QOF Plus Year 1 - Detailed Summary - Imperial College London
QOF Plus Year 1 - Detailed Summary - Imperial College London
QOF Plus Year 1 - Detailed Summary - Imperial College London
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Quality and Outcomes<br />
Framework <strong>Plus</strong><br />
Towards world class healthcare for all
The <strong>QOF</strong>+ approach<br />
<strong>QOF</strong>+ is a major quality improvement initiative for primary care in Hammersmith & Fulham,<br />
developed jointly by NHS Hammersmith and Fulham and <strong>Imperial</strong> <strong>College</strong> <strong>London</strong>. The PCT has<br />
earmarked £2 million annual funding to implement the comprehensive initiative over the next 3<br />
years with the aim of achieving a step-change in quality and to address local priorities.<br />
Building on the success of the pay-for-performance model introduced through the national<br />
Quality and Outcomes Framework (<strong>QOF</strong>), practices will be rewarded with <strong>QOF</strong>+ points for<br />
achievement of higher thresholds for a selected number of existing national <strong>QOF</strong> indicators.<br />
These indicators were chosen as attainment would result in significant health benefits and are<br />
areas where Hammersmith and Fulham are currently underperforming:<br />
Asthma<br />
Hypertension<br />
CHD<br />
Cervical screening<br />
Diabetes<br />
Mental health<br />
Stroke<br />
Additionally, practices will be rewarded for achievement of new <strong>QOF</strong>+ indicators which have<br />
been developed in clinical and non-clinical domains covering the following areas:<br />
CVD primary prevention<br />
Alcohol<br />
Smoking<br />
Smoking in pregnancy<br />
Breastfeeding<br />
Screening for tuberculosis<br />
Ethnicity<br />
Records<br />
Patient experience<br />
Patient safety<br />
Patient information<br />
Why have a local <strong>QOF</strong>?<br />
It is anticipated that introduction of a local <strong>QOF</strong> would confer a number of advantages, including<br />
more robust performance reporting, mainstreaming quality through templates and coverage of a<br />
greater number of areas.<br />
Development and implementation of a local <strong>QOF</strong> may also contribute to PCTs fulfilling their<br />
functions as world class commissioners, investing locally to achieve the greatest health gains.<br />
The concept of developing a national <strong>QOF</strong> has recently received backing from the National Audit<br />
Office and the NHS Next Stage Review.<br />
1
Why run a separate scheme?<br />
Early data suggest that the introduction of the national <strong>QOF</strong> has resulted in a moderate<br />
improvement in patient care outcomes for some conditions. Local Enhanced Services (LES)<br />
already provide scope for local development within the General Medicine Services (GMS)<br />
contract to tackle local priorities and reduce health inequalities.<br />
Despite this, there are some key limitations to both national <strong>QOF</strong> and LES, and <strong>QOF</strong>+ may<br />
contribute to addressing these:<br />
1 Insufficient focus on health outcomes:<br />
The <strong>QOF</strong>+ advantage:<br />
The current national <strong>QOF</strong> thresholds have arguably been set too low and once the<br />
threshold is achieved, there are no further incentives to tackle the most challenging groups<br />
of patients, increasing the chance of widening<br />
health inequalities. Increased upper<br />
thresholds for selected existing national <strong>QOF</strong> indicators encourages practices to reach<br />
more challenging patient groups, with the aim of decreasing health inequalities, and<br />
achieving significant health benefits.<br />
2 Insufficient focus on primary prevention<br />
The <strong>QOF</strong>+ advantage:<br />
New clinical indicators developed as part of <strong>QOF</strong>+ have been designed specifically to focus<br />
on primary prevention.<br />
3 Nationally set targets don’t always reflect the local needs of patients<br />
The <strong>QOF</strong>+ advantage:<br />
With <strong>QOF</strong>+, new clinical and non-clinical indicators have been developed in response to<br />
analysis of local health needs in Hammersmith and Fulham.<br />
4 LES are often complex and uptake and monitoring can be problematic<br />
The <strong>QOF</strong>+ advantage:<br />
Evaluations of recently introduced LES and local Shared Care schemes (including CVD<br />
Primary Prevention, Smoking Cessation and Alcohol) in Hammersmith and Fulham<br />
highlighted a number of problems with these schemes, in terms of their complexity and<br />
design and the level of uptake by practices. These highlight a need for widespread<br />
implementation in a way that is easily understood.<br />
<strong>QOF</strong>+ provides a more robust<br />
performance reporting using templates for data entry combined with a training and<br />
support package for practices.<br />
2
How <strong>QOF</strong>+ works...<br />
Payment<br />
<strong>QOF</strong>+ has adopted the same approach to payment as the national <strong>QOF</strong> scheme, using the same<br />
value for a <strong>QOF</strong>+ point (1 point = £124.60). Like <strong>QOF</strong>, <strong>QOF</strong>+ includes a combination of all-ornothing<br />
and payment stage indicators, re-uses the concept of exception reporting and<br />
determines remuneration using a system of population and prevalence-weighted point<br />
allocation.<br />
Training & Support<br />
A <strong>QOF</strong>+ Training and Support package has been developed to support implementation of <strong>QOF</strong>+.<br />
The package encompasses a whole range of learning styles and preferences. Features include:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<strong>QOF</strong>+ Resource Pack for new indicator areas<br />
In-house practice training<br />
Educational meetings<br />
Individual practice training budgets<br />
IT support<br />
<strong>QOF</strong>+ email support service<br />
Provision of monthly feedback of performance to practices<br />
Administration<br />
Practices will receive regular feedback on attainment for new indicators, together with IT tools to<br />
help with data entry and manage patient groups at a practice level. This enables practices to see<br />
who is on the new disease registers and identify those who still need treating.<br />
Monitoring & Evaluation<br />
A programme of multimodal evaluation, currently under development, aims to assist monitoring<br />
of the scheme and to support the PCT in its efforts to better understand health inequalities within<br />
Hammersmith and Fulham. It is hoped that this evaluation will assist in the identification and<br />
design of future indicator areas.<br />
Anonymised medical records of all registered patients will be stored centrally by the PCT through<br />
the use of the APOLLO IT system by practices. This will enable analysis of performance, improved<br />
practice profiling, equity assessment using patient-level data, and provision of monthly feedback<br />
of performance to practices, as part of the wider training and support package which has been<br />
developed to support <strong>QOF</strong>+. This will be a rich source of decision support data for the PCT.<br />
3
How <strong>QOF</strong>+ has been developed...<br />
Engagement with local practices and other local provider services, feedback from patients and<br />
discussions with national and international experts in health care quality improvement provided<br />
insights which informed the development of the scheme.<br />
Extension of existing clinical <strong>QOF</strong> targets<br />
A number of existing <strong>QOF</strong> indicators were identified as candidates that might benefit from<br />
additional incentivisation through the provision of revised upper targets. Indicator selection was<br />
weighted towards those whose attainment confers significant potential health benefits at a<br />
population level and where current attainment in Hammersmith and Fulham is below that seen<br />
nationally.<br />
Design and development of the new indicators for <strong>QOF</strong>+<br />
Potential sources for new indicator areas were identified and prioritised on the basis of being<br />
both local and national priorities. These were subjected to a consultation with local stakeholders<br />
to select areas for indicator development for the first year of the scheme. The clinical areas<br />
selected were identified as priorities on the basis of being included in both the Hammersmith and<br />
Fulham PCT Annual Public Health Report and in the Key Performance Indicators from the<br />
Healthcare Commission. Indicators are likely to change for subsequent years of <strong>QOF</strong>+ in line with<br />
latest best evidence and potential changes to national <strong>QOF</strong> indicators.<br />
Literature reviews of the evidence base were undertaken for each selected indicator area to<br />
inform development of indicators.<br />
Proposed new indicators were assessed using the OECD criteria of importance, scientific<br />
soundness and feasibility. Each indicator was also assessed for clarity. This assessment was<br />
informed by the views of local practices, a local stakeholder panel (through a structured<br />
consultation with the aim of achieving consensus for the clinical and records domains), local<br />
provider services and national and international experts in the proposed indicator areas.<br />
The PCT Health Informatics Team was consulted to ensure that proposed indicators would work<br />
within primary care IT systems, and practice templates for new indicator areas were designed for<br />
use within EMIS and VISION systems<br />
Training & Support<br />
The development of a training and support package to support <strong>QOF</strong>+ was informed by<br />
consultation with local and national experts, analysis of data on achievement for existing <strong>QOF</strong> for<br />
individual practices, and a training and support needs assessment conducted among all local<br />
practices.<br />
4
For more information<br />
If you would like any further information about <strong>QOF</strong>+, please contact:<br />
<br />
<br />
Josip Car<br />
Project Executive & Clinical Lead<br />
josip.car@hf-pct.nhs.uk<br />
Tel 020 3313 7175<br />
Miles Freeman<br />
Project Executive & Management lead<br />
miles.freeman@hf-pct.nhs.uk<br />
<br />
<br />
5
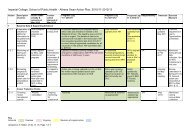
<strong>Summary</strong> of indicators<br />
Higher thresholds for existing clinical <strong>QOF</strong> indicators<br />
Practices will receive a fixed number of <strong>QOF</strong>+ points for reaching or exceeding each of two higher<br />
thresholds for the indicators detailed below. Point awards will be in addition to those allocated under<br />
<strong>QOF</strong> and based on attainment at close of business on March 31 2010.<br />
<strong>QOF</strong><br />
<strong>QOF</strong>+<br />
Indicator<br />
Upper Threshold<br />
Threshold<br />
(Tolerance) †<br />
Points<br />
ASTHMA 6. The percentage of patients with asthma who have had an<br />
asthma review in the previous 15mths<br />
BP 5. The percentage of patients with hypertension in whom the last blood<br />
pressure (measured in the previous 9 months) is ≤150/90<br />
CHD 6. The percentage of patients with coronary heart disease in whom the<br />
last blood pressure reading (measured in the previous 15 months) is<br />
≤150/90<br />
CHD 8. The percentage of patients with coronary heart disease whose last<br />
measured total cholesterol (measured in the previous 15 months) is<br />
≤5mmol/l<br />
CHD 10. The percentage of patients with coronary heart disease who are<br />
currently treated with a beta blocker (unless a contraindication or sideeffects<br />
are recorded)<br />
CS 1. The percentage of patients aged from 25 to 64 whose notes record<br />
that a cervical smear has been performed in the last five years<br />
DM 12. The percentage of patients with diabetes in whom the last blood<br />
pressure is ≤145/85<br />
DM 17. The percentage of patients with diabetes whose last measured total<br />
cholesterol within the previous 15 months is ≤5mmol/l<br />
DM 20. The percentage of patients with diabetes in whom the last HBA1c is<br />
7.5 or less in the previous 15 months<br />
MH 6. The percentage of patients on the register who have a<br />
comprehensive care plan documented in the records agreed between<br />
individuals, their family and/or carers as appropriate<br />
STROKE 6. The percentage of patients with a history of TIA or stroke in<br />
whom the last blood pressure reading (measured in the previous 15<br />
months) is ≤150/90 in the previous 15 months<br />
STROKE 8. The percentage of patients with a history of TIA or stroke in<br />
whom the last total cholesterol (measured in the previous 15 months) is 5<br />
mmol/l or less<br />
70% 95% (3%) 10<br />
70% 90% (2%) 29<br />
70% 98% (1%) 6<br />
70% 87% (2%) 7<br />
60% 87% (1%) 14<br />
80% 88% (7%) 35<br />
60% 86% (1%) 5<br />
70% 88% (1%) 9<br />
50% 77% (1%) 20<br />
50% 97% (1%) 3<br />
70% 96% (1%) 6<br />
60% 85% (1%) 5<br />
Under the current <strong>QOF</strong> 2009/10 proposal, DM20 will be replaced by DM23, which lowers the target for<br />
HbA1c to ≤7.0. We recognise that attaining this more aggressive target will require significant effort<br />
involving potentially large numbers of patients. To reward practices as they progress towards the revised<br />
goal, we propose to retain DM20 within <strong>QOF</strong>+ until the end of March 2010. Since DM20 attainment status<br />
will no longer be available through QMAS, feedback will instead be provided through the same<br />
mechanism of monthly reporting used for the new <strong>QOF</strong>+ clinical indicators.<br />
The introduction of a second, lower threshold aims only to address the concern that practices which<br />
missed the original single target by small absolute numbers of patients would receive no payment at all.<br />
This focus is why the gap between lower and upper thresholds is small in percentage terms.<br />
6
New <strong>QOF</strong>+ Indicators<br />
Point awards will be based on attainment at close of business on November 30 2009.<br />
Cardiovascular disease prevention<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
Payment<br />
stages<br />
+ CVD PREVENT 1. The percentage of patients on the Practice CVD At-Risk Register whose notes<br />
have a Blood Pressure recorded in the previous 17 months<br />
+ CVD PREVENT 2. The percentage of patients on the Practice CVD At-Risk Register whose notes<br />
have a record of BMI measured in the previous 17 months<br />
8 40-90%<br />
8 40-90%<br />
+ CVD PREVENT 3. The percentage of patients on the Practice CVD At-Risk Register whose notes<br />
have a baseline record of total and HDL cholesterol recorded in the previous 17 months<br />
8 40-90%<br />
+ CVD PREVENT 4. The percentage of patients on the Practice CVD At-Risk Register for whom there<br />
is a record of a fasting blood glucose in the previous 17 months<br />
+ CVD PREVENT 5. The percentage of patients on the Practice CVD At-Risk Register whose notes<br />
have a record of family history of CHD in first degree relatives (parents, brothers, sisters, or children<br />
of a patient)<br />
+ CVD PREVENT 6. The percentage of patients on the Practice CVD At-Risk Register whose notes<br />
have a record of family history of diabetes in first degree relatives (parents, brothers, sisters, or<br />
children of a patient)<br />
8 40-90%<br />
8 40-90%<br />
8 40-90%<br />
+ CVD PREVENT 7. The percentage of patients on the Practice CVD At-Risk Register who have been<br />
offered lifestyle advice on exercise, and appropriate dietary changes within the previous 17 months<br />
10 40-90%<br />
+ CVD PREVENT 8. The percentage of patients on the Practice CVD At-Risk Register who have been<br />
offered statin therapy (in line with 2008 NICE Guidance on Lipid Modification) as part of their<br />
primary prevention management strategy<br />
10 40-90%<br />
It is prerequisite that in order to receive payment for + CVD PREVENT 1, practices have achieved the<br />
existing <strong>QOF</strong> RECORDS 11 Indicator (The BP of patients aged 45 and over is recorded in the preceding 5<br />
years for at least 65% of patients.)<br />
Alcohol<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
Payment<br />
stages<br />
+ ALCOHOL 1. The percentage of patients on one or more practice registers for CVD At-Risk,<br />
Diabetes, Stroke and TIA, Hypertension and CHD who have had AUDIT-C or FAST recorded on the<br />
practice system within the previous 17 months<br />
15 20-70%<br />
+ ALCOHOL 2. The proportion of patients who screen positive using either AUDIT-C or FAST within<br />
the previous 17 months who are subsequently recorded as having a brief intervention for alcohol<br />
misuse<br />
30 40-90%<br />
It is prerequisite that in order to receive payment for + ALCOHOL 2, practices shall have reached the lower<br />
threshold for + ALCOHOL 1.<br />
7
Smoking<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
Payment<br />
stages<br />
+ SMOKING 1. The percentage of patients aged over 15 years whose notes record smoking status<br />
in the past 17 months, or whose most recent recorded smoking status, recorded over the age of<br />
25, indicated that they had never smoked<br />
20 40-90%<br />
+ SMOKING 2. The percentage of patients aged over 15 years who smoke whose notes contain a<br />
record that smoking cessation advice or referral to a local smoking cessation service has been<br />
offered within the previous 17 months<br />
10 40-90%<br />
Smoking in pregnancy<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
Payment<br />
stages<br />
+ SMOKING IN PREG 1. The percentage of pregnant women whose notes record their smoking<br />
status at the time of their first booking appointment in primary care<br />
+ SMOKING IN PREG 2. The percentage of pregnant women who smoke whose notes contain a<br />
record that at the time of their first antenatal booking appointment in primary care they have been<br />
given smoking cessation advice and details of the local NHS Stop Smoking Services and the NHS<br />
pregnancy smoking helpline (0800 169 9 169)<br />
3 70-90%<br />
5 70-90%<br />
Breastfeeding<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
Payment<br />
stages<br />
+ BREASTFEEDING 1. The percentage of women who are recorded as being pregnant on or after<br />
December 01 2008, and who at their antenatal booking appointment in primary care have been<br />
given specific information on breastfeeding, including information on breastfeeding workshops<br />
+ BREASTFEEDING 2. The percentage of babies born since December 01 2008 and breast fed at 6-8<br />
weeks whose record indicates that breastfeeding support contact has been offered to the babies’<br />
mother at the time of the 6-8 week check<br />
+ BREASTFEEDING 3. At least 80% of babies born since December 01 2008 have a record of feeding<br />
method at the time of the 6-8 week check<br />
4 70-90%<br />
6 70-90%<br />
3 -<br />
Ethnicity<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
Payment<br />
stages<br />
+ ETHNICITY 1. The percentage of patients on one or more practice registers for: CVD At-Risk,<br />
Hypertension, CHD, Diabetes, Mental Health and Stroke and TIA whose notes record their ethnicity<br />
and first language<br />
+ ETHNICITY 2. The percentage of patients who have newly registered with the practice from<br />
December 01 2008 whose notes record their ethnicity and first language<br />
30 60-90%<br />
20 90-100%<br />
8
Records<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
Payment<br />
stages<br />
+ PRESCRIPTION 1. The percentage of individual repeat medications issued which have a diagnosis<br />
in the electronic medical record relating to that medication<br />
+ REFERRALS 1. The percentage of outpatient referrals coded on clinical system with speciality and<br />
diagnosis recorded<br />
45 40-90%<br />
50 70-90%<br />
+ CARERS 1. Carer status is recorded for 100% of new registrations 6 -<br />
+ OSTEOARTHRITIS 1. The practice is able to produce a register of patients who have osteoarthritis 1 -<br />
+ RHEUMATOID ARTHRITIS 1. The practice is able to produce a register of patients who have<br />
rheumatoid arthritis<br />
1 -<br />
+ ECZEMA 1. The practice is able to produce a register of patients who have eczema 1 -<br />
+ PSORIASIS 1. The practice is able to produce a register of patients who have psoriasis 1 -<br />
New patient screening<br />
Indicator<br />
+ PATIENT REGISTRATION 1. The practice is trained in and implements the PCT TB Early Referral Protocol to identify<br />
and refer patients who are newly registered at the Practice and who are new entrants to the UK from countries with a<br />
high TB prevalence<br />
<strong>QOF</strong>+<br />
points<br />
5<br />
Patient information<br />
Indicator<br />
+ PATIENT INFORMATION 1. The practice uses the PCT practice information leaflet template for patients which is<br />
designed to include information on the following:<br />
Preventative services such as stop smoking, immunization and screening<br />
Choice / Choose & Book<br />
PCT’s Patient Advice & Liaison Service and complaints team<br />
Walk-in and urgent care centres<br />
Practice opening times including extended hours<br />
Information for patients in a range of languages informing them of their right to interpreting services during<br />
appointments<br />
+ PATIENT INFORMATION 2. The practice takes responsibility for regularly updating practice information on the NHS<br />
choices website<br />
+ PATIENT INFORMATION 3. The practice has up to date patient information about local training and support for self<br />
management (in the form of posters and leaflets) and that these are clearly displayed for patients in waiting areas<br />
<strong>QOF</strong>+ points<br />
3<br />
7<br />
3<br />
9
Patient experience<br />
Indicator<br />
<strong>QOF</strong>+<br />
points<br />
+ PATIENT EXPERIENCE 1. The practice takes part in the national patient satisfaction survey 3<br />
+ PATIENT EXPERIENCE 2. The practice takes part in a PCT-led feedback session based on the results of the national<br />
patient satisfaction survey and agrees an action plan including explicit and appropriate targets that can be used in the<br />
following 2 years to assess the extent to which the action plan is implemented<br />
+ PATIENT EXPERIENCE 3. The practice shares with patients the results and action plan from the national patient<br />
satisfaction survey. This should be through information leaflets and poster(s) in the practice’s waiting and reception<br />
area, and through the Practice’s Patient Participation Group where this exists<br />
+ PATIENT EXPERIENCE 4. The practice can show satisfactory objective evidence of implementing and achieving the<br />
action plan agreed with the PCT following the PCT-led feedback session based on the results of the national patient<br />
satisfaction survey. Deviations from the action plan must be described and explained<br />
+ PATIENT EXPERIENCE 5. The practice has a register of patients who need signing and interpreting support for<br />
appointments, including a record of first language spoken<br />
+ PATIENT EXPERIENCE 6. The practice offers double length appointments to patients identified as needing interpreting<br />
and signing support and to all patients on the learning disabilities register<br />
+ PATIENT EXPERIENCE 7. 100% of carers who are newly registered with the Practice on or after December 01 2008 have<br />
a record of being advised by the Practice that they can ask Social Services for an assessment of their own needs<br />
+ PATIENT EXPERIENCE 8. The practice has a system in place for taking the special needs of carers into account,<br />
including when allocating appointments and issuing prescriptions<br />
5<br />
10<br />
30<br />
5<br />
7<br />
5<br />
5<br />
+ PATIENT EXPERIENCE 9. A named carer is recorded for at least 90% of patients on the learning disability register 5<br />
+ PATIENT EXPERIENCE 10. The practice scores better than the national average on their patients’ response to question<br />
Q7 “Think about the last time you tried to see a doctor fairly quickly. Were you able to see a doctor on the same day or<br />
in the next two days the GP surgery or health centre was open?” posed as part of the 2008/09 national patient<br />
satisfaction survey<br />
+ PATIENT EXPERIENCE 11. The practice scores better than the national average on their patients’ response to question<br />
Q5a “In the past 6 months, how easy have you found getting through on the phone?” posed as part of the 2008/09<br />
national patient satisfaction survey<br />
20<br />
20<br />
Patient safety<br />
Indicator<br />
<strong>QOF</strong>+ points<br />
+ PATIENT SAFETY 1. The practice submits significant event analysis (SEA) summaries to an annual PCT audit 4<br />
+ PATIENT SAFETY 2. The practice can show evidence of reporting incidents or near misses involving harm/potential<br />
harm to patients via the national reporting and learning system (NRLS) using the standard e-reporting form<br />
+ PATIENT SAFETY 3. The practice has a system for ensuring that all practice staff have had CRB checks within the last<br />
three years<br />
+ PATIENT SAFETY 4. The practice has a system in place to assist, where appropriate, with the multi-agency referral<br />
process for investigations relating to the protection of children and vulnerable adults, including acknowledging any<br />
referrals or requests for information within 2 working days<br />
+ PATIENT SAFETY 5. The practice has a system in place for identifying vulnerable children, and this includes cases where<br />
a parent is known to be a substance misuser, has a severe mental health problem, or where there is domestic violence<br />
+ PATIENT SAFETY 6. The case conference notes of all children who are the subject of a Child Protection Plan are scanned<br />
into the child’s medical records<br />
+ PATIENT SAFETY 7. The practice has a system in place for ensuring that where a child has been the subject of a child<br />
protection plan, this is recorded as a Significant Active problem in the records of the child, the parents and other<br />
members of the household, and that this leads to effective flagging of records<br />
4<br />
5<br />
7<br />
8<br />
5<br />
5<br />
© Copyright NHS Hammersmith and Fulham 2009<br />
© Copyright eHealth Unit, Department of Primary Care and Social Medicine, <strong>Imperial</strong> <strong>College</strong> 2008<br />
10