Effect of early goal directed therapy on tissue perfusion in patients ...
Effect of early goal directed therapy on tissue perfusion in patients ...
Effect of early goal directed therapy on tissue perfusion in patients ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
World J Emerg Med, Vol 4, No 2, 2013<br />
Orig<strong>in</strong>al Article<br />
117<br />
<str<strong>on</strong>g>Effect</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>early</str<strong>on</strong>g> <str<strong>on</strong>g>goal</str<strong>on</strong>g> <str<strong>on</strong>g>directed</str<strong>on</strong>g> <str<strong>on</strong>g>therapy</str<strong>on</strong>g> <strong>on</strong> <strong>tissue</strong><br />
perfusi<strong>on</strong> <strong>in</strong> <strong>patients</strong> with septic shock<br />
Yuan-hua Lu 1 , L<strong>in</strong>g Liu 2 , Xiao-hua Qiu 2 , Q<strong>in</strong> Yu 2 , Yi Yang 2 , Hai-bo Qiu 2<br />
1<br />
ICU, Jiangxi Prov<strong>in</strong>cial People’s Hospital, Nanchang 330006, Ch<strong>in</strong>a<br />
2<br />
Critical Care Medic<strong>in</strong>e, Zh<strong>on</strong>g-da Hospital Affiliated to Southeast University, Nanj<strong>in</strong>g 210009, Ch<strong>in</strong>a<br />
Corresp<strong>on</strong>d<strong>in</strong>g Author: Hai-bo Qiu, Email: haiboq2000@yahoo.com.cn<br />
BACKGROUND: This study aimed to observe the effect <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>early</str<strong>on</strong>g> <str<strong>on</strong>g>goal</str<strong>on</strong>g> <str<strong>on</strong>g>directed</str<strong>on</strong>g> <str<strong>on</strong>g>therapy</str<strong>on</strong>g> (EGDT)<br />
<strong>on</strong> <strong>tissue</strong> perfusi<strong>on</strong>, microcirculati<strong>on</strong> and <strong>tissue</strong> oxygenati<strong>on</strong> <strong>in</strong> <strong>patients</strong> with septic shock.<br />
METHODS: Patients with <str<strong>on</strong>g>early</str<strong>on</strong>g> septic shock (
118 Lu et al<br />
World J Emerg Med, Vol 4, No 2, 2013<br />
EGDT may not be sufficient for <strong>patients</strong> with septic shock.<br />
Microcirculati<strong>on</strong> dysfuncti<strong>on</strong> <strong>in</strong> <strong>patients</strong> with septic<br />
shock is characterized by the low density <str<strong>on</strong>g>of</str<strong>on</strong>g> perfused<br />
small vessels and the heterogeneity <str<strong>on</strong>g>of</str<strong>on</strong>g> microvascular<br />
blood flow. [4,5] Microcirculatory perfusi<strong>on</strong> <strong>in</strong>dices are<br />
more markedly impaired <strong>in</strong> n<strong>on</strong>survivors compared with<br />
survivors, and microvascular dysfuncti<strong>on</strong> is associated<br />
with organ failure. [4–6] In additi<strong>on</strong>, microcirculatory<br />
alterati<strong>on</strong>s <strong>in</strong> <strong>patients</strong> with septic shock are <strong>in</strong>dependent<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> macrocirculati<strong>on</strong>. [6,7] Tissue oxygenati<strong>on</strong> measured <strong>in</strong><br />
peripheral <strong>tissue</strong> as transcutaneous pressure <str<strong>on</strong>g>of</str<strong>on</strong>g> oxygen<br />
and carb<strong>on</strong> dioxide (PtcO 2 , PtcCO 2 ) is <str<strong>on</strong>g>early</str<strong>on</strong>g>, and more<br />
sensitive <strong>in</strong>dices reflect<strong>in</strong>g hypoperfusi<strong>on</strong> and hypoxia <strong>in</strong><br />
shock [8,9] and trends <str<strong>on</strong>g>of</str<strong>on</strong>g> PtcO 2 are related to the prognosis<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>patients</strong>. [10,11] As a result, m<strong>on</strong>itor<strong>in</strong>g <str<strong>on</strong>g>of</str<strong>on</strong>g> resuscitati<strong>on</strong><br />
dur<strong>in</strong>g EGDT can help to identify <strong>tissue</strong> hypoperfusi<strong>on</strong>.<br />
The present study aims to <strong>in</strong>vestigate the effects <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
EGDT <strong>on</strong> <strong>tissue</strong> perfusi<strong>on</strong> by m<strong>on</strong>itor<strong>in</strong>g <str<strong>on</strong>g>of</str<strong>on</strong>g> PtcO 2 , PtcCO 2<br />
and subl<strong>in</strong>gual microcirculati<strong>on</strong> before and after EGDT.<br />
METHODS<br />
Patients<br />
Patients with <str<strong>on</strong>g>early</str<strong>on</strong>g> septic shock (
World J Emerg Med, Vol 4, No 2, 2013<br />
119<br />
(EVLW), extra-vascular lung water <strong>in</strong>dex (EVLWI),<br />
oxygen delivery (DO 2 ), oxygen c<strong>on</strong>sumpti<strong>on</strong> (VO 2 ),<br />
oxygen extracti<strong>on</strong> rate (O 2 ext), and lactate (Lac).<br />
Microcirculati<strong>on</strong> <strong>in</strong>dexes were PVD, PPV, MFI, and<br />
heterogeneity <strong>in</strong>dex. Tissue oxygenati<strong>on</strong> <strong>in</strong>dexes<br />
<strong>in</strong>cluded PtcO 2 , PtcCO 2 , PtcO 2 /FiO 2 , PtcO 2 shunt [(PaO 2 –<br />
PtcO 2 )/PaO 2 ], PtcCO 2 <strong>in</strong>dex (PtcCO 2 /PaCO 2 ), and PCO 2<br />
gap (difference between PtcCO 2 and PaCO 2 ).<br />
Implementati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT and data collecti<strong>on</strong><br />
Protocol <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT<br />
Fluid resuscitati<strong>on</strong> was d<strong>on</strong>e to achieve a CVP <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
8 to 12 mmHg. If the MAP was less than 65 mmHg,<br />
vasopressors were given to ma<strong>in</strong>ta<strong>in</strong> a mean arterial<br />
pressure <str<strong>on</strong>g>of</str<strong>on</strong>g> at least 65 mmHg and ur<strong>in</strong>e output <str<strong>on</strong>g>of</str<strong>on</strong>g> at least<br />
0.5 mL/kg per hour. If central venous oxygen saturati<strong>on</strong><br />
(ScvO 2 ) was less than 70%, red cells were transfused to<br />
achieve a hematocrit <str<strong>on</strong>g>of</str<strong>on</strong>g> at least 30%. After the CVP, MAP,<br />
and hematocrit were thus optimized, if the ScvO 2 was less<br />
than 70%, dobutam<strong>in</strong>e was adm<strong>in</strong>istered until the ScvO 2<br />
was 70% or higher or until a maximal dose <str<strong>on</strong>g>of</str<strong>on</strong>g> 20 µg per<br />
kilogram per m<strong>in</strong>ute was given.<br />
Criteria <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT<br />
The criteria for EGDT were as follows: MAP≥65<br />
mmHg, CVP 8–12 mmHg, ScvO 2 ≥70%, and ur<strong>in</strong>e output<br />
≥0.5 mL/kg per hour.<br />
Data collecti<strong>on</strong><br />
Data <str<strong>on</strong>g>of</str<strong>on</strong>g> hemodynamics, microcirculati<strong>on</strong> and <strong>tissue</strong><br />
oxygenati<strong>on</strong> <strong>in</strong>dex were collected before and after<br />
EGDT.<br />
Statistical analysis<br />
Data were presented as mean ±SD, if they accorded<br />
with normal distributi<strong>on</strong> or presented as a median and<br />
<strong>in</strong>terquartile range (IQR) (M [P25, P75]). Paired sample<br />
Student's t test and Wilcox<strong>on</strong>'s rank-sum test were<br />
used as appropriate. Variable correlati<strong>on</strong> was analyzed<br />
with Pears<strong>on</strong>'s product-moment correlati<strong>on</strong> coefficient<br />
method. Statistical significance was set when P
120 Lu et al<br />
World J Emerg Med, Vol 4, No 2, 2013<br />
<str<strong>on</strong>g>Effect</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT <strong>on</strong> systemic oxygenati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<strong>patients</strong> with septic shock<br />
ScvO 2 after EGDT was higher than that before<br />
EGDT (P0.05)<br />
and so was between DO 2 , VO 2 and others (Table 3).<br />
<str<strong>on</strong>g>Effect</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT <strong>on</strong> subl<strong>in</strong>gual microcirculati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>patients</strong> with septic shock<br />
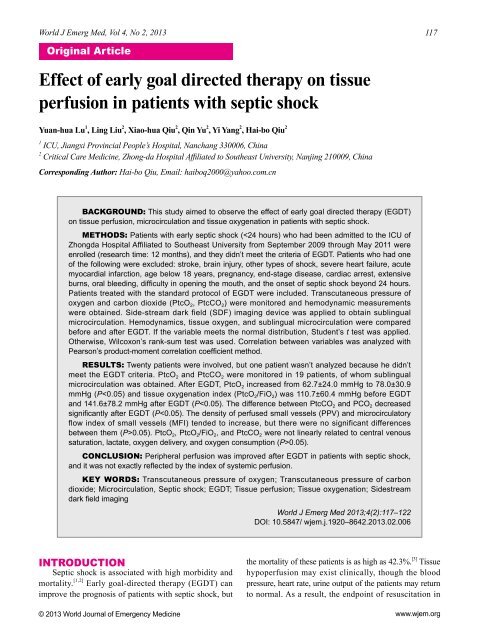
Subl<strong>in</strong>gual microcirculati<strong>on</strong> was m<strong>on</strong>itored <strong>in</strong> 4<br />
<strong>patients</strong>. TVD, PVD, PPV, MFI and heterogeneity <strong>in</strong>dexes<br />
were not changed significantly before and after EGDT<br />
(P>0.05). But PPV and MFI showed the trend <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>in</strong>creas<strong>in</strong>g<br />
(P was 0.051 and 0.074 respectively) (Table 4 and Figure 1).<br />
Table 3. The effect <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT <strong>on</strong> systemic oxygenati<strong>on</strong> dur<strong>in</strong>g the<br />
period <str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock (n=19)<br />
Variables Before EGDT After EGDT t /Z P<br />
pH 7.425±0.058 7.405±0.043 3.177 0.005<br />
ScvO 2 0.766±0.081 0.807±0.062 2.907 0.009<br />
DO 2 (mL•m<strong>in</strong> –1 •m –2 ) 618.0±252.5 677.5±250.9 1.419 0.181<br />
VO 2 (mL•m<strong>in</strong> –1 •m –2 ) 117.8±53.1 113.5±36.8 0.411 0.688<br />
O 2 ext 0.202±0.071 0.176±0.050 1.622 0.131<br />
Lac (mmol/L) 2.28±1.50 2.22±1.06 0.332 0.744<br />
PaO 2 (mmHg) 84.7 (69.2–119.2) 85.1 (81.3–102.6) 0.241 0.809<br />
PcvO 2 (mmHg) 48.4 (39.4–49.9) 49.4 (43.3–53.9) 2.335 0.020<br />
PaO 2 /FiO 2 (mmHg) 153.8 (105.8– 221.7) 163.5 (116.0–206.0) 0.684 0.494<br />
Ur<strong>in</strong>e output<br />
(mL/kg per hour)<br />
1.14±1.21 2.08±1.73 3.362 0.003<br />
Table 4. The effect <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT <strong>on</strong> microcirculati<strong>on</strong> dur<strong>in</strong>g the period <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
septic shock (n=4)<br />
Variables Before EGDT After EGDT t P<br />
TVD (mm/mm 2 ) 20.16±5.05 19.48±4.85 0.290 0.791<br />
PVD (mm/mm 2 ) 16.14±4.81 17.88±4.19 0.578 0.604<br />
PPV (%) 74.05±15.63 85.73±8.39 3.160 0.051<br />
MFI 1.56±0.49 2.23±0.17 2.704 0.074<br />
Heterogeneity <strong>in</strong>dex 0.29±0.05 0.26±0.14 0.479 0.665<br />
TVD: total small vessel density; PVD: perfused small vessel density;<br />
PPV: proporti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> perfused small vessels; MFI: microcirculatory flow<br />
<strong>in</strong>dex.<br />
A<br />
Figure 1. The subl<strong>in</strong>gual microcirculati<strong>on</strong> before and after EGDT <strong>in</strong><br />
<strong>on</strong>e patient. A: Before EGDT, sludged <strong>in</strong>dividual erythrocytes can be<br />
seen <strong>in</strong> microvessels; B: After EGDT, <strong>in</strong>dividual erythrocytes cannot<br />
be seen <strong>in</strong> microvessels.<br />
B<br />
<str<strong>on</strong>g>Effect</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT <strong>on</strong> <strong>tissue</strong> oxygenati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<strong>patients</strong> with septic shock<br />
PtcO 2 and PtcO 2 /FiO 2 after EGDT <strong>in</strong>creased more<br />
significantly than those before EGDT (P0.05). PtcCO 2 was<br />
l<strong>in</strong>ear related to MAP (r=–0.354, P=0.029) (Figure 3), but<br />
Table 5. The effect <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT <strong>on</strong> <strong>tissue</strong> oxygenati<strong>on</strong> (n=19)<br />
Variables Before EGDT After EGDT P<br />
PtcO 2 (mmHg) 62.7±24.0 78.0±30.9 0.016<br />
PtcO 2 /FiO 2 (mmHg) 110.7±60.4 141.6±78.2 0.015<br />
PtcO 2 shunt 0.309±0.355 0.185±0.300 0.024<br />
PtcCO 2 (mmHg) 37.0 (31.0–46.0) 36.0 (29.0–41.0) 0.009<br />
PtcCO 2 <strong>in</strong>dex 1.05 (0.87–1.23) 1.02 (0.85–1.12) 0.025<br />
PCO 2 gap (mmHg) 1.7 (–5.0–6.1) 0.6 (–5.50–3.50) 0.040<br />
PtcO 2 shunt=(PaO 2 –PtcO 2 )/PaO 2 ; PtcCO 2 <strong>in</strong>dex=PtcCO 2 /PaCO 2 ; PCO 2<br />
gap=PtcCO 2 –PaCO 2 .<br />
PtcO 2 /FiO 2 (mmHg)<br />
400<br />
350<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
y=2.088x–36.64<br />
R 2 =0.125<br />
P=0.029<br />
0<br />
40 50 60 70 80 90 100 110<br />
MAP (mmHg)<br />
Figure 2. The correlati<strong>on</strong> between PtcO 2 /FiO 2 and MAP (n=19).<br />
PtcO 2 (mmHg)<br />
400<br />
350<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
y=0.276x+58.28<br />
R 2 =0.125<br />
P=0.029<br />
0<br />
40 50 60 70 80 90 100 110<br />
MAP (mmHg)<br />
Figure 3. The correlati<strong>on</strong> between PtcCO 2 and MAP (n=19).<br />
www.wjem.org
World J Emerg Med, Vol 4, No 2, 2013<br />
121<br />
not to CO, CI, SV, SVI, EVLW and EVLWI (P>0.05).<br />
The correlati<strong>on</strong> between <strong>tissue</strong> oxygenati<strong>on</strong><br />
<strong>in</strong>dex and systemic oxygenati<strong>on</strong> <strong>in</strong>dex<br />
No correlati<strong>on</strong> was found am<strong>on</strong>g PtcO 2 , DO 2 , VO 2 ,<br />
O 2 ext, ScvO 2 , PaO 2 , PvO 2 and Lac (All P>0.05). PtcO 2 /<br />
FiO 2 was not l<strong>in</strong><str<strong>on</strong>g>early</str<strong>on</strong>g> related to DO 2 , VO 2 , O 2 ext, ScvO 2 ,<br />
PvO 2 and Lac (All P>0.05). There was no correlati<strong>on</strong><br />
between PtcCO 2 and DO 2 , VO 2 , O 2 ext, ScvO 2 and Lac<br />
(All P>0.05).<br />
DISCUSSION<br />
Hypoxia due to <strong>tissue</strong> and organ hypoperfusi<strong>on</strong><br />
was the essence <str<strong>on</strong>g>of</str<strong>on</strong>g> shock. As a result, <str<strong>on</strong>g>early</str<strong>on</strong>g> correcti<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>tissue</strong> and organ hypoxia was essential dur<strong>in</strong>g shock<br />
resuscitati<strong>on</strong>. Unfortunately, <strong>tissue</strong> hypoperfusi<strong>on</strong> and<br />
hypoxia might still exist although hemodynamic <strong>in</strong>dexes<br />
such as BP, HR, ur<strong>in</strong>e output, ScvO 2 and systemic<br />
oxygenati<strong>on</strong> <strong>in</strong>dex such as DO 2 were with<strong>in</strong> the normal<br />
range. [10] Recogniti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the above limitati<strong>on</strong>s with global<br />
m<strong>on</strong>itor<strong>in</strong>g has stimulated efforts to look for 'biomarkers'<br />
at the regi<strong>on</strong>al level. C<strong>on</strong>sequently, it is necessary to<br />
identify the tools <str<strong>on</strong>g>of</str<strong>on</strong>g> m<strong>on</strong>itor<strong>in</strong>g <str<strong>on</strong>g>of</str<strong>on</strong>g> shock resuscitati<strong>on</strong><br />
from the macrocirculati<strong>on</strong> to microcirculati<strong>on</strong>, from<br />
global oxygenati<strong>on</strong> to <strong>tissue</strong> oxygenati<strong>on</strong>. And SDF<br />
and <strong>tissue</strong> oxygen tensi<strong>on</strong> were the possible m<strong>on</strong>itor<strong>in</strong>g<br />
technologies.<br />
The oxygen debt theory <str<strong>on</strong>g>of</str<strong>on</strong>g> shock <strong>in</strong>dicates that shock<br />
is a state <str<strong>on</strong>g>of</str<strong>on</strong>g> hypoperfusi<strong>on</strong> at the cellular level that occurs<br />
when DO 2 to the <strong>tissue</strong>s falls below VO 2 requirements,<br />
and thus represents an imbalance between <strong>tissue</strong> DO 2 and<br />
VO 2 . [13] In the EGDT study ScvO 2 reflect<strong>in</strong>g the balance<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> DO 2 and VO 2 is used as an endpo<strong>in</strong>t <str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock<br />
resuscitati<strong>on</strong> and it improves the prognosis <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>patients</strong><br />
with septic shock. But EGDT <strong>patients</strong> still have a high<br />
mortality, and many <strong>patients</strong> who met the criteria <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
EGDT still have <strong>tissue</strong> hypoperfusi<strong>on</strong> and hypoxia. Hence,<br />
meet<strong>in</strong>g the criteria <str<strong>on</strong>g>of</str<strong>on</strong>g> EGDT does not mean the match<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> DO 2 and VO 2 and the correcti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>tissue</strong> hypoxia .<br />
In additi<strong>on</strong>, impairment <str<strong>on</strong>g>of</str<strong>on</strong>g> oxygen extracti<strong>on</strong> is <strong>on</strong>e <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the ma<strong>in</strong> characteristics <str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock. [14] Thus <strong>patients</strong><br />
with septic shock still have the evidence <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>tissue</strong> hypoxia<br />
though DO 2 is normal or supernormal after treatment.<br />
Microcirculati<strong>on</strong> dysfuncti<strong>on</strong> exists dur<strong>in</strong>g the period<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock, and it is <strong>in</strong>dependent from correcti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
macrocirculati<strong>on</strong> dysfuncti<strong>on</strong>. In our study, PPV and MFI<br />
showed the trend <str<strong>on</strong>g>of</str<strong>on</strong>g> improvement compared with those<br />
before the treatment, similar to the study <str<strong>on</strong>g>of</str<strong>on</strong>g> Trzeciak and<br />
colleagues. [5] But the heterogeneity <str<strong>on</strong>g>of</str<strong>on</strong>g> microcirculati<strong>on</strong><br />
was not improved because <str<strong>on</strong>g>of</str<strong>on</strong>g> the small sample size.<br />
Therefore, further cl<strong>in</strong>ical study is needed.<br />
Yu et al [15,16] observed that oxygen challenge test<br />
(OCT) greater than 21 mmHg denotes the improvement<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>tissue</strong> perfusi<strong>on</strong> dur<strong>in</strong>g shock resuscitati<strong>on</strong>, and<br />
treat<strong>in</strong>g <strong>patients</strong> with septic shock to an OCT value<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> 40 mmHg or more might provide an endpo<strong>in</strong>t <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
resuscitati<strong>on</strong> with better survival than resuscitat<strong>in</strong>g<br />
to DO 2 and ScvO 2 . Our study revealed that PtcO 2 and<br />
PtcO 2 /FiO 2 <strong>in</strong>creased and PtcCO 2 , PtcO 2 shunt, PtcCO 2<br />
<strong>in</strong>dex and PCO 2 gap decreased after EGDT, <strong>in</strong>dicat<strong>in</strong>g<br />
that EGDT improved the local <strong>tissue</strong> oxygenati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<strong>patients</strong> with septic shock.<br />
The correlati<strong>on</strong> between <strong>in</strong>dex <str<strong>on</strong>g>of</str<strong>on</strong>g> global perfusi<strong>on</strong><br />
and systemic oxygenati<strong>on</strong> such as lactate and ScvO 2 and<br />
local <strong>tissue</strong> oxygenati<strong>on</strong> <strong>in</strong>dex such as PtcO 2 has rarely<br />
been studied. A study [17] revealed that oxygen <strong>tissue</strong><br />
saturati<strong>on</strong> (StO 2 ) is less or not related to SvO 2 , ur<strong>in</strong>e<br />
output and lactate, suggest<strong>in</strong>g that global perfusi<strong>on</strong> is<br />
not c<strong>on</strong>sistent with local <strong>tissue</strong> perfusi<strong>on</strong>. In our study,<br />
PtcO 2 , PtcO 2 /FiO 2 and PtcCO 2 were not correlated to<br />
DO 2 , VO 2 , O 2 ext, ScvO 2 and lactate, show<strong>in</strong>g that global<br />
<strong>tissue</strong> perfusi<strong>on</strong> and oxygenati<strong>on</strong> were not <strong>in</strong> accord with<br />
local perfusi<strong>on</strong> and oxygenati<strong>on</strong>.<br />
LIMITATIONS<br />
First, the sample size was small especially the sample<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>patients</strong> who had microcirculati<strong>on</strong> data. Sec<strong>on</strong>d, septic<br />
shock was largely due to pneum<strong>on</strong>ia, not c<strong>on</strong>sistent with<br />
the cause <str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock <strong>in</strong> ICU. Third, randomizati<strong>on</strong><br />
and bl<strong>in</strong>dness were not adopted <strong>in</strong> the study <strong>in</strong> additi<strong>on</strong><br />
to the design <str<strong>on</strong>g>of</str<strong>on</strong>g> a c<strong>on</strong>trol group. C<strong>on</strong>sequently,<br />
subjective factors could not be removed completely and<br />
c<strong>on</strong>found<strong>in</strong>g factors and bias could not be vanished.<br />
In c<strong>on</strong>clusi<strong>on</strong>, EGDT could improve local <strong>tissue</strong><br />
perfusi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>patients</strong> with septic shock and global<br />
perfusi<strong>on</strong> might not reflect local <strong>tissue</strong> perfusi<strong>on</strong> dur<strong>in</strong>g<br />
the resuscitati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock.<br />
ACKNOWLEDGEMENTS<br />
We are grateful to teacher B<strong>in</strong>g-wei Chen, who is work<strong>in</strong>g<br />
at School <str<strong>on</strong>g>of</str<strong>on</strong>g> Public Health <str<strong>on</strong>g>of</str<strong>on</strong>g> Southeast University, for his help<br />
<strong>in</strong> statistical analysis. We are also thankful to doctors and nurses<br />
work<strong>in</strong>g <strong>in</strong> the Zh<strong>on</strong>g-da Hospital Affiliated to Southeast University.<br />
Fund<strong>in</strong>g: N<strong>on</strong>e.<br />
Ethical approval: The present study was approved Ethical<br />
www.wjem.org
122 Lu et al<br />
World J Emerg Med, Vol 4, No 2, 2013<br />
Committee <str<strong>on</strong>g>of</str<strong>on</strong>g> Zh<strong>on</strong>gda Hospital Affiliated to Southeast University,<br />
Nanj<strong>in</strong>g, Ch<strong>in</strong>a.<br />
C<strong>on</strong>flicts <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>in</strong>terest: The authors have no compet<strong>in</strong>g <strong>in</strong>terests<br />
relevant to the present study.<br />
C<strong>on</strong>tributors: Lu YH proposed and wrote the paper. All authors<br />
c<strong>on</strong>tributed to edit<strong>in</strong>g the f<strong>in</strong>al manuscript for c<strong>on</strong>tent and style.<br />
REFERENCES<br />
1 Annane D, Aegerter P, Jars-Gu<strong>in</strong>cestre MC, Guidet B; CUB-<br />
Réa Network. Current epidemiology <str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock: the CUB-<br />
Réa Network. Am J Respir Crit Care Med 2003; 168: 165–172.<br />
2 Marty P, Roquilly A, Vallée F, Luzi A, Ferré F, Fourcade O, et<br />
al. Lactate clearance for death-predicti<strong>on</strong> <strong>in</strong> severe sepsis or<br />
septic shock <strong>patients</strong> dur<strong>in</strong>g the first 24 hours <strong>in</strong> Intensive Care<br />
Unit. An observati<strong>on</strong>al study. Ann Intensive Care 2013; 3: 3.<br />
3 Rivers E, Nguyen B, Havstad S, Ressler J, Muzz<strong>in</strong> A, Knoblich<br />
B, et al. Early <str<strong>on</strong>g>goal</str<strong>on</strong>g>-<str<strong>on</strong>g>directed</str<strong>on</strong>g> <str<strong>on</strong>g>therapy</str<strong>on</strong>g> <strong>in</strong> the treatment <str<strong>on</strong>g>of</str<strong>on</strong>g> severe<br />
sepsis and septic shock. N Engl J Med 2001; 345: 1368–1377.<br />
4 De Backer D, Creteur J, Preiser JC, Dubois MJ, V<strong>in</strong>cent JL.<br />
Microvascular blood flow is altered <strong>in</strong> <strong>patients</strong> with sepsis. Am<br />
J Respir Crit Care Med 2002; 166: 98–104.<br />
5 Trzeciak S, Dell<strong>in</strong>ger RP, Parrillo JE, Guglielmi M, Bajaj J,<br />
Abate NL, et al. Early microcirculatory perfusi<strong>on</strong> derangements<br />
<strong>in</strong> <strong>patients</strong> with severe sepsis and septic shock: relati<strong>on</strong>ship to<br />
hemodynamics, oxygen transport, and survival. Ann Emerg<br />
Med 2007; 49: 88–98, 98.e1–2.<br />
6 Sakr Y, Dubois MJ, De Backer D, Creteur J, V<strong>in</strong>cent JL.<br />
Persistent microcirculatory alterati<strong>on</strong>s are associated with<br />
organ failure and death <strong>in</strong> <strong>patients</strong> with septic shock. Crit Care<br />
Med 2004; 32: 1825–1831.<br />
7 De Backer D, Creteur J, Dubois MJ, Sakr Y, Koch M, Verdant<br />
C, et al. The effects <str<strong>on</strong>g>of</str<strong>on</strong>g> dobutam<strong>in</strong>e <strong>on</strong> microcirculatory<br />
alterati<strong>on</strong>s <strong>in</strong> <strong>patients</strong> with septic shock are <strong>in</strong>dependent <str<strong>on</strong>g>of</str<strong>on</strong>g> its<br />
systemic effects. Crit Care Med 2006; 34: 403–408.<br />
8 Tremper KK, Waxman K, Shoemaker WC. <str<strong>on</strong>g>Effect</str<strong>on</strong>g>s <str<strong>on</strong>g>of</str<strong>on</strong>g> hypoxia<br />
and shock <strong>on</strong> transcutaneous PO 2 values <strong>in</strong> dogs. Crit Care<br />
Med 1979; 7: 526–531.<br />
9 Tremper KK, Shoemaker WC, Shippy CR, Nolan LS.<br />
Transcutaneous PCO 2 m<strong>on</strong>itor<strong>in</strong>g <strong>on</strong> adult <strong>patients</strong> <strong>in</strong> the ICU<br />
and the operat<strong>in</strong>g room. Crit Care Med 1981; 9: 752–755.<br />
10 Waxman K, Sadler R, Eisner ME, Applebaum R, Tremper KK,<br />
Mas<strong>on</strong> GR. Transcutaneous oxygen m<strong>on</strong>itor<strong>in</strong>g <str<strong>on</strong>g>of</str<strong>on</strong>g> emergency<br />
department <strong>patients</strong>. Am J Surg 1983; 146: 35–38.<br />
11 Tatevossian RG, Wo CC, Velmahos GC, Demetriades D,<br />
Shoemaker WC. Transcutaneous oxygen and CO2 as <str<strong>on</strong>g>early</str<strong>on</strong>g><br />
warn<strong>in</strong>g <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>tissue</strong> hypoxia and hemodynamic shock <strong>in</strong> critically<br />
ill emergency <strong>patients</strong>. Crit Care Med 2000; 28: 2248–2253.<br />
12 Society <str<strong>on</strong>g>of</str<strong>on</strong>g> Critical Care Medic<strong>in</strong>e <str<strong>on</strong>g>of</str<strong>on</strong>g> Ch<strong>in</strong>ese Medical<br />
Associati<strong>on</strong>. Guidel<strong>in</strong>es for hemodynamic m<strong>on</strong>itor<strong>in</strong>g and<br />
support <str<strong>on</strong>g>of</str<strong>on</strong>g> adult <strong>patients</strong> with severe sepsis and septic shock.<br />
Ch<strong>in</strong> J Emerg Med 2007; 16: 121–126.<br />
13 Barbee RW, Reynolds PS, Ward KR. Assess<strong>in</strong>g shock<br />
resuscitati<strong>on</strong> strategies by oxygen debt repayment. Shock 2010;<br />
33: 113–122.<br />
14 Harrois A, Huet O, Duranteau J. Alterati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> mitoch<strong>on</strong>drial<br />
functi<strong>on</strong> <strong>in</strong> sepsis and critical illness. Curr Op<strong>in</strong> Anaesthesiol<br />
2009; 22: 143–149.<br />
15 Yu M, Morita SY, Daniel SR, Chapital A, Waxman K, Sever<strong>in</strong>o<br />
R. Transcutaneous pressure <str<strong>on</strong>g>of</str<strong>on</strong>g> oxygen: a n<strong>on</strong><strong>in</strong>vasive and <str<strong>on</strong>g>early</str<strong>on</strong>g><br />
detector <str<strong>on</strong>g>of</str<strong>on</strong>g> peripheral shock and outcome. Shock 2006; 26:<br />
450–456.<br />
16 Yu M, Chapital A, Ho HC, Wang J, Takanishi D Jr. A<br />
prospective randomized trial compar<strong>in</strong>g oxygen delivery versus<br />
transcutaneous pressure <str<strong>on</strong>g>of</str<strong>on</strong>g> oxygen values as resuscitative <str<strong>on</strong>g>goal</str<strong>on</strong>g>s.<br />
Shock 2007; 27: 615–622.<br />
17 Le<strong>on</strong>e M, Blidi S, Ant<strong>on</strong><strong>in</strong>i F, Meyssignac B, Bord<strong>on</strong> S, Garc<strong>in</strong><br />
F, et al. Oxygen <strong>tissue</strong> saturati<strong>on</strong> is lower <strong>in</strong> n<strong>on</strong>survivors<br />
than <strong>in</strong> survivors after <str<strong>on</strong>g>early</str<strong>on</strong>g> resuscitati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> septic shock.<br />
Anesthesiology 2009; 111: 366–371.<br />
Received December 10, 2012<br />
Accepted after revisi<strong>on</strong> April 16, 2013<br />
www.wjem.org