Remineralization with CPP-ACP: - GC Europe
Remineralization with CPP-ACP: - GC Europe
Remineralization with CPP-ACP: - GC Europe
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
mid<br />
<strong>Remineralization</strong> <strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong>:<br />
minimum intervention, maximum return<br />
the evidence<br />
Hands on,<br />
drills off<br />
Remineralisation <strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong>’ to MIH:<br />
the treatment protocol<br />
Remineralisation<br />
<strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong><br />
MID<br />
resources<br />
Issue 3
Prevention starts <strong>with</strong><br />
risks identification<br />
and personal motivation<br />
Plaque Indicator Kit from <strong>GC</strong>.<br />
Identify plaque cariogenicity and age <strong>with</strong>in 5 minutes<br />
<strong>GC</strong> EUROPE N.V.<br />
Head Office<br />
Tel. +32.16.74.10.00<br />
info@gceurope.com<br />
www.gceurope.com<br />
<strong>GC</strong> UNITED KINGDOM Ltd.<br />
Tel. +44.1908.218.999<br />
info@uk.gceurope.com<br />
www.uk.gceurope.com<br />
Plaque formation is a<br />
normal occurrence for<br />
most of the population.<br />
To determine the potential<br />
damage plaque can cause<br />
and discover exactly which<br />
plaque sites are more<br />
problematic than others can<br />
be difficult to identify.<br />
Plaque Indicator Kit is a simple and<br />
inexpensive test that quickly identifies<br />
and visually communicates the problem<br />
to motivate and educate patients.<br />
Minimum<br />
Intervention
minimum intervention, maximum return<br />
What’s inside<br />
MID 3 video<br />
4. MID Worldwide<br />
mid<br />
Issue 3<br />
Thanks to the cooperation of academia, the profession and industry leadership<br />
by <strong>GC</strong>, Minimum Intervention Dentistry principles are adopted and promoted<br />
around the world, to the ultimate bene t of the patient community.<br />
6. Q&A<br />
Dr Graham Mount answers a question about what he has found to be the most<br />
e ective way to apply <strong>CPP</strong>-<strong>ACP</strong><br />
7. Resources<br />
Networks, websites, books, events and journal articles relating<br />
to advances in MID<br />
8. Practice perspectives<br />
• Hands on, drills off<br />
10. Clinical corner<br />
• MIH: the evidence and treatment protocol<br />
• White spot reversal protocol<br />
• Topical <strong>CPP</strong>-<strong>ACP</strong> crème (Tooth Mousse): more evidence<br />
that demands a verdict<br />
26. Evidence<br />
• A closer look at remineralisation and <strong>CPP</strong>-<strong>ACP</strong><br />
30. MI toolkit<br />
• Tooth Mousse: All you need to know<br />
mi.gceurope.com
worldwide<br />
MID Worldwide<br />
Thanks to the cooperation of academia, the profession and industry leadership<br />
by <strong>GC</strong>, Minimum Intervention Dentistry principles are adopted and promoted<br />
around the world, to the ultimate bene t of the patient community.<br />
Dr Matteo Basso<br />
As a student, I did my internship in<br />
the Department of Periodontology<br />
at the University of Milan, directed by<br />
Professor Roberto Weinstein. In that<br />
department, the concepts of minimally<br />
invasive dentistry had been rmly<br />
ingrained for many years and advanced periodontal<br />
procedures were envied and admired nationally and<br />
internationally. Here I learnt the importance of the<br />
preservation of healthy tissue as a fundamental condition<br />
for the success of treatment, both functionally and<br />
aesthetically. After graduation and obtaining a PhD, I<br />
became the head of restorative dentistry at the university<br />
dental clinic, IRCCS Galeazzi Orthopaedic Institute<br />
in Milan (Italy). There, I realized it was a good approach<br />
to change concepts of minimally invasive therapy,<br />
Italy MID<br />
possible only when a disease is already established,<br />
towards the concept of ‘minimum intervention’, in other<br />
words to intervene when the disease has not yet had an<br />
irreversible e ect on the teeth and gums.<br />
The literature helped us to comprehend what ‘minimum<br />
intervention’ actually is. And so, the traditional<br />
department of restorative dentistry quickly evolved<br />
into a new department, built on these ideas, called the<br />
Center of Aesthetic and Mininvasive Oral Rehabilitation<br />
(CROME). The goal of this centre is to intervene early in<br />
carious disease, seeking not only to treat cavities, however<br />
necessary, but also to understand why the carious<br />
lesions manifested themselves in the rst place. One of<br />
our challenges is to see if you can change the susceptibility<br />
of patients in order to protect their teeth and masticatory<br />
ability. It was not so easy to explain to patients<br />
all the reasons and the importance of this approach,<br />
4 mid worldwide<br />
mi.gceurope.com
China<br />
but after several years, we can say that the programme<br />
is a big success in tooth preservation. To create a form of<br />
restorative dentistry that can prevent the intervention of<br />
the periodontist, the prosthodontist or implantologist for<br />
as long as possible is the main goal for me and my sta .<br />
The adoption of the MID, once understood, is very<br />
simple. However, we cannot hide that the rst and biggest<br />
challenge is the identi cation of clear guidelines for the<br />
correct application of MID into the clinical reality of each<br />
dentist. Still too many dentists observe the magni cent<br />
results of some colleagues who publish books and<br />
magazines on MID, but still wonder how they can integrate<br />
it into their own situations. Some are even afraid to make<br />
the patients pay for preventive diagnostic procedures, and<br />
therefore they prefer not to perform diagnosis and tests,<br />
intervening when there is already an established disease<br />
or, even worse, when the disease can be only treated<br />
Dr Zhouqun Yan, <strong>GC</strong> China<br />
There is an increasing awareness of MI among the Chinese<br />
dental profession. This is due to information in international<br />
journals and returning overseas dentists who have studied<br />
abroad for postgraduate degrees or special research projects.<br />
However, due to the requirement of an import license for any<br />
item regarded as a dental device, most ‘state of the art’ items<br />
including MI products are not available for Chinese dentists at the same time as<br />
other countries. Some successful items take years to satisfy the strict governmental<br />
requirements. To emphasise this, Tooth Mousse was only launched in China at<br />
the end of 2009. At present, most of the products available in China t into the<br />
repair category of the MI concept and products like <strong>GC</strong> Fuji IX GP are popular in<br />
government dental clinics. It is di cult to embrace the complete MI concept in<br />
the majority of government clinics at this stage but private dentists have already<br />
realized the MI concept of diagnosis, prevention and repair is the future.<br />
In the large cities like Beijing and Shanghai, it is possible to run a successful<br />
dental practice based on MI principles. However, more information and education<br />
about MI is the key to boost the concept in these cities.<br />
<strong>GC</strong> Fuji IX GP is the bestselling MI product in China and complies <strong>with</strong> the<br />
‘easier, faster and better’ concept of Dr Gordon Christensen and other leading<br />
clinicians around the world. Economic reasons dictate that only the hand-mix<br />
version of Fuji IX GP is popular here. This special high strength glass ionomer<br />
has changed the way dentists work throughout China. It is also important to<br />
understand that China is a developing country and the ART technique is very<br />
important in remote areas. <strong>GC</strong> is working together <strong>with</strong> local KOLs and government<br />
departments to boost the availability of ART there. Fuji IX GP is the key to<br />
the success in these areas and overall sales have doubled over the past 2 years.<br />
MI dentistry is the future. It is not only a <strong>GC</strong> story but the future for the<br />
dental profession everywhere in the world. It is not something that costs extra<br />
money but can help dentists earn more. MI will eventually reduce costs for<br />
patients if they are also educated in proper oral care and embrace the principles<br />
as there will be less invasive treatment necessary. One of the exciting long<br />
term projects will be to work <strong>with</strong> policymakers to train dental professionals to<br />
identify and heal early lesions rather than watch and wait for them to progress<br />
to cavitation. MI will mean that dentists and nurses will be busier than ever but<br />
<strong>with</strong> many new and di erent roles in the practice.<br />
conservatively <strong>with</strong> the ‘drill, ll and bill’ option.<br />
Sometimes dentists are not helped by di erent<br />
situations in <strong>Europe</strong>an countries: for example, in some<br />
countries there is no profession of the dental hygienist,<br />
a role in other countries which is championing the MID<br />
drive. The MID principles are certainly not so easy to<br />
introduce immediately into clinical daily practice, because<br />
it requires dentists to evaluate their own resources<br />
(sta , hygienist, number of dental chairs, availability of<br />
patients) and sometimes to signi cantly change their<br />
habits of diagnosis and treatments.<br />
Minimum intervention dentistry is a eld that is in<br />
continuous expansion. Its potential results, in terms of<br />
successful treatment <strong>with</strong> aesthetic success and conservation<br />
of the masticatory function, are huge compared<br />
to its di usion, which is unfortunately still small <strong>with</strong>in<br />
the national territory.<br />
mid worldwide<br />
5
Q&A<br />
The question below was sent to<br />
Dr Graham Mount in response<br />
to his article in MID 2<br />
Name: Jack Stellpflug<br />
Country: USA<br />
Question: Can Dr Mount comment on the most effective way he has found to apply CCP-<strong>ACP</strong>?<br />
Answer – Dr Graham Mount<br />
Dear Jack Stellpflug,<br />
The material CCP-<strong>ACP</strong>, developed in Melbourne, came from a desire to be able to<br />
remineralise a demineralised enamel or dentine lesion in depth. As you are aware the<br />
application of fluoride in one form or another will tend to remineralise the surface<br />
first and will tend to prevent the further penetration of ions in to the depths of the<br />
lesion. This may well minimize the further demineralisation of the area but it will not<br />
overcome the level of porosity of the tooth structure in depth. In other words a ‘white<br />
spot lesion’ may well remain visible to the naked eye even though the lesion is sealed<br />
from further loss of ions in the short term.<br />
On the other hand the <strong>CPP</strong>-<strong>ACP</strong> will penetrate to the full depth of the<br />
demineralisation and will successfully deposit both calcium and phosphate ions to<br />
the full depth of the lesion thus overcoming the ‘white spot’ entirely. Add the fluoride<br />
ion to it and the resistance to further demineralisation will be further enhanced – that<br />
is, use Tooth Mousse Plus.<br />
This means that the preferred timing and method of application will be to apply<br />
when the disease is first diagnosed and before any other fluoride therapy has<br />
been introduced. The most effective way is to make a personal plastic ‘pull-down’<br />
specifically for the patient. Apply daily, carry out normal hygiene then apply pulldown<br />
loaded <strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong> paste and leave in place for say 15 minutes on each<br />
occasion. Treatment may need to last for 2 weeks or thereabouts, longer if desired.<br />
As part of an overall anti-caries discipline for the high risk patient or one <strong>with</strong> cervical<br />
sensitivity it can also be applied <strong>with</strong> the finger after cleaning any time and leave it<br />
on the teeth for as long as you like. It will wash away quite quickly of course but in<br />
the meantime will have transferred a reasonable dose of ions to the dentine beneath<br />
assisting in closing over the tubules.<br />
Yours sincerely,<br />
Graham Mount<br />
Melbourne, Australia<br />
6 q&a<br />
mi.gceurope.com
MID resources<br />
This is a collection of online resources on MID for dental professionals and patients<br />
Online<br />
Dental Village<br />
Dentalvillage is an online resource developed my two dental hygienists,<br />
Dave Bridges and Tim Ives who are passionate about raising the profi le<br />
of MID among the public and healthcare professions. The site has up<br />
to date information on this fresh approach to preventing dental decay<br />
and periodontal (gum) diseases.<br />
Excerpt: The focus is on maximum conservation of demineralised, noncavitated<br />
enamel and dentine. Once control of the infection is achieved,<br />
the patient’s caries risk status and evidence of lesion demineralisation<br />
can be monitored over extended periods. These principles can also<br />
be applied to the treatment and management of periodontal disease.<br />
Minimally Invasive Periodontal Management relies heavily on patient<br />
involvement, ownership and management of their own disease. The<br />
patient reduces their own infl ammation under guidance of the clinician<br />
and operative treatment is kept as minimal as possible.<br />
Click here: dentalvillage.co.uk<br />
Dental Caries Classi cation Grid<br />
An online resource run by Graham Mount, Wyatt Rory Hume and<br />
Brian Monteith has an interactive dental caries classifi cation grid<br />
based on MID principles that introduces an alternative to the GV Black<br />
classifi cation system.<br />
Excerpt: A revised understanding of the caries lesion<br />
In recent times the term “Minimal Intervention Dentistry” has been<br />
coined to describe a new approach to the treatment of early carious<br />
lesions. It is now clearly acknowledged that caries is a bacterial disease<br />
and treatment should therefore revolve primarily around overcoming<br />
the infection.<br />
Click here: http://www.midentistry.org/grid.html<br />
California Dental Association Journal Back Issues<br />
The California Dental Association has made the back issues of its journal<br />
available for download online through its website.<br />
Excerpt: The Journal of the California Dental Association is an awardwinning<br />
monthly peer-reviewed scientifi c publication keeps dentists<br />
up-to-date about scientifi c advances, business management strategies<br />
and new products. It also features thought-provoking editorials,<br />
comprehensive statewide continuing education listings, California<br />
practices for sale, and dentistry’s favourite humour columnist - Dr Bob,<br />
Robert E. Horseman, DDS.<br />
Click here: http://www.cda.org/publications/journal_of_the_<br />
california_dental_association<br />
MID patient factsheet<br />
Academy of General Dentistry has compiled a useful document that<br />
explains the principles of MID to patients<br />
Click here: http://www.midentistry.com/AGD-MI.pdf<br />
Professor Brian Nový articles<br />
Professor Nový is featured in the USA<br />
version of the MID ezine, compiled by <strong>GC</strong><br />
America – click here to read the issue<br />
He is a renowned MID advocate and<br />
here is a list of some of his most recent<br />
publications:<br />
The Material Science of Minimally<br />
Invasive Restorations. Compendium of<br />
Continuing Education in Dentistry, July<br />
2008.<br />
Salivary Diagnostics: Practical<br />
Applications. AGD Impact. September 2009.<br />
Glass ionomers: Invaluable materials in<br />
today’s dental operatory. National Network<br />
for Oral Health Access Quarterly Newsletter.<br />
Winter 2009: 2(1).<br />
Profi le in Oral Health: Treating the Caries<br />
Disease, an interview <strong>with</strong> Dr. Brian B. Nový.<br />
Dental Town Magazine. April 2009 10(4):<br />
90-94.<br />
Dental Caries: A pH mediated disease.<br />
Journal of the California Dental Hygienist’s<br />
Association, Winter 2010: 25(1).<br />
Social media<br />
Here is an overview of MID related resources<br />
that you can follow through social media<br />
Facebook<br />
MI Paste (Tooth Mousse) fanpage<br />
Click here: http://www.facebook.com/#!/<br />
mi.paste?ref=ts<br />
Twitter<br />
MI Paste (Tooth Mousse)<br />
Click here: http://twitter.com/mipaste<br />
Carifree<br />
Click here: http://twitter.com/CariFree<br />
resources<br />
7
Hands on, drills off<br />
Dr Kirk Young is the practice principal and owner of Young’s Dental Practice, which was<br />
awarded the 2009 Preventive Practice of the Year award. MID recently spoke to him about his<br />
practice and what motivates him to pursue MID.<br />
“I always<br />
preferred<br />
doing<br />
prevention<br />
rather than<br />
extractions<br />
anyway”<br />
MID: What goes into achieving the title of<br />
Preventive Practice of the Year?<br />
Dr Kirk Young: According to the judges<br />
of this award, our dedication to improving<br />
patient care, passion and enthusiasm for MID<br />
in our practice is evident. In our practice we<br />
also have a physiotherapy and sports injury<br />
clinic and this all contributes to us being an<br />
overall preventive practice. An essential part<br />
of our success is excellent teamwork: from the<br />
reception staff, the nurses to the hygienists<br />
and dentists.<br />
The MI systems, materials and techniques<br />
that we have put in place at the practice<br />
have taken us many years to implement fully<br />
and we have spent a great deal of time and<br />
consideration on each. It certainly didn’t<br />
happen overnight!<br />
Years ago I was looking for a mentor in<br />
dentistry to inspire me. I met Hien Ngo at<br />
a conference and heard him speak quite<br />
a few times and his ideas influenced me<br />
tremendously. I always preferred doing<br />
prevention rather than extractions anyway.<br />
Another move in the right direction came<br />
when we stopped being an NHS practice<br />
four years ago. When the new NHS contract<br />
was announced I realised that the prevention<br />
component was not included. I felt we couldn’t<br />
give patients adequate care in prevention on<br />
the NHS so we became a private practice.<br />
We told the patients what was happening<br />
and why we were changing and they<br />
had already become used to our way of<br />
performing preventive dentistry. We always<br />
try to keep the patients involved – our<br />
website has many resources on MID and<br />
prevention for them.<br />
Winning the award has been a great<br />
recognition for the whole team and confirmed<br />
to us that what we are doing <strong>with</strong> MID and<br />
prevention is the way forward.<br />
MID: What techniques and strategies have<br />
you found to work best for doing preventive<br />
dentistry?<br />
Dr Kirk Young: Keeping patients informed<br />
is crucial. We have to show them what we<br />
have to offer and we do this through our<br />
newsletter, which every patient receives at a<br />
recall appointment. In it we publish content<br />
about the benefits of MID and prevention,<br />
and we highlight the equipment that helps<br />
us to practice preventively, such as Cariescan,<br />
The Wand, Healozone and Velopex.<br />
Using an intraoral camera is another<br />
excellent way get the patient involved in the<br />
problem. You don’t just tell them they have a<br />
disease, but you also show them where it is,<br />
how it looks and what it is doing. One of the<br />
cornerstones of MID is that it’s not a one way<br />
partnership between the patient and dentist.<br />
You need increased patient involvement to<br />
make this work.<br />
Education the team is another important<br />
facet and we have spent a great deal of time<br />
training together <strong>with</strong> the whole team. When<br />
the team members fully understand the<br />
8 practice perspectives<br />
mi.gceurope.com
enefits of MID they can explain it better to<br />
the patients and communicate the benefits<br />
more effectively to them.<br />
We also make use of questionnaires and<br />
work through these <strong>with</strong> the patients, in order<br />
to assess their caries risk. Our staff members<br />
are fully trained to undertake this because we<br />
find that sometimes the patients feel more<br />
comfortable to share this kind of information<br />
<strong>with</strong> the staff members. Everyone is focused on<br />
the practice having healthy and happy patients.<br />
MID: To what extent do you conduct practice<br />
based research in MID topics?<br />
Dr Kirk Young: Everything is recorded<br />
in our practice. Every patient fills out a<br />
comprehensive MID questionnaire, which<br />
is evaluated at every recall to see what<br />
treatment has worked or to monitor the<br />
progress. Our practice management software<br />
allows us to record all this data so we can<br />
chart the patient’s progress at each recall. At<br />
every appointment we measure the caries<br />
risk using the ‘traffic light system’ which is<br />
determined by using the intra-oral camera<br />
and questionnaires. All the oral hygiene and<br />
dietary advice given to each patient is also<br />
recorded to we can track their behaviour.<br />
Last year my practice data was used by Dr<br />
Avijit Banerjee at a conference presentation.<br />
I think it’s important to not only practice MID<br />
but to record and capture how we are treating<br />
patients so we can build the evidence base.<br />
MID: What advice would you give dentists<br />
who are considering moving over to an MIDcentered<br />
practice model?<br />
Dr Kirk Young:<br />
• Invest in team building and training.<br />
• Teach patients to self-prevent tooth decay<br />
proactively, rather than treating it reactively<br />
• Build your practice systems up gradually<br />
• Go to talks, attend courses <strong>with</strong> your team,<br />
join study groups; try to get as much<br />
information about MID as you can.<br />
• Invest in dental caries detection systems<br />
such as Diagnodent, Cariescan, SapproLife<br />
and use them every day<br />
• Make use of remineralisation products – they<br />
have a huge body of evidence behind them<br />
that support their efficacy<br />
• Keep on top of new developments: Air<br />
abrasion is another emerging aspect to MID<br />
- new research shows that bioactiveglass<br />
material can cut through enamel very<br />
quickly and can kickstart the reminerlisation<br />
process in the teeth<br />
I am still surprised to see how few dentists<br />
have intraoral cameras in their practices. In<br />
some countries this is second nature. I hope<br />
to see this change in the UK. MID is the<br />
buzzword in dentistry at the moment, it is no<br />
longer a marginal activity, everyone is talking<br />
about it. It is the way forward for dentistry<br />
For more information about the practice visit<br />
www.youngsdentalpractice.co.uk<br />
A day in the life at Young’s Dental Practice<br />
Sally Wright, practice manager<br />
I enjoy most being part of a team who are all working towards the same goal - for all clients to be<br />
dentally fit etc. I also enjoy organising Kirk’s lectures and taking part in them and co-ordinating<br />
<strong>with</strong> the dental companies supporting MID. I probably gain most enjoyment from patient<br />
interaction especially when involving them in their care which includes oral health, diet and<br />
grinding advice.<br />
My specific roles include educating patients by oral hygiene instruction and diet advice,<br />
grinding appliance demonstration and advice. I also give patients information on the techniques<br />
and equipment we use such as air abrasion for MID. I am responsible for doing MID marketing by creating leaflets,<br />
website updates and brochures. I help <strong>with</strong> MID lectures and discussions <strong>with</strong> GDPs / VDPs and I advise patients on<br />
different most up to date products to assist them at home in prevention.<br />
I think we have been so successful as a team because we are all big believers in MID. We also spend a large<br />
amount of time <strong>with</strong> our patients implementing MID and great part of it is education. We also use intra-oral cameras<br />
routinely for examinations and patients are offered separate time <strong>with</strong> a DCP for any advice.<br />
practice perspectives<br />
9
MIH: the evidence and treatment protocols<br />
By Dr Felicity Crombie and Dr David Manton<br />
While developmental defects have long been<br />
identified in human enamel, recently a new condition<br />
has been described: molar incisor hypomineralisation<br />
(MIH). First suggested as a distinct diagnosis by<br />
Weerheijm et al in 2001 it is defined as demarcated,<br />
qualitative defects of enamel (hypomineralisation) of<br />
systemic origin of one to four permanent first molars,<br />
frequently associated <strong>with</strong> affected incisors 1. Given<br />
the propensity of affected molars to break down<br />
rapidly and/or develop caries there is some debate<br />
as to whether this condition constitutes a new entity<br />
or has simply become more apparent as caries rates<br />
decrease and accurate diagnosis improves, both in<br />
regards to differentiating between true hypoplasia<br />
and post-eruptive breakdown (PEB) and recognition<br />
of abnormal caries patterns/presentation. The<br />
distribution of the condition is often asymmetric,<br />
<strong>with</strong> marked variation in severity common <strong>with</strong>in an<br />
individual. The likelihood that incisors are affected<br />
has been reported to increase as the number and<br />
severity of molar lesions increases 2 .<br />
Affected teeth present patients and clinicians<br />
alike <strong>with</strong> many challenges <strong>with</strong> aesthetic issues,<br />
hypersensitivity, difficulty achieving adequate local<br />
analgesia and difficulty providing adequate and<br />
enduring restorations all reported in association <strong>with</strong><br />
MIH1,3. Children <strong>with</strong> teeth affected by MIH undergo<br />
up to ten times the treatment of unaffected children<br />
by the age of 8 years and have significantly higher<br />
levels of dental anxiety<br />
and phobia 4,5. These<br />
factors combined<br />
<strong>with</strong> the<br />
fact that extraction is often the most appropriate<br />
definitive treatment option means general<br />
anaesthetic management, <strong>with</strong> its attendant increase<br />
in risk and cost, is often required 6-8.<br />
Prevalence<br />
Prevalence studies are increasingly investigating MIH<br />
specifically and using newly developed indices tailored<br />
for this purpose 9,10 ; however the majority of published<br />
studies have used either non-standard indices or<br />
the Developmental Defects of Enamel (DDE) Index.<br />
Caution must therefore be applied when interpreting<br />
prevalence data as the DDE Index has the potential to<br />
both over- and under- estimate the true prevalence<br />
of MIH since: MIH is not the only cause of demarcated<br />
enamel defects; caries, PEB, restoration and extraction<br />
are not accounted for by the DDE Index and PEB may<br />
be classified incorrectly as hypoplasia.<br />
A recent review of MIH prevalence data found that<br />
the prevalence varied widely <strong>with</strong> values from 2.4%<br />
to 40.2% reported11. The majority of studies were<br />
performed using <strong>Europe</strong>an populations and ranged<br />
from 2.4% in Germany and Bulgaria to 37.5% in<br />
Denmark. Worldwide a low prevalence has been<br />
reported in Hong Kong (2.8%) and Libya (2.9%)<br />
increasing to 13.7% in Kenya, 22% in Australia<br />
and up to 40.2% in Brazil. The lack of standardized<br />
examination protocols as well as the aforementioned<br />
index limitations must be considered when<br />
comparing these results. Although difficult to<br />
establish given the lack of reliable, comparable<br />
prevalence data worryingly many clinicians feel the<br />
prevalence of MIH is increasing3, 12.<br />
Aetiological factors<br />
The limitations of experimental design and study<br />
comparability identified for prevalence data also<br />
apply to a review of MIH aetiology. Bearing this in<br />
mind a critical literature review found: very little<br />
evidence to support a relationship between<br />
breast-feeding or fluoride exposure and<br />
demarcated enamel defects; moderate<br />
evidence that exposure to PCB/dioxins may<br />
be associated <strong>with</strong> an increased prevalence<br />
of these lesions; maternal factors, birth<br />
complications, nutritional status, childhood<br />
illness and medical conditions appear to<br />
exert some influence on the prevalence<br />
of enamel defects generally, but the type of<br />
defect and the specific aetiological factors<br />
are not yet clear 13 . It is also likely that, in<br />
addition to the environmental exposures<br />
so far identified, genetic susceptibility may<br />
10 clinical corner<br />
mi.gceurope.com
the disease itself, the associated fever, the treatment<br />
administered or a combination which is responsible 14.<br />
Tooth properties<br />
As <strong>with</strong> the clinical presentation of MIH, lesions<br />
studied in vitro are often highly variable, however<br />
some significant findings for enamel affected by MIH<br />
include: increased porosity; decreased hardness;<br />
decreased mineral content; increased carbonate<br />
content; increased protein content and abnormal<br />
ultrastructure, etching patterns and bonding<br />
properties. Discrete areas of >25% porosity have<br />
been observed, though the bulk of lesions are less<br />
than 10%. Both microhardness and nanohardness<br />
is significantly reduced (up to a 70% reduction) as<br />
is mineral content (> 45% decrease) compared to<br />
normal enamel 15-17 . For both hardness and mineral<br />
content the gradient is abnormal <strong>with</strong> harder and<br />
more mineralised enamel found toward the dentinoenamel<br />
junction 16,17. For each of these properties the<br />
most severe areas are almost always in the outer half<br />
of enamel and a surface layer of reduced porosity and<br />
increased hardness and mineral content is observed,<br />
even in areas <strong>with</strong> PEB, while cervical regions appear<br />
unaffected. Higher carbon levels have been reported<br />
using secondary ion mass spectrometry which can<br />
reflect either a higher proportion of carbonated<br />
apatite or increased organic component 18 : in fact<br />
it appears to be a combination, <strong>with</strong> MIH lesions<br />
containing 3-15 times the protein (primarily<br />
exogenous) and 1.6 times the carbonate content of<br />
normal enamel 14,19.<br />
The ultrastructure of the enamel, observed under<br />
scanning electron microscopy (SEM) is also affected<br />
<strong>with</strong> increased disorganisation, abnormal prism<br />
core and inter-prismatic appearance and abnormal<br />
etching patterns reported 20,21 . The enamel-adhesive<br />
interface is markedly different and associated <strong>with</strong><br />
reduced bond strengths to resin composite, however<br />
in the majority of cases failure was cohesive <strong>with</strong>in<br />
the enamel 22 . Bacterial invasion of dentine tubules,<br />
and associated inflammatory change (secondary<br />
“Children <strong>with</strong> teeth affected by<br />
MIH undergo up to ten times the<br />
treatment of unaffected children<br />
by the age of 8 years and have<br />
significantly higher levels of dental<br />
anxiety and phobia”<br />
dentine formation), under apparently intact<br />
hypomineralised enamel has also been demonstrated<br />
using SEM techniques 23. Other investigations of<br />
the pulp status of MIH affected teeth have reported<br />
increased expression of an inflammatory mediator<br />
implicated in pain development, an increase in<br />
immune cells and increased innervation and<br />
vascularisation, providing a reason for the increased<br />
sensitivity and refractory nature <strong>with</strong> anaesthesia of<br />
these teeth 24,25.<br />
Management<br />
Unfortunately it is, as yet, impossible to use evidence<br />
based dentistry in the treatment of MIH as, while<br />
recommendations are supported theoretically by<br />
research evidence, only very limited clinical data<br />
is available. Generally it is advised clinicians utilize<br />
the apparently sound cervical enamel for bonding<br />
of ‘permanent’ restorations as marginal breakdown<br />
is otherwise commonly observed, however this<br />
strategy does involve the sacrifice of a great amount<br />
of enamel 26-28. Glass ionomer cements are often<br />
recommended, especially for early protection of<br />
the enamel, but currently there is no evidence<br />
beyond anecdotal for using this material either in<br />
vitro or in vivo 26, 27 . Despite this a recent <strong>Europe</strong>an<br />
Academy of Paediatric Dentistry policy document<br />
for MIH management included GIC restorations in its<br />
recommendations 29 .<br />
Also suggested was the use of preformed crowns<br />
which have been found to perform well and do not<br />
1: Hypomineralised tooth demonstrating both severe (post-eruptive breakdown on distal cusps) and mild (white<br />
demarcated opacity on mesio-buccal cusp tip) lesions. 2: Polished hypomineralised lesion demonstrating demarcated<br />
defect edge. 3: Polarised light image (water imbibition) demonstrating surface layer of improved physical properties in<br />
area of post-eruptive breakdown (blue layer). 4: Clinical images of hypomineralised teeth demonstrating demarcated<br />
opacities, post-eruptive breakdown and cavitation even before complete eruption.<br />
treatment plan<br />
11
vitro or in vivo 26, 27. Despite this a recent <strong>Europe</strong>an<br />
Academy of Paediatric Dentistry policy document<br />
for MIH management included GIC restorations in its<br />
recommendations 29 .<br />
Also suggested was the use of preformed crowns<br />
which have been found to perform well and do not<br />
need extensive tooth preparation thus conserving<br />
maximum tooth structure, and therefore options, for<br />
future treatments as these restorations cannot really<br />
be considered a permanent solution 29,30. Given the<br />
eventual outcome the restoration cycle, the rapidity<br />
<strong>with</strong> which MIH teeth can pass through this cycle<br />
and the costs associated <strong>with</strong> treatment (potentially<br />
endodontic treatment, fixed prosthodontics and<br />
eventual replacement <strong>with</strong> an implant at a relatively<br />
young age as other options are exhausted) it<br />
is recommended that extraction, ideally <strong>with</strong><br />
consultation and co-ordination <strong>with</strong> orthodontic<br />
advice, be considered for severely affected teeth.<br />
Acceptable outcomes, even <strong>with</strong>out (but preferably<br />
<strong>with</strong>) orthodontic intervention, can be achieved<br />
and cases should be assessed as to whether this<br />
option is more appropriate if extensive treatment<br />
seems otherwise inevitable 6,7,29 . It is commonly<br />
requested that extractions be delayed until the most<br />
orthodontically favourable time in which case interim<br />
restorations or preventive strategies may be needed<br />
in the interim. Preventive advice is based on the early<br />
caries/remineralisation model utilizing <strong>CPP</strong>-<strong>ACP</strong>,<br />
fluoride products and fissure sealants, however again<br />
the efficacy of such treatments is anecdotal only 29.<br />
References<br />
1. Weerheijm, K.L., B. Jalevik, and S. Alaluusua, Molar-incisor<br />
hypomineralisation. Caries Research, 2001. 35(5): p. 390-1.<br />
2. Weerheijm, K.L., et al., Prevalence of cheese molars in<br />
eleven-year-old Dutch children. Journal of Dentistry for<br />
Children, 2001. 68(4): p. 259-62.<br />
3. Crombie, F.A., et al., Molar incisor hypomineralization: a survey<br />
of members of the Australian and New Zealand Society<br />
of Paediatric Dentistry. Aust Dent J, 2008. 53(2): p. 160-6.<br />
4. Leppaniemi, A., P.L. Lukinmaa, and S. Alaluusua, Nonfluoride<br />
hypomineralizations in the permanent first molars<br />
and their impact on the treatment need. Caries Research,<br />
2001. 35(1): p. 36-40.<br />
5. Jalevik, B. and G.A. Klingberg, Dental treatment, dental fear<br />
and behaviour management problems in children <strong>with</strong><br />
severe enamel hypomineralization of their permanent first<br />
molars. International Journal of Paediatric Dentistry, 2002.<br />
12(1): p. 24-32.<br />
6. Williams, J.K. and A.J. Gowans, Hypomineralised first<br />
permanent molars and the orthodontist. <strong>Europe</strong>an Journal<br />
of Paediatric Dentistry, 2003. 4(3): p. 129-32.<br />
7. Mejare, I., E. Bergman, and M. Grindefjord, Hypomineralized<br />
molars and incisors of unknown origin: treatment outcome<br />
at age 18 years. International Journal of Paediatric<br />
Dentistry, 2005. 15(1): p. 20-8.<br />
8. Crabb, J.J. and W.P. Rock, Treatment planning in relation<br />
to the first permanent molar. British Dental Journal, 1971.<br />
131(9): p. 396-401.<br />
9. Jalevik, B., et al., The prevalence of demarcated opacities<br />
in permanent first molars in a group of Swedish children.<br />
Acta Odontologica Scandinavica, 2001. 59(5): p. 255-60.<br />
10. Jasulaityte, L., J.S. Veerkamp, and K.L. Weerheijm, Molar<br />
incisor hypomineralization: review and prevalence data<br />
from the study of primary school children in Kaunas/Lithuania.<br />
<strong>Europe</strong>an Archives of Paediatric Dentistry: Official<br />
Journal of the <strong>Europe</strong>an Academy of Paediatric Dentistry,<br />
2007. 8(2): p. 87-94.<br />
11. Jalevik, B., Prevalence and Diagnosis of Molar-Incisor-<br />
Hypomineralisation (MIH): A systematic review. Eur Arch<br />
Paediatr Dent. 11(2): p. 59-64.<br />
12. Weerheijm, K.L. and I. Mejare, Molar incisor hypomineralization:<br />
a questionnaire inventory of its occurrence in<br />
member countries of the <strong>Europe</strong>an Academy of Paediatric<br />
Dentistry (EAPD). International Journal of Paediatric Dentistry,<br />
2003. 13(6): p. 411-6.<br />
13. Crombie, F., D. Manton, and N. Kilpatrick, Aetiology of<br />
molar-incisor hypomineralization: a critical review. Int J<br />
Paediatr Dent, 2009. 19(2): p. 73-83.<br />
14. 57th Annual ORCA Congress July 7-10, 2010, Montpellier,<br />
France Abstracts. Caries Research. 44(3): p. 172-244.<br />
15. Mahoney, E., et al., Mechanical properties across hypomineralized/hypoplastic<br />
enamel of first permanent molar teeth.<br />
<strong>Europe</strong>an Journal of Oral Sciences, 2004. 112(6): p. 497-502.<br />
16. Fearne, J., P. Anderson, and G.R. Davis, 3D X-ray microscopic<br />
study of the extent of variations in enamel density in first<br />
permanent molars <strong>with</strong> idiopathic enamel hypomineralisation.<br />
British Dental Journal, 2004. 196(10): p. 634-8;<br />
discussion 625.<br />
17. Anonymous, 56th Congress of the <strong>Europe</strong>an-Organisation-for-Caries-Research<br />
(ORCA), Budapest, HUNGARY, July<br />
01 -04, 2009. Caries Research, 2009. 43(3): p. 179-241.<br />
18. Jalevik, B., et al., Secondary ion mass spectrometry and<br />
X-ray microanalysis of hypomineralized enamel in human<br />
permanent first molars. Archives of Oral Biology, 2001.<br />
46(3): p. 239-47.<br />
19. Mangum, J.E., et al., Surface integrity governs the<br />
proteome of hypomineralised enamel. Journal of Dental<br />
Research, Accepted for publication, April 2010.<br />
20. Mahoney, E.K., et al., Mechanical properties and microstructure<br />
of hypomineralised enamel of permanent teeth.<br />
Biomaterials, 2004. 25(20): p. 5091-100.<br />
21. Jalevik, B., W. Dietz, and J.G. Noren, Scanning electron<br />
micrograph analysis of hypomineralized enamel in<br />
Affected anterior teeth tend to present aesthetic<br />
problems only, rather than the breakdown, sensitivity<br />
and increased caries risk found when molars are<br />
involved. Management is therefore usually more<br />
straightforward and options include: microabrasion,<br />
bleaching and sealant and direct or eventually<br />
indirect restorations to improve the appearance 29.<br />
In conclusion, the apparent increasing prevalence<br />
of MIH creates the need for greater practitioner<br />
knowledge regarding the diagnosis of the condition<br />
and also the treatment options possible.<br />
About the authors<br />
Dr Felicity Crombie completed<br />
her BDSc <strong>with</strong> Honours at the<br />
University of Melbourne and works<br />
in private practice as well as teaching<br />
undergraduates. In 2007 Dr Crombie<br />
started her PhD studies investigating<br />
the properties of molars affected<br />
by enamel hypomineralisation and<br />
subsequently has published and presented on the<br />
topic of molar hypomineralisation<br />
locally and internationally.<br />
David John Manton [BDSc MDSc<br />
PhD FRACDS FICD] is the convener<br />
of Paediatric Dentistry at the<br />
Cooperative Centre for Oral Health<br />
Science, Melbourne Dental School,<br />
University of Melbourne.<br />
permanent first molars. International Journal of Paediatric<br />
Dentistry, 2005. 15(4): p. 233-240.<br />
22. William, V., et al., Microshear bond strength of resin<br />
composite to teeth affected by molar hypomineralization<br />
using 2 adhesive systems. Pediatric Dentistry, 2006. 28(3):<br />
p. 233-41.<br />
23. Fagrell, T.G., et al., Bacterial invasion of dentinal tubules<br />
beneath apparently intact but hypomineralized enamel<br />
in molar teeth <strong>with</strong> molar incisor hypomineralization.<br />
International Journal of Paediatric Dentistry, 2008. 18(5): p.<br />
333-340.<br />
24. Rodd, H.D., et al., Pulpal status of hypomineralized permanent<br />
molars. Pediatric Dentistry, 2007. 29(6): p. 514-20.<br />
25. Rodd, H.D., et al., Pulpal expression of TRPV1 in molar incisor<br />
hypomineralisation. <strong>Europe</strong>an Archives of Paediatric<br />
Dentistry: Official Journal of the <strong>Europe</strong>an Academy of<br />
Paediatric Dentistry, 2007. 8(4): p. 184-8.<br />
26. William, V., L.B. Messer, and M.F. Burrow, Molar incisor hypomineralization:<br />
review and recommendations for clinical<br />
management. Pediatric Dentistry, 2006. 28(3): p. 224-32.<br />
27. Mathu-Muju, K. and J.T. Wright, Diagnosis and treatment<br />
of molar incisor hypomineralization. Compendium of<br />
Continuing Education in Dentistry, 2006. 27(11): p. 604-10;<br />
quiz 611.<br />
28. Lygidakis, N.A., A. Chaliasou, and G. Siounas, Evaluation<br />
of composite restorations in hypomineralised permanent<br />
molars: a four year clinical study. <strong>Europe</strong>an Journal of<br />
Paediatric Dentistry, 2003. 4(3): p. 143-8.<br />
29. Lygidakis, N.A., et al., Best Clinical Practice Guidance for<br />
clinicians dealing <strong>with</strong> children presenting <strong>with</strong> Molar-<br />
Incisor-Hypomineralisation (MIH) An EAPD Policy Document.<br />
Eur Arch Paediatr Dent, 2010. 11(2): p. 75-82.<br />
30. Zagdwon, A.M., S.A. Fayle, and M.A. Pollard, A prospective<br />
clinical trial comparing preformed metal crowns and cast<br />
restorations for defective first permanent molars. <strong>Europe</strong>an<br />
Journal of Paediatric Dentistry, 2003. 4(3): p. 138-42.<br />
12 clinical corner<br />
mi.gceurope.com
White spot reversal protocol<br />
The following protocols were developed by clinicians in their own<br />
dental practices in the USA, and published by <strong>GC</strong> America.<br />
Steps to white spot reversal<br />
• Take photos of the white spot lesion prior to the<br />
start.<br />
• It is important during microabrasion for the<br />
clinician not to over abrade the tooth surface,<br />
careful attention needs to be paid to the etching<br />
materials, their concentrations and application<br />
time.<br />
• Apply 37% phosphoric acid gel to white spot<br />
lesions, (10/15 sec. To 2 min. – suggested to be<br />
conservative), Rinse.<br />
• Gently pumice for 10 - 20 sec., (<strong>with</strong> non<br />
fluoridated, non glycerine pumice - suggest flour of<br />
pumice), Rinse.<br />
• Review the effect sometimes may have to etch a<br />
second time.<br />
• Some dentists prefer to pumice first, then etch.<br />
• Apply thick layer of MI Paste to the etched teeth for<br />
5 minutes.<br />
• Instruct patient to use MI Paste 2X daily for 5<br />
minutes.<br />
• Custom tray is optional.<br />
• Have patient return for evaluation in 7 -10 days.<br />
• Repeat procedure if necessary.<br />
Successful cases<br />
Clinician: Dr Scott Munro - Racine, WI, USA<br />
Before<br />
After<br />
Treatment protocol followed:<br />
09/18/07 3 Minute Etch, 5 Minute MI Paste Treatment<br />
09/24/07 3 Minute Etch, 5 Minute MI Paste Treatment<br />
10/04/07 3 Minute Etch, 5 Minute MI Paste Treatment<br />
10/15/07 3 Minute Etch, 5 Minute MI Paste Treatment<br />
- Bleach 15% Opalescence<br />
10/18/07 3 Minute Etch, 5 Minute MI Paste Treatment-<br />
Bleach 15% Opalescence<br />
11/01/07 3 Minute Etch, 5 Minute MI Paste Treatment<br />
11/29/07 3 Minute Etch, 5 Minute MI Paste Treatment<br />
Notes<br />
• No restorative work was done on patient<br />
• MI Paste was used and some light microabrasion<br />
was done on cusp tips. #9 wasn’t bleached<br />
internally, but was whitened <strong>with</strong> ZOOM in office.<br />
Patient wore trays for 5 minutes, twice daily.<br />
clinical corner<br />
13
Clinician: Dr Stephanie Benton - Grand Rapids, MI, USA<br />
Before<br />
Treatment protocol followed:<br />
• Teeth were etched twice, for 20 second intervals.<br />
• No pumice was used.<br />
• MI Paste was placed immediately on teeth following etching and wore trays at night time only.<br />
• Immediate results were seen over the first weekend.<br />
• Patient continued to wear the trays for 2-3 weeks at night time.<br />
Clinician: Dr Brett Kessler - Denver, CO, USA<br />
Before<br />
Before close-up<br />
Treatment protocol followed:<br />
• Etched # 8 & 9 for 3 minutes<br />
• Gave MI Paste <strong>with</strong> trays to 15 minutes before bed,<br />
after 3 days<br />
• Patient used MI Paste for the spots were gone.<br />
14<br />
clinical corner<br />
After<br />
After<br />
After close-up<br />
• The after photos are 2 weeks after the one time<br />
etching and daily use.<br />
• The patient used approximately 1/2 of the tube of<br />
MI Paste to achieve these results.<br />
mi.gceurope.com
Clinician: Dr Ivan A. Serdar - San Francisco, CA, USA<br />
Before<br />
After<br />
Treatment protocol followed:<br />
12/02/08 - Pumice, rinse, 1 minute etch <strong>with</strong> 37%<br />
Phosphoric acid, rinse, blot, 5 minutes MI Paste.<br />
01/07/09 - Pumice, rinse, 1 minute etch <strong>with</strong> 37%<br />
Phosphoric acid, rinse, blot, 5 minutes MI Paste.<br />
01/26/09 - Pumice, rinse, minute etch <strong>with</strong><br />
Phosphoric acid, rinse, blot, minutes Paste.<br />
02/25/09 - Pumice, rinse, 1 minute etch <strong>with</strong> 37%<br />
Phosphoric acid, rinse, blot, 5 minutes MI Paste.<br />
04/01/09 - Pumice, rinse, 1 minute etch <strong>with</strong> 37%<br />
Phosphoric acid, rinse, blot, 5 minutes MI Paste.<br />
04/29/09 - Pumice, rinse, 1 minute etch <strong>with</strong> 37%<br />
Phosphoric acid, rinse, blot, 5 minutes MI Paste.<br />
Notes<br />
Patient used trays at home for the duration of this<br />
treatment and placed MI Paste in her trays for 5<br />
minutes, twice a day. Patient also used regular<br />
strength Whitestrips at home for three weeks.<br />
Clinician: Dr Rubin and Dr Pong - Cincinnati, OH, USA<br />
Before<br />
After<br />
Treatment protocol followed:<br />
• 2 Minute etch <strong>with</strong> 37% phosphoric acid (blue gel)<br />
• Heavy pumice<br />
• Dispense tube of MI Paste or MI Paste Plus. Patient<br />
apply/rub<br />
• MI Paste <strong>with</strong> finger to affected areas for 10<br />
seconds, daily at bedtime. Re-evaluate in 2 weeks<br />
• Repeat sequence as needed for desired result.<br />
• Treatment was over the course of 1 month<br />
9/3/2008-9/29/2008.<br />
clinical corner<br />
15
Topical <strong>CPP</strong>-<strong>ACP</strong> crème (Tooth Mousse):<br />
more evidence that demands a verdict<br />
By Laurence J Walsh<br />
Casein Phosphopeptide-Amorphous Calcium<br />
Phosphate (<strong>CPP</strong>-<strong>ACP</strong>) is a unique naturally derived<br />
protein-based remineralizing technology which is now<br />
used globally in chewing gums and topical crèmes.<br />
The unique phosphopeptides are derived from milk<br />
caseins, and are complexed <strong>with</strong> amorphous calcium<br />
phosphate, to form stable complexes which are<br />
nanoparticles of some 2 nm in diameter <strong>with</strong> a large<br />
surface area for mineral exchange Cross et al. 2006).<br />
The configuration of the <strong>ACP</strong> in the <strong>CPP</strong>-<strong>ACP</strong> complex<br />
differs completely from that found in macromolecular<br />
aggregates of <strong>ACP</strong>, as has been included in some<br />
current prophylaxis pastes and bleaching gels.<br />
<strong>CPP</strong>-<strong>ACP</strong> nanocomplexes act as biological<br />
calcium phosphate delivery vehicles, and are<br />
able to boost levels of bio-available calcium and<br />
phosphate in saliva and plaque fluid <strong>with</strong>out causing<br />
indiscriminate precipitation of calcium salts. This<br />
makes this material particularly effective in the<br />
remineralization of early enamel lesions, and in the<br />
treatment of other types of enamel opacities. The<br />
efficacy of these nanocomplexes as anti-cariogenic<br />
agents has been demonstrated in numerous animal<br />
and in situ human caries studies (Reynolds 1997,<br />
1998, 2008, 2009; Cross et al. 2007), as well as in<br />
clinical trials. Over the past decade, the use of<br />
products containing <strong>CPP</strong>-<strong>ACP</strong> nanocomplexes has<br />
become a well established part of clinical practice<br />
across the globe. The clinical use of this technology<br />
is supported by a large body of refereed papers and<br />
conference presentations as well as by systematic<br />
reviews, the highest form of evidence in the<br />
pyramid of evidence-base practice. For example, a<br />
2006 systematic review focused on chewing gums<br />
and lozenges enriched <strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong> (Yengopal &<br />
Mickenautsch, 2006 & 2009), identified over 120<br />
journal articles on <strong>CPP</strong>-<strong>ACP</strong> technology, which<br />
included laboratory trials and animal studies as well<br />
as clinical trials and numerous in situ clinical studies.<br />
In Australia and in many other parts of the world,<br />
the most commonly used <strong>CPP</strong>-<strong>ACP</strong> product is the<br />
topical crème which contains 10% <strong>CPP</strong>-<strong>ACP</strong>. This<br />
product, which is known alternatively as Tooth<br />
Mousse or MI Paste, is intended for both in-office<br />
and at-home use. The purpose of this article is<br />
to summarize the global research effort which<br />
underpins the current clinical applications of Tooth<br />
Mousse (TM) and its related fluoride-containing<br />
counterpart, Tooth Mousse Plus (TMP). The article<br />
draws on the refereed literature, including both<br />
journal papers and presentations at international and<br />
regional meetings of the International Association for<br />
Dental Research (IADR), the peak international body<br />
for dental research, over the period from January<br />
2002 to August 2010.<br />
Bio-availability of calcium and phosphate ions<br />
In most preventive protocols, TM is applied daily in a<br />
pea-size amount using a finger to the labial surfaces<br />
of the teeth immediately before bed. By dissolving<br />
slowly, the material contributes bio-available calcium<br />
and phosphates to the saliva, and is able to promote<br />
remineralization at a time when salivary defenses are<br />
at their lowest point. TM can be used in patients of all<br />
ages as the material is classified as safe to ingest.<br />
The release of ions from TM has been examined in<br />
considerable detail. The release of ions at neutral pH<br />
was reported by Paterson et al. (2008) who dissolved<br />
TM directly into deionized water and then used a<br />
calcium ion-selective electrode to measure calcium<br />
ion release. The free calcium ion concentration in<br />
the solution increased <strong>with</strong> time in a saturating<br />
exponential manner, <strong>with</strong> approximately 95 % release<br />
after only 15 minutes. This rapid release means that<br />
when the crème is applied to tooth surfaces there<br />
will be a rapid increase in calcium ion concentration<br />
in the plaque fluid and saliva. Their supersaturation<br />
for calcium <strong>with</strong> respect to tooth enamel drives<br />
remineralization and prevents mineral loss.<br />
Comparative studies <strong>with</strong> a broad range<br />
of toothpastes, gels, liquids claimed to have<br />
remineralizing or desensitizing actions (including<br />
NovaMin ®, ClinPro ® Tooth Creme, Clin Pro 5000,<br />
and ReminPro ®) reveal that calcium contained in<br />
these products has low water solubility and poor<br />
bio-availability, unlike the situation for TM and TMP.<br />
The level of water soluble calcium per gram of crème<br />
in TM or TMP (321.8 ± 2.6 µmol/g) is some 14 times<br />
or greater than any of these other products (Cai et<br />
al. 2009; Yasuda et al. 2010). Tooth Mousse Plus also<br />
has been shown to contain the highest amount of<br />
water soluble phosphate (245.7 ± 2.7 µmol/g) of any<br />
currently available products. The rapid release of<br />
calcium ions (<strong>with</strong>in 1 hour) has been confirmed in<br />
other studies of TM, including those conducted by<br />
commercial competitors (Burwell et al. 2009).<br />
The high water solubility and bioavailability of the<br />
calcium, phosphate and fluoride in TM and TMP is<br />
due to this being a protein technology (containing<br />
casein phosphopeptides), whereas all other marketed<br />
16 Clinical corner<br />
www.gceurope.com
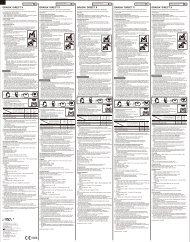
Table 1. Prevention and treatment of enamel caries using Tooth Mousse in laboratory models<br />
Author Year Location Design Outcomes<br />
products are inorganic in nature and lack the ability<br />
to stabilize the calcium and phosphate ions.<br />
Prevention of mineral loss in caries models<br />
Topical application of TM immediately before a<br />
cariogenic challenge has been shown to prevent<br />
Enamel caries<br />
Sato 2003 Tokyo Enamel slabs <strong>with</strong> demin gel TM buffered acids produced<br />
(microhardness) by S. mutans<br />
TM reduced enamel demin from<br />
acidic gel and S. mutans fermentation.<br />
Takamizawa 2005 Tokyo Enamel slabs <strong>with</strong> demin gel TM preserved the inorganic component<br />
(ultrasound) of enamel by preventing demin.<br />
Sakaguchi 2005 Tokyo Enamel slabs <strong>with</strong> demin gel TM preserved the inorganic component<br />
(QLF) of enamel by preventing demin.<br />
Sudjalimi 2006 Melbourne Extracted teeth in demin gel TM reduced mineral loss around<br />
(QLF) orthodontic brackets.<br />
Manton 2007 Melbourne Enamel slabs <strong>with</strong> white TM caused more remin of white spot<br />
spot lesions lesions than human saliva.<br />
Lovel 2007 Liverpool Enamel slabs <strong>with</strong> white TM was more effective than 1000 ppm<br />
spot lesions (QLF) F toothpaste in promoting remin of WSL<br />
Kim 2007 South Korea Enamel slabs <strong>with</strong> WSL TM was more effective than 3000 ppm<br />
(microhardness) F solution in preventing demin.<br />
Kumar 2008 Hong Kong Enamel slabs <strong>with</strong> WSL TM remineralized WSL and showed a<br />
higher remineralizing potential when<br />
applied after the use of a fluoride<br />
toothpaste.<br />
Adebayo 2008 Melbourne Enamel slabs TM treatment of intact enamel<br />
improves resistance to phosphoric<br />
acid etching<br />
Kao 2008 West Virginia Enamel slabs TM treatment increases acid resistance<br />
of enamel when exposed to a demin gel.<br />
Setien 2008 Dallas Enamel slabs <strong>with</strong> WSL TM treatment increased the<br />
(microhardness) microhardness of demineralized enamel.<br />
Theerapiboon 2008 Bangkok Enamel slabs <strong>with</strong> WSL (PLM) TM treatment reduced lesion volume<br />
and caused remin in WSL in both<br />
permanent and deciduous enamel.<br />
Huang 2008 Minneapolis Enamel slabs eroded TM treatment improved enamel<br />
<strong>with</strong> Coke® hardness more than artificial saliva.<br />
Kallayahi 2008 Bangkok Enamel slabs TM treatment protected enamel from<br />
(microhardness) softening from cola drink exposure.<br />
Behnan 2009 Ann Arbor Enamel slabs TM prevented enamel demineralization<br />
(QLF) around orthodontic brackets during<br />
an in-vitro acid challenge.<br />
Elsayad 2009 Cairo Molar teeth <strong>with</strong> demin TM caused remin, which was enhanced<br />
when F was added simultaneously.<br />
Chapman 2010 Bristol Enamel slabs (profilometry) TMP and TMP reduced enamel surface<br />
loss from citric acid challenge.<br />
F = fluoride, QLF = Quantitative light fluorescence; PLM = polarizing light microscopy, WSL = white spot lesions.<br />
demineralization of enamel during subsequent<br />
challenge, and also to reduce the pH reduction<br />
caused by S. mutans fermentation (Sato et al. 2003).<br />
This capacity to buffer acids produced by cariogenic<br />
bacteria adds to other ecological effects of TM on<br />
dental plaque. TM has benefits in preventing root<br />
clinical corner<br />
17
surface caries as well as enamel caries (Tables 1-3).<br />
Numerous laboratory studies have documented that<br />
TM is more effective than saliva for remineralization<br />
after caries- and erosion-like assaults to the enamel<br />
(Table 1). This holds true regardless of the methods<br />
which are used to assess the integrity of the<br />
enamel. Preventive benefits of TM and TMP are now<br />
recognized to extend to root surfaces as well as<br />
enamel (Table 2), and evidence of arrest and reversal<br />
of root surface caries has also been presented (Vlacic<br />
et al. 2007).<br />
As well as effects mediated through promoting<br />
remineralization and inhibiting demineralization, it is<br />
now recognized that TM can exert ecological effects<br />
on the dental plaque biofilm. A recent large scale<br />
clinical trial reported that daily use of TM in infants<br />
from the time of first tooth eruption had similar<br />
effects on plaque acid production as daily use of<br />
0.12% chlorhexidine gel (Plonka et al. 2010).<br />
Visible reversal of white spot carious lesions<br />
Early case reports of visible reversal of enamel white<br />
spot lesions (WSL) in young adult patients in Australia<br />
Table 2. Other Laboratory Studies of Tooth Mousse<br />
(Walsh 2004; Walsh 2007) and later in Japan (from 2002)<br />
(Reynolds & Walsh, 2005), <strong>Europe</strong> (Ardu et al. 2007) and<br />
North America (Milnar, 2007) have been followed by in<br />
situ studies of laboratory-created WSL (Manton et al.<br />
2007) and full scale randomized controlled clinical trials<br />
in patients <strong>with</strong> naturally occurring WSL (Andersson<br />
et al. 2006; Kitasako et al. 2009; Bailey et al. 2009; Zhou<br />
et al. 2009; Yazicioglu et al. 2010). Cases of reversal of<br />
moderate fluorosis have also been presented (Walsh<br />
2003; Walsh 2004; Reynolds & Walsh 2005; Walsh 2007;<br />
Ng & Manton 2007).<br />
Recent reviews have concluded that predictable<br />
remineralization of enamel white spot lesions<br />
(WSL) can be achieved clinically by using frequent<br />
applications of TM as a self-administered topical<br />
therapy (Ilena et al. 2009; Reynolds 2009). This<br />
significant body of work (summarized in Table 3)<br />
demonstrates that dramatic cosmetic changes occur<br />
in enamel as WSL undergo reversal during treatment<br />
<strong>with</strong> TM on a daily basis. A particular risk group where<br />
TM is useful for gaining regression of white spot<br />
lesions is patients who are undergoing orthodontic<br />
treatment (Table 4).<br />
Author Year Location Design Outcomes<br />
Root caries<br />
Hicks 2005 Houston Root segments <strong>with</strong> demin gel TM enhanced the resistance of root<br />
(PLM) surfaces to artificial caries formation,<br />
when compared <strong>with</strong> fluoride rinse<br />
(0.05% NaF).<br />
Rahiotis 2007 Athens Dentine slabs <strong>with</strong> demin gel TM treatment reduced demin and<br />
enhanced remin of dentine.<br />
Xie 2007 Chicago Root segments <strong>with</strong> demin gel TM treatment increased the hardness<br />
(microhardness) of dentine.<br />
Trajtenberg 2007 Houston Root segments <strong>with</strong> demin gel TM treatment improved caries<br />
(PLM) resistance of root surfaces.<br />
Garcia-Godoyi 2009 Fort Lauderdale Root segments <strong>with</strong> demin gel TM and TMP protected root surfaces<br />
(PLM) from an artificial caries challenge.<br />
Other applications<br />
Wong 2010 Melbourne Teeth undergoing bleaching A 2 week application of TM prior to<br />
the use of an in-office bleaching gel did<br />
not adversely affect the bleaching<br />
effectiveness, but reduced the levels of<br />
hydrogen peroxide entering the pulp<br />
chamber.<br />
Augustson 2010 Minneapolis Enamel eroded <strong>with</strong> HCl After HCL erosion, 60 minutes exposure<br />
(microhardness) to TMP or TM (but not 3000 ppm F rinse)<br />
increased the enamel hardness. Greater<br />
recovery seen <strong>with</strong> TMP than <strong>with</strong> TM.<br />
Gomes 2010 San Paulo De-proteinated enamel TM applied after in-office bleaching<br />
helped to restore the glossy nature of<br />
the enamel surface.<br />
18 Clinical corner<br />
www.gceurope.com
Table 3. Selected clinical studies of <strong>CPP</strong>-<strong>ACP</strong> products<br />
Author Year Location Design Outcomes<br />
While it is now well established that TM can cause<br />
reversal of WSL, it is remarkable that there are as<br />
yet no clinical trials or case reports in the literature<br />
showing visual reversal of enamel WSL for other<br />
agents such as NovaMin or ClinPro Tooth Crème<br />
which claim to have remineralizing actions.<br />
TMP is a potent agent for promoting regression and<br />
reversal of WSL. Mixtures of <strong>CPP</strong>-<strong>ACP</strong> <strong>with</strong> fluoride<br />
(TMP) and <strong>CPP</strong>-ACFP solutions have been shown<br />
to remineralize enamel subsurface lesions in vitro<br />
by depositing fluorapatite. This remineralization is<br />
accompanied by improved translucency and reduced<br />
opacity of the white spot lesions, as reversal occurs<br />
and mineral content increases (Cochrane et al. 2006).<br />
Chewing Gums<br />
Cai 2003 Melbourne RCT, in situ model, N=10, Incorporation of <strong>CPP</strong>-<strong>ACP</strong> into a lozenge<br />
over 14 days increased enamel subsurface lesion<br />
remineralization relative to a control<br />
sugar-free lozenge.<br />
Manton 2005 Melbourne RCT, in situ model, N=10, <strong>CPP</strong>-<strong>ACP</strong> gum produced 75-107% more<br />
over 14 days remineralization than sugar-free gums.<br />
Cai 2006 Melbourne RCT, in situ model, N=10, <strong>CPP</strong>-<strong>ACP</strong> gum produced more<br />
over 14 days remineralization than chewing <strong>with</strong><br />
placebo gum. Extended acid challenge<br />
of the remineralized lesions showed that<br />
the mineral formed was more acid<br />
resistant.<br />
Iijima 2006 Nagasaki RCT, in situ model, N=20, <strong>CPP</strong>-<strong>ACP</strong> gum produced remin of<br />
over 14 days subsurface enamel <strong>with</strong> mineral of<br />
higher crystallinity and greater acid<br />
resistance than when remin occurs <strong>with</strong><br />
saliva.<br />
Morgan 2008B Melbourne RCT, N=2720 children, <strong>CPP</strong>-<strong>ACP</strong> sugar-free gum slowed<br />
over 2 years progression and enhanced regression of<br />
approximal caries relative to a control<br />
sugar-free gum.<br />
Toothpaste<br />
Reynolds 2006 Melbourne RCT, in situ model, N=10, Toothpaste <strong>with</strong> 2% <strong>CPP</strong>-<strong>ACP</strong> produced<br />
over 14 days remin similar to 2800 ppm F toothpaste.<br />
Rao 2009 Manipal RCT, N=150 children, Toothpaste <strong>with</strong> 2% <strong>CPP</strong> caused a<br />
over 2 years significant reduction in caries increment<br />
versus placebo, and was equally as<br />
effective as a toothpaste containing<br />
1190 ppm F.<br />
Mouthrinse<br />
Shen 2006 Melbourne RCT, in situ model, N=10, Mouthrinse containing 0.5% <strong>CPP</strong>-<strong>ACP</strong><br />
over 10 days at pH 5.5 produced greater remin of<br />
enamel subsurface lesions than the<br />
same rinse at pH of 7.0.<br />
RCT = randomized controlled clinical trial.<br />
Treatment of cervical dentinal hypersensitivity (CDH)<br />
There is a significant literature regarding the strong<br />
interactions which occur between TM and dentine<br />
(Adebayo et al. 2008 A&B, 2009, 2010). One of the first<br />
clinical trials using TM to treat CDH was undertaken<br />
in Belgium in 2004. The study involved 11 private<br />
practitioners, whose patients <strong>with</strong> CDH were instructed<br />
to apply TM for 21 days, immediately after the evening<br />
brushing, leaving the material for 3 minutes, and<br />
spreading it across the mouth, and then leaving it<br />
in place during sleep. The patient cohort reported a<br />
reduction in sensitivity, particularly to stimulation <strong>with</strong><br />
air as opposed to tactile stimuli. Daily diaries which<br />
recorded symptoms of CDH showed a progressive<br />
clinical corner<br />
19
eduction from the first day of treatment over the<br />
following 3 weeks. Half of the treated patients reported<br />
that the general reduction in CDH symptoms was<br />
sufficiently great that they wished to repeat the<br />
treatment if symptoms of sensitivity recurred (Poitevin<br />
et al. 2004). A later series of randomized controlled<br />
clinical trials conducted in Brisbane showed that TM<br />
reduced sensitivity to air, osmotic, thermal and tactile<br />
stimuli, <strong>with</strong> equal effectiveness to potassium nitrate<br />
toothpaste (Walsh et al. 2006; Vlacic 2007, Walsh 2010).<br />
This finding has been confirmed by more recent studies<br />
(Duan et al. 2009). This aligns <strong>with</strong> studies which show<br />
that a single application of TM can coat and partially<br />
occlude dentine tubules, and resist thermocycling<br />
(Hiller et al. 2008), but is insufficient to give permanent<br />
resolution of sensitivity symptoms (Table 5).<br />
Tooth Mousse Plus<br />
<strong>CPP</strong> is able to stabilize amorphous calcium fluoride<br />
phosphate (<strong>CPP</strong>-ACFP), which allows additive effects<br />
on remineralization compared <strong>with</strong> the fluoride or<br />
Table 4. Clinical trials showing reversal of WSL by Tooth Mousse<br />
<strong>CPP</strong>-<strong>ACP</strong> alone (Cochrane et al. 2006; Sakaguchi<br />
et al. 2006). Moreover, <strong>CPP</strong>-<strong>ACP</strong> promotes the<br />
incorporation of fluoride into plaque and sub-surface<br />
enamel, producing effects superior to those which<br />
can be achieved using fluoride alone (Reynolds<br />
et al. 2006) (Table 5). Early studies showed that<br />
addition of 900 ppm fluoride to TM increased the<br />
acid resistance of the product formed when enamel<br />
lesions were remineralized, compared <strong>with</strong> using<br />
TM alone (Kariya et al. 2004). This level of fluoride<br />
was designed to provide the correct ionic ratio of<br />
components for remineralization. The inclusion of<br />
fluoride in TM to create TMP has been shown to<br />
enhance the resistance of enamel surfaces to in vitro<br />
caries formation, compared <strong>with</strong> TM or fluoride alone<br />
(Hicks 2006). A range of studies support the greater<br />
potential of TMP as a treatment agent over and above<br />
TM (Table 6).<br />
Direct comparisons of TMP <strong>with</strong> TM show the<br />
superior remineralizing capabilities of Tooth Mousse<br />
Plus, however, because of its fluoride content (900<br />
Author Year Location Design Outcomes<br />
Reversal of white spot lesions<br />
Manton 2006 Melbourne RCT, in situ model, N=6, TM produced 551% more remin of<br />
over 10 days enamel WSL than the placebo crème.<br />
Sakaguchi 2006 Tokyo In situ study, N=5 subjects, TM gave greater remin than 950 ppm<br />
7 days fluoride toothpaste, and even greater<br />
remin occurred <strong>with</strong> TMP, indicating<br />
synergy of fluoride <strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong>.<br />
Vlacic 2007 Brisbane RCT, N=16, over 12 months TM in patients <strong>with</strong> salivary dysfunction<br />
arrested cervical lesions, and improved<br />
the stimulated salivary flow rate and pH<br />
over time.<br />
Andresson 2007 Halmstad Cohort study, N=26, TM caused a reduction in post-<br />
over 12 months orthodontic WSL over time, and was<br />
better than F mouthwash combined<br />
<strong>with</strong> F toothpaste.<br />
Morgan 2008A Melbourne RCT, N=45 subjects, 12 weeks TM produced more regression of WSL<br />
remaining after orthodontics than the<br />
placebo control at 12 weeks.<br />
Kitasako 2009 Tokyo Cohort study, N=7 subjects, TM produced remineralization of WSL<br />
6 months over 6 months, and increased the surface<br />
pH of the lesions (using a micro sensor).<br />
Zhou 2009 Changchun Cohort study, N=10 subjects, TMP reduced visible enamel<br />
2 months demineralization and improved the<br />
appearance of long-standing post-<br />
orthodontic WSL.<br />
Reynolds 2010 Melbourne RCT, in situ model, N=6, TM and TMP (but not ClinPro) increased<br />
over 10 days salivary calcium and phosphate levels,<br />
and caused remin of enamel WSL.<br />
Yazicioglu 2010 Istanbul Cohort study, N=26, TMP caused remineralization of WSL on<br />
over 28 days both smooth and occlusal surfaces.<br />
20 Clinical corner<br />
www.gceurope.com
ppm), TMP is not suitable for use in children aged<br />
less than 7 years, because of concerns regarding<br />
ingestion of fluoride.<br />
<strong>CPP</strong>-<strong>ACP</strong> inclusion in chewing gums<br />
The inclusion of <strong>CPP</strong>-<strong>ACP</strong> in chewing gums (such as<br />
Recaldent ) is a well established caries preventive<br />
measure (Table 3). Early studies of this approach used<br />
in situ studies (Cai et al. 2003) and then progressed<br />
to randomized, double blind cross-over designs to<br />
compare <strong>CPP</strong>-<strong>ACP</strong> containing gums <strong>with</strong> several<br />
commercial sugar-free gums. Subjects in these<br />
studies chewed the various gums for a 20 minute<br />
period 4 times per day for 14 days. By using paired<br />
Table 5. Selected clinical studies of Tooth Mousse<br />
enamel half slabs, precise determinations of mineral<br />
levels could be made. These studies showed that <strong>CPP</strong>-<br />
<strong>ACP</strong> gum produced 75-107% more remineralization<br />
than sugar-free gums (Manton 2005). It is well known<br />
that xylitol-based gums reduces the caries increment,<br />
but have little or no effect on approximal caries<br />
(Antonio et al. 2009). In contrast, gums containing<br />
<strong>CPP</strong>-<strong>ACP</strong> are highly effective at remineralizing<br />
WSL, and have been shown to arrest and reverse<br />
approximal lesions in a large scale clinical trial<br />
(Morgan et al. 2008 A & B).<br />
Recaldent gum is ideally suited to both child and<br />
adult patients where a lifestyle activity is linked to<br />
sub-clinical dehydration, and the patient suffers the<br />
Author Year Location Design Outcomes<br />
Cervical dentinal hypersenitivity<br />
Poitevin 2004 Leuvin Cohort study, N=61 subjects, TM reduced sensitivity air and tactile<br />
over 21 days stimuli.<br />
Kowalczyk 2006 Poland Cohort study, N=13 subjects, A single application of TM gave<br />
over 4 weeks immediate benefit on response to air<br />
stimulation. There was no further<br />
treatment so relapse occurred.<br />
Walsh 2006 Brisbane RCT, N=36 subjects, TM reduced sensitivity to air, osmotic,<br />
over 56 days, versus thermal and tactile stimuli, <strong>with</strong> equal<br />
potassium nitrate toothpaste effectiveness to potassium nitrate<br />
toothpaste.<br />
Vlacic 2007 Brisbane RCT, N=12, over 12 months TM caused a progressive reduction in<br />
sensitivity to air stimulation, and also<br />
improved stimulated salivary flow and pH.<br />
Duan 2009 Wuhan RCT, N=30 subjects, 14 days TM reduced sensitivity <strong>with</strong> equal<br />
effectiveness to potassium nitrate gel.<br />
Other applications<br />
Aytepe 2008 Istanbul Cohort study, N=15 children, TM elevated saliva buffering capacity<br />
56 days and plaque pH over 8 weeks in children<br />
<strong>with</strong> cerebral palsy.<br />
Caruana 2009 London RCT, N=15 subjects TM applied immediately before a sucrose<br />
challenge reduced plaque acid<br />
production.<br />
Rahiotis 2009 Athens Cohort study, N=6 subjects, A single application of TM forms a<br />
8 hours. surface coating which attaches to metal<br />
surfaces, making these smoother. These<br />
surface films retain calcium phosphates.<br />
Amornpipithkul 2009 Bangkok Cohort study, N=21 children, Daily application of TM increased plaque<br />
14 days calcium and inorganic phosphate levels<br />
in a time-dependent manner.<br />
Baroni 2010 Bologna Cohort study, n=30 children, TM improved the morphology and<br />
3 years microstructure of the enamel in teeth<br />
affected by molar incisor hypoplasia.<br />
Plonka 2010 Brisbane RCT, N=345 infants, 2 years TM suppressed the emergence of S.<br />
mutans in the oral microflora, and<br />
lowered dental plaque acid production.<br />
clinical corner<br />
21
problems from depressed salivary pH and flow under<br />
resting conditions. Because gum can be incorporated<br />
into a range of outdoor and exerting activities, the<br />
introduction of Recaldent gum should be considered<br />
for patients who undertake strenuous activity, for<br />
example, through outdoor exercise, outdoor work, or<br />
Table 6. Studies of <strong>CPP</strong>-<strong>ACP</strong> <strong>with</strong> fluoride (Tooth Mousse Plus)<br />
gym training sessions. The timing is important since<br />
the stimulation of salivary flow achieved by the gum<br />
will occur at a time when otherwise resting flow and<br />
pH would be depressed. Recaldent gum provides an<br />
excellent preventive effect, and is easily incorporated<br />
into a busy modern lifestyle.<br />
Author Year Location Design Outcomes<br />
Kariya 2004 Tokyo In vitro, enamel slabs <strong>with</strong> TMP reduced enamel mineral loss<br />
demin gel compared <strong>with</strong> TM. Acid resistance of<br />
remineralized lesions was greater for<br />
TMP compared <strong>with</strong> TM.<br />
Hicks 2006 Houston In vitro, enamel slabs <strong>with</strong> TMP enhanced the resistance of enamel<br />
demin gel surfaces to in vitro caries formation<br />
compared <strong>with</strong> TM or fluoride alone.<br />
Itthagarun 2006 Gold Coast In vitro, enamel slabs <strong>with</strong> TM remineralized initial enamel lesions,<br />
demin gel and gave more remineralization when<br />
applied as a topical coating after the use<br />
of fluoride toothpaste.<br />
Sudjalimi 2006 Melbourne In vitro, extracted teeth in TMP was better at reduced mineral loss<br />
demin gel (QLF) around orthodontic brackets than TM<br />
or fluoride alone.<br />
Reynolds 2006 Melbourne RCT, in situ model, N=10, Toothpaste containing 2% <strong>CPP</strong>-<strong>ACP</strong><br />
over 14 days plus 1100 ppm F was superior to paste<br />
<strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong> alone and to 2800 ppm F<br />
toothpaste. Remineralized lesions were<br />
relatively acid resistant.<br />
Reynolds 2006 Melbourne RCT, N=10, over 14 days Mouthrinses containing 2% <strong>CPP</strong>-<strong>ACP</strong><br />
plus 450 ppm F increased the<br />
incorporation of fluoride ions into plaque<br />
to achieve over double that obtained<br />
<strong>with</strong> 450 ppm F rinse alone.<br />
Sakaguchi 2006 Tokyo In situ study, N=5 subjects, TMP gave greater remin than either TM<br />
7 days or 950 ppm fluoride toothpaste.<br />
Kim 2007 Sth Korea In vitro, enamel slabs <strong>with</strong> TMP was more effective than TM alone<br />
WSL (microhardness) or 3000 ppm F solution in preventing<br />
demin.<br />
Turssi 2008 San Paulo In vitro, enamel slabs <strong>with</strong> Treatment of eroded enamel <strong>with</strong> TMP<br />
erosion lesions (microhardness) reduced progression of erosion<br />
compared <strong>with</strong> the untreated control.<br />
Cochrane 2008 Melbourne In vitro, enamel slabs <strong>with</strong> WSL <strong>CPP</strong>-<strong>ACP</strong> and <strong>CPP</strong>-ACFP solutions<br />
promoted high levels of remineralization<br />
throughout the body of enamel WSL.<br />
Hamba 2010 Tokyo In vitro, enamel slabs <strong>with</strong> TMP prevented demineralization more<br />
demin gel (micro CT) effectively than TM <strong>with</strong>out F, and F alone.<br />
Hicks 2010 Houston In vitro, enamel slabs <strong>with</strong> TMP reduced lesion depths as effectively<br />
demin gel (PLM) as a 5000 ppm F toothpaste despite<br />
having a fluoride content of only 900<br />
ppm F.<br />
Cochrane 2010 Melbourne In vitro, enamel slabs <strong>with</strong> TMP produced high percentages of<br />
WSL and orthodontic brackets remineralization of WSL, which reduced<br />
the extent of enamel damage caused by<br />
bracket removal subsequently.<br />
RCT = randomized controlled clinical trial.<br />
22 Clinical corner<br />
www.gceurope.com
Extending the range of clinical applications<br />
The addition of <strong>CPP</strong>-<strong>ACP</strong> to existing foods has<br />
been shown to enhance their dental health<br />
benefits. Addition of <strong>CPP</strong>-<strong>ACP</strong> to cheese and milk<br />
at concentrations from 0.2-0.5% has been shown<br />
in laboratory studies to reduce mineral loss in<br />
enamel cased by acid exposure, and to enhance<br />
remineralization (Minami et al. 2004; Walker et al.<br />
2009).<br />
Likewise, TM has been shown to increase the<br />
hardness of enamel which has been eroded by<br />
repeated contact <strong>with</strong> acidic drinks such as colas,<br />
improving mineral uptake beyond that possible<br />
<strong>with</strong> saliva alone (Sukasaem et al. 2006; Huang &<br />
Tantbironj 2008). Topical application of TM reduces<br />
the extent of softening and mineral loss caused by<br />
subsequent exposure to erosive beverages (Kallayathi<br />
et al. 2008).<br />
<strong>CPP</strong>-<strong>ACP</strong> has potential as an additive to acidic<br />
drinks to prevent dental erosion. A key factor in such<br />
an approach is to estimate the lowest concentration<br />
of <strong>CPP</strong>-<strong>ACP</strong> which can be added to erosive drinks to<br />
eliminate the risk of erosion to enamel. Past research<br />
work on this topic has explored this issue using<br />
Powerade, to which was added varying amounts<br />
of <strong>CPP</strong>-<strong>ACP</strong> from 0.063% up to 0.25%. Analysis of<br />
the surface characteristics of enamel slabs in the<br />
laboratory setting using stereomicroscopy, scanning<br />
electron microscopy and surface profilometry<br />
demonstrated that adding <strong>CPP</strong>-<strong>ACP</strong> at 0.25% raised<br />
the pH from 2.70 to 3.90, and lowered the titratable<br />
acidity from 1.83 to 1.36). Enamel loss from etching<br />
reduced from 3.87µm to 0.19µm, which was identical<br />
to enamel samples kept in distilled water (0.25µm).<br />
A reduction in the erosive step defect occurred at<br />
concentrations down to 0.09%. Overall, the erosive<br />
potential of Powerade was attenuated or eliminated<br />
completely by the addition of low concentrations of<br />
<strong>CPP</strong>-<strong>ACP</strong> (Ramalingham et al. 2002 & 2005).<br />
There is also interest in including <strong>CPP</strong>-<strong>ACP</strong> in dental<br />
materials, such as glass ionomer cements (Mazzaoui<br />
et al. 2003) and zinc oxide non-eugenol temporary<br />
References<br />
O. ADEBAYO, M. BURROW, and M. TYAS. SEM<br />
evaluation of casein phosphopeptide-amorphous<br />
calcium phosphate-treated and conditioned<br />
enamel. J Dent Res 87(Spec Iss C):1, 2008A.<br />
O.A. ADEBAYO, M.F. BURROW, and M.J.<br />
TYAS. Dentine bonding after <strong>CPP</strong>-<strong>ACP</strong> paste<br />
treatment <strong>with</strong> and <strong>with</strong>out conditioning. J Dent<br />
36(12):1013-1024, 2008B.<br />
O.A. ADEBAYO, M.F. BURROW, and M.J. TYAS.<br />
An SEM evaluation of conditioned and bonded<br />
enamel following carbamide peroxide bleaching<br />
and casein phosphopeptide-amorphous calcium<br />
phosphate (<strong>CPP</strong>-<strong>ACP</strong>) treatment. J Dent<br />
37(4):297-306, 2009.<br />
O.A. ADEBAYO, M.F. BURROW, and M.J. TYAS.<br />
Resin-dentine interfacial morphology following<br />
<strong>CPP</strong>-<strong>ACP</strong> treatment. J Dent 38(2):96-105, 2010.<br />
C. AMORNPIPITHKUL, S. SANGUANSIN, and<br />
P. LEELATAWEEWUD. The Effects of Casein-<br />
Phosphopeptide-Amorphous-Calcium-Phosphate<br />
Paste on Plaque Calcium and Phosphate. J Dent<br />
Res 88(Spec Iss C):190, 2009.<br />
A. ANDERSSON, S. TWETMAN, K. SKÖLD-<br />
LARSSON, and L.G. PETERSSON. Lesion<br />
regression <strong>with</strong> <strong>CPP</strong>/<strong>ACP</strong>-containing cream<br />
assessed by laser fluorescence. J Dent Res<br />
85(Spec Iss B):2539, 2006.<br />
A. ANDERSSON, K. SKÖLD-LARSSON,<br />
cements used in crown and bridgework. Both lines<br />
of investigation have been followed, <strong>with</strong> the logic<br />
being to provide greater resistance to mineral loss<br />
at restoration margins, and reduced permeability of<br />
cut dentine beneath temporary crowns, respectively.<br />
Addition of up to 8.0% <strong>CPP</strong>-<strong>ACP</strong> into zinc oxide<br />
cements appears to be viable in terms of the<br />
compressive strength and film thickness achieved<br />
(Wong et al. 2006).<br />
A particularly interesting application of TM is the<br />
management of pathological tooth wear from acid<br />
regurgitation or severe bruxism (Meyers 2008).<br />
As well as prevebting dental erosion, laboratory<br />
studies suggest that frequent application of TM<br />
reduces enamel wear under conditions simulating<br />
bruxism and acid regurgitation, probably due to its<br />
lubrication properties (Ranjitkar et al. 2006, 2007,<br />
2008, 2009A&B). TM is able to reduce abrasive and<br />
acid-accelerated dentine wear (Narayana et al. 2006),<br />
supporting the use for TMP in patients <strong>with</strong> severe<br />
tooth wear from these differing causal pathways.<br />
Benefit has also been suggested for prevention of<br />
erosion from frequent consumption of wine (Piekarz<br />
et al. 2008).<br />
About the author:<br />
Professor LAURENCE WALSH BDSc<br />
PhD DDSc <strong>GC</strong>Ed FFOP(RCPA) FICD<br />
FPFA Laurence Walsh is Professor<br />
of Dental Science and Head of<br />
the School of Dentistry at the<br />
University of Queensland. He is a<br />
dental specialist in special needs<br />
dentistry and maintains a part time clinical practice<br />
in that field. Laurence is actively involved in the<br />
dental profession at a range of levels both nationally<br />
and internationally and has been involved in the<br />
development and assessment of chair-side diagnostic<br />
tools which use saliva and dental plaque. He is<br />
currently involved in studies of novel approaches for<br />
remineralisation of enamel and caries prevention.<br />
A. HALLGREN, L.G. PETERSSON and S.<br />
TWETMAN. Effect of a dental cream containing<br />
amorphous cream phosphate complexes on<br />
white spot lesion regression assessed by laser<br />
fluorescence. Oral Health Prev Dent 7;5(3):229-<br />
233, 2007.<br />
A.G. ANTONIO, V. PIERRO, and L.C. MAIA.<br />
Xylitol-based candies/lozenges: What is the<br />
evidence for caries-preventive effects? J Dent<br />
Res 88(Spec Iss A):2528, 2009.<br />
S. ARDU, N.V. CASTIONI, N. BENBACHIR, and<br />
I. KREJCI. Minimally invasive treatment of white<br />
spot enamel lesions. Quintessence Int 38(8):633-<br />
636, 2007.<br />
clinical corner<br />
23
D.G. AUGUSTSON, D. TANTBIROJN, and<br />
A. VERSLUIS. Recovery of Enamel Surface<br />
Hardness after Hydrochloric Acid Erosion. J Dent<br />
Res 89(Spec Iss B):4187, 2010.<br />
Z. AYTEPE, E.B. TUNA, D. ONER OZDAS, and<br />
E. YAMAC. Effect of <strong>CPP</strong>-<strong>ACP</strong> on Oral Health of<br />
Cerebral Palsy Children. J Dent Res 87(Spec<br />
Iss B):3343, 2008.<br />
D.L. BAILEY, G.G. ADAMS, C.E. TSAO, A.<br />
HYSLOP, K. ESCOBAR, D.J. MANTON, E.C.<br />
REYNOLDS and M.V. MORGAN. Regression<br />
of post-orthodontic lesions by a remineralizing<br />
cream. J Dent Res 88(12):1148-1153, 2009.<br />
C. BARONI, S. CHERSONI, S. MARCHIONNI,<br />
and C. PRATI. Supplementation of Molar Incisor<br />
Hypoplasia Affected Teeth: SEM/EDX study. J<br />
Dent Res 89(Spec Iss B):3845, 2010.<br />
S.M. BEHNAN, A.O. ARRUDA, H. HASSON,<br />
W. SOHN, C. GONZÁLEZ-CABEZAS, and M.C.<br />
PETERS. J Dent Res 88(Spec Iss A):2051,<br />
2009.<br />
A.K. BURWELL, and D. MUSCLE. Sustained<br />
Calcium Ion and pH Release from Calcium<br />
Phosphate-Containing Dentifrices. J Dent Res<br />
88(Spec Iss A):1936, 2009.<br />
F. CAI, Y. YUAN, C. REYNOLDS, and E.<br />
REYNOLDS. Water soluble calcium, phosphate<br />
and fluoride of various dental products. J Dent<br />
Res 88(Spec Iss B):57, 2009.<br />
F. CAI, P. SHEN, M.V. MORGAN, and E.C.<br />
REYNOLDS: <strong>Remineralization</strong> of enamel<br />
subsurface lesions<br />
in situ by sugar-free lozenges containing casein<br />
phosphopeptide-amorphous calcium phosphate.<br />
Aust Dent J 48(4): 240-243, 2003.<br />
P.C. CARUANA, S.A. MULAIFY, R. MOAZZEZ<br />
and D BARTLETT. The effect of casein and<br />
calcium containing paste on plaque pH following<br />
a subsequent carbohydrate challenge. J Dent<br />
37(7):522-526, 2009.<br />
A. CHAPMAN, S.B. JONES, and N.X. WEST.<br />
Different Ways of Applying <strong>GC</strong>-Dentifrice to<br />
Reduce Tooth Tissue Loss. J Dent Res 89(Spec<br />
Iss B):4793, 2010.<br />
N.J. COCHRANE, F. CAI, and E.C. REYNOLDS.<br />
QLF and TMR analysis of <strong>CPP</strong>-ACFP<br />
remineralized enamel in vitro. J Dent Res<br />
85(Spec Iss B):0192, 2006.<br />
N.J. COCHRANE, and E. REYNOLDS. Enamel<br />
Remineralisation <strong>with</strong> Casein Phosphopeptidestabilised<br />
Amorphous Calcium Fluoride<br />
Phosphate Complexes. J Dent Res 87(Spec Iss<br />
B):51, 2008.<br />
N.J. COCHRANE, R.J. MAYNE, S. RATNESER,<br />
M.G. WOODS, and E.C. REYNOLDS. Enamel<br />
Remineralisation Reduced Iatrogenic Enamel<br />
Damage During Orthodontic Adhesive Removal.<br />
J Dent Res 89(Spec Iss B):3647, 2010.<br />
K.J. CROSS, T.J. ATTARD, N.L. HUQ, and E.C.<br />
REYNOLDS. Structure and 15N-Dynamics of<br />
Casein Phosphopeptide-Amorphous Calcium<br />
Phosphate Nanocomplexes. J Dent Res<br />
85(Spec Iss B):2534, 2006.<br />
K.J. CROSS, N.L. HUQ and E.C. REYNOLDS.<br />
Casein phosphopeptides in oral healthchemistry<br />
and clinical applications. Curr Pharm<br />
Des 13(8):793-800, 2007.<br />
Y. DUAN, G. WANG, B. MATIS, X. CHENG,<br />
and Z. JIANG. Evaluation of the Efficacy of New<br />
Desensitizing Agents. J Dent Res 88(Spec Iss<br />
B):153, 2009.<br />
I. ELSAYAD, A. SAKR and Y. BADR.<br />
Combining casein phosphopeptide-amorphous<br />
calcium phosphate <strong>with</strong> fluoride: synergistic<br />
remineralization potential of artificially<br />
demineralized enamel or not? J Biomed Opt<br />
14(4):044039, 2009.<br />
F. GARCIA-GODOY, C.E. GARCIA-GODOY,<br />
C.M. FLAITZ, and J. HICKS. <strong>CPP</strong>-<strong>ACP</strong> Paste<br />
and <strong>ACP</strong>-Fluoride Varnish: In Vitro Root Caries. J<br />
Dent Res 88(Spec Iss A):2047, 2009.<br />
M. GOMES, C. FRANCCI, F.P. RODRIGUES, C.<br />
MIYAZAKI, N. SILIKAS, and D. WATTS. Effects<br />
of Pre and Post-Bleaching Agents on Enamel<br />
Gloss-Retention. J Dent Res 89(Spec Iss B):376,<br />
2010.<br />
J. HICKS. Casein Phosphopeptide-Amorphous<br />
Calcium Phosphate Paste: Root Surface Caries<br />
Formation. J Dent Res 84(Spec Iss A): 3275,<br />
2005.<br />
J. HICKS. Amorphous Calcium Phosphate-<br />
Casein Phosphopeptide Paste: Effect on Enamel<br />
Caries Formation. J Dent Res 85(Spec Iss A):<br />
2006, 2005.<br />
J. HICKS and C. FLAITZ. Effect of Calcium-<br />
Phosphate <strong>with</strong> Fluoride on Enamel Caries In<br />
Vitro. J Dent Res 89(Spec Iss A): 1213, 2010.<br />
K.A. HILLER, A.M. SCHNEIDER, and G.<br />
SCHMALZ. Topical coating of dentin tubuli by a<br />
calcium-phosphate containing paste. J Dent Res<br />
87(Spec Iss C):0702, 2008.<br />
A. HUANG, and D. TANTBIROJN.<br />
<strong>Remineralization</strong> of Eroded Teeth Using <strong>CPP</strong>-<br />
<strong>ACP</strong> Paste. J Dent Res 87(Spec Iss B):3267,<br />
2008.<br />
Y. IIJIMA, M. NISHIMURA, and S. IIJIMA. Acid<br />
Resistance of Remineralized Enamel by a<br />
Sugar-free Chewing Gum. J Dent Res 85(Spec<br />
Iss B):0184, 2006.<br />
A. ITTHAGARUN. <strong>Remineralization</strong> of Calcium<br />
Phosphopeptide-Amorphous Calcium Phosphate<br />
(<strong>CPP</strong>-<strong>ACP</strong>) on Caries-like Lesions. J Dent Res<br />
85(Spec Iss B): 010, 2005.<br />
U. KALLAYATHI, M. PANICH, and S.<br />
POOLTHONG. Effect of <strong>CPP</strong>-<strong>ACP</strong> Paste and<br />
Fluoride Gel on Eroded Enamel. J Dent Res<br />
87(Spec Iss B):0448, 2008.<br />
E.C. KAO, S. HODNETT, P. NGAN, C. MARTIN,<br />
and E. GUNEL. <strong>Remineralization</strong> Potential of<br />
Casein Phosphopeptide-Amorphous Calcium<br />
Phosphate - Confocal Microscopy Study. J Dent<br />
Res 87(Spec Iss A):0107, 2008.<br />
S. KARIYA, T. SATO, Y. SAKAGUCHI, and E.<br />
YOSHII. Fluoride Effect on Acid Resistance<br />
Capacity of <strong>CPP</strong>-<strong>ACP</strong> Containing Material. J<br />
Dent Res 83(Spec Iss A): 2045, 2004.<br />
K.B. KIM, S.M. KIM, N.K. CHOI, and K.H.<br />
YANG. <strong>Remineralization</strong> of the artificial caries<br />
lesion using <strong>CPP</strong>-<strong>ACP</strong> and Fluoride. J Dent Res<br />
86(Spec Iss B): 3280, 2007.<br />
Y. KITASAKO, K. SHIDA, K. MATIN, M. IKEDA,<br />
and J. TAGAMI. Effects of <strong>CPP</strong>-<strong>ACP</strong> on Enamel<br />
pH and Salivary Cariogenic Bacteria. J Dent Res<br />
88(Spec Iss A): 2048, 2009.<br />
A. KOWALCZYK, B. BITULINSKI, M.<br />
JAWORSKA, A. KIERKLO, M. PWAINSKA and<br />
E. DABROWSKA. Evaluation of the product<br />
based on Recaldent technology in the treatment<br />
of dentin hypersensitivity. Adv Med Sci 51 Suppl<br />
1:40-42, 2006.<br />
V.L. KUMAR, A. ITTHAGARUN and N.M. KING.<br />
The effect of casein phosphopeptide-amorphous<br />
calcium phosphate on remineralization of<br />
artificial caries-like lesions: an in vitro study. Aust<br />
Dent J 53(1):34-40, 2008.<br />
C. LLENA, L. FORNER and P. BACA.<br />
Anticariogenicity of casein phosphopeptideamorphous<br />
calcium phosphate: a review of the<br />
literature. J Contemp Dent Pract 10(3):1-9, 2009.<br />
S.F. LOVEL, N. PENDER, and S.M. HIGHAM. In<br />
vitro study to determine remineralising efficacy of<br />
casein phosphopeptide. J Dent Res 86(Spec Iss<br />
B):0063, 2007.<br />
D.J. MANTON, F. CAI, N. COCHRANE, G.D.<br />
WALKER, P. SHEN, G. ADAMS, L.B. MESSER,<br />
C. REYNOLDS, and E.C. REYNOLDS. In Situ<br />
Remineralisation by Sugar-Free Gums, One<br />
Containing <strong>CPP</strong>-<strong>ACP</strong>. J Dent Res 84(Spec Iss<br />
B): 0020, 2005<br />
D.J. MANTON, P. SHEN, F. CAI, N.J.<br />
COCHRANE, C. REYNOLDS, L.B. MESSER,<br />
and E.C. REYNOLDS. Remineralisation of White<br />
Spot Lesions in situ by Tooth Mousse. J Dent<br />
Res 85(Spec Iss B):0185, 2006.<br />
D.J. MANTON, F. CAI, L.J. MESSER, and<br />
E.C. REYNOLDS. Remineralisation of Enamel<br />
Subsurface Lesions in vitro by Tooth Mousse.<br />
J Dent Res 85(Spec Iss B):10, 2006.<br />
S.A. MAZZAOUI, M.F. BURROW, M.J.<br />
TYAS, S.G. DASHPER, D. EAKINS and<br />
E.C. REYNOLDS. Incorporation of Casein<br />
Phosphopeptide-Amorphous Calcium Phosphate<br />
into a Glass-ionomer Cement.<br />
J Dent Res 82(11): 914-918, 2003.<br />
I.A. MEYERS. Diagnosis and management<br />
of the worn dentition: risk management and<br />
prerestorative strategies for the oral and dental<br />
environment. Ann R Australas Coll Dent Surg 19:<br />
27-30, 2008.<br />
F.J. MILNAR. Considering biomodification and<br />
remineralization techniques as adjuncts to vital<br />
tooth-bleaching regimens. Compend Contin<br />
Educ Dent 28:234-240, 2007.<br />
K. MINAMI, D. INABA, M. YONEMITSU, M.<br />
KOGANEI, and M. ODA. Effects of Cheese<br />
and Milk Containing <strong>CPP</strong>-<strong>ACP</strong> on Enamel<br />
<strong>Remineralization</strong>. J Dent Res 83(Spec Iss A):<br />
2049, 2004<br />
M.V. MORGAN, D. BAILEY, G. ADAMS, C.<br />
TSAO, A. HYSLOP, K. ESCOBAR, D. MANTON,<br />
and E. REYNOLDS. A Clinical Trial Measuring<br />
White Spot Lesion Progression and Regression.<br />
J Dent Res 87(Spec Iss B): 0112, 2008A.<br />
M.V. MORGAN, G.G. ADAMS, D.L. BAILEY, C.E.<br />
TSAO, S.L. FISCHMAN and E.C. REYNOLDS.<br />
The anticariogenic effect of sugar-free gum<br />
containing <strong>CPP</strong>-<strong>ACP</strong> nanocomplexes on<br />
approximal caries determined using digital<br />
bitewing radiography. Caries Res 42(3):171-184,<br />
2008B.<br />
T. NARAYANA, S. RANJITKAR, J.A. KAIDONIS,<br />
G.C. TOWNSEND, and L.C. RICHARDS. An in<br />
vitro study of wear prevention in dentine. J Dent<br />
Res 85(Spec Iss B):2424, 2006.<br />
F. NG and D.J. MANTON. Aesthetic<br />
management of severely fluorosed incisors in an<br />
adolescent female. Aust Dent J 52(3):243-248,<br />
2007.<br />
I.J. PATERSON, T.N. CLOUGH, and P.<br />
ANDERSON. Calcium Ion Release from a<br />
Commercial Tooth Mousse. J Dent Res 87(Spec<br />
Iss C):0452, 2008.<br />
C. PIEKARZ, S. RANJITKAR, D. HUNT and J.<br />
24 Clinical corner<br />
www.gceurope.com
McINTYREJ. An in vitro assessment of the role<br />
of Tooth Mousse in preventing wine erosion. Aust<br />
Dent J 53(1): 22-25, 2008.<br />
K.A. PLONKA, M. PUKALLUS, A. BARNETT,<br />
T. HOLCOMBE, L.J. WALSH, and W.K. SEOW.<br />
Reducing Mutans Streptococci Colonisation: A<br />
Longitudinal Study Comparing Three Agents. J<br />
Dent Res 89(Spec Iss B):89, 2010.<br />
A. POITEVIN, M. PEUMANS, J. DE MUNCK,<br />
M. BRAEM, and B. VAN MEERBEEK. Clinical<br />
Effectiveness of a <strong>CPP</strong>-<strong>ACP</strong> Crème for Tooth<br />
Hypersensitivity Treatment. J Dent Res 83(Spec<br />
Iss B): 0136, 2004.<br />
C. RAHIOTIS and G. VOUGIOUKLAKIS. Effect<br />
of a <strong>CPP</strong>-<strong>ACP</strong> agent on the demineralization<br />
and remineralization of dentine in vitro. J Dent<br />
35(8):695-698, 2007.<br />
C. RAHIOTIS, G. VOUGIOUKLAKIS, and G.<br />
ELIADES. AFM and FTIR Characterization of<br />
Surfaces Treated <strong>with</strong> <strong>CPP</strong>-<strong>ACP</strong> Agent. J Dent<br />
Res 88(Spec Iss B):339, 2009.<br />
L. RAMALINGAM, L. B MESSER, and E.C.<br />
REYNOLDS. An in vitro investigation of the<br />
effects of casein phosphopeptide-stabilized<br />
amorphous calcium phosphate (<strong>CPP</strong>-<strong>ACP</strong>) on<br />
erosion of human dental enamel by a sports<br />
drink. J Dent Res 81(Spec Iss B): 2810, 2002.<br />
L. RAMALINGAM, L. B MESSER, and E.C.<br />
REYNOLDS. Adding casein phosphopeptideamorphous<br />
calcium phosphate to sports drinks to<br />
eliminate in vitro erosion. Pediatr Dent 27: 61-67,<br />
2005.<br />
S. RANJITKAR, J.A. KAIDONIS, G.C.<br />
TOWNSEND, and L.C. RICHARDS. Enamel<br />
wear prevention under conditions simulating<br />
bruxism and acid regurgitation. J Dent Res<br />
85(Spec Iss B):2428, 2006.<br />
S. RANJITKAR, J.A. KAIDONIS, G.C.<br />
TOWNSEND, and L.C. RICHARDS. The role of<br />
Tooth Mousse in preventing enamel wear. J Dent<br />
Res 86(Spec Iss B):0375, 2007.<br />
S. RANJITKAR, J.M. RODRIGUEZ, D.W.<br />
BARTLETT, J.A. KAIDONIS, G.C. TOWNSEND,<br />
and L.C. RICHARDS. The role of Tooth Mousse<br />
in reducing erosive tooth wear. J Dent Res<br />
87(Spec Iss B):2500, 2008.<br />
S. RANJITKAR, J.A. KAIDONIS, L.C.<br />
RICHARDS and G.C. TOWNSEND. The effect of<br />
<strong>CPP</strong>-<strong>ACP</strong> on enamel wear under severe erosive<br />
conditions. Arch Oral Biol 54(6):527-532, 2009A.<br />
S. RANJITKAR, K.M. RODRIGUEZ, J.A.<br />
KAIDONIS, L.C. RICHARDS, G.C. TOWNSEND<br />
and D.W. BARTLETT. The effect of casein<br />
phosphopeptide-amorphous calcium phosphate<br />
on erosive enamel and dentine wear by<br />
toothbrush abrasion. J Dent 37(4):250-254,<br />
2009B.<br />
S.K. RAO, G.S. BHAT, S. ARADHYA, A. DEVI<br />
and M. BHAT. Study of the Efficacy of Toothpaste<br />
Containing Casein Phosphopeptide in the<br />
Prevention of Dental Caries: a Randomized<br />
Controlled Trial in 12- to 15-Year-Old High Caries<br />
Risk Children in Bangalore, India. Caries Res<br />
43:430-435, 2009.<br />
E.C. REYNOLDS. <strong>Remineralization</strong> of enamel<br />
subsurface lesions by casein phosphopeptidestabilized<br />
calcium phosphate solutions. J Dent<br />
Res 76(9):1587-1595, 1997.<br />
E.C. REYNOLDS. Anticariogenic complexes<br />
of amorphous calcium phosphate stabilized by<br />
casein phosphopeptides: a review. Spec Care<br />
Dentist. 18(1):8-16, 1998.<br />
E.C. REYNOLDS. Calcium phosphate-based<br />
remineralization systems: scientific evidence?<br />
Aust Dent J 53(3):268-273, 2008.<br />
E.C. REYNOLDS. Casein phosphopeptideamorphous<br />
calcium phosphate: the scientific<br />
evidence. Adv Dent Res 21(1):25-29, 2009.<br />
E.C. REYNOLDS and L.J. WALSH. Additional<br />
aids to the remineralization of tooth structure.<br />
In: Mount GJ and Hume WR. Preservation<br />
and restoration of teeth, 2nd edition. Brisbane,<br />
Knowledge Books and Software 2005.<br />
E.C. REYNOLDS, N.J. COCHRANE, P. SHEN,<br />
F. CAI, G.D. WALKER, M.V. MORGAN, and<br />
C. REYNOLDS. Improved Plaque Uptake and<br />
Enamel <strong>Remineralization</strong> by Fluoride <strong>with</strong> <strong>CPP</strong>-<br />
<strong>ACP</strong> J Dent Res 85(Spec Iss B):2538, 2006.<br />
E. REYNOLDS, F. CAI, P. SHEN, G. WALKER,<br />
Y. YUAN, N. COCHRANE, D. MANTON, and C.<br />
REYNOLDS. Comparison of Tooth Mousse (MI<br />
Paste) <strong>with</strong> Clinpro in situ. J Dent Res 89(Spec<br />
Iss B):3645, 2010.<br />
Y. SAKAGUCHI, S. KATO, T. SATO, S. KARIYA,<br />
and L. CHEN. Preventing Acid Induced Enamel<br />
Demineralization Using <strong>CPP</strong>-<strong>ACP</strong> Containing<br />
Paste. J Dent Res 84(Spec Iss A): 2055, 2005.<br />
Y. SAKAGUCHI, S. KATO, T. SATO, S. KARIYA,<br />
S. NAGAO, and L. CHEN. <strong>Remineralization</strong><br />
Potential of <strong>CPP</strong>-<strong>ACP</strong> and Its Synergy <strong>with</strong><br />
Fluoride. J Dent Res 85(Spec Iss B):0191, 2006.<br />
V.J. SETIEN, M. KOIKE, P. RAGHUNATH, and<br />
K. AJLOUNI. Enamel Hardening Properties of<br />
Two Dental Pastes. J Dent Res 87(Spec Iss<br />
B):0926, 2008.<br />
T.R. SUDJALIM, M.G. WOODS, D.J. MANTON,<br />
and E.C. REYNOLDS. 0770 Prevention of<br />
Demineralisation Around Orthodontic Brackets<br />
In-vitro. J Dent Res 85(Spec Iss B):0770, 2006.<br />
T. SATO, K. YAMANAKA, and E. YOSHII. 1007<br />
Caries Prevention Potential of a Tooth-coating<br />
Material Containing Casein Phosphopeptide-<br />
Amorphous Calcium Phosphate (<strong>CPP</strong>-<strong>ACP</strong>). J<br />
Dent Res 82(Spec Iss B): 1007, 2003.<br />
H. SUKASAEM, M. PANICH, and S.<br />
POOLTHONG. Effect of <strong>CPP</strong>-<strong>ACP</strong> on Hardness<br />
of Enamel Eroded by Cola-drink. J Dent Res<br />
85(Spec Iss B):1673, 2006.<br />
T. TAKAMIZAWA, K. YAMAGUCHI, M.<br />
MIYAZAKI, K. HINOURA, and B.K. MOORE.<br />
Effect of <strong>CPP</strong>-<strong>ACP</strong> Paste on Demineralization of<br />
Bovine Tooth. J Dent Res 84(Spec Iss A): 1916,<br />
2005.<br />
U. THEERAPIBOON, R. PUANAIYAKA, and C.<br />
MANEENUT. <strong>Remineralization</strong> of Artificial Caries<br />
by <strong>CPP</strong>-<strong>ACP</strong> Paste. J Dent Res 87(Spec Iss<br />
B):3274, 2008.<br />
C.P. TRAJTENBERG, C. FLAITZ, and J. HICKS.<br />
<strong>CPP</strong>-<strong>ACP</strong> Paste <strong>with</strong> Fluoride: In Vitro Root<br />
Surface Caries Formation. J Dent Res 86(Spec<br />
Iss A):0500, 2007.<br />
C.P. TURSSI, F.A. MAEDA, D.C.F. MESSIAS,<br />
F.C. REHDER NETO, D. GALAFASSI, and M.C.<br />
SERRA. 2499 Progression of erosion following<br />
use of calcium and phosphorus compounds. J<br />
Dent Res 87(Spec Iss B):2499, 2008.<br />
J. VLACIC. In vivo and in vitro investigations<br />
of laser and non-laser therapies in treatment<br />
of root surface erosion and root surface caries.<br />
PhD thesis, University of Queensland, Brisbane,<br />
2007.<br />
J. VLACIC, I.A. MEYERS and L.J.WALSH.<br />
Combined <strong>CPP</strong>-<strong>ACP</strong> and photoactivated<br />
disinfection (PAD) therapy in arresting root<br />
surface caries: a case report. Brit Dent J<br />
203(8):457-459, 2007.<br />
G.D. WALKER, F. CAI, P. SHEN, D.L. BAILEY,<br />
Y, YUAN, N.J. COCHRANE, C. REYNOLDS<br />
and E.C. REYNOLDS. Consumption of milk<br />
<strong>with</strong> added casein phosphopeptide-amorphous<br />
calcium phosphate remineralizes enamel<br />
subsurface lesions in situ. Aust Dent J 54(3):245-<br />
249, 2009.<br />
L.J. WALSH. Tooth Mousse Portfolio. <strong>GC</strong> Asia<br />
Dental Pte Ltd, Singapore, 2003.<br />
L.J. WALSH. Tooth Mousse Portfolio 2. <strong>GC</strong> Asia<br />
Dental Pte Ltd, Singapore, 2004.<br />
L.J. WALSH. Tooth Mousse: Anthology of<br />
Applications, <strong>GC</strong> Asia Dental Pte Ltd, Singapore,<br />
2007.<br />
L.J. WALSH. The effects of <strong>GC</strong> Tooth Mousse on<br />
cervical dentinal sensitivity: a controlled clinical<br />
trial. Internat Dent (Australas Edn) 5(1):16-23,<br />
2010.<br />
L.J. WALSH, W.S. WANG, A. CAKAR, C.<br />
DEVANI, K.K. TRAN, and A. HALL. Effect of<br />
<strong>CPP</strong>-<strong>ACP</strong> versus Potassium Nitrate on Cervical<br />
Dentinal Hypersensitivity. J Dent Res 85(Spec<br />
Iss B):0947, 2006.<br />
R. WONG, J. PALAMARA, and P.R. WILSON.<br />
Incorporation of Casein Phosphopeptide-<br />
Amorphous Calcium Phosphate into a Temporary<br />
Cement. J Dent Res 85(Spec Iss B):0653, 2006.<br />
R.H. WONG, A.W. WONG, D. SIVAPALAN,<br />
M.H. NGUYEN, A.M. HO, A.S. WANG, and S.E.<br />
LAU. Penetration of Bleaching Agents in Tooth<br />
MousseTM Treated Bovine Incisors. J Dent Res<br />
89(Spec Iss B):4019, 2010.<br />
K. YAMAGUCHI, M. MIYAZAKI, T.<br />
TAKAMIZAWA, H INAGE and B.K. MOORE.<br />
Effect of <strong>CPP</strong>-<strong>ACP</strong> paste on mechanical<br />
properties of bovine enamel as determined by an<br />
ultrasonic device. J Dent 34(3):230-236, 2006.<br />
E. YASUDA, T. SATO, S. KATO, L. CHEN, and<br />
E. YOSHII. Comparative Study on <strong>CPP</strong>-<strong>ACP</strong> and<br />
TCP Based Products. J Dent Res 89(Spec Iss<br />
A):317, 2010.<br />
O. YAZICIOGLU, B. YAMAN, A. GULER, R.<br />
ASIYEV, and F. KORAY. Quantitative Evaluation<br />
of the Effect <strong>CPP</strong>-<strong>ACP</strong> on Enamel Caries. J Dent<br />
Res 89(Spec Iss B):3232, 2010.<br />
V. YENGOPAL and S. MICKENAUTSCH.<br />
Casein Phosphopeptide-Amorphous Calcium<br />
Phosphate (<strong>CPP</strong>-<strong>ACP</strong>) – a Systematic Review. J<br />
Dent Res 85(Spec Iss C): 010, 2006.<br />
V. YENGOPAL and S. MICKENAUTSCH. Caries<br />
preventive effect of casein phosphopeptideamorphous<br />
calcium phosphate (<strong>CPP</strong>-<strong>ACP</strong>): a<br />
meta-analysis. Acta Odontol Scand 21:1-12,<br />
2009.<br />
Q. XIE, C.D. WU, and A.K.B. BEDRAN-RUSSO.<br />
<strong>Remineralization</strong> Effects of <strong>CPP</strong>-<strong>ACP</strong> and<br />
Proanthocyanidin on Artificial Root Caries. J<br />
Dent Res 86(Spec Iss A):0512, 2007.<br />
C.H. ZHOU, X.H. SUN, X.C. ZHU.<br />
Quantification of remineralized effect of casein<br />
phosphopeptiode-amorphous calcium phosphate<br />
on post-orthodontic white spot lesion. Shanghai<br />
Kou Qiang Yi Xue 18(5): 449-454, 2009.<br />
clinical corner<br />
25
A closer look at remineralisation and <strong>CPP</strong>-<strong>ACP</strong><br />
As a publication, MID believes in the importance of informing dentists about the<br />
evidence available on MI topics so they can make scientifically sound choices in the<br />
treatment of their patients. In the research-clinical application jigsaw puzzle, it is<br />
essential to make all the pieces fit in order to see the whole picture.<br />
This process is outlined in the flow diagram below<br />
Systematic review -> academic explanation -> clinical application<br />
Systematic Review<br />
Title: Caries preventive effect of casein phosphopeptideamorphous<br />
calcium phosphate (<strong>CPP</strong>-<strong>ACP</strong>): a meta-analysis<br />
Objective. This systematic review <strong>with</strong> meta-analyses<br />
sought to answer the following question: ‘‘Does <strong>CPP</strong>-<strong>ACP</strong><br />
[casein phosphopeptide-amorphous calcium phosphate],<br />
when introduced into the oral environment, provide any<br />
caries-preventive benefit superior to that of any other<br />
intervention or placebo?’’<br />
Material and methods. Seven electronic databases were<br />
searched for trials relevant to the review question. Twelve<br />
articles were accepted after application of inclusion and<br />
exclusion criteria.<br />
Results. Of the accepted articles, five in situ<br />
randomized control trials (RCT) could be pooled for metaanalyses.<br />
During the short-term (7_21 days) in situ trials,<br />
participants wore appliances containing enamel slabs that<br />
were analyzed in the laboratory after exposure to <strong>CPP</strong>-<br />
<strong>ACP</strong>. The pooled in situ results showed a weighted mean<br />
difference (WMD) of the percentage remineralization<br />
scores in favor of chewing gum <strong>with</strong> 18.8 mg <strong>CPP</strong>-<strong>ACP</strong> as<br />
compared to chewing gum <strong>with</strong>out <strong>CPP</strong>-<strong>ACP</strong> (WMD _8.01;<br />
95% CI: _10.54 to _5.48; p_0.00001), as well as compared<br />
to no intervention (WMD_13.56; 95% CI: _16.49 to _10.62;<br />
p_0.00001). A significant higher remineralization effect<br />
was also observed after exposure to 10.0 mg <strong>CPP</strong>-<strong>ACP</strong><br />
(_7.75; 95% CI: _9.84 to _5.66; p_0.00001). One long-term<br />
in vivo RCT (24 months) <strong>with</strong> a large sample size (n_2720)<br />
found that the odds of a tooth surface’s progressing to<br />
caries was 18% less in subjects who chewed sugar-free<br />
gum containing 54 mg <strong>CPP</strong>-<strong>ACP</strong> than in control subjects<br />
who chewed gum <strong>with</strong>out <strong>CPP</strong>-<strong>ACP</strong> (p_ 0.03).<br />
Conclusion. Within the limitations of this systematic<br />
review <strong>with</strong> meta-analysis, the results of the clinical in<br />
situ trials indicate a short-term remineralization effect of<br />
<strong>CPP</strong>-<strong>ACP</strong>. Additionally, the promising in vivo RCT results<br />
suggest a caries preventing effect for long-term clinical<br />
<strong>CPP</strong>-<strong>ACP</strong> use. Further randomized control trials are<br />
needed in order to confirm these initial results in vivo.<br />
Article details :<br />
Yengopal V, Mickenautsch S. Caries preventive effect of<br />
casein phosphopeptide-amorphous calcium phosphate<br />
(<strong>CPP</strong>-<strong>ACP</strong>): a meta-analysis. Acta Odontol Scand 2009; 67:<br />
321-32.<br />
The academic explanation<br />
Dr Steffen Mickenautsch,<br />
academic researcher in<br />
Johannesburg, South Africa<br />
MID: Of all the studies available<br />
on this subject, why were you<br />
only able to use 5 for your meta<br />
analysis?<br />
Steffen Mickenautsch: Firstly, we<br />
had to exclude other studies because they were either:<br />
conducted in the laboratory and not in the clinic; done on<br />
animal and not on human tissue or did not compare <strong>CPP</strong>-<br />
<strong>ACP</strong> against anything else.<br />
The problem <strong>with</strong> studies from the laboratory is that<br />
one really cannot be sure that the results would be the<br />
same in the ‘real’ world. The same is valid when studying<br />
the effect of treatments on animal tissue. The results of<br />
either are important to justify whether studies should be<br />
conducted on patients or not, because it is not ethical<br />
to study new treatments on humans if laboratory and/<br />
or animal studies show that these are not successful.<br />
Therefore, laboratory and/or animal studies are important<br />
first steps for testing new drugs or treatments before they<br />
can be allowed to be tested on humans. However, in our<br />
systematic review we wanted to know whether <strong>CPP</strong>-<br />
<strong>ACP</strong> is beneficial for clinical use on patients and neither,<br />
laboratory nor animal studies, can answer this question.<br />
That is why we had to exclude them.<br />
Clinical studies that fail to compare a new type of<br />
treatment against another, (preferably the type of standard<br />
treatment commonly used to date) are unable to answer<br />
the question whether the new treatment is better, the same<br />
or worse. But this was exactly what we were trying to find<br />
out, thus we could not include these types of studies either.<br />
After all these considerations we had 11 studies<br />
available to work <strong>with</strong>. From these, 5 were similar enough<br />
to be combined in a meta-analysis. A meta-analysis is a<br />
statistical method by which the separate results of several<br />
studies are combined to one average result. However, in<br />
order to be able to do this the studies need to be similar,<br />
e.g. in their methods and outcomes, before they can be<br />
combined. Otherwise the meta-analysis would produce<br />
meaningless results.<br />
26 evidence<br />
mi.gceurope.com
We reviewed the other 6 studies separately in our<br />
systematic review <strong>with</strong>out including them in the metaanalysis.<br />
MID: What criteria did the 5 that you selected meet and<br />
why is this important?<br />
Steffen Mickenautsch: These 5 studies compared <strong>CPP</strong>-<br />
<strong>ACP</strong> against other types of treatments. They provided<br />
information on how well each, the <strong>CPP</strong>-<strong>ACP</strong> and the other<br />
treatment worked on patients and then compared both<br />
results to find out which one was better. This was exactly<br />
what we needed to know. In addition, they all fulfilled the<br />
requirements for meta-analysis; they all used <strong>CPP</strong>-<strong>ACP</strong> in<br />
dental chewing gum; they included the same <strong>CPP</strong>-<strong>ACP</strong><br />
concentration; study length and used the same type of<br />
other treatment for comparison.<br />
MID: Please explain your introduction: “The advantages<br />
of meta-analysis over qualitative synthesis is that it<br />
provides the opportunity to identify a treatment effect as<br />
statistically significant (p
MID: In your conclusion it states that this meta<br />
analysis shows that <strong>CPP</strong>-<strong>ACP</strong> does have a short term<br />
remineralising effect – what should a practising dentist<br />
who reads this understand about this statement?<br />
Steffen Mickenautsch: If a patient is identified to have a<br />
high caries activity or a high risk to develop cavities in the<br />
near future, the established short-term effect promises<br />
that <strong>CPP</strong>-<strong>ACP</strong> is able to stop the further progression of<br />
(non-cavitated) carious lesions and is able to prevent the<br />
development of such. Therefore, <strong>CPP</strong>-<strong>ACP</strong> may be used<br />
as one immediate intervention in the treatment of such<br />
patients.<br />
MID: You also looked at one study that examined the<br />
long-term effect of <strong>CPP</strong>-<strong>ACP</strong> – what were the important<br />
elements of this particular study?<br />
Steffen Mickenautsch: In that study, patients were given<br />
<strong>CPP</strong>-<strong>ACP</strong> containing chewing gum over the period of 2<br />
years and were compared to similar patients that chewed<br />
sugar-free chewing gum <strong>with</strong>out <strong>CPP</strong>-<strong>ACP</strong>. The result<br />
showed that patients using the <strong>CPP</strong>-<strong>ACP</strong> containing gum<br />
had 18% lesser likelihood of caries progression. This result<br />
was statistically significant, thus very unlikely to be a<br />
coincident. All patients had active caries and the <strong>CPP</strong>-<strong>ACP</strong><br />
gum showed to be more effective to stop further progress<br />
of the existing carious lesions. In that regard one has to<br />
remember that sugar-free chewing gum is considered<br />
to be effective against caries too. That means, that the<br />
group of patients <strong>with</strong>out the <strong>CPP</strong>-<strong>ACP</strong> would have also<br />
experienced an anticaries effect. Only, this effect was<br />
observed to be larger in the <strong>CPP</strong>-<strong>ACP</strong> group.<br />
MID: Is this systematic review conclusive or is more<br />
research needed?<br />
Steffen Mickenautsch: From an academic point of view,<br />
the current knowledge about <strong>CPP</strong>-<strong>ACP</strong> allows us to be<br />
optimistic about the claim that <strong>CPP</strong>-<strong>ACP</strong> is effective<br />
against caries. The currently available studies provide<br />
evidence that this claim is not only plausible but also<br />
tends to prove it to be correct rather than disproving it. To<br />
have more high quality research will be of advantage to<br />
validate and strengthen this claim even further.<br />
“In my practice the compliance rate and repurchase<br />
of the Tooth Mousse / Mi paste has<br />
been very high, and this indicates to me that<br />
the patients are happy <strong>with</strong> the results, and<br />
find value in the products.”<br />
Andrew Brostek<br />
The clinical application<br />
Dr Andrew Brostek, private<br />
dentist in Perth, Australia<br />
MID: For how many years have you<br />
been using Tooth Mousse/MI Paste<br />
in your practice?<br />
Andrew Brostek: I began soon<br />
after it was first made available in<br />
Australia, but have used it more<br />
intensively in the last three years.<br />
MID: What factors made you decide to start using it in<br />
your practice and recommend it to your patients in the<br />
first place?<br />
Andrew Brostek: After being exposed to the information<br />
about <strong>CPP</strong>-<strong>ACP</strong> presented at several Continuing Education<br />
courses, and then reading some of the early studies<br />
published by Professor Eric Reynolds and his University<br />
of Melbourne research group, I realised that using<br />
the products containing <strong>CPP</strong>-<strong>ACP</strong> (<strong>GC</strong> Tooth Mousse<br />
/ Mi Paste, Tooth Mousse Plus (<strong>CPP</strong>-ACFP) and the <strong>GC</strong><br />
Recaldent chewing gum) had great potential to benefit<br />
my patients.<br />
MID: After reading the abstract of the meta-analysis<br />
on the remineralising effect of <strong>CPP</strong>-<strong>ACP</strong>, how will this<br />
affect the way in which you use and prescribe Tooth<br />
Mousse/MI Paste in your practice, if at all?<br />
Andrew Brostek: The publication of this meta-analysis<br />
review reinforces my own belief in the effectiveness of<br />
<strong>CPP</strong>-<strong>ACP</strong>, based on my own clinical experiences <strong>with</strong><br />
compliant patients. Evidence based dentistry is essential<br />
to guide clinicians in improving treatment protocols, and<br />
I await further data from in vivo trials to confirm these<br />
results. In terms of prescribing, I use the fluoride versions<br />
<strong>CPP</strong>-ACFP i.e. Tooth Mousse Plus/ Mi Paste Plus for high<br />
risk patients over the age of 7 years, as study results show<br />
an increased lesion preventive effect <strong>with</strong> the fluoride<br />
combination. I usually prescribe nightly application of a<br />
pea-sized amount of the Tooth Mousse Plus / Mi paste<br />
Plus (immediately before bed), but in very high caries<br />
rate patients, I prescribe both a morning and nightly<br />
application, <strong>with</strong> concomitant use of Recaldent gum<br />
at least twice per day (10 minutes per application). As<br />
evidenced by studies, chewing the <strong>CPP</strong>-<strong>ACP</strong> gum, three<br />
times per day was very effective in caries-rate reduction.<br />
MID: Do you find this meta-analysis easy to interpret,<br />
in terms of applying this to your daily practice?<br />
Andrew Brostek: My understanding of the value of metaanalysis<br />
is to provide a more objective assessment of the<br />
available statistically significant literature. So yes, it does<br />
have value to me in suggesting improved protocols. Again<br />
28 evidence<br />
mi.gceurope.com
Patient <strong>with</strong> extensive white spot lesions After two months, showing partial remineralisation after<br />
twice daily application of <strong>CPP</strong>-<strong>ACP</strong><br />
speaking as a full-time clinician, I am very interested in any<br />
improvement in caries-preventive benefit and particularly<br />
in achieving enamel remineralisation.<br />
My daily practice protocols vary depending on the<br />
patient lesion presentation. For poor compliance patients<br />
<strong>with</strong> rampant caries, I mainly rely on prescribing twicedaily<br />
brushing <strong>with</strong> a high-dose fluoride (5000 ppm)<br />
toothpaste, and clinician-applied fluoride varnish at recall.<br />
The prevention of demineralisation by the use of high<br />
concentrations of fluoride is of critical importance in our<br />
anti-caries chemical armentarium.<br />
But for compliant high-risk patients <strong>with</strong> multiple early<br />
lesions (white-spot lesions) I use a slightly different protocol<br />
emphasising the use of <strong>CPP</strong>-<strong>ACP</strong>. To achieve increased<br />
remineralisation of these white spot lesions, especially<br />
in younger people <strong>with</strong> unaesthetic anterior lesions, I<br />
prescribe daily <strong>CPP</strong>-<strong>ACP</strong> (or <strong>CPP</strong>-ACFP) Tooth Mousse / Mi<br />
Paste application, in combination <strong>with</strong> twice-daily tooth<br />
brushing <strong>with</strong> a lower fluoride concentration (1000 ppm)<br />
toothpaste. This allows greater sub-surface remineralisation<br />
of non-cavitated lesions, evidenced over time by the<br />
reversal of the white-spot appearance. Unfortunately<br />
utilising a higher 5000 ppm fluoride toothpaste will seal<br />
off the unaesthetic surface scar rapidly, not allowing the<br />
deeper subsurface remineralisation to occur. Of course,<br />
regular effective plaque removal, diet and lifestyle<br />
modification, normal saliva quality and quantity, are all<br />
important factors in modifying the disease risk and aiding<br />
in tooth remineralisation.<br />
MID: As a busy clinician, how do you keep yourself<br />
updated on developments in clinical evidence in<br />
dentistry, particularly in MID?<br />
Andrew Brostek: That’s a tough question, as most<br />
of us are fairly busy in our own dental practices. The<br />
role of Continuing Education courses is important and<br />
attendance is compulsory in Australia. Belonging to<br />
various professional dental bodies helps, as it entitles you<br />
to some dental journal subscriptions, and staying current<br />
is important. I think that allows most of us to entertain our<br />
own specific dental interests.<br />
MID: Some dental academics say that clinicians and the<br />
practice-based evidence they record is very important<br />
in filling the gaps left by academic research studies.<br />
Have you captured and recorded any interesting data<br />
on remineralisation <strong>with</strong> Tooth Mousse/MI Paste since<br />
you’ve started using it? If so, what are some of the<br />
most interesting trends that you’ve noticed?<br />
Andrew Brostek: I find recording practice-based<br />
evidence hard to do in a typical busy day. Many of you<br />
may identify <strong>with</strong> my daily problems, where some patients<br />
come late to appointments, or extra ‘pain’ patients are<br />
over-booked into an already busy schedule. My main<br />
contribution is to have my dental camera handy to<br />
document any interesting dental issues quickly.<br />
My belief in <strong>CPP</strong>-<strong>ACP</strong> has been reinforced by observing<br />
non-cavitated white-spot lesions becoming remineralised<br />
over periods of between six weeks and 3 months <strong>with</strong><br />
regular daily use of the Tooth Mousse / Mi paste by<br />
the patient. Progress is easy to observe, as the lesions<br />
change from the surface white scar to a relatively normal<br />
tooth appearance. The clinical protocol I use to achieve<br />
this is quite simple: The enamel lesion is etched <strong>with</strong><br />
phosphoric acid for 10 seconds and then Tooth Mousse /<br />
Mi Paste is immediately applied. The patient then applies<br />
the Tooth Mousse nightly until lesion reversal occurs. In<br />
difficult cases, I might re-etch at one-month recall, or<br />
even additionally at the two-month recall, to aid <strong>CPP</strong>-<strong>ACP</strong><br />
penetration by removing surface protein from the enamel.<br />
In my practice the compliance rate and re-purchase<br />
of the Tooth Mousse / Mi paste has been very high, and<br />
this indicates to me that the patients are happy <strong>with</strong><br />
the results, and find value in the products. Many of the<br />
mothers are also using the <strong>CPP</strong>-<strong>ACP</strong> products on their<br />
younger children’s teeth for caries prevention.<br />
In conjunction <strong>with</strong> our individual patient caries risk<br />
assessment protocols (diet /lifestyle analyses, and the use<br />
of saliva and plaque testing on select patients) and then<br />
specific treatment targeting (such as the use of <strong>CPP</strong>-<strong>ACP</strong>),<br />
my dental hygienists and I believe we are benefitting our<br />
patients, and practising modern 21st century dentistry.<br />
evidence<br />
29
MI toolkit<br />
1<br />
30 mi toolkit<br />
mi.gceurope.com<br />
2<br />
4
What’s inside the tube?<br />
Tooth Mousse, also known as MI Paste in<br />
some regions of the world, is considered the<br />
number one remineralizing paste that is<br />
backed by sound scientific evidence.<br />
For low to medium risk patients, MI Paste<br />
or Tooth Mousse is recommended. However,<br />
for patients <strong>with</strong> high risk, MI Paste<br />
Plus/Tooth Mousse Plus contains<br />
additional 900ppm Flouride and<br />
is therefore better suited to<br />
their oral health requirements.<br />
3<br />
Studies that prove the clinical superiority of <strong>GC</strong> Tooth<br />
Mousse/MI Paste are:<br />
z The only remineralizing cream <strong>with</strong> proven a scientific<br />
record <strong>with</strong> more then 200 scientific references<br />
and having sold material for more than 160 million<br />
applications worldwide since the original Australasian<br />
introduction in 2002<br />
Abstract 3645 - IADR 2010, Barcelona, Spain. Comparison of Tooth<br />
Mousse (MI Paste) <strong>with</strong> Clinpro in situ. E Reynolds, F Cai, P. Shen, G<br />
Walker, Y Yuan, N Cochrane, D Manton, C Reynolds. Oral Health CRC,<br />
Melbourne Dental School, University of Melbourne, Australia<br />
z Searching from 7 databases and about 3500 articles, it<br />
has been concluded that Tooth Mousse/MI Paste Plus<br />
does <strong>Remineralization</strong> and has Caries protection effect.<br />
V. YENGOPAL & S. MICKENAUTSCH. University of the Witwatersrand,<br />
South Africa. Acta Odontologica Scandinavica 2009<br />
Click on the numbers to learn more<br />
1. <strong>GC</strong> Tooth Mousse offers Three-in-One solution<br />
5<br />
2. Uses for Tooth Mousse/MI Paste<br />
mi toolkit<br />
3. Contraindications<br />
4. Application methods<br />
5. Packaging<br />
6. Additional instructions<br />
6<br />
31
The Science behind Remin<br />
The only Reminaralizing cream <strong>with</strong> proven a Scientific record <strong>with</strong> more then 200<br />
scientific references and having sold material for more than 160 million applications<br />
worldwide since the original Australasian introduction in 2002*<br />
Articles identified through<br />
keyword search in<br />
databases (n=3459)<br />
Articles included for more<br />
detailed review (n=35)<br />
Articles accepted (n=12)<br />
Randomized control trials<br />
(n=11)<br />
Randomized control trials<br />
included in meta-analysis<br />
(n=5)<br />
Articles <strong>with</strong>out relevance<br />
to review questions<br />
excluded (n=3424)<br />
Articles excluded due<br />
to non-compliance <strong>with</strong><br />
exclusion criteria (n=3424)<br />
Systematic review (n=1)<br />
Randomized control trials<br />
not included in metaanalysis<br />
(n=6)<br />
Searching from 7 databases and about 3500 articles, it has been concluded that Tooth Mousse/MI<br />
Paste Plus does <strong>Remineralization</strong> and has Caries protection effect.*<br />
*V. YENGOPAL & S. MICKENAUTSCH. University of the Witwatersrand, South Africa. Acta Odontologica Scandinavica 2009<br />
32 mi toolkit<br />
mi.gceurope.com
PLACEBO<br />
RECALDENT HIGH FLOURIDE PRODUCTS<br />
PLACEBO PASTE<br />
1000PPM F PASTE<br />
CLINPRO<br />
5000PPM F PASTE<br />
TOOTH MOUSSE<br />
MI PASTE PLUS<br />
Notice no change in the demineralised White<br />
Spot Lesion after the use of a Placebo Paste<br />
Notice the hard hypermineralised layer<br />
formed due to the very high fluoride ppm,<br />
this acts like a hard shell preventing the<br />
<strong>Remineralization</strong> of the underlying White<br />
Spot Lesion lesion.<br />
Concluding that Ca and PO4 are the most<br />
crucial elements for <strong>Remineralization</strong> and<br />
Fluoride only acts as a catalyst.<br />
Notice no Hard impervious layer as compared<br />
to High Fluoride containing products.<br />
Tooth Mousse and MI Paste Plus show a<br />
uniform <strong>Remineralization</strong> of the Enamel and<br />
Dentine structures. However, MI Paste Plus<br />
shows higher <strong>Remineralization</strong> due to the fact<br />
that Fluoride acts as a catalyst to encourage<br />
Calcium and Phosphate to enter inside the<br />
Tooth structure<br />
*Abstract 3645 - IADR 2010, Barcelona, Spain. Comparison of Tooth Mousse (MI Paste) <strong>with</strong> Clinpro in situ. E Reynolds, F Cai, P. Shen, G Walker,<br />
Y Yuan, N Cochrane, D Manton, C Reynolds. Oral Health CRC, Melbourne Dental School, University of Melbourne, Australia<br />
mi toolkit<br />
33
minimum intervention, maximum return<br />
mid<br />
Issue 3