Protocol for infection surveillance - Hampshire Hospitals NHS ...
Protocol for infection surveillance - Hampshire Hospitals NHS ...
Protocol for infection surveillance - Hampshire Hospitals NHS ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
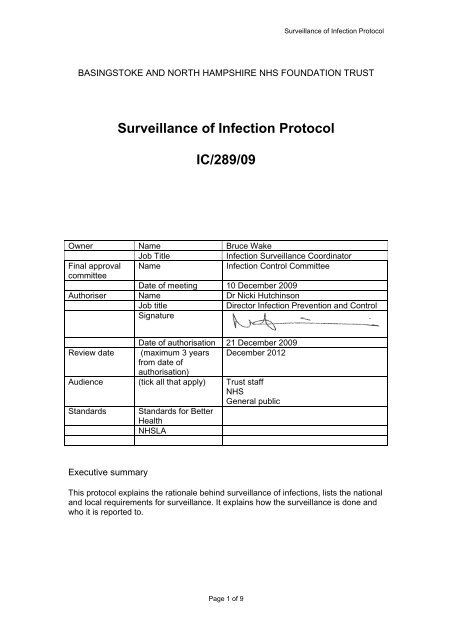
Surveillance of Infection <strong>Protocol</strong><br />
BASINGSTOKE AND NORTH HAMPSHIRE <strong>NHS</strong> FOUNDATION TRUST<br />
Surveillance of Infection <strong>Protocol</strong><br />
IC/289/09<br />
Owner Name Bruce Wake<br />
Job Title<br />
Infection Surveillance Coordinator<br />
Final approval Name<br />
Infection Control Committee<br />
committee<br />
Date of meeting 10 December 2009<br />
Authoriser Name Dr Nicki Hutchinson<br />
Job title<br />
Director Infection Prevention and Control<br />
Signature<br />
Date of authorisation 21 December 2009<br />
Review date (maximum 3 years December 2012<br />
from date of<br />
authorisation)<br />
Audience (tick all that apply) Trust staff<br />
<strong>NHS</strong><br />
General public<br />
Standards Standards <strong>for</strong> Better<br />
Health<br />
<strong>NHS</strong>LA<br />
Executive summary<br />
This protocol explains the rationale behind <strong>surveillance</strong> of <strong>infection</strong>s, lists the national<br />
and local requirements <strong>for</strong> <strong>surveillance</strong>. It explains how the <strong>surveillance</strong> is done and<br />
who it is reported to.<br />
Page 1 of 9
Surveillance of Infection <strong>Protocol</strong><br />
CONTENTS<br />
Page<br />
1.0 Introduction 3<br />
2.0 Surgical Site Infection Surveillance 3<br />
2.1 Background 3<br />
2.2 Aims 3<br />
2.3 SSIS targets 3<br />
3.0 SSIS Coordinator Responsibilities 4<br />
3.1 Data collection 4<br />
3.2 Submission of data 4<br />
3.3 Reconciliation of submitted data 4<br />
3.4 Data sharing 5<br />
4.0 Staphylococcus aureus Surveillance and Reporting 5<br />
4.1 Background 5<br />
4.2 Coordinator Responsibilities 5<br />
4.3 Data collection 5<br />
4.4 Submission of data 6<br />
4.5 Reconciliation of submitted data 6<br />
4.6 Recording data locally 6<br />
5.0 Clostridium difficile Reporting 6<br />
5.1 Coordinator Responsibilities 6<br />
5.2 Data collection 6<br />
5.3 Submission of data 6<br />
5.4 Reconciliation of submitted data 7<br />
5.5 Recording data locally 7<br />
6.0 All Significant Bacteraemia 7<br />
6.1 Coordinator responsibilities 7<br />
6.2 Recording data locally 7<br />
7.0 Norovirus outbreaks 8<br />
8.0 Enhanced Influenza A H1N1 Surveillance 8<br />
9.0 Enhanced Invasive Group A Streptococcus Surveillance 8<br />
9.1 Data sharing 8<br />
10.0 Alert Organisms 8<br />
10.1 Coordinator responsibilities 9<br />
10.2 Data sharing 9<br />
11.0 Miscellaneous 9<br />
Page 2 of 9
Surveillance of Infection <strong>Protocol</strong><br />
1.0 Introduction<br />
Infections acquired in hospital are recognised to be associated with significant<br />
morbidity. They result in extended length of hospital stay, pain, discom<strong>for</strong>t and<br />
sometimes prolonged or permanent disability.<br />
In “Getting ahead of the Curve”- a strategy <strong>for</strong> infectious diseases (Department of<br />
Health, DOH 2003), the prevention of HCAI was highlighted as a priority <strong>for</strong> action by<br />
the Chief Medical Officer. An important component of the strategy <strong>for</strong> action included<br />
<strong>surveillance</strong>. This data is fedback nationally to the HPA and locally to the SHA and<br />
PCT as required within contract schedules. Within BNHFT <strong>surveillance</strong> data is<br />
shared with the Board of Directors, the executive committee and the divisional<br />
boards. At present <strong>surveillance</strong> is undertaken <strong>for</strong> the following <strong>infection</strong>s:<br />
Surgical site <strong>infection</strong>s<br />
Staphylococcus aureus bacteraemias including MRSA<br />
C difficile<br />
Significant hospital acquired bacteraemias especially IV line related <strong>infection</strong>s<br />
Invasive group A streptococcal <strong>infection</strong>s<br />
Norovirus outbreaks<br />
Swine flu (H1N1)<br />
2.0 Surgical Site Infection Surveillance<br />
2.1 Background<br />
Surgical site <strong>infection</strong>s (SSI) account <strong>for</strong> approximately 10% of all Health care<br />
acquired <strong>infection</strong>s (HCAI) and is estimated to double the cost of patient care<br />
resulting in an additional average 6.5 days of hospital stay. (Health Protection<br />
Agency) HPA.<br />
The (DOH) steering group on HCAI recommended that Surgical Site Infection<br />
Surveillance (SSIS) in Orthopaedic surgery, become mandatory from April 2004 in all<br />
English Trusts, along with voluntary areas of SSIS, which include general,<br />
gynaecology, vascular, and cardiac surgery.<br />
2.2 Aims<br />
One of the key aims of this <strong>surveillance</strong> service is to enable participating hospitals to<br />
compare their rates of SSI in a specific group of surgical procedures against a<br />
benchmark (the pooled mean rate of other participating hospitals). For this<br />
comparison to be valid the data collection methods used by participating hospitals<br />
must be similar. This requires active <strong>surveillance</strong> where designated, trained<br />
personnel use a variety of methods to identify cases of <strong>infection</strong> (HPA). Research<br />
has shown that well organised <strong>surveillance</strong> and <strong>infection</strong> control programmes that<br />
include feedback of <strong>infection</strong> rates to surgeons were associated with significant<br />
reduction in SSI.<br />
2.3 SSIS targets<br />
• Surgical procedures commonly per<strong>for</strong>med or associated with high risk of<br />
<strong>infection</strong>.<br />
• Surgery that requires at least three days post-operative hospital stay and<br />
where maximum benefit from <strong>surveillance</strong> is likely to be obtained. It excludes<br />
endoscopy, diagnostic procedures and wounds not closed in theatre (HPA).<br />
Page 3 of 9
Surveillance of Infection <strong>Protocol</strong><br />
Note:<br />
• If an implant has not been inserted, SSIS should be stopped on the 30 th day<br />
after the operation (as <strong>infection</strong> after this time would not meet the definition of<br />
SSI).<br />
• If an implant has been inserted SSIS should continue <strong>for</strong> 1 year after the<br />
operation (as an <strong>infection</strong> may meet SSI definition). Any patients readmitted with<br />
joint <strong>infection</strong> will be monitored by the coordinator.<br />
3.0 The SSI Coordinator Responsibilities<br />
• Collecting data from (medical & nursing notes / clinical personnel / positive<br />
microbiology cultures).<br />
• Analysing data<br />
• Forwarding data to the HPA via a web link<br />
• Acting as a point of contact to receive data from the HPA( quarterly reports)<br />
• Sharing data results<br />
Note: SSIS can be undertaken at local level if deemed necessary<br />
3.1 Data collection<br />
• Review operating theatre lists to identify patients <strong>for</strong> specific chosen category.<br />
• Visit patient from first post- operative day until discharge (three occasions<br />
advised by Health Protection Agency) HPA.<br />
• Use assigned data collection <strong>for</strong>m provided by the HPA.<br />
• Make the patient aware of the relevance of SSIS / confidentiality of<br />
in<strong>for</strong>mation / dissemination of results.<br />
• All patients to receive a booklet on “Monitoring surgical wounds <strong>for</strong> <strong>infection</strong>”(<br />
HPA) Coordinator contact details are on the back of booklet.<br />
• Verbal consent is taken from the patient, to receive a follow up telephone call<br />
between four and six weeks post discharge, regarding wound status.<br />
Alternatively a post discharge questionnaire can be given to the patient to be<br />
completed at 30 day post discharge and returned to the Infection Surveillance<br />
Coordinator. This post discharge <strong>surveillance</strong> is a mandatory requirement by<br />
the SSIS database.<br />
• Liase with microbiology, regarding wound swab results to confirm SSI.<br />
• Collect relevant data via Sapphire computer system :- (ASA score, duration of<br />
operation, grade of surgeon).<br />
• Identify, and monitor patients readmitted with SSI and in<strong>for</strong>m HPA.<br />
• Liase with planning department to confirm admission / discharge list to ensure<br />
that no patients have been overlooked in specific category.<br />
• Check discharge operation code via PMS system.<br />
3.2 Submission of data<br />
• Data is submitted via a password protected electronic weblink to the HPA.<br />
• Each record entered is given a serial number and this is used between the<br />
Trust and the HPA <strong>for</strong> any further correspondence regarding the patient.<br />
• Coordinator keeps own database <strong>for</strong> reference.<br />
3.3 Reconciliation of submitted data<br />
Approximately 4 weeks after the end of the <strong>surveillance</strong> period each participating<br />
hospital will be asked to confirm the number of <strong>for</strong>ms they have submitted <strong>for</strong> that<br />
period and <strong>for</strong> how many of these SSI has been reported. This allows the<br />
Page 4 of 9
Surveillance of Infection <strong>Protocol</strong><br />
<strong>surveillance</strong> of patients still in hospital at the end of the <strong>surveillance</strong> period to be<br />
completed and ensures that all the data has been received by the coordinating<br />
centre and is included in the individual hospital report.<br />
3.4 Data sharing<br />
Coordinator receives HPA report via e.mail and <strong>for</strong>wards to:<br />
• Surgeons<br />
• Nursing staff (wards / theatres / specialist)<br />
• Managerial staff<br />
• Physiotherapy & Occupational Therapy (orthopedic patients)<br />
• Infection Control Committee<br />
• Trust Board<br />
• Liases with Public Relations department to ensure public awareness of SSIS<br />
results through:<br />
o<br />
o<br />
The Trust website<br />
A Visual display all clinical areas<br />
4.0 Staphylococcus aureus Surveillance and Reporting<br />
4.1 Background<br />
Since October 2005, all MRSA Hospital and Community acquired bacteraemia <strong>for</strong> the<br />
Trust are reported via a web link to the HPA - Mandatory Enhanced Surveillance<br />
Scheme (MESS). This new enhanced reporting system allows the capture of a more<br />
comprehensive data set on MRSA than the quarterly mandatory <strong>surveillance</strong><br />
scheme. The core mandatory MRSA <strong>surveillance</strong> schemes continue to operate<br />
independently of this enhanced scheme.<br />
MESS gives trusts a more accurate picture of their situation and contributes to<br />
building a better evidence base regarding risk factors <strong>for</strong> <strong>infection</strong>s. The enhanced<br />
reporting system:<br />
• Enables reports to be entered in “real time” as they occur.<br />
• Allows Trusts to specify the department or speciality where the patient was<br />
being treated when the <strong>infection</strong> was identified<br />
• Allows calculation of speciality specific MRSA rates.<br />
• Allows <strong>for</strong> seperation of MRSA bacteraemia <strong>infection</strong>s identified within 2 days<br />
of admission from those identified after 2 days.<br />
The DOH aims to have a national reduction of MRSA bacteraemia of 50% by 2008.<br />
From April 2006 the HPA introduced voluntary reporting of MSSA bacteraemia.<br />
Basingstoke and North <strong>Hampshire</strong> Hospital Foundation Trust has utilised this<br />
<strong>surveillance</strong> since its inauguration.<br />
4.2 Coordinator responsibilities include<br />
4.3 Data collection<br />
• Liases daily with the Consultant Microbiologist and the ICNet system, to<br />
identify all MRSA & MSSA positive blood culture episodes (and their source)<br />
detected in BNHFT laboratory, whether clinically significant or not, whether<br />
treated or not, whether acquired in the Trust or elsewhere.<br />
Page 5 of 9
Surveillance of Infection <strong>Protocol</strong><br />
Note:<br />
• Positive blood cultures from the same patient within 14 days of the initial<br />
culture are considered to be part of the original episode and should not be<br />
reported<br />
• Positive blood cultures more than 14 days apart should be reported as these<br />
are considered to be a new episode.<br />
4.4 Submission of data<br />
Data is entered via a password protected web link to the HPA which includes:<br />
• Core Dataset<br />
• Risk Factor page (this is <strong>for</strong> Trust in<strong>for</strong>mation only, to help with root cause<br />
analysis (RCA). It is not in<strong>for</strong>mation <strong>for</strong> publication by the HPA or Department<br />
of Health.<br />
4.5 Reconciliation of submitted data<br />
• Trusts using the website have access to all the data they have entered.<br />
• This can be compared to a regional and national aggregate also available to<br />
Trusts from the website<br />
4.6 Recording data locally<br />
A database has been developed to record in<strong>for</strong>mation regarding MRSA and MSSA<br />
bacteraemia. This database is used to create in<strong>for</strong>mation in spreadsheet <strong>for</strong>mat <strong>for</strong><br />
display on the Trust Reporting Warehouse computer drive. The database is also<br />
used to record results of RCA and as a learning resource.<br />
5.0 Clostridium difficile reporting<br />
Clostridium difficile has been included in the MESS reporting scheme by the HPA<br />
in April 2007. Coordinator enters cases via the website on a daily or weekly basis.<br />
5.1 Coordinator responsibilities include<br />
5.2 Data collection<br />
Note:<br />
• Liaises daily with the Consultant Microbiologist and the ICNet system, to<br />
identify all C.difficile toxin positive episodes (and their source) detected in<br />
BNHFT laboratory, whether clinically significant or not, whether treated or not,<br />
whether acquired in the Trust or elsewhere.<br />
• Positive C.difficile toxin assays from the same patient within 28 days of the<br />
initial positive assay are considered to be part of the original episode and<br />
should not be reported.<br />
• Positive C.difficile toxin assays more than 28 days apart should be reported<br />
as these are considered to be a new episode or recurrence or relapse.<br />
5.3 Submission of data<br />
Data is entered via a password protected web link to the HPA which includes:<br />
Page 6 of 9
Surveillance of Infection <strong>Protocol</strong><br />
• Core Dataset<br />
• Risk Factor page (this is <strong>for</strong> Trust in<strong>for</strong>mation only, to help with root cause<br />
analysis (RCA). It is not in<strong>for</strong>mation <strong>for</strong> publication by the HPA or Department<br />
of Health.<br />
5.4 Reconciliation of submitted data<br />
• Trusts using the website have access to all the data they have entered.<br />
• This can be compared to a regional and national aggregate also available to<br />
Trusts from the website<br />
5.5 Recording data locally<br />
A database has been developed to record in<strong>for</strong>mation regarding C.difficile <strong>infection</strong>.<br />
This database is used to create in<strong>for</strong>mation in spreadsheet <strong>for</strong>mat <strong>for</strong> display on the<br />
Trust Reporting Warehouse computer drive. The database is also used to record<br />
results of RCA and as a learning resource.<br />
6.0 All Significant Bacteraemia<br />
Coordinator collects, analyses, and shares data on all significant bacteraemia in<br />
order:<br />
• To support change as necessary<br />
• Review clinical practice<br />
• Teach and train staff<br />
• Update policies<br />
6.1 Coordinator responsibilities include:<br />
• Liaison with Consultant Microbiologist and ICNet system to identify all<br />
significant bacteraemia.<br />
Compiles monthly figures to reveal:<br />
• Total number of bacteraemia<br />
• Total number of significant hospital and community acquired bacteraemia<br />
• Type and source of hospital and community acquired bacteraemia<br />
• Risk factors related to hospital acquired bacteraemia to identify<br />
contamination rate via:<br />
o Central IV catheter<br />
o Peripheral IV catheter<br />
o Surgical site <strong>infection</strong><br />
o Ventilator associated <strong>infection</strong><br />
o Urinary catheter<br />
• Identify hospital acquired bacteraemia each clinical area<br />
6.2 Recording data locally<br />
A database has been developed to record in<strong>for</strong>mation regarding significant<br />
bacteraemia. This database is used to create in<strong>for</strong>mation in spreadsheet <strong>for</strong>mat <strong>for</strong><br />
display on the Trust Reporting Warehouse computer drive. The database is also<br />
used to record results of RCA and as a learning resource.<br />
Page 7 of 9
Surveillance of Infection <strong>Protocol</strong><br />
7.0 Norovirus outbreaks<br />
Hospital outbreaks of Norovirus are reported to the Health Protection Agency via a<br />
web link. Norovirus outbreaks are also reported through the Trust Incident Reporting<br />
system and recorded as Serious Untoward Incidents. It is there<strong>for</strong>e important to<br />
record the number of patients and staff affected and their location at time of <strong>infection</strong><br />
to facilitate investigation.<br />
The Infection Surveillance Coordinator will:<br />
• Record the number of patients and staff affected and location<br />
• Liaise with hospital managers to determine whether wards are closed.<br />
• Report to the HPA via web link www.hpa-bioin<strong>for</strong>matics.org.uk/NoroOBK<br />
8.0 Enhanced Influenza A H1N1 Surveillance<br />
Enhanced <strong>surveillance</strong> of H1N1 Influenza A (swine Flu) was instigated by the HPA in<br />
August 2009. This programme requires that each Trust report all hospitalised<br />
patients who have contracted H1N1 Flu A.<br />
The Surveillance Coordinator will:<br />
• Liaise with the Laboratory to determine all positive H1N1 patients<br />
• Determine those patients hospitalised<br />
• Report to HPA all Hospitalised patients via web link nww.flusurv.nhs.uk<br />
• Coordinate the gathering of case histories with clinical staff<br />
9.0 Enhanced Invasive Group A Streptococcus Surveillance<br />
Invasive Group A Streptococcus <strong>surveillance</strong> identifies those <strong>infection</strong>s from usually<br />
sterile sites and where the <strong>infection</strong> causes a major disease state.<br />
• Reports are generated on an electronic spreadsheet and can be emailed to<br />
the HPU, <strong>Hampshire</strong> and Isle of Wight Office.<br />
• Surveillance is only required when instigated by the Health Protection<br />
Agency. The HPA will decide upon a start date and finish date.<br />
9.1 Data sharing<br />
• The Infection Control Committee Meeting<br />
• The Trust Governance Board<br />
• The three Divisional Boards<br />
• The Executive Committee.<br />
• Visual display of MRSA & MSSA bacteraemia results throughout the Trust, <strong>for</strong><br />
patient and public awareness.<br />
• Trust Reporting Warehouse computer drive<br />
10.0 Alert Organisms<br />
Alert organisms are those that may have a significant impact on the management of<br />
the hospital and identify potential problems with <strong>infection</strong> prevention and control. The<br />
organisms included are:<br />
• MRSA as colonisation and as <strong>infection</strong>, whether community or hospital<br />
acquired.<br />
Page 8 of 9
• C. difficile as recorded on the Trust Surveillance database.<br />
• All Staph aureus <strong>infection</strong>s<br />
• Group A Streptococcus <strong>infection</strong>s<br />
• Group B Streptococcus <strong>infection</strong>s and colonisation<br />
• Group C Streptococcus <strong>infection</strong><br />
• Extended Spectrum Beta-Lactamase producers (ESBL)<br />
• Enteric pathogens<br />
10.1 Coordinator responsibilities include:<br />
Surveillance of Infection <strong>Protocol</strong><br />
Ensuring data link to Microbiology data system <strong>for</strong> updated in<strong>for</strong>mation on a monthly<br />
basis. Interpretation of data from microbiology to spreadsheet and other <strong>for</strong>mats<br />
10.2 Data sharing<br />
• The Infection Control Committee Meeting<br />
• The Trust Governance Board<br />
• The three Divisional Boards<br />
• The Clinical Governance Board.<br />
• Trust Reporting Warehouse computer drive<br />
11.0 Miscellaneous<br />
The Infection Surveillance Coordinator will assist where necessary with in<strong>for</strong>mation<br />
relating to <strong>infection</strong> prevalence, <strong>for</strong> the purposes of satisfying requests relating to<br />
Freedom of In<strong>for</strong>mation and Patient Advice and Liaison.<br />
The coordinator will assist the Infection Control Team with the development of gantt<br />
charts, databases and spreadsheets to aid documenting outbreaks<br />
Page 9 of 9