Pseudomonilethrix type II and pili bifurcati - Test Page for Apache
Pseudomonilethrix type II and pili bifurcati - Test Page for Apache
Pseudomonilethrix type II and pili bifurcati - Test Page for Apache
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
4 Beasley KL, Cooley GE, Kao GF, Lowitt MH, Burnett JW,<br />
Aurelian L. Herpes simplex vegetans: atypical genital<br />
herpes infection in a patient with common variable<br />
immunodeficiency. J Am Acad Dermatol 1997; 37: 860–863.<br />
5 Samaratunga H, Weedon D, Musgrave N, McCallum N.<br />
Atypical presentation of herpes simplex (chronic<br />
hypertrophic herpes) in a patient with HIV infection.<br />
Pathology 2001; 33: 532–535.<br />
6 Fangman WL, Rao CH, Myers SA. Hypertrophic herpes<br />
simplex virus in HIV patients. J Drugs Dermatol 2003; 2:<br />
198–201.<br />
7 Fox PA, Barton SE, Francis N et al. Chronic erosive herpes<br />
simplex virus infection of the penis, a possible immune<br />
reconstitution disease. HIV Med 1999; 1: 10–18.<br />
8 Fife KH, Crumpacker CS, Mertz GJ, Hill EL, Boone GS.<br />
Recurrence <strong>and</strong> resistance patterns of herpes simplex virus<br />
following cessation of > or = 6 years of chronic suppression<br />
with acyclovir. Acyclovir Study Group. J Infect Dis 1994; 169:<br />
1338–1341.<br />
9 Pechère M, Wunderli W, Trellu-Toutous L, Harms M, Saurat<br />
JH, Krischer J. Treatment of acyclovir-resistant herpetic<br />
ulceration with topical foscarnet <strong>and</strong> antiviral sensitivity<br />
analysis. Dermatology 1998; 197: 278–280.<br />
10 Bevilacqua F, Marcello A, Toni M et al. Acyclovir resistance/<br />
susceptibility in herpes simplex virus <strong>type</strong> 2 sequential<br />
isolates from an AIDS patient. J Acquir Immune Defic Syndr<br />
1991; 4: 967–969.<br />
DOI: 10.1111/j.1468-3083.2006.01561.x<br />
? 18 ?Letter Letters LETTERS 2006to<br />
to the TO the Editor THE Editor EDITOR<br />
<strong>Pseudomonilethrix</strong> <strong>type</strong> <strong>II</strong> <strong>and</strong> <strong>pili</strong><br />
<strong>bifurcati</strong><br />
Editor<br />
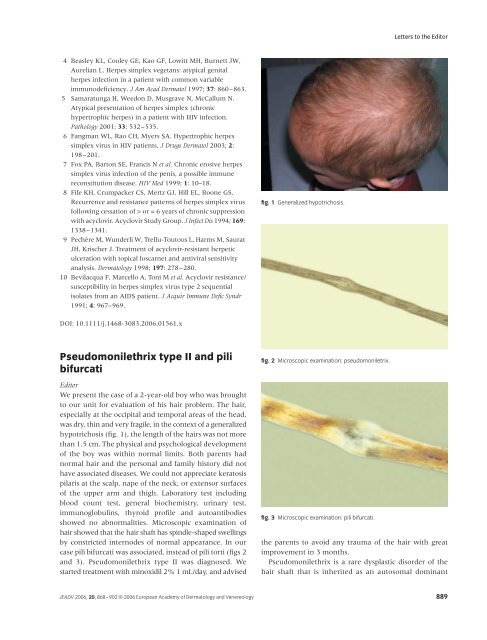
We present the case of a 2-year-old boy who was brought<br />
to our unit <strong>for</strong> evaluation of his hair problem. The hair,<br />
especially at the occipital <strong>and</strong> temporal areas of the head,<br />
was dry, thin <strong>and</strong> very fragile, in the context of a generalized<br />
hypotrichosis (fig. 1), the length of the hairs was not more<br />
than 1.5 cm. The physical <strong>and</strong> psychological development<br />
of the boy was within normal limits. Both parents had<br />
normal hair <strong>and</strong> the personal <strong>and</strong> family history did not<br />
have associated diseases. We could not appreciate keratosis<br />
pilaris at the scalp, nape of the neck, or extensor surfaces<br />
of the upper arm <strong>and</strong> thigh. Laboratory test including<br />
blood count test, general biochemistry, urinary test,<br />
immunoglobulins, thyroid profile <strong>and</strong> autoantibodies<br />
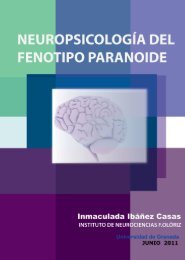
showed no abnormalities. Microscopic examination of<br />
hair showed that the hair shaft has spindle-shaped swellings<br />
by constricted internodes of normal appearance. In our<br />
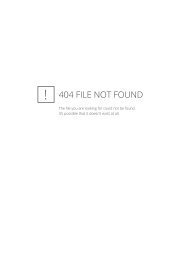
case <strong>pili</strong> <strong>bifurcati</strong> was associated, instead of <strong>pili</strong> torti (figs 2<br />
<strong>and</strong> 3). <strong>Pseudomonilethrix</strong> <strong>type</strong> <strong>II</strong> was diagnosed. We<br />
started treatment with minoxidil 2% 1 mL/day, <strong>and</strong> advised<br />
fig. 1 Generalized hypotrichosis.<br />
fig. 2 Microscopic examination: pseudomoniletrix.<br />
fig. 3 Microscopic examination: <strong>pili</strong> <strong>bifurcati</strong>.<br />
Letters to the Editor<br />
the parents to avoid any trauma of the hair with great<br />
improvement in 3 months.<br />
<strong>Pseudomonilethrix</strong> is a rare dysplastic disorder of the<br />
hair shaft that is inherited as an autosomal dominant<br />
JEADV 2006, 20, 868–902 © 2006 European Academy of Dermatology <strong>and</strong> Venereology 889
Letters to the Editor<br />
trait with high penetrance but variable expressivity. It was<br />
first described by Bentley-Phillips <strong>and</strong> Bayles 1 in 1973 <strong>and</strong><br />
clinically affects the whole scalp as a generalized hypotrichosis<br />
or just the occipital area. <strong>Pseudomonilethrix</strong> usually<br />
starts in the first months of life, although, in some<br />
cases, it does not become apparent until childhood. No<br />
follicular papules can be seen on physical examination. 2<br />
<strong>Pseudomonilethrix</strong> has been classiffied in three different<br />
<strong>type</strong>s: I, familiar pseudomonilethrix of Bentley-Phillips<br />
(autosomal dominant inheritance); <strong>II</strong>, acquired pseudomonilethrix<br />
in dysplastic disorders with hair fragility<br />
(inheritance profile depending on the dysplastic disorder);<br />
<strong>and</strong> <strong>II</strong>I, iatrogenic pseudomonilethrix. 3<br />
Diagnosis can be easily made by microscopic examination<br />
of the hair shaft. Elliptical nodes <strong>for</strong>m along the hair shaft<br />
at variable intervals <strong>and</strong> separated by narrower internodes.<br />
Differential diagnosis with monilethrix is obligated.<br />
Monilethrix is an autosomal dominant disorder characterized<br />
by a beaded appearance of the hair due to periodic<br />
thinning of the shaft. 4 The pheno<strong>type</strong> results in hair fragility<br />
<strong>and</strong> patchy dystrophic alopecia. Keratosis pilaris<br />
is almost invariably associated with monilethrix unlike<br />
pseudomonilethrix. Concomitant ectodermal defects<br />
have been reported in the literature as dental abnormalities,<br />
juvenile cataracts, <strong>and</strong> some neurologic defects that<br />
appear as a cognitive deficiency or epilepsy. Pili torti or<br />
partial <strong>for</strong>ms of trichorrhexis nodosa have been associated<br />
with the second <strong>type</strong> of this hair disorder. There are<br />
no previous reports of <strong>pili</strong> <strong>bifurcati</strong> <strong>and</strong> pseudomonilethrix<br />
in the literature, as the clinical case that we<br />
present. The avoidance of trauma is the most effective<br />
method of managing this anomaly. 5<br />
R Ruiz-Villaverde,† A Villanova-Mateu,‡<br />
R Ortega del Olmo,‡ D Sanchez-Cano§<br />
†Dermatology Unit, Hospital de Poniente, El Ejido, Almería,<br />
†Dermatology Unit, Hospital Clínico Universitario de Granada,<br />
<strong>and</strong> ‡Internal Medicine, Hospital Clínico Universitario de<br />
Granada, Granada, Spain, *Corresponding author, Lopez Font<br />
n°10 5°A4, 18004-Granada, Spain,<br />
E-mail: ismenios@hotmail.com<br />
References<br />
1 Bentley-Phillips B, Bayles MA. A previously undescribed<br />
hereditary hair anomaly pseudo-monilethrix. Br J Dermatol<br />
1973; 89: 159–167.<br />
2 Rogers M. Hair shaft abnormalities: Part <strong>II</strong>. Australas J<br />
Dermatol 1996; 37: 1–11.<br />
3 Ferr<strong>and</strong>o J, Fontarnau R, Haussman G. Is pseudomonilethrix<br />
an artifact? Int J Dermatol 1990; 29: 380–381.<br />
4 Camacho-Martinez F, Ferr<strong>and</strong>o J. Hair shaft dysplasias. Int J<br />
Dermatol 1988; 27: 71–80.<br />
5 Sotiriou E, Sotiriadis D. Monilethrix. Eur J Pediatr Dermatol<br />
2002; 12: 101–104.<br />
DOI: 10.1111/j.1468-3083.2006.01564.x<br />
? 18 ?Letter Letters LETTERS 2006to<br />
to the TO the Editor THE Editor EDITOR<br />
Adult-onset Langerhans cell<br />
histiocytosis confined to the skin<br />
Editor<br />
Langerhans cell histiocytosis (LCH) is a clonal, pleomorphic<br />
disease of unknown aetiology, with the<br />
accumulation of local or disseminated atypical histiocytic<br />
cells staining positively <strong>for</strong> S-100 <strong>and</strong> CD-1a, <strong>and</strong> causing<br />
damage in the bones, lungs, mucocutaneous structures<br />
<strong>and</strong> endocrine organs. 1 The condition is generally diagnosed<br />
in infancy <strong>and</strong> childhood, but onset in adulthood<br />
can occasionally occur. The eruption is usually diffuse or<br />
manifests as part of a multisystemic disease, <strong>and</strong> up to 25–<br />
50% of patients with LCH will present initially with a<br />
cutaneous rash. 1–5 Cutaneous manifestations are heterogenous<br />
<strong>and</strong> similar both in children <strong>and</strong> adults. 1,2 LCH<br />
confined to the skin is uncommon among reported cases<br />
of adults. 2–8 We describe a rare case of adult-onset LCH<br />
presenting as cutaneous lesions located symmetrically on<br />
the scalp, groin <strong>and</strong> inframammarian areas, <strong>and</strong> review the<br />
literature <strong>for</strong> previous adult cases of isolated cutaneous<br />
LCH.<br />
A 38-year-old woman presented to our dermatology<br />
department with a-two-year duration of red, painful skin<br />
ulcerations in the inframammary <strong>and</strong> inguinal areas<br />
located bilaterally, <strong>and</strong> severe crusting <strong>and</strong> scaling of the<br />
scalp. Skin examination showed diffuse yellowish crusting<br />
with erosions involving the scalp <strong>and</strong> extending beyond<br />
the hairline onto the <strong>for</strong>ehead (fig. 1) <strong>and</strong> symmetrically<br />
distributed sharp-edged, ulcerated plaques with a small<br />
fig. 1 Erythematous, erosive, ulcerated plaques on right inframammarian<br />
fold.<br />
890 JEADV 2006, 20, 868–902 © 2006 European Academy of Dermatology <strong>and</strong> Venereology