To view the presentation in its entirety, please visit www.vinfen.org.
To view the presentation in its entirety, please visit www.vinfen.org.
To view the presentation in its entirety, please visit www.vinfen.org.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
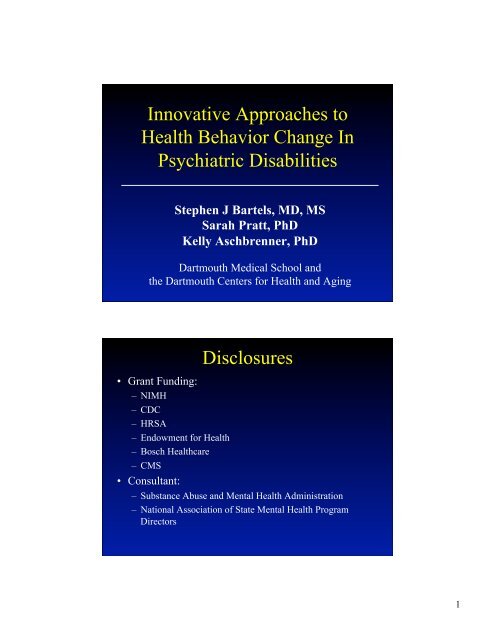
Innovative Approaches to<br />
Health Behavior Change In<br />
Psychiatric Disabilities<br />
Stephen J Bartels, MD, MS<br />
Sarah Pratt, PhD<br />
Kelly Aschbrenner, PhD<br />
Dartmouth Medical School and<br />
<strong>the</strong> Dartmouth Centers for Health and Ag<strong>in</strong>g<br />
• Grant Fund<strong>in</strong>g:<br />
– NIMH<br />
– CDC<br />
– HRSA<br />
– Endowment for Health<br />
– Bosch Healthcare<br />
– CMS<br />
• Consultant:<br />
Disclosures<br />
– Substance Abuse and Mental Health Adm<strong>in</strong>istration<br />
– National Association of State Mental Health Program<br />
Directors<br />
1
Over<strong>view</strong><br />
• The Context: High rates of medical<br />
comorbidity, early mortality, and nurs<strong>in</strong>g<br />
home placement for persons with SMI<br />
• Five research based <strong>in</strong>terventions and <strong>the</strong>ir<br />
potential applications<br />
• Putt<strong>in</strong>g it toge<strong>the</strong>r <strong>in</strong> <strong>the</strong> context of <strong>the</strong><br />
current health care environment<br />
Longevity: An American Success Story<br />
<strong>in</strong> Population Health?<br />
Life Expectancy At Birth<br />
In <strong>the</strong> year: Men Women<br />
1900 47.1 50.7 <br />
1990 71.8 78.8 <br />
2020 75.7 82.3 <br />
2050 79.7 85.6 <br />
Source: National Center for Health Statistics, U.S. Decennial Life Tables for<br />
1989-91, vol. 1, no. 3, Some Trends and Comparisons of United States Life<br />
Table Data: 1900-91. Hyattsville, MD; 1999, p. 2, Table A.<br />
2
Global Life Expectancy Disparities:<br />
Expl: US (79 yrs) vs. Ethiopia (55 yrs)<br />
Pop Quiz<br />
What large population group <strong>in</strong> <strong>the</strong> USA has <strong>the</strong> follow<strong>in</strong>g<br />
characteristics?<br />
• 25-30 year shorter life span than <strong>the</strong> general population<br />
• Similar life expectancy to people <strong>in</strong> Ethiopia<br />
• A decl<strong>in</strong><strong>in</strong>g life expectancy over <strong>the</strong> past 3 decades<br />
• Disproportionate risk of death from dramatically<br />
<strong>in</strong>creased preventable cardiometabolic risk factors<br />
• Substandard health care for common chronic illnesses<br />
• Presents a paradigm for a high-risk, disadvantaged<br />
cardiovascular health disparity population<br />
3
The Epidemic of Premature Death <strong>in</strong><br />
Middle-aged Persons with Mental Illness<br />
The average life expectancy <strong>in</strong> <strong>the</strong> US has steadily <strong>in</strong>creased<br />
to 77.9 years (<strong>in</strong>creas<strong>in</strong>g by almost 5 years s<strong>in</strong>ce <strong>the</strong> 90s alone)<br />
At <strong>the</strong> same time……….<br />
For people with serious mental illness:<br />
The average life expectancy is 53 yrs.<br />
50 is <strong>the</strong> New 75<br />
An Epidemic of Early Mortality:<br />
Mean Years of Potential Life Lost<br />
Year AZ MO OK RI TX UT<br />
1997 26.3 25.1 28.5<br />
1998 27.3 25.1 28.8 29.3<br />
1999 32.2 26.8 26.3 29.3 26.9<br />
2000 31.8 27.9 24.9<br />
Compared with <strong>the</strong> general population, persons with<br />
major mental illness lose 25-30 years of normal life span<br />
Colton CW, Manderscheid RW. Prev Chronic Dis [serial onl<strong>in</strong>e] 2006 Apr [date cited].<br />
Available at: URL:http://<strong>www</strong>.cdc.gov/pcd/issues/2006/apr/05_0180.htm<br />
4
Cardiovascular Disease Is Primary Cause<br />
of Death <strong>in</strong> Persons with Mental Illness*<br />
Percentage of deaths<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
MO OK RI TX UT VA<br />
Heart Disease Cancer Cerebrovascular<br />
Chronic Respiratory Accidents Diabetes<br />
Influenza/Pneumonia<br />
Suicide<br />
*Average data from 1996-2000.<br />
Colton CW, Manderscheid RW. Prev Chronic Dis [serial onl<strong>in</strong>e] 2006 Apr [date cited].<br />
Available at URL: http://<strong>www</strong>.cdc.gov/pcd/issues/2006/apr/05_0180.htm<br />
Cardiovascular Disease (CVD) Risk<br />
Factors<br />
Modifiable Risk<br />
Factors<br />
Estimated Prevalence and Relative Risk (RR)<br />
Schizophrenia<br />
Bipolar Disorder<br />
Obesity 45–55%, 1.5-2X RR 1 26% 5<br />
Smok<strong>in</strong>g 50–80%, 2-3X RR 2 55% 6<br />
Diabetes 10–14%, 2X RR 3 10% 7<br />
Hypertension ≥18% 4 15% 5<br />
Dyslipidemia Up to 5X RR 8<br />
1. Davidson S, et al. Aust N Z J Psychiatry. 2001;35:196-202. 2. Allison DB, et al. J Cl<strong>in</strong> Psychiatry. 1999; 60:215-220.<br />
3. Dixon L, et al. J Nerv Ment Dis. 1999;187:496-502. 4. Herran A, et al. Schizophr Res. 2000;41:373-381.<br />
5. MeElroy SL, et al. J Cl<strong>in</strong> Psychiatry. 2002;63:207-213. 6. Ucok A, et al. Psychiatry Cl<strong>in</strong> Neurosci. 2004;58:434-437.<br />
7. Cassidy F, et al. Am J Psychiatry. 1999;156:1417-1420. 8. Allebeck. Schizophr Bull. 1999;15(1)81-89.<br />
5
Mean Change <strong>in</strong> Weight With<br />
Antipsychotics<br />
Weight Change (kg)<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
-1<br />
-2<br />
-3<br />
Estimated Weight Change at 10 Weeks on “Standard” Dose<br />
13.2<br />
11.0<br />
†<br />
8.8<br />
6.6<br />
4.4<br />
*<br />
2.2<br />
0<br />
-2.2<br />
-4.4<br />
-6.6<br />
Weight Change (lb)<br />
*4–6 week pooled data (Marder SR et al. Schizophr Res. 2003;1;61:123-36; † 6-week data adapted from Allison DB,<br />
Mentore JL, Heo M, et al. Am J Psychiatry. 1999;156:1686-1696; Jones AM et al. ACNP; 1999.<br />
Receipt of Quality of Care Indicators<br />
100%<br />
80%<br />
60%<br />
40%<br />
20%<br />
37.0%<br />
50.1% 51.8%<br />
27.0%<br />
58.4%<br />
70.3%<br />
0%<br />
p
Early, Disproportionate, and<br />
Inappropriate Institutionalization<br />
<strong>in</strong> Nurs<strong>in</strong>g Homes<br />
Nurs<strong>in</strong>g Home Placement, Schizophrenia, and Age<br />
Overall Age 40-64 Age 65+<br />
.04/.14<br />
OR=1.9***<br />
95% CI=1.5-2.2<br />
OR=3.6***<br />
95% CI=2.8-4.7<br />
OR=1.1<br />
95% CI=0.8-1.4<br />
Andrews , 2009<br />
7
5 Models Integrat<strong>in</strong>g<br />
Rehabilitation, Health &<br />
Fitness Promotion, and Health<br />
Care Management<br />
I. Group-Based Rehabilitation and Health<br />
Care Management<br />
Help<strong>in</strong>g Older People Experience<br />
Success (HOPES)<br />
• Multi-site RCT (n=183, mean age 60) Mass<br />
Mental, NSMHA, Community Council of<br />
Nashua<br />
• Group Skills Tra<strong>in</strong><strong>in</strong>g Classes: Skills tra<strong>in</strong><strong>in</strong>g<br />
<strong>in</strong> community liv<strong>in</strong>g skills, social skills, and<br />
health self-management<br />
• Health Management: Health education,<br />
monitor<strong>in</strong>g, facilitation, & coord<strong>in</strong>ation of<br />
primary & preventive health by HM Nurse<br />
8
Curriculum:<br />
7 Skills Tra<strong>in</strong><strong>in</strong>g Modules<br />
1. Mak<strong>in</strong>g <strong>the</strong> Most of Leisure Time<br />
2. Communicat<strong>in</strong>g Effectively<br />
3. Us<strong>in</strong>g Medications Effectively<br />
4. Liv<strong>in</strong>g Independently <strong>in</strong> <strong>the</strong> Community<br />
5. Mak<strong>in</strong>g and Keep<strong>in</strong>g Friends<br />
6. Mak<strong>in</strong>g <strong>the</strong> Most of Health Care Vis<strong>its</strong><br />
7. Healthy Liv<strong>in</strong>g<br />
9
Nurse Health<br />
Care Management Component<br />
• Intake Assessment<br />
• Health exam<strong>in</strong>ation<br />
• Medication list<br />
• Vital signs monitor<strong>in</strong>g<br />
• Preventive health care<br />
• Disease specific goals<br />
• Action plan<br />
• Health care proxy<br />
• Health Education<br />
• Accompany <strong>visit</strong> to<br />
physician with<br />
consumer<br />
• Medical <strong>in</strong>formation<br />
communication<br />
• Monthly (or more<br />
frequent) vis<strong>its</strong><br />
11
Summary:<br />
Results 2 and 3 Year Follow-up<br />
• Improved Community Function<strong>in</strong>g<br />
• Decreased Negative Symptoms<br />
• Improved Self-efficacy<br />
• Improved Liv<strong>in</strong>g Skills<br />
• Greater Acquisition of Health Care<br />
Advance Directives<br />
• Greater Receipt of Preventive Health Care<br />
Screen<strong>in</strong>g<br />
Individually Tailored Rehabilitation<br />
HOPES-I<br />
• 5-Year Career Development Award from<br />
National Institute of Mental Health<br />
• Two sites: CMHCs <strong>in</strong> NH<br />
• Phase 1: Manual ref<strong>in</strong>ement<br />
• Phase 2: Feasibility with 8-10 people<br />
• Phase 3: Pre-Post Pilot with 40 receiv<strong>in</strong>g<br />
HOPES-I<br />
12
HOPES-I Content<br />
5 Skills Tra<strong>in</strong><strong>in</strong>g Modules<br />
1. Mak<strong>in</strong>g <strong>the</strong> Most of Leisure Time (6)<br />
2. Communicat<strong>in</strong>g Effectively (8)<br />
3. Liv<strong>in</strong>g Independently <strong>in</strong> <strong>the</strong> Community (8)<br />
4. Mak<strong>in</strong>g and Keep<strong>in</strong>g Friends (8)<br />
5. Healthy Liv<strong>in</strong>g (8)<br />
Applications for HOPES<br />
• HOPES as a potential core <strong>in</strong>tervention for<br />
community providers to address <strong>the</strong> ag<strong>in</strong>g<br />
population of adults (50+) with SMI<br />
currently resid<strong>in</strong>g <strong>in</strong> <strong>the</strong> community<br />
• Olmstead Mandate and ADA: HOPES as a<br />
model program to enable persons with SMI<br />
resid<strong>in</strong>g <strong>in</strong> nurs<strong>in</strong>g homes to be discharged<br />
back to <strong>the</strong> community<br />
13
II. Improv<strong>in</strong>g Primary Health Care<br />
Encounters for People with SMI<br />
Prepare, Ask, Communicate, Tell: P.A.C.T.<br />
• Feasibility trial of a brief <strong>in</strong>tervention to improve<br />
primary care encounters for older persons with SMI at<br />
cardiometabolic risk<br />
• Consumer tra<strong>in</strong><strong>in</strong>g (Peer Co-led)<br />
– Prepar<strong>in</strong>g to productively use <strong>the</strong> medical encounter<br />
– Strategies for communicat<strong>in</strong>g health <strong>in</strong>formation<br />
– Identify<strong>in</strong>g personal health targets<br />
– Use of tools to facilitate collaborative care plann<strong>in</strong>g<br />
14
P.A.C.T. Consumer Tra<strong>in</strong><strong>in</strong>g<br />
(90 m<strong>in</strong>ute session x 9 weeks)<br />
• Group based skills tra<strong>in</strong><strong>in</strong>g: Develop skills to<br />
communicate and use tools to facilitate self-advocacy<br />
dur<strong>in</strong>g <strong>visit</strong><br />
• Health Promotion Education: Learn to identify<br />
achievable lifestyle goals relat<strong>in</strong>g to smok<strong>in</strong>g cessation,<br />
exercise and nutrition, and resources for ongo<strong>in</strong>g support<br />
• Social Support Session: Tra<strong>in</strong><strong>in</strong>g for family members<br />
and significant o<strong>the</strong>rs to help navigate medical<br />
encounters, support health behavior change and healthy<br />
behaviors<br />
P.A.C.T. Physician Tra<strong>in</strong><strong>in</strong>g<br />
• Guidel<strong>in</strong>es for address<strong>in</strong>g<br />
cardiovascular risks <strong>in</strong> people with SMI<br />
• Patient centered communication skills<br />
• Collaborative goal identification<br />
15
Provider Tra<strong>in</strong><strong>in</strong>g<br />
(30 m<strong>in</strong>ute session)<br />
• Tra<strong>in</strong><strong>in</strong>g Video: Strategies for providers to<br />
improve communication, patient activation,<br />
and engage <strong>in</strong> shared decisions for prevention<br />
and treatment<br />
• Handout: ADA/APA guidel<strong>in</strong>es for screen<strong>in</strong>g<br />
and monitor<strong>in</strong>g of CVD risk <strong>in</strong> people with<br />
SMI. Evidence-based <strong>in</strong>terventions <strong>in</strong>clud<strong>in</strong>g<br />
obesity, tobacco use, hyperlipidemia,<br />
hypertension, and diabetes<br />
Consumer and Provider Tra<strong>in</strong><strong>in</strong>g Videos<br />
16
Application for P.A.C.T.<br />
• Support<strong>in</strong>g <strong>the</strong> “Person-Centered Medical<br />
Home” for persons with SMI<br />
• Enhanc<strong>in</strong>g behavioral activation, shared<br />
decision-mak<strong>in</strong>g <strong>in</strong> <strong>the</strong> primary care<br />
encounter and improved health behaviors<br />
• Prepar<strong>in</strong>g PCPs to support and enhance<br />
engagement and collaborative goal sett<strong>in</strong>g<br />
III. Integrated Illness Self-Management<br />
and Nurse Disease Management:<br />
Integrated Illness Management and<br />
Recovery(NIMH R34 MH074786)<br />
• Individualized <strong>in</strong>tegrated illness self-management<br />
skills tra<strong>in</strong><strong>in</strong>g provided by a Masters level cl<strong>in</strong>ician<br />
• Co-located medical disease management provided<br />
by a public health nurse <strong>in</strong> <strong>the</strong> community mental<br />
health center focus<strong>in</strong>g on metabolic/cardiovascular,<br />
and pulmonary disorders (hypertension,<br />
hyperlipidemia, congestive heart failure, diabetes,<br />
cardiovascular disease, and COPD)<br />
17
Integrated Illness Management<br />
and Recovery Sessions<br />
Weekly sessions aimed at:<br />
Establish<strong>in</strong>g goals steps towards recovery and<br />
wellness<br />
Increas<strong>in</strong>g knowledge through education of<br />
psychiatric and medical problems<br />
Enhanc<strong>in</strong>g self-management skills<br />
through skills tra<strong>in</strong><strong>in</strong>g, cognitive<br />
behavioral, and motivational<br />
<strong>in</strong>terventions.<br />
I-IMR Disease Management<br />
• Comprehensive <strong>in</strong>itial evaluation of health and<br />
receipt of preventive health services<br />
• Establishment of health care goals<br />
• Track<strong>in</strong>g & promotion of preventive health<br />
care, acute problems, chronic medical<br />
illnesses<br />
• Periodic assessment of health status<br />
• Health education and support for selfmanagement<br />
of medical problems<br />
18
Integrated Illness Management and<br />
Recovery<br />
IMR<br />
• Recovery<br />
• Psychoeducation<br />
• Stress and mental illness<br />
• Social Supports and MH<br />
• Psych Med Adherence<br />
• Psych Relapse Prevent<br />
• Psych Problem Solv<strong>in</strong>g<br />
• Cop<strong>in</strong>g with Psych Sx<br />
• Substance Abuse<br />
• Navigat<strong>in</strong>g <strong>the</strong> Mental Health<br />
System<br />
I-IMR<br />
• Wellness<br />
• Health education<br />
• Stress and health<br />
• Social supports and wellness<br />
• Medical med adherence<br />
• Medical relapse prevent<br />
• Medical problem solv<strong>in</strong>g<br />
• Cop<strong>in</strong>g with pa<strong>in</strong><br />
• Medication misuse<br />
• Navigat<strong>in</strong>g <strong>the</strong> Physical Health<br />
Care System<br />
Integrated Illness Management and Recovery (NIMH R34 MH074786)<br />
20
I-IMR Evaluation<br />
• NIMH R34 Pilot Study<br />
– RCT n=70 adults with SMI age 50+<br />
– 2 CMHCs <strong>in</strong> NH<br />
• Thresholds (Chicago) Pilot Study<br />
– RCT n=50 ethnically diverse adults<br />
with SMI age 50+<br />
Summary of Major F<strong>in</strong>d<strong>in</strong>gs<br />
Compar<strong>in</strong>g I-IMR and TAU<br />
• Client Rated Illness<br />
Self-Management:<br />
– Knowledge of Symptoms,<br />
Meds, Cop<strong>in</strong>g<br />
– Relapse Prevention Plann<strong>in</strong>g<br />
• Cl<strong>in</strong>ician Rated Illness<br />
Self-Management<br />
– Symptom Distress<br />
– Symptoms Affect<strong>in</strong>g<br />
Function<strong>in</strong>g<br />
• Trend for Stanford Chronic<br />
Disease Self-Management<br />
Scale<br />
• Trend for Greater Physical<br />
Activity<br />
• Trend for Better COPD Self<br />
Management<br />
21
Summary of Major F<strong>in</strong>d<strong>in</strong>gs<br />
Compar<strong>in</strong>g I-IMR and TAU<br />
Significant Differences for<br />
Primary Care Encounter:<br />
|<br />
• Trend- Greater Active Role<br />
Communicat<strong>in</strong>g Questions<br />
• Greater Information<br />
Seek<strong>in</strong>g<br />
Significant Difference for<br />
Psychiatric MD Encounter:<br />
• Information Seek<strong>in</strong>g<br />
• Trend: Less Decision<br />
Mak<strong>in</strong>g Autonomy<br />
Application for I-IMR<br />
• Integration with<strong>in</strong> programs of chronic<br />
disease self-management targettng <strong>the</strong><br />
highest cost, most complex <strong>in</strong>dividuals<br />
• A unique program of self-management and<br />
care management for BOTH SMI and<br />
chronic health conditions<br />
22
IV. Improv<strong>in</strong>g Health Care: Automated<br />
Remote Telemedic<strong>in</strong>e Disease Management<br />
Health Buddy ® : Electronic unit connected to a phone l<strong>in</strong>e<br />
provides two-way communication between healthcare<br />
providers and patients.<br />
Pilot study funded by<br />
Endowment for Health<br />
and Bosch Healthcare<br />
100 participants age 18+ with SMI plus CHF, COPD,<br />
Diabetes, or CAD) enrolled <strong>in</strong> 12 month RCT crossover<br />
design (HB v. wait list control)<br />
Automated Daily:<br />
- Self-monitor<strong>in</strong>g<br />
- Health Data Entry<br />
- Self-management<br />
Education<br />
- Remote DM<br />
Nurse Monitor<strong>in</strong>g<br />
23
Application for Health Buddy<br />
• Targeted home-based management and<br />
monitor<strong>in</strong>g of complex, co-occurr<strong>in</strong>g medical<br />
and mental health conditions.<br />
• For “unstable” high-risk <strong>in</strong>dividuals with<br />
recent emergency service use, hospitalizations,<br />
or o<strong>the</strong>r <strong>in</strong>dicators for daily prompt<strong>in</strong>g of self<br />
management and remote monitor<strong>in</strong>g.<br />
24
V. Prevention: Fitness Promotion<br />
In SHAPE: A Program with<br />
Several Components<br />
1. Individualized fitness and healthy lifestyle<br />
assessment<br />
2. Individual meet<strong>in</strong>gs (weekly) with a Health<br />
Mentor (certified fitness tra<strong>in</strong>er)<br />
3. Free membership to local fitness centers (YMCA;<br />
Dance-exercise center; Womens fitness center)<br />
4. Group Exercise and Healthy Eat<strong>in</strong>g Education<br />
5. Group health educational/motivational<br />
Celebrations<br />
The In SHAPE Health Mentor Program<br />
25
Dartmouth Center for Ag<strong>in</strong>g<br />
Research on In SHAPE<br />
1. Endowment for Health: Pilot Evaluation of a Fitness<br />
Promotion Intervention for People with SMI<br />
2. CDC: R01 DD000140 Promot<strong>in</strong>g Health & Function<strong>in</strong>g <strong>in</strong><br />
Persons with SMI<br />
3. NIMH: R01MH078052 Health Promotion and Fitness for<br />
Younger and Older Adults with SMI<br />
4. NIMH: R01MH089811 Statewide Intervention to Reduce<br />
Early Mortality <strong>in</strong> Persons With Mental Illness<br />
5. CMS: 1B1CMS330880 NH Medicaid Wellness Incentives<br />
Program (Medicaid Incentives for Prevention of Chronic<br />
Diseases)<br />
Bridg<strong>in</strong>g <strong>the</strong> Gap from Community<br />
to Research to Population Health<br />
Community<br />
Development<br />
Identification<br />
of Need,<br />
Community<br />
Coalition<br />
Development of<br />
In SHAPE<br />
Model<br />
Research<br />
Academic<br />
Research<br />
Partnership,<br />
1 st Pilot Study<br />
Effectiveness<br />
RCT Studies<br />
(CDC, NIMH)<br />
Implementation<br />
State Medicaid<br />
Policy Change<br />
Support<strong>in</strong>g<br />
Susta<strong>in</strong>ability<br />
Statewide<br />
Implementation<br />
and Evaluation<br />
26
Can <strong>in</strong>tegrated health promotion be<br />
implemented and susta<strong>in</strong>ed as a core service<br />
across an entire state system?<br />
• Statewide roll-out over 3 years <strong>in</strong>clud<strong>in</strong>g<br />
leadership, tra<strong>in</strong><strong>in</strong>g, technical support,<br />
and track<strong>in</strong>g of outcomes and costs<br />
• In SHAPE target<strong>in</strong>g patient health<br />
behaviors:<br />
Exercise, nutrition, smok<strong>in</strong>g cessation +<br />
• Academic Detail<strong>in</strong>g (AD) target<strong>in</strong>g<br />
physician screen<strong>in</strong>g and prescrib<strong>in</strong>g<br />
practices (NIMH R01, PI: Bartels)<br />
In SHAPE Implementation Study: ISIS<br />
• 5 year study funded by NIMH (12/1/09 – 11/30/14)<br />
• Evaluates phased-<strong>in</strong> implementation of In SHAPE +<br />
Academic Detail<strong>in</strong>g across 8 CMHCs <strong>in</strong> NH<br />
• Provides fund<strong>in</strong>g for .5FTE (Health Mentor or<br />
Program Coord<strong>in</strong>ator) for 15 months<br />
• Provides FREE In SHAPE tra<strong>in</strong><strong>in</strong>g and technical<br />
assistance<br />
• Primary Study Questions: Implementation Process,<br />
Effectiveness of In SHAPE, Cost<br />
27
Application for In SHAPE<br />
• Targeted Prevention of chronic health<br />
conditions and Wellness Health Promotion as<br />
an <strong>in</strong>tegrated component of service delivery<br />
• Prevention of chronic health conditions<br />
associated with obesity, sedentary lifestyle, and<br />
poor nutrition, <strong>in</strong>clud<strong>in</strong>g diabetes,<br />
hyperlipidemia, hypertension, cardiovascular,<br />
and cerebrovascular disease<br />
CMS Request for Proposals<br />
• Question: Can <strong>in</strong>centives help to<br />
prevent chronic diseases <strong>in</strong> at-risk<br />
Medicaid populations?<br />
28
NH Medicaid Wellness<br />
Incentives Program<br />
• $10 M for 5 year project<br />
• One of only 10 states funded<br />
• Three types of <strong>in</strong>centives:<br />
– Access to fitness facilities & activities<br />
– Transportation to reduce barriers to<br />
fitness<br />
– Rewards for healthy behaviors<br />
(attendance at fitness facilities, smok<strong>in</strong>g<br />
cessation programm<strong>in</strong>g, and smok<strong>in</strong>g<br />
abst<strong>in</strong>ence)<br />
Over<strong>view</strong> of WIP Program and<br />
Evaluation Design<br />
• Goal: Reduce cardiovascular risk <strong>in</strong><br />
smokers and overweight/obese consumers<br />
• 4 Weight Management and 3 Smok<strong>in</strong>g<br />
Cessation Programs offered at all 10<br />
CMHCs <strong>in</strong> NH<br />
• Enroll 2500 <strong>in</strong> WM and 200 <strong>in</strong> SC<br />
• Consumers can choose <strong>the</strong> programs <strong>in</strong><br />
which <strong>the</strong>y are will<strong>in</strong>g to participate<br />
29
Supported Fitness & Weight Management<br />
(age 18+, BMI>25, sedentary)<br />
Group 1: Group 2: Group 3: Group 4: <br />
Fitness Club <br />
In Shape + Weight <br />
In SHAPE Program Weight Watchers<br />
Membership<br />
Watchers<br />
1A: 2A: 3A: 4A: <br />
Same as 1A + <strong>in</strong>dividual Free membership <br />
Free gym mebership for up <br />
Same as groups 2A & <br />
sessions with fitness ($20/month) for up to <br />
to 24 months ($20/month)<br />
3A<br />
tra<strong>in</strong>er up to 24 months 24 months<br />
1B: 2B: 3B: 4B:<br />
Same as above + $5/each <br />
(up to $15/wk) for go<strong>in</strong>g to <br />
gym<br />
Same as above + <br />
$5/each (up to $15/wk) <br />
for go<strong>in</strong>g to gym w/out <br />
tra<strong>in</strong>er<br />
Same as above + $10 <br />
to attend one weekly <br />
meet<strong>in</strong>g<br />
Same as above plus <br />
rewards <strong>in</strong> Groups 2B <br />
&3B <br />
Supported Smok<strong>in</strong>g Cessation<br />
Programs<br />
Group 1: Group 2: Group 3: <br />
Prescriber Referral + <br />
Telephone CBT<br />
$15 for signed <br />
prescriber letter + $5/ea <br />
for 12 sessions <br />
Prescriber Referral + <br />
Facilitated Quitl<strong>in</strong>e<br />
Prescriber Referral Only<br />
1A: 2A: 3A: <br />
$15 for signed prescriber <br />
letter + $20/ea for 3 <br />
sessions <br />
$50 for signed prescriber <br />
letter<br />
1B: 2B: 3B: <br />
Extra rewards for 1 <br />
abst<strong>in</strong>ence attempt<br />
Extra rewards for 1 <br />
abst<strong>in</strong>ence attempt<br />
Extra rewards for 1 <br />
abst<strong>in</strong>ence attempt<br />
Rewards for Abst<strong>in</strong>ence: When participants quit, can come to IC<br />
MWF and earn $50/ea for abst<strong>in</strong>ence (CO
Putt<strong>in</strong>g it <strong>To</strong>ge<strong>the</strong>r<br />
• HOPES: Ag<strong>in</strong>g persons with SMI, Olmstead<br />
and Nurs<strong>in</strong>g Discharge & Diversion<br />
• P.A.C.T: Behavioral activation, shared goal<br />
sett<strong>in</strong>g, and <strong>the</strong> “medical home” for SMI<br />
• I-IMR: Integrated physical and mental health<br />
self-management<br />
• Health Buddy: High risk, high service users<br />
with SMI and unstable health conditions<br />
• In SHAPE: Prevention, <strong>in</strong>tegrated wellness<br />
health promotion<br />
Putt<strong>in</strong>g it <strong>To</strong>ge<strong>the</strong>r: From Prevention to<br />
Chronic Disease Management<br />
Underly<strong>in</strong>g<br />
Risk Factors<br />
Patient<br />
Symptoms & Life style<br />
Poor health behaviors<br />
Poverty, Un<strong>in</strong>surance<br />
Lack of self management<br />
Provider<br />
Lack of knowledge<br />
Compet<strong>in</strong>g demands<br />
Therapeutic nihilism<br />
System<br />
Limited onsite capacity<br />
Lack of medical home<br />
Lack of reimbursement<br />
for prevention & health<br />
promotion programs<br />
Adapted from Druss, 2007<br />
Proximal<br />
Risk Factors<br />
Lifestyle:<br />
Inactivity, poor<br />
diet, smok<strong>in</strong>g<br />
Medications<br />
Integrated Wellness:<br />
Diet, Exercise<br />
Smok<strong>in</strong>g Cessation<br />
Medication Switch<strong>in</strong>g<br />
Cardiometabolic<br />
Risk Factors<br />
↑ Weight<br />
Glucose<br />
↑ Lipids<br />
↑ BP<br />
Rout<strong>in</strong>e<br />
Health<br />
Screen<strong>in</strong>g<br />
Poor<br />
Quality<br />
Detection,<br />
Treatment<br />
CAD<br />
DM<br />
Integrated:<br />
Disease Mangmt.<br />
Care Management<br />
Self-Management<br />
31
Putt<strong>in</strong>g it <strong>To</strong>ge<strong>the</strong>r:<br />
The Context and Opportunity<br />
• The Demographic Imperative<br />
• CMMI and beyond: Dually Eligible and<br />
Long- term Care ACOs<br />
• Health Homes and Health Neighborhoods for<br />
Persons with SMI and Disabilities<br />
• CMS & ACA: Health Promotion and Prevention<br />
• Olmstead Decision, <strong>the</strong> ADA and CMS:<br />
Nurs<strong>in</strong>g home de<strong>in</strong>stitutionalization and diversion<br />
Potential New Research<br />
Opportunities<br />
• Use of smartphone and o<strong>the</strong>r technology for<br />
prompt<strong>in</strong>g, monitor<strong>in</strong>g, and support of wellness<br />
• Engag<strong>in</strong>g families and social networks for<br />
health behavior change<br />
• Peer led and peer supported <strong>in</strong>terventions<br />
• F<strong>in</strong>ancial <strong>in</strong>centives for health behavior change<br />
• Ethnically and culturally tailored health<br />
promotion and illness management <strong>in</strong>terventions<br />
32
The Health Promotion Research Team<br />
The Center for Ag<strong>in</strong>g Research<br />
33