maturity-onset diabetes of the young (mody) - GGH Journal
maturity-onset diabetes of the young (mody) - GGH Journal
maturity-onset diabetes of the young (mody) - GGH Journal
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
MODY As a Paradigm<br />
for Type 2 DM<br />
The advances in our understanding <strong>of</strong> MOOY are relevant<br />
to our understanding <strong>of</strong> <strong>the</strong> genetics and pathophysiology<br />
<strong>of</strong> type 2 OM in general. This is exemplified<br />
by <strong>the</strong> identification <strong>of</strong> mutations in MOOY genes in subjects<br />
with late-<strong>onset</strong> type 2 OM.2-4 Fur<strong>the</strong>rmore, <strong>the</strong>re<br />
is <strong>of</strong>ten variation within MOOY pedigrees with regard to<br />
<strong>the</strong> age <strong>of</strong> <strong>onset</strong> such that multiple affected members in<br />
some MOOY pedigrees may have <strong>onset</strong> <strong>of</strong> disease after<br />
age 40. While <strong>the</strong> later age at diagnosis sometimes<br />
reflects a delay in ascertainment because <strong>of</strong> a mild phenotype,<br />
it also suggests that o<strong>the</strong>r factors, both genetic<br />
and environmental, may modify <strong>the</strong> expression <strong>of</strong> <strong>diabetes</strong><br />
due to specific mutations in MOOY gene loci. This<br />
leads to <strong>the</strong> consideration that mild mutations or polymorphisms<br />
in MOOY genes may result in only a slight<br />
impairment <strong>of</strong> protein function and, <strong>the</strong>refore, may contribute<br />
to <strong>the</strong> expression <strong>of</strong> <strong>diabetes</strong> in a polygenic con-text.<br />
A common polymorphism at codon 98 <strong>of</strong> <strong>the</strong> HNF-1 a<br />
gene (MODY3), which is not linked to OM in a Mendelian<br />
fashion, is never<strong>the</strong>less associated with reduced serum<br />
C-peptide and a reduced insulin response to glucose<br />
challenge. The prevalent yet incompletely penetrant<br />
D76N mutation in IPF-1 (MODY4) is associated with<br />
marked impairment in insulin secretion even in normal homeostasis, with some subjects remaining well controlled<br />
on diet or sulfonylureas and o<strong>the</strong>rs progressing<br />
glucose-tolerant carriers <strong>of</strong> <strong>the</strong> mutation. Oigenic inheritance<br />
in a family with late-<strong>onset</strong> type 2 OM has been<br />
documented in which <strong>the</strong> severity <strong>of</strong> <strong>the</strong> diabetic phenotype<br />
appears to relate to <strong>the</strong> cosegregation <strong>of</strong> 2 distinct<br />
mutations in 2 different pancreatic transcription factor<br />
genes, IPF-1 (MODY4) and 181, a transcriptional regulator<br />
<strong>of</strong> GLUT2 gene expression. Mutations that impair<br />
[3-cell compensatory mechanisms also could act in<br />
concert with genetic defects in insulin action to cause<br />
<strong>diabetes</strong>.<br />
POSSIBLE<br />
ROLE OF GENETIC SCREENING<br />
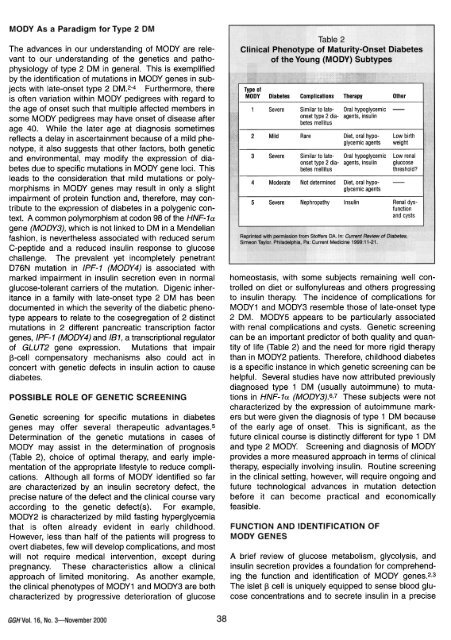
to insulin <strong>the</strong>rapy. The incidence <strong>of</strong> complications for<br />
MOOY1 and MOOY3 resemble those <strong>of</strong> late-<strong>onset</strong> type<br />
2 OM. MOOY5 appears to be particularly associated<br />
with renal complications and cysts. Genetic screening<br />
can be an important predictor <strong>of</strong> both quality and quantity<br />
<strong>of</strong> life (Table 2) and <strong>the</strong> need for more rigid <strong>the</strong>rapy<br />
than in MOOY2 patients. Therefore, childhood <strong>diabetes</strong><br />
is a specific instance in which genetic screening can be<br />
helpful. Several studies have now attributed previously<br />
diagnosed type 1 OM (usually autoimmune) to mutations<br />
in HNF-1a (MODY3).6,7 These subjects were not<br />
characterized by <strong>the</strong> expression <strong>of</strong> autoimmune markers<br />
but were given <strong>the</strong> diagnosis <strong>of</strong> type 1 OM because<br />
<strong>of</strong> <strong>the</strong> early age <strong>of</strong> <strong>onset</strong>. This is significant, as <strong>the</strong><br />
future clinical course is distinctly different for type 1 OM<br />
Genetic screening for specific mutations in <strong>diabetes</strong><br />
genes may <strong>of</strong>fer several <strong>the</strong>rapeutic advantages.5<br />
Determination <strong>of</strong> <strong>the</strong> genetic mutations in cases <strong>of</strong><br />
MODY may assist in <strong>the</strong> determination <strong>of</strong> prognosis and type 2 MOOY. Screening and diagnosis <strong>of</strong> MOOY<br />
(Table 2), choice <strong>of</strong> optimal <strong>the</strong>rapy, and early implementation<br />
<strong>of</strong> <strong>the</strong> appropriate lifestyle to reduce compli-cations. <strong>the</strong>rapy, especially involving insulin. Routine screening<br />
provides a more measured approach in terms <strong>of</strong> clinical<br />
Although all forms <strong>of</strong> MODY identified so far in <strong>the</strong> clinical setting, however, will require ongoing and<br />
are characterized by an insulin secretory defect, <strong>the</strong> future technological advances in mutation detection<br />
precise nature <strong>of</strong> <strong>the</strong> defect and <strong>the</strong> clinical course vary before it can become practical and economically<br />
according to <strong>the</strong> genetic defect(s). For example, feasible.<br />
MODY2 is characterized by mild fasting hyperglycemia<br />
that is <strong>of</strong>ten already evident in early childhood. FUNCTION AND IDENTIFICATION OF<br />
However, less than half <strong>of</strong> <strong>the</strong> patients will progress to MODY GENES<br />
overt <strong>diabetes</strong>, few will develop complications, and most<br />
will not require medical intervention, except duringpregnancy. A brief review <strong>of</strong> glucose metabolism, glycolysis, and<br />
These characteristics allow a clinical insulin secretion provides a foundation for comprehending<br />
<strong>the</strong> function and identification <strong>of</strong> MODY genes.2,3<br />
approach <strong>of</strong> limited monitoring. As ano<strong>the</strong>r example,<br />
<strong>the</strong> clinical phenotypes <strong>of</strong> MODY1 and MODY3 are both The islet ~ cell is uniquely equipped to sense blood glucose<br />
concentrations and to secrete insulin in a characterized by progressive deterioration <strong>of</strong> glucose<br />
precise<br />
<strong>GGH</strong>Vol. 16, No.3-November 2000<br />
38