong>The</strong> survey<br />
also asked about disadvantages<br />
of living with HIV—the<br />
risk of experiencing health<br />
problems in the future was<br />
the number one answer, while<br />
psychosocial effects such as<br />
stigma and the risk of infecting<br />
someone else were also<br />
highly ranked.<br />
Deeks closed the twoday<br />
workshop by declaring<br />
Verdult’s presentation the<br />
“highlight of the meeting,”<br />
and remarking on the spirit<br />
of collaboration among the<br />
attendees. Barré-Sinoussi said<br />
that next steps include the<br />
efforts of the working groups,<br />
including a newly added<br />
social sciences research team<br />
and an ethics working group,<br />
as well as a call for more cure<br />
research funding and collaboration.<br />
<strong>The</strong> next IAS Towards<br />
an HIV Cure workshop is<br />
scheduled for immediately<br />
prior to the 2013 international<br />
conference in Kuala Lumpur,<br />
Malaysia.<br />
Other news on<br />
the cure front<br />
A group of patients in France<br />
who became infected with<br />
HIV and then started on<br />
antiretroviral therapy (ART)<br />
early in the post-infection<br />
period have shown no signs<br />
of a resurgence of their Hiv<br />
infection seven years after<br />
being taken off therapy.<br />
“<strong>The</strong>se results suggest<br />
that…antiretroviral treatment<br />
should be started very early<br />
after infection,” said Charline<br />
Bacchus, lead researcher<br />
of the study at the French<br />
National Agency for Research<br />
on AIDS and Viral Hepatitis<br />
(ANRS).<br />
<strong>The</strong> patients in the ANRS<br />
EP47 VISCONTI cohort (known<br />
as the Visconti Cohort) have<br />
an extremely low reservoir of<br />
HIV in their <strong>cells</strong> similar to that<br />
of “HIV controller” patients.<br />
HIV controllers are those who<br />
are able to control their HIV<br />
infection without the use of<br />
ART for an extended period of<br />
time, and represent about one<br />
out of every 300 people who<br />
have HIV.<br />
In the study, 12 patients<br />
started therapy within 10<br />
weeks of infection, were on<br />
therapy for an average of<br />
three years, and were able to<br />
control HIV after an average<br />
of seven years off therapy.<br />
At a press conference Asier<br />
Saez-Cirión, one of the study<br />
investigators, said they<br />
were interested in finding<br />
out whether HIV controller<br />
status could be induced. He<br />
estimated that 5–15% of those<br />
treated early could eventually<br />
control HIV off therapy. But<br />
don’t stop those HIV meds<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 35
COnfEREnCE uPdATE<br />
AIdS 2012<br />
washiNgtoN, d.c.<br />
just yet—not only would we<br />
need to figure out how to<br />
identify who would have this<br />
type of response to early<br />
treatment, but also get those<br />
individuals onto treatment<br />
immediately following infection.<br />
<strong>The</strong> other question one<br />
might ask is, could some of<br />
those in the study already<br />
have been HIV controllers to<br />
begin with? While the genetic<br />
alleles commonly associated<br />
with HIV controllers was not<br />
found in these patients t<strong>here</strong><br />
may be other factors playing<br />
a role, which researchers now<br />
are trying to uncover.<br />
Another study looked<br />
at two men who had been<br />
infected with Hiv for many<br />
years, on suppressive antiretroviral<br />
therapy (ART), and<br />
who underwent treatment of<br />
lymphoma via an allogenic<br />
(meaning foreign, or from<br />
another donor) stem cell<br />
transplantation. Both patients<br />
received a milder form of<br />
chemotherapy, known as the<br />
conditioning regimen, prior<br />
to transplant, which allowed<br />
them to stay on their ART during<br />
and after the transplant.<br />
One patient was on Atripla,<br />
the other on Isentress/<br />
Truvada. HIV was detectable<br />
in their <strong>cells</strong> immediately after<br />
the transplant, but the transplanted<br />
donor <strong>cells</strong> replaced<br />
the patients’ own lymphocytes<br />
over time. <strong>The</strong> amount<br />
of HIV DNA in their blood<br />
<strong>cells</strong> decreased and became<br />
undetectable, for up to two<br />
years now in one patient and<br />
three-and-a-half years in the<br />
other. CD4s declined in both<br />
patients initially, followed by<br />
a robust CD4 increase in one<br />
patient, and the stabilization<br />
and no further decline of<br />
CD4s in the other.<br />
Unlike Timothy Ray<br />
Brown, the “Berlin” patient,<br />
who received <strong>cells</strong> that were<br />
resistant to HIV because they<br />
lacked the CCR5 receptor,<br />
these patients received <strong>cells</strong><br />
that were CCR5+. It is believed<br />
that the antiretroviral treatment<br />
protected the donor<br />
<strong>cells</strong> from becoming infected,<br />
leading one researcher to refer<br />
to it as “a form of PrEP [preexposure<br />
prophylaxis] at the<br />
cellular level.” Further tissue<br />
sampling and analytic treatment<br />
interruption will need to<br />
be conducted to assess the full<br />
extent of the reduction of HIV<br />
in the reservoir.<br />
At a press conference<br />
held the same day these two<br />
studies were presented, David<br />
Margolis, MD, University of<br />
North Carolina at Chapel<br />
Hill, was asked by a reporter<br />
about the media’s role in<br />
reporting on cure advances<br />
responsibly and accurately,<br />
while at the same time not<br />
giving too much hope or creating<br />
complacency.<br />
“That’s your job,” said<br />
Margolis. “We are very<br />
careful about what we say<br />
[as researchers], and we’ve<br />
defined cure several different<br />
ways. Different kinds of<br />
cure and eradication mean<br />
different things to different<br />
people, and have different<br />
levels of value. Perhaps we<br />
should come up with a word,<br />
like ‘complicated-eradicationchemo-immunotherapy,’<br />
to<br />
slow people down. But you<br />
can’t argue with the goal and<br />
you can’t get t<strong>here</strong> without<br />
working on it—and I can’t say<br />
how long it will take.”<br />
Drug updates<br />
by eNid vázquez<br />
Complera, the newest single<br />
tablet regimen (STR), comprised<br />
of rilpivirine (Edurant)<br />
plus emtricitabine/tenofovir<br />
(Truvada), continues to hold<br />
its own. Previously, it had<br />
been shown to be non-inferior<br />
to Atripla, another STR, made<br />
of efavirenz (Sustiva) plus<br />
emtricitabine/tenofovir. This<br />
time, however, it has been<br />
shown to maintain an undetectable<br />
viral load (of less<br />
than 50 copies/mL) in people<br />
who were switching from<br />
a Norvir-boosted protease<br />
inhibitor (PI) combination.<br />
<strong>The</strong>se were 24-week<br />
results in nearly 500 individuals,<br />
of whom two-thirds were<br />
switched to Complera and the<br />
rest maintained on their PI<br />
regimen. Overall total cholesterol,<br />
LDL (“bad cholesterol”),<br />
and triglycerides decreased<br />
to a greater extent among<br />
those switched than on those<br />
maintained on their PI. <strong>The</strong><br />
differences were statistically<br />
significant.<br />
“We all know that regimen<br />
simplification improves quality<br />
of life,” said Frank Palella, MD,<br />
of Northwestern University<br />
when he presented these<br />
results from the SPIRIT study.<br />
Also continuing to do<br />
well: the still investigational<br />
elvitegravir and dolutegravir,<br />
both integrase inhibitor medications<br />
(INSTIs). In 96-week<br />
results from Study 145, elvitegravir<br />
continued to be noninferior<br />
(as it was in earlier<br />
48-week results) to Isentress,<br />
the only INSTI currently on<br />
the market. Development of<br />
INSTI drug resistance was<br />
low (about 7%) and similar<br />
with both medications. <strong>The</strong><br />
700 participants in this study<br />
were treatment-experienced,<br />
so they were less likely to<br />
achieve undetectable viral<br />
load. Overall, 47.6% of the 351<br />
participants on dolutegravir<br />
had undetectable viral loads,<br />
compared to 45% of those on<br />
Isentress.<br />
In 48-week results from<br />
the SPRING-2 study, dolutegravir<br />
was as effective as<br />
Isentress, with 88% vs. 85% of<br />
participants in the two groups<br />
achieving undetectable viral<br />
load. <strong>The</strong> participants were<br />
treatment-naïve (first time<br />
on HIV therapy), See more<br />
dolutegravir news in Briefly.<br />
GETTInG A BOOST<br />
<strong>The</strong> investigational drug cobicistat<br />
(COBI), which boosts<br />
drug levels (a “pharmacoenhancer”),<br />
was given with<br />
Reyataz plus Truvada and<br />
compared to Norvir-boosted<br />
Reyataz plus Truvada, a<br />
preferred regimen under<br />
U.S. treatment guidelines. In<br />
Phase 3 study results after 48<br />
weeks, cobicistat-boosted<br />
reyataz was non-inferior<br />
to Norvir-boosted reyataz,<br />
with high rates of virologic<br />
success (viral loads of less<br />
than 50 copies per mL) and<br />
similar safety and tolerability.<br />
Nearly 700 individuals participated<br />
in Study 114.<br />
“Cobicistat appears to be<br />
an effective drug for boosting<br />
36 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
PHOTO: © iAS/RyAn RAyBuRn-COMMERCiAliMAgE.nET<br />
protease inhibitor levels,<br />
with greater potential for coformulation,”<br />
said presenter<br />
Joel Gallant, MD, MPH of<br />
Johns Hopkins University<br />
School of Medicine. He noted<br />
the various co-formulations<br />
of cobicistat with protease<br />
inhibitors that are in development.<br />
Moreover, he pointed<br />
out that, “[Norvir]-boosted<br />
Reyataz is known to be a<br />
lipid-friendly regimen and<br />
cobicistat is no different.”<br />
“This is all good news,”<br />
said session co-facilitator<br />
Christine Katlama, MD, of<br />
Hospitalier Pitie-Salpetriere in<br />
Paris, “because all the drugs<br />
work and when they don’t<br />
work t<strong>here</strong> is no resistance.”<br />
Risky business<br />
for sex workers<br />
Several sessions looked at<br />
abuses that put sex workers<br />
at risk for HIV—and we’re not<br />
talking sex.<br />
Instead, it’s police actions<br />
around the world—including<br />
<strong>here</strong> in the United States—to<br />
confiscate condoms and<br />
to use them as evidence<br />
of prostitution that puts<br />
sex workers at risk for HIV.<br />
Advocates<br />
said the situation is<br />
such that many sex<br />
workers are afraid<br />
to carry condoms<br />
because of the police<br />
harassment this can<br />
cause. In fact, even<br />
outreach workers<br />
have been followed<br />
by the police so that<br />
sex workers can be<br />
arrested when they<br />
take the condoms<br />
offered. As advocates<br />
pointed out, it is<br />
not illegal to carry<br />
condoms. Rather,<br />
confiscation serves as another<br />
avenue of illegal detention<br />
and intimidation.<br />
Moreover, criminalization<br />
of consensual sex work keeps<br />
workers under dangerous conditions.<br />
In the “Criminalizing<br />
Condoms and Sex Work”<br />
session, Acasia Shields, author<br />
of Criminalizing Condoms, a<br />
report from the Open Society<br />
Foundation, said, “Police<br />
routinely search sex workers<br />
to confiscate and destroy condoms.<br />
This affects their ability<br />
to practice safe sex and they<br />
know it.”<br />
Of the U.S. sex workers<br />
surveyed, 52% said they<br />
were afraid to carry condoms<br />
because of fear of police<br />
harassment. Shields said<br />
other abuses include<br />
threats of arrest to<br />
exhort sex,<br />
and beating<br />
or raping sex<br />
workers.<br />
Discussing<br />
the findings<br />
from the first<br />
national congress<br />
of sex workers in<br />
Bangladesh, Simon<br />
mY BOdY, mY BuSInESS: Discussing sex workers’ issues.<br />
Risen, MD, MPH, PhD, of Save<br />
the Children, said, “Violence<br />
against female sex workers<br />
spreads far beyond individual<br />
incidents and factually is gender-based<br />
violence.” Among<br />
other recommendations, Save<br />
the Children in Bangladesh<br />
says behavioral change campaigns<br />
should be aimed at<br />
changing community perceptions<br />
and creating acceptance<br />
of sex workers in mainstream<br />
society, and that maternal and<br />
child services should focus<br />
more on issues related to sex<br />
workers.<br />
Darby Hickey of the Los<br />
Angeles chapter of SWOP<br />
(Sex Workers Outreach<br />
Project), said, “We think<br />
sometimes that countries like<br />
the United States are a world<br />
apart from countries like<br />
Bangladesh, but unfortunately,<br />
we face the same issues.<br />
It is about law and about<br />
policy change, but also about<br />
how police operate outside<br />
the range of law. So we need<br />
to change policies, holding<br />
police accountable, and<br />
address the wider societal<br />
indifference and downright<br />
hostility.” She said efforts to<br />
“rescue and save” sex workers<br />
should be called “arrest<br />
and abuse.”<br />
In the session titled “<strong>The</strong><br />
Oldest Profession: Is Sex<br />
Work Work?,” Naomi Akers<br />
said equating sex work with<br />
human trafficking is insulting<br />
and hurts both sex workers,<br />
who are targeted by raids,<br />
and victims of trafficking,<br />
who aren’t helped at all.<br />
“When you’re doing sex work,<br />
of course you see it as work.<br />
It buys you food and helps<br />
you take care of your family,”<br />
she said, calling trafficking<br />
“horrible.”<br />
Deanna Kerrigan of the<br />
Johns Hopkins Bloomberg<br />
School of Public Health in<br />
Baltimore detailed findings<br />
of higher HIV risk among sex<br />
workers around the world, and<br />
said support for sex workers’<br />
groups, as well as human and<br />
health rights is critical for all<br />
sex workers, including men<br />
and transgender people.<br />
Labor rights, the focus of the<br />
session, would help to eliminate<br />
stigma and discrimination<br />
and increase HIV prevention<br />
efforts for this group of workers,<br />
she said. Richard Howard<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 37
COnfEREnCE uPdATE<br />
AIdS 2012<br />
washiNgtoN, d.c.<br />
of the International Labour<br />
Office (ILO) said, “Decent<br />
work [as outlined by ILO]<br />
should exist for all human<br />
beings, regardless of whether<br />
it’s legal or not, whether it<br />
takes place in a formal or<br />
informal environment.”<br />
Underscoring the human<br />
rights issues affecting sex<br />
workers were protests against<br />
the U.S. Consulate for denying<br />
them visas to attend the<br />
conference.<br />
In the final analysis, the<br />
sex workers movement advocates<br />
for decriminalization of<br />
sex work as the most important<br />
way of protecting their<br />
human rights.<br />
“<strong>The</strong> epidemic is not<br />
driven by the lack of a pill<br />
or a gadget, the epidemic is<br />
driven by repression,” said<br />
plenary speaker Cheryl Overs,<br />
Senior Research Fellow at<br />
the Michael Kirby Centre for<br />
Public Health and Human<br />
Rights at Monash University<br />
in Melbourne.<br />
She founded a sex workers’<br />
rights organization in<br />
Australia in the ‘80s and the<br />
Global Network of Sex Work<br />
Projects in the ‘90s. She has<br />
worked in HIV policy and programming<br />
for male, female,<br />
and transgender sex workers<br />
in more than 20 developing<br />
countries. “And that brings<br />
me to law and policy,” she<br />
continued. “Sex workers<br />
from Sweden to Singapore<br />
to Swaziland all say that the<br />
greatest threat to their health<br />
and human rights is the law<br />
that makes it impossible to<br />
find safe places to work, and<br />
prevents them from having<br />
the same protections as other<br />
workers and other citizens.”<br />
At the center of research<br />
A look behind the National institutes of Health<br />
story aNd photographs by rick guasco<br />
With an annual budget<br />
approaching $31 billion, the<br />
National Institutes of Health<br />
(NIH) is the medical research<br />
agency of the federal government<br />
and the largest source of<br />
funding in the world for medical<br />
research. the NiH is also<br />
a driving force behind AiDs<br />
and Hiv vaccine research;<br />
10% of the agency’s budget<br />
—$3 billion—goes toward<br />
HIV/AIDS, funding research<br />
conducted at academic, commercial,<br />
and private labs, as<br />
well as at NIH headquarters in<br />
Bethesda, Maryland.<br />
Some 75 buildings are<br />
scattered throughout the<br />
312-acre NIH campus. During<br />
the International AIDS<br />
Conference, the agency<br />
hosted a press tour of two<br />
of those buildings, offering a<br />
closer look at the role the NIH<br />
plays in clinical research and<br />
treatment.<br />
ThE VACCInE CEnTER<br />
Opened in 2000, the Vaccine<br />
Research Center is a five-story<br />
facility w<strong>here</strong> research is done<br />
to find vaccines not only for<br />
HIV, but for influenza, Ebola<br />
virus, and other diseases that<br />
pose global health risks.<br />
Gary J. Nabel, MD, PhD,<br />
director of the Vaccine<br />
Research Center, opened the<br />
tour, explaining how the facility<br />
serves as an “intellectual<br />
hub” by putting all the stages<br />
of vaccine research and<br />
development under one roof.<br />
Basic research is<br />
first conducted to find a<br />
promising vaccine candidate.<br />
A vaccine is of<br />
little use, however, if it<br />
can’t be efficiently and<br />
safely mass-produced,<br />
so it undergoes test<br />
production for good<br />
manufacturing practices<br />
and quality control.<br />
From t<strong>here</strong>, a successful<br />
candidate then goes<br />
to clinical trials to<br />
determine how safe it is<br />
for patient use. Results<br />
from the trials are<br />
reviewed in a series of<br />
assessments. If the vaccine<br />
candidate doesn’t<br />
pass this process with<br />
flying colors, it goes<br />
back to basic research,<br />
and the cycle begins<br />
again. <strong>The</strong> three-phase<br />
cycle can take 10–18 years<br />
for a would-be<br />
vaccine to complete.<br />
Nabel said that the search<br />
for a vaccine has been<br />
elusive, because, “HIV is constantly<br />
mutating, changing its<br />
genetic make-up and protein<br />
structure.”<br />
“HIV is a sugar-coated<br />
virus,” Nabel explained.<br />
Sugars produced by the body<br />
are converted into proteins by<br />
the virus. “This makes it invisible<br />
to the body’s immune<br />
system, which does not perceive<br />
the virus as a threat.”<br />
However, Nabel offered<br />
some perspective on the<br />
VACCInE ChIEf: <strong>The</strong> NIH’s Vaccine<br />
Research Center is headed by<br />
Dr. Gary J. Nabel.<br />
search for an HIV vaccine.<br />
Although it took 17 years to<br />
develop a vaccine against<br />
hepatitis B, he pointed out<br />
that a polio vaccine took<br />
45 years.<br />
“A vaccine is at least 10<br />
years into our future,” Nabel<br />
said. “What we’ve learned is<br />
that HIV is a very crafty virus.”<br />
While one or two vaccine<br />
candidates look promising, it<br />
will be at least until mid-2013<br />
before an assessment can be<br />
made, and a little longer to<br />
evaluate more mature data,<br />
Nabel said. Even if a vaccine<br />
38 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
were discovered today, it<br />
would take at least four years<br />
of additional testing and evaluation<br />
before it could become<br />
publicly available.<br />
ThE CLInICAL<br />
RESEARCh CEnTER<br />
Next stop on the tour was<br />
the Mark O. Hatfield Clinical<br />
Research Center, a hospital<br />
w<strong>here</strong> 1,500 clinical trials for<br />
a variety of illnesses (including<br />
HIV/AIDS) are conducted.<br />
Opened in 2005, the Hatfield<br />
Clinical Research Center is<br />
connected to the Warren<br />
Grant Magnuson Clinical<br />
Center, built in 1953, to form<br />
the largest hospital in the U.S.<br />
dedicated to clinical research.<br />
<strong>The</strong> Clinical Research<br />
Center has spawned numerous<br />
treatments, from the<br />
first pediatric chemotherapy<br />
to development of AZT,<br />
the first anti-HIV drug. <strong>The</strong><br />
center houses an HIV clinic<br />
that treats 500 patients, only<br />
one or two of whom are ever<br />
in-patients.<br />
Dr. Henry Masur is the<br />
research center’s Director of<br />
Critical Care Medicine, but has<br />
focused the major part of his<br />
career on HIV and its associated<br />
complications. Although<br />
a research institution, Masur<br />
said the clinic recognizes the<br />
importance of keeping HIVpositive<br />
patients connected<br />
to care. That’s why while<br />
half the clinic’s nursing staff<br />
is in research, the other half<br />
of the nurses are also case<br />
managers.<br />
Hepatitis C is a major concern<br />
for people who are HIVpositive,<br />
Masur said. T<strong>here</strong><br />
are 3–5 million people who<br />
have hep C out of 314 million<br />
Americans. While the current<br />
standard of care for hepatitis<br />
C can sometimes be difficult<br />
to tolerate and only helps to<br />
clear the virus in about onethird<br />
to one-half of patients,<br />
recent advances have raised<br />
the cure rate to 75% and<br />
higher. Masur said advances<br />
in treatment look even more<br />
promising, comparing them to<br />
the advent of protease inhibitors<br />
and combination therapy<br />
for HIV that came in 1995.<br />
As people are now living<br />
longer with HIV, Masur said<br />
the research center is beginning<br />
to look at aging and<br />
other complications. “We’ll<br />
soon be examining neurocognitive<br />
issues,” he said.<br />
“Beyond anecdotally, does it<br />
happen, and if so, what can<br />
we do to reverse it?”<br />
“Knowledge is bi-directional,”<br />
Masur said. “What<br />
we learn in the lab will help<br />
patients. But t<strong>here</strong> is a lot we<br />
can learn from patients and<br />
put to use.”<br />
CLInICAL CARE: Dr. Henry Masur (above) introduces Senora<br />
Mitchell, a medical clerk who has been with the Hatfield Clinical<br />
Research Center’s HIV clinic since 1987. “I love my work,” Mitchell<br />
said. “I get to make a difference every day.”<br />
mOdEST ACCOmmOdATIOnS: You might expect that an<br />
examination room in the most prominent medical research<br />
hospital in the country, if not the world, would look better than<br />
this. But Masur noted that taxpayers pay for NIH facilities, so the<br />
exam room looks the same as at any other doctor’s office.<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 39
ScEnES<br />
FROm<br />
A WEEk<br />
THAT WAS<br />
words & images<br />
by rick guasco<br />
BEYonD THE HEaDLInEmaking<br />
sessions of<br />
the International AIDS<br />
Conference, t<strong>here</strong> was much to<br />
see and do inside and away from<br />
Washington, D.C.’s convention<br />
center. “What would an AIDS<br />
conference be without a little<br />
protesting?” said an unflappable<br />
Secretary of State Hilary Clinton<br />
as a small group of demonstrators<br />
rose and chanted when she took<br />
the stage on opening day.<br />
During a panel discussion<br />
addressing the efficiency of<br />
overseas anti-AIDS efforts, Bill<br />
Gates spoke candidly: “<strong>The</strong><br />
amount of money we have [now]<br />
is not enough to treat everyone.<br />
We’re in a period of incredible<br />
uncertainty about how much this<br />
funding will stay strong. Even the<br />
uncertainty creates instability in<br />
how the investment ahead will<br />
be made. <strong>The</strong> voices of the AIDS<br />
community are going to have to<br />
be louder than ever.”<br />
<strong>The</strong> week of the conference<br />
offered opportunities to honor<br />
the fallen and plea for the living.<br />
Visitors to the AIDS Memorial<br />
Quilt, displayed on the Mall, could<br />
not only see the panels, but also<br />
recite the names of those memorialized<br />
by the Quilt.<br />
In the streets, approximately<br />
1,000 marchers took their messages<br />
to the White House.<br />
Discordant voices—demonstrating<br />
for sex workers’ rights, against<br />
Wall Street, opposing HIV criminalization<br />
laws—were united by<br />
one refrain, “cure AIDS now.”<br />
40 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM
the mirror haS<br />
tWo faceS<br />
A personal account of using facial filler for lipoatrophy<br />
by Jeff berry<br />
eVER SIncE IT FIRST BEgan aPPEaRIng wITH<br />
some regularity in people with HIV in the mid 1990’s,<br />
lipoatrophy has earned its well deserved reputation<br />
as the Scarlet Letter of HIV, also known as “the look.”<br />
Lipoatrophy is the loss of subcutaneous fat under the skin, most<br />
notably in the face, but also in the butt, arms, and legs, and is<br />
thought to be part of a larger syndrome called lipodystrophy,<br />
which is the redistribution of fat in the body and can include buffalo<br />
hump, enlarged breasts, and visceral fat in the abdomen.<br />
It can sometimes be extremely disfiguring,<br />
and almost always causes some level<br />
of emotional distress, even depression,<br />
and oftentimes self-imposed isolation in<br />
those who suffer from its stigmatizing<br />
effects. It can also affect ad<strong>here</strong>nce to HIV<br />
medications, and deter people from starting<br />
treatment in the first place.<br />
<strong>The</strong> cause of lipoatrophy has been<br />
linked to certain HIV medications, most<br />
notably d4T (Zerit, stavudine) and to a lesser<br />
extent AZT (Retrovir, zidovudine) and<br />
ddI (Videx, didanosine); other HIV meds,<br />
including some protease inhibitors; and it<br />
has also been linked to HIV itself. D4T is<br />
rarely prescribed in the U.S. anymore, but is<br />
still widely used in many developing countries<br />
due to its availability and low cost.<br />
While we don’t see as many new cases of<br />
lipoatrophy <strong>here</strong> in the U.S. with those who<br />
have since initiated therapy using newer<br />
and less-toxic antiretrovirals, it is still prevalent<br />
among those using d4T in developing<br />
countries, although d4T continues to fall<br />
out of favor with providers and is used less<br />
and less as more and newer drugs become<br />
available in those regions.<br />
For those who have been treated with<br />
some of these older, more toxic drugs<br />
(when that was all that was available),<br />
many have developed the sunken cheeks,<br />
veiny arms and legs, and loss of fat in the<br />
butt to the point w<strong>here</strong> it is uncomfortable<br />
to sit for more than a short period of time.<br />
Once you discontinue taking a drug like<br />
d4T, you can sometimes stop the lipoatrophy<br />
from progressing any further, but it<br />
can take a long time to see any reversal of<br />
its effects, if ever, so some people will turn<br />
to using facial fillers to replace the fat in<br />
the face that has been lost.<br />
I have written several articles in the<br />
past, for both PoSITIVELY awaRE and<br />
<strong>The</strong><strong>Body</strong>.com, about my experiences<br />
dealing with the physical and emotional<br />
aspects of having lipoatrophy and its<br />
stigmatizing effects, as well as my experience<br />
using a facial filler, Sculptra (known<br />
then as New-Fill) back in 2001. <strong>The</strong> results<br />
I saw in 2001 were only moderate, and<br />
disappeared within about six months to<br />
a year, mainly due to the fact that I only<br />
received two treatments because that was<br />
all that I could afford.<br />
In THE FaLL oF LaST YEaR, I<br />
decided to revisit the idea of receiving<br />
another round of facial filler<br />
treatments, and I went to see Dr. Dan<br />
Berger of Northstar Medical Center in<br />
Chicago for a consultation. Dr. Berger, who<br />
also writes for PoSITIVELY awaRE, and<br />
has over 12 years of experience providing<br />
Sculptra, recommended that I undergo<br />
five or six “sessions” due to the level of<br />
facial lipoatrophy that I had. Facial lipoatrophy<br />
is graded on a scale of 1 to 5, with 1<br />
being mild, and 5 being severe—mine was<br />
severe, between grade 4 and 5. During<br />
each session, I was to receive injections of<br />
two vials, or one “kit” of Sculptra, one vial<br />
for each side of my face.<br />
Sculptra, or injectable poly-L-lactic<br />
acid, is one of only two FDA approved<br />
treatments in the U.S. for HIV-associated<br />
facial lipoatrophy, the other being<br />
Radiesse. Both of these injectables work<br />
by being absorbed into the body and<br />
stimulating the growth of the body’s own<br />
collagen, so they are not permanent fillers.<br />
T<strong>here</strong> are other fillers available (see<br />
table, page 43) that are also used for<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 41
FAcE On: Berry before his initial treatment, and three months after the sixth and last session.<br />
facial lipoatrophy, but they are permanent<br />
and can sometimes cause serious side<br />
effects and allergic reactions (as can both<br />
Sculptra and Radiesse). Only one is FDA<br />
approved (Silikon 1000) and none are<br />
approved for use in HIV. Anecdotally, I’ve<br />
heard of people who have used them and<br />
are pleased with their results, but personally<br />
I did not want to use something that<br />
was going to be permanent.<br />
I felt comfortable using Sculptra because<br />
I had used it before and I already knew what<br />
to expect, but also because I would be getting<br />
six treatments instead of two, so I was<br />
hoping to experience better results this time<br />
around. Plus, as Dr. Berger explained it, after<br />
getting six treatments, my face would never<br />
go back to the way it was before receiving<br />
Sculptra, and I would only require a “touchup”<br />
session once a year.<br />
<strong>The</strong> cost of Sculptra is expensive, running<br />
about $1,700 for one kit (two vials),<br />
or $850 per 367.5 mg vial, which also<br />
includes the cost for the session—doctor,<br />
time, and procedure. Most insurance<br />
companies still consider its use to be a<br />
cosmetic treatment and are t<strong>here</strong>fore<br />
likely to refuse to cover the drug as well as<br />
the procedure. However, if you are initially<br />
denied, you should appeal and see if you<br />
can get them to recognize it as a medical<br />
necessity (which it really is). Recognizing<br />
the high cost and lack of coverage by most<br />
plans, and the great need of those who<br />
have this condition, the manufacturer created<br />
a patient assistance program (PAP)<br />
for people with HIV that assists in helping<br />
to pay for Sculptra. However, a new<br />
company (Valeant) recently took over the<br />
PAP, and it now only covers those with up<br />
to $61,940 in annual income, and provides<br />
just two kits plus one follow up kit after a<br />
two-year period. Under the PAP Sculptra is<br />
free for those with an annual income less<br />
than 200% of the Federal Povery Level<br />
($22,340 for an individual, slightly higher<br />
based on family size and in Alaska and<br />
Hawaii), and then on a sliding scale above<br />
this amount and up to $61,940. <strong>The</strong> staff<br />
at Northstar was very helpful in getting<br />
me set up with the PAP, and in November<br />
of 2011 I received my first treatment.<br />
IT IS VERY ImPoRTanT THaT THE<br />
physician who is performing the procedure<br />
be trained specifically in the<br />
use of Sculptra and how to properly<br />
inject it, which requires a certain threading,<br />
or tunneling, technique. According to the<br />
package label, “during the first injection<br />
session with Sculptra, only a limited correction<br />
should be made. <strong>The</strong> contour deficiency<br />
should be under-corrected, never<br />
fully corrected or overcorrected (overfilled)<br />
during any injection session. Re-evaluate<br />
the patient no sooner than two weeks after<br />
the injection session to determine if additional<br />
correction is needed.”<br />
Each session only takes around 40-45<br />
minutes, and it would begin with Dr.<br />
Berger marking my face with a white<br />
pencil to guide him while injecting the<br />
Sculptra. Starting with ice packs on my<br />
face to minimize the swelling, and then<br />
a local anesthetic to numb my face, he<br />
would begin injecting the filler into different<br />
areas of my face, using his hands<br />
to help “move” the filler into place once it<br />
was injected. Even with the local anesthetic,<br />
I experienced a good deal of discomfort<br />
when the needles went in and he tunneled,<br />
especially during the first couple of sessions<br />
when t<strong>here</strong> was little fat in my face<br />
for him to work with. But the discomfort<br />
was only temporary, and when the session<br />
was over, I was left with some temporary<br />
swelling, a few marks, and on occasion,<br />
some slight bruising, but the swelling went<br />
down in a few hours and any marks or<br />
bruising were gone within a day or two.<br />
Following each session, and according<br />
to the package label, I was to “massage in<br />
a circular fashion the treated areas for five<br />
minutes, five times per day for five days,”<br />
in an effort to stimulate collagen growth<br />
and “even out” the facial filler under my<br />
42 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM<br />
“AfTER” PHOTO: CHRiS KnigHT
SOuRCE: fACiAlwASTing.ORg<br />
FAcE OFF: Commonly used options for HIV-related facial lipoatrophy<br />
PRoDUcT TYPE/SESSIonS aPPRoVED? coST<br />
Sculptra<br />
Poly-L-lactic acid<br />
Radiesse<br />
Calcium hydroxylapatite<br />
(CaHA) microsp<strong>here</strong>s<br />
Silikon 1000<br />
Microdroplets<br />
Bioalcamid<br />
Polyalkylimide gel<br />
pMMA<br />
Polymethylmethacrylate<br />
skin. I went back for five more sessions,<br />
one every four weeks.<br />
Non-permanent;<br />
3–7 or more sessions<br />
needed.<br />
Non-permanent;<br />
2–3 or more sessions<br />
needed.<br />
Permanent;<br />
4–6 or more sessions<br />
needed.<br />
Permanent;<br />
1–2 sessions needed.<br />
Permanent;<br />
1–2 sessions needed.<br />
PaTIEnTS aRE aDVISED THaT<br />
after the initial treatment and<br />
within a week the effects will<br />
completely disappear, and the<br />
contour of the face returns to how it was<br />
before. With each subsequent session,<br />
however, you begin to see the cumulative<br />
benefit of each successive treatment, and<br />
the effects are more noticeable and last<br />
longer. By the third or fourth treatment, I<br />
was really looking more and more like my<br />
old self, and couldn’t wait for each following<br />
treatment, pain or no pain!<br />
Treatment advocate Nelson Vergel<br />
warns that not everyone experiences the<br />
same level of results. “Some people in my<br />
online discussion group, especially those<br />
with moderate to more advanced cases of<br />
facial lipoatrophy, have complained of poor<br />
response with Sculptra after spending a few<br />
thousand dollars for several sessions that<br />
did not end up restoring their faces.” Vergel,<br />
founder of FacialWasting.org and pozhealth<br />
at yahoogroups.com, says that some of<br />
them end up getting silicone microdroplets<br />
in the U.S. or flying to Mexico to get permanent<br />
options like PMMA (see table, above).<br />
FDA approved. Patient Assistance for product only<br />
(under $61,940 yearly income):<br />
www.needymeds.org/papforms/<br />
sculpt1039.pdf. Labor cost average<br />
$400 per session. Full price: $1,100<br />
per session for product.<br />
FDA approved. Patient Assistance available: www.<br />
radiesse-fl.com/Physician-section/<br />
Patient-access-program/<br />
Full price: $1,200 per session.<br />
Off-label use; FDA approved for<br />
intraocular injections to treat<br />
CMV-related retinal detachment.<br />
Not FDA approved. Available in<br />
Canada, Mexico, and Europe.<br />
Not FDA approved. Available in<br />
Mexico and Brazil. American version<br />
Artefil is too expensive for<br />
the amount required.<br />
Of course, nothing is perfect, and t<strong>here</strong><br />
are side effects associated with Sculptra.<br />
<strong>The</strong> most common side effects reported<br />
in studies are bruising, swelling, discomfort,<br />
and rash, but these typically resolve<br />
within a few days to a few weeks. T<strong>here</strong> is<br />
a “device-related adverse event” called an<br />
injection site subcutaneous papule, which<br />
is a small lump or bump under the skin, the<br />
onset of which can occur anyw<strong>here</strong> from<br />
a few weeks to a few years afterward. I<br />
experienced several of these lumps, one<br />
under my left eye, and two under my<br />
right temple (sometimes if you get these<br />
papules you can feel them under your<br />
skin, but they are barely noticeable—other<br />
times they can be more visible). T<strong>here</strong> are<br />
also more serious adverse events that can<br />
potentially occur, so be sure to read the<br />
full package label.<br />
In THE EnD, FoR mE THE FEw<br />
small lumps, the cost of treatment,<br />
and the pain were all a small price to<br />
pay for what it has ultimately done for<br />
my self-esteem. I feel better about myself<br />
overall, because I look healthier. <strong>The</strong> effect<br />
for me was subtle, most people didn’t really<br />
notice or say anything, other than “you look<br />
rested” or “you look really great!”<br />
No Patient Assistance Program.<br />
$400–800 per session, depending on<br />
the physician.<br />
$4,500 average total. Two sessions.<br />
Infections reported after 3–4 years.<br />
$2,000 average cost for total reconstruction.<br />
Patient assistance in Tijuana:<br />
www.MedicalPMMA.com<br />
I realize that I am very lucky to have a<br />
decent-paying job that has afforded me the<br />
ability to benefit from this treatment, and<br />
that many others are not as fortunate. I also<br />
realize that even though the HIV treatments<br />
available today are much less likely to<br />
cause facial lipoatrophy (if at all), the fear<br />
of developing facial lipoatrophy still may<br />
deter some people from ever starting treatment,<br />
or may cause those who are on treatment<br />
to be less than fully ad<strong>here</strong>nt to their<br />
regimen. While Medicare finally agreed to<br />
cover the procedure a few years ago, the<br />
amount that they reimburse is well below<br />
what providers charge. That is why I plan to<br />
continue to advocate for insurance companies,<br />
Medicare, and Medicaid to cover this<br />
procedure at a reasonable amount, much<br />
in the same way that breast reconstruction<br />
is provided to women with breast cancer<br />
who have undergone a mastectomy. <strong>The</strong><br />
benefit of these treatments is vital to the<br />
psychological well-being and quality of life<br />
for so many people living with HIV who are<br />
affected by this condition.<br />
go to www.sculptra.us for more<br />
information. For a list of providers trained<br />
in the use of Sculptra, visit www.sculptraaesthetic.com.<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 43
SEARCh<br />
fOR An hIV<br />
SPECIALIST<br />
Finding an Hiv<br />
specialist<br />
is easy with<br />
AAHivM’s<br />
referral link:<br />
www.aahivm.org.<br />
enter your ZiP<br />
code on the<br />
home page,<br />
and click<br />
on the “Go”<br />
button for<br />
a list of Hiv<br />
specialists<br />
near you.<br />
ASk ThE hIV SPECIALIST<br />
HELEn c. koEnIg, mD, mPH<br />
Safe sex is<br />
for seniors, too<br />
Q:<br />
i am a 65-year-old womaN.<br />
I lost my husband six years ago and<br />
have finally decided to enter the dating<br />
world again. My friends have convinced<br />
me to go on a cruise especially for single seniors,<br />
but my daughter is giving me all kinds of warnings<br />
about sexually transmitted diseases and HIV. HIV didn’t<br />
even exist back when I first became sexually active.<br />
Seriously, how great is my risk of contracting such<br />
diseases? After all, we are all going to be senior citizens<br />
and I’m not going on this cruise intending to “hook up”<br />
(as they say). Is all this safe sex stuff really necessary?<br />
A:<br />
as you head for the suN,<br />
the all-you-can-eat buffets, and the<br />
cruise festivities, don’t forget to pack<br />
some condoms with your sun block.<br />
While the risk of bringing home HIV or another sexually<br />
transmitted infection (STI) is not high, it’s not zero<br />
either. You are joining a growing population of women<br />
who are sexually active in their 60s and 70s and, unfortunately<br />
seeing a higher rate of STIs than ever before.<br />
What really is your risk of acquiring an STI? This<br />
depends entirely on the partner or partners with whom<br />
you choose to be sexually active, what type of sex you<br />
choose to have (oral, vaginal, or anal) and whether<br />
you choose to use protection or not. You have no way<br />
of knowing the sexual history of the men you’ll meet<br />
or their risk of having an STI. Studies have shown that<br />
even doctors, after taking a complete sexual history in<br />
a medical setting, are still terrible at predicting whether<br />
someone has HIV. Your prospective partners may<br />
not know they have STIs, as many can be present for<br />
months or years without symptoms, including HIV.<br />
Women who have been in a monogamous relationship<br />
for the last 20 or 30 years, or for whom sex hasn’t<br />
been an issue, may find it difficult to think about buying<br />
and asking their partner to use condoms. But <strong>here</strong> are<br />
some good reasons to brave that aisle at the drug store<br />
before you hit the high seas, as well as empowering<br />
yourself enough to make sure they’re used:<br />
44 SEPTEMBER+OCTOBER 2012 POSiTivElyAwARE.COM<br />
n<br />
3,500 women over age 45 were diagnosed with<br />
AIDS in 2009. People over the age of 50 now<br />
account for 15% of new HIV/AIDS diagnoses, and<br />
over 35% of all deaths from AIDS.<br />
n <strong>The</strong> highest percentage of trichomoniasis (a parasitic<br />
infection, considered the most common curable STI)<br />
is now actually in women over 50. Also on the menu<br />
are syphilis, gonorrhea, chlamydia, hepatitis B and C,<br />
herpes, and human papilloma virus.<br />
n Postmenopausal women are at a particularly high<br />
risk of acquiring HIV and other STIs because the<br />
vaginal wall is thinner as a result of lower estrogen<br />
levels and the immune system is not as strong as it<br />
used to be.<br />
You can’t control the risk of STIs in your partners,<br />
but you can control the risk of bringing one home<br />
yourself with correct condom use. Perhaps you think it’s<br />
“the man’s job” to come prepared with protection, but<br />
I encourage you to bring your own as backup! Chances<br />
are, the condom colors, flavors, and textures out t<strong>here</strong><br />
have changed a bit since you last looked. Lubricants<br />
now also come in wider varieties and are important<br />
if you experience vaginal dryness, both for your own<br />
comfort and to prevent condoms from tearing. So pack<br />
some protection and enjoy the festivities ahead!<br />
illuSTRATiOn © KARlKOTASinC
PHOTO: CHERyl MAnn<br />
WhOLISTIC PICTuRE<br />
SUE SaLTmaRSH<br />
Battle of the sexes?<br />
with all the evideNce that t<strong>here</strong> is iNdeed<br />
a “war on women” being waged by “conservatives,”<br />
it’s hard not to feel a “feministic” response. I am not a<br />
feminist. But I am also not in favor of any woman being<br />
forced to have a child she cannot support financially,<br />
emotionally, physically, or spiritually, just as no man<br />
should be forced into fatherhood that he doesn’t want<br />
and can’t do well.<br />
But I digress. Some feminists have been heard to<br />
say that no man would be <strong>here</strong> without his mother’s<br />
body having created him. I have to wonder how they<br />
could have missed the fact that a man (the sperm had<br />
to come from one of them, after all) was also involved<br />
in that creation. But then, I thought, couldn’t such<br />
biological criteria be used to argue the case for the<br />
opposite side of every agenda? Women have testosterone<br />
too and yet the number of female-only causes<br />
far outweighs male-only ones. At this stage of human<br />
history, I doubt that t<strong>here</strong> is any black or white person<br />
who doesn’t carry a gene inherited from an ancestor of<br />
the other color and yet we have racism from both sides.<br />
And, as I’ve said before, aren’t people who develop<br />
cancer after years of chain smoking just as deserving of<br />
the medical care and treatment they need to survive as<br />
people who acquire HIV after years of unprotected sex<br />
with multiple partners?<br />
When feminists angrily accuse me of misogyny, I<br />
stand by my belief that BOTH sexes are as valuable and<br />
as worthy of living as the other. And yet, if a man published<br />
a calendar called “How is a jar of Vaseline better<br />
than a woman?” I’ve no doubt he would be verbally castrated<br />
by the very women who publish “How is a cucumber<br />
better than a man?” And, by the way, the word for<br />
the female equivalent of misogyny, misandry, rarely sees<br />
the light of day, though both obviously exist in full force.<br />
I have frequently been amazed by the number of<br />
commercials on PBS and other progressive media<br />
sources that tout the urgent need to get more girls to<br />
become scientists, engineers, and mathematicians.<br />
What about the boys who are truly, innately passionate<br />
about math and science? And w<strong>here</strong> are the commercials<br />
urging more boys to become nurses, teachers, and<br />
dancers? Fact is that each sex has natural tendencies<br />
and the problem is not in getting<br />
people to go against those natural<br />
leanings, but in the rest of us<br />
accepting whatever choices they<br />
make. As a former girl, I can tell you<br />
that t<strong>here</strong> is nothing on Earth that<br />
could’ve induced me to become a<br />
scientist, engineer, or mathematician.<br />
Why should I have been forced<br />
into a field I had no interest in? Why<br />
should any boy be forced to take<br />
Home Ec over Shop, to play the flute instead of football,<br />
or vice versa against his own interest?<br />
Throughout history, t<strong>here</strong> have been courageous<br />
activists of both sexes fighting for things that were<br />
good for everybody. Without Elizabeth Cady Stanton<br />
and Susan B. Anthony, the issue of women voting might<br />
never have come to the forefront, but it took 56 men in<br />
Congress to pass the amendment that gave women the<br />
right to vote. Rosa Parks and Martin Luther King were<br />
both crucial to the civil rights movement, but it was<br />
Lyndon Johnson, a white guy from Texas, who made it<br />
the law of the land.<br />
We need to stop putting each other in neat little<br />
boxes. People—every sex, every race, every religion,<br />
every size, every age, with every illness—have to decide<br />
for themselves what’s worth fighting for in this lifetime.<br />
Since 2009, we’ve had a lot of people, many who call<br />
themselves Christians and/or Republicans, deciding<br />
that the only thing worth fighting for is whatever goes<br />
against everyone who doesn’t look, believe, or act<br />
like them. But now we also have more, including some<br />
Christians/Republicans, waking up, shaking off complacency,<br />
and standing together in all their glorious varieties<br />
to fight for justice, equality, and the things that are<br />
best for the Whole.<br />
“Men should be advocates for all and not just their<br />
own gender!” feminists stridently shout. Shouldn’t<br />
women? Shouldn’t we all? Regardless of the composition<br />
of our chromosomes, we are all human. None of us<br />
would be <strong>here</strong> without the contributions of both male<br />
and female. So I propose we stop being “feminists” or<br />
“masculinists” (See? not even a word for it!) and do our<br />
best to become humanists.<br />
Breathe deep. Live Long.<br />
we need to<br />
stop putting<br />
each<br />
other in neat<br />
little boxes.<br />
regardless<br />
of the composition<br />
of<br />
our chromosomes,<br />
we are all<br />
human.<br />
POSiTivElyAwARE.COM SEPTEMBER+OCTOBER 2012 45
On September 21,<br />
take your best shot<br />
against HIV.<br />
a day with hiv<br />
Whether we’re positive or negative, we are all affected by HIV. Take your best shot<br />
against HIV/AIDS—take part in A Day with HIV, the HIV awareness and anti-stigma<br />
campaign presented by PoSITIVELY awaRE. On Sept. 21, use your smartphone or digital<br />
camera and take a snapshot of a moment of your life. Upload your picture and story to<br />
ADaywithHIV.com or email them to photo@adaywithhiv.com. Select<br />
pictures will appear in a special section of the November+December<br />
issue of PoSITIVELY awaRE. Additional pictures will be featured on<br />
ADayWithHIV.com.<br />
GET In ThE PICTuRE.<br />
aDaywithHIV.com