Effects of ibuprofen, diclofenac, naproxen, and piroxicam on ... - Sigo
Effects of ibuprofen, diclofenac, naproxen, and piroxicam on ... - Sigo
Effects of ibuprofen, diclofenac, naproxen, and piroxicam on ... - Sigo
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Nezvalova-Henriksen et al.<br />
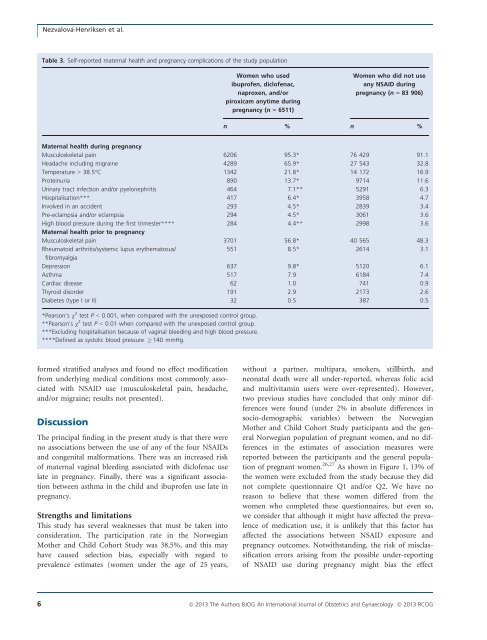
Table 3. Self-reported maternal health <str<strong>on</strong>g>and</str<strong>on</strong>g> pregnancy complicati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> the study populati<strong>on</strong><br />
Women who used<br />
ibupr<str<strong>on</strong>g>of</str<strong>on</strong>g>en, dicl<str<strong>on</strong>g>of</str<strong>on</strong>g>enac,<br />
<str<strong>on</strong>g>naproxen</str<strong>on</strong>g>, <str<strong>on</strong>g>and</str<strong>on</strong>g>/or<br />
<str<strong>on</strong>g>piroxicam</str<strong>on</strong>g> anytime during<br />
pregnancy (n = 6511)<br />
Women who did not use<br />
any NSAID during<br />
pregnancy (n = 83 906)<br />
n % n %<br />
Maternal health during pregnancy<br />
Musculoskeletal pain 6206 95.3* 76 429 91.1<br />
Headache including migraine 4289 65.9* 27 543 32.8<br />
Temperature > 38.5°C 1342 21.8* 14 172 16.9<br />
Proteinuria 890 13.7* 9714 11.6<br />
Urinary tract infecti<strong>on</strong> <str<strong>on</strong>g>and</str<strong>on</strong>g>/or pyel<strong>on</strong>ephritis 464 7.1** 5291 6.3<br />
Hospitalisati<strong>on</strong>*** 417 6.4* 3958 4.7<br />
Involved in an accident 293 4.5* 2839 3.4<br />
Pre-eclampsia <str<strong>on</strong>g>and</str<strong>on</strong>g>/or eclampsia 294 4.5* 3061 3.6<br />
High blood pressure during the first trimester**** 284 4.4** 2998 3.6<br />
Maternal health prior to pregnancy<br />
Musculoskeletal pain 3701 56.8* 40 565 48.3<br />
Rheumatoid arthritis/systemic lupus erythematosus/<br />
551 8.5* 2614 3.1<br />
fibromyalgia<br />
Depressi<strong>on</strong> 637 9.8* 5120 6.1<br />
Asthma 517 7.9 6184 7.4<br />
Cardiac disease 62 1.0 741 0.9<br />
Thyroid disorder 191 2.9 2173 2.6<br />
Diabetes (type I or II) 32 0.5 387 0.5<br />
*Pears<strong>on</strong>’s v 2 test P < 0.001, when compared with the unexposed c<strong>on</strong>trol group.<br />
**Pears<strong>on</strong>’s v 2 test P < 0.01 when compared with the unexposed c<strong>on</strong>trol group.<br />
***Excluding hospitalisati<strong>on</strong> because <str<strong>on</strong>g>of</str<strong>on</strong>g> vaginal bleeding <str<strong>on</strong>g>and</str<strong>on</strong>g> high blood pressure.<br />
****Defined as systolic blood pressure 140 mmHg.<br />
formed stratified analyses <str<strong>on</strong>g>and</str<strong>on</strong>g> found no effect modificati<strong>on</strong><br />
from underlying medical c<strong>on</strong>diti<strong>on</strong>s most comm<strong>on</strong>ly associated<br />
with NSAID use (musculoskeletal pain, headache,<br />
<str<strong>on</strong>g>and</str<strong>on</strong>g>/or migraine; results not presented).<br />
Discussi<strong>on</strong><br />
The principal finding in the present study is that there were<br />
no associati<strong>on</strong>s between the use <str<strong>on</strong>g>of</str<strong>on</strong>g> any <str<strong>on</strong>g>of</str<strong>on</strong>g> the four NSAIDs<br />
<str<strong>on</strong>g>and</str<strong>on</strong>g> c<strong>on</strong>genital malformati<strong>on</strong>s. There was an increased risk<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> maternal vaginal bleeding associated with dicl<str<strong>on</strong>g>of</str<strong>on</strong>g>enac use<br />
late in pregnancy. Finally, there was a significant associati<strong>on</strong><br />
between asthma in the child <str<strong>on</strong>g>and</str<strong>on</strong>g> ibupr<str<strong>on</strong>g>of</str<strong>on</strong>g>en use late in<br />
pregnancy.<br />
Strengths <str<strong>on</strong>g>and</str<strong>on</strong>g> limitati<strong>on</strong>s<br />
This study has several weaknesses that must be taken into<br />
c<strong>on</strong>siderati<strong>on</strong>. The participati<strong>on</strong> rate in the Norwegian<br />
Mother <str<strong>on</strong>g>and</str<strong>on</strong>g> Child Cohort Study was 38.5%, <str<strong>on</strong>g>and</str<strong>on</strong>g> this may<br />
have caused selecti<strong>on</strong> bias, especially with regard to<br />
prevalence estimates (women under the age <str<strong>on</strong>g>of</str<strong>on</strong>g> 25 years,<br />
without a partner, multipara, smokers, stillbirth, <str<strong>on</strong>g>and</str<strong>on</strong>g><br />
ne<strong>on</strong>atal death were all under-reported, whereas folic acid<br />
<str<strong>on</strong>g>and</str<strong>on</strong>g> multivitamin users were over-represented). However,<br />
two previous studies have c<strong>on</strong>cluded that <strong>on</strong>ly minor differences<br />
were found (under 2% in absolute differences in<br />
socio-demographic variables) between the Norwegian<br />
Mother <str<strong>on</strong>g>and</str<strong>on</strong>g> Child Cohort Study participants <str<strong>on</strong>g>and</str<strong>on</strong>g> the general<br />
Norwegian populati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> pregnant women, <str<strong>on</strong>g>and</str<strong>on</strong>g> no differences<br />
in the estimates <str<strong>on</strong>g>of</str<strong>on</strong>g> associati<strong>on</strong> measures were<br />
reported between the participants <str<strong>on</strong>g>and</str<strong>on</strong>g> the general populati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> pregnant women. 26,27 As shown in Figure 1, 13% <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the women were excluded from the study because they did<br />
not complete questi<strong>on</strong>naire Q1 <str<strong>on</strong>g>and</str<strong>on</strong>g>/or Q2. We have no<br />
reas<strong>on</strong> to believe that these women differed from the<br />
women who completed these questi<strong>on</strong>naires, but even so,<br />
we c<strong>on</strong>sider that although it might have affected the prevalence<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> medicati<strong>on</strong> use, it is unlikely that this factor has<br />
affected the associati<strong>on</strong>s between NSAID exposure <str<strong>on</strong>g>and</str<strong>on</strong>g><br />
pregnancy outcomes. Notwithst<str<strong>on</strong>g>and</str<strong>on</strong>g>ing, the risk <str<strong>on</strong>g>of</str<strong>on</strong>g> misclassificati<strong>on</strong><br />
errors arising from the possible under-reporting<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> NSAID use during pregnancy might bias the effect<br />
6 ª 2013 The Authors BJOG An Internati<strong>on</strong>al Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> Obstetrics <str<strong>on</strong>g>and</str<strong>on</strong>g> Gynaecology ª 2013 RCOG