healthcare operations utilization protocols 2007 - Health Plan of ...
healthcare operations utilization protocols 2007 - Health Plan of ...
healthcare operations utilization protocols 2007 - Health Plan of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
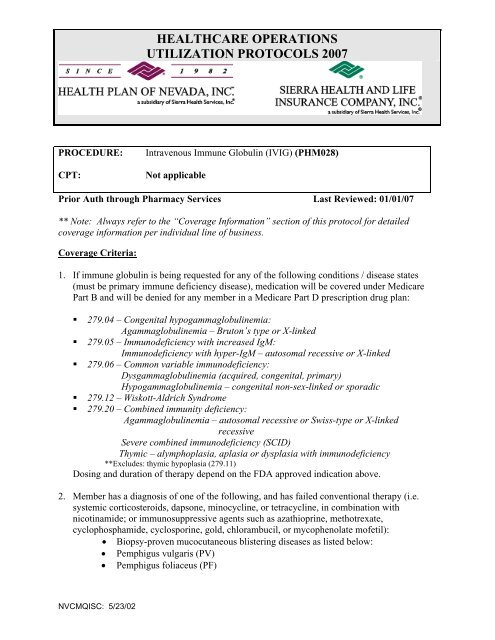
HEALTHCARE OPERATIONS<br />
UTILIZATION PROTOCOLS <strong>2007</strong><br />
PROCEDURE:<br />
CPT:<br />
Intravenous Immune Globulin (IVIG) (PHM028)<br />
Not applicable<br />
Prior Auth through Pharmacy Services Last Reviewed: 01/01/07<br />
** Note: Always refer to the “Coverage Information” section <strong>of</strong> this protocol for detailed<br />
coverage information per individual line <strong>of</strong> business.<br />
Coverage Criteria:<br />
1. If immune globulin is being requested for any <strong>of</strong> the following conditions / disease states<br />
(must be primary immune deficiency disease), medication will be covered under Medicare<br />
Part B and will be denied for any member in a Medicare Part D prescription drug plan:<br />
• 279.04 – Congenital hypogammaglobulinemia:<br />
Agammaglobulinemia – Bruton’s type or X-linked<br />
• 279.05 – Immunodeficiency with increased IgM:<br />
Immunodeficiency with hyper-IgM – autosomal recessive or X-linked<br />
• 279.06 – Common variable immunodeficiency:<br />
Dysgammaglobulinemia (acquired, congenital, primary)<br />
Hypogammaglobulinemia – congenital non-sex-linked or sporadic<br />
• 279.12 – Wiskott-Aldrich Syndrome<br />
• 279.20 – Combined immunity deficiency:<br />
Agammaglobulinemia – autosomal recessive or Swiss-type or X-linked<br />
recessive<br />
Severe combined immunodeficiency (SCID)<br />
Thymic – alymphoplasia, aplasia or dysplasia with immunodeficiency<br />
**Excludes: thymic hypoplasia (279.11)<br />
Dosing and duration <strong>of</strong> therapy depend on the FDA approved indication above.<br />
2. Member has a diagnosis <strong>of</strong> one <strong>of</strong> the following, and has failed conventional therapy (i.e.<br />
systemic corticosteroids, dapsone, minocycline, or tetracycline, in combination with<br />
nicotinamide; or immunosuppressive agents such as azathioprine, methotrexate,<br />
cyclophosphamide, cyclosporine, gold, chlorambucil, or mycophenolate m<strong>of</strong>etil):<br />
• Biopsy-proven mucocutaneous blistering diseases as listed below:<br />
• Pemphigus vulgaris (PV)<br />
• Pemphigus foliaceus (PF)<br />
NVCMQISC: 5/23/02
HEALTHCARE OPERATIONS<br />
UTILIZATION PROTOCOLS <strong>2007</strong><br />
• Bullous pemphigoid (BP)<br />
• Mucous membrane pemphigoid (MMP)(a.k.a., cicatricial pemphigoid)<br />
• Epidermolysis bullosa acquista (EBA)<br />
‣ ACTION: Will approve for 6 months<br />
3. ** NOTE: May be approved in patients with rapidly progressive disease in whom a clinical<br />
response could not be affected quickly enough using conventional agents. In such situations,<br />
IVIg therapy should be given along with conventional treatment(s) and the IVIg would be<br />
used only until conventional therapy could take effect.<br />
4. Patient has a diagnosis <strong>of</strong> CIDP (Chronic Idiopathic Demyelinating<br />
5. Approval for other, <strong>of</strong>f-label indications will be considered on a case-by-case basis with<br />
clinical information submitted.<br />
6. For Approval for other, <strong>of</strong>f-label indications will be considered on a case-by-case basis with<br />
clinical information submitted.<br />
7. Per Medicare coverage guidance, may be approved for other indications in Medicare<br />
members if it is supported in the recognized compendia.<br />
8. If the above criteria are not met, the request will be denied.<br />
Coverage Information – IVIG<br />
Senior Dimensions MA-PD plans – covered under the Medicare Part B benefit only if<br />
medication is being used for one <strong>of</strong> the diagnoses listed in #1 above; applicable 20% coinsurance<br />
will apply and will NOT apply to TrOOP. Covered under Medicare Part D<br />
benefit for all other diagnoses with the applicable specialty drug co-insurance and WILL<br />
apply to TrOOP. All claims will adjudicate through the pharmacy on-line claims system.<br />
Sierra RX – covered under the Medicare Part B benefit only if medication is being used for<br />
one <strong>of</strong> the diagnoses listed in #1 above; direct member to their Part B carrier. Covered<br />
under Medicare Part D benefit for all other diagnoses with the applicable specialty drug coinsurance;<br />
will adjudicate through the pharmacy online claims system and WILL apply to<br />
-2-<br />
This guideline is to be used in the decision-making process and does not represent standards <strong>of</strong> care <strong>of</strong> an individual<br />
patient. The use <strong>of</strong> this guideline should not substitute for the pr<strong>of</strong>essional judgment <strong>of</strong> a provider which takes into<br />
account the unique problems and circumstances <strong>of</strong> the individual patient. They are proprietary documents and may<br />
not be copied or distributed without express permission.
HEALTHCARE OPERATIONS<br />
UTILIZATION PROTOCOLS <strong>2007</strong><br />
TrOOP.<br />
Sierra Spectrum/Sierra Nevada Spectrum covered under the Medicare Part B benefit<br />
only if medication is being used for one <strong>of</strong> the diagnoses listed in #1 above; applicable 20%<br />
co-insurance will apply. Claims WILL adjudicate on-line and will NOT apply to TrOOP.<br />
Covered under Medicare Part D benefit for all other diagnoses with the applicable specialty<br />
drug co-insurance; will adjudicate through the pharmacy online claims system and WILL<br />
apply to TrOOP.<br />
All other lines <strong>of</strong> business: Covered as a Medical Benefit – prior authorization required<br />
General Information<br />
Intravenous immunoglobulin (IVIG) is used as replacement therapy in patients with a primary<br />
humoral immune deficiency. IVIG products are also commonly used for <strong>of</strong>f-label purposes. It<br />
is estimated that 50% to 70% <strong>of</strong> all IVIG prescriptions are written for <strong>of</strong>f-label purposes.<br />
However, information on many <strong>of</strong> the <strong>of</strong>f-label uses in the medical literature is from<br />
inadequately uncontrolled studies and case reports.<br />
FDA Approved Indications<br />
1. Immunodeficiency syndrome: For the maintenance treatment <strong>of</strong> patients who are unable to<br />
produce sufficient amounts <strong>of</strong> IgG antibodies. It may be used in disease states such as<br />
congenital agammaglobulinemia, common variable hypogammaglobulinemia, x-linked<br />
immunodeficiency with or without hyper IgM, Wiskott-Aldrich syndrome and combined<br />
immunodeficiency<br />
2. Idiopathic thrombocytopenia purpura (ITP) (Gamimune N, Gammagard S/D, Polygam S/D,<br />
Sandoglobulin, Venoglobulin-S only): Treatment should not be considered curative.<br />
Administer to patients who require a rapid, temporary rise in platelet count (e.g., prior to<br />
surgery, to control excessive bleeding or to defer splenectomy)<br />
3. B-cell chronic lymphocytic leukemia (CLL) (Gammagard S/D, Polygam S/D): For the<br />
prevention <strong>of</strong> bacterial infections in patients with hypogammaglobulinemia or recurrent<br />
bacterial infections associated with B-cell CLL.<br />
4. Kawasaki syndrome (Iveegam only)<br />
5. Bone marrow transplantation (BMT) (Gamimune N only): For the prevention <strong>of</strong> systemic<br />
and local infections, interstitial pneumonia <strong>of</strong> infectious and idiopathic etiologies and acute<br />
graft-vs-host disease in patients<br />
6. Pediatric HIV infection (Gamimune N only)<br />
-3-<br />
This guideline is to be used in the decision-making process and does not represent standards <strong>of</strong> care <strong>of</strong> an individual<br />
patient. The use <strong>of</strong> this guideline should not substitute for the pr<strong>of</strong>essional judgment <strong>of</strong> a provider which takes into<br />
account the unique problems and circumstances <strong>of</strong> the individual patient. They are proprietary documents and may<br />
not be copied or distributed without express permission.
HEALTHCARE OPERATIONS<br />
UTILIZATION PROTOCOLS <strong>2007</strong><br />
Unlabeled uses: IGIVs may also be useful in chronic fatigue syndrome; quinidine-induced<br />
thrombocytopenia; chronic inflammatory demyelinating polyneuropathy; Guillain-Barre<br />
syndrome<br />
Dosing Recommendations<br />
1. Immunodeficiency syndrome<br />
a. Sandoglobulin: Administer 100–400 mg/kg/month by infusion. Increase to 300mg/kg if<br />
IgG serum level is 100mg/kg are<br />
recommended.<br />
c. Gammar-P IV: Administer 200 to 400mg/kg every 3 to 4 weeks in adults.<br />
d. Gamimune N: Administer 100 to 200mg/kg/month. The dosage may be given more<br />
frequently or increased as high as 400 mg/kg (8 mL/kg) if the clinical response is<br />
inadequate or the level <strong>of</strong> IgG is insufficient<br />
e. Iveegam: 200mg/kg/month. Doses <strong>of</strong> 800 mg/kg/month have been tolerated<br />
f. Polygam S/D: 100mg/kg/month. An initial dose <strong>of</strong> 200 to 400 mg/kg may be<br />
administered to individualize treatment.<br />
g. Venoglobulin-S: 200mg/kg/month<br />
-4-<br />
This guideline is to be used in the decision-making process and does not represent standards <strong>of</strong> care <strong>of</strong> an individual<br />
patient. The use <strong>of</strong> this guideline should not substitute for the pr<strong>of</strong>essional judgment <strong>of</strong> a provider which takes into<br />
account the unique problems and circumstances <strong>of</strong> the individual patient. They are proprietary documents and may<br />
not be copied or distributed without express permission.
HEALTHCARE OPERATIONS<br />
UTILIZATION PROTOCOLS <strong>2007</strong><br />
2. ITP<br />
a. Sandoglobulin: 400mg/kg for 2 to 5 consecutive days<br />
b. Venoglobulin-S: 2000mg/kg over < 5 days for induction therapy. Maintenance therapy:<br />
1000 mg/kg may be administered as needed to maintain platelet counts <strong>of</strong> 30,000/mm 3 in<br />
children and 20,000/mm 3 in adults or to prevent bleeding episodes in the interval<br />
between infusions.<br />
c. Gamimune N: 400mg/kg may be given as a single infusion. If an adequate response<br />
does not result, the dose can be increased to 800 to 1000mg/kg given as a single infusion.<br />
Maintenance: If platelet count falls to < 30,000/mm 3 or if the patient manifests clinically<br />
significant bleeding, 400mg/kg may be given as a single infusion. If an adequate<br />
response does not result, the dose can be increased to 800 to 1000mg/kg given as a single<br />
infusion. Maintenance infusions may be administered intermittently as clinically<br />
indicated to maintain a platelet count > 30,000/mm 3 .<br />
d. Gammagard S/D: 1000mg/kg. Need for additional doses can be determined by clinical<br />
response and platelet count. Give up to 3 doses on alternate days if required.<br />
e. Polygam S/D: 1g/kg. A need for additional doses can be determined by clinical<br />
response and platelet count. Give up to three separate doses on alternate days, if required<br />
3. CLL<br />
a. Gammagard S/D: 1000mg/kg<br />
b. Polygam S.D: 1g/kg<br />
4. Kawasaki syndrome – Iveegam only: 400mg/kg/day for 4 consecutive days or a single dose<br />
<strong>of</strong> 2000mg/kg given over a 10-hour period. Initiate treatment within 10 days <strong>of</strong> onset <strong>of</strong> the<br />
disease. Treatment regimen should include aspirin, 100mg/kg each day through the 14 th day<br />
<strong>of</strong> illness, then 3 to 5mg/kg/day thereafter for 5 weeks.<br />
5. Bone Marrow Transplantation - Gamimune N only: 500mg/kg (10ml/kg) beginning on days<br />
7 and 2 pre-transplant or at the time conditioning therapy for transplantation is begun, then<br />
weekly through the 90-day post-transplant period.<br />
6. Pediatric HIV infection - Gamimune N only: 400mg/kg (8ml/kg) every 28 days.<br />
Bibliography<br />
1. NIH Consensus Development Conference. Intravenous Immunoglobulin Prevention and<br />
Treatment <strong>of</strong> Disease. JAMA; December 26, 1990-Vol 264. No.24; 3189-3193<br />
2. Knapp MJ, et al. Drug Reviews: Clinical uses <strong>of</strong> intravenous immune globulin. Clinical<br />
Pharmacy; Vol 9 Jul 1990:509-529<br />
3. Consensus Statement. Recommendations for Off-Label Use <strong>of</strong> Intravenously<br />
Administered Immunoglobulin Preparations. JAMA, June 21, 1995-Vol 273. No.23;<br />
-5-<br />
This guideline is to be used in the decision-making process and does not represent standards <strong>of</strong> care <strong>of</strong> an individual<br />
patient. The use <strong>of</strong> this guideline should not substitute for the pr<strong>of</strong>essional judgment <strong>of</strong> a provider which takes into<br />
account the unique problems and circumstances <strong>of</strong> the individual patient. They are proprietary documents and may<br />
not be copied or distributed without express permission.
HEALTHCARE OPERATIONS<br />
UTILIZATION PROTOCOLS <strong>2007</strong><br />
1865-1870<br />
4. UHC Updates Off-Label Use Recommendations for Intravenous Immunoglobulin.<br />
Clinical Practice Alert, February/March 1999-Volume 8, Number 2; 1-2.<br />
5. Immune Globulin Intravenous (IVIG), Facts and Comparisons, Inc., St. Louis, MO,<br />
2004.<br />
6. Micromedex <strong>Health</strong>Care Series, Drugdex® 2005<br />
-6-<br />
This guideline is to be used in the decision-making process and does not represent standards <strong>of</strong> care <strong>of</strong> an individual<br />
patient. The use <strong>of</strong> this guideline should not substitute for the pr<strong>of</strong>essional judgment <strong>of</strong> a provider which takes into<br />
account the unique problems and circumstances <strong>of</strong> the individual patient. They are proprietary documents and may<br />
not be copied or distributed without express permission.