Laboratory Variables That May Affect Test Results in Prothrombin ...
Laboratory Variables That May Affect Test Results in Prothrombin ...
Laboratory Variables That May Affect Test Results in Prothrombin ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
124<br />
science [coagulation and hematology]<br />
<strong>Laboratory</strong> <strong>Variables</strong> <strong>That</strong> <strong>May</strong> <strong>Affect</strong><br />
<strong>Test</strong> <strong>Results</strong> <strong>in</strong> Prothromb<strong>in</strong> Times<br />
(PT)/International Normalized Ratios (INR)<br />
David L. McGlasson, MS, CLS/NCA, H, ASCP<br />
59th Cl<strong>in</strong>ical Research Squadron/MSRL, Lackland AFB, TX<br />
DOI: 10.1309/RT9D02JXCHY8V9HM<br />
Monitor<strong>in</strong>g patients on oral<br />
anticoagulant therapy (OAT) requires<br />
constant monitor<strong>in</strong>g by physicians<br />
us<strong>in</strong>g highly sophisticated coagulation<br />
test<strong>in</strong>g.<br />
The World Health Organization (WHO)<br />
put forth the idea for prothromb<strong>in</strong><br />
time standardization based on a<br />
mathematical formula known as the<br />
International Normalized Ratios (INR)<br />
Because manufacturers provide<br />
limited guidel<strong>in</strong>es for <strong>in</strong>struments, the<br />
laboratory should validate its values<br />
by perform<strong>in</strong>g local on-site<br />
International Sensitivity Index (ISI)<br />
calibration.<br />
In a MMWR report dated August<br />
24, 2001 the follow<strong>in</strong>g circumstances<br />
on “Adverse events and deaths associated<br />
with laboratory errors at a hospital-Pennsylvania,<br />
2001” were reported.<br />
On August 3, 2001, the Center for Disease<br />
Control (CDC) was contacted by<br />
the Pennsylvania Department of Health<br />
(PADOH) to assist with an <strong>in</strong>vestigation<br />
of laboratory errors that may have contributed<br />
to the deaths of at least 2 persons<br />
tak<strong>in</strong>g the anticoagulant drug<br />
warfar<strong>in</strong> (Coumad<strong>in</strong>, DuPont Pharmaceuticals<br />
M, Wilm<strong>in</strong>gton DE). The<br />
Food and Drug Adm<strong>in</strong>istration (FDA)<br />
also was <strong>in</strong>vestigat<strong>in</strong>g this <strong>in</strong>cident. The<br />
monitor<strong>in</strong>g of warfar<strong>in</strong>’s anticoagulant<br />
effect is accomplished by perform<strong>in</strong>g 2<br />
laboratory assays: the prothromb<strong>in</strong> time<br />
(PT) and the INR. The INR is a<br />
numeric value calculated from the PT, a<br />
clott<strong>in</strong>g assay result, and the ISI, which<br />
<strong>in</strong>dicated the sensitivity of the reagent<br />
used to perform the assay. The WHO<br />
recommends that INR values be used by<br />
physicians to compare laboratory results<br />
between reagent/<strong>in</strong>strument comb<strong>in</strong>ations<br />
at different <strong>in</strong>stitutions.<br />
Dur<strong>in</strong>g June 4 through July 25,<br />
2001 the hospital laboratory <strong>in</strong> Pennsylvania<br />
reported 2,146 test with correct<br />
PT results but with <strong>in</strong>correctly calculated<br />
INR results. The mathematical formula<br />
required for calculat<strong>in</strong>g the INR<br />
uses a reagent-specific number, the ISI,<br />
which is usually furnished by the manufacturer<br />
of the reagent. In June, the hospital<br />
laboratory did not verify the new<br />
reagent used <strong>in</strong> the coagulation analyzer<br />
for perform<strong>in</strong>g the PT assay. As a result,<br />
the ISI used to calculate the INR was<br />
<strong>in</strong>correct for the reagent used. For approximately<br />
7 weeks, the reported INRs<br />
were falsely low. Several physicians<br />
who <strong>in</strong>terpreted these results <strong>in</strong>creased<br />
their patients’ doses of coumad<strong>in</strong>. In<br />
several cases, this led to the patient’s<br />
OAT regimen be<strong>in</strong>g compromised. 1 One<br />
subject previously had coronary bypass<br />
surgery and was hav<strong>in</strong>g the INR<br />
followed on an outpatient basis. He<br />
started hav<strong>in</strong>g bleed<strong>in</strong>g from the gums<br />
and was bruis<strong>in</strong>g easily. At the orig<strong>in</strong>al<br />
hospital laboratory the INR result was<br />
2.62, which is <strong>in</strong> the therapeutic range.<br />
He then went to another hospital to have<br />
the INR repeated. <strong>That</strong> result yielded an<br />
INR of 5.7, which was very high. His<br />
cardiologist directed the patient to discont<strong>in</strong>ue<br />
the coumad<strong>in</strong> dos<strong>in</strong>g for 4<br />
days. 2 Investigations are also under way<br />
by PADOH, Centers for Medicare and<br />
Medicaid Services (CMS), and CDC to<br />
identify other patient morbidity and<br />
mortality associated with the error, its<br />
possible causes, and the steps needed to<br />
laboratorymedic<strong>in</strong>e> february 2003> number 2> volume 34<br />
©<br />
prevent its recurrence. The FDA is review<strong>in</strong>g<br />
possible deficiencies <strong>in</strong> the<br />
manufacturer’s reagent package label<strong>in</strong>g.<br />
Discussion<br />
Monitor<strong>in</strong>g patients on OAT requires<br />
constant monitor<strong>in</strong>g by physicians us<strong>in</strong>g<br />
highly sophisticated coagulation test<strong>in</strong>g.<br />
The most frequently used assay is the PT.<br />
Standardization of the PT test results has<br />
proven to be difficult because of the<br />
abundance of manufacturer thromboplast<strong>in</strong>s<br />
and <strong>in</strong>strumentation available<br />
throughout the world.<br />
Physicians monitor patients on OAT<br />
by frequently perform<strong>in</strong>g repeat measurement<br />
of the PT assay. By do<strong>in</strong>g this<br />
they can adequately monitor the subjects<br />
warfar<strong>in</strong> <strong>in</strong>take. They are then able to<br />
ma<strong>in</strong>ta<strong>in</strong> each subject <strong>in</strong> a designated<br />
therapeutic range. There are many variables<br />
<strong>in</strong> the performance of the PT that<br />
may affect the test result. These <strong>in</strong>clude<br />
the specimen collection, process<strong>in</strong>g of<br />
the sample, <strong>in</strong>strumentation used to perform<br />
the assay, and the sensitivity of the<br />
thromboplast<strong>in</strong> used to perform the PT<br />
assay. Each thromboplast<strong>in</strong>’s sensitivity<br />
is determ<strong>in</strong>ed by the <strong>in</strong>dividual ISI.<br />
Manufacturers <strong>in</strong>dividual thromboplast<strong>in</strong><br />
reagent sensitivity to the Vitam<strong>in</strong> K dependent<br />
coagulation factors affected by<br />
warfar<strong>in</strong> have a wide range of variability.<br />
This has created problems for physicians<br />
when try<strong>in</strong>g to monitor patients <strong>in</strong><br />
different <strong>in</strong>stitutions with different<br />
reagent/<strong>in</strong>strument comb<strong>in</strong>ations. A subject<br />
monitored with a low sensitivity<br />
reagent (high ISI) may give a low PT<br />
time of 14 seconds. While the same patient<br />
when us<strong>in</strong>g a high sensitivity<br />
reagent (low ISI) may give a time of 18
seconds. These results may drastically<br />
affect the <strong>in</strong>terpretation of the PT assay<br />
and the warfar<strong>in</strong> dosage <strong>in</strong> the <strong>in</strong>dividual<br />
patients. 3<br />
The WHO <strong>in</strong> 1977 <strong>in</strong>troduced a standardized<br />
thromboplast<strong>in</strong> that was touted<br />
as an <strong>in</strong>ternational reference preparation<br />
(IRP). The hope was that each laboratory<br />
could develop a reference range for PT<br />
test<strong>in</strong>g that was to be compared to the<br />
IRP range. Tak<strong>in</strong>g this <strong>in</strong>itial step further<br />
the WHO <strong>in</strong> 1983 then put forth the idea<br />
for PT standardization based on a mathematical<br />
formula (INR) that uses the elements<br />
of the PT assay.<br />
The INR then would be the PT result<br />
that a laboratory would obta<strong>in</strong> if the test<br />
were performed us<strong>in</strong>g the standardized<br />
WHO reference thromboplast<strong>in</strong> reagent<br />
with an assigned ISI value of 1.0. Each<br />
assigned thromboplast<strong>in</strong> ISI could then<br />
compare the <strong>in</strong>dividual reagent sensitivity<br />
to an IRP that has been calibrated with a<br />
WHO reference plasma. The INR is calculated<br />
us<strong>in</strong>g the follow<strong>in</strong>g formula 3 :<br />
INR = (patient PT) ISI<br />
Mean normal PT<br />
Each <strong>in</strong>dividual laboratory would<br />
supply the mean normal PT. The INR<br />
method would then allow the physician to<br />
compare the PT results with different laboratories<br />
reagent/<strong>in</strong>strument<br />
comb<strong>in</strong>ations. Manufacturers now produce<br />
a wide variety of thromboplast<strong>in</strong><br />
with ISI values rang<strong>in</strong>g from 0.9 to 3.0.<br />
This wide range of ISI will produce a<br />
huge difference of PT results. 3 The INR<br />
was designed to correct for this<br />
difference. Therefore, if a patient were<br />
travel<strong>in</strong>g from one city to another the<br />
physician would have the advantage of<br />
expect<strong>in</strong>g a standardized INR value to<br />
ma<strong>in</strong>ta<strong>in</strong> a patient’s OAT range.<br />
As observed <strong>in</strong> the case report improper<br />
assignment of ISI values with different<br />
reagent/<strong>in</strong>strument comb<strong>in</strong>ations<br />
can result <strong>in</strong> cl<strong>in</strong>ically significant <strong>in</strong>accurate<br />
values. This difference <strong>in</strong> ISI values<br />
resulted <strong>in</strong> improper management of a<br />
large group of patients on OAT with catastrophic<br />
consequences. Huge<br />
differences <strong>in</strong> INR values have been reported<br />
when there are significant differences<br />
between low versus high ISI<br />
sensitivities <strong>in</strong> thromboplast<strong>in</strong>s. 4,5<br />
Preanalytic <strong>Variables</strong> of INR<br />
<strong>Test</strong><strong>in</strong>g<br />
Citrate Concentration<br />
Prothromb<strong>in</strong> time assays are<br />
performed on citrated platelet-poor<br />
plasma. The concentration of the sodium<br />
citrate anticoagulant can affect the PT time<br />
thus affect<strong>in</strong>g the INR value. 6-8 In the<br />
United States, until recently,<br />
approximately 80% of the PT assays were<br />
performed <strong>in</strong> plasma that was collected<br />
us<strong>in</strong>g vacuta<strong>in</strong>er tubes that conta<strong>in</strong>ed 3.8%<br />
(129 mol/L) sodium citrate. In 1998,<br />
NCCLS Subcomittee on Coagulation<br />
started to recommend that a 3.2% (109<br />
mol/L) sodium citrate concentration be<br />
used for most coagulation studies. This<br />
concentration was selected because the<br />
WHO was calibrat<strong>in</strong>g thromboplast<strong>in</strong>s<br />
us<strong>in</strong>g the 3.2% concentration. 9 Other <strong>in</strong>ternational<br />
standardization organizations also<br />
recommend us<strong>in</strong>g the 3.2% citrated anticoagulant.<br />
The osmolality of the 3.2% concentration<br />
is apparently closer to plasma.<br />
Higher INR values have been found <strong>in</strong><br />
some thromboplast<strong>in</strong> reagents <strong>in</strong> plasma<br />
collected with 3.8% citrated vacuta<strong>in</strong>er<br />
tubes. In one direct comparison study between<br />
the 2 citrate concentrations us<strong>in</strong>g a<br />
low ISI thromboplast<strong>in</strong>, the INR difference<br />
<strong>in</strong> 18.0% of the specimens showed a INR<br />
difference of 0.7. In another study, the difference<br />
on all specimens gave an average<br />
difference of 19.0%. The lower the ISI<br />
value is the more difference the citrate<br />
concentration makes <strong>in</strong> the INR results. 9 In<br />
platelet studies and test<strong>in</strong>g of blood bank<br />
products such as cryoprecipitate, the 3.8%<br />
citrate concentration is still recommended.<br />
Specimen Handl<strong>in</strong>g<br />
Improper specimen collection can<br />
also drastically affect the PT assay thus<br />
affect<strong>in</strong>g the INR value. This area has<br />
become controversial due to a number of<br />
studies that discuss the length of time<br />
and how a specimen can be stored be<br />
perform<strong>in</strong>g a PT assay. One study<br />
showed that storage of specimens for up<br />
to 6 hours at room temperature did not<br />
affect the PT results. 10 In another study,<br />
it was found that specimens from patients<br />
who were on low dose warfar<strong>in</strong> could be<br />
shipped overnight at room temperature<br />
©<br />
laboratorymedic<strong>in</strong>e> february 2003> number 2> volume 34<br />
without significantly chang<strong>in</strong>g the INR<br />
values. 11 Another study looked at specimens<br />
stored as whole blood. It found<br />
that after 3 days stored at room temperature<br />
that there was no significant change<br />
<strong>in</strong> the INR. 12 NCCLS guidel<strong>in</strong>es from<br />
1998 stated that uncentrifuged<br />
specimens for the PT/INR test or centrifuged<br />
plasma left of top of the separated<br />
cells stored at various temperatures<br />
from 2 to 24°C should be run with<strong>in</strong> 24<br />
hours from the time the sample was obta<strong>in</strong>ed<br />
from the test subject. 13 The PT<br />
results may vary from the time of collection<br />
of the specimen and storage of the<br />
sample if the subject was receiv<strong>in</strong>g hepar<strong>in</strong><br />
and was on OAT. The laboratory<br />
must be sure that the thromboplast<strong>in</strong> has<br />
a hepar<strong>in</strong> neutralizer to counteract the<br />
effects of hepar<strong>in</strong>. Evidence has also<br />
been presented that if specimens are<br />
stored at approximately 4°C that the<br />
PT/INR results may be shortened due to<br />
cold activation of FVII. 9 Our recommendation<br />
is that all specimens should be<br />
treated as if they were the last specimens<br />
that could be obta<strong>in</strong>ed from the test subject<br />
without hav<strong>in</strong>g to recollect the sample.<br />
If another assay is required, such as<br />
an APTT or factor assay, the prolonged<br />
storage times of >4 hours would possibly<br />
render the specimen compromised<br />
and required the patient to have a second<br />
venipuncture. This <strong>in</strong>creases time and<br />
expense for all concerned.<br />
More recently it has been discovered<br />
that the coagulation tube has been<br />
found to be a cl<strong>in</strong>ically significant<br />
source of variability <strong>in</strong> coagulation test<strong>in</strong>g.<br />
There has been controversy <strong>in</strong> us<strong>in</strong>g<br />
“partial-draw tubes” which required less<br />
vacuum to manufacture which resulted<br />
<strong>in</strong> 1.8 mL or 2.7 mL blood draws versus<br />
the conventional 4.5 mL draw with the<br />
blood to anticoagulant ratio of 9:1. S<strong>in</strong>ce<br />
the partial-draw tubes filled more slowly<br />
than the so-called full-draw tubes to<br />
platelets may have been activated due to<br />
lengthy exposure to shear forces aris<strong>in</strong>g<br />
from exposure to shear forces aris<strong>in</strong>g<br />
from draw<strong>in</strong>g blood <strong>in</strong>to the <strong>in</strong>creased<br />
headspace. The activated platelets then<br />
may release platelet-factor 4 or phospholipids<br />
which could compromise coagulation<br />
test<strong>in</strong>g. 14<br />
125
126<br />
Instrumentation<br />
There are over 300 different methods<br />
of perform<strong>in</strong>g a PT assay <strong>in</strong> the United<br />
States alone. Because of this wide variety<br />
of test<strong>in</strong>g it is almost impossible for manufacturers<br />
to provide accurate reagent/<strong>in</strong>strument<br />
specific ISI values for each<br />
reagent/<strong>in</strong>strument comb<strong>in</strong>ation. The<br />
WHO protocol for assign<strong>in</strong>g ISI values<br />
to thromboplast<strong>in</strong> reagents is determ<strong>in</strong>ed<br />
by perform<strong>in</strong>g a manual tilt-tube method<br />
<strong>in</strong> quadruplicate. 15 Laboratories then<br />
have to depend on manufacturers to accurately<br />
assign the proper ISI of their<br />
reagents based on some adaptation of<br />
the WHO protocol. 16 Therefore, the <strong>in</strong>strumentation<br />
can vastly affect the PT<br />
test results. If a coagulation laboratory is<br />
us<strong>in</strong>g a reagent from one company and<br />
an <strong>in</strong>strument from another supplier they<br />
have to rely on the reagent companies<br />
generic assignment of mechanical or<br />
photo-optic ISI values. Laboratories may<br />
not be aware that different automated<br />
coagulation systems can directly affect<br />
the ISI and the INR result. There may be<br />
dist<strong>in</strong>ct differences between mechanical<br />
and photo-optical coagulation systems<br />
with different reagents. 16,17 In our <strong>in</strong>stitution,<br />
we performed a protocol with 7<br />
different reagent/<strong>in</strong>strument comb<strong>in</strong>ations<br />
on the same specimens. 16 In many specimens,<br />
we saw cl<strong>in</strong>ically significant differences<br />
of INR values between the<br />
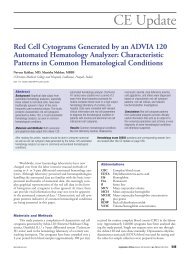
different reagent/ comb<strong>in</strong>ations. T1 dis-<br />
plays some of these INR result<br />
differences. Observe that the specimen<br />
#1180 has an INR value of 3.95 with<br />
one reagent/<strong>in</strong>strument comb<strong>in</strong>ation and<br />
7.16 with another system. This is an<br />
81.3% difference. The 3.95 value might<br />
be considered a high therapeutic range<br />
value that would probably require no<br />
<strong>in</strong>tervention. The 7.16 INR might cause<br />
some <strong>in</strong>stitutions to consider this result a<br />
panic value. Many other variables can<br />
affect the coagulation <strong>in</strong>strument ISI sensitivity<br />
used <strong>in</strong> the PT analysis. These are<br />
temperatures of the system and reagents,<br />
accuracy of volume of the reagents be<strong>in</strong>g<br />
dispensed, and the citrate concentration of<br />
the specimen collected. 15,16<br />
Look<strong>in</strong>g for a simpler method to locally<br />
calibrate ISI values we performed a<br />
protocol at our <strong>in</strong>stitution that was sponsored<br />
by Dade Behr<strong>in</strong>g M (Deerfield, IL)<br />
us<strong>in</strong>g a calibration system supplied by Precision-Biologic<br />
M (Dartmouth, NS, Canada).<br />
Precision Biologic has proposed a simplified<br />
method of locally calibrat<strong>in</strong>g the<br />
reagent ISI us<strong>in</strong>g a 5-day ISI calibration<br />
protocol. The method used a set of 5 OAT<br />
frozen plasmas and 1 normal frozen plasma<br />
that are assayed aga<strong>in</strong>st a standard (WHO<br />
IRP) thromboplast<strong>in</strong>. The frozen OAT calibrators<br />
and the normal plasma encompassed<br />
the 4 therapeutic categories used <strong>in</strong> OAT<br />
(4.5). Two recent<br />
papers discussed <strong>in</strong> detail how any laboratory<br />
can use the frozen calibrator plasma<br />
Comparison of Selected INR Differences of Human Subject’s Plasma<br />
laboratorymedic<strong>in</strong>e> february 2003> number 2> volume 34<br />
©<br />
method to locally calibrate their reagent/<strong>in</strong>strument<br />
comb<strong>in</strong>ations and how they would<br />
affect subject and manufacturers suggestions<br />
for ISI values with many different<br />
thromboplast<strong>in</strong>s and <strong>in</strong>struments. 15,17 Laboratories<br />
that run PT/INR assays can then set<br />
up there own ISI calibration of the locally<br />
used thromboplast<strong>in</strong>. This method may be<br />
the most practical for improv<strong>in</strong>g <strong>in</strong>ter-laboratory<br />
INR agreement. See the results <strong>in</strong><br />
T2 and T3 on differences <strong>in</strong> local and<br />
manufacturer calibrations of ISIs that were<br />
used <strong>in</strong> our study. 14<br />
Hepar<strong>in</strong> Effects on PT/INR<br />
<strong>Test</strong><strong>in</strong>g<br />
Unfractionated hepar<strong>in</strong> contam<strong>in</strong>ation<br />
can adversely affect the results of a<br />
PT/INR assay. Many subjects start<strong>in</strong>g on<br />
OAT are com<strong>in</strong>g off hepar<strong>in</strong> therapy,<br />
which could give physicians problems<br />
with falsely elevated INR values when<br />
try<strong>in</strong>g to establish basel<strong>in</strong>e INR ranges<br />
for patients. Each manufacturer’s thromboplast<strong>in</strong><br />
has an <strong>in</strong>dividual sensitivity to<br />
the effect of hepar<strong>in</strong>. Some reagents<br />
have a hepar<strong>in</strong> neutralizer present such<br />
as polybrene or protam<strong>in</strong>e sulfate that<br />
can counteract the effects of hepar<strong>in</strong> <strong>in</strong><br />
the therapeutic range so the PT/INR results<br />
are not compromised. However,<br />
reagents without a hepar<strong>in</strong> neutralizer<br />
present have been found to have PT results<br />
prolonged <strong>in</strong> some subjects by as<br />
long as 10 seconds. This could lead to<br />
Human MLA 900C CI+ MLA 900C T-D MLA 900C T-R MLA 1600C T-D STA CI+ STA T-D STA T-R<br />
Sample<br />
1167 2.77 3.41 3.72 3.62 2.68 3.24 3.41<br />
1181 2.53 3.2 3.65 3.36 2.64 2.85 2.91<br />
1180 3.95 5.98 5.83 7.16 4.02 4.93 5.05<br />
1398 2.94 3.94 3.44 4.14 3.06 3.61 3.35<br />
1393 3.57 4.98 4.48 5.0 3.57 4.39 4.18<br />
1391 3.03 4.14 3.41 4.43 3.13 3.82 3.14<br />
1684 3.72 5.82 4.99 6.29 3.99 5.57 4.47<br />
1688 2.95 3.94 3.93 4.44 3.12 3.7 3.79<br />
1814 3.15 1.97 4.0 4.85 3.24 4.23 3.58<br />
1669 3.25 2.41 3.66 3.93 3.24 4.29 3.28<br />
T1<br />
Done on the STA and MLA 900 C with thromboplast<strong>in</strong>s: Neoplast<strong>in</strong>e CI+, Diagnostica Stago (CI+); Thromboplast<strong>in</strong> D, Pacific-Hemostasis (T-D); Recombiplast<strong>in</strong>, Hemolance (T-R) and<br />
the MLA 1600C with T-D only.
Summary of Mean INR <strong>Results</strong> on 25 Normal Patient Samples Before and After Local ISI Calibration<br />
Instrument Reagent Mean INR Us<strong>in</strong>g Mean INR Us<strong>in</strong>g Difference <strong>in</strong><br />
Vendor-Assigned ISI Locally Calibrated ISI INR Means (%)<br />
Diagnostica Stago/STA Neoplast<strong>in</strong>e CI+ 1.24 1.29 -3.9<br />
Thromborel S 1.12 1.13 -0.9<br />
Thromboplast<strong>in</strong> C+ 1.96 1.76 10.1<br />
Innov<strong>in</strong> 0.92 1.00 -8.5<br />
Sysmex CA 540 Neoplast<strong>in</strong>e CI+ 1.24 1.09 11.9<br />
Thromborel S 1.06 1.02 3.4<br />
Thromboplast<strong>in</strong> C+ 1.95 1.81 7.4<br />
Innov<strong>in</strong> 1.02 0.92 10.3<br />
Dade-Behr<strong>in</strong>g BCS Neoplast<strong>in</strong>e CI+ 1.24 1.16 6.9<br />
Thromborel S 1.06 1.02 3.5<br />
Thromboplast<strong>in</strong> C+ 1.77 1.57 11.1<br />
Innov<strong>in</strong> 0.90 1.07 -18.9<br />
Summary of Mean INR <strong>Results</strong> on 95 Patient OAT Samples Before and After Local ISI Calibration<br />
Instrument Reagent Mean INR Us<strong>in</strong>g Mean INR Us<strong>in</strong>g Difference <strong>in</strong> <strong>Results</strong> >10%<br />
Vendor-Assigned ISI Locally Calibrated ISI INR Means (%) Difference<br />
Diagnostica Stago/STA Neoplast<strong>in</strong>e CI+ 2.58 2.69 4.1 0.0<br />
Thromborel S 2.56 2.58 0.8 0.0<br />
Thromboplast<strong>in</strong> C+ 2.39 2.15 10.0 37.1<br />
Innov<strong>in</strong> 2.45 2.67 7.9 22.1<br />
Sysmex CA 540 Neoplast<strong>in</strong>e CI+ 3.46 2.90 16.1 63.9<br />
Thromborel S 2.69 2.58 4.1 0.0<br />
Thromboplast<strong>in</strong> C+ 2.82 2.60 7.8 27.8<br />
Innov<strong>in</strong> 2.49 2.25 9.6 39.2<br />
Dade-Behr<strong>in</strong>g BCS Neoplast<strong>in</strong>e CI+ 2.81 2.60 7.5 20.6<br />
Thromborel S 2.67 2.57 3.7 0.0<br />
Thromboplast<strong>in</strong> C+ 2.86 2.51 12.6 52.6<br />
Innov<strong>in</strong> 2.66 3.29 16.4 64.9<br />
serious patient mismanagement dur<strong>in</strong>g<br />
OAT. There is no current evidence that<br />
the hepar<strong>in</strong> neutralizers may neutralize<br />
the presence of low molecular weight<br />
hepar<strong>in</strong>. Each <strong>in</strong>stitution should check<br />
the effect of a therapeutic dose of unfractionated<br />
hepar<strong>in</strong> aga<strong>in</strong>st their<br />
reagent/<strong>in</strong>strument system.<br />
Possible Effect of a Lupus<br />
Anticoagulant (LA) on PT/INR<br />
The recommended therapeutic range<br />
of INR for OAT <strong>in</strong> patients with the presence<br />
of a LA is currently 2.5 to 3.5. This<br />
is still a controversial subject. It has<br />
been suggested that us<strong>in</strong>g the INR to<br />
monitor these patients may be <strong>in</strong>adequate<br />
due to <strong>in</strong>terference by the presence of a<br />
LA on the clot-based PT assay. Some<br />
<strong>in</strong>vestigators have suggested us<strong>in</strong>g the<br />
prothromb<strong>in</strong>-proconvert<strong>in</strong> assay <strong>in</strong> lieu<br />
of the PT/INR for patients with this disorder<br />
s<strong>in</strong>ce it doesn’t appear to be<br />
affected by a LAs <strong>in</strong>hibitory actions. 3<br />
Others have suggested measur<strong>in</strong>g coagulation<br />
factors II and X by either chromogenic<br />
or 1-stage clott<strong>in</strong>g assays based<br />
on at least 3 dilutions to lessen the LA<br />
<strong>in</strong>hibitory effect. 3 Other <strong>in</strong>vestigators<br />
found little effect of the presence of a LA<br />
on PT/INR results us<strong>in</strong>g different thromboplast<strong>in</strong>s<br />
and <strong>in</strong>struments. One small exception<br />
was a subgroup of 6 patients <strong>in</strong><br />
which a recomb<strong>in</strong>ant thromboplast<strong>in</strong><br />
©<br />
laboratorymedic<strong>in</strong>e> february 2003> number 2> volume 34<br />
T2<br />
T3<br />
(Innov<strong>in</strong>, Dade-Behr<strong>in</strong>g) was used. 3 One<br />
recent study performed a protocol to see if<br />
subjects who have the presence of anticardiolip<strong>in</strong><br />
antibodies without the presence<br />
of an LA to see if the INR assay was affected<br />
us<strong>in</strong>g local specific ISIs with 11<br />
different thromboplast<strong>in</strong>s. No effect on the<br />
INR results was observed. 18 In another<br />
study us<strong>in</strong>g 11 different LA positive, 11<br />
negative LA subjects, and 7 different<br />
thromboplast<strong>in</strong>s, the presence of an LA<br />
did not disturb the laboratory tests for<br />
monitor<strong>in</strong>g subjects on OAT. 19 Each <strong>in</strong>stitution<br />
should check their own reagent/<strong>in</strong>strument<br />
comb<strong>in</strong>ation with positive LA<br />
plasmas to determ<strong>in</strong>e if the LA <strong>in</strong>terference<br />
is an issue <strong>in</strong> their laboratory.<br />
127
128<br />
Report<strong>in</strong>g of PT/INR results<br />
There cont<strong>in</strong>ues to be no consensus<br />
on the method of report<strong>in</strong>g INR values for<br />
conditions other than OAT. Many laboratories<br />
report only the INR for all PT measurements<br />
s<strong>in</strong>ce the INR is simply a<br />
mathematical conversion of the PT us<strong>in</strong>g<br />
the ISI. 9 Many laboratories have been reluctant<br />
to convert to low ISI thromboplast<strong>in</strong>s<br />
because the prolonged PTs are thought<br />
to be confus<strong>in</strong>g to physicians used to<br />
shorter PTs with high ISI (less sensitive)<br />
reagents. This may be true when a PT is<br />
ordered for situations other than monitor<strong>in</strong>g<br />
OAT. 9 A situation such as a preoperative<br />
coagulation screen or liver diseases<br />
can confuse the issue of INR report<strong>in</strong>g. It<br />
has been suggested by some cl<strong>in</strong>icians to<br />
use 2 systems for report<strong>in</strong>g PT results.<br />
One result for patients on OAT and<br />
another for subjects not on OAT has been<br />
<strong>in</strong>stituted at some facilities. There is data<br />
that suggests that the INR value is appropriate<br />
for use <strong>in</strong> patients beg<strong>in</strong>n<strong>in</strong>g anticoagulation<br />
as well as <strong>in</strong> subjects with other<br />
coagulation disorders (eg, liver<br />
impairment). The range of PT prolongation<br />
appears to be greater for patients on<br />
OAT than for patients with liver disease or<br />
dissem<strong>in</strong>ated <strong>in</strong>travascular coagulation, but<br />
the PT and INR has been shown to correlate<br />
<strong>in</strong> a l<strong>in</strong>ear fashion when reagents of<br />
vary<strong>in</strong>g ISI were compared. Some experts<br />
have proposed report<strong>in</strong>g the INR <strong>in</strong> lieu of<br />
the PT for all patients, but suggested the<br />
best way to accomplish this would be to<br />
have an <strong>in</strong>ternational consensus conference.<br />
This has still not been accomplished<br />
as recently as the 2001 International Society<br />
of Thrombosis and Hemostasis Conference<br />
<strong>in</strong> Paris, France. In the subcommittee<br />
conference that dealt with this issue, there<br />
was still no consensus on how to use the<br />
INR for other than those subjects on OAT.<br />
Some notable cl<strong>in</strong>icians and<br />
researchers have publicly stated that the<br />
INR is recommended as the most appropriate<br />
means for report<strong>in</strong>g PT results <strong>in</strong><br />
patients who are stable, orally anticoagulated.<br />
They have suggested that the INR is<br />
not appropriate for use <strong>in</strong> other cl<strong>in</strong>ical<br />
situations (eg, liver disease, hereditary<br />
factor deficiencies, rout<strong>in</strong>e screen<strong>in</strong>g, preoperative<br />
test<strong>in</strong>g, and detect<strong>in</strong>g vitam<strong>in</strong> K<br />
deficiency). There is little or no <strong>in</strong>formation<br />
available on the use of the INR report<strong>in</strong>g<br />
of drug-<strong>in</strong>duced coagulation defects <strong>in</strong><br />
subjects on OAT. Does a s<strong>in</strong>gle coagulation<br />
factor deficiency, such as a factor<br />
FVII deficiency, have a significant effect<br />
on the INR? 9 This could present problems<br />
<strong>in</strong> cl<strong>in</strong>ical sett<strong>in</strong>gs where the INR only is<br />
reported.<br />
Fairweather and colleagues 9 presented<br />
a further argument aga<strong>in</strong>st the use of report<strong>in</strong>g<br />
INRs only. The presence of a<br />
mildly prolonged PT may be the only clue<br />
to a cl<strong>in</strong>ically significant coagulopathy.<br />
However, the upper range of normal is<br />
obscured by the exponential nature of the<br />
INR calculation. The example they used<br />
discussed the upper limit of normal for 2<br />
reagents, which correspond to a PT ratio<br />
of 1.2. This would correspond to an INR<br />
of 1.2 for a reagent with an ISI of 1.0 and<br />
an INR of 1.4 for a reagent with an ISI of<br />
2.0. The problem would then be <strong>in</strong> <strong>in</strong>terpret<strong>in</strong>g<br />
the INR values <strong>in</strong> the range of 1.3<br />
to 1.4. One local hospital <strong>in</strong> our area went<br />
to INR value report<strong>in</strong>g because the surgeons<br />
would mis<strong>in</strong>terpret what they perceived<br />
to be mildly prolonged PTs.<br />
Consequently, they would order freshfrozen<br />
plasma for surgeries unnecessarily.<br />
F<strong>in</strong>al Notes<br />
The accuracy and precision of the INR<br />
is dependent on the PT assay and the ISI of<br />
thromboplast<strong>in</strong>. Other researchers have<br />
noted that s<strong>in</strong>ce the ISI is the exponent of<br />
the INR equation, the higher the ISI<br />
assigned to thromboplast<strong>in</strong>s the greater the<br />
imprecision of the INR as a result of the<br />
mathematical outcome. 20 In support of this<br />
<strong>in</strong>formation we discovered, <strong>in</strong> a study, that<br />
when the INR approaches 3.0 or greater<br />
the discrepancy <strong>in</strong> the INR value was between<br />
different reagent/<strong>in</strong>strument systems.<br />
Therefore the large difference <strong>in</strong> assigned<br />
ISI values is probably the most important<br />
variable that <strong>in</strong>fluences the poor correlation<br />
seen <strong>in</strong> different laboratories reagent/<strong>in</strong>strument<br />
comb<strong>in</strong>ations. Thromboplast<strong>in</strong>s with<br />
an ISI less than 1.2 produce a wider range<br />
of values <strong>in</strong> the PT and PT ratio. Consequently,<br />
the precision of the INR is similarly<br />
improved. S<strong>in</strong>ce the calculation of the<br />
INR requires us<strong>in</strong>g the ISI exponentially,<br />
the farther the ISI value is from 1.0, the<br />
less accurate the INR values will be.<br />
laboratorymedic<strong>in</strong>e> february 2003> number 2> volume 34<br />
©<br />
Manufacturer assigned ISIs, not specific to<br />
the local reagent/<strong>in</strong>strument set-up, may<br />
<strong>in</strong>troduce even more <strong>in</strong>accuracy.<br />
Instrumentation can also greatly <strong>in</strong>fluence<br />
the INR values. Because manufacturers<br />
provide limited guidel<strong>in</strong>es for <strong>in</strong>strument<br />
assigned ISIs, the laboratory should validate<br />
its coumad<strong>in</strong> <strong>in</strong>fluenced INR values<br />
by perform<strong>in</strong>g local on-site ISI calibration.<br />
If the laboratory <strong>in</strong> Pennsylvania had a protocol<br />
for locally calibrat<strong>in</strong>g their ISI values,<br />
the disaster that occurred with the <strong>in</strong>accurate<br />
ISI be<strong>in</strong>g used may have been averted.<br />
1. Adverse events and deaths associated with laboratory<br />
errors at a hospital-Pennsylvania, 2001. MMWR.<br />
2001:710-711.<br />
2. McCullough, Marie. Lab error deaths may now total<br />
five. The Inquirer (Philadelphia, PA), August 3, 2001.<br />
3. McGlasson DL. A review of variables affect<strong>in</strong>g<br />
PTs/INRs. Cl<strong>in</strong> Lab Sci. 1999;12:353-358.<br />
4. Cunn<strong>in</strong>gham MT, Johnson GF, Pennell BJ, et al. The<br />
reliability of manufacturer-determ<strong>in</strong>ed, <strong>in</strong>strumentspecific<br />
<strong>in</strong>ternational sensitivity <strong>in</strong>dex values for<br />
calculat<strong>in</strong>g the <strong>in</strong>ternational normalized ratio. AJCP.<br />
1994;102:128-133.<br />
5. Ts’ao C, Swedlund J, Neofotistos D. Implications of<br />
use of low <strong>in</strong>ternational sensitivity <strong>in</strong>dex<br />
thromboplast<strong>in</strong>s <strong>in</strong> prothromb<strong>in</strong> test<strong>in</strong>g. Arch Pathol<br />
Lab Med. 1994;118:1183-1187.<br />
6. Duncan EM, Casey CR, Duncan BM, et al. Effect of<br />
concentration of trisodium citrate anticoagulant on<br />
calculation of the <strong>in</strong>ternational normalized ratio and<br />
the <strong>in</strong>ternational sensitivity <strong>in</strong>dex of thromboplast<strong>in</strong>.<br />
Thromb Haemost. 1994;72:84-88.<br />
7. Adcock JM, Kressen DC, Marlar RA. Effect of 3.2%<br />
vs. 3.8% sodium citrate on rout<strong>in</strong>e coagulation<br />
test<strong>in</strong>g. Am J Cl<strong>in</strong> Pathol. 1997;107:105-110.<br />
8. Dwyre AL, Giles AR, Key LA, et al. The effects of<br />
sodium citrate anticoagulant concentration, storage on<br />
or off cellular matrix, and specimen age on<br />
prothromb<strong>in</strong> time INR us<strong>in</strong>g a low ISI (1.06) rabbit<br />
bra<strong>in</strong> thromboplast<strong>in</strong>. Thromb Haemost. 1995;73:1237.<br />
9. Fairweather RB, Ansell J, Anton M, et al. College of<br />
American Pathologists Conference XXXI on<br />
laboratory monitor<strong>in</strong>g of anticoagulant therapy:<br />
<strong>Laboratory</strong> monitor<strong>in</strong>g of oral anticoagulant therapy.<br />
Arch Pathol Med. 1998;122:768-781.<br />
10. NCCLS H21-A3. Collection, transport, and<br />
process<strong>in</strong>g of blood specimens for coagulation<br />
test<strong>in</strong>g and general performance of coagulation<br />
assays; approved guidel<strong>in</strong>e-3rd ed. 1998;18:20.<br />
11. Van den Besselaar AMHP, Halem-Visser LP,<br />
Loeliger EA. The use of evacuated tubes for blood<br />
collection <strong>in</strong> oral anticoagulant control. Thromb<br />
Haemost. 1983;50:676-677.<br />
12. Raskob GE, Durica SS, Owen WL, et al. Monitor<strong>in</strong>g<br />
low-dose warfar<strong>in</strong> therapy be a central laboratory<br />
and implications for cl<strong>in</strong>ical trials and patient care:<br />
the coumad<strong>in</strong> aspir<strong>in</strong> re<strong>in</strong>farction (CARS) pilot study<br />
group. Am J Cardiol. 1996;78:1074-1076.<br />
13. Bagl<strong>in</strong> T, Ludd<strong>in</strong>gton R. Reliability of delayed INR<br />
determ<strong>in</strong>ation: Implication for decentralized<br />
anticoagulant care with off-site blood sampl<strong>in</strong>g. Br J.<br />
Haematol. 1997;96:431-434.<br />
14. Foubister Vida. Quick on the draw-coagulation tube<br />
response. CAP Today. 2002;16:38-42.
15. McGlasson DL, Hickman JR, More LE, et al.<br />
Discrepancies <strong>in</strong> <strong>in</strong>ternational normalized ratios<br />
(INR) <strong>in</strong> sw<strong>in</strong>e and humans. Cl<strong>in</strong> Lab Sci.<br />
1998;11:156-160.<br />
16. McGlasson DL. A Comparison of <strong>in</strong>ternational<br />
normalized ratios after local calibration of thromboplast<strong>in</strong><br />
<strong>in</strong>ternational sensitivity <strong>in</strong>dexes. Accepted for<br />
Publication <strong>in</strong> Cl<strong>in</strong>ical <strong>Laboratory</strong> Science.<br />
17. Adcock DM, Johnston M. Evaluation of frozen<br />
plasma calibrants for enhanced standardization of the<br />
<strong>in</strong>ternational (INR): A multi-center study. Thromb<br />
Hemost. 2002;87:74-79.<br />
18. Mant MJ, Stang L, Etches WS. Warfar<strong>in</strong> monitor<strong>in</strong>g<br />
<strong>in</strong> patients with anticardiolip<strong>in</strong> antibodies, but<br />
without lupus anticoagulants. Thrombosis Research.<br />
2000;99:477-482.<br />
19. Bijsterveld NR, Middeldorp S, Berends F, et al.<br />
Monitor<strong>in</strong>g therapy with vitam<strong>in</strong> K antagonists <strong>in</strong><br />
patients with lupus anticoagulant: effect on different<br />
tests for INR determ<strong>in</strong>ation. J Thrombosis<br />
Thrombolysis. 2000;9:263-269.<br />
20. Van den Besselaar AMHP. Field study for<br />
lyophilized plasmas for local prothromb<strong>in</strong> time<br />
calibration <strong>in</strong> the Netherlands. J Cl<strong>in</strong> Pathol.<br />
1997;50:371-374.