Anthropometric Measurements
Anthropometric Measurements
Anthropometric Measurements
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
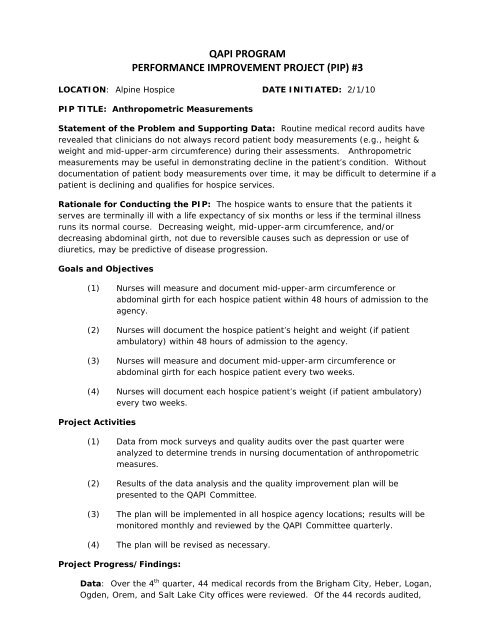
QAPI PROGRAM<br />
PERFORMANCE IMPROVEMENT PROJECT (PIP) #3<br />
LOCATION: Alpine Hospice DATE INITIATED: 2/1/10<br />
PIP TITLE: <strong>Anthropometric</strong> <strong>Measurements</strong><br />
Statement of the Problem and Supporting Data: Routine medical record audits have<br />
revealed that clinicians do not always record patient body measurements (e.g., height &<br />
weight and mid-upper-arm circumference) during their assessments. <strong>Anthropometric</strong><br />
measurements may be useful in demonstrating decline in the patient’s condition. Without<br />
documentation of patient body measurements over time, it may be difficult to determine if a<br />
patient is declining and qualifies for hospice services.<br />
Rationale for Conducting the PIP: The hospice wants to ensure that the patients it<br />
serves are terminally ill with a life expectancy of six months or less if the terminal illness<br />
runs its normal course. Decreasing weight, mid-upper-arm circumference, and/or<br />
decreasing abdominal girth, not due to reversible causes such as depression or use of<br />
diuretics, may be predictive of disease progression.<br />
Goals and Objectives<br />
(1) Nurses will measure and document mid-upper-arm circumference or<br />
abdominal girth for each hospice patient within 48 hours of admission to the<br />
agency.<br />
(2) Nurses will document the hospice patient’s height and weight (if patient<br />
ambulatory) within 48 hours of admission to the agency.<br />
(3) Nurses will measure and document mid-upper-arm circumference or<br />
abdominal girth for each hospice patient every two weeks.<br />
(4) Nurses will document each hospice patient’s weight (if patient ambulatory)<br />
every two weeks.<br />
Project Activities<br />
(1) Data from mock surveys and quality audits over the past quarter were<br />
analyzed to determine trends in nursing documentation of anthropometric<br />
measures.<br />
(2) Results of the data analysis and the quality improvement plan will be<br />
presented to the QAPI Committee.<br />
(3) The plan will be implemented in all hospice agency locations; results will be<br />
monitored monthly and reviewed by the QAPI Committee quarterly.<br />
(4) The plan will be revised as necessary.<br />
Project Progress/Findings:<br />
Data: Over the 4 th quarter, 44 medical records from the Brigham City, Heber, Logan,<br />
Ogden, Orem, and Salt Lake City offices were reviewed. Of the 44 records audited,
18% (8/44) contained nursing documentation of mid-upper-arm circumference within<br />
48 hours of admission to the agency, and 18% (8/44) contained documentation of the<br />
patient’s height and weight within 48 hours of admission.<br />
Plan for Improvement<br />
Threshold<br />
(1) The Clinical Director or designee from each office site will be responsible for<br />
collecting data related to the measuring and documenting of mid-upper-arm<br />
circumference or abdominal girth and height and weight on the nursing<br />
assessments.<br />
(2) The Clinical Director or designee will educate his/her nursing staff on the<br />
requirement for the routine measuring and documenting of anthropometric<br />
measurements.<br />
(3) The Quality Improvement Manager will provide in-service training to the<br />
Clinical Director or designee (i.e., auditor) on audit procedures and use of the<br />
audit tool.<br />
(4) The auditor will randomly select medical records to review each month. The<br />
quantity chosen will equal at least 25% of the office’s average daily census<br />
(ADC). For example, if the ADC for the previous month was 30, the auditor<br />
would review 8 medical records.<br />
(5) The auditor will submit completed audit tools to the Quality Improvement<br />
Manager by the 7 th day of the following month.<br />
(6) The Quality Improvement Manager will collect and analyze the data,<br />
observing for trends or patterns, and report findings and recommendations<br />
for improvement to the QAPI Committee each quarter.<br />
(7) The QAPI Committee will review findings and recommendations each quarter<br />
and revise the plan as needed to improve outcomes.<br />
(8) The Clinical Directors and Quality Improvement Manager will collaborate to<br />
ensure auditors and clinical staff members receive ongoing feedback on<br />
compliance findings and information on any revisions to the performance<br />
improvement plan.<br />
90% for all criteria<br />
Methodology<br />
Data Sources: Initial Nursing Assessment, Recertification Nursing Assessment, Nursing<br />
Progress Note<br />
Data Collection: Quality assurance audit tool<br />
Process: Clinical Record Review of 25% of average daily census (ADC)<br />
Frequency: Monthly