Computerized Method of Visual Acuity Testing - University of Arizona
Computerized Method of Visual Acuity Testing - University of Arizona
Computerized Method of Visual Acuity Testing - University of Arizona
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
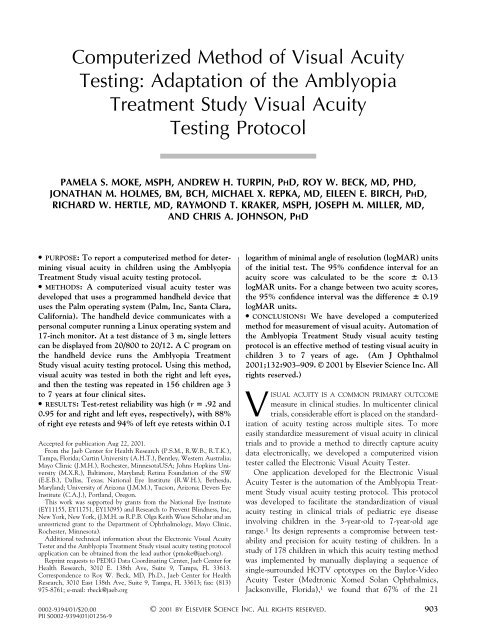
<strong>Computerized</strong> <strong>Method</strong> <strong>of</strong> <strong>Visual</strong> <strong>Acuity</strong><br />
<strong>Testing</strong>: Adaptation <strong>of</strong> the Amblyopia<br />
Treatment Study <strong>Visual</strong> <strong>Acuity</strong><br />
<strong>Testing</strong> Protocol<br />
PAMELA S. MOKE, MSPH, ANDREW H. TURPIN, PHD, ROY W. BECK, MD, PHD,<br />
JONATHAN M. HOLMES, BM, BCH, MICHAEL X. REPKA, MD, EILEEN E. BIRCH, PHD,<br />
RICHARD W. HERTLE, MD, RAYMOND T. KRAKER, MSPH, JOSEPH M. MILLER, MD,<br />
AND CHRIS A. JOHNSON, PHD<br />
● PURPOSE: To report a computerized method for determining<br />
visual acuity in children using the Amblyopia<br />
Treatment Study visual acuity testing protocol.<br />
● METHODS: A computerized visual acuity tester was<br />
developed that uses a programmed handheld device that<br />
uses the Palm operating system (Palm, Inc, Santa Clara,<br />
California). The handheld device communicates with a<br />
personal computer running a Linux operating system and<br />
17-inch monitor. At a test distance <strong>of</strong> 3 m, single letters<br />
can be displayed from 20/800 to 20/12. A C program on<br />
the handheld device runs the Amblyopia Treatment<br />
Study visual acuity testing protocol. Using this method,<br />
visual acuity was tested in both the right and left eyes,<br />
and then the testing was repeated in 156 children age 3<br />
to 7 years at four clinical sites.<br />
● RESULTS: Test-retest reliability was high (r .92 and<br />
0.95 for and right and left eyes, respectively), with 88%<br />
<strong>of</strong> right eye retests and 94% <strong>of</strong> left eye retests within 0.1<br />
Accepted for publication Aug 22, 2001.<br />
From the Jaeb Center for Health Research (P.S.M., R.W.B., R.T.K.),<br />
Tampa, Florida; Curtin <strong>University</strong> (A.H.T.), Bentley, Western Australia;<br />
Mayo Clinic (J.M.H.), Rochester, MinnesotaUSA; Johns Hopkins <strong>University</strong><br />
(M.X.R.), Baltimore, Maryland; Retina Foundation <strong>of</strong> the SW<br />
(E.E.B.), Dallas, Texas; National Eye Institute (R.W.H.), Bethesda,<br />
Maryland; <strong>University</strong> <strong>of</strong> <strong>Arizona</strong> (J.M.M.), Tucson, <strong>Arizona</strong>; Devers Eye<br />
Institute (C.A.J.), Portland, Oregon.<br />
This work was supported by grants from the National Eye Institute<br />
(EY11155, EY11751, EY13095) and Research to Prevent Blindness, Inc,<br />
New York, New York, (J.M.H. as R.P.B. Olga Keith Wiess Scholar and an<br />
unrestricted grant to the Department <strong>of</strong> Ophthalmology, Mayo Clinic,<br />
Rochester, Minnesota).<br />
Additional technical information about the Electronic <strong>Visual</strong> <strong>Acuity</strong><br />
Tester and the Amblyopia Treatment Study visual acuity testing protocol<br />
application can be obtained from the lead author (pmoke@jaeb.org).<br />
Reprint requests to PEDIG Data Coordinating Center, Jaeb Center for<br />
Health Research, 3010 E. 138th Ave, Suite 9, Tampa, FL 33613.<br />
Correspondence to Roy W. Beck, MD, Ph.D., Jaeb Center for Health<br />
Research, 3010 East 138th Ave, Suite 9, Tampa, FL 33613; fax: (813)<br />
975-8761; e-mail: rbeck@jaeb.org<br />
logarithm <strong>of</strong> minimal angle <strong>of</strong> resolution (logMAR) units<br />
<strong>of</strong> the initial test. The 95% confidence interval for an<br />
acuity score was calculated to be the score 0.13<br />
logMAR units. For a change between two acuity scores,<br />
the 95% confidence interval was the difference 0.19<br />
logMAR units.<br />
● CONCLUSIONS: We have developed a computerized<br />
method for measurement <strong>of</strong> visual acuity. Automation <strong>of</strong><br />
the Amblyopia Treatment Study visual acuity testing<br />
protocol is an effective method <strong>of</strong> testing visual acuity in<br />
children 3 to 7 years <strong>of</strong> age. (Am J Ophthalmol<br />
2001;132:903–909. © 2001 by Elsevier Science Inc. All<br />
rights reserved.)<br />
VISUAL ACUITY IS A COMMON PRIMARY OUTCOME<br />
measure in clinical studies. In multicenter clinical<br />
trials, considerable effort is placed on the standardization<br />
<strong>of</strong> acuity testing across multiple sites. To more<br />
easily standardize measurement <strong>of</strong> visual acuity in clinical<br />
trials and to provide a method to directly capture acuity<br />
data electronically, we developed a computerized vision<br />
tester called the Electronic <strong>Visual</strong> <strong>Acuity</strong> Tester.<br />
One application developed for the Electronic <strong>Visual</strong><br />
<strong>Acuity</strong> Tester is the automation <strong>of</strong> the Amblyopia Treatment<br />
Study visual acuity testing protocol. This protocol<br />
was developed to facilitate the standardization <strong>of</strong> visual<br />
acuity testing in clinical trials <strong>of</strong> pediatric eye disease<br />
involving children in the 3-year-old to 7-year-old age<br />
range. 1 Its design represents a compromise between testability<br />
and precision for acuity testing <strong>of</strong> children. In a<br />
study <strong>of</strong> 178 children in which this acuity testing method<br />
was implemented by manually displaying a sequence <strong>of</strong><br />
single-surrounded HOTV optotypes on the Baylor-Video<br />
<strong>Acuity</strong> Tester (Medtronic Xomed Solan Ophthalmics,<br />
Jacksonville, Florida), 1 we found that 67% <strong>of</strong> the 21<br />
© 2001 BY ELSEVIER SCIENCE INC. ALL RIGHTS RESERVED.<br />
0002-9394/01/$20.00 903<br />
PII S0002-9394(01)01256-9
3-year-olds, 87% <strong>of</strong> the 60 4-year olds, and 96% <strong>of</strong> the 72<br />
5- to 7-year olds successfully completed the testing <strong>of</strong> both<br />
eyes. Test-retest reliability was high (r .82), with 93% <strong>of</strong><br />
retests within 0.1 logMAR units <strong>of</strong> the initial test. The<br />
95% confidence interval (CI) for an acuity score was<br />
calculated to be the score 0.125 logMAR units. For a<br />
change between two acuity scores, the 95% confidence<br />
interval was the difference 0.18 logMAR units.<br />
Our experience in using this acuity testing protocol on<br />
the Baylor-Video <strong>Acuity</strong> Tester in the Amblyopia Treatment<br />
Study 1 (a randomized multicenter clinical trial<br />
comparing part-time patching to atropine treatment for<br />
moderate amblyopia) identified several reasons for a computerized<br />
version <strong>of</strong> the testing protocol. First, some<br />
members <strong>of</strong> our Pediatric Eye Disease Investigator Group<br />
were unable to participate in our amblyopia trials, because<br />
they did not have a Baylor-Video <strong>Acuity</strong> Tester and future<br />
availability was limited. Second, acuity testers required<br />
considerable training to minimize errors resulting from<br />
manual administration <strong>of</strong> the testing protocol on the<br />
Baylor-Video <strong>Acuity</strong> Tester. Third, presentation <strong>of</strong> surrounded<br />
optotypes larger than 20/125 on the Baylor-Video<br />
<strong>Acuity</strong> Tester required moving to a shorter testing distance<br />
where patient movement toward or away from the monitor<br />
has a proportionally greater effect on visual acuity measurement<br />
accuracy than it does at longer testing distances.<br />
Fourth, automation <strong>of</strong> the protocol could potentially reduce<br />
the variability in how the testing procedure is<br />
conducted in a multicenter study.<br />
Herein, we describe the development <strong>of</strong> the Electronic<br />
<strong>Visual</strong> <strong>Acuity</strong> Tester, its application to the Amblyopia<br />
Treatment Study visual acuity protocol, and the results <strong>of</strong><br />
a study that assessed test-retest reliability.<br />
METHODS<br />
THE ELECTRONIC VISUAL ACUITY TESTER CONSISTS OF A<br />
handheld device that uses the Palm operating system<br />
version 3.5.0 (Palm, Inc, Santa Clara, California) and a<br />
personal computer running a Linux operating system and<br />
the Super VGA Graphics Library version 1.4.3. The<br />
handheld device and personal computer are connected by<br />
a serial cable (Figure 1). Stimuli are high-contrast blackand-white<br />
letters with luminance <strong>of</strong> 85 to 105 candelas/m 2<br />
and contrast <strong>of</strong> 98%. Both HOTV and Sloan letter sets are<br />
available for testing. Single letters are presented, framed<br />
with crowding bars that are spaced either a half-letter<br />
width or full-letter width around the letter. With a 17-inch<br />
monitor at 1600 by 1200 resolution, letters can be displayed<br />
from 20/800 to 20/12 at a test distance <strong>of</strong> 3 m.<br />
Letters are rendered on the monitor by manipulating the<br />
individual points on the display screen, known as pixels<br />
(picture element). Letter sizes are executed by translating<br />
octave steps to the number <strong>of</strong> pixels for a given stroke<br />
width, beginning with three pixels for a 20/12 letter.<br />
FIGURE 1. Electronic <strong>Visual</strong> <strong>Acuity</strong> Tester. The Electronic<br />
<strong>Visual</strong> <strong>Acuity</strong> Tester consists <strong>of</strong> a handheld device that uses the<br />
Palm operating system (Palm, Inc, Santa Clara, California)<br />
connected by a serial cable to a personal computer running a<br />
Linux operating system. Both HOTV and Sloan letter sets are<br />
available for testing. With a 17-inch monitor at 1600 by 1200<br />
resolution, single letters can be displayed from 20/800 to 20/12<br />
at a test distance <strong>of</strong> 3 m.<br />
Programs on the personal computer render the letters,<br />
provide serial communication with the handheld device,<br />
and store test results. Programs on the handheld device<br />
provide prompts for the tester, send display instructions to<br />
the personal computer, and transmit test results to the<br />
personal computer for storage. The size <strong>of</strong> each letter<br />
presentation can either be controlled by the tester or can<br />
be determined based on the patient’s responses by a<br />
program on the handheld device. All programs are written<br />
in the C programming language. In our development, we<br />
have used a Palm handheld device.<br />
The handheld device programs provide the option for<br />
customized entry <strong>of</strong> patient identifiers and demographic<br />
data before testing. During testing, the handheld screen<br />
shows the current letter presentation, asks whether the<br />
subject gave a correct or incorrect response, and prompts<br />
for confirmation <strong>of</strong> the correct/incorrect selection. When<br />
confirmed, the handheld device instructs the personal<br />
computer to write the response to disk and then render the<br />
next letter presentation. At each phase transition, the<br />
tester is given instructions for continuing the test. Upon<br />
test completion, the subject’s final acuity score is displayed.<br />
The Amblyopia Treatment Study visual acuity testing<br />
protocol 1 was converted to a C program on the Electronic<br />
<strong>Visual</strong> <strong>Acuity</strong> Tester. The testing protocol, which is<br />
904 AMERICAN JOURNAL OF OPHTHALMOLOGY<br />
DECEMBER 2001
described in Table 1, consists <strong>of</strong> the presentation <strong>of</strong><br />
single-surrounded optotypes in four steps: a screening<br />
phase, a first threshold determination (phase 1), reinforcement<br />
phase, and a second threshold determination (phase<br />
2). For the testing <strong>of</strong> young children, the HOTV letter set<br />
with half-width crowding bars is used. For older children<br />
and adults, the Sloan letter set can be used. The letter<br />
displayed on the monitor is randomly determined with the<br />
stipulation that there be no sequential repeated letters.<br />
We verified the accuracy <strong>of</strong> the computer program in<br />
adhering to the Amblyopia Treatment Study visual acuity<br />
testing protocol by performing 500 simulated tests. For 400<br />
tests, score sheets from actual testing using the acuity<br />
TABLE 1. Amblyopia Treatment Study <strong>Visual</strong> <strong>Acuity</strong> <strong>Testing</strong> Protocol<br />
Single letters with surround bars are presented in four phases: screening, phase 1 (first threshold determination), reinforcement, and<br />
phase 2 (second threshold determination).<br />
● In phase 1 and phase 2, up to four single letters are sequentially presented at each logMAR level* that is tested.<br />
● A level is considered to be passed if three <strong>of</strong> three or three <strong>of</strong> four letters are correct and “failed” if two letters at a level are missed.<br />
● <strong>Testing</strong> <strong>of</strong> a level stops as soon as criteria are met for either “pass” or “fail.”<br />
Screening<br />
Starting from either 20/100 or 20/400, single letters, in sequential descending logMAR sizes, are shown until one is missed.<br />
1. Tester selects 20/100 or 20/400 size letter to present as starting point (depending on the expectation <strong>of</strong> visual acuity level based on<br />
previous testing or a pretest).<br />
2. If response is correct, letter at next smallest logMAR level is presented and testing continues sequentially with one letter per logMAR<br />
level through 20/20 until there is an incorrect response.<br />
3. If starting point was 20/100 and response is incorrect at either 20/100 or 20/80, screening is restarted at 20/400.<br />
4. If screening starts at 20/400 and response is incorrect, testing continues sequentially with one letter per logMAR level through 20/800<br />
until there is a correct response.<br />
● If 20/800 is missed, 20/800 becomes the starting level for phase 1.<br />
Phase 1<br />
Starting two logMAR levels above the missed level in screening, the smallest logMAR level at which three <strong>of</strong> three or three <strong>of</strong> four letters<br />
are correctly identified is determined.<br />
1. Up to four single letters are sequentially presented two logMAR levels above the level missed in screening<br />
● Exception: if 20/20 was correct in screening, phase 1 starts at 20/30.<br />
● Exception: if 20/800 or 20/640 was missed in screening, phase 1 starts at 20/800.<br />
2. If first tested level is failed, testing continues at sequentially larger logMAR levels until a level is passed.<br />
● If 20/800 is failed, phase 1 ends, the reinforcement phase is omitted, and 20/800 is retested in phase 2.<br />
3. If first tested level is passed, testing continues at sequentially smaller logMAR levels until a level is failed.<br />
Reinforcement Phase<br />
In order to get the child whose attention is drifting back on track, three letters larger than the phase 1 threshold are sequentially<br />
presented.<br />
1. Starting three levels larger than the level missed in phase 1, three successively smaller single letters are presented.<br />
● Exception: if the level failed in phase 1 is 20/500 or 20/640, three 20/800 letters are shown for reinforcement.<br />
● Note: the reinforcement phase responses do not contribute to the visual acuity score, and even if the responses are incorrect the test<br />
proceeds to phase 2.<br />
Phase 2<br />
The last level missed in phase 1 is retested and if “passed,” testing continues until a level is “failed.‘<br />
1. Up to four single letters are sequentially-presented at the last level missed in phase 1.<br />
2. If the level is failed, testing stops.<br />
3. If the level is passed, testing continues at sequentially smaller logMAR levels until a level is failed.<br />
Final <strong>Visual</strong> <strong>Acuity</strong> Score<br />
The visual acuity score is the smallest logMAR level passed in phase 1 or phase 2.<br />
*logMAR levels (Snellen equivalents): 20/800, 20/640, 20/500, 20/400, 20/320, 20/250, 20/200, 20/160, 20/125, 20/100, 20/80, 20/63,<br />
20/50, 20/40, 20/32, 20/25, 20/20, 20/16, 20/12<br />
protocol that was conducted on the Baylor-Video <strong>Acuity</strong><br />
Tester in the Amblyopia Treatment Study 1 were used to<br />
enter responses on the handheld device in the same order<br />
as the real testing to verify that the proper testing sequence<br />
was followed and that the final visual acuity score was the<br />
same. This was supplemented by entering responses for 100<br />
additional tests from a Baylor-Video <strong>Acuity</strong> Tester score<br />
sheet that was completed to simulate all possible sequences<br />
<strong>of</strong> letter size presentations.<br />
A test-retest reliability study was conducted at four<br />
clinical sites to evaluate the Amblyopia Treatment Study<br />
visual acuity testing protocol using single-surrounded<br />
HOTV letters on the Electronic <strong>Visual</strong> <strong>Acuity</strong> Tester.<br />
VOL. 132, NO. 6 COMPUTERIZED VISUAL ACUITY TESTING<br />
905
Subjects were 3 to 7 years old. Informed consent for<br />
study participation was obtained from a parent or<br />
guardian. First the right and then the left eye <strong>of</strong> each<br />
child was tested and, after a short break, the right and<br />
left eyes were retested by the same examiner. The visual<br />
acuity score on each test was recorded as a logMAR<br />
equivalent. A matching card containing the HOTV<br />
letters was used so that the child could point to a letter<br />
rather than verbalize a response.<br />
There was no formalized training for the vision testers.<br />
However, each was familiar with the acuity testing protocol<br />
and conducted acuity testing using the Electronic<br />
<strong>Visual</strong> <strong>Acuity</strong> Tester at least once before the study to<br />
become familiar with the use <strong>of</strong> the handheld device.<br />
Only children who completed the testing <strong>of</strong> both eyes were<br />
included in the test-retest analysis. Frequency distributions <strong>of</strong><br />
the differences in visual acuity scores between the first and<br />
second test <strong>of</strong> each eye were constructed, and Pearson<br />
correlation coefficients were computed separately for the right<br />
and left eye data (the eye-specific results were slightly<br />
different, so they are reported separately). The correlation<br />
between the difference in test-retest score and the<br />
age <strong>of</strong> the subject also was assessed with the Pearson<br />
correlation coefficient. Test-retest reliability was also<br />
assessed using the method <strong>of</strong> Bland-Altman, 2 plotting<br />
the test-retest difference versus the mean test-retest<br />
score. Similar analyses were conducted for the interocular<br />
difference data. The standard error <strong>of</strong> measurement<br />
for the test was computed separately for each eye<br />
and then averaged for reporting and establishing a 95%<br />
confidence interval for an acuity score. 3 A 95% confidence<br />
interval for a change in an acuity score from a<br />
baseline value was computed by two methods; one based<br />
on the standard error <strong>of</strong> measurement from the first test<br />
and one based on the standard deviation <strong>of</strong> the testretest<br />
differences. These were calculated separately for<br />
right and left eyes and then averaged. The confidence<br />
interval for the interocular difference was based on the<br />
standard deviation <strong>of</strong> the test-retest difference in interocular<br />
difference. Statistical analyses were performed<br />
using SAS (personal computer version 8.01).<br />
RESULTS<br />
ONE HUNDRED FIFTY-SIX CHILDREN WERE INCLUDED IN THE<br />
study. One site contributed data on 95 children (61%) and<br />
the remaining three secondary sites data on 61 children<br />
(39%). The mean age <strong>of</strong> the children was 5.6 1.4 years;<br />
51% were males and 78% were Caucasian. Seventy-three<br />
<strong>of</strong> the children (47%) had no ocular cause for decreased<br />
acuity in both eyes, 60 (38%) had amblyopia in one eye,<br />
and the rest had other specified causes for decreased acuity.<br />
Most <strong>of</strong> the amblyopic eyes had only a mild decrease in<br />
visual acuity (78% were 20/50 or better). The distributions<br />
TABLE 2. Baseline Characteristics <strong>of</strong> Children in the<br />
Reliability Analysis<br />
Baseline Characteristic N 156<br />
Age in years (mean SD)<br />
Age in years n (%)<br />
5.6 1.4<br />
3 22 (14%)<br />
4 39 (25%)<br />
5 37 (24%)<br />
6 24 (15%)<br />
7 34 (22%)<br />
Male gender, n (%)<br />
Ethnicity, n (%)<br />
80 (51%)<br />
Caucasian 122 (78%)<br />
African American 17 (11%)<br />
Hispanic 3 (2%)<br />
Asian 5 (3%)<br />
American Indian 2 (1%)<br />
Mixed 2 (1%)<br />
Other 5 (3%)<br />
Developmental delay, n (%)<br />
Clinical diagnosis, n (%)<br />
Right eye<br />
11 (7%)<br />
Normal* 106 (68%)<br />
Uncorrected refractive error 6 (4%)<br />
Amblyopia 31 (20%)<br />
Other<br />
Left eye<br />
13 (8%)<br />
Normal* 101 (65%)<br />
Uncorrected refractive error 5 (3%)<br />
Amblyopia 35 (22%)<br />
Other<br />
<strong>Visual</strong> acuity in initial test<br />
15 (10%)<br />
† (median [quartiles]<br />
in logMAR units)<br />
Right eye 0.1 (0.0, 0.3)<br />
Left eye 0.1 (0.0, 0.3)<br />
Previously tested with isolated surrounded<br />
HOTV letters, n (%) ‡<br />
93 (60%)<br />
*”Normal” includes corrected refractive error.<br />
† Includes both normal and abnormal eyes.<br />
‡<br />
Child had previous visual acuity test using isolated surrounded<br />
HOTV letters, although not necessarily this protocol.<br />
<strong>of</strong> clinical diagnosis and visual acuity were similar in right<br />
and left eyes (Table 2).<br />
In right eyes, the correlation between the initial and the<br />
retest visual acuity scores was 0.92, with 88% <strong>of</strong> the retest<br />
scores within 0.1 logMAR units <strong>of</strong> the initial test score<br />
(0.1 logMAR units represents 1 logMAR line on an acuity<br />
chart). In left eyes, the correlation was 0.95, with 94% <strong>of</strong><br />
retests within 0.1 logMAR units <strong>of</strong> the initial test score<br />
(Figure 2). Data plotted as the test-retest difference versus<br />
the mean test-retest acuity suggested that test-retest reliability<br />
did not vary with the level <strong>of</strong> visual acuity (Figure<br />
3). In the 60 eyes with amblyopia, the correlation between<br />
the initial and the retest visual acuity scores was 0.96, with<br />
906 AMERICAN JOURNAL OF OPHTHALMOLOGY<br />
DECEMBER 2001
FIGURE 2. Distribution <strong>of</strong> test-retest differences in acuity scores (N 156). A negative difference indicates that the repeat acuity<br />
test score was worse than the initial score. Eighty-eight percent <strong>of</strong> right eyes and 94% <strong>of</strong> left eyes were within 0.1 logarithm <strong>of</strong><br />
minimal angle <strong>of</strong> resolution (logMAR) units on retest. The 95% confidence interval for an individual acuity score was calculated<br />
to be the score 0.13 logMAR units. The 95% confidence interval for an individual test-retest difference was calculated to be the<br />
score 0.19 logMAR units.<br />
FIGURE 3. Bland-Altman 2 plot <strong>of</strong> test-retest difference versus average test-retest acuity (N 156). Data plotted as the test-retest<br />
difference versus the mean test-retest acuity suggested that test-retest reliability did not vary with the level <strong>of</strong> visual acuity. A<br />
negative difference indicates that the repeat acuity test score was worse than the initial score.<br />
93% <strong>of</strong> the retest scores within 0.1 logMAR units <strong>of</strong> the<br />
initial test score. The test-retest reliability appeared similar<br />
across the age range <strong>of</strong> the subjects in the study (correlation<br />
between the difference in test-retest acuity scores and<br />
age 0.02 for right eyes and 0.07 for left eyes, Figure 4).<br />
More eyes had a better rather than a worse acuity on the<br />
retest, and the mean retest acuity was slightly better than<br />
the initial acuity (in right eyes, 33% better versus 18%<br />
worse, mean difference 0.022 0.10, P .01; and in<br />
left eyes, 33% better versus 17% worse, mean difference <br />
0.017 0.09, P .02). This better retest acuity score was<br />
present for younger (3 to 4 years old) and older (5 to 7<br />
years old) children, for children who had and who did not<br />
have prior experience with HOTV testing, and for eyes<br />
with amblyopia (data not shown). There was no tendency<br />
for subjects in whom both eyes were classified as normal to<br />
VOL. 132, NO. 6 COMPUTERIZED VISUAL ACUITY TESTING<br />
907
FIGURE 4. Test-retest difference versus age in years (N 156). Test-retest reliability appeared similar across the age range <strong>of</strong> the<br />
subjects in the study. The correlation between the difference in test-retest acuity scores and age 0.02 for right eyes and 0.07<br />
for left eyes. A negative difference indicates that the repeat acuity test score was worse than the initial score.<br />
FIGURE 5. Distribution <strong>of</strong> test-retest differences in interocular difference scores (N 156). A negative difference indicates that<br />
the interocular difference on the repeat testing was larger than the interocular difference on the initial testing. The 95% confidence<br />
interval for an individual interocular difference was calculated to be the interocular difference 0.18 logMAR units. The 95%<br />
confidence interval and for an individual interocular difference difference between two tests was calculated to be the interocular<br />
difference 0.25 logMAR units.<br />
have a better acuity score in the left eye than in the right<br />
eye (N 73; mean interocular difference 0.0 0.11 in<br />
both the initial test and repeat test).<br />
The 95% confidence interval for an acuity score was<br />
calculated to be the score 0.13 logMAR units (based on<br />
the standard error <strong>of</strong> measurement <strong>of</strong> 0.069). For a change<br />
between two acuity scores, the 95% confidence interval<br />
was the difference 0.19 logMAR units (when based on<br />
either the standard error <strong>of</strong> measurement or on the 0.096<br />
standard deviation <strong>of</strong> the test-retest difference).<br />
The interocular difference test-retest correlation was<br />
0.89. The retest interocular difference was within one<br />
logMAR level (0.1 logMAR units) <strong>of</strong> the initial interocular<br />
difference in 81% (Figure 5). The 95% confidence<br />
interval for the interocular difference was calculated to be<br />
the interocular difference 0.18 logMAR units and for a<br />
908 AMERICAN JOURNAL OF OPHTHALMOLOGY<br />
DECEMBER 2001
change in interocular difference to be the difference <br />
0.25 logMAR units.<br />
DISCUSSION<br />
WE HAVE DEVELOPED A PERSONAL COMPUTER–BASED VIsual<br />
acuity testing system controlled by a handheld device<br />
running the Palm operating system and programmed to run<br />
the Amblyopia Treatment Study visual acuity testing<br />
protocol. Our results indicate that this testing procedure<br />
has very good reliability for the measurement <strong>of</strong> visual<br />
acuity in children 3 to 7 years old. These results are similar<br />
to those we obtained when the Amblyopia Treatment<br />
Study acuity testing protocol was evaluated with manual<br />
administration on a Baylor-Video <strong>Acuity</strong> Tester. 1 In our<br />
Baylor-Video <strong>Acuity</strong> Tester study, testability ranged from<br />
67% in 3-year-olds to 96% in 5- to 7-year-olds. Testability<br />
should not differ between the Baylor-Video <strong>Acuity</strong> Tester<br />
or Electronic <strong>Visual</strong> <strong>Acuity</strong> Tester, because from the<br />
child’s perspective, the testing procedure is identical<br />
whether it is conducted on the Baylor-Video <strong>Acuity</strong> Tester<br />
or on the Electronic <strong>Visual</strong> <strong>Acuity</strong> Tester. Two <strong>of</strong> our four<br />
sites did evaluate testability with the Electronic <strong>Visual</strong><br />
<strong>Acuity</strong> Tester and in developmentally normal children<br />
found it to be 85% in 27 3-year-olds, 94% in 35 4-yearolds,<br />
and 100% in 71 5- to 7-year-olds.<br />
We were surprised that the mean acuity was slightly<br />
better in both eyes on the repeat test compared with the<br />
initial test, particularly because this phenomenon was not<br />
related to either younger age or to lack <strong>of</strong> prior experience<br />
with HOTV testing and because there was no suggestion<br />
that the left eyes tested better than the right eyes (testing<br />
order was right eye, left eye). In reviewing our data from<br />
the Baylor-Video <strong>Acuity</strong> Tester reliability study, we found<br />
a similar phenomenon for right eyes but not for left eyes.<br />
These findings suggest that there might be either a small<br />
learning effect or increased comfort level that can lead to<br />
a slightly better acuity on repeat testing. Regarding the<br />
clinical importance <strong>of</strong> a small improvement <strong>of</strong> visual acuity<br />
on repeat testing, the results <strong>of</strong> both this study and our<br />
prior Baylor-Video <strong>Acuity</strong> Tester study indicate that we<br />
can be reasonably certain <strong>of</strong> a real difference only if it is<br />
two or more logMAR levels. With this requirement, the<br />
learning/comfort effect, which appears on average to be on<br />
the order <strong>of</strong> one-fourth <strong>of</strong> a logMAR level, is likely to be<br />
inconsequential in the interpretation <strong>of</strong> whether a true<br />
change in acuity has occurred.<br />
In the clinical management <strong>of</strong> children with amblyopia,<br />
considerable weight is given by some clinicians to the<br />
interocular difference. As we found in the Baylor-Video<br />
<strong>Acuity</strong> Tester reliability study, 1 we again found that the<br />
test-retest reliability <strong>of</strong> the interocular difference was<br />
slightly lower than that <strong>of</strong> the visual acuity measurements<br />
themselves. This was true even when the analysis was<br />
limited to the children with unilateral amblyopia (data not<br />
shown).<br />
Our results compare favorably with the few studies that<br />
have evaluated the reliability <strong>of</strong> visual acuity testing<br />
methods in children. For line HOTV acuity testing,<br />
Harvey and associates 4 reported test-retest rank correlation<br />
coefficients <strong>of</strong> 0.81 for 36 3.5-year-olds and 0.85 for 48<br />
4.5-year-olds as part <strong>of</strong> the multicenter Cryotherapy for<br />
Retinopathy <strong>of</strong> Prematurity Study. However, 10% <strong>of</strong> retests<br />
differed from the initial test by more than 3 logMAR<br />
lines. Using the Glasgow acuity cards, McGraw and<br />
associates 5 reported that 95% <strong>of</strong> retests were within one<br />
logMAR level <strong>of</strong> an initial test in 68 visually normal<br />
children who had a mean age <strong>of</strong> 5.3 years.<br />
In summary, we have developed a computerized method<br />
for visual acuity testing and have successfully adapted the<br />
Amblyopia Treatment Study visual acuity testing protocol<br />
to test children with this system. For a clinical trial, the<br />
advantages <strong>of</strong> using this computerized method <strong>of</strong> testing<br />
over manual testing include better standardization <strong>of</strong> the<br />
testing procedure across multiple sites, decreased training<br />
requirements for the technicians administering the test,<br />
ability to test acuity up to 20/800 with single-surrounded<br />
optotypes at a 3-m test distance, and ability to directly<br />
capture the testing data electronically without the need to<br />
manually record every response on a score sheet. The<br />
primary disadvantage is cost when compared with manual<br />
testing using eye charts; the cost <strong>of</strong> the components <strong>of</strong> the<br />
system (personal computer, monitor, handheld device) is<br />
about $750. In addition to the Amblyopia Treatment<br />
Study visual acuity protocol, we are currently developing<br />
an adaptive testing strategy for testing older children and<br />
adults using the Electronic <strong>Visual</strong> <strong>Acuity</strong> Tester as an<br />
alternative to the Early Treatment Diabetic Retinopathy<br />
Study method which has been the gold-standard for<br />
measuring visual acuity in clinical trials.<br />
REFERENCES<br />
1. Holmes JM, Beck RW, Repka MX, et al. The amblyopia<br />
treatment study visual acuity testing protocol. Arch Ophthalmol<br />
2001;119:1345–1353.<br />
2. Bland JM, Altman DG. Statistical methods for assessing<br />
agreement between two methods <strong>of</strong> clinical measurement.<br />
Lancet 1986;1:307–310.<br />
3. Crocker L, Algina J. Introduction to classical and modern test<br />
theory. Fort Worth, Texas: Harcourt Brace Jovanovich College<br />
Publishers, 1986:150–151.<br />
4. Harvey EM, Dobson V, Tung B, Quinn GE, Hardy RJ. Interobserver<br />
agreement for grating acuity and letter acuity assessment<br />
in 1- to 5.5-year olds with severe retinopathy <strong>of</strong><br />
prematurity. Invest Ophthalmol Vis Sci 1999:1565–1576.<br />
5. McGraw PV, Winn B, Gray LS, Elliott DB. Improving the<br />
reliability <strong>of</strong> visual acuity measures in young children. Ophthalmic<br />
Physiol Opt 2000;20:173–184.<br />
VOL. 132, NO. 6 COMPUTERIZED VISUAL ACUITY TESTING<br />
909