Monitoring Hydration Status in Our Clients - Canadian Association of ...
Monitoring Hydration Status in Our Clients - Canadian Association of ...
Monitoring Hydration Status in Our Clients - Canadian Association of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Parameters <strong>of</strong> <strong>Hydration</strong> <strong>Status</strong><br />
A client’s hydration status can be measured via several<br />
parameters.<br />
Weight—mild to severe dehydration can manifest as a<br />
rapid five to over 10 per cent loss <strong>in</strong> body weight.<br />
Blood pressure—low blood pressure or orthostatic<br />
hypotension (a rapid drop <strong>in</strong> blood pressure when<br />
go<strong>in</strong>g from ly<strong>in</strong>g to sitt<strong>in</strong>g or from sitt<strong>in</strong>g to stand<strong>in</strong>g)<br />
may <strong>in</strong>dicate dehydration.<br />
Ur<strong>in</strong>e output—a reduction <strong>in</strong> ur<strong>in</strong>e production from typical<br />
volumes generally <strong>in</strong>dicates a decrease <strong>in</strong> fluid <strong>in</strong>take.<br />
BUN:serum creat<strong>in</strong><strong>in</strong>e ratio—an elevated blood<br />
urea nitrogen (BUN) level with a normal or low serum<br />
creat<strong>in</strong><strong>in</strong>e level may <strong>in</strong>dicate under-hydration; however,<br />
an elevated BUN alone may not be an accurate <strong>in</strong>dicator<br />
<strong>of</strong> hydration status, especially <strong>in</strong> clients with renal<br />
impairment. A BUN: serum creat<strong>in</strong><strong>in</strong>e ratio greater than<br />
20:1 is a red flag for dehydration.<br />
Serum sodium—an elevated serum sodium level may<br />
<strong>in</strong>dicate dehydration; however, because other factors<br />
may impact the serum sodium level this should not<br />
be used alone to identify dehydration.<br />
When dehydration has been identified and a rehydration<br />
plan has been <strong>in</strong>itiated, it is important to<br />
monitor the client’s alertness, ur<strong>in</strong>e output, blood<br />
pressure, pulse and daily weight.<br />
Consequences <strong>of</strong> Dehydration<br />
Dehydration is one <strong>of</strong> the most common nutritionrelated<br />
problems <strong>in</strong> long-term care; it can be life<br />
threaten<strong>in</strong>g and may result <strong>in</strong> the follow<strong>in</strong>g:<br />
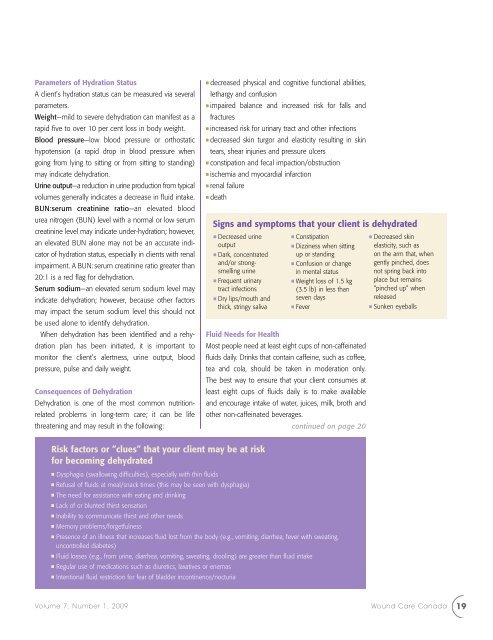
Risk factors or “clues” that your client may be at risk<br />
for becom<strong>in</strong>g dehydrated<br />
■ decreased physical and cognitive functional abilities,<br />
lethargy and confusion<br />
■ impaired balance and <strong>in</strong>creased risk for falls and<br />
fractures<br />
■ <strong>in</strong>creased risk for ur<strong>in</strong>ary tract and other <strong>in</strong>fections<br />
■ decreased sk<strong>in</strong> turgor and elasticity result<strong>in</strong>g <strong>in</strong> sk<strong>in</strong><br />
tears, shear <strong>in</strong>juries and pressure ulcers<br />
■ constipation and fecal impaction/obstruction<br />
■ ischemia and myocardial <strong>in</strong>farction<br />
■ renal failure<br />
■ death<br />
Signs and symptoms that your client is dehydrated<br />
■ Decreased ur<strong>in</strong>e<br />
output<br />
■ Dark, concentrated<br />
and/or strongsmell<strong>in</strong>g<br />
ur<strong>in</strong>e<br />
■ Frequent ur<strong>in</strong>ary<br />
tract <strong>in</strong>fections<br />
■ Dry lips/mouth and<br />
thick, str<strong>in</strong>gy saliva<br />
■ Constipation<br />
■ Dizz<strong>in</strong>ess when sitt<strong>in</strong>g<br />
up or stand<strong>in</strong>g<br />
■ Confusion or change<br />
<strong>in</strong> mental status<br />
■ Weight loss <strong>of</strong> 1.5 kg<br />
(3.5 lb) <strong>in</strong> less than<br />
seven days<br />
■ Fever<br />
Fluid Needs for Health<br />
Most people need at least eight cups <strong>of</strong> non-caffe<strong>in</strong>ated<br />
fluids daily. Dr<strong>in</strong>ks that conta<strong>in</strong> caffe<strong>in</strong>e, such as c<strong>of</strong>fee,<br />
tea and cola, should be taken <strong>in</strong> moderation only.<br />
The best way to ensure that your client consumes at<br />
least eight cups <strong>of</strong> fluids daily is to make available<br />
and encourage <strong>in</strong>take <strong>of</strong> water, juices, milk, broth and<br />
other non-caffe<strong>in</strong>ated beverages.<br />
cont<strong>in</strong>ued on page 20<br />
■ Dysphagia (swallow<strong>in</strong>g difficulties), especially with th<strong>in</strong> fluids<br />
■ Refusal <strong>of</strong> fluids at meal/snack times (this may be seen with dysphagia)<br />
■ The need for assistance with eat<strong>in</strong>g and dr<strong>in</strong>k<strong>in</strong>g<br />
■ Lack <strong>of</strong> or blunted thirst sensation<br />
■ Inability to communicate thirst and other needs<br />
■ Memory problems/forgetfulness<br />
■ Presence <strong>of</strong> an illness that <strong>in</strong>creases fluid lost from the body (e.g., vomit<strong>in</strong>g, diarrhea, fever with sweat<strong>in</strong>g,<br />
uncontrolled diabetes)<br />
■ Fluid losses (e.g., from ur<strong>in</strong>e, diarrhea, vomit<strong>in</strong>g, sweat<strong>in</strong>g, drool<strong>in</strong>g) are greater than fluid <strong>in</strong>take<br />
■ Regular use <strong>of</strong> medications such as diuretics, laxatives or enemas<br />
■ Intentional fluid restriction for fear <strong>of</strong> bladder <strong>in</strong>cont<strong>in</strong>ence/nocturia<br />
■ Decreased sk<strong>in</strong><br />
elasticity, such as<br />
on the arm that, when<br />
gently p<strong>in</strong>ched, does<br />
not spr<strong>in</strong>g back <strong>in</strong>to<br />
place but rema<strong>in</strong>s<br />
“p<strong>in</strong>ched up” when<br />
released<br />
■ Sunken eyeballs<br />
Volume 7, Number 1, 2009 Wound Care Canada<br />
19